Abstract
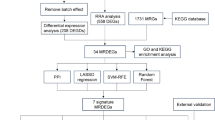
To investigate the potential pathogenesis of metabolic dysfunction-associated steatotic liver disease (MASLD) by using bioinformatics approaches. Data from three MASLD-related datasets (GSE89632, GSE72756 and GSE49541) were downloaded from the Gene Expression Omnibus (GEO) database and merged for analysis. Differentially expressed genes (DEGs) were identified via the limma package in R (|logFC|> 1, adjusted p value < 0.05). Functional enrichment analysis was conducted via Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathways and gene set enrichment analysis (GSEA). Protein‒protein interaction (PPI) network analysis was used to identify hub genes related to MASLD. 1278 DEGs (1238 upregulated, 40 downregulated) related to MASLD were identified. GO analysis revealed that the DEGs were involved mainly in the regulation of membrane potential (BP), the monoatomic ion channel complex (CC) and postsynaptic neurotransmitter receptor activity (MF). KEGG analysis highlighted neuroactive ligand-receptor interactions and taste transduction pathways, which were downregulated in MASLD. PPI network analysis identified 10 hub genes: PIK3CD, PIK3R2, PIK3R1, PIK3R3, PIK3CB, PIK3CA, SRC, PIK3CG, PIK3R5 and PIK3R6. This study identified 10 hub genes associated with MASLD, primarily involved in the PI3K/AKT signaling pathway, which could serve as biomarkers for MASLD diagnosis and progression, with the pathway potentially becoming a new therapeutic target.
Similar content being viewed by others
Introduction
Metabolic dysfunction-associated steatotic liver disease (MASLD) is a metabolic stress-related liver injury characterized by excessive accumulation of fat in the liver. The global prevalence of MASLD in the general adult population ranges from 6.3 to 45%, with a median of 25.2%1. The prevalence of MASLD in China is at a moderate to high level, exceeding 25%2. The spectrum of MASLD includes metabolic dysfunction-associated steatosis, metabolic dysfunction-associated steatohepatitis (MASH), cirrhosis and hepatocellular carcinoma (HCC)3. The liver-related mortality rates for MASLD patients and MASH patients are 0.77 per 1000 person-years and 11.77 per 1000 person-years, respectively, and the all-cause mortality rates are 15.44 per 1000 person-years and 25.56 per 1000 person-years, respectively4.
The etiology and pathogenesis of MASLD are multifactorial and not yet fully understood. Insulin resistance (IR), lipid metabolism disorders, inflammation, the environment and imbalances in the gut microbiota imbalance may all contribute to the occurrence and development of MASLD5. Recent studies have highlighted the strong association between MASLD and inflammatory burden6,7. IR, obesity, and other metabolic abnormalities can lead to a state of chronic low-grade inflammation, which is a key factor in the pathogenesis of MASLD8. Moreover, IR leads to adipose tissue dysfunction via the secretion of adipokines and pro-inflammatory cytokines, thereby potentiating inflammation. At the cellular level, these processes result in oxidative stress and DNA damage in hepatocytes, which, combined with inflammation, are thought to eventually lead to fibrosis and cirrhosis9. Hence inflammation related pathways could be involved in the pathogenesis of MASLD.
At present, the treatment methods for MASLD include lifestyle interventions, drug therapy and complication management10. Effective treatments for MASLD remain challenging because the understanding of its pathogenesis is incomplete.
Over the past few decades, methodologies in systems biology have significantly advanced our comprehension of the molecular mechanisms underlying biological phenomena and pathologies11. These innovative strategies have played crucial roles in deciphering complex molecular interactions and associations across a spectrum of diseases. In order to identify new diagnostic and therapeutic targets for MASLD, we used bioinformatics approaches to explore potentially relevant biomarkers and the pathogenesis of MASLD in the present study.
Methods
Data acquisition and preliminary processing
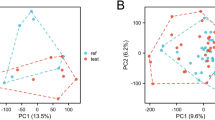
Three MASLD-related datasets (GSE89632 series deposited by Allard JP et al., GSE72756 series deposited by Chuanzheng S et al. and GSE49541 series deposited by Caba O et al.) were downloaded from the Gene Expression Omnibus (GEO) database in NCBI (http://www.ncbi.nlm.nih.gov/gds/). The details of the datasets are presented in Table 1. GSE89632, GSE72756 and GSE49541 were merged to create a comprehensive dataset. The combined dataset contains 101 MASLD samples and 44 healthy control (HC) samples. Normalization of the data was conducted for batch effect correction via the ComBat function from the R package sva12. Further normalization was then applied via the normalizeBetweenArrays function from the R package limma13. The homogeneity of the data distribution after normalization was assessed by constructing box plots.
Identifcation of differential expressed genes (DEGs) associated with MASLD
The limma package in R was used to identify DEGs between the MASLD samples and HC group samples in the combined dataset. |logFC|> 1 and adjusted p value < 0.05 were set as the criteria for selection. A heatmap was created to represent the results visually.
Functional enrichment analysis of DEGs
As a standard method for functional enrichment studies, Gene Ontology (GO) analysis14 includes biological process (BP), molecular function (MF) and cellular component (CC) analyses. GO and Kyoto Encyclopedia of Genes and Genomes (KEGG) signaling pathway enrichment analyses were performed via the R package “clusterProfiler” in our study. The p value < 0.05 was considered to indicate significant enrichment.
Gene set enrichment analysis (GSEA) is a method that differs from traditional enrichment analyses as it is used to identify whether certain biological pathways are significantly affected within a gene set. Unlike methods that focus solely on the statistical significance of differential expression, GSEA takes into account the overall expression trend and consistency across a set of genes rather than just the individual significance of each gene. This approach allows GSEA to detect coordinated changes in gene expression that may not be apparent through traditional differential expression analysis, thus providing a more comprehensive view of the biological processes that are altered under specific conditions. The ClusterProfiler package of R software was used for GSEA of DEGs to explore the potential mechanism of MASLD preliminarily. p < 0.05 and FDR (q value) < 0.25 were considered the critical values for significant enrichment.
Network analysis of protein–protein interactions (PPIs) of DEGs and identification of MASLD-related hub genes
The STRING database (http://string-db.org/) was used to generate a PPI network for DEGs to investigate PPIs. The species was limited to “Homo sapiens”, and a medium confidence score > 0.9 was considered statistically significant. The PPI network relationship diagram was subsequently imported into the Cytoscape 3.9.1 platform and MCODE (Molecular Complex Detection) plugin was used to identify significant subnetworks within the PPI network. “In Whole Network” was chosen to identify clusters across the entire PPI network. The Degree Cutoff was set to 2 to filter out isolated nodes. The K-core was set to 2 to focus on subnetworks with a minimum level of connectivity. For cluster finding, the Node Score Cutoff was set to 0.2, Haircut was enabled to trim peripheral nodes, Fluff was disabled to maintain strict cluster boundaries, and the Max Depth from Seed was set to 100 to ensure a comprehensive search. The Cytohuba plugin’s Matthews correlation coefficient (MCC) algorithm was subsequently used to screen the top 10 genes on the basis of their importance in the PPI network as hub genes.
Results
Identification of DEGs related to MASLD
In total, 1278 DEGs related to MASLD were identified, with 1238 genes exhibiting a substantial increase in expression and 40 genes showing a marked decrease in expression in MASLD samples compared with healthy control samples. A heatmap of the DEGs in the dataset is plotted in Fig. 1.
Results of enrichment analysis
As shown in Fig. 2, in the GO category, most of the DEGs were involved in the regulation of membrane potential, embryonic organ development, the ovulation cycle, embryonic organ morphogenesis and the regulation of postsynaptic membrane potential (BP); monoatomic ion channel complex, transporter complex, transmembrane transporter complex, synaptic membrane and interphotoreceptor matrix (CC); and postsynaptic neurotransmitter receptor activity, neurotransmitter receptor activity, neurotransmitter receptor activity involved in the regulation of postsynaptic membrane potential, gated channel activity and transmitter − gated monoatomic ion channel activity involved in the regulation of postsynaptic membrane potential (MF).
The KEGG enrichment results indicated that the DEGs were involved in neuroactive ligand − receptor interaction, taste transduction, cytokine − cytokine receptor interaction, MAPK signaling pathway, autoimmune thyroid disease, the cAMP signaling pathway and the JAK − STAT signaling pathway (Fig. 3).
KEGG enrichment analysis. KEGG pathway analysis was performed using data from the KEGG database(Kanehisa Laboratories; https://www.kegg.jp)15,16.
The GSEA results revealed that the neuroactive ligand–receptor interaction and taste transduction pathways were significantly downregulated in the MASLD group compared with those in the normal control group (Fig. 4).
Construction of the PPI network and identification of hub genes
A total of 1278 DEGs were input into the STRING database for PPI network analysis. After removing DEGs with different expression tendencies and isolated nodes from the PPI network, a total of 1331 nodes and 1471 edges were included, with an average node degree of 2.21 (Fig. 5). The top 10 genes, as identified by the MCC algorithm via the cytoHubba plugin in Cytoscape, were designated as hub genes, which included PIK3CD, PIK3R2, PIK3R1, PIK3R3, PIK3CB, PIK3CA, SRC, PIK3CG, PIK3R5 and PIK3R6 (Fig. 6).
Discussion
As a significant global public health burden, MASLD is highly prevalent on all continents. MASLD, particularly its severe form known as MASH, is capable of advancing to severe liver conditions such as cirrhosis and HCC. MASH is increasingly recognized as the second leading cause of liver transplants in the United States, following chronic hepatitis C, and its prevalence continues to rise17. However, the underlying mechanisms of MASLD are still unclear. Investigating the pathogenesis of MASLD and finding effective treatments for MASLD are highly important. Many literatures have confirmed that MASLD, as well as related conditions like metabolic syndrome, obesity, type 2 diabetes mellitus, and hypertension, are all associated with significant inflammatory changes18,19,20. Liu YJ et al. reported that ACMSD inhibitors could mitigate inflammation and DNA damage, thereby reversing MASLD/MASH21. This study aims to provide some clues to support the pathogenesis and pharmacological studies of MASLD.
In our study, compared with healthy control individuals, 1278 DEGs related to MASLD were identified (1238 upregulated and 40 downregulated DEGs). According to the GO category, the DEGs were mostly involved in the regulation of membrane potential (BP), monoatomic ion channel complex (CC) and postsynaptic neurotransmitter receptor activity (MF). The liver is one of the most abundant organs in mitochondria. Growing evidence indicates that mitochondrial metabolism plays an important role in the development of MASLD in various ways. Mitochondrial dysfunction impairs the import and oxidation of fatty acids in mitochondria, leading to lipid accumulation and hepatic steatosis, which represents the initial stage of MASLD22. In MASLD, increased fatty acid oxidation and mitochondrial dysfunction lead to excessive ROS production, which damages mitochondrial components and creates a vicious cycle of oxidative stress, contributing to hepatocyte injury, inflammation, and fibrosis23. The mitochondrial membrane potential is an important indicator of mitochondrial function, reflecting the respiratory function and energy metabolism status of mitochondria. A decrease in the mitochondrial membrane potential is closely related to the occurrence and development of MASLD24,25. Monoatomic ion channel complex refers to a protein complex that spans across a membrane and phospholipid bilayer, allowing for the selective transport of monatomic ions along its electrochemical gradient. Previous studies have indicated that Ca2+ channel expression varies led to an imbalance in intracellular calcium levels, increased endoplasmic reticulum stress, impaired mitochondrial function and reduced autophagy, all of which contributed to the progression of MASLD26. The correlation between postsynaptic neurotransmitter receptor activity and MASLD is currently unclear. Yang Z et al. reported that neurotransmitters of the sympathetic nervous system (such as catecholamines and neuropeptide Y) could affect liver metabolism and the inflammatory response by activating specific receptors in the liver (such as adrenergic receptors and Y1 receptors), which suggested that postsynaptic receptor activity may indirectly affect the development of MASLD by affecting sympathetic nervous system activity in the liver27.
Our KEGG enrichment results indicated that the DEGs were involved mainly in neuroactive ligand–receptor interactions and taste transduction. GSEA further revealed that, compared with those in the normal control group, neuroactive ligand–receptor interactions and taste transduction pathways were significantly downregulated in the MASLD group. Wang A et al. confirmed that neuroactive ligand–receptor interactions played an important role in the common pathological mechanism of heart failure with a preserved ejection fraction and MASLD28. A longitudinal cohort study involving 33,899 Korean participants revealed that decreased overall autonomic modulation and vagal activity increased the risk of MASLD29. Sun W et al. reported consistent findings in the Chinese population30. Neuroactive ligand–receptor interactions encompasses a variety of neuroactive ligands and receptors that are involved in modulating metabolic and inflammatory processes, both of which are central to the development of MASLD. Neurotransmitters such as glutamate and GABA have been shown to influence insulin sensitivity and lipid metabolism through their respective receptors31. Additionally, as neuroactive ligands, leptin and adiponectin can regulate appetite and energy metabolism through receptors in the hypothalamus. Leptin can activate the JAK2 signaling pathway through its receptor Ob Rb, thereby activating signaling pathways such as STAT3, STAT5, MAPK, or AKT/mTOR, leading to IR. Adiponectin improves IR by activating the AMPK and PI3K/Akt signaling pathways through its receptors AdipoR1 and AdipoR232,33.
Taste transduction is traditionally associated with taste perception in the oral cavity, but emerging evidence suggests that it may also play a role in metabolic disorders and liver diseases, such as MASLD. Sarnelli G et al. confirmed that taste receptors such as TAS1R and TAS2R were expressed not only in the oral cavity but also in the gastrointestinal tract, where they modulated the release of enterohormones like glucagon-like peptide-1 (GLP-1) and peptide YY (PYY). These hormones play crucial roles in regulating glucose homeostasis, satiety, and energy balance, all of which are disrupted in MASLD34,35. It is reported that taste receptors in the gut could influence gut microbiota composition and function, thereby exacerbating inflammation and contribute to liver disease progression36.
We further identified 10 hub genes closely related to the occurrence of MASLD in the PPI network, including PIK3CD, PIK3R2, PIK3R1, PIK3R3, PIK3CB, PIK3CA, SRC, PIK3CG, PIK3R5 and PIK3R6. The PIK3 family is a class of phosphatidylinositol 3-kinases (PI3Ks) that play important roles in various physiological processes within cells, including cell proliferation, survival, metabolism and migration37. The PIK3 family can be divided into three different categories on the basis of their structure and function: type I, type II and type III. Type I PI3Ks, consisting of a catalytic subunit and a regulatory subunit, are the most extensively studied. The catalytic subunit includes four subtypes, α, β, γ and δ, which are encoded by the PIK3CA, PIK3CB, PIK3CG and PIK3CD genes, respectively. The regulatory subunits include PIK3R1, PIK3R2 and PIK3R3, which encode p85α, p85β and p55γ, respectively. The PIK3 family participates in the regulation of various cellular functions, such as cell survival, growth, metabolism and blood glucose homeostasis, through the PI3K/AKT signaling pathway38,39. The PI3K/AKT signaling pathway plays an important role in multiple mechanisms related to the presence and development of MASLD, such as lipid metabolism, the inflammatory response and IR. Previous studies have shown that activation of the PI3K/AKT signaling pathway can reduce intracellular lipid accumulation and inflammation levels, thereby alleviating MASLD. Vascular endothelial growth factor B (VEGFB) improves IR in MASLD through the PI3K/AKT signaling pathway. Wu D et al. reported that impaired PI3K/AKT signaling exacerbated IR in tissues, which lead to accelerated development of MASLD40. It has been reported that the overexpression of PIK3R3 promoted hepatic fatty acid oxidation by inducing PPAR α expression through PIK3R3, thereby improving the fatty liver phenotype induced by a high-fat diet in mice41. As a key regulatory subunit of the PI3K/AKT signaling pathway, downregulation of PIK3R3 expression may impair the full activation of this pathway, thereby contributing to IR, promoting hepatic lipid deposition, and consequently precipitating and exacerbating MASLD. It is reported that hesperetin mitigates oxidative stress in the liver through the PI3K/AKT-Nrf2 signaling pathway, and this antioxidant action further suppresses inflammation driven by NF-κB during the development of MASLD42. Liu B et al. demonstrated that scoparone improved hepatic inflammation in mice with MASLD by regulating the PI3K/AKT/mTOR pathway in macrophages43. SRC is a nonreceptor tyrosine kinase associated with multiple signaling pathways. We speculate that SRC may affect the occurrence and development of MASLD via the PI3K/AKT signaling pathway. We can develop inhibitors or activators targeting the hub genes to modulate the activity of the PI3K/AKT pathway for the treatment of MASLD. Sun C et al. reported that Pueraria flavonoids induced autophagy through the PI3K/AKT/mTOR signaling pathway, improved MASLD in obese mice and reduced intracellular lipid deposition by inhibiting lipid synthesis and the release of proinflammatory cytokines44. Wu YC et al. also reported that nucleoporin 85 mitigated lipid metabolism and inflammation by modulating the PI3K/AKT signaling pathway in MASLD45. Several drugs targeting the PI3K/AKT pathway have entered clinical trials or been approved for cancer treatment. For instance, Alpelisib (an PI3K inhibitor) and Capivasertib (an AKT inhibitor) have been approved by the US Food and Drug Administration (FDA) for treating breast cancer23,46. Further studies are needed to determine whether these drugs can be used for the treatment of MASLD.
In conclusion, 10 hub genes associated with MASLD, which are involved mainly in the PI3K/AKT signaling pathway, were identified in our study via bioinformatics methods. These genes can serve as biomarkers for monitoring the initiation and progression of MASLD, providing new means for its early diagnosis, and the PI3K/AKT signaling pathway may become a new therapeutic target for MASLD. We will further conduct cell and animal model experiments to validate our conclusions.
Data availability
Three MASLD-related datasets (GSE89632 series deposited by Allard JP et al., GSE72756 series deposited by Chuanzheng S et al. and GSE49541 series deposited by Caba O et al.) were downloaded from the Gene Expression Omnibus (GEO) database in NCBI (http://www.ncbi.nlm.nih.gov/gds/).
References
Riazi, K. et al. The prevalence and incidence of NAFLD worldwide: A systematic review and meta-analysis. The Lancet. Gastroenterol. Hepatol. 7, 851–861. https://doi.org/10.1016/s2468-1253(22)00165-0 (2022).
Zhou, J. et al. Epidemiological features of NAFLD from 1999 to 2018 in China. Hepatology (Baltimore, MD) 71, 1851–1864. https://doi.org/10.1002/hep.31150 (2020).
Chen, Y. Y. & Yeh, M. M. Non-alcoholic fatty liver disease: A review with clinical and pathological correlation. J. Formosan Med. Associat. Taiwan Yizhi 120, 68–77. https://doi.org/10.1016/j.jfma.2020.07.006 (2021).
Younossi, Z. M. et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology (Baltimore, MD) 64, 73–84. https://doi.org/10.1002/hep.28431 (2016).
Juanola, O., Martínez-López, S., Francés, R. & Gómez-Hurtado, I. Non-alcoholic fatty liver disease: Metabolic, genetic, epigenetic and environmental risk factors. Int. J. Environ. Res. Public Health 18, 5227. https://doi.org/10.3390/ijerph18105227 (2021).
Kosekli, M. A. & Aktas, G. The systemic immune inflammation index is a reliable and novel risk factor for metabolic dysfunction-associated fatty liver disease. Curr. Med. Res. Opin. 41, 247–251. https://doi.org/10.1080/03007995.2025.2463952 (2025).
Kosekli, M. A. et al. The association between serum uric acid to high density lipoprotein-cholesterol ratio and non-alcoholic fatty liver disease: The abund study. Rev. Assoc. Med. Bras. 1992(67), 549–554. https://doi.org/10.1590/1806-9282.20201005 (2021).
Nakamura, T. et al. Pathogenic mechanisms of metabolic dysfunction-associated steatotic liver disease (MASLD)-associated hepatocellular carcinoma. Cells 14, 428. https://doi.org/10.3390/cells14060428 (2025).
Phoolchund, A. G. S. & Khakoo, S. I. MASLD and the development of HCC: Pathogenesis and therapeutic challenges. Cancers 16, 259. https://doi.org/10.3390/cancers16020259 (2024).
Rong, L. et al. Advancements in the treatment of non-alcoholic fatty liver disease (NAFLD). Front. Endocrinol. 13, 1087260. https://doi.org/10.3389/fendo.2022.1087260 (2022).
Dadashkhan, S. et al. Deciphering crucial genes in multiple sclerosis pathogenesis and drug repurposing: A systems biology approach. J. Proteomics 280, 104890. https://doi.org/10.1016/j.jprot.2023.104890 (2023).
Leek, J. T., Johnson, W. E., Parker, H. S., Jaffe, A. E. & Storey, J. D. The sva package for removing batch effects and other unwanted variation in high-throughput experiments. Bioinformatics (Oxford, England) 28, 882–883. https://doi.org/10.1093/bioinformatics/bts034 (2012).
Moreira, O. C. et al. Mitochondrial function and mitophagy in the elderly: Effects of exercise. Oxid. Med. Cell. Longev. 2017, 2012798. https://doi.org/10.1155/2017/2012798 (2017).
Yu, G. Gene ontology semantic similarity analysis using GOSemSim. Methods Mol. Biol. (Clifton, N.J.) 2117, 207–215. https://doi.org/10.1007/978-1-0716-0301-7_11 (2020).
Kanehisa, M. Toward understanding the origin and evolution of cellular organisms. Protein Sci.: Public. Protein Soc. 28, 1947–1951. https://doi.org/10.1002/pro.3715 (2019).
Kanehisa, M., Furumichi, M., Sato, Y., Matsuura, Y. & Ishiguro-Watanabe, M. KEGG: Biological systems database as a model of the real world. Nucleic Acids Res. 53, D672–D677. https://doi.org/10.1093/nar/gkae909 (2025).
Guo, X., Yin, X., Liu, Z. & Wang, J. Non-alcoholic fatty liver disease (NAFLD) pathogenesis and natural products for prevention and treatment. Int. J. Mol. Sci. 23, 15489. https://doi.org/10.3390/ijms232415489 (2022).
Dedemen, B., Duman, T. T., Dedemen, M. M. & Aktas, G. Effect of sodium glucose Co-transporter 2 inhibitor use on anthropometric measurements and blood glucose in obese and non-obese type 2 diabetic patients. Clin. Nutr. ESPEN 63, 515–519. https://doi.org/10.1016/j.clnesp.2024.07.016 (2024).
Aktas, G. Association between the prognostic nutritional index and chronic microvascular complications in patients with type 2 diabetes mellitus. J. Clin. Med. 12, 5952. https://doi.org/10.3390/jcm12185952 (2023).
Aktas, G. et al. Poorly controlled hypertension is associated with elevated serum uric acid to HDL-cholesterol ratio: A cross-sectional cohort study. Postgrad. Med. 134, 297–302. https://doi.org/10.1080/00325481.2022.2039007 (2022).
Liu, Y. J. et al. ACMSD inhibition corrects fibrosis, inflammation, and DNA damage in MASLD/MASH. J. Hepatol. 82, 174–188. https://doi.org/10.1016/j.jhep.2024.08.009 (2025).
Wei, Y., Rector, R. S., Thyfault, J. P. & Ibdah, J. A. Nonalcoholic fatty liver disease and mitochondrial dysfunction. World J. Gastroenterol. 14, 193–199. https://doi.org/10.3748/wjg.14.193 (2008).
He, Y. et al. Targeting PI3K/Akt signal transduction for cancer therapy. Signal Transduct. Target. Ther. 6, 425. https://doi.org/10.1038/s41392-021-00828-5 (2021).
Zheng, Y., Wang, S., Wu, J. & Wang, Y. Mitochondrial metabolic dysfunction and non-alcoholic fatty liver disease: New insights from pathogenic mechanisms to clinically targeted therapy. J. Transl. Med. 21, 510. https://doi.org/10.1186/s12967-023-04367-1 (2023).
Nakanishi, T. et al. An implication of the mitochondrial carrier SLC25A3 as an oxidative stress modulator in NAFLD. Exp. Cell Res. 431, 113740. https://doi.org/10.1016/j.yexcr.2023.113740 (2023).
Chen, X., Zhang, L., Zheng, L. & Tuo, B. Role of Ca(2+) channels in non-alcoholic fatty liver disease and their implications for therapeutic strategies (Review). Int. J. Mol. Med. 50, 1–10. https://doi.org/10.3892/ijmm.2022.5169 (2022).
Yang, Z. et al. The role of nuclear receptors in the pathogenesis and treatment of non-alcoholic fatty liver disease. Int. J. Biol. Sci. 20, 113–126. https://doi.org/10.7150/ijbs.87305 (2024).
Wang, A. et al. Heart failure with preserved ejection fraction and non-alcoholic fatty liver disease: New insights from bioinformatics. ESC Heart Fail. 10, 416–431. https://doi.org/10.1002/ehf2.14211 (2023).
Jung, I. et al. Autonomic imbalance increases the risk for non-alcoholic fatty liver disease. Front. Endocrinol. 12, 752944. https://doi.org/10.3389/fendo.2021.752944 (2021).
Sun, W. et al. Association between non-alcoholic fatty liver disease and autonomic dysfunction in a Chinese population. QJM: Month. J. Associat. Physicians 108, 617–624. https://doi.org/10.1093/qjmed/hcv006 (2015).
Huang, X. T. et al. Activation of N-methyl-D-aspartate receptor regulates insulin sensitivity and lipid metabolism. Theranostics 11, 2247–2262. https://doi.org/10.7150/thno.51666 (2021).
Jiménez-Cortegana, C. et al. Role of leptin in non-alcoholic fatty liver disease. Biomedicines 9, 762. https://doi.org/10.3390/biomedicines9070762 (2021).
Adolph, T. E., Grander, C., Grabherr, F. & Tilg, H. Adipokines and non-alcoholic fatty liver disease: Multiple interactions. Int. J. Mol. Sci. 18, 1649. https://doi.org/10.3390/ijms18081649 (2017).
Sarnelli, G. et al. Taste and the Gastrointestinal tract: From physiology to potential therapeutic target for obesity. Int. J. Obesity Suppl. 9, 1–9. https://doi.org/10.1038/s41367-019-0012-6 (2019).
Kinnamon, S. C. & Finger, T. E. Recent advances in taste transduction and signaling. F1000Research 8, https://doi.org/10.12688/f1000research.21099.1 (2019).
Yang, M., Massad, K., Kimchi, E. T., Staveley-O’Carroll, K. F. & Li, G. Gut microbiota and metabolite interface-mediated hepatic inflammation. Immunometabolism (Cobham, Surrey) 6, e00037. https://doi.org/10.1097/in9.0000000000000037 (2024).
Luo, Q. et al. Targetable leukaemia dependency on noncanonical PI3Kγ signalling. Nature 630, 198–205. https://doi.org/10.1038/s41586-024-07410-3 (2024).
Huang, D. et al. Evaluation of the PIK3 pathway in peripheral T-cell lymphoma and NK/T-cell lymphoma. Br. J. Haematol. 189, 731–744. https://doi.org/10.1111/bjh.16435 (2020).
Liu, Y. et al. Pan-cancer analysis on the role of PIK3R1 and PIK3R2 in human tumors. Sci. Rep. 12, 5924. https://doi.org/10.1038/s41598-022-09889-0 (2022).
Wu, D. et al. Hydrogen sulfide attenuates high-fat diet-induced non-alcoholic fatty liver disease by inhibiting apoptosis and promoting autophagy via reactive oxygen species/phosphatidylinositol 3-kinase/AKT/mammalian target of rapamycin signaling pathway. Front. Pharmacol. 11, 585860. https://doi.org/10.3389/fphar.2020.585860 (2020).
Yang, X. et al. PIK3R3 regulates PPARα expression to stimulate fatty acid β-oxidation and decrease hepatosteatosis. Exp. Mol. Med. 50, e431. https://doi.org/10.1038/emm.2017.243 (2018).
Li, J. et al. Hesperetin ameliorates hepatic oxidative stress and inflammation via the PI3K/AKT-Nrf2-ARE pathway in oleic acid-induced HepG2 cells and a rat model of high-fat diet-induced NAFLD. Food Funct. 12, 3898–3918. https://doi.org/10.1039/d0fo02736g (2021).
Liu, B. et al. Scoparone improves hepatic inflammation and autophagy in mice with nonalcoholic steatohepatitis by regulating the ROS/P38/Nrf2 axis and PI3K/AKT/mTOR pathway in macrophages. Biomed. Pharmacotherapy Biomedecine Pharmacotherapie 125, 109895. https://doi.org/10.1016/j.biopha.2020.109895 (2020).
Sun, C. et al. Induction of autophagy via the PI3K/Akt/mTOR signaling pathway by Pueraria flavonoids improves non-alcoholic fatty liver disease in obese mice. Biomed. Pharmacotherapy Biomed. Pharmacotherapie 157, 114005. https://doi.org/10.1016/j.biopha.2022.114005 (2023).
Wu, Y. C. et al. NUP85 alleviates lipid metabolism and inflammation by regulating PI3K/AKT signaling pathway in nonalcoholic fatty liver disease. Int. J. Biol. Sci. 20, 2219–2235. https://doi.org/10.7150/ijbs.92337 (2024).
Turner, N. C. et al. Capivasertib in hormone receptor-positive advanced breast cancer. N. Engl. J. Med. 388, 2058–2070. https://doi.org/10.1056/NEJMoa2214131 (2023).
Funding
This work was supported by the National Science and Technology Major Project (No. 81570536).
Author information
Authors and Affiliations
Contributions
Cuiping Shao and Youqing Xu conceived and designed the study. Cuiping Shao collected and analyzed the data, and wrote the initial draft of the manuscript. Youqing Xu provided substantial input on the study design, critically reviewed the manuscript, and contributed to the final revisions. All the authors have read and approved this manuscript.
Corresponding authors
Ethics declarations
Competing interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shao, C., Xu, Y. PI3K/AKT signaling pathway plays an important role in the pathogenesis of metabolic dysfunction-associated steatotic liver disease. Sci Rep 15, 20593 (2025). https://doi.org/10.1038/s41598-025-07612-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-07612-3