Abstract
Three- and four-part proximal humeral fractures are common in young and elderly populations. Open reduction and fixation with a locking plate is a commonly used surgical technique; however, it is associated with a high incidence of complications. This study aimed to retrospectively evaluate the clinical effectiveness of open reduction and fixation with a locking plate for treating three- and four-part proximal humeral fractures and to analyze potential risk factors for complications. The clinical data of 126 patients with three-part (57 cases) or four-part (69 cases) fractures of the proximal humerus who presented to our center between January 2014 and January 2024 were selected. At the final follow-up (i.e., 12 months post-operation), the postoperative clinical efficacy was evaluated by comparing the Constant-Murley score, Disabilities of the Arm, Shoulder and Hand (DASH) score, Visual Analog Scale (VAS) score, and range of motion (ROM) of the shoulder joint between the affected side and the unaffected side. Additionally, the relationships between the clinical efficacy and the loss angle of the humeral neck-shaft angle (NSA) as well as the loss humeral head height (HHH) were analyzed. In addition, we also analyzed the most common complications among the patients and the associated risk factors. In the evaluation of clinical efficacy, there were no significant differences in the ROM of the shoulder joint and clinical scores between the unaffected side and the affected side of the patients at 12 months postoperatively (P > 0.05). The analysis of the relationship between the clinical efficacy, the loss angle of the NSA, and the loss of HHH showed that for patients with proximal humerus fractures (PHF), there was a significant negative correlation between the postoperative flexion, abduction, external rotation, and internal rotation of the shoulder joint on the affected side, the Constant score, and both the loss angle of the postoperative neck-shaft angle and the height of the humeral head, while there was a positive correlation with the Disabilities of the Arm, Shoulder, and Hand (DASH) score. In the analysis of complications, it was found that the incidence rates of shoulder joint stiffness and internal fixation failure were significantly higher than that of humeral head necrosis. Their occurrences were highly correlated with factors such as age, diabetes, osteoporosis, fracture healing time, rotator cuff repair, rehabilitation methods, medial cortical bone defect, calcar screw, calcar distance, calcar ratio, reduction quality, and so on. In conclusion, in clinical practice, surgical strategies should be tailored to individual patient profiles, incorporating comprehensive preoperative assessments of age, comorbidities (e.g., osteoporosis, diabetes), and fracture morphology. Optimization of surgical precision (e.g., anatomical reduction, calcar screw placement) and adherence to evidence-based postoperative rehabilitation protocols are critical to mitigate risks of complications and maximize therapeutic efficacy.
Similar content being viewed by others
Introduction
Proximal humerus fracture (PHF) is a common injury among the elderly population, accounting for 5–6% of all types of fractures1. With the increase of the aging population, the prevalence of proximal humerus fractures is also continuously rising2. Complex proximal humerus fractures (three-part or four-part fractures), either due to comminuted fractures, significant displacement, and severe soft tissue injuries, or due to poor bone quality, rotator cuff degeneration, etc., pose great challenges during the treatment process. They often have poor prognosis and a high disability rate, bringing a relatively heavy burden to patients and society3.
Complex proximal humeral fractures mainly consist of three-part or four-part fractures. For patients with surgical contraindications, conservative treatment is the main approach, which is mainly applicable to patients with relatively good fracture stability (such as slight displacement and an intact soft tissue hinge), those whose overall physical condition cannot tolerate the risks of surgery, and patients with low functional requirements (such as the elderly or those with a sedentary lifestyle). The reduction can be maintained by using a brace and combined with rehabilitation training, and individualized treatment can be carried out according to the different conditions of patients. However, for those without surgical contraindications, surgical treatment represents the optimal method to improve the prognosis and enhance functional recovery. The major surgical approaches for complex proximal humerus fractures include open reduction locking plates, closed reduction intramedullary nailing, and shoulder arthroplasty2. Closed reduction intramedullary nailing is mainly applicable to surgical neck fractures or fracture types accompanied by fracture lines extending into the humeral shaft. It has the advantages of minimal invasion and biomechanics4. However, for complex proximal humerus fractures, closed reduction has the disadvantages of being difficult to achieve anatomical reduction of the fractures, involving complex surgical procedures, providing unreliable fixation of the fracture fragments, and causing damage to the rotator cuff5. Shoulder arthroplasty includes hemiarthroplasty and reverse shoulder arthroplasty, which are mainly applicable to elderly patients with four-part fractures, a high risk of humeral head necrosis, or severe osteoporosis. For patients with intact rotator cuff function, hemiarthroplasty is preferred, while reverse shoulder arthroplasty is mainly adopted for elderly patients with complex proximal humerus fractures and rotator cuff insufficiency6,7. However, with the increase in the number of cases and the delay in follow-up time, complications after reverse shoulder arthroplasty, such as acromion fractures, scapular neck impingement, infection, glenohumeral joint dislocation, and other complications, are attracting the attention of clinicians8.
The emergence of locking plates has changed the concept of fracture treatment and improved the treatment outcomes of fractures. The Proximal Humerus Internal Locking System (PHILOS) locking pate is mainly applicable to three-part or four-part fractures (such as displacement in multiple locations including the greater tuberosity, lesser tuberosity, and surgical neck) and is especially suitable for patients with osteoporotic fractures. The angular stability between the screws and the plate increases the stability between the fracture fragments and the neck-shaft angle. At the same time, the anatomical design can assist in the anatomical reduction of the fracture. For complex proximal humerus fractures, it can also achieve anatomical reduction and firm fixation, preserve the integrity of the autologous tissues, and restore good function simultaneously. Therefore, the Proximal Humerus Internal Locking System is one of the earliest and most widely used treatment methods for proximal humerus fractures in clinical practice9. However, the extensive application of the Proximal Humerus Internal Locking System in the treatment of proximal humerus fractures has also led to a relatively large number of complications, such as internal fixation failure, postoperative shoulder joint stiffness, humeral head necrosis, etc., which severely affect the prognosis of patients10. However, there have been few reports in previous articles on which specific clinical intervention measures can reduce complications.
The study proposes to solve the following problems: (1) to assess the clinical efficacy of locking plates in the treatment of three- and four-part fractures of the proximal humerus; and (2) to analyze the most common postoperative complications and associated risk factors.
Patients and methods
General information
This study was approved by the Ethics Committee of the General Hospital of Ningxia Medical University (KYLL-2024-1460). A total of 527 patients with humeral fractures who were treated at our center from January 2014 to January 2024 were selected. Among them, there were 153 cases of distal humeral fractures (i.e., fractures in the supracondylar and intercondylar regions of the humerus), 176 cases of humeral shaft fractures (fractures between 1 and 2 cm below the surgical neck of the humerus and 2 cm above the humeral condyle), and 198 cases of proximal humeral fractures. Among the 135 patients who met the inclusion and exclusion criteria of this study, 3 patients refused to participate in the study, and 6 patients were lost to follow-up during the one-year follow-up period. The remaining 126 patients were included in this study, and their postoperative conditions were analyzed (Fig. 1). None of all the patients had shoulder joint dislocation or neurovascular injury. All of them voluntarily participated in this study and signed the informed consent form.
Inclusion and exclusion criteria
Inclusion criteria: (1) The proximal humerus fracture was diagnosed clinically; (2) Fresh closed fractures resulting from trauma; (3) Neer typed it as types III and IV; (4) Surgical approach using locking plate internal fixation; (5) Preoperative bone density testing; (6) Postoperative compliance was high, with a follow-up period of not less than 12 months; (7) The contralateral shoulder has no history of trauma or degenerative joint disease.
Exclusion Criteria: (1) Open, multiple fractures; (2) Pathologic fracture; (3) Missing patients or those with missing follow-up information; (4) Those who show severe damage to other organs that affect joint function scores and joint function exercises; (5) Combined nerve and blood vessel injury.
Team composition and preoperative assessment
Our center is composed of a team of 9 chief physicians. Each surgeon has more than 15 years of experience in trauma surgery, and all surgeons adopt a unified protocol for surgery, reduction, and postoperative management. All the patients treated by these 9 chief physicians from January 2014 to January 2024 were included in this study. Through the inclusion and exclusion criteria of this study, 126 patients who finally met the criteria were screened out to participate in the study.
-
(1)
Preoperatively, all the 9 surgeons determined based on the CT images that the bone mass or volume available for fixation within the humeral head was sufficient and selected an appropriate Proximal Humerus Internal Locking System (PHILOS) locking plate (DePub Synthes, Oberdorf, Switzerland).
-
(2)
Through imaging examinations such as X-ray and CT, it is determined whether there is a medial cortical bone defect. For patients with medial cortical bone defects (such as comminution of the medial column and discontinuity in the Calcar region) or those with a varus tendency of the humeral head (the head-shaft angle < 120°) after reduction, a humeral calcar screw is inserted. Before the operation, the bone condition in the Calcar area, the type of fracture, the degree of displacement, etc., were precisely measured to determine the appropriate length, diameter, and implantation angle of the Calcar screws (Fig. 2).
Radiographic measurements of a representative patient. (a) The humeral head height (HHH) was defined as the distance between uppermost edge of the plate and the uppermost part of the humeral head; (b) The humeral neck-shaft angle (NSA) was defined as the angle between a line that is perpendicular to the articular segment or atomic neck of the humerus and a line that bisects the humeral shaft; (c) Tip distance is defined as the distance from the calcar screw to the articular surface of the humeral head. (d) The calcar distance refers to the distance from the calcar screw to the calcar.
Surgical method
All patients underwent either “brachial plexus anesthesia” or “general anesthesia” and were positioned in the “beach chair position” with the affected shoulder elevated. A standardized “deltopectoral approach” was employed for surgical access. The incision began “2 cm above the coracoid process,” extended over the coracoid, and followed the groove between the deltoid and pectoralis major muscles, creating a “10–15 cm curvilinear incision.” After incising the skin and subcutaneous tissue, the fracture fragments were exposed, and hematomas or fragmented bone debris were meticulously removed. The fracture fragments were reduced anatomically and fixed using a “proximal humeral locking plate system (PHILOS).” For greater tuberosity (GT) and lesser tuberosity (LT) fragments, reduction was achieved using #2 Ethibond sutures for traction combined with point-to-point reduction forceps to ensure anatomical alignment. For patients with medial cortical defects, a calcar screw (typically a 6.5–7.0 mm cancellous bone screw) was inserted into the medial proximal humerus (calcar region). The screw head was positioned flush with or slightly below the cortical surface. During screw placement, the trajectory was aligned with the calcar axis and maintained at an angle of “30°–45° relative to the humeral shaft” to optimize fixation stability. Fluoroscopic imaging (C-arm) confirmed satisfactory fracture reduction and hardware placement. After ensuring stable fixation, the surgical site was irrigated thoroughly. A “drainage tube” was routinely placed, and the wound was closed in layers. Postoperatively, the affected limb was immobilized with a “triangular sling,” and “prophylactic antibiotics” were administered to all patients to prevent infection.
Postoperative management
In the early postoperative period (1 to 2 weeks), patients are mainly guided to perform active flexion and extension activities of the fingers and wrist joints, as well as isometric contraction exercises of the upper limb muscles. In the middle postoperative period (2 to 6 weeks), passive movement training of the shoulder joint is gradually increased, such as pendulum exercises, assisted abduction, and forward flexion exercises. In the late postoperative period (after 6 weeks), the active range of motion and strength training items of the shoulder joint are steadily increased to gradually restore the normal function of the shoulder joint.
Data collection
-
(1)
General information: gender, age, fracture type, smoking history, history of diabetes mellitus, osteoporosis, and whether standardized rehabilitation, remedial rehabilitation, or self-directed rehabilitation exercises were carried out after the operation.
-
(2)
Indicators related to the operation: the time from injury to operation, the operation time, the intraoperative blood loss, the postoperative drainage volume, the fracture healing time, and whether the rotator cuff was strengthened and repaired during the operation.
-
(3)
Indicators related to imaging: whether the medial cortical bone was intact, whether a humeral calcar screw was inserted, the intraoperative distance of the humeral calcar (that is, the distance from the humeral calcar screw to the humeral calcar), the humeral calcar ratio (that is, the ratio of the distance from the humeral calcar to the lower screw to the diameter of the humeral head), the distance from the head end (that is, the distance from the lower screw to the articular surface of the humeral head), and the reduction quality.
Observation indicators
-
(1)
During the operation, record the NSA and the HHH. When conducting an outpatient follow-up 12 months after the operation, recheck the X-ray films. Measure the NSA and HHH on the anteroposterior view of the shoulder joint, and calculate the angle loss of the NSA and the height loss of the HHH from the time of the operation to 12 months after the operation.
-
(2)
Twelve months after the operation, evaluate the fracture healing situation through X-ray films; record the Constant-Murley scores, DASH scores, and VAS pain scores of the affected side and the healthy side of the patients, as well as the angles of shoulder joint flexion, abduction, external rotation, and internal rotation, and compare the range of motion of the shoulder joints and the clinical scores between the affected side and the healthy side.
-
(3)
Record the situation of postoperative complications.
Evaluation criteria
-
(1)
Start counting the postoperative drainage volume on the day of the operation, and remove the drainage tube until the drainage volume is less than 30 ml within 24 h.
-
(2)
Osteoporosis: The age is ≥ 65 years old; in bone mineral density testing, a T value ≤ -2.5 is defined as osteoporosis. For patients with osteoporosis, anti-osteoporosis treatment is immediately administered upon admission.
-
(3)
Formal rehabilitation exercises: Start to receive rehabilitation exercises guided by professional rehabilitation therapists two weeks after the operation.
-
(4)
Remedial rehabilitation exercises: Begin to receive rehabilitation exercises guided by professional rehabilitation therapists two months after the operation.
-
(5)
Self-directed rehabilitation exercises: Conduct active rehabilitation exercises on one’s own without the guidance of professional rehabilitation therapists after the operation.
-
(6)
Reduction quality: Medial head-shaft displacement of < 5 mm, greater tuberosity cranialization of < 5 mm, and varus or valgus angulation of 120°–150° were considered. If all 3 criteria were met, the fracture was considered adequately reduced; otherwise, it is considered a poor reduction11.
-
(7)
Failure of internal fixation: Change in NSA > 5° or change in HHH > 3 mm determines internal fixation failure12.
-
(8)
Bone union: The disappearance of the fracture line and the presence of trabecular bridging on plain X-ray films are used to determine that the fracture has healed.
-
(9)
Shoulder joint stiffness13,14,15,16: Core criteria: (a) Measurement of the range of motion (ROM): external rotation < 30°, abduction < 90°; (b) Imaging examination: X-ray/MRI excludes osteoarthritis and rotator cuff injury. Auxiliary criteria: Constant-Murley score < 70 and Disabilities of the Arm, Shoulder, and Hand (DASH) score > 30.
Statistical methods
The statistical software packages SPSS 22.0 and R 4.3.1 were used to analyze the data. The Shapiro-Wilk test was employed to verify the normal distribution of the data. Continuous variables conforming to the normal distribution were expressed as mean ± standard deviation (\(\overline {{\text{x}}}\) ± s); variables that did not follow a normal distribution were expressed as the median M (p25, p75); categorical variables were presented as frequencies and percentages. For continuous data conforming to the normal distribution, an independent samples t-test was used, and for data that did not follow a normal distribution, a nonparametric rank sum test was applied; for categorical variables, a chi-square test was used (expected frequency ≥ 5). In the analysis of clinical efficacy, since the data were not normally distributed, the Kruskal-Wallis test and Spearman correlation analysis were adopted. In the analysis of complications, first, univariate logistic regression (P < 0.05) was used to screen for potential risk factors. Second, the screened variables were included in the multivariate logistic regression to calculate the odds ratio (OR) and 95% confidence interval. Next, the goodness-of-fit of the model was evaluated by the Hosmer-Lemeshow test and the receiver operating characteristic (ROC) curve. Finally, a Least Absolute Shrinkage and Selection Operator (LASSO) regression model was established, and its robustness was evaluated by cross-validation and the bootstrap method. A P value < 0.05 was considered to indicate a statistically significant difference.
Results
General statistics
Among the 126 patients who were treated with locking plates for proximal humerus three and four part fractures, the mean age was 63.40 ± 11.75, of which 51 were male, 75 were female, 57 were Neer type III, 69 were Neer type IV, 45 were smokers, 30 patients with a history of previous diabetes mellitus, 41 were osteoporotic, 49 accepted formal rehabilitation, 30 remedial rehabilitation, and self-directed rehabilitation 47 cases (Table 1).
Analysis of the efficacy of post-operative shoulder joint function in patients with PHF
At the last follow-up, the analysis of the postoperative efficacy in patients with PHF showed that there were no statistically significant differences in the range of motion of the affected shoulder joint and the clinical scores between the affected shoulder joint and the unaffected shoulder joint after the operation (P > 0.05). This indicates that the PHILOS locking plate treatment has a good therapeutic effect on complex proximal humeral fractures (Table 2).
Correlation analysis between shoulder function and postoperative imaging at the final postoperative follow-up in patients with PHF
Spearson’s correlation analysis showed that the angle of postoperative NSA loss (difference between NSA at 12 months postoperatively and intraoperative NSA) and HHH loss (difference between HHH at 12 months postoperatively and intraoperative HHH) in patients with PHF showed a significant negative correlation with shoulder flexion, abduction, external rotation, internal rotation, and Constant scores, and positive correlation with DASH scores and VAS scores (Table 3).
Significance analysis between shoulder function and rehabilitation method at the final postoperative follow-up in patients with PHF
The Kruskal-Wallis test analysis showed that there was a statistically significant difference between postoperative shoulder function and the choice of rehabilitation modality in patients with PHF (P < 0.05). The shoulder joint function of patients who received formal rehabilitation exercise was better than that of patients with remedial rehabilitation and self-rehabilitation, with the shoulder joint function of patients receiving remedial rehabilitation being better than those practicing self-rehabilitation (Table 4).
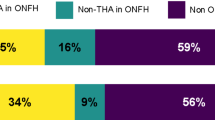
Complications
During the 1-year postoperative follow-up period, the statistical results of complications showed that there were 11 cases of internal fixation failure (5 cases of Neer type III and 6 cases of Neer type IV), with an incidence rate of 8.73%; 3 cases of necrosis of the humeral head (1 case of Neer type III and 2 cases of Neer type IV), with an incidence rate of 2.38%; and 13 cases of stiffness of the shoulder joint (5 cases of Neer type III and 8 cases of Neer type IV), with an incidence rate of 10.32% (Table 5).
Univariate analysis of complications
Univariate comparisons showed that gender, typing, smoking, time from injury to surgery, time to surgery, intraoperative bleeding, postoperative drainage, and tip distance were not statistically significantly associated with the development of complications (P > 0.05), whereas age, diabetes mellitus, osteoporosis, fracture healing time, medial cortical bone defect, calcar distance, calcar ratio, restoration quality, and rehabilitation method were risk factors for the occurrence of complications, the difference was statistically significant (P < 0.05) (Table 6).
Comparison of the correlation analysis between postoperative complications and various indicators
Correlation analysis showed that complications were positively correlated with age, diabetes mellitus, osteoporosis, fracture healing time, calcar distance, calcar ratio, medial cortical bone defect, and self-directed rehabilitation; and negatively correlated with rotator cuff repair, calcar screw, reduction quality, and formal rehabilitation; and did not correlate with remedial rehabilitation (Table 7).
Logistic multifactorial logistic regression analysis of postoperative complications and various indicators
In the correlation analysis, the correlation between calcar distance, calcar ratio, and complications was particularly significant, and both were excluded from inclusion in the multifactorial analysis in order to avoid effects on other variables in the multifactorial analysis; furthermore, remedial rehabilitation showed no correlation with complications, and therefore remedial rehabilitation was also excluded from inclusion in the multifactorial analysis.
Multifactorial logistic regression showed that age, diabetes mellitus, osteoporosis, fracture healing time, formal rehabilitation, self-directed rehabilitation, rotator cuff repair, calcar screws, medial cortical bone defect, and reduction quality were independent risk factors for the occurrence of complications (Table 8).
The goodness-of-fit of the model was evaluated by the Hosmer-Lemeshow test and the receiver operating characteristic (ROC) curve
In the Hosmer-Lemeshow test, the chi-square (χ²) value was 2.86, the degrees of freedom (df) was 8, and the P-value was 0.943 (P > 0.05). Moreover, the area under the ROC curve of each variable was greater than 0.5, which indicates that the model has a good goodness-of-fit (Figs. 3, 4 and 5)
Receiver operating characteristic (ROC) curves of clinical parameters for outcome prediction. Caption: The figure presents the diagnostic performance of clinical parameters in predicting postoperative outcomes. The y-axis denotes sensitivity (%), and the x-axis represents “100 − Specificity (%)”, illustrating the trade-off between true positive and false positive rates across classification thresholds.
Receiver operating characteristic (ROC) curves for predicting outcomes in the surgical index group. The figure evaluates the diagnostic performance of two key parameters in predicting postoperative outcomes within the surgical index group. The y-axis represents sensitivity (%), and the x-axis represents “100 − Specificity (%)”, reflecting the trade-off between true positive and false positive rates across classification thresholds.
Receiver operating characteristic (ROC) curves of radiographic parameters. The figure illustrates the diagnostic performance of radiographic parameters in predicting postoperative complications. The y-axis represents sensitivity (%), and the x-axis shows “100 − Specificity (%)”, reflecting classification efficacy across varying thresholds.
LASSO regression analysis
The LASSO regression showed that age, osteoporosis, diabetes, fracture healing time, calcar screws, rotator cuff repair, reduction quality, medial cortical bone loss, standardized rehabilitation, and self-directed rehabilitation were the predictive factors for the risk of postoperative complications. The model achieved a balance between variable selection and predictive performance and was verified for its robustness (Tables 9 and 10; Figs. 6 and 7).
Variable selection and model performance across regularization parameters. The left y-axis (bars) represents the number of retained variables, and the right y-axis (line) indicates the binomial deviance. The x-axis shows the regularization intensity (Log(λ)). As Log(λ) increases from − 9 (weak regularization) to -2 (strong regularization), the number of variables decreases from 18 to 0, while the binomial deviance declines from 1.4 to 0.6. The vertical dashed line marks the optimal λ value (Log(λ) = − 4) selected by 10-fold cross-validation, retaining 9 variables with a deviance of 0.8. This balance minimizes overfitting while preserving predictive accuracy.
Discussion
Currently, the clinical treatment of complex proximal humerus fractures is mainly based on PHILOS locking plate internal fixation as the gold standard of treatment17. However, the efficacy of PHILOS locking plate for the treatment of proximal humerus three- and four-part fractures and the incidence of postoperative complications are still subject to considerable controversy18. The study was conducted by evaluating the efficacy of using PHILOS locking plates for the treatment of proximal humerus fractures of the third and fourth parts of the humerus and the risk factors associated with complications.
In terms of clinical efficacy, the results of the last follow-up showed that there were no significant statistical differences in the range of motion of the affected shoulder joint and the clinical scores between the affected shoulder joint and the unaffected shoulder joint (P > 0.05). This indicates that the PHILOS locking plate treatment has good clinical efficacy for complex proximal humeral fractures. Rongfeng Sheet et al.19 showed in the results of a study that during the follow-up at 12 months after the operation, the Constant-Murley score of the affected shoulder joint was 87.58 points and the Visual Analogue Scale (VAS) score was 0 point, which was basically consistent with the results of this study. Gracitelli et al.20 reported in a prospective study that for the treatment of proximal humeral fractures (excluding four-part fractures) with locking plates, at 12 months after the operation, the average Constant-Murley score of the affected shoulder joint was 71.5 points, the DASH score was 14.3 points, and the VAS score was 1.3 points. There were differences compared with the results of this study. There may be many factors accounting for these differences, such as age, the absence of the four-part fracture type, underlying diseases, etc. Plathe et al.17 reported in a prospective randomized controlled trial that at the last follow-up, the flexion angle during the active movement of the affected shoulder joint was 127° and the abduction angle was 122°, which was similar to the results of this study. However, this experiment did not count the external rotation and internal rotation angles of the shoulder joint. In addition, the efficacy analysis in this study showed that the patients’ postoperative shoulder functional outcome had a high correlation with postoperative NSA loss angle and HHH loss; the greater the angle of NSA loss, the greater the HHH loss, and the worse the shoulder functional outcome, which was consistent with the results reported by Lei Zhao et al.12 in a study. Meanwhile, this study also found that the rehabilitation method had a significant effect on the functional outcome of the shoulder joint, and the postoperative shoulder joint autonomy and mobility of patients who chose formal rehabilitation were significantly better than those who received remedial rehabilitation and self-directed rehabilitation, and those who received remedial rehabilitation were better than those who received self-directed rehabilitation. Therefore, we believe that patients receiving as much formal rehabilitation as possible in the postoperative period contributes to improved functional outcomes of the shoulder. It should be noted that in this study, there was no control set for the affected shoulder joint at 3 months, 6 months, 12 months, etc. after surgery, and there was a potential bias due to the lack of a concurrent randomized control group. However, by comparing the affected shoulder joint with the healthy side and integrating relevant literature data, the efficacy of the PHILOS plate in the treatment of three- and four-part fractures of the proximal humerus was effectively highlighted.
In the analysis of complications, this study found that the incidence of internal fixation failure was 8.73%, AVN was 2.38%, and postoperative shoulder stiffness was 10.32% in 126 patients, for a total incidence of 21.43%. The incidence of complications in the treatment of proximal humerus fractures with PHILOS locking plates has been reported in the literature to vary from 17.8–35.7%21,22,23, with the incidence of internal fixation failure ranging from 0–23%24,25,26, which is consistent with the results of this study. The incidence of AVN has also been reported in the literature to range from 6–34%9,27, which differs from the results of this article. Martetschlager et al.28 reported that compared with the deltoid split approach, the deltopectoral approach involves a wider range of tissues, and it is prone to damaging the branches of the anterior circumflex artery (an important source of blood supply to the humeral head). Moreover, the surgical trauma is relatively greater, which is likely to trigger a stronger inflammatory response. This may interfere with the local blood circulation, resulting in a higher incidence of humeral head necrosis in patients. In this study, the deltopectoral approach was adopted without being compared with the deltoid split approach, which is one of the limitations of this study. In addition, it has also been reported in the literature29,30,31 that the placement of calcar screws may increase the risk of AVN, and the use of bone cement to enhance the stability of PHILOS locking plates has been shown in the data to have favorable clinical outcomes with a decrease in the complication rate.
In this study, patients were categorized into complication and no complication groups by the presence or absence of postoperative complications, and in univariate analysis and Spearson correlation analysis, it was concluded that: age, diabetes mellitus, osteoporosis, formal rehabilitation, self-directed rehabilitation, fracture healing time, rotator cuff repair, calcar screw, calcar distance, calcar ratio, medial cortical bone defect, and the restoration quality were associated with the occurrence of complications, and the difference was statistically significant (p < 0.05). In order to control for confounding factors interfering with the results of the study, a logistic multifactorial analysis was performed, which showed that the above indicators were independent risk factors for complications. In addition, in this study, the goodness-of-fit of the model was evaluated through the Hosmer-Lemeshow test and the ROC curve. The results showed that the χ² value of the model was 2.86, the df was 8, and the P-value was 0.943 (P > 0.05). Moreover, the area under the ROC curve of each variable was greater than 0.5, indicating that the model had a good goodness-of-fit. Finally, a LASSO regression model was established in this study, and its robustness was evaluated by means of cross-validation and the bootstrap method. The results showed that the model achieved a balance between variable selection and predictive performance, and it had good robustness.
Analyze the risk factors: As the patients’ age increases, the healing time of the fracture ends prolongs, thus leading to an increased risk of complications. When patients have osteoporosis, this leads to poorer screw and plate holding power and susceptibility to internal fixation failure21,32. Similarly, diabetic patients can affect the blood supply at the fracture break, leading to necrosis of the humeral head or prolonging the fracture healing time33 and easily increasing the risk of complications. Formal rehabilitation patients under the guidance of a professional rehabilitator are able to effectively exercise their shoulder joint function and avoid complications caused by inappropriate exercise times or modalities. And the strengthening repair of rotator cuff helps the functional recovery of shoulder joint and the stabilization of humeral head, and reduces the occurrence of postoperative complications, which is of great significance in the treatment of PHF34. The medial cortex is the weight-bearing structure of the proximal humerus, and its deficiency may easily lead to inversion and collapse of the humeral head, whereas the calcar screw can effectively fixate the calcar area, so that the fracture end can be stabilized and prevented from being displaced when multiple forces are applied3,35. In addition, this study found significant differences in calcar distance and calcar ratio between the complication group and the no-complication group (20.45 mm vs. 7.68 mm, 33.36% vs. 19.85%, P < 0.05). Padegimas et al.11 reported in a study that controlling for calcar distance < 12 mm and calcar ratio < 25% was the optimal position for calcar screw placement, and this finding is consistent with the results of this study.
Conclusion
The application of PHILOS locking plates in the treatment of three- and four-part proximal humeral fractures demonstrates distinct clinical advantages, including improved postoperative shoulder mobility, enhanced functional recovery of self-care capacity, and a reduced incidence of complications (e.g., avascular necrosis, implant failure). In clinical practice, surgical strategies should be tailored to individual patient profiles, incorporating comprehensive preoperative assessments of age, comorbidities (e.g., osteoporosis, diabetes), and fracture morphology. Optimization of surgical precision (e.g., anatomical reduction, calcar screw placement) and adherence to evidence-based postoperative rehabilitation protocols are critical to mitigate risks of complications and maximize therapeutic efficacy.
Limitations
First, the sample size of this study is relatively small, and it is a single-center study. Some of the data may contain subjective factors from the respondents, which may lead to information bias in the statistical analysis. Second, this study has time limitations, making it impossible to conduct longer-term or more in-depth observations and analyses. Then, this study only analyzed the efficacy of anatomical locking plates in the treatment of proximal humerus fractures and did not compare it with other surgical methods (such as intramedullary nail techniques or shoulder arthroplasty), resulting in a lack of diversity in the research findings. After that, although all surgeries followed standardized protocols, the involvement of nine surgeons has introduced potential variability in technical operations (such as surgical skills, instrument preferences, etc.), and these factors may have an impact on treatment outcomes such as the complication rate and functional recovery. Finally, this study did not collect and analyze the relevant data on the drug treatment situation of diabetic patients and their long-term blood glucose levels and failed to further analyze the impact of diabetes on fracture healing.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PHF:
-
Proximal humerus fracture
- ROM:
-
Range of motion
- CT:
-
Computerized tomography
- DASH:
-
Disabilities of the arm, shoulder and hand
- VAS:
-
Visual analogue scale
- PHILOS:
-
Proximal humerus anatomical locking plates
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under curve
- NSA:
-
Humeral neck-shaft angle
- HHH:
-
Humeral head height
- AVN:
-
Avascular necrosis of the humeral head
- df:
-
Degrees of freedom
- GT:
-
Greater tuberosity
- LT:
-
Lesser tuberosity
References
Rangan, A. et al. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: the PROFHER randomized clinical trial. JAMA 313, 1037–1047 (2015).
Klug, A., Gramlich, Y., Wincheringer, D., Schmidt-Horlohé, K. & Hoffmann, R. Trends in surgical management of proximal humeral fractures in adults: a nationwide study of records in Germany from 2007 to 2016. Arch. Orthop. Trauma. Surg. 139, 1713–1721 (2019).
Laux, C. J., Grubhofer, F., Werner, C. M. L., Simmen, H. P. & Osterhoff, G. Current concepts in locking plate fixation of proximal humerus fractures. J. Orthop. Surg. 12, 137 (2017).
Sears, B. W., Hatzidakis, A. M. & Johnston, P. S. Intramedullary fixation for proximal humeral fractures. J. Am. Acad. Orthop. Surg. 28, e374–e383 (2020).
Fakler, J. K. M., Hogan, C., Heyde, C. E. & John, T. Current concepts in the treatment of proximal humeral fractures. Orthopedics 31, 42–51 (2008).
Khair, M. M., Dines, J. S. & Dines, D. M. Shoulder arthroplasty: return to sport. Sports Health. 7, 87–89 (2015).
Mauch, F. & Huth, J. Revision of anatomic shoulder arthroplasty. Orthopadie Heidelb Ger. 52, 137–143 (2023).
Boileau, P. Complications and revision of reverse total shoulder arthroplasty. Orthop. Traumatol. Surg. Res. 102, S33–S43 (2016).
Sproul, R. C., Iyengar, J. J., Devcic, Z. & Feeley, B. T. A systematic review of locking plate fixation of proximal humerus fractures. Injury 42, 408–413 (2011).
Ranson, R. et al. No change in outcome ten years following locking plate repair of displaced proximal humerus fractures. Eur. J. Orthop. Surg. Traumatol. Orthop. Traumatol. 32, 1195–1200 (2022).
Padegimas, E. M. et al. Defining optimal Calcar screw positioning in proximal humerus fracture fixation. J. Shoulder Elb. Surg. 26, 1931–1937 (2017).
Zhao, L. et al. Comparison of the effects of proximal humeral internal locking system (PHILOS) alone and PHILOS combined with fibular allograft in the treatment of Neer three- or four-part proximal humerus fractures in the elderly. Orthop. Surg. 11, 1003–1012 (2019).
Neviaser, A. S. & Neviaser, R. J. Adhesive capsulitis of the shoulder. J. Am. Acad. Orthop. Surg. 19, 536–542 (2011).
Cho, C. H. et al. Definition, diagnosis, treatment, and prognosis of frozen shoulder: a consensus survey of shoulder specialists. Clin. Orthop. Surg. 12, 60–67 (2020).
Constant, C. R. & Murley, A. H. A clinical method of functional assessment of the shoulder. Clin. Orthop. 1, 160–164 (1987).
Hudak, P. L., Amadio, P. C. & Bombardier, C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The upper extremity collaborative group (UECG). Am. J. Ind. Med. 29, 602–608 (1996).
Plath, J. E. et al. Locking nail versus locking plate for proximal humeral fracture fixation in an elderly population: a prospective randomised controlled trial. BMC Musculoskelet. Disord. 20, 20 (2019).
Clavert, P., Adam, P., Bevort, A., Bonnomet, F. & Kempf, J. F. Pitfalls and complications with locking plate for proximal humerus fracture. J. Shoulder Elb. Surg. 19, 489–494 (2010).
She, R., Zhang, B., Jiang, K., Yang, S. & Zhang, Y. Cement-augmented screw fixation with PHILOS plating for osteoporotic proximal humeral fractures: an observation of mid- and long-term curative efficacy. Orthop. Surg. 15, 3108–3117 (2023).
Gracitelli, M. E. C. et al. Locking intramedullary nails compared with locking plates for two- and three-part proximal humeral surgical neck fractures: a randomized controlled trial. J. Shoulder Elb. Surg. 25, 695–703 (2016).
Court-Brown, C. M. & McQueen, M. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. J. Bone Joint Surg. Am. 91, 2771 (2009).
Sun, Q. et al. Locking plates versus intramedullary nails in the management of displaced proximal humeral fractures: a systematic review and meta-analysis. Int. Orthop. 42, 641–650 (2018).
Sun, Q., Wu, X., Wang, L. & Cai, M. The plate fixation strategy of complex proximal humeral fractures. Int. Orthop. 44, 1785–1795 (2020).
Voigt, C., Geisler, A., Hepp, P., Schulz, A. P. & Lill, H. Are polyaxially locked screws advantageous in the plate osteosynthesis of proximal humeral fractures in the elderly? A prospective randomized clinical observational study. J. Orthop. Trauma. 25, 596–602 (2011).
Lin, T., Xiao, B., Ma, X., Fu, D. & Yang, S. Minimally invasive plate osteosynthesis with a locking compression plate is superior to open reduction and internal fixation in the management of the proximal humerus fractures. BMC Musculoskelet. Disord. 15, 206 (2014).
Verdano, M. A. et al. Can the osteosynthesis with locking plates be a better treatment for unstable fractures of the proximal humerus? Musculoskelet. Surg. 98, 27–33 (2014).
Thanasas, C., Kontakis, G., Angoules, A., Limb, D. & Giannoudis, P. Treatment of proximal humerus fractures with locking plates: a systematic review. J. Shoulder Elb. Surg. 18, 837–844 (2009).
Martetschläger, F. et al. Plating of proximal humeral fractures. Orthopedics 35, e1606–e1612 (2012).
Jung, W. B., Moon, E. S., Kim, S. K., Kovacevic, D. & Kim, M. S. Does medial support decrease major complications of unstable proximal humerus fractures treated with locking plate? BMC Musculoskelet. Disord. 14, 102 (2013).
Krappinger, D. et al. Predicting failure after surgical fixation of proximal humerus fractures. Injury 42, 1283–1288 (2011).
Lescheid, J., Zdero, R., Shah, S., Kuzyk, P. R. T. & Schemitsch, E. H. The biomechanics of locked plating for repairing proximal humerus fractures with or without medial cortical support. J. Trauma. 69, 1235–1242 (2010).
Egol, K. A. et al. Early complications in proximal humerus fractures (OTA types 11) treated with locked plates. J. Orthop. Trauma. 22, 159–164 (2008).
Moayeri, A. et al. Fracture risk in patients with type 2 diabetes mellitus and possible risk factors: a systematic review and meta-analysis. Ther. Clin. Risk Manag. 13, 455–468 (2017).
Ma, J. et al. Effectiveness analysis of proximal humerus internal locking system plate combined with rotator cuff reinforcement suture in treatment of Neer type IV proximal humerus fracture. J. Reparative Reconstr. Surg. 36, 1465–1470 (2022).
Gardner, M. J. et al. The importance of medial support in locked plating of proximal humerus fractures. J. Orthop. Trauma. 21, 185–191 (2007).
Funding
Natural Science Foundation of Ningxia Province, 2023AAC02064.
Author information
Authors and Affiliations
Contributions
H.M.: study concept and design, literature screening, and initial writing. J.S. and X.M.: data extraction, revision of the manuscript. Z.Y.: critical revision of included studies. H.S. and D.C.: statistical support. L.S. and P.Z.: revision of manuscript. Z.Q.: primary writing, revision of the manuscript, study concept and design, statistical support, and critical revision of the manuscript. All authors have made substantive contributions to this study and manuscript, and all have reviewed the final paper before its submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study followed the standards of the Declaration of Helsinki and was approved by the Ethics Committee of the General Hospital of Ningxia Medical University (KYLL-2024-1460).
Informed consent
Informed consent was obtained from all subjects and/or their legal guardian(s).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ma, H., Sun, J., Ma, X. et al. Retrospective analysis of open reduction and locking plate fixation in three and four part proximal humeral fractures with efficacy and complications. Sci Rep 15, 23081 (2025). https://doi.org/10.1038/s41598-025-07119-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-07119-x
Keywords
This article is cited by
-
Locking plates versus intramedullary nails for the treatment of two- and three-part proximal humerus fractures in patients older than 60 years: a meta-analysis
European Journal of Orthopaedic Surgery & Traumatology (2025)