Abstract
This study aimed to evaluate the nonlinear association between prognostic nutritional index (PNI) and mortality in geriatric hip fractures. Geriatric patients with hip fractures were screened between January 2015 and September 2019. We collected the demographic information and followed up on the survival data. Multivariate Cox proportional hazards regression model and restricted cubic spline were used to identify the linear and nonlinear associations between PNI and post-operative mortality. This study included two thousand one hundred and fifteen patients who met the criteria. There were 1443 females, accounting for 68.23% of all patients. The mean age was 79.36 ± 6.74 years. The mean follow-up period was 38.57 ± 17.96 months. There were 636 all-cause deaths. In primary linear association, PNI was associated with mortality (HR = 0.95; 95%CI: 0.93–0.97; P < 0.0001) in the adjusted model. However, it was nonlinear that the real association between PNI and mortality. Through two-piecewise Cox proportional hazards regression model analysis, we found that 50.3 was an inflection point. When PNI was less than 50.3, there was an association between PNI and mortality (HR = 0.94; 95%CI: 0.92–0.96; P < 0.0001). For every one-unit increase in PNI, the mortality of patients decreased by 6%. When PNI was greater than 50.3, the mortality became relatively stable and no longer changed with PNI (HR = 1.03, 95%CI:0.99–1.07; P = 0.1469). The results were stable when the patients were divided into subgroups as different confounding factors in stratification analysis. PNI is a vital predictor of mortality for patients with hip fractures. We found that 50.3 was a significant clinical inflection point. When the PNI is less than 50.3, the mortality decreases as the PNI increases. When PNI is more than 50.3, the mortality rate tends to be stable and maintained at a low level. Therefore, PNI should be assessed when the elderly hip fractures for preoperative risk stratification and beyond its threshold.
Similar content being viewed by others
Introduction
Hip fracture is a common injury in the elderly, characterized by high rates of disability and mortality1,2. Elderly patients with hip fractures often experience malnutrition and a decline in immune function3. Studies have indicated that patients with poor nutritional status are at higher risk of early post-operative complications, such as pneumonia, deep vein thrombosis, and pressure ulcers4. In addition, some studies have shown that nutritional status and nutritional treatment were associated with outcomes and mortality in patients with hip fractures5,6,7. It was also reported in a retrospective cohort study that early nutritional interventions might reduce mortality rates and shorten rehabilitation8. Therefore, nutritional status in patients with hip fractures is a crucial factor in fracture recovery.
The Prognostic Nutritional Index (PNI) is a widely used clinical indicator for assessing nutritional and immune status9. PNI was derived from serum albumin levels and peripheral blood lymphocyte counts. In recent years, more and more studies have focused on the role of PNI in prognostic evaluation across various diseases4,10,11,12, particularly in elderly patients with hip fractures13,14,15. Studies have shown that PNI is closely related to mortality in elderly patients with hip fractures, with lower PNI levels correlating with an increased risk of post-operative complications and death4. Furthermore, PNI indirectly reflects patients’ burden of underlying diseases16,17,18. Many elderly patients with hip fractures have comorbid chronic conditions such as diabetes16, cardiovascular diseases17, and chronic obstructive pulmonary disease18. These conditions not only affect nutrient absorption but also exacerbate inflammatory responses. This vicious cycle impairs post-operative recovery and increases the risk of complications and mortality. Therefore, PNI could be an effective indicator for assessing post-operative prognosis in elderly hip fracture patients.
Most studies reported that PNI was only linearly associated with death4,13,14,15. However, the association between PNI and mortality in geriatric hip fractures was not sufficiently detailed. In some cases, a linear relationship may be able to explain trends between the variables. However, the reality is that the actual relationship is not always linear in the field of hip fractures19,20,21. Analyzing curvilinear relationships is necessary to reveal the complex relationships between variables more comprehensively and accurately. With nonlinear regression modelling, researchers can improve prediction accuracy and better understand the underlying mechanisms or processes.
Therefore, this study aimed to explore and evaluate the nonlinear association between PNI and mortality in elderly patients with hip fractures. Clinically, preoperative assessment of PNI could help identify high-risk patients early, allowing for timely nutritional interventions and immune support treatment to improve nutritional and immune status, reduce post-operative complications, and lower mortality.
Materials and methods
Institutional review boards approval
In this retrospective cohort study, we screened patients with hip fractures from January 1, 2015, to September 30, 2019, at the largest trauma center in Northwest China. This study received approval from the Ethics Committee of Honghui Hospital (Approval No. 202201009). Due to the retrospective nature of the study, Ethics Committee of Honghui Hospital waived the need of obtaining informed consent. All procedures involving human subjects adhered to the ethical standards in the 1964 Declaration of Helsinki and its subsequent amendments. The study has been reported following the STROCSS 2021 guidelines22.
Participants
Demographic and clinical data of the patients were extracted from their original medical records. The inclusion criteria were: (1) patients aged 65 years or older; (2) diagnosis of femoral neck or intertrochanteric fracture confirmed by X-ray or computed tomography; (3) patients undergoing surgical treatment at the hospital; (4) availability of clinical data during hospitalization. The exclusion criterion was the inability to contact patients or their families via telephone to ascertain survival status.
Hospital treatment
All patients were diagnosed with hip fractures by X-ray examination at admission. The hospital treatment of hip fractures is divided into three types according to the patient’s age and personal condition: closed/open reduction internal fixation (CRIF/ORIF), hemiarthroplasty (HA), and total hip arthroplasty (THA). For patients with intertrochanteric fractures, CRIF/ORIF was usually performed. The patient was placed on a traction table, and then a proximal femoral nail anti-rotation was inserted by minimal incision after having an acceptable reduction. For patients with femoral neck fractures, arthroplasty is usually performed. We used the posterior approach to undergo the HA or THA procedure. The patients receiving CRIF/ORIF and arthroplasty were asked to have partial weight-bearing two weeks and two days after the operations.
Endpoint events
The endpoint event in this study was the mortality rate in the follow-up.
Variables
The variables collected in this study were as follows: age, sex, injury mechanism, fracture classification, hypertension, diabetes, arrhythmia, hemorrhagic stroke, dementia, ischemic stroke, cancer, multiple injuries, chronic obstructive pulmonary disease (COPD), hepatitis, gastritis, treatment strategy, time to admission, time to operation, operation time, blood loss, infusion, lymphocytes count, albumin, PNI, urea, follow up, and mortality. Admission PNI was calculated as serum albumin (g/L) + 5×total lymphocyte count (×109/L).
The dependent variable was mortality, and the independent variable was the PNI.
Follow-up
After discharge, patients’ family members were contacted by telephone from Jan 2022 to Mar 2022 to record survival status and survival time. Two medical professionals conducted telephone follow-ups.
Statistics analysis
Continuous variables were reported as mean ± standard deviation (SD), and categorical variables were given as frequencies and percentages. We used χ2, the One-way ANOVA, or the Kruskal-Whallis H test for differences among PNI subgroups. Based on the criteria of P < 0.1 in univariate analysis and the previously reported factors, we selected the needed adjusted variables and introduced them into multivariate analysis. We used the multivariate Cox proportional hazards regression model to test the association between PNI and mortality. To test the robustness of our results, we performed a sensitivity analysis. We converted PNI into a categorical variable according to the tertiles, and we calculated the P for trend to verify the results of PNI as the continuous variable and to examine the possibility of nonlinearity.
To account for the nonlinear relationship between PNI and mortality, we used the Cox proportional hazards regression model with restricted cubic spline and the smooth curve fitting with penalized spline method to address nonlinearity. Besides, the two-piecewise Cox regression model was also used to explain the existence of inflection points in nonlinearity association. In addition, we draw the Kaplan–Meier survival curves to illustrate the trend in different subgroups.
All analyses were performed using statistical software packages R (http://www.R-project.org, R Foundation) and EmpowerStats (http://www.empowerstats.com, X&Y Solutions Inc., Boston, MA, USA). Hazards ratios (HR) and 95% confidence interval (CI) were calculated. A P-value < 0.05 (two-sided) was considered a high association probability.
Results
Patient characteristics
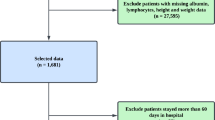
We screened 3115 patients in the digital medical system. After deleting 336 patients without PNI data, 478 were lost to follow-up, and 186 patients received no-surgical treatment. A total of 2115 patients who met the inclusion criteria were included in our study. The flow chart is shown in Fig. 1.
According to the distribution of individual PNI levels, we divided the patients into three groups: 655 low PNI (38.21 ± 2.50) group, 715 medium PNI (43.14 ± 1.07) group and 745 high PNI (48.08 ± 3.81) group. The demographic information of patients is shown in Table 1. There were 1443 females, accounting for 68.23% of all patients, with 413, 479, and 551 females in low, medium and high PNI groups, respectively. The mean age of the total sample was 79.36 ± 6.74 years. There were 1529 intertrochanteric fractures and 586 femoral neck fractures. The time to admission and time to operation were 77.45 ± 246.93 h and 4.27 ± 2.53 days, respectively.
The comorbidities were the following: 1031 hypertension, 411 diabetes, 1086 CHD, 668 arrhythmias, 591 ischemic stroke, 41 hemorrhagic stroke, and 139 associated injuries. There were three treatment strategies, 1519 CRIF/ORIF, 562 HA, and 34 THA. As for operation time and blood loss, there were no statistical differences among the groups.
The mean follow-up period was 38.57 ± 17.96 months. After the operation, there were 636 all-cause deaths, with 285 in low PNI, 207 in medium PNI and 144 in high PNI group. The main causes of death reported by family members were natural debility, with some patients dying from pulmonary infection or acute myocardial infarction. These patients all had poor nutritional status and significant weight loss before death.
Univariate analysis of the association between variates and mortality
We used the univariate Cox regression analysis to screen the important variates necessary to adjust in multivariate analysis, as shown in Table 2. According to the criteria of P < 0.1 and the previously reported factors, we found these confounding factors to adjust: age, sex, CHD, arrhythmia, ischemic stroke, cancer, dementia, hepatitis, time to operation, time to admission, and urea.
Multivariate analysis between preoperative PNI and one-year mortality
We used the Cox proportional hazards regression model to assess the association between PNI and mortality. In Table 3, PNI was associated with mortality (HR = 0.95; 95%CI: 0.93–0.97; P < 0.0001) in the adjusted model II when PNI was a continuous variate. The results were stable when we divided PNI into low, medium and high groups. In the adjusted model II, compared to the low PNI group, the medium PNI group could decrease the mortality by 29% (HR = 0.71; 95%CI: 0.59–0.86; P = 0.0003), the high PNI group could decrease the mortality by 44% (HR = 0.56; 95%CI: 0.46–0.69; P < 0.0001). However, the interval between high/medium was 0.56/0.71 = 0.78, which is higher than 0.71 or 0.56. Thus, there was a potential nonlinear association between PNI and mortality.
Curve fitting and analysis of threshold or saturation effect
As shown in Fig. 2, there was a curvilinear correlation between PNI and mortality after adjusting for confounding factors. Through two-piecewise Cox proportional hazards regression model analysis, we found that 50.3 was an inflection point, as shown in Table 4. When PNI was less than 50.3, there was an association between PNI and mortality (HR = 0.94; 95%CI: 0.92–0.96; P < 0.0001). For every one-unit increase in PNI, the mortality of patients decreased by 6%. When PNI was greater than 50.3, the mortality became relatively stable and no longer changed with PNI (HR = 1.03, 95%CI:0.99–1.07; P = 0.1469).
The Kaplan–meier survival curves
The Kaplan–Meier survival curves according to PNI subgroups and inflection point of 50.3 are shown in Fig. 3 and Fig. 4. The decreasing slope was higher in the low PNI group and the PNI < 50.3 group.
Stratification analysis
We performed a stratification analysis to test the stability of the nonlinearity association, as shown in Table 5. When the patients were divided into subgroups with different confounding factors, we found that despite different inflection points, most of the P for log-likelihood ratio test reached statistical differences.
Discussion
The present study explored the association between PNI and mortality in geriatric hip fractures. A curve association between PNI and mortality in geriatric patients with hip fractures was found through a two-piecewise Cox proportional hazards regression model with restricted cubic spline. A PNI of 50.3 was the inflection point in the curve fitting, with PNI highly associated with mortality at PNI < 50.3 (HR = 0.94). Every one-unit increase in PNI was associated with a decreasing 6% in incidence of mortality. When PNI was > 50.3, the prognostic nutrition status had the minimum influence on mortality. There were various inflection points in the stratification analysis, but they were close to the total sample analysis. Therefore, PNI was an important risk factor for mortality, and early nutritional supplementation higher than 50.3 of PNI may be suitable for prognosis. Clinically, preoperative assessment of PNI could help identify high-risk patients early, allowing for timely nutritional interventions and immune support treatment to reduce post-operative complications and mortality. For patients with low PNI, preoperative nutritional support and monitoring of recovery should be prioritized.
In fact, models for predicting the prognosis of elderly hip fracture patients have always been a hot topic. However, the prerequisite for building a reliable model is figuring out the real relationship between each predictor and mortality, in which the nonlinear relationship is essential. This study found a nonlinear association between preoperative PNI level and post-operative mortality. This result will help us consider its particular correlation when modelling in the future.
As for the association between preoperative PNI and mortality, most studies reported that PNI was the risk factor for post-operative prognosis13,14,15. PNI could be an important predictor of prognosis in hip fracture15. Three small sample studies reported the predictive role of PNI on mortality. It was reported that the cut-off value of PNI in predicting mortality was 32.5, but the area under the curve was 0.66023. In a 925-patient study, the cut-off was 34.475, with 69.7% sensitivity and 51.1% specificity24. In a study with 924 patients14, Chen et al. concluded that the optimal cut-off of PNI for predicting mortality was set as 45.275 with 67.4% sensitivity, 69.2% specificity, and 0.727 under the curve. In a study of 3351 hip patients aged 45 or older, the results showed that medium (HR = 0.66) and high (HR = 0.61) PNI were associated with lower 2-year mortality compared to low PNI4. Based on the above work, we built the nonlinear association between PNI and mortality and found the safe PNI value supported by a mean 38.57 months follow-up. A PNI of 50.3 was the inflection point in this study, which was higher than the cut-off value reported by other studies. The potential reasons were the difference in study design, sample size, statistical method, and population specificity of elderly hip fracture. Firstly, this study was designed as a retrospective cohort study with 2115 individual patients with more than 3-year follow-up. All the patients were aged 65 or older in our study, while there were young hip fractures in the large sample size study4. Secondly, we used the Cox proportional hazards regression model with restricted cubic spline and the smooth curve fitting with penalized spline method to address nonlinearity. While most current studies used a generalized linear regression or predictive model, they failed to capture the nonlinear relationship between PNI and mortality. We found that the effect of PNI on mortality was more significant in the low-value interval of PNI < 50.3. In contrast, most of the other studies used a united linear model4 or predictive model14,23,24 to analyze the role of PNI. Linear regression may underestimate the significant effect of PNI < 50.3, while curvilinear regression can reveal this trend more sensitively. Thirdly, elderly hip fracture patients may require higher PNI levels to maintain a favorable prognosis due to fracture trauma and perioperative stress5. In addition, our study showed a 6% reduction in mortality for each one unit increase in PNI when PNI < 50.3. The degree of reduction reported by other studies was lower or not clearly quantified4,14,23,24. The mortality was 30% (636/2115) in our study, which was higher than in other studies4,14,23,24. Studies with extended follow-up periods may have observed more interference from PNI-related and non-PNI-related factors. We think that the length of the follow-up period may affect the statistical results of the mortality rate.
The relationship between PNI and morbidity and mortality in elderly hip fracture patients is a combination of nutritional, immune and inflammatory interactions. Low PNI values reflect poor general health in patients, resulting in a significantly higher risk of post-operative complications and death25,26. The potential mechanisms were the following. First, low PNI reflects malnutrition status, including low serum albumin. Albumin is an important indicator of nutritional status, and its decline usually indicates inadequate protein intake, metabolic disturbances or insufficient energy reserves. Elderly hip fracture patients are prone to malnutrition, delayed wound healing, poor fracture healing, and increased risk of post-operative complications and length of stay27. Second, a low PNI reflects immunosuppression; the lymphocyte count in the PNI is an important measure of immune status28, and a low PNI usually means that a patient’s immune function is impaired. The immune system of elderly patients is already more fragile, and the immunosuppressive state is further exacerbated by fractures and surgical trauma28. In addition, the traumatic inflammatory response triggered by a fracture further depletes immune resources, decreasing lymphocytes and reducing the body’s ability to fight infections29. Third, elderly hip fracture patients often have chronic underlying medical conditions (e.g., cardiovascular disease, diabetes, etc.) that can further exacerbate a decreased PNI30,31. A low PNI state may exacerbate the overall vulnerability of the body, making it more difficult for patients to withstand the traumatic stresses associated with fractures and surgery32. However, this effect from PNI was minimal when the PNI reached 50.3. Therefore, it is necessary to clarify that interventional studies of albumin support, anti-inflammatory therapy, and immune-enhancing therapies are threshold effects in the future. Based on the above mechanisms, the following interventions may help to improve patient prognosis: preoperative optimization of nutrition, preoperative strengthening of immunity, and adjusting nutritional support strategies in conjunction with PNI levels to avoid further nutritional deterioration. In fact, a meta-analysis showed that oral nutritional supplementation could nearly reduce the risk of total complications, improve serum albumin and shorten stay in hospital33.
PNI is a comprehensive indicator that reflects the patient’s nutritional status and immune function, and a lower PNI predicts an increased mortality rate. PNI not only aids surgeons in better-assessing patients’ nutritional and immune status but also provides clinical evidence for preoperative risk stratification and personalized treatment strategy. Early intervention and comprehensive management could help to improve post-operative outcomes, reduce mortality, and enhance the quality of life32,33,34,35,36.
Surely, there are some potential limitations in the study. First, post-operative osteoporosis treatment was important to the prognosis for hip fractures. However, due to long time spans, patients or their families cannot accurately remember detailed anti-osteoporosis medication information. Thus, there is significant information bias in anti-osteoporosis treatment, and we could not obtain accurate information. Second, due to pain and difficulty with transportation after fracture, we rarely performed bone mineral density (BMD) testing, in which hip BMD was an independent risk factor for post-operative mortality following injury37. Third, since the patients were not hospitalized at the time of death, or even if hospitalized, no autopsy was performed, the final cause of death was difficult to determine. These factors would introduce information bias. Therefore, it would be better to expand the sample size to cover more regions and ethnic populations to improve the extrapolation of the findings.
Conclusion
PNI is a vital predictor of mortality for patients with hip fractures. We found that 50.3 was a significant clinical inflection point. When the PNI is less than 50.3, the mortality decreases as the PNI increases. When PNI is more than 50.3, the mortality rate tends to be stable and maintained at a low level. Therefore, PNI should be assessed when the elderly hip fractures for preoperative risk stratification and beyond its threshold.
Data availability
Xi’an Honghui Hospital implemented the data. According to relevant regulations, the data could not be shared but could be requested from the correspondence author.
References
Bhandari, M. & Swiontkowski, M. Management of acute hip Fracture[J]. N Engl. J. Med. 377 (21), 2053–2062 (2017).
Berry, S. D., Kiel, D. P. & Colón-Emeric, C. Hip fractures in older adults in 2019[J]. JAMA 321 (22), 2233–2234 (2019).
Zanetti, M. et al. Poor nutritional status but not cognitive or functional impairment per se independently predict 1 year mortality in elderly patients with hip-fracture[J]. Clin. Nutr. 38 (4), 1607–1612 (2018).
Wang, Y. et al. Prognostic nutritional index with postoperative complications and 2-year mortality in hip fracture patients: an observational cohort study[J]. Int. J. Surg. 109 (11), 3395–3406 (2023).
Malafarina, V. et al. Nutritional status and nutritional treatment are related to outcomes and mortality in older adults with hip Fracture[J]. Nutrients 10 (5), 555 (2018).
Rempel, A. N., Rigassio Radler, D. L. & Zelig, R. S. Effects of the use of oral nutrition supplements on clinical outcomes among patients who have undergone surgery for hip fracture: A literature review[J]. Nutr. Clin. Pract. 38 (4), 775–789 (2023).
Dagnelie, P. C., Willems, P. C. & Jørgensen, N. R. Nutritional status as independent prognostic factor of outcome and mortality until five years after hip fracture: a comprehensive prospective study[J]. Osteoporos. Int. 35 (7), 1273–1287 (2024).
Yokoyama, K., Ukai, T. & Watanabe, M. Effect of nutritional status before femoral neck fracture surgery on postoperative outcomes: a retrospective study[J]. BMC Musculoskelet. Disord. 22 (1), 1027 (2021).
Zhou, Y. et al. Modified frailty index combined with a prognostic nutritional index for predicting postoperative complications of hip fracture surgery in Elderly[J]. J. Invest. Surg. 35 (10), 1739–1746 (2022).
Li, J. et al. Preoperative albumin-to-globulin ratio and prognostic nutritional index predict the prognosis of colorectal cancer: a retrospective study[J]. Sci. Rep. 13 (1), 17272 (2023).
Shi, J. et al. Cholesterol-modified prognostic nutritional index (CPNI) as an effective tool for assessing the nutrition status and predicting survival in patients with breast cancer[J]. BMC Med. 21 (1), 512 (2023).
Zhang, L. et al. Prognostic nutritional index as a prognostic biomarker for Gastrointestinal cancer patients treated with immune checkpoint inhibitors[J]. Front. Immunol. 14, 1219929 (2023).
Popp, D. et al. Predictive feasibility of the Graz malnutrition screening, controlling nutritional status score, geriatric nutritional risk index, and prognostic nutritional index for postoperative Long-Term mortality after surgically treated proximal femur Fracture[J]. Nutrients 16 (24), 4280 (2025).
Chen, Y. M. et al. Prognostic nutritional index (PNI) is an independent predictor for functional outcome after hip fracture in the elderly: a prospective cohort study[J]. Arch. Osteoporos. 19 (1), 107 (2024).
Katsuyama, Y. et al. Development and Validation of a Prognostic Scoring System for 1-year Mortality in Older Patients with Hip fractures[J]53afae195 (Age & Ageing, 2024). 9.
Ning, Y. et al. Association of prognostic nutritional index with the risk of all-cause mortality and cardiovascular mortality in patients with type 2 diabetes: NHANES 1999–2018[J]. BMJ Open. Diabetes Res. Care. 11 (5), e003564 (2023).
Tsuda, S. et al. The association of controlling nutritional status score and prognostic nutritional index with cardiovascular diseases: the Fukuoka kidney disease registry Study[J]. J. Atheroscler Thromb. 30 (4), 390–407 (2022).
Xu, Y. et al. Association between nutrition-related indicators with the risk of chronic obstructive pulmonary disease and all-cause mortality in the elderly population: evidence from NHANES[J]. Front. Nutr. 11, 1380791 (2024).
Zhang, W. S. et al. The heart rate on admission was associated with the mortality in elderly patients with hip fractures: a retrospective cohort study from a trauma centre in Northwestern China[J]. BMJ Open. 15 (1), e093662 (2025).
Zhang, Y. N., Xiao, P. & Zhang, B. F. The association between preoperative serum cholinesterase and all-cause mortality in geriatric patients with hip fractures: a cohort study of 2387 patients[J]. Perioperative Med. 13 (1), 82 (2024).
Zhang, B. F. et al. Early admission is better-the time to admission (TTA) is associated with one-year mortality in hip fracture[J]. Int. J. Surg. 110 (12), 7880–7888 (2024).
Mathew, G. et al. STROCSS. : Strengthening the reporting of cohort, cross-sectional and case-control studies in surgery[J]. Int J Surg, 2021, 96: 106165. (2021).
Arslan, K. et al. Predictive value of prognostic nutritional index on postoperative intensive care requirement and mortality in geriatric hip fracture patients[J]. North. Clin. Istanb. 11 (3), 249–257 (2024).
Yilmaz, S., Kurt, M. & Dülgeroğlu, T. C. Investigation of the predictive value of systemic immune inflammation index (SII) and prognostic nutritional index (PNI) on mortality in patients with endoprosthesis after hip fracture[J]. Med. (Baltim). 103 (18), e38063 (2024).
Jia, S. et al. The predictive value of the prognostic nutritional index for all-cause mortality and cardiovascular mortality in frail population: insights from NHANES 2007–2018[J]. J. Nutr. Health Aging. 28 (5), 100216 (2024).
Letois, F. et al. Nutrition and mortality in the elderly over 10 years of follow-up: the Three-City study[J]. Br. J. Nutr. 116 (5), 882–889 (2016).
Zhang, W. et al. Association between preoperative serum albumin levels and length of stay in elderly patients with hip fractures: A nonlinear relationship[J]. Medicine 104 (2), e41200 (2025).
Vural, A., Dolanbay, T. & Yagar, H. Hemoglobin, albumin, lymphocyte and platelet (HALP) score for predicting early and late mortality in elderly patients with proximal femur fractures[J]. PLoS ONE [Electronic Resource]. 20 (1), e0313842 (2025).
Sedlář, M. et al. Early and Subacute Inflammatory Response and long-term Survival after Hip Trauma and surgery[J]60431–436 (Archives of Gerontology & Geriatrics, 2015). 3.
Tang, J. et al. Prognostic nutritional index as a predictor of cardiovascular and all-cause mortality in American adults with hypertension: results from the NHANES database[J]. Front. Cardiovasc. Med. 11, 1465379 (2025).
Zhang, J. et al. Prognostic nutritional index as a risk factor for diabetic kidney disease and mortality in patients with type 2 diabetes mellitus[J]. Acta Diabetol. 60 (2), 235–245 (2022).
Fabian, E. et al. Nutritional supplementation affects postoperative oxidative stress and duration of hospitalization in patients with hip fracture[J]. Wien Klin. Wochenschr. 123 (3–4), 88–93 (2011).
Chen, B. et al. Effect of oral nutritional supplementation on outcomes in older adults with hip fractures and factors influencing compliance[J]. Bone Joint J., 105–B (11): 1149–1158. (2023).
Liu, M. et al. The role of perioperative oral nutritional supplementation in elderly patients after hip surgery[J]. Clin. Interv. Aging. 10, 849–858 (2015).
Malafarina, V. et al. Effectiveness of nutritional supplementation on sarcopenia and recovery in hip fracture patients. A multi-centre randomized trial[J]. Maturitas 101, 42–50 (2017).
Eneroth, M., Olsson, U. B. & Thorngren, K. G. Nutritional supplementation decreases hip fracture-related complications[J]. Clin. Orthop. Relat. Res. 451, 212–217 (2006).
Ge, Y. et al. Association between hip bone mineral density and mortality risk after hip fracture: A prospective cohort Study[J]. Calcif Tissue Int. 113 (3), 295–303 (2023).
Acknowledgements
Not applicable.
Funding
This work was supported by the Foundation of Xi’an Municipal Health Commission (Grant Number: 2024ms15) and the Innovative Promotion Program - Science and Technology Innovation Team (2024RS-CXTD-86).
Author information
Authors and Affiliations
Contributions
According to the definition given by the International Committee of Medical Journal Editors (ICMJE), the authors listed above qualify for authorship based on making one or more of the substantial contributions to the intellectual content of the following: Conceived and designed the study: Bin-Fei Zhang.Performed the study: Peng Yang, Lin Liu, Zhi Yang and Bin-Fei ZhangAnalyzed the data: Peng Yang and Bin-Fei ZhangWrote the manuscript: Peng Yang and Bin-Fei ZhangAll authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Honghui Hospital, Xi’an Jiaotong University (No. 202201009).
Consent to publish
The work described has not been published before (except in the form of an abstract or as part of a published lecture, review, or thesis); it is not under consideration for publication elsewhere, and all co-authors have approved its publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yang, P., Liu, L., Yang, Z. et al. Threshold effect of prognostic nutritional index on mortality in geriatric hip fracture patients. Sci Rep 15, 22241 (2025). https://doi.org/10.1038/s41598-025-08123-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-08123-x