Abstract
Symptoms of diaphragm dysfunction, such as exertional dyspnea and decreased exercise tolerance, share similarities with the symptoms of skeletal muscle mass reduction caused by conditions like sarcopenia. Given that the diaphragm is also a skeletal muscle, sarcopenia may be associated with diaphragm dysfunction, but the specifics of this relationship remain unclear. This study aimed to assess the relationship between diaphragm function—measured by ultrasonography (thickness, thickening fraction, and excursion)—and muscle mass of the extremities, trunk, and whole body using bioimpedance analysis. We recruited older adults from an outpatient clinic for swallowing rehabilitation or frailty. Muscle mass was measured through bioimpedance analysis, and diaphragm function was evaluated with ultrasonography. The relationships between diaphragm ultrasound results and muscle mass measurements were analyzed with regression models adjusted for age, sex, and height. The study included 114 participants (mean age 78.0 years; 45.6% male). The skeletal muscle index was 7.2 kg/m² for men and 5.9 kg/m² for women, with 20% meeting the Asian Working Group for Sarcopenia 2019 criteria. Diaphragm excursion during deep breathing was significantly associated with muscle mass of the extremities, trunk, and whole body (p < 0.001 in simple analysis; p < 0.01 in multiple analysis). Diaphragm thickness and thickening fraction showed no significant associations with muscle mass. Diaphragm excursion could be an adequate indicator of sarcopenia in cases where limb-based measurement is not possible, and therefore unreliable.
Similar content being viewed by others
Introduction
Sarcopenia is the decline in skeletal muscle mass and strength caused by aging, malnutrition, lack of exercise, and chronic diseases. Sarcopenia is associated with an increase in falls, fractures, hospitalization, and death, as well as a decrease in activities of daily living (ADL) and physical function, which potentially leads to a decline in quality of life in older adults and an increase in social security costs. Therefore, early diagnosis and intervention for sarcopenia are critically important1. Additionally, respiratory muscle strength, such as maximal inspiratory pressure, is lower in patients with sarcopenia and the prevalence of sarcopenia reaches 50–60% in patients with acute lung injury2,3. Against this background, the concept of respiratory sarcopenia, which focuses on the decline in respiratory muscle strength and mass, has been proposed in recent years4. In this context, the concept of respiratory sarcopenia, characterized by the coexistence of reduced respiratory muscle strength and mass, has recently been proposed, in contrast to global sarcopenia, which is defined by the coexistence of decreased skeletal muscle function and mass1,4. When evaluating respiratory sarcopenia, the diaphragm is used as an indicator of respiratory muscle mass. However, specific methods for quantifying respiratory muscle mass and corresponding cutoff values have not yet been established4.
The diaphragm functions not only as a critical respiratory muscle but also as a core muscle that helps maintain postural stability; its dysfunction is tied to respiratory impairments and challenges in physical function and balance5,6,7,8,9. Given the similarities between diaphragm dysfunction and the symptoms of sarcopenia, and that the diaphragm is a skeletal muscle, hypotheses of a relationship between diaphragm function and overall skeletal muscle mass have been proposed10.
Ultrasonography, a minimally invasive imaging method, is increasingly used to evaluate diaphragm function. It has traditionally been utilized to predict successful extubation of intubated patients and to diagnose diaphragmatic paralysis5,11,12,13,14. In diaphragm ultrasonography, primary evaluation indices include diaphragm thickness (Tdi), thickening fraction (TF) during respiration, and diaphragm excursion (DE), and it is known that the most appropriate evaluation indicator varies depending on the clinical situation15.
However, research on the relationship between diaphragm function and overall muscle mass is limited, and it is not yet clear which of these indices—Tdi, TF, or DE—is more strongly associated with muscle mass. No previous studies have simultaneously assessed all three ultrasound parameters in the same participants16. Therefore, this study aimed to examine the relationship between indices of diaphragm function measured by ultrasonography (Tdi, TF, DE) and muscle mass of the extremities, trunk, and whole-body skeletal muscle mass. This study aimed to provide novel insight into the relevance of diaphragm ultrasound measures as indicators of systemic muscle loss.
Methods
Study population and setting
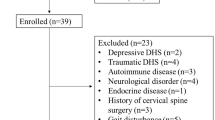
This study recruited patients who visited the Swallowing Rehabilitation Outpatient Clinic at Tokyo Medical and Dental University Hospital in Tokyo, the Frailty Outpatient Clinic at Tokyo Metropolitan Institute for Geriatrics and Gerontology in Tokyo, and the Frailty Outpatient Clinic at Hitachiomiya Saiseikai Hospital in Hitachiomiya, Ibaraki Prefecture between May 2023 and April 2024. All patients gave informed consent before inclusion. Individuals aged 65 years or older who could walk independently and follow instructions were included in the study. Exclusion criteria included those with symptoms suggestive of acute infection, individuals with implanted medical devices such as pacemakers, those using home oxygen therapy, those with communication difficulties, those who did not provide consent, and those deemed unsuitable by the researchers (e.g., those predicted to have significant frailty making it challenging to complete the tests). Participants underwent medical interviews regarding their lifestyle history, medical history, medication history, ADL (Barthel Index), and cognitive function (mini-mental state examination). Additionally, measurements were taken of their height, weight, waist circumference, calf circumference, blood pressure, handgrip strength, and gait speed over a 4-meter walk. Moreover, using bioelectrical impedance analysis (BIA) with the Inbody S10 or Inbody 770 (Inbody Japan Inc., Tokyo, Japan), the muscle mass of the whole body and different regions, total skeletal muscle mass (SMM), and skeletal muscle index (SMI) were measured. The SMI was defined by existing research and sarcopenia diagnostic criteria as the appendicular skeletal muscle mass (ASM) divided by height squared (kg/m²)17,18. When measuring muscle mass by region, skeletal muscle could not be measured in isolation; therefore, trunk muscle mass (TMM) includes smooth muscle and cardiac muscle. The diaphragm ultrasound examination, respiratory function test, and respiratory muscle strength test were performed after the medical interview and physical examination.
Ultrasound measurements of the diaphragm
The right hemidiaphragm’s Tdi, TF, and DE were assessed seated, using an ultrasound imaging system (ARIETTA 50® or FC1®, FUJIFILM, Japan). For measuring Tdi and TF in B-mode, a linear probe was placed longitudinally and perpendicular to the chest wall between the 8th and 9th intercostal spaces along the anterior to mid-axillary lines, with adjustments made to avoid the ribs. The probe was positioned so that a portion of the lung was visible at the end of inspiration. At this location, we measured the Tdi at the end of expiration during quiet breathing, corresponding to the functional residual capacity (FRC), and at the end of inspiration during deep breathing. Tdi was defined as the distance between the pleural line’s midpoint and the peritoneal line’s midpoint (Supplementary Figure S1A). TF was calculated using the formula: 100 × ([Tdi at the end of deep inspiration − Tdi at FRC]/Tdi at FRC) [%].
For DE measurement, a sector probe was similarly positioned, placed longitudinally and perpendicular to the chest wall, with adjustments made to avoid the ribs and ensure that the lung did not overlap with the diaphragm dome during deep breathing. In M-mode, the cursor line was adjusted to be as perpendicular as possible to the tangent of the diaphragm at the posterior two-thirds of the diaphragm dome, and the position change between deep inspiration and deep expiration was measured (Supplementary Figure S1B). All diaphragm ultrasonography was performed by trained physicians or technicians. These examinations were performed by two physicians and one sonographer who had received the same training of diaphragm ultrasound examination. If the findings were clear, a single examination was performed. If clear findings were not obtained, the examination was repeated until clear findings were obtained.
Spirometric and respiratory muscle studies
Respiratory function and respiratory muscle strength tests were conducted using a spirometer (DISCOM-51 by Chest M.I. Inc., Tokyo, Japan, at Hitachiomiya Saiseikai Hospital and AutoSpiratory AS507 by Minato Medical Science at other facilities) in accordance with the guidelines established by the American Thoracic Society and the European Respiratory Society and updated in 201919. In a seated position, forced vital capacity, forced expiratory volume in one second, forced expiratory volume in one second/forced vital capacity ratio, maximal inspiratory pressure, and maximal expiratory pressure was measured.
Statistical analyses
The differences in the mean values between males and females were compared for the diaphragm ultrasound results (Tdi, TF, DE) using the Student’s t-test. The relationships between the diaphragm ultrasound results and muscle mass measurements were analyzed using simple and multiple regression analyses adjusted for age, sex, and height. Statistical significance was established when a p-value was less than 0.05. All data analyses were performed using STATA version 18.0, supplied by StataCorp LLC, College Station, TX, USA.
Results
Participants
In total, 115 participants who met the inclusion criteria were recruited, and 114 individuals aged 65 years or older who provided informed consent were included in the study. The participants’ characteristics are shown in Table 1. The mean age of the participants was 78.0 ± 6.7 years, the mean BMI was 23.4 ± 3.3 kg/m², the mean Barthel Index was 98.3 ± 4.2, and the mean mini-mental state examination score was 27.4 ± 3.1. Of participants, 10.5% had a history of cerebrovascular disease, but none had residual effects, such as limb paralysis. Only two cases (1.8%) had a history of neurological diseases other than cerebrovascular disorders.
Muscle mass
The results of the muscle mass measurements using BIA are presented in Table 2. The mean SMI was 7.2 ± 0.7 kg/m² for males and 5.9 ± 0.7 kg/m² for females, with 20.0% of participants meeting the AWGS2019 criteria for sarcopenia16.
Diaphragm ultrasonography
The results of the diaphragm ultrasound examinations are shown in Table 3. The thickness of the right diaphragm at FRC was measurable in all 114 cases, with a mean of 2.1 ± 0.6 mm. The TF during deep breathing was measurable in 112 cases, with a mean of 88.7 ± 44.9%; no statistically significant differences were observed between males and females for either measurement. By contrast, DE was measurable in 107 cases, with a mean of 44.4 ± 14.0 mm, and a significant difference was observed between males and females, with a mean DE of 48.8 ± 13.7 mm in males and 41.0 ± 13.4 mm in females (p = 0.004).
Relationships between diaphragm ultrasound measurements and muscle mass parameters: single and multiple regression analyses
The relationship between each diaphragm ultrasound measurement (Tdi, TF, DE) and various muscle mass parameters (ASM, TMM, SMM, SMI) was analyzed using univariate linear regression analysis (Table 4). No significant associations were found between Tdi and TF and any muscle mass parameters. By contrast, DE showed statistically significant associations with ASM, TMM, SMM, and SMI (all p < 0.001) (Supplementary Figure S2).
Next, multiple regression analyses adjusted for age, sex, and height were performed (Table 5). Similar to the univariate analysis, no statistically significant causal relationships were observed between Tdi and TF and the muscle mass parameters. However, significant causal relationships were found between DE and ASM (p = 0.004), TMM (p < 0.001), SMM (p = 0.003), and SMI (p = 0.002) (Supplementary Figure S3).
Discussion
In this study, we examined the relationship between various diaphragm ultrasound parameters (Tdi, TF, DE) and muscle mass measurements obtained by BIA (ASM, TMM, SMM, SMI) in older outpatients in Japan. Both single regression analysis and multiple regression analyses adjusted for age, sex, and height showed that DE had a statistically significant association with ASM, TMM, SMM, and SMI. By contrast, Tdi and TF were not associated with any muscle mass measurements.
To date, a few small studies have evaluated the relationship between diaphragmatic function and sarcopenia or skeletal muscle mass in older adults18. They report that (i) Tdi is thinner in sarcopenic patients than in non-sarcopenic patients (30 sarcopenic patients); (ii) a decrease of DE during deep breathing is related to loss of muscle mass (12 patients who have muscle mass loss); and (iii) ASM/BMI is related to Tdi (45 healthy individuals)20,21,22. All of these studies were limited by a small sample size and the measurement of only Tdi or DE. Therefore, more extensive and comprehensive research was required. Compared with previous studies, this study evaluated the relationship between all diaphragm ultrasound parameters (Tdi, TF, DE) and muscle mass measurements in Asian adults with a sample size that was more than twice as large. It demonstrated that DE during deep breathing was significantly associated with both local muscle mass and overall skeletal muscle mass. Specifically, we showed that for each 10 mm increase in DE, muscle mass increased by approximately 0.5 kg (ASM, 0.4 kg; TMM, 0.5 kg; and SMM, 0.5 kg) and SMI increased by 0.1 kg/m².
In this study, among the diaphragm ultrasound parameters, only DE was significantly associated with muscle mass. Some previous reports show that the thickness and cross-sectional area of the rectus femoris and gastrocnemius muscles in older individuals, as measured by ultrasound, correlate with total muscle mass as assessed by BIA and dual-energy x-ray absorptiometry23,24. However, other studies have found that, compared with younger individuals, the rectus femoris and rectus abdominis are thinner in older adults, while the diaphragm is thicker23,24. Our findings are consistent with previous studies that suggest the thickness of the diaphragm may not accurately reflect overall skeletal muscle mass in older adults. In this study, we did not directly evaluate diaphragmatic fat infiltration or morphological changes. However, previous studies have reported that echogenicity of the diaphragm and fat infiltration in limb skeletal muscles increases with aging, and diaphragm muscle fibers show hypertrophy in early aging mice25,26,27. The hypothesis based on these findings that diaphragmatic hypertrophy and fat infiltration occur with aging could potentially explain why Tdi and TF were not significantly associated with muscle mass in this study. However, further anatomical and pathological studies are needed to validate these mechanisms.
Standard screening and muscle strength evaluation items for sarcopenia include handgrip strength, gait speed, calf circumference, and SMI. Handgrip strength and calf circumference are particularly convenient indicators because of their reasonable validity, ease of implementation, low cost, and minimal risk17,18,28,29. However, there are situations where both handgrip strength and calf circumference may not accurately reflect overall muscle strength and mass because both are specific to the limbs. For example, in patients with rheumatoid arthritis, handgrip strength did not differ between sarcopenic and non-sarcopenic groups, while in patients with edema, calf circumference underestimated the prevalence of sarcopenia by approximately 10%29,30.
Although the diaphragm is a skeletal muscle of the trunk, DE was significantly associated with skeletal muscle mass in both the limbs and the entire body in this study. This suggests that DE may reflect systemic muscle loss and could potentially serve as a complementary or alternative indicator for sarcopenia, particularly in clinical scenarios where limb-based measurements are difficult or inaccurate due to joint disorders, edema, or impaired ADL. While diaphragm ultrasound requires specific devices and examiner training, it may be a valuable tool for sarcopenia screening in such populations. Future research should investigate its diagnostic ability for sarcopenia, as well as its impact on comprehensive long-term outcomes such as cognitive function, ADL, and overall mortality in older people.
This study has several limitations. First, participants were outpatients recruited from high-level medical institutions, and most had preexisting conditions, with a much higher prevalence of diabetes (57.9%) than the general Japanese population aged 20 to 79 years (8.8%)31. However, the average Barthel Index score was high (98.3), indicating that participants were still relatively functional and likely comparable to community-dwelling older adults with independent ADL. Nevertheless, the sample may not fully represent the broader population, introducing possible selection bias. Second, since this study is an observational cross-sectional study, it is not possible to infer a causal relationship between diaphragm ultrasound parameters and skeletal muscle mass. Furthermore, although ultrasound was used to evaluate the diaphragm, not all participants were examined using the same device, and no external validation using gold standard methods such as DXA was performed, which may limit the generalizability of the results of this study. Third, while all examiners underwent the same training and were certified, we did not assess inter- or intra-rater reliability in this study. Previous research has shown generally good reliability for Tdi and DE, but measurement variability cannot be entirely ruled out32,33. Fourth, technical challenges in visualization during deep breathing led to the inability to measure TF in two cases (1.8%) and DE in seven cases (6.1%), primarily due to lung overlap with the diaphragm. This may affect the generalizability of DE-related findings. Finally, potential confounding factors such as nutritional status or inflammatory conditions were not measured and may have influenced the observed associations.
In conclusion, we examined the relationship of appendicular skeletal muscle mass, trunk muscle mass, and overall skeletal muscle mass, with diaphragm function in older people. Diaphragm excursion during deep breathing (DE) was significantly associated with muscle mass, while diaphragm thickness (Tdi) and thickening fraction (TF) were not associated with muscle mass.
Data availability
The datasets generated during and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADL:
-
Activities of daily living
- Tdi:
-
Diaphragm thickness
- TF:
-
Thickening fraction
- DE:
-
Diaphragm excursion
- BIA:
-
Bioelectrical impedance analysis
- SMM:
-
Skeletal muscle mass
- SMI:
-
Skeletal muscle index
- ASM:
-
Appendicular skeletal muscle mass
- TMM:
-
Trunk muscle mass
- FRC:
-
Functional residual capacity
- SD:
-
Standard deviation
- MMSE:
-
Mini-mental state examination
- %VC:
-
Percent vital capacity
- FEV1/FVC:
-
Forced expiratory volume in one second / forced vital capacity
- COPD:
-
Chronic obstructive pulmonary disease
- CI:
-
Confidence interval
- Coef:
-
Coefficient
References
Xu, J., Wan, C. S., Ktoris, K., Reijnierse, E. M. & Maier, A. B. Sarcopenia is associated with mortality in adults: A systematic review and Meta-Analysis. Gerontology. 68, 361–376. https://doi.org/10.1159/000517099 (2022).
Morisawa, T. et al. The relationship between sarcopenia and respiratory muscle weakness in Community-Dwelling older adults. Int. J. Environ. Res. Public. Health. 18, 13257. https://doi.org/10.3390/ijerph182413257 (2021).
Sheean, P. M. et al. The prevalence of sarcopenia in patients with respiratory failure classified as normally nourished using computed tomography and subjective global assessment. J. Parenter. Enter. Nutr. 38, 873–879. https://doi.org/10.1177/0148607113500308 (2014).
Miyazaki, S., Tamaki, A., Wakabayashi, H. & Arai, H. Definition, diagnosis, and treatment of respiratory sarcopenia. Curr. Opin. Clin. Nutr. Metab. Care. 27, 210–218. https://doi.org/10.1097/mco.0000000000001003 (2024).
McCoolFD & TzelepisGE Dysfunction of the diaphragm. N Engl. J. Med. 366, 932–942. https://doi.org/10.1056/nejmra1007236 (2012).
Hodges, P. W., Butler, J. E., McKenzie, D. K. & Gandevia, S. C. Contraction of the human diaphragm during rapid postural adjustments. J. Physiol. 505, 539–548. https://doi.org/10.1111/j.1469-7793.1997.539bb.x (1997).
Bordoni, B. & Zanier, E. Anatomic connections of the diaphragm: influence of respiration on the body system. J. Multidiscip Healthc. 6, 281–291. https://doi.org/10.2147/jmdh.s45443 (2013).
Sannasi, R. et al. Diaphragm and core stabilization exercises in low back pain: A narrative review. J. Bodyw. Mov. Ther. 36, 221–227. https://doi.org/10.1016/j.jbmt.2023.07.008 (2023).
Kocjan, J. et al. Impact of diaphragm function parameters on balance maintenance. PLoS One. 13, e0208697. https://doi.org/10.1371/journal.pone.0208697 (2018).
Merrell, A. J. & Kardon, G. Development of the diaphragm -- a skeletal muscle essential for mammalian respiration. FEBS J. 280, 4026–4035. https://doi.org/10.1111/febs.12274 (2013).
Prada, G. et al. Tracheal, lung, and diaphragmatic applications of M-Mode ultrasonography in anesthesiology and critical care. J. Cardiothorac. Vasc Anesth. 35, 310–322. https://doi.org/10.1053/j.jvca.2019.11.051 (2021).
Mahmoodpoor, A. et al. Diaphragm ultrasound to predict weaning outcome: systematic review and meta-analysis. Anaesthesiol. Intensive Ther. 54, 164–174. https://doi.org/10.5114/ait.2022.117273 (2022).
Patel, A. S., O’Donnell, C., Parker, M. J. & Roberts, D. H. Diaphragm paralysis definitively diagnosed by ultrasonography and postural dependence of dynamic lung volumes after seven decades of dysfunction. Lung. 185, 15–20. https://doi.org/10.5114/ait.2022.117273 (2007).
Boussuges, A., Brégeon, F., Blanc, P., Gil, J. M. & Poirette, L. Characteristics of the paralysed diaphragm studied by M-mode ultrasonography. Clin. Physiol. Funct. Imaging. 39, 143–149. https://doi.org/10.1111/cpf.12549 (2019).
Yamada, T. et al. Diaphragm ultrasonography: reference values and influencing factors for thickness, thickening fraction, and excursion in the seated position. Lung. 202, 83–90. https://doi.org/10.1007/s00408-023-00662-2 (2024).
Siniscalchi, C., Nouvenne, A., Cerundolo, N., Meschi, T. & Ticinesi, A. On behalf of the Parma Post-Graduate specialization school in Emergency-Urgency medicine interest group on thoracic U. Diaphragm ultrasound in different clinical scenarios: A review with a focus on older patients. Geriatr. (Basel). 9, 70. https://doi.org/10.3390/geriatrics9030070 (2024).
Chen, L. K. et al. Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J. Am. Med. Dir. Assoc. 21, 300–307e2. https://doi.org/10.1016/j.jamda.2019.12.012 (2021).
Cruz-Jentoft, A. J. et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 48, 16–31. https://doi.org/10.1093/ageing/afz046 (2019).
Graham, B. et al. Standardization of spirometry 2019 update. An official American thoracic society and European respiratory society technical statement. Am. J. Respir Crit. Care Med. 200, e70–e88. https://doi.org/10.1164/rccm.201908-1590st (2019).
Deniz, O. et al. Diaphragmatic muscle thickness in older people with and without sarcopenia. Aging Clin. Exp. Res. 33, 573–580. https://doi.org/10.1007/s40520-020-01565-5 (2021).
Zeng, B. et al. Prediction of loss of muscle mass in sarcopenia using ultrasonic diaphragm excursion. Contrast Media Mol. Imaging. 2021, 4754705. https://doi.org/10.1155/2021/4754705 (2021).
Lee, Y., Son, S., Kim, D. K. & Park, M. W. Association of diaphragm thickness and respiratory muscle strength with indices of sarcopenia. Ann. Rehabil Med. 47, 307–314. https://doi.org/10.5535/arm.23081 (2023).
Zhao, R. et al. Evaluation of appendicular muscle mass in sarcopenia in older adults using ultrasonography: A systematic review and Meta-Analysis. Gerontology. 68, 1174–1198. https://doi.org/10.1159/000525758 (2022).
Özkal, Ö. et al. Assessment of core and lower limb muscles for static/dynamic balance in the older people: an ultrasonographic study. Age Ageing. 48, 881–887. https://doi.org/10.1093/ageing/afz079 (2019).
Messa, G. A. M. et al. Morphological alterations of mouse skeletal muscles during early ageing are muscle specific. Exp. Gerontol. 125, 110684. https://doi.org/10.1016/j.exger.2019.110684 (2019).
van Doorn, J. L. M. et al. Association of diaphragm thickness and echogenicity with age, sex, and body mass index in healthy subjects. Muscle Nerve. 66, 197–202. https://doi.org/10.1002/mus.27639 (2022).
Avesani, C. M. et al. Muscle fat infiltration in chronic kidney disease: a marker related to muscle quality, muscle strength and sarcopenia. J. Nephrol. 36, 895–910. https://doi.org/10.1007/s40620-022-01553-0 (2023).
Rijk, J. M., Roos, P. R., Deckx, L., van den Akker, M. & Buntinx, F. Prognostic value of handgrip strength in people aged 60 years and older: A systematic review and meta-analysis. Geriatr. Gerontol. Int. 16, 5–20. https://doi.org/10.1111/ggi.12508 (2016).
Ishida, Y. et al. Impact of edema on length of calf circumference in older adults. Geriatr. Gerontol. Int. 19, 993–998. https://doi.org/10.1111/ggi.13756 (2019).
Ekici, R. et al. Prevalence of sarcopenia and clinical implications in patients with newly diagnosed rheumatoid arthritis. Nutrition. 90, 111353. https://doi.org/10.1016/j.nut.2021.111353 (2021).
Tatsumi, Y. & Ohkubo, T. Hypertension with diabetes mellitus: significance from an epidemiological perspective for Japanese. Hypertens. Res. 40, 795–806. https://doi.org/10.1038/hr.2017.67 (2017).
Testa, A. et al. Ultrasound M-mode assessment of diaphragmatic kinetics by anterior transverse scanning in healthy subjects. Ultrasound Med. Biol. 37, 44–52. https://doi.org/10.36416/1806-3756/e20200064 (2011).
Boer, W. et al. Diagnostics (Basel). 3;15(1):90. https://doi.org/10.3390/diagnostics15010090 (2025).
Acknowledgements
The authors are grateful to Hiroyuki Nagata, Mao Kawamura, Masayuki Kojima, Megumi Iwama, Mikiko Hatsutori, Motoi Noara, Noriko Kikuchi, Noriko Sato, Rika Nonaka, Seiichi Suzuki, Taro Minami, Tomohiro Kato, Yosuke Matsuzaki, and Yuji Murao for their efforts in data collection and management of the research environment. We also thank Philippa Gunn, D.Phil., from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by S.O., T.Y., T.S., S.M., K.N., K.Y., A.H., T.M., K.T. and Y.T.. S.O., T.Y., R.H. and A.H. analyzed and interpreted the data. S.O. wrote the first draft with input from T.Y.. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Shuji Ouchi, Toru Yamada, Takahiro Shinohara, Suguru Mabuchi, Kazuharu Nakagawa, Kanako Yoshimi, Ayane Horike, Tatsuya Mayama, Kenji Toyoshima, Yoshiaki Tamura, Ryoichi Hanazawa, Akihiro Hirakawa, Hiroyuki Ichige, Haruka Tohara, and Masayoshi Hashimoto have no relevant financial or non-financial interests to disclose. Financial interests: Atsushi Araki has received research funding from Sumitomo Pharma Co. Ltd., Ono Pharmaceutical Co. Ltd., Novo Nordisk Pharma Ltd. Takeshi Ishida has received support for the endowed chair funded by Hitachiomiya City. Takuma Kimura has received research funding from C.U.C. Inc.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board of Tokyo Medical and Dental University (protocol code M2022-293-02, date of approval: March 20th, 2023).
Consent to participate
Written informed consent was obtained from all participants involved in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ouchi, S., Yamada, T., Shinohara, T. et al. Association between diaphragm excursion and whole-body muscle mass in older adults: an observational study. Sci Rep 15, 23762 (2025). https://doi.org/10.1038/s41598-025-08997-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-08997-x