Abstract
This study aims to investigate the association between lipid accumulation product (LAP) levels and osteoarthritis (OA) in participants with normal BMI, and the potential role of the systemic inflammation response index (SIRI) in this association. Participants with normal BMI from the national health and nutrition examination survey (NHANES) database (2009–2018) were included. A weighted multivariable logistic regression was used to analyze the association between LAP levels and OA, and mediation analysis was applied to explore the role of SIRI in this relationship. Among 2408 participants with normal BMI, the average age was 43.85 ± 17.68 years, with 1240 (55%) women, and 210 (8.72%) participants recorded as having OA. Compared with the first quartile, the highest quartile of LAP levels was significantly associated with higher OA prevalence and higher SIRI levels [OA (AOR = 1.969, 95% CI 1.035–3.745, P = 0.039); SIRI (AOR = 1.174, 95% CI 1.029–1.489, P = 0.029)], especially in young women. Compared with the first quartile, the highest quartile of SIRI levels was significantly associated with higher OA prevalence [AOR = 1.542, 95% CI 1.010–2.356, P = 0.045], particularly in young women. The highest quartile of LAP levels was significantly associated with higher OA prevalence, with a portion of the association mediated by SIRI (10.30%), with mediation proportions of 8.92% in younger individuals and 8.69% in women. Even with normal BMI, high LAP levels are significantly associated with a higher prevalence of OA, with part of the association mediated by systemic inflammation, especially in young women.
Similar content being viewed by others
Introduction
Osteoarthritis (OA) is a chronic joint disease characterized primarily by joint dysfunction, pain, and stiffness1. As of 2020, over 500 million people worldwide are affected by OA, making it one of the leading causes of disability2. Currently, the treatment of OA is mainly surgical, with joint prostheses being the only effective option3. However, there are limitations to the longevity of joint prostheses4. Therefore, the prevention and management of OA have become crucial intervention strategies5. Obesity is a chronic metabolic disease characterized by a state of low-grade systemic inflammation. The lipid accumulation product (LAP) is a novel, sex-specific adiposity indicator based on waist circumference (WC) and triglyceride (TG) levels, used to reflect the accumulation of visceral fat and lipid metabolism abnormalities6.
The accumulation of visceral fat can lead to metabolic disturbances, which in turn promote a state of systemic inflammation in the body7. The systemic inflammation response index (SIRI) is a comprehensive index based on the Neutrophil, Monocyte, and Lymphocyte ratio, which provides a more holistic reflection of the body’s inflammatory and immune balance. Our previous studies have already confirmed a significant association between high SIRI levels and an increased risk of OA8.
This study aims to explore the association between LAP levels and OA risk in individuals with normal BMI in the United States, as well as the role of SIRI in this relationship.
Materials and methods
Study design and population
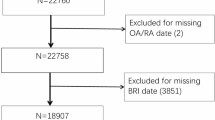
This study is based on data from the national health and nutrition examination survey (NHANES), including 49,693 participants from the years 2009 to 2018. NHANES is a rigorous, complex, and multi-stage probability sampling study, and all participants provided informed consent and received approval from the NCHS Institutional Review Board. According to the inclusion and exclusion criteria, the final cohort of this study included 2408 U.S. adults with a normal BMI (Fig. 1).
Exposure and outcome
LAP
The calculation of LAP differs by gender, as follows:
(1) LAP (Male) = [WC (cm)−65] × TG (mmol/L).
(2) LAP (Female) = [WC (cm)−58] × TG (mmol/L).
SIRI
In this study, the calculation formula for SIRI9 = [(neutrophil count × monocyte count)/lymphocyte count], The team found that SIRI did not follow a normal distribution and therefore applied a log2 transformation (Fig. S1).
Waist-height ratio (WHtR)
Classification is made in accordance with the standards proposed by the European Congress on Obesity (CEO, 2019: http://ecoico2020.com/) and NICE (NICE, 2023: https://www.nice.org.uk/guidance/cg189): normal (< 0.5), central obesity (≥ 0.5).
Self-reported OA
In this study, the inclusion of OA and Non-OA participants was based on the self-reported OA status in the survey questionnaire10. Specific questions related to OA status are provided in (Table S1).
Covariates
The covariates included in this study were selected based on their association with OA and previous similar studies. These covariates encompass a range of demographic and health-related variables11. Detailed information on the covariates and their groupings can be found in (Table S2).
Statistical analysis
This study utilized the NHANES database. Due to the complexity of NHANES’ sampling design, the sample weights for participants from 2009–2018 were applied in accordance with NHANES analysis and reporting guidelines to ensure national representativeness. Data analysis for this study was performed using R software (version 4.2.1) and Empower Stats (version 2.0).
Continuous variables in the baseline data are presented as means ± standard deviations, and categorical variables are presented as frequencies (percentages). Differences in characteristics between the OA and Non-OA groups were evaluated using Student’s t-test for continuous variables and chi-square test for categorical variables. The geometric mean and 95% confidence intervals (CI) for LAP, SIRI, and OA were reported. Survey-weighted linear regression was used for continuous variables, while survey-weighted chi-square tests were used for categorical variables to compare baseline characteristics.
Prior to analysis, the team identified that SIRI was not normally distributed, so a log2 transformation was applied. To ensure uniformity, LAP was also standardized. Three different statistical models were used: Model 1 (unadjusted), Model 2 (adjusted for age, gender, and race), and Model 3 (adjusted for age, gender, race, education level, smoking, drinking, hypertension, and diabetes). Additionally, to further assess whether there is a dose-response relationship between LAP-z (LAP-z refers to the standardized LAP variable, which was derived by applying z-score transformation to the raw LAP values) and OA prevalence across the three models, LAP-z was modeled as both a continuous variable (with logarithmic transformation) and as categorical based on tertiles, exploring the relationship between LAP-z and OA prevalence.
Mediation analysis
To assess whether systemic inflammation (measured by the systemic inflammation response index, SIRI) mediated the association between lipid accumulation product (LAP) and osteoarthritis (OA), we conducted a formal mediation analysis using a counterfactual-based approach. The analysis was performed in accordance with the causal inference framework developed by VanderWeele and implemented using the mediation package in R. We specified LAP as the independent variable (exposure), OA as the binary dependent variable (outcome), and SIRI as the mediator. All continuous variables were standardized (Z-transformed) prior to modeling to facilitate interpretability and model convergence. The natural direct effect (NDE), natural indirect effect (NIE), and total effect (TE) were estimated through nonparametric bootstrapping with 1,000 iterations to obtain robust confidence intervals. The mediation proportion was calculated as NIE/TE × 100%, representing the proportion of the total effect of LAP on OA that is mediated by SIRI.
All mediation models were adjusted for potential confounders including age, sex, race/ethnicity, education level, smoking status, alcohol use, hypertension, and diabetes. We also performed stratified mediation analyses by age (< 60 vs ≥ 60 years) and sex to assess effect modification.
All statistical tests were two-tailed, with a significance level set at P < 0.05.
Result
Basic characteristics of participants
Table 1 presents data from 2408 participants aged ≥ 20 years with a normal BMI. The mean age was (43.9 ± 17.7) years, with 1,240 (55%) females. Among these, 210 (8.72%) participants were diagnosed with osteoarthritis (OA). Compared to the first tertile, participants in the highest tertile of LAP levels were generally older, more likely to be male, less educated, and predominantly Non-Hispanic White. Additionally, they were more likely to have been diagnosed with hypertension and diabetes. These participants also had a higher likelihood of smoking, excessive alcohol consumption, and higher BMI and WHtR indices.
Association between high LAP levels and increased OA prevalence
Figure 2 shows that, after performing weighted multivariable regression analysis, participants in the highest tertile of LAP levels had a significantly higher risk of OA compared to those in the first tertile (AOR = 1.969, 95% CI 1.035–3.745, P = 0.039), particularly among younger women (Tables S3,4).
Association between high LAP levels and elevated SIRI levels
Figure 3 shows that, after performing weighted multivariable regression analysis, participants in the highest tertile of LAP levels had significantly higher SIRI levels compared to those in the first tertile (AOR 1.174, 95% CI 1.029–1.489, P = 0.029), particularly among younger women (Table S5).
Association between high SIRI levels and elevated OA prevalence
Figure 4 demonstrates that, after conducting weighted multivariable regression analysis, participants in the highest tertile of SIRI levels had a significantly higher prevalence of OA compared to those in the first tertile (AOR 1.542, 95% CI 1.010–2.356, P = 0.045), particularly among younger women (Table S6).
Mediation analysis
Figure 5 shows that, after conducting weighted multivariable regression analysis, participants in the highest tertile of LAP levels had a significantly higher prevalence of OA compared to those in the first tertile. Part of this association (10.30%) was mediated by SIRI, with mediation proportions of 8.92% in younger individuals and 8.69% in women (Fig. S2).
Discussion
In this study, a total of 2,408 participants were included, comprising 1,240 females and 1,168 males, with 210 (8.72%) participants reporting OA. Compared to the first tertile, participants in the highest tertile of LAP levels had a significantly higher prevalence of both OA and SIRI levels [OA (AOR 1.969, 95% CI 1.035–3.745, P = 0.039); SIRI (AOR 1.174, 95% CI 1.029–1.489, P = 0.029)]. Additionally, compared to the first tertile, participants in the highest tertile of SIRI levels had a significantly higher prevalence of OA [AOR = 1.542, 95% CI 1.010–2.356, P = 0.045]. Furthermore, the association between the highest tertile of LAP levels and a higher OA prevalence was partly mediated by SIRI (10.30%).
To date, this study is the first to use the NHANES database to analyze the association between LAP, SIRI, and the prevalence of OA. OA is a degenerative joint disease characterized by cartilage degeneration, osteophyte formation, narrowing of the joint space, and degenerative inflammation, which are the key pathological mechanisms of OA12. It is well-established that factors such as gender, age, obesity, and inflammation are closely related to the development of OA13. Unlike the irreversible nature of age and gender, obesity is a controllable environmental factor. Obesity is a risk factor for a variety of diseases, and with the increasing prevalence of obesity, the correlation between obesity and OA has gained more attention14. It is widely accepted that excess adipose tissue in obese patients increases biomechanical stress on weight-bearing joints, leading to friction and overload. When the physiological load on the cartilage exceeds normal limits, cartilage damage may occur. Additionally, biomechanical factors can also affect the receptors on the cartilage surface, triggering a cascade of growth factors, cytokines, matrix metalloproteinases, and signaling proteins, further promoting the development of OA. However, biomechanical factors alone cannot explain OA in non-weight-bearing joints15. With the advancement of molecular biology, it has become increasingly clear that adipose tissue is not only an energy storage and supply organ but also the largest endocrine organ in the body. Through endocrine, paracrine, and autocrine mechanisms, adipose tissue secretes a variety of adipokines, inflammatory mediators, and signaling proteins that participate in the pathogenesis of OA. Therefore, excess adipose tissue in obese patients has become a risk factor for the development and progression of OA16. LAP, a novel adipose tissue function indicator based on WC and TG levels, and gender, is used to estimate fat accumulation and distribution6. Unlike LDL-C, which shows limited sensitivity to visceral fat dysfunction, TG levels rise early in metabolic syndrome and better reflect ectopic lipid storage17. LAP was therefore intentionally constructed using WC and TG to capture visceral adiposity and lipid metabolic abnormalities in a clinically simple yet pathophysiologically relevant manner. LAP provides a good representation of the body’s lipid storage status and has demonstrated better recognition and predictive abilities for cardiovascular diseases and other health conditions in clinical settings18.
Immune inflammation plays a crucial role in the onset and progression of OA, making the control of inflammatory responses important for both the prevention and treatment of OA. Inflammatory cytokines contribute to the pathogenesis of OA by disrupting the balance between catabolic and anabolic processes in joint tissues. When this balance is disturbed, it leads to the progressive degradation of articular cartilage, which plays a key biomechanical role in the joints, ultimately resulting in the gradual loss of joint function and pain19. C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are the most commonly used laboratory markers of systemic inflammatory diseases, and they are elevated in inflammatory joint diseases such as rheumatoid arthritis (RA). OA was once considered a non-inflammatory joint disease, with inflammatory serum markers like CRP not elevated in OA20. However, recent studies have shown that high-sensitivity CRP (hs-CRP) and ESR are elevated in OA patients and are closely associated with disease progression and prognosis21.
In recent years, the SIRI has emerged as a novel marker of systemic inflammation, and its predictive value for disease prognosis has been demonstrated in various types of cancer. SIRI is calculated as (neutrophil count × monocyte count)/lymphocyte count, integrating both pro-inflammatory (neutrophils and monocytes) and anti-inflammatory (lymphocytes) components to reflect the balance between immune activation and suppression. Originally proposed in oncology22, SIRI has since been widely recognized in metabolic and inflammatory diseases for its superior capacity to characterize systemic immune-inflammatory states compared to single markers like CRP or NLR. In contrast to CRP-which may remain normal in low-grade inflammation-SIRI captures broader immune dysregulation, making it particularly relevant for OA8, where chronic, subclinical inflammation plays a key pathogenic role. Moreover, SIRI is derived from routine blood counts, offering a practical, low-cost, and scalable biomarker for epidemiologic studies. In this context, our findings support the clinical utility of SIRI in linking visceral adiposity to joint degeneration, highlighting its potential as a mechanistic mediator and early warning tool for OA in populations with normal BMI but hidden metabolic risk.
However, no studies have reported on the relationship between SIRI and OA. In this study, we found that SIRI follows a right-skewed non-normal distribution, and therefore, log transformation was applied before data analysis. The results show that SIRI reflects the systemic inflammation levels in OA patients and has been proven to be a strong predictor of disease activity, joint damage, and radiographic progression. Higher SIRI values were significantly associated with an increased risk of OA, worse disease activity, and poor prognosis. Moreover, the observed associations between higher lipid accumulation product (LAP), elevated systemic inflammation response index (SIRI), and increased OA prevalence remained robust in subgroup analyses, particularly among younger individuals and women. This finding suggests that early metabolic and inflammatory disturbances may contribute to OA risk even before the conventional age threshold. Furthermore, among the 2,408 included participants, 1,240 (55%) were women. The more pronounced associations in females-especially those under age 60-raise the possibility that menopausal transition may play a role. Although the NHANES dataset lacks direct indicators of menopausal status, it is well documented that estrogen decline during menopause may exacerbate adiposity, systemic inflammation, and cartilage degeneration. Therefore, hormonal factors could plausibly influence the relationship between LAP, SIRI, and OA in women. Wang et al. found that excessive obesity leads to inflammatory responses, oxidative stress, and mitochondrial dysfunction23. In this study, mediation analysis revealed that part of the association between LAP and OA was mediated by SIRI, with a mediation proportion of 10.30% (P < 0.001). This suggests that even in individuals with a normal BMI, high LAP levels are associated with an increased risk of OA, and part of this association is mediated by systemic inflammation.
This study has several notable strengths. First, it leveraged data from NHANES, a large, nationally representative survey with a rigorous multi-stage probability sampling design, which enhances the reliability and generalizability of the findings. Second, by focusing specifically on individuals with normal BMI, the study uniquely isolates the impact of visceral adiposity and systemic inflammation on osteoarthritis (OA) risk, highlighting associations that may be overlooked when relying solely on BMI. Third, the use of mediation analysis offers mechanistic insight, demonstrating that systemic inflammation, as measured by SIRI, partially mediates the relationship between lipid accumulation (LAP) and OA. However, several limitations should be noted. Due to the observational and cross-sectional nature of NHANES, causal relationships between LAP, SIRI, and OA cannot be established, and longitudinal studies are needed to validate the temporal and causal pathways of the observed associations. Additionally, OA diagnosis was based on self-reported survey data rather than clinical or radiographic confirmation, which may lead to recall bias and diagnostic misclassification, particularly for early-stage or asymptomatic cases. Furthermore, as illustrated in Fig. 1, only 2,408 out of 28,833 eligible participants (8.4%) were included in the final analysis due to missing data on key anthropometric, biochemical, and inflammatory markers. Although these exclusions were essential to ensure analytic rigor and internal validity for multivariable-adjusted and mediation models, the substantial reduction in sample size may introduce potential selection bias and limit generalizability.
Conclusion
This study provides new insights into the relationship between LAP, SIRI, and OA risk in U.S. adults with normal BMI. High levels of LAP are associated with a higher likelihood of OA, with part of this association mediated by systemic inflammation. Therefore, clinical screening, monitoring, and health education focused on LAP levels could be an important public health strategy for adults with normal BMI. The study also observed age- and gender-related differences, suggesting that prevention and intervention strategies for OA should be tailored for younger individuals and women.
Data availability
All data analyzed during this study are available online (https://www.cdc.gov/nchs/nhanes/index.htm).
Abbreviations
- OA:
-
Osteoarthritis
- NHANES:
-
National health and nutrition examination survey
- LAP:
-
Lipid accumulation product
- SIRI:
-
Systemic inflammation response index
- WC:
-
Waist circumference
- TG:
-
Triglyceride
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
- RA:
-
Rheumatoid arthritis
- hs-CRP:
-
High-sensitivity CRP
References
Wang, Y. et al. Methotrexate to treat hand osteoarthritis with synovitis (METHODS): an Australian, multisite, parallel-group, double-blind, randomised, placebo-controlled trial. Lancet 402 (10414), 1764–1772 (2023).
Hunter, D. J., March, L. & Chew, M. Osteoarthritis in 2020 and beyond: a lancet commission. Lancet 396 (10264), 1711–1712 (2020).
Heijman, M. W. J. et al. Association of low-dose colchicine with incidence of knee and hip replacements: Exploratory analyses from a randomized, controlled double-blind trial. Ann. Intern. Med. 176 (6), 737–742 (2023).
Damsted, C. et al. Effect of exercise therapy versus surgery on mechanical symptoms in young patients with a meniscal tear: a secondary analysis of the DREAM trial. Br. J. Sports Med. 57 (9), 521–527 (2023).
Ma, X. et al. Excessive intake of sugar: An accomplice of inflammation. Front. Immunol. 13, 988481 (2022).
Qiao, T. et al. Association between abdominal obesity indices and risk of cardiovascular events in Chinese populations with type 2 diabetes: a prospective cohort study. Cardiovasc. Diabetol. 21 (1), 225 (2022).
Kolb, H. Obese visceral fat tissue inflammation: from protective to detrimental?. BMC Med. 20 (1), 494 (2022).
He, Q., Wang, Z., Mei, J., Xie, C. & Sun, X. Relationship between systemic immune-inflammation index and osteoarthritis: a cross-sectional study from the NHANES 2005–2018. Front. Med. (Lausanne) 11, 1433846 (2024).
Cheng, W. et al. Higher systemic immune-inflammation index and systemic inflammation response index levels are associated with stroke prevalence in the asthmatic population: a cross-sectional analysis of the NHANES 1999–2018. Front. Immunol. 14, 1191130 (2023).
Centers for Disease Control and Prevention. The NHANES 2017–2018 Anthropometry Procedures Manual. (accessed 9 April 2021); https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/manuals.aspx?BeginYear=2017
European and International Congress on Obesity, ECO-ICO. (accessed 9 April 2021); http://ecoico2020.com/
Hanly, R. J. et al. The outcome of cemented acetabular components in total hip arthroplasty for osteoarthritis defines a proficiency threshold: Results of 22,956 cases from the australian orthopaedic association national joint replacement registry. J. Arthroplasty. 34 (8), 1711–1717 (2019).
Katz, J. N., Arant, K. R. & Loeser, R. F. Diagnosis and treatment of hip and knee osteoarthritis: A review. JAMA 325 (6), 568–578 (2021).
Messier, S. P. et al. Effect of diet and exercise on knee pain in patients with osteoarthritis and overweight or obesity: A randomized clinical trial. JAMA 328 (22), 2242–2251 (2022).
Batushansky, A. et al. Fundamentals of OA. An initiative of osteoarthritis and cartilage. Obesity and metabolic factors in OA. Osteoarthr. Cartil. 30 (4), 501–515 (2022).
Kolasinski, S. L. et al. 2019 American college of rheumatology/arthritis foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthr. Rheumatol. 72 (2), 220–233 (2020).
Kirkpatrick, C. F. et al. Nutrition interventions for adults with dyslipidemia: A clinical perspective from the national lipid association. J. Clin. Lipidol. 17 (4), 428–451 (2023).
Shi, Y. et al. Relationship between the lipid accumulation product index and arterial stiffness in the Chinese population with hypertension: A report from the China H-type hypertension registry study. Front. Cardiovasc. Med. 8, 760361 (2021).
Bai, X. et al. Chondrocyte targeting gold nanoparticles protect growth plate against inflammatory damage by maintaining cartilage balance. Mater. Today Bio. 23, 100795 (2023).
Salis, Z. & Sainsbury, A. Association between change in body mass index and knee and hip replacements: A survival analysis of seven to ten years using multicohort data. Arthr. Care Res. (Hoboken) 75 (6), 1340–1350 (2023).
Wen, L. et al. The value of high-sensitivity C-reactive protein in hand and knee radiographic osteoarthritis: data from the Dong-gu study. Clin. Rheumatol. 37 (4), 1099–1106 (2018).
Zhang, S. & Cheng, T. Prognostic and clinicopathological value of systemic inflammation response index (SIRI) in patients with breast cancer: a meta-analysis. Ann. Med. 56 (1), 2337729 (2024).
Wang, L. et al. The association between overweight and obesity on bone mineral density in 12 to 15 years old adolescents in China. Med. (Baltimore) 100 (32), e26872 (2021).
Funding
This research was funded by Jiangsu Province Science and Technology Plan (No. SBE2021740210).
Author information
Authors and Affiliations
Contributions
Q.H designed and conducted the research; J.M collected and analyzed data; Q.H, D.Z contributed to visualization; Q.H and J.M revised the figures and manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The NHANES program was approved by the National Center for Health Statistics (NCHS) Ethics Review Board and all participants signed an informed consent form.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, D., Mei, J. & He, Q. Systemic inflammation partially mediates the association between lipid accumulation and osteoarthritis in normal BMI adults. Sci Rep 15, 21301 (2025). https://doi.org/10.1038/s41598-025-06249-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-06249-6