Abstract
Cisplatin is a widely used, effective chemotherapy drug. However, its application is often limited by severe side effects, including testicular toxicity. Cisplatin-induced testicular damage is primarily driven by oxidative stress and inflammation. Ferroptosis has recently been identified to contribute to cisplatin-testicular toxicity. Morin hydrate (MH) is a naturally occurring flavonoid known for its powerful antioxidant, anti-inflammatory, and anti-apoptotic properties. The study was designed to evaluate the protective effects of MH against cisplatin-induced testicular toxicity in Wistar albino rats. Rats were given MH 50 mg/kg, p.o. daily for fourteen days, seven days before the injection of cisplatin 8 mg/kg. Assessment of sperm quality, testosterone, luteinizing hormone levels, and oxidative stress markers were carried out. Also, steroidogenesis and ferroptosis-related gene expressions were assessed. Results: Our findings demonstrated that MH significantly corrected the antioxidant/oxidant balance, evidenced by increased superoxide dismutase, glutathione peroxidase, and Nrf2/heme oxygenase-1 (HO-1) expression and reduced malondialdehyde in testicular tissue. Also, MH ameliorated the negative changes in sperm quality, hormone levels, and testicular histology induced by cisplatin, and this was accompanied by upregulation of steroidogenesis gene expressions (17β-HSD, 3β-HSD, and star). Moreover, MH inhibited cisplatin-induced ferroptosis via the modulation of ferroptosis genes’ expression (ACSL4, SLC7A11, and TFRC) and the reduction of iron accumulation in testicular tissue. Conclusion: MH effectively protected against cisplatin-induced testicular toxicity by reducing oxidative stress and inhibiting ferroptosis signalling. This study points out that MH might mitigate iron-mediated apoptosis through the downregulation of Nrf2/HO-1 signaling, providing a potential therapeutic strategy for preventing infertility in male patients undergoing cisplatin chemotherapy.
Similar content being viewed by others
Introduction
Cisplatin (CIS) is a platinum-based chemotherapy agent with broad antitumor activity against solid tumours, including testicular, ovarian, bladder, and lung cancers1. Despite being indispensable in oncology2,3. The clinical efficacy of cisplatin is often compromised by its dose-limiting side effects due to its inability to distinguish between cancerous and normal cells; one of the biggest concerns is testicular toxicity4. This toxicity is significant in young patients, as it can lead to infertility due to damage to the testicular tissue, resulting in impaired spermatogenesis and disruption of testosterone production5,6. The underlying mechanisms of CIS-induced testicular damage are multifaceted, involving oxidative stress, apoptosis, and inflammation7,8,9. One of the main causes of testicular injury is oxidative stress. This condition arises when the excessive production of reactive oxygen species (ROS) surpasses the antioxidant defense systems in testicular cells, resulting in cellular damage8,10,11.
Additionally, ferroptosis has been recently identified as a key pathway in CIS-induced tissue damage12. Ferroptosis is a regulated non-apoptotic cell death triggered by iron metabolism and lipid peroxidation. In ferroptosis, the accumulation of free iron can exacerbate oxidative damage, leading to lipid peroxidation, destruction of the lipid membrane, and subsequent cell death, contributing to testicular cell degeneration13,14,15. Notably, heme oxygenase-1 (HO-1) has been discovered to be a critical factor in ferroptosis. HO-1 is a stress-responsive enzyme that modulates oxidative stress and iron metabolism16,17, and its downregulation might contribute to iron dysregulation and ferroptosis2,3 and, consequently, exacerbation of testicular damage. Understanding the interplay between oxidative stress, steroidogenesis, and ferroptosis in CIS-induced testicular toxicity is yet to be demonstrated. Moreover, the role of HO-1 in iron-mediated cell death in this context is underexplored.
To counteract the deleterious effects of CIS, attention has shifted toward potential protective agents that can mitigate testicular toxicity without compromising the anticancer efficacy of CIS. Among the various agents studied, morin hydrate (MH), a naturally occurring flavonoid, has shown promising results. MH possesses strong antioxidant, anti-inflammatory, and anti-apoptotic properties, making it a suitable candidate for protecting against CIS-induced toxicities18,19. Studies have demonstrated that MH can reduce oxidative damage, preserve testicular architecture, and improve sperm quality in different animal models of testicular toxicity20,21,22. In addition, MH has been shown to restore the activity of superoxide dismutase (SOD), and catalase downregulated by CIS in both the renal and the hepatic tissues23,24. Despite the promising protective effects of MH, the specific molecular pathways of protection, particularly concerning ferroptosis, are not well understood. Studies to date have focused on the overall reduction of oxidative stress and histopathological improvements in testicular tissue without delving into the precise molecular signalling pathways involved.
Therefore, this manuscript aims to address these critical knowledge gaps by investigating the protective effects of MH on CIS-induced testicular toxicity in rats, particularly the modulation of oxidative stress, inflammatory responses, and ferroptosis. We will also investigate the interplay between the HO-1 and ferroptosis signalling pathways in the protection afforded by MH against CIS-induced testicular damage. By providing a deeper understanding of these mechanisms, this study aims to advance the development of therapeutic strategies that can protect male fertility in cancer patients undergoing CIS chemotherapy without compromising the drug’s antitumor efficacy.
Materials and methods
Drugs and chemicals
The chemotherapeutic agent CIS, used to induce testicular damage, was obtained from EBEWE Pharma (GmbH. Nfg. KG, Australia). MH (M4008, CAS number 654055-01-3) was purchased from Sigma Aldrich (St. Louis, MO, USA). Other chemicals used were of high analytical grade, sourced from Merck (Darmstadt, Germany) or Sigma-Aldrich (St. Louis, MO), and prepared according to standard protocols.
In-vivo study
Animals and experimental design
Thirty-two adult male Wistar albino rats (150–200 g) from the Bio-Resource Unit at the College of Pharmacy, King Saud University, Saudi Arabia, were used. Rats were housed at a standard temperature and humidity with a 12-hour light/dark cycle, and they had free access to food and water. The experiment’s design was carried out in accordance with the recommendations of the Institutional Animal Care and Use Committee (IACUC), and the study protocol was approved by the Research Ethics Committee at King Saud University (KSU-SE-23-115) and the Institutional Review Board, King Abdullah Bin Abdulaziz University Hospital (24–0146). Rats were randomly divided into four groups (8 rats/group) as follows: Group I (Control): rats were daily given the vehicle solution for 14 days and were injected with saline on the 7th day i.p.; Group II (CIS): Rats were given vehicle solution orally for 14 days, and were injected with a single dose of CIS (8 mg/kg) (i.p.)25, on the 7th day of the experiment. Group III (CM): rats were given MH (50 mg/kg BW in normal saline) orally by oral gavage for 14 days23, seven days before and after CIS injection (8 mg/kg, i.p.) on the 7th day of the experiment. Group IV (M): rats were given MH (50 mg/kg BW in normal saline) orally by oral gavage for 14 days.
Twenty-four hours post-injection (on day 15), the rats were anesthetized using carbon dioxide (CO2). The blood samples were collected via cardiac puncture under anaesthesia, using sterile syringes to ensure minimal stress and contamination. The samples were then transferred into appropriate tubes for serum separation. Blood samples were centrifuged at 3000 rpm at 4 °C for 30 min to obtain clear sera, which were then stored at -80 °C. The testes were immediately excised, weighed, and washed. The collected testes were divided into several parts: the first part of the testis tissues was fixed in 10% neutral buffered formalin for histological and immunohistochemical analysis. Other parts of the testis samples were kept at -80 °C for biochemical and molecular analysis.
Sperm count and morphology
At the end of the experiment, after the rats were euthanized, the cauda epididymis was extracted and sliced. Subsequently, it was immersed in 2 mL phosphate-buffered saline (PBS) at a pH of 7.4, maintained at 37 °C. The sperm suspension was diluted with PBS (pH 7.2) at a 1:20 ratio. Total sperm count was determined using a hemocytometer. Sperm viability and the total number were counted in five squares and multiplied by 106 to obtain the final volume26. Also, epididymal sperm morphology was assessed by staining a smear using hematoxylin and eosin (H and E) and examination using a light microscope at 1000X.
Determination of testosterone and luteinizing hormones (LH)
The levels of testosterone and LH were measured in serum using highly sensitive enzyme-linked immunosorbent assay (ELISA) kits (Milpitas and Northbrook, USA).
Histopathological and immunohistochemical (IHC) examination
The testis’ samples fixed in formalin were stained with H and E, and they were studied using a light microscope to evaluate spermatogenesis. They were classified using Johnsen’s criteria27. The germinal epithelium of the tubules was assessed for separate testes, and the mean Johnsen score was calculated for different rats. Also, areas and volumes of seminiferous tubules in the testes were measured.
The IHC analysis was used to examine the changes in the immunoreactivity of testicular Nrf2 and HO-1 expression using anti-Nrf2 (Proteintech 16396-AP, Germany-diluted 1:300) and anti-HO-1 (ab13248—Abcam, diluted 1:200). The detailed methodology is provided as a supplementary file.
Assessment of oxidative stress and inflammatory biomarkers in testicular tissues
Testicular malondialdehyde (MDA), glutathione peroxidase (GPx), and superoxide dismutase (SOD) activity were measured using kits from Biodiagnostics (Giza, Egypt) according to the manufacturer’s instructions. Meanwhile, the expression levels of tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6) were measured by ELISA kits from Sigma-Aldrich (St. Louis, MO, USA), catalogue number (RAB0480), and from Abcam (Cambridge, UK), catalogue number (ab234570), respectively.
Assessment of testicular ferrous level
The testicular ferrous level was measured using a kit from BioDiagnostic (Giza, Egypt), according to the manufacturer’s instructions.
Quantification of mRNA expression by real-time polymerase chain reaction (RT-PCR) for Steroidogenesis and ferroptosis related genes
Variations in the gene expression of steroidogenesis-related genes; 17β-Hydroxysteroid dehydrogenases (17β-HSD), 3β-Hydroxysteroid dehydrogenases (3β-HSD), and steroidogenic acute regulatory protein (STAR) and ferroptosis-related genes; acyl-CoA synthetase long-chain family 4 (ACSL4), transferrin receptor 1 (Tfr1) gene (TFRC), and the cystine/glutamate antiporter (SLC7A11), were determined by RT-PCR. The reactions utilized the SYBR Green qPCR Master Mix Kit (Applied Biosystems by Thermo Fisher Scientific Inc., Warrington, UK) along with the primer pairs listed in Table 1 and Glyceraldehyde 3-phosphate dehydrogenase (GAPDH) (Cat. No. PCR-PDA-HSA-GAPDH-12) as the reference gene (HavenSci, Innovation Center, KAUST, Thuwal 23955, Saudi Arabia). The detailed method is provided as supplementary material.
In-vitro study
Cell culture and treatment
Both the non-tumorigenic cell line (MCF-10 A) and the breast cancer cell line (MCF-7) were obtained from the Natural and Health Sciences Research Centre in Riyadh, Saudi Arabia. All cell lines were passed in a humidified incubator at 37 °C with 5% CO2 after being cultivated in their DMEM media with 10% FBS, 100 U/mL penicillin, and 100 µg/mL streptomycin. According to conventional protocols, cells were trypsinized and passed at 80–90% confluence.
Determination of anticancer activity and cytotoxicity
The MTT (3-[4,5-dimethylthiazol-2-yl]-2,5 diphenyl tetrazolium bromide) assay was used to assess the anticancer activity and cytotoxicity of CIS alone and in combination with MH (CM). The MCF-7 and MCF-10 A cells were plated in 96-well plates (5000 cells/well) and given 24 h to adhere. For 72 h, cells were treated with serial dilutions of CIS, MH, and CM. 20 µL of 20 mM MTT dissolved in PBS was added after the old media was replaced, and the mixture was incubated for three hours at 37 °C with 5% CO2. After carefully removing the MTT solution, 100 µL of dimethyl sulfoxide (DMSO) was added to dissolve the violet formazan crystals. Cell viability as a proportion of untreated cells was used to express the findings. Half-maximal inhibitory concentration (IC50) for CIS, M, and CM was calculated to evaluate the anticancer activity.
Selectivity index (SI)
To verify the effect of MH on the SI of CIS against cancer cells, we also examined the cytotoxic effect on the non-tumorigenic cell line MCF10A. We calculated the selectivity ratio of non-cancerous cells (MCF10A) to cancer cells (MCF-7) using a specified formula: SI = IC50 of normal cells/IC50 of cancer cells.
A SI value ≥ 10 was assumed to belong to a selected promising agent that can be further studied. Evaluating the anti-cancer activity of a compound without considering its selectivity index (SI) is a poor predictor for further clinical studies. The ideal therapeutic agent should preferentially target and kill cancer cells while sparing normal cells28.
Statistical analysis
The results are presented as the mean ± standard error of the mean (SEM). Statistical analysis and multiple comparisons were conducted using one-way ANOVA followed by the Tukey post-hoc test with GraphPad Prism 9. The results were considered significant if the P value < 0.05.
Results
Effect of MH and CIS on changes in body weights and testicular weight
The results showed that the group treated with MH alone had outcomes similar to the control group across all evaluated parameters, indicating that MH treatment does not negatively impact testicular function. In comparison to the control group, rats treated with CIS exhibited a significant decrease in body weight change comparable to the control group (49.7%, P < 0.01). However, treatment with MH significantly mitigated body weight change as compared to the CIS group (62.6%, P < 0.01). As well as, MH alone in the M group didn’t show a significant change compared to the control group. Furthermore, there was no significant change in testis weight between all treated groups (Fig. 1). The testis index (testis weight/body weight ratio) was significantly elevated in rats treated with CIS, as compared to the control group (16.7%, P < 0.01). However, treatment with MH significantly mitigated the testis index change as compared to the CIS group (12.3%, P < 0.05).
Effect of morin hydrate and cisplatin on changes in body weights and testicular weight. data are expressed as mean ± SEM, n = 6. a and b indicate statistical differences from the control and CIS group, respectively, (p < 0.05) using ANOVA followed by Tukey Kramer as a post hoc test. CIS cisplatin, CM cisplatin and morin hydrate, M morin hydrate.
Effect of MH and CIS on sperm indices and hormonal assays
Table 2 shows that rats treated with CIS showed a significant (P < 0.001) reduction in sperm count and viability (Table 2), along with a notable increase in the percentage of sperm with morphological abnormalities compared to the control group, as clear in Fig. 2. However, the simultaneous administration of M to CIS-treated rats significantly amended (P < 0.001) sperm count, viability, and mortality ratio (Table 2) and reduced the percentage of abnormal sperm morphology.
Effects of Morin Hydrate and Cisplatin on Sperm Morpholology and Testosterone and Luteinizing Hormone Levels in Rats. Photomicrograph of Sperm in Different Groups. (A) control epidydimal sperm showing normal rat sperm, head (black arrow), hook (green arrow), straight tail (red arrow). (B) epidydimal sperm treated with cisplatin displaying deformed rat sperm, distorted head (black arrow), and bent tail (red arrow). (C) photomicrograph of epidydimal sperm in cisplatin and morin hydrate treated group showing some deformed rat sperm, bent tail (red arrow), flattened hook (green arrow). (D) photomicrograph of epidydimal sperm treated with morin hydrate revealing healthy rat sperm, head (black arrow), hook (green arrow), straight tail (red arrow) (H&E-1000X). (E) Testosterone hormone level in different groups. (F) LH hormone level in different groups. Data were expressed as mean ± SEM (n = 6). a, b and c indicate statistical differences from the control, CIS and CM group, respectively (p < 0.05) using ANOVA followed by Tukey Kramer as a post hoc test. CIS cisplatin, CM cisplatin and morin hydrate, M morin hydrate, LH Luteinizing hormone.
As indicated in Fig. 2, CIS treatment caused a considerable reduction in serum reproductive hormones’ levels, either testosterone (41.1%) (3.32 ± 0.12 vs. 8.06 ± 0.18, P ≤ 0.001) and LH (74.2%) (21.2 ± 1.63 vs. 80.3 ± 3.8, P < 0.001 ng/ml) relative to control rats. Notably, treatment of the CIS-exposed rats with MH significantly increased serum levels of testosterone (5.97 ± 0.68 vs. 3.49 ± 0.2 ng/ml, P < 0.001) and LH (60.5 ± 3.7 vs. 21.2 ± 1.63 ng/ml, P < 0.001).
Effect of MH on CIS-induced testicular histopathological changes according to Johnsen score
Seven days following i.p CIS-injection, the toxic effects of CIS on testicular tissues were confirmed by histopathological examination. In untreated control and MH-treated groups, testes showed the normal structure of seminiferous tubules surrounded by interstitial tissues filled with Leydig cells; seminiferous tubules were scored 10 when filled with a complete set of spermatogenesis stages (Fig. 3A,D), and thus the Johnsen Score was 10 in the two previous groups. Meanwhile, seminiferous tubules of rats treated with CIS displayed a marked decrease in areas and volumes, the majority of spermatogenesis stages were absent (Fig. 3B), and the pathological Johnsen Score was very low, reaching 5. Moreover, rats in the CM group revealed obvious improvement in most of the stages that appeared, except necrotic foci (Fig. 3C), and raised the Johnsen Score to reach 9.
Photomicrograph of control testes showing normal seminiferous tubules, interstitial tissue (IT), Leydig cells (black arrow), spermatogonia (green arrow), spermatocyte A (blue arrow), spermatocyte B (yellow arrow), spermatozoa (brown arrow), and Sertoli cell (red arrow). Photomicrograph of testes tissues from rat in cisplatin group displaying minimized seminiferous tubules and necrotic foci (N), while the testes in cisplatin and morin hydrate treated group showing improved seminiferous tubules (ST), necrotic foci (N), testes from morin hydrate treated group revealing healthy seminiferous tubules, IT, spermatogonia (green arrow), spermatocyte A (blue arrow), spermatocyte B (yellow arrow), and spermatozoa (brown arrow) (H&E-400X).
On the other hand, in the assay for areas and volumes of seminiferous tubules in testes, there was a significant reduction (P < 0.01) in the area and volumes in the CIS-treated group as compared to the control group. At the same time, there was no significant improvement in the areas and volumes in CM treated with MH (Table 3).
Morin hydrate attenuated the oxidative stress and inflammatory biomarkers in testicular tissues in rats treated with cisplatin
The levels of GPX and MDA in testicular tissue, along with SOD activity across the various treatment groups, are depicted in Fig. 4. When compared to the healthy control group, rats treated with CIS exhibited a notable decrease in SOD activity (57.5 ± 2.08 vs. 79.7 ± 2.38, P ≤ 0.01) Figure (4-a) and GPX levels (1 ± 0.04 vs. 1.55 ± 0.07 U/g, P ≤ 0.01) Figure (4-b). In contrast, MDA levels significantly increased (151 ± 6.3 vs. 114 ± 2.6 mmol/g, P ≤ 0.01), Figure (4-c). MH treatment mitigated oxidative stress compared to CIS. The GPX levels (1.61 ± 0.12 vs. 1 ± 0.04, P ≤ 0.001) and SOD activity (82.7 ± 5.6 vs. 57.5 ± 2.08, P ≤ 0.001) Fig. 4 (a & b), respectively, were significantly higher in the MH-treated group compared to the CIS group. However, no significant change was observed in MDA levels between the two groups. Administration of MH had noticeable effects on the oxidative stress parameters, with a significant increase in SOD activity (107 ± 2.28 vs. 79.7 ± 2.3, P ≤ 0.01) and GPX levels (1.74 ± 0.04 vs. 1.55 ± 0.04 U/g, P ≤ 0.001) compared to the control group Fig. 4 (a & b), along with a significant decrease in MDA levels (97.2 ± 6.3 vs. 114 ± 2.6 mmol/g, P ≤ 0.001) Figure (4-c).
Morin hydrate attenuates oxidative stress and inflammatory response in cisplatin-induced testicular toxicity in rats. Treatment of rats with 8 mg/kg CIS on day 7 decreased (a) SOD & (b) GPX in the CIS group, increased testes, (c) MDA and (d) TNF-α, and decreased (e) IL-6 levels. Data are mean ± SEM (n = 6). a, b, and c were found to be statistically significant when compared to the control, CIS, and CM groups, respectively (P < 0.05), using ANOVA followed by Tukey-Kramer as a post hoc test. CIS cisplatin, CM cisplatin and morin hydrate, M morin hydrate, MDA malondialdehyde, SOD superoxide dismutase, GPX glutathione peroxidase, TNF-α tumor necrosis factor-α, IL-6 interleukin-6.
As anticipated, the CIS group exhibited a significant increase in TNF-α levels compared to the control group (56.1 ± 2.7 vs. 34.2 ± 1.69 pg/ml, P ≤ 0.001). At the same time, there was a significant decrease in IL-6 level in testes in the CIS group compared to the control group (37.2 ± 0.7 vs. 54.5 ± 3.02 pg/ml, P ≤ 0.001). On the contrary, Fig. 4d and e showed the treatment with MH resulted in a significant reduction of CIS-induced inflammatory effects in TNF- α (39 ± 0.42 vs. 56.1 ± 2.7, P ≤ 0.001), and there was an increase in IL-6 in MH-administered rats as compared to CIS group (52.3 ± 1.5 pg/ml, P ≤ 0.001) Fig. 4d and e respectively.
Morin hydrate attenuated the cisplatin-induced changes in Nrf2 and HO-1 expression
In the present study, CIS caused a significant downregulation of both testicular Nrf2 and HO-1 expression by 87% and 71.9%, respectively, compared to the control group (Figs. 5B and 6B). However, co-treatment with MH led to an upregulation of Nrf2 and HO-1 expression by 74.65% and 53.17% (P < 0.05), respectively, relative to the CIS group (Fig. 5).
Photomicrographs of Nuclear factor erythroid 2-related factor-2 (Nrf2) and Hemeoxygenase-1 (HO-1), immunostained testis sections, Scale bar 25 µ and 50 µ, respectively. (A) The control rat showed a normal immune reaction, and (B) the section from a rat exposed to CIS showed a marked decrease in the immune reactivity in testis cells. (C) Testis section from rats exposed to CIS and morin, showing recovery of the immune reactivity in the testis cells. (D) Quantitative immunoexpression of Nrf2. Data are mean ± SEM (n = 6). a and b were found to be statistically significant compared to the control and CIS groups, respectively, P < 0.05 using ANOVA followed by Tukey-Kramer as a post hoc test. CIS cisplatin, CM cisplatin and morin hydrate. Black Circle: high expression of Nrf-2, Red Star: High expression of HO-1.
Morin Hydrate Increased (a) STAR, (b) 3β-HSD, (c) 17β-HSD, (d) TFRC, and (f) SLC7A11 mRNA, and Suppressed that of (g) ACSL4 in CIS-induced Testicular Toxicity in Rats. Data are mean ± SEM, (n = 3). a and b were found to be statistically significant when compared to the control and CIS groups, respectively, P < 0.05 using ANOVA followed by Tukey Kramer as a post hoc test. (h) MH decreased the ferrous overload induced by CIS in rats. Data were expressed as mean ± SEM (n = 6). a, b, and c were found to be statistically significant when compared to the control, CIS, and CM group, respectively, P < 0.05 using ANOVA followed by Tukey Kramer as a post hoc test. CIS cisplatin, CM cisplatin and morin hydrate, M morin hydrate.
Morin hydrate modulates cisplatin-induced changes in mRNA expression of steroidogenesis and ferroptosis-related genes and testicular ferrous level
The mRNA expression of StAR, 3β-HSD, 17β-HSD, TFRC, and SLC7A11 genes was significantly declined (P ≤ 0.001) in the CIS group as compared to the control group (Fig. 6a-f), respectively; it is noted that the administration of MH has a significant impact on the expression of these genes. On the other hand, CIS caused a significant elevation (P ≤ 0.001) in ACSL4 mRNA expression, which was relatively corrected with MH supplementation (Fig. 6g). The ferrous level was significantly elevated in the CIS group as compared to the control group, while there was a significant decrease in the MH-treated group as compared to the CIS and control groups (Fig. 6h).
Effect of morin hydrate on the anticancer activity and cytotoxicity of cisplatin
MH (when combined with CIS) was shown to potentiate the anticancer activity of CIS against cancer cells, as evidenced by the decrease in IC50 compared with CIS alone. While sparing normal cells from damage, leading to fewer side effects (Table 4).
The selectivity towards cancer was determined by assessing the cytotoxic effect of morin on a non-tumorigenic cell line, MCF10A. MH demonstrated a moderate anticancer efficacy against MCF-7 cells with Ic50 45 ± 0.7 µM, while CIS showed an excellent anticancer efficacy with Ic50 6.29 ± 1.29 µM. However, MH exhibited selectivity index values greater than CIS, indicating a higher selectivity towards cancer cells compared to non-cancerous cells (Fig. 7).
Discussion
CIS is an effective anticancer drug used for solid tumors and other malignancies. It belongs to platinum chemotherapeutic agents that interfere with DNA replication in cancer29. Despite its effectiveness, it can cause severe testicular damage, which eventually leads to male infertility in humans30,31 and animals32,33. Several studies indicate that plant-derived phytochemicals possess protective attributes against the tissue damage induced by anti-cancer drugs and may offer additional anti-cancer effects per se34,35,36. These attributes are primarily related to antioxidant, anti-inflammatory, and immunoregulatory mechanisms. MH is a natural phytochemical found in various plant families, particularly Moraceae37. It exhibits diverse therapeutic benefits against oxidative stress, inflammation, cognitive dysfunction, diabetes, and cancer19,37. Herein, we evaluated the role of MH in lessening CIS-induced testicular damage in rats, pointing to alterations in steroidogenesis, oxidative stress, ferroptosis, and inflammatory markers.
In this work, to induce acute testicular damage, a single dose of CIS was injected IP, and our results revealed that CIS significantly reduced BW while absolute testicular weight remained largely unchanged. Of note, CIS was administered as a single dose on day 7, with an acute effect but not long enough to alter testicular weight. Besides, the small size of the testes can, sometimes, make the detection of weight differences more challenging. Some studies reported no significant reduction in absolute testis weight after CIS administration31,38, and this was parallel with our finding, whereas others showed a reduction in the weight of the testes and the epididymides, and this reduction could be dose33 and time-dependent39.
Measuring other parameters, such as sperm indices, testicular morphology, and hormone levels, was the subsequent step to assess the impact of CIS on testicular functions. We found that CIS induced serious testicular alterations, evidenced by the destruction of seminiferous tubules, the site of sperm production, with severe necrotic foci. These alterations led to reductions in spermatogenesis, sperm count, and viability. Morphological abnormalities of epididymal45r sperm, such as head distortion, tail bending, and flattened hook, as well as degenerative alterations, were detected. Unlike ejaculated sperm, epididymal sperm are a prime choice for studying any changes in sperm quality and function due to their functional maturation and sample consistency. In addition, the epididymis is the site for sperm maturation, storage, and removal of deteriorating sperm40,41. Similarly, studies in rats exposed to CIS have shown a significant reduction in sperm count, motility, and viability by increasing DNA fragmentation42,43,44. Furthermore, CIS impairs spermatogenesis by destroying germ and Sertoli cells and decreasing the diameters of seminiferous tubules, leading to testicular atrophy and degeneration32,45,46. Morphological abnormalities in sperm, such as tail defects and head distortions, were also observed after CIS exposure7,44,47. According to Zhang et al., HE staining demonstrated that CIS increased the distance between the seminiferous tubules and disrupted the Leydig cells and spermatogonia. It further decreased the quantity of sperm in the epididymal duct39. These changes are attributed to the imbalance in oxidant-antioxidant levels, which cause oxidative damage to tissue proteins, lipids, and DNA. The long-term persistence of these abnormalities may result in permanent male infertility, especially with higher doses of CIS48.
In the context of hormones, rats that received CIS showed disruption in the pituitary-gonadal axis and an apparent reduction in testosterone and LH. They also exhibited a significant downregulation in testicular gene expression of 3β-HSD, 17ß-HSD, and STAR. These genes encode for gonadal proteins that have a major role in regulating steroidogenesis. In agreement with our findings, previous work showed that CIS decreases serum testosterone levels by inhibiting steroidogenic enzymes and reducing LH stimulatory effects11. It also suppresses the expression of key steroidogenic genes, including STAR10, and induces the proliferation of Leydig cells, thus testosterone production49,50. Testosterone synthesis occurs in Leydig cells under the influence of LH Stimulation. Indeed, StAR controls the rate-limiting step in steroidogenesis by facilitating cholesterol transport to the mitochondrial membrane51,52. Other enzymes, 3β-HSD and 17β-HSD, catalyze the subsequent steps involved in testosterone synthesis53.
Based on our findings, we revealed for the first time that MH ameliorated CIS-induced testicular injury by reversing changes in sperm indices, seminiferous tubules, and steroidogenesis. It also improved the sperm count, viability, and morphology, which was associated with its ameliorative effects on histological changes evidenced by the reduction in necrotic foci and improvement of areas and volumes of seminiferous tubules. Moreover, significant increases were found in steroidogenic hormones and genes in rats treated with CIS and MH. The ability of MH to ameliorate testicular damage caused by numerous toxicants, including titanium dioxide54, Bisphenol-A55, procarbazine20, acrylamide22, dutasteride-tamsulosin56, and bicalutamide57 has been previously reported, yet its effects on CIS-induced testicular damage need further investigation. Additionally, MH improves sperm parameters, including count, motility, and morphology20,57. Most of these studies revealed the protective effect of MH in preventing histopathological alterations in the sperm and testicular tissue, enhancing testosterone release, and sperm indices.
Given that oxidative stress plays a role in CIS-induced testicular injury, MH’s antioxidant properties may help to lessen such injury. CIS-intoxicated rats showed a significant increase in oxidative stress as it lowered GPX and SOD activity and elevated MDA levels in the testicular tissue. It also decreased HO-1 protein immunoexpression. CIS increases the production of ROS30,58, which induces testicular cell apoptosis44. Zhang has reported a significant increase in MDA and a decrease in the antioxidant SOD activity in a time-dependent manner39. Furthermore, CIS can hydrolyze into extremely reactive species that can interfere with mitochondrial oxidative phosphorylation, causing Ca++ overload and disturbing Ca++ homeostasis59. This is another possible cause of reducing the activity of antioxidant enzymes like GPX and SOD and increasing lipid peroxidation products60,61.
HO-1 plays a crucial role in protecting against CIS-induced nephrotoxicity. Studies have shown that HO-1 deficiency exacerbates CIS-induced renal injury in mice, while its induction or overexpression of HO-1 attenuates CIS-induced apoptosis and cytotoxicity62,63. HO-1 induction also alleviates CIS-induced reproductive toxicity in male rats by reducing oxidative stress and inflammation in the testes64. The protective effects of HO-1 are mediated through its antioxidant, anti-inflammatory, and anti-apoptotic properties65. On the other hand, simultaneous administration of MH with CIS restored the oxidative balance, upregulated HO-1 expression, and reduced inflammatory markers. According to earlier research, MH possessed antioxidant properties. Studies have shown that MH protects against CIS-induced renal damage through ameliorating oxidative stress, upregulating the Nrf-2/HO-1 signalling pathway, and inhibiting inflammation and apoptosis66. In rodent testes, it enhances the antioxidant defense protein level, mainly GSH level and enzyme activities such as SOD, GPX, and catalase, in a dose-dependent manner22. It also reduces lipid peroxidation that has been induced due to acrylamide22 and dutasteride-tamsulosin testicular toxicity56,61. These studies suggest that MH could be a potential therapeutic agent for preserving testicular function and fertility while minimizing oxidative stress in the face of various toxic insults.
Maintaining sufficient levels of iron plays a crucial role in spermatogenesis, testosterone synthesis, and fertility67,68. Within seminiferous tubules, the internal iron regulation cycle protects developing sperm cells from iron fluctuations69. Iron deficiency in testicular tissue can result in testosterone reduction, impaired spermatogenesis, and increased oxidative stress68,70. On the contrary, iron overload can also negatively impact testicular functions by triggering oxidative stress and ferroptosis, which involves iron-based lipid peroxidation67. Herein, we measured the effect of CIS on ferroptosis markers and assessed how MH might counteract this unique form of cell death. CIS-induced ferroptosis is evidenced by iron overload in the testes, and this was reported previously in CIS-induced testicular injury12, nephrotoxicity71, and ototoxicity72. Additionally, our findings indicate that a reduction in GPX4, a critical antioxidant enzyme dependent on GSH, increases lipid peroxidation and subsequent ferroptosis. CIS also altered the mRNA expression of genes involved in regulating ferroptosis, such as iron uptake, antioxidant defense, and lipid metabolism, particularly 8it/downregulated TFRC and SLC7A11 genes, and# upregulated ACLS4 gene expression.
The TFRC gene encodes for transferrin receptor 1, which is responsible for importing iron into the cells73. Downregulation of TFRC expression with CIS induced further Fe + 2 accumulation and increased iron-dependent lipid peroxidation74,75. In the current study, the downregulation of TFRC gene mRNA expression can be explained, as previously mentioned by Victor M Corral et al. They suggested that the TFRC mRNA degradation is regulated through the iron-responsive mechanism. In the presence of iron overload, the RNA binding of the iron regulatory proteins (IRPs) is suppressed, leading to increased TFRC mRNA degradation and decreased iron uptake76. Moreover, the SLC7A11 gene encodes the solute carrier family 7-member 11 protein, an amino acid transporter of cystine that is involved in GSH synthesis. As a negative regulator for ferroptosis, the inhibition of SLC7A11 can induce ferroptosis67. ACSL4 encodes for acyl-CoA synthetase long-chain family member 4, an enzyme that forms the precursors for phospholipid synthesis and is a positive regulator for ferroptosis77.
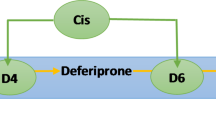
When MH was given alongside CIS, however, regular levels of these markers were restored. The iron overload was reduced, and normal expressions of ferroptosis genes were obtained. This suggested that MH could inhibit CIS-induced ferroptosis as one of the main mechanisms involved in testicular damage, Fig. 8. As far as we know, this work is the first of its kind to reveal the protective effect of MH against ferroptosis in CIS-induced testicular damage. Some studies used ferrostatin-1 (a ferroptosis inhibitor) or deferoxamine (an iron chelator) to protect against CIS-induced damage72,78. However, no studies have been found in the literature to investigate the ferroptosis signalling pathway as a protective mechanism of MH against CIS-induced testicular toxicity79. Therefore, ferroptosis inhibition has been identified as a potential treatment strategy to alleviate CIS-induced damage in various tissues, suggesting potential therapeutic strategies for preventing CIS-related toxicities.
A schematic diagram of the effect of morin on cisplatin-induced testicular toxicity. HO-1 Hemeoxygenase-1, MDA malondialdehyde, SOD superoxide dismutase, GPX glutathione peroxidase, TNF-α tumor necrosis factor-α, IL-6, interleukin-6, LH Luteinizing hormone, ACSL4 acyl-CoA synthetase long-chain family 4, TFRC transferrin receptor 1 (Tfr1) gene, SLC7A11 cystine/glutamate antiporter, 17β-HSD 17β-Hydroxysteroid dehydrogenases, 3β-HSD 3β-Hydroxysteroid dehydrogenases, STAR steroidogenic acute regulatory protein.
As a consequence of oxidative stress, CIS elevated the inflammatory cytokines, primarily TNF-α. However, this was not the case for IL-6, as our results revealed that CIS significantly reduced testicular IL-6 levels, while after MH administration, the levels of IL-6 increased. This can be explained by the dual role of IL-6 as a double-edged sword80,81. IL-6 promotes anti- and pro-inflammatory outcomes in the brain tissue depending on the levels, cellular source, and targets of the IL-6 itself80. In addition, IL-6 plays a crucial role in supporting the function of Sertoli cells and germ cells82,83. Despite the previous studies, there has not been any published research regarding the role of IL-6 in testicular dysfunction in rats treated with MH. Our results were in accordance with a study of CIS-induced testicular dysfunction, where no IL-6 immunoreactivity was detected in the testicular tissue. They proposed that CIS could directly influence the cells that produce IL-6 or the targeted cells, and the immunoreactivity of IL-6 reappeared after secretome treatment in spermatogenic cells84.
To further determine whether MH might interfere with CIS anticancer activity or enhance it, we performed a dose-response experiment on the breast cancer cell line MCF-7. The result revealed that MH did not interfere with CIS cytotoxicity; instead, it was slightly enhanced in the CIS and MH combination. Its anticancer efficacy has been demonstrated in various cancers, including liver, breast, and ovarian cancer85,86. In breast cancer cell line MCF-7, MH alone showed a moderate cytotoxic effect. This might be a result of the difference in cancer origin and cancer cell properties. It exerts its anticancer effects by different mechanisms, including apoptosis induction, cell cycle arrest, production of ROS, and other pathways87. These results demonstrate that concurrent use of MH with CIS exhibits a dual beneficial action. It reduces the adverse effects of CIS on testicular tissue and enhances its anticancer potency, potentially allowing for a lower therapeutic dose of CIS.
Then, the MH’s selectivity was assessed on a non-cancerous breast cell line, MCF-10 A. Compared to CIS, MH was more selective for cancer cells, and when combined with CIS, it increased the death of cancer cells while preserving normal cells and potentially reducing side effects. In parallel with our findings, MH has more selectivity for cancer cells than non-cancerous ones, as its IC50 is lower in squamous carcinoma cells than in normal oral mucosa cells88. Therefore, the combination of MH with anticancer agents like CIS may protect normal cells from chemotherapy-induced tissue damage and enhance CIS efficacy.
The present study has encountered some potential limitations. We assessed testicular iron level without evaluating the expression of its controlling proteins, such as transferrin and ferritin, which are involved in iron regulation. This might provide further insights into the mechanisms underlying CIS-induced ferroptosis. In addition, performing the spermatic kinetic analysis, which counts the individual testicular sperm populations, could help to characterize the impact of CIS and MH on the individual testicular populations. Despite these limitations, our study provides, for the first time, the potential role of MH on CIS-induced testicular injury with special emphasis on the role of ferroptosis mechanisms. Further investigations should address these issues to provide a more in-depth understanding of such injury.
Conclusion
CIS had an endocrine and reproductive toxic impact, as evidenced by changing sperm indices and lowering levels of LH and testosterone, as well as downregulation of steroidogenic genes. However, the use of MH could be a promising approach for mitigating CIS-induced toxicity while potentially enhancing its anticancer effects. MH ameliorated the CIS-mediated induction of oxidative stress, inflammatory, and ferroptosis signalling, which are considered the main mechanisms of testicular damage and poor sperm health. Our study is the first to shed light on the involvement of the ferroptosis pathway in the molecular mechanism of protection afforded by MH against CIS. Further investigations are warranted to deeply explore the pathomechanisms and protection.
Data availability
Data is provided within the manuscript or supplementary information files. Raw data details is available upon request from the corresponding author amibadr@ksu.edu.sa, amirabadr2005@yahoo.com.
8. References
Badr, A. M. et al. TLR4/inflammasomes cross-talk and pyroptosis contribute to N-acetyl cysteine and chlorogenic acid protection against cisplatin-induced nephrotoxicity. Pharmaceuticals 16 (3), 337 (2023).
Ranasinghe, R., Mathai, M. L. & Zulli, A. Cisplatin for cancer therapy and overcoming chemoresistance. Heliyon 8 (9), e10608 (2022).
Zhang, C., Xu, C., Gao, X. & Yao, Q. Platinum-based drugs for cancer therapy and anti-tumor strategies. Theranostics 12 (5), 2115–2132 (2022).
Ferrara, N. & Kerbel, R. S. Angiogenesis as a therapeutic target. Nature 438 (7070), 967–974 (2005).
Zavattaro, M. et al. Gonadal failure and infertility in cancer survivors: Clinical management and strategies for prevention. Front. Horm. Res. 54, 58–68 (2021).
Lampe, H., Horwich, A., Norman, A., Nicholls, J. & Dearnaley, D. P. Fertility after chemotherapy for testicular germ cell cancers. J. Clin. Oncol. 15 (1), 239–245 (1997).
Ismail, H. Y. et al. Cisplatin-induced azoospermia and testicular damage ameliorated by adipose-derived mesenchymal stem cells. Biol. Res. 56 (1).
Abdel-Latif, R. et al. Cisplatin-induced reproductive toxicity and oxidative stress: Ameliorative effect of kinetin. Antioxidants 11, 863 (2022).
Afsar, T., Razak, S., khan, M. R. & Almajwal, A. Acacia hydaspica ethyl acetate extract protects against cisplatin-induced DNA damage, oxidative stress and testicular injuries in adult male rats. BMC Cancer 17 (1).
Al-Bader, M. & Kilarkaje, N. Effects of bleomycin, etoposide and cisplatin treatment on Leydig cell structure and transcription of steroidogenic enzymes in rat testis. Eur. J. Pharmacol. 747, 150–159 (2015).
Mori Sequeiros García, M. et al. Cisplatin inhibits testosterone synthesis by a mechanism that includes the action of reactive oxygen species (ROS) at the level of P450scc. Chem. Biol. Interact. 199 (3), 185–191. (2012).
Fan, Z. et al. Ferroptosis is crucial for cisplatin induced sertoli cell injury via n6-methyladenosine dependent manner. World J. Mens. Health 42 (4) (2024).
Yuan, W., Sun, Z., Ji, G. & Hu, H. Emerging roles of ferroptosis in male reproductive diseases. Cell Death Discov. 9 (1), 1–13 (2023).
Ma, T. L. et al. Focus on ferroptosis regulation: Exploring novel mechanisms and applications of ferroptosis regulator. Life Sci. 307 (2022).
Liu, Y. et al. Effects of ferroptosis on male reproduction. Int. J. Mol. Sci. 23 (13).
Consoli, V., Sorrenti, V., Grosso, S. & Vanella, L. Heme oxygenase-1 signaling and redox homeostasis in physiopathological conditions. Biomolecules 11 (4), 589 (2021).
de Oliveira, J., Denadai, M. B. & Costa, D. L. Crosstalk between heme oxygenase-1 and iron metabolism in macrophages: Implications for the modulation of inflammation and immunity. Antioxidants 11 (5). (2022).
Rajput, S. A., Wang, X. & qi, Yan, H. C. Morin hydrate: A comprehensive review on novel natural dietary bioactive compound with versatile biological and pharmacological potential. Biomed. Pharmacother. 138. (2021).
Goyal, A., Dubey, N., Agrawal, A., Verma, A. & Sharma, R. Therapeutic potential of morin: special focus on cognitive dysfunction, diabetes mellitus and cancer. Pharmacol. Res. - Mod. Chin. Med. 9, 100318 (2023).
Olayinka, E. T., Ore, A., Adeyemo, O. A. & Ola, O. S. The role of flavonoid antioxidant, morin in improving procarbazine-induced oxidative stress on testicular function in rat. Porto Biomed. J. 4 (1), e28. (2018).
Kumar, R., Kumar, V., Gurusubramanian, G., Rathore, S. S. & Roy, V. K. Morin hydrate ameliorates heat-induced testicular impairment in a mouse model. Mol. Biol. Rep. 51 (1), 1–19 (2024).
Kucukler, S., Caglayan, C., Darendelioğlu, E. & Kandemir, F. M. Morin attenuates acrylamide-induced testicular toxicity in rats by regulating the NF-κB, Bax/Bcl-2 and PI3K/Akt/mTOR signaling pathways. Life Sci. 261, 118301 (2020).
Athira, K. V. et al. Morin hydrate mitigates cisplatin-induced renal and hepatic injury by impeding oxidative/nitrosative stress and inflammation in mice. J. Biochem. Mol. Toxicol. 30 (12), 571–579 (2016).
Zhang, R. et al. Cellular protection of morin against the oxidative stress induced by hydrogen peroxide. Chem. Biol. Interact. 177 (1), 21–27. (2009).
Nambu, A. & Kumamoto, Y. Studies of spermatogenic damages induced by anti-cancer agent and anti-androgenic agents in rat testes. Nihon Hinyokika Gakkai Zasshi 86 (7), 1221–1230. (1995).
Omar, N. N., Mosbah, R. A., Sarawi, W. S., Rashed, M. M. & Badr, A. M. Rifaximin protects against malathion-induced rat testicular toxicity: A possible clue on modulating gut microbiome and inhibition of oxidative stress by mitophagy. Molecules 27 (13), 4069 (2022).
Erdemir, F. et al. The effect of sertraline, paroxetine, fluoxetine and escitalopram on testicular tissue and oxidative stress parameters in rats. Int. Braz. J. Urol. 40 (1), 100–108. (2014).
Indrayanto, G., Putra, G. S. & Suhud, F. Validation of in-vitro bioassay methods: application in herbal drug research. Profiles Drug Subst. Excip Relat. Methodol. 46, 273–307 (2021).
Ahmed, E. A., Omar, H. M., elghaffar, S. K. A., Ragb, S. M. M. & Nasser, A. Y. The antioxidant activity of vitamin C, DPPD and L-cysteine against Cisplatin-induced testicular oxidative damage in rats. Food Chem. Toxicol. 49 (5), 1115–1121. (2011).
Ghafouri-Fard, S. et al. Effects of chemotherapeutic agents on male germ cells and possible ameliorating impact of antioxidants. Biomed. Pharmacother. 142 (2021).
Tharmalingam, M. D. et al. Cisplatin and carboplatin result in similar gonadotoxicity in immature human testis with implications for fertility preservation in childhood cancer. BMC Med. 18 (1) (2020).
Sawhney, P., Giammona, C. J., Meistrich, M. L. & Richburg, J. H. Cisplatin-induced long-term failure of spermatogenesis in adult C57/Bl/6J mice. J. Androl. 26 (1), 136–145 (2005).
Soni, K. K. et al. Dose-dependent effects of cisplatin on the severity of testicular injury in Sprague Dawley rats: Reactive oxygen species and endoplasmic reticulum stress. Drug Des. Dev. Ther. 10, 3959–3968. (2016).
Elefsiniotis, I. S. et al. Tamoxifen induced hepatotoxicity in breast cancer patients with pre-existing liver steatosis: the role of glucose intolerance. Eur. J. Gastroenterol. Hepatol. 16 (6), 593–538 (2004).
Fang, Z. et al. Short-term tamoxifen administration improves hepatic steatosis and glucose intolerance through JNK/MAPK in mice. Signal Transduct. Target Ther. 8 (1) (2023).
Labbe, G., Pessayre, D. & Fromenty, B. Drug-induced liver injury through mitochondrial dysfunction: mechanisms and detection during preclinical safety studies. Fundam. Clin. Pharmacol. 22 (4), 335–353.
Balaga, V. K. R. et al. Morin: A comprehensive review on its versatile biological activity and associated therapeutic potential in treating cancers. Pharmacol. Res. - Mod. Chin. Med. 7, 100264 (2023).
Favareto, A. P. A., Nogueira, L. C., Pontes, D. A., de Fátima Paccola Mesquita, S. & Camargo, I. C. C. Evaluation of testicular tissue of adult rats treated with cisplatin incorporated into the liposome. Microsc. Res. Technol. 78 (4), 323–329 (2015).
Zhang, J. et al. Activation of MT1/MT2 to protect testes and leydig cells against cisplatin-induced oxidative stress through the SIRT1/Nrf2 signaling pathway. Cells 11 (10) (2022).
Marengo, S. R. Maturing the sperm: unique mechanisms for modifying integral proteins in the sperm plasma membrane. Anim. Reprod. Sci. 105 (1–2), 52–63 (2008).
Chen, H., Alves, M. B. R. & Belleannée, C. Contribution of epididymal epithelial cell functions to sperm epigenetic changes and the health of progeny. Hum. Reprod. 28 (1), 51–66 (2021).
Ataman, J. E. & Baxter-grillo, D. Morphological evaluation of cisplatin-induced testicular & damage in wistar rats. Nigerian J. Life Sci. 4(1), 16–25 (2022).
Gamini, C. Dose dependent alterations in epididymal sperm counts of cisplatin or carboplatin treated male wistar rats. (2009).
Adelakun, S. A., Akintunde, O. W., Ogunlade, B., Peter, A. B. & Siyanbade, J. A. BCL-2 and BAX expression and germ cell apoptosis following the intervention of 1-isothiocyanato-4-methylsulfinylbutane in cisplatin-induced testicular toxicity and sperm DNA fragmentation in Sprague-Dawley rat. Aspects Mol. Med. 4, 100055 (2024).
Favareto, A. P. A., Fernandez, C. D. B., da Silva, D. A. F., Anselmo-Franci, J. A. & Kempinas, W. D. G. Persistent impairment of testicular histology and sperm motility in adult rats treated with Cisplatin at peri-puberty. Basic Clin. Pharmacol. Toxicol. 109 (2), 85–96. (2011).
Hejazi, S. Toxicity effect of cisplatin-treatment on rat testis tissue. J. Mens Health 8 (3), 235 (2011).
Morphological evaluation of cisplatin-induced testicular & damage in wistar rats. Nigerian J. Life Sci. 2276–7029 (2024).
Walke, G., Gaurkar, S. S., Prasad, R., Lohakare, T. & Wanjari, M. The impact of oxidative stress on male reproductive function: Exploring the role of antioxidant supplementation. Cureus 15 (7), e42583. (2023).
Ings, J. S. & Van Der Kraak, G. J. Characterization of the mRNA expression of StAR and steroidogenic enzymes in zebrafish ovarian follicles. Mol. Reprod. Dev. 73 (8), 943–954 (2006).
Oduwole, O. O., Peltoketo, H. & Huhtaniemi, I. T. Role of follicle-stimulating hormone in spermatogenesis. Front. Endocrinol. (Lausanne). 9, 427599 (2018).
Wang, Y., Chen, F., Ye, L., Zirkin, B. & Chen, H. Steroidogenesis in Leydig cells: Effects of aging and environmental factors. Reproduction 154 (4), R111–122. (2017).
Miller, W. L. & Bose, H. S. Early steps in steroidogenesis: intracellular cholesterol trafficking: thematic review series: genetics of human lipid diseases. J. Lipid Res. 52 (12), 2111–2135 (2011).
Bremer, A. A. & Miller, W. L. Regulation of steroidogenesis. Cell. Endocrinol. Health Dis. 207–227. (2014).
Shahin, N. N. & Mohamed, M. M. Nano-sized titanium dioxide toxicity in rat prostate and testis: Possible ameliorative effect of morin. Toxicol. Appl. Pharmacol. 334, 129–141 (2017).
Asadi-Fard, Y. et al. Morin improves Bisphenol-A-induced toxicity in the rat testicular mitochondria and sperms. JBRA Assist. Reprod. 27 (2), 174 (2023).
Olayinka, E. T. & Adewole, K. E. Ameliorative effect of morin on dutasteride-tamsulosin-induced testicular oxidative stress in rat. J. Complement. Integr. Med. 18 (2), 327–337.
Olayinka, E. T. et al. Preservation of antioxidant defense system by Morin in bicalutamide-induced rat testicular toxicity. Ife J. Sci. 23 (1), 115–122 (2021).
Wang, T. E. et al. Counteracting cisplatin-induced testicular damages by natural polyphenol constituent honokiol. Antioxidants 9 (8), 1–21 (2020).
Dasari, S. & Bernard Tchounwou, P. Cisplatin in cancer therapy: molecular mechanisms of action. Eur. J. Pharmacol. 740, 364–378. (2014).
Zhu, H. et al. Gss deficiency causes age-related fertility impairment via ROS-triggered ferroptosis in the testes of mice. Cell. Death Dis. 14 (12), 845 (2023).
Cellat, M. et al. Protective effect of Smilax excelsa L. pretreatment via antioxidant, anti-inflammatory effects, and activation of Nrf-2/HO-1 pathway in testicular torsion model. J. Food Biochem. 46 (8), e14161 (2022).
Bolisetty, S., Traylor, A., Joseph, R., Zarjou, A. & Agarwal, A. Proximal tubule-targeted heme oxygenase-1 in cisplatin-induced acute kidney injury. Am. J. Physiol. Renal Physiol. 310 (5), 385–394. (2016).
Shiraishi, F. et al. Heme oxygenase-1 gene ablation or expression modulates cisplatin-induced renal tubular apoptosis. Am. J. Physiol. Renal Physiol. 278 (5) (2000).
Heeba, G. H., Hamza, A. A. & Hassanin, S. O. Induction of Heme oxygenase-1 with Hemin alleviates cisplatin-induced reproductive toxicity in male rats and enhances its cytotoxicity in prostate cancer cell line. Toxicol. Lett. 264, 38–50 (2016).
Zarjou, A. et al. Paracrine effects of mesenchymal stem cells in cisplatin-induced renal injury require heme oxygenase-1. Am. J. Physiol. Renal Physiol. 300 (1) (2011).
Singh, M. P., Chauhan, A. K. & Kang, S. C. Morin hydrate ameliorates cisplatin-induced ER stress, inflammation and autophagy in HEK-293 cells and mice kidney via PARP-1 regulation. Int. Immunopharmacol. 56, 156–167 (2018).
Yang, X. et al. Review of the role of ferroptosis in testicular function. Nutrients 14 (24) (2022).
Tsao, C. W. et al. The effects of iron status on testosterone biosynthesis and testicular antioxidant capacity in male rats. FASEB J. 31 (S1), 460 (2024).
Leichtmann-Bardoogo, Y. et al. Compartmentalization and regulation of iron metabolism proteins protect male germ cells from iron overload. Am. J. Physiol. Endocrinol. Metab. 302 (12) (2012).
Zhang, F. L. et al. Multi-omics analysis reveals that iron deficiency impairs spermatogenesis by gut-hormone synthesis axis. Ecotoxicol. Environ. Saf. 248, 114344 (2022).
Ikeda, Y. et al. The involvement of ferroptosis on cisplatin-induced nephrotoxicity. In Proceedings for Annual Meeting of The Japanese Pharmacological Society 93, 060 (2020).
Mei, H. et al. Inhibition of ferroptosis protects House Ear Institute-Organ of Corti 1 cells and cochlear hair cells from cisplatin-induced ototoxicity. J. Cell Mol. Med. 24 (20), 12065–12081 (2020).
Gammella, E., Buratti, P., Cairo, G. & Recalcati, S. The transferrin receptor: The cellular iron gate. Metallomics 9 (10), 1367–1375. (2017).
Park, E. & Chung, S. W. ROS-mediated autophagy increases intracellular iron levels and ferroptosis by ferritin and transferrin receptor regulation. Cell Death Dis. 10 (11), 1–10. (2019).
Wang, Z., Yao, X., Wang, K. & Wang, B. TFR1-mediated iron metabolism orchestrates tumor ferroptosis and immunity in non-small cell lung cancer. J. Environ. Pathol. Toxicol. Oncol. 43 (2), 1–12 (2024).
Corral, V. M., Schultz, E. R., Eisenstein, R. S. & Connell, G. J. Roquin is a major mediator of iron-regulated changes to transferrin receptor-1 mRNA stability. Science 24 (4), 102360. (2021).
Doll, S. et al. ACSL4 dictates ferroptosis sensitivity by shaping cellular lipid composition. Nat. Chem. Biol. 13 (1), 91–98 (2016).
Liu, W. J. et al. Deferoxamine counteracts cisplatin resistance in A549 lung adenocarcinoma cells by increasing vulnerability to glutamine deprivation-induced cell death. Front. Oncol. 11. (2022).
Wendlocha, D., Kubina, R., Krzykawski, K. & Mielczarek-Palacz, A. Selected Flavonols targeting cell death pathways in cancer therapy: The latest achievements in research on apoptosis, autophagy, necroptosis, pyroptosis, ferroptosis, and cuproptosis. Nutrients 16 (8) (2024).
García-Juárez, M. & Camacho-Morales, A. Defining the role of anti- and pro-inflammatory outcomes of interleukin-6 in mental health. Neuroscience 492, 32–46 (2022).
Blanchard, F., Duplomb, L., Baud’huin, M. & Brounais, B. The dual role of IL-6-type cytokines on bone remodeling and bone tumors. Cytokine Growth Factor Rev. 20 (1), 19–28. (2009).
Lampiao, F. & du Plessis, S. S. TNF-alpha and IL-6 affect human sperm function by elevating nitric oxide production. Reprod. Biomed. 17 (5), 628–631 (2024).
Zhang, H. et al. Interleukin-6 disrupts blood-testis barrier through inhibiting protein degradation or activating phosphorylated ERK in Sertoli cells. Sci. Rep. 4. (2014).
Gan, R. Y. Regulation and functions of interleukin-6 in the mammalian testis. Int. J. Modern Biol. Med. 5 (2), 81–90 (2014).
Xu, M. & Zhang, Y. Morin inhibits ovarian cancer growth through the inhibition of NF-κB signaling pathway. Anticancer Agents Med. Chem. 19 (18), 2243–2250 (2024).
Solairaja, S., Andrabi, M. Q., Dunna, N. R. & Venkatabalasubramanian, S. Overview of morin and its complementary role as an adjuvant for anticancer agents. Nutr. Cancer 73 (6), 927–942 (2021).
Mottaghi, S. & Abbaszadeh, H. The anticarcinogenic and anticancer effects of the dietary flavonoid, morin: Current status, challenges, and future perspectives. Phytother. Res. 35 (12), 6843–6861 (2024).
Brown, J., O’Prey, J. & Harrison, P. R. Enhanced sensitivity of human oral tumours to the flavonol, morin, during cancer progression: Involvement of the Akt and stress kinase pathways. Carcinogenesis 24 (2), 171–177 (2003).
Acknowledgements
The authors extend their appreciation to Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2025R3713), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
Funding
This research was funded by Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2025R713), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
Author information
Authors and Affiliations
Contributions
Developing and planning the study; Y. Mahran, A. Badr. Performing in vivo experiments; Y. Mahran, A. Badr, R. Ali, D. Alsultan, S. Almufadhili, D. Almasud. Data validation, curation, and Data visualization; all Authors, Writing the original draft and reviewing; Y. Mahran, A. Badr, W. Sarawi, and I. Hasan; performing the in vitro and molecular experiments: S. Aloyouni, M. Alkahtani and Lastly, the published version of the manuscript has been approved by authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mahran, Y., Badr, A.M., Aloyouni, S. et al. Morin hydrate protects against cisplatin-induced testicular toxicity by modulating ferroptosis and steroidogenesis genes’ expression and upregulating Nrf2/Heme oxygenase-1. Sci Rep 15, 22720 (2025). https://doi.org/10.1038/s41598-025-08235-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-08235-4