Abstract
Compound mylabris capsules (CMC) are widely used in the treatment of various malignant tumors; however, their mechanisms of action in diffuse large B-cell lymphoma (DLBCL) remain poorly understood. To address this, we analyzed DLBCL-related datasets from GEO and TCGA, identifying 943 key genes through differential expression gene analysis and weighted gene co-expression network analysis. By constructing a drug-active ingredient-target network, we determined the top five active CMC ingredients and their associated 1053 gene targets. Intersection analysis between CMC targets and key DLBCL genes revealed 50 overlapping targets. Enrichment analysis highlighted critical pathways, including the cell cycle and p53 signaling. Single-cell RNA sequencing further demonstrated that these targets are predominantly expressed in DLBCL tumor cell subsets. Protein-protein interaction network analysis identified pivotal genes such as CDK1 and CDK2, which showed robust diagnostic and prognostic value, as confirmed by receiver operating characteristic and survival analyses. Molecular docking and dynamics simulations validated the high binding affinity of sitosterol (a primary CMC component) to these targets. In vitro experiments demonstrated that sitosterol significantly inhibits DLBCL cell proliferation and induces apoptosis. In conclusion, our study elucidates the anti-tumor effects of CMC (mainly sitosterol) in DLBCL, mediated through the regulation of targets like CDK1 and CDK2. These findings provide critical evidence supporting the therapeutic potential of CMC in DLBCL treatment.
Similar content being viewed by others
Introduction
Diffuse large B-cell lymphoma (DLBCL) constitutes approximately 30% of non-Hodgkin lymphoma (NHL) cases, making it the most common pathological subtype. DLBCL typically manifests as rapidly enlarging lymph nodes or extranodal masses and can potentially involve any tissue or organ. Most patients are diagnosed at an advanced stage1. The development and application of targeted therapies have enabled a significant number of DLBCL patients to achieve clinical remission, and in some cases, a cure. However, the heterogeneity of lymphoma leads to post-treatment resistance in 40% of patients, severely impacting survival outcomes and prognosis. This constitutes one of the major challenges in DLBCL treatment2. Consequently, there is an urgent need to search for more effective therapeutic agents.
Recently, traditional Chinese medicine (TCM) has gained recognition in cancer treatment. It primarily exerts its anti-tumor effects through various mechanisms such as immune function regulation, tumor cell proliferation inhibition, tumor cell apoptosis induction, and cellular energy metabolism modulation. TCM’s advantages include having multiple targets and exhibiting low toxicity3. Clinical practice indicates that integrating TCM with anti-tumor therapies can not only significantly prolong the survival of cancer patients but also markedly enhance their quality of life4.
Compound mylabris capsules (CMC) have found extensive clinical use in treating various cancers, including primary liver, lung, rectal, and malignant lymphoma5,6. However, the underlying mechanisms of CMC’s action in DLBCL are yet to be fully understood. This study seeks to elucidate the therapeutic effects and potential mechanisms of CMC in DLBCL, leveraging approaches such as transcriptomic data analysis, single-cell data analysis, network pharmacology, molecular docking, and molecular dynamics simulation (Fig. 1).
Materials and methods
Acquisition of DLBCL data
To retrieve DLBCL-related datasets comprehensively, we accessed the NCBI Gene Expression Omnibus database (http://www.ncbi.nlm.nih.gov/geo/) and downloaded expression data for DLBCL and Reactive Lymphoid Hyperplasia (RLH), with a primary focus on the GSE32018 dataset. The GSE32018 dataset, sequenced on the GPL6480 platform, comprises 22 lymph node tissue samples from DLBCL and 7 RLH samples (Table S1). In addition, we employed two external datasets, namely the TCGA (Table S2) and GSE181063 datasets, for validation and prognosis analysis. The GSE181063 dataset, sequenced on the GPL14951 platform, includes 811 (Table S3) lymph tissue samples collected from patients diagnosed with DLBCL. The normalize between a arrays algorithm was utilized to normalize the data.
Acquisition of differentially expressed genes (DEGs)
Following data normalization, we employed the “limma” package to analyze DEGs between the 22 DLBCL and the 7 RLH samples. Using a threshold of adjusted P-values < 0.05 and |LogFC|>0.58 for screening, we utilized the “ggplot2” and “ComplexHeatmap” packages to plot the volcano and heatmap of the DEGs.
Weighted gene co-expression network analysis (WGCNA)
We employed the WGCNA package for the analysis of the DLBCL GSE32018 dataset. Initially, we transformed the gene expression matrix into a Pearson correlation coefficient matrix and computed the soft thresholding power to ensure the matrix conformed to the scale-free network distribution characteristics. Subsequently, we converted the correlation coefficient matrix into an adjacency matrix, computed the dissimilarity coefficient between nodes, and built a hierarchical clustering tree. Based on these steps, we identified and fitted gene co-expression modules. For a more in-depth analysis, we incorporated phenotype-related information to pinpoint key modules associated with DLBCL. All the identified modules were denoted by module eigengenes (ME), where ME symbolizes the primary component of the gene expression profile within a specific module. We determined the intersection between key module genes and DEGs to identify target genes for DLBCL in subsequent analyses.
Screening of CMC active ingredients and target acquisition
We derived the active ingredients of nine traditional Chinese medicines, namely Mylabris, Ginseng, Hedysarum Multijugum Maxim, Sparganii Rhizoma, Scutellariae Barbatae Herba, Zedoary, Cornus Officinalis Sieb, Glossy Privet, and Licorice, from the Traditional Chinese Medicine Systems Pharmacology Database and Analysis Platform (TCMSP, https://www.tcmsp-e.com/#/database). As the TCMSP database lacks the active ingredients of Eleutherococcus senticosus and Bear Bile Powder, we sourced these from the HERB database (http://herb.ac.cn/) and relevant literature, respectively7. The selection criteria for all active ingredients were set as Oral Bioavailability (OB) ≥ 30% and Drug-Likeness (DL) ≥ 0.18. Subsequently, we procured the SMILES numbers of these active ingredients from the PubChem database (https://pubchem.ncbi.nlm.nih.gov/) and inputted them into the SwissTarget Prediction database (http://www.swisstargetprediction.ch/index.php) for corresponding gene target prediction. Finally, we standardized all target information using the Uniprot database (https://www.uniprot.org/).
Construction of drug-active ingredient-target network diagram
We utilized R software to analyze the shared components between DLBCL target genes and CMC predicted targets. The results were visualized employing the “ggplot2” and “VennDiagram” packages. Subsequently, we imported the CMC-DLBCL shared targets and active ingredients into Cytoscape software to construct a network diagram depicting drug-active ingredient-target interactions. The principal active ingredients of CMC for DLBCL treatment were identified based on Degree (DC) values.
Enrichment analysis
To delve deeper into the biological implications of DEGs, we employed the “clusterProfiler” package for Gene Set Enrichment Analysis (GSEA) and visualized the results using the “ggplot2” package. Additionally, we conducted Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analyses on the shared targets of CMC-DLBCL using the Srplot website, with “human” selected as the species. The GO enrichment analysis primarily encompasses the biological process (BP), cellular component (CC), and molecular function (MF).
Single-cell RNA-seq data analysis and identification of DLBCL-related genes
To elucidate the subcellular expression level of drug target genes in DLBCL tissues, we acquired single-cell sequencing data of seven DLBCL cases from two sources: four from the GSE182434 dataset in the GEO database and three from the “EGAD00001008311” accession on the “https://ega-archive.org” website. We processed this data using the Seurat package (version 4.1.0) in R software, and processed the data with the criteria of “af$nFeature_RNA ≥ 100 and af$nFeature_RNA ≤ 6000, af$percent.mt ≤ 50”. Following cell filtration based on the specified criteria, we employed the Harmony R package (version 1.0) for data integration and batch effect removal. Subsequently, the Uniform Manifold Approximation and Projection (UMAP) dimensionality reduction technique was used for cell clustering and visualization. Utilizing the CellMarker database (http://xteam.xbio.top/CellMarker/), we performed matching analysis and annotation on the cell groups within the single-cell RNA-seq data. Lastly, R was used to display the “singscore” distribution of essential pharmacological targets in various cell subtypes.
Construction of protein-protein interaction (PPI) network and identification of key genes
The screened common targets of CMC-DLBCL were uploaded to the String online database (https://cn.string-db.org/) with “Homo sapiens” selected as the species to generate a PPI network diagram for CMC treatment of DLBCL. Interaction data in TSV format was imported into Cytoscape 3.9.1 software, and the CytoNCA plugin was utilized to compute DC values for key gene identification.
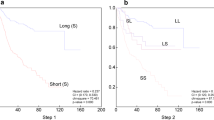
Receiver operating characteristic (ROC) curve analysis and survival analysis
The “pROC” package in R was utilized to plot the ROC curve and compute the Area Under the Curve (AUC), thereby evaluating the diagnostic value of the essential genes. This was followed by visualization using “ggplot2”. The GSE181063 dataset was employed to plot the Kaplan-Meier survival curve, facilitating the assessment of the prognostic value of the essential genes.
Molecular docking
The 2D structure of small molecule ligands was obtained from the PubChem database (http://pubchem.ncbi.nlm.nih.gov/). This structure was then inputted into Chem Office 20.0 software to generate its 3D structure, which was subsequently saved as a mol2 file. The RCSB PDB database (http://www.rcsb.org/) was then used to select protein targets with high-resolution crystal structures, which served as molecular docking receptors. The proteins were dehydrated and dephosphorylated using PyMOL2.6.0 software, and then saved as PDB files. The Molecular Operating Environment 2019 software was utilized to minimize the energy of the compounds, preprocess the target proteins, and identify active pockets. Finally, MOE 2019 was run to perform molecular docking, with the number of calculations set to 50. The binding activity between the two was evaluated based on the binding energy, and the results were visualized using PyMOL2.6.0 and Discovery Studio 2019 software.
Molecular dynamics simulation
Molecular Dynamics simulation on the complex were performed for 100 ns using Gromacs 2023. The protein was parameterized using the CHARMM 36 force field8, while the ligand topology was constructed with GAFF2 force field parameters. Periodic boundary conditions were applied, and the protein-ligand complex was positioned within a cubic box. The box was filled with water molecules using the TIP3P water model9. Electrostatic interactions were handled using the Particle Mesh Ewald (PME) and Verlet al.gorithms. Subsequently, isothermal-isochoric ensemble equilibration and isothermal-isobaric ensemble equilibration were performed for 100,000 steps, with a coupling constant of 0.1 ps and a simulation duration of 100 ps. Van der Waals and Coulomb interactions were calculated using a cutoff value of 1.0 nm. Finally, the system was subjected to molecular dynamics simulation under a constant temperature of 300 K and pressure of 1 bar, using Gromacs 2023. The simulation totaled 5,000,000 steps, with a step size of 2 fs, over a total duration of 100 ns.
Cell culture
Human B-cell lymphoma cell lines Pfeiffer and U2932 were purchased from the Cell Bank of the Chinese Academy of Sciences (Shanghai, China). The cells were cultured in RPMI-1640 medium (C11875500bt, Gibco, USA) supplemented with 10% fetal bovine serum (10099141 C, Gibco, USA) and 1% penicillin-streptomycin (15140-122, Gibco, USA) at 37 °C and 5% CO₂ in a constant temperature incubator (Thermo Fisher Scientific, USA).
CCK-8 assay
Pfeiffer and U2932 cells were seeded in 96-well plates at a density of 5 × 105 cells/well and treated with different concentrations (0, 2, 5, 10, 50, 100 and 300 ng/mL) of sitosterol. After 48 h of drug treatment, the operation was carried out according to the instructions of the CCK-8 kit (BA00208, Bioss, China), and finally, the absorbance values of each well were measured at a wavelength of 450 nm using a microplate reader (BioTek Instrument, Thermo Fisher Scientific, USA).
Apoptosis experiment
Cell apoptosis was detected using the FITC Annexin V Apoptosis Detection Kit (556547, BD Pharmingen, USA). Pfeiffer cells were treated with 14 ng/mL sitosterol, and U2932 cells were treated with 6 ng/mL sitosterol. The cell concentration was adjusted to 1 × 10⁶ cells/mL. The Annexin V-FITC and PI double staining was performed according to the kit instructions. The flow cytometry (DxFLEX, Beckman Coulter, USA) was used for detection, and the data analysis was conducted using Flowjo software (version 10.0).
Statistical analysis
In this study, all statistical analyses were performed using R software (version 4.3.1). ANOVA tests were used for the differential expression analysis of key genes and flow cytometry data. A P value of less than 0.05 was considered statistically significant, with significance levels indicated as follows: *P < 0.05, **P < 0.01, ***P < 0.001, and ****P < 0.0001.
Results
Data processing and acquisition of DEGs
The GSE32018 dataset was downloaded from the GEO database, followed by normalization of the raw sequencing data, and subsequent calculation of the DEGs between DLBCL and RLH. Among these genes, 1180 were upregulated and 1237 were downregulated. The top 30 DEGs are displayed in the volcano plot and heatmap (Fig. 2A,B).
Enrichment analysis of DEGs and pathway in DLBCL. (A,B) Volcano map and heat map of GSE32018 dataset DEGs. (C) Enrichment analysis results of hallmarks pathway of DEGs. (D) Network map of gene regulatory relationships from enrichment analysis of hallmarks pathway. (E,F) hallmarks pathway enrichment analysis in DLBCL is activated and inhibited signaling pathways. (G) Results of KEGG pathway enrichment analysis of DEGs. (H,I) KEGG pathway enrichment analysis of activated and inhibited signaling pathways in DLBCL.
Enrichment analysis
Hallmarks pathway enrichment of DEGs between DLBCL and RLH was assessed using GSEA analysis (Fig. 2C). The analysis revealed enrichment of MYC targets, G2M checkpoint, mTORC1 signaling, mitotic spindle, DNA repair, and E2F targets in the DLBCL group (Fig. 2E). The enriched signaling pathways exhibited a network regulation relationship with each other (Fig. 2D). Inhibition of the UV response DN and KRAS signaling DN was inhibited (Fig. 2F). Using GSEA analysis, the KEGG pathway enrichment of DEGs between DLBCL and RLH was evaluated (Fig. 2G). The analysis demonstrated activation of proteasome, pyrimidine metabolism, valine leucine and isoleucine degradation, purine metabolism, DNA replication, and cell cycle, while the hematopoietic cell lineage, cell adhesion molecules CAMs, neuroactive ligand receptor interaction, and cytokine cytokine receptor interaction were inhibited (Fig. 2H,I). These findings suggest that signaling pathways, including DNA replication and cell cycle regulation, may have a significant role in DLBCL development.
WGCNA
WGCNA analysis was performed using microarray data from GSE32018. No significant outliers were identified in the data through outlier detection (Fig. 3A). A soft threshold power of 6 and a scale-free index of 0.9 were obtained, indicating reasonable connectivity (Fig. 3B). Construction of the topological overlap matrix and correlation matrix between the data genes was followed by the building of the co-expression network and the drawing of the clustering dendrogram with dynamic tree cuts and merged dynamic maps (Fig. 3C,D). The data clustering results were eventually classified into 7 modules (Fig. 3E). Calculation of correlation coefficients between the modules and DLBCL-related phenotypes revealed that the MEbrown module had the strongest correlation with DLBCL (cor = 0.65, p = 1e-04). Figure 3F displays the correlation heatmap between these modules. Good correlation within the MEbrown module was demonstrated by scatter plots of module membership (MM) and gene significance (GS) (cor = 0.67, p < 1e-200) (Fig. 3G). Therefore, the MEbrown module may serve as an optimised module for elucidating DLBCL features. An intersection of 4402 key module genes with DEGs yielded 943 DLBCL target genes (Fig. 4A).
Identification of WGCNA module genes. (A) Sample tree and characteristic heat map. (B) Select the soft threshold. (C,D) Cluster tree of WGCNA. (E) Correlation between gene modules and DLBCL and RLH. (F) Correlation between modules. (G) Scatterplot of the correlation between MM and GS in brown modules.
Acquisition and enrichment analysis of CMC-DLBCL common target. (A) DLBCL target genes acquisition. (B) CMC-DLBCL common targets acquisition. (C) Drug-active ingredient-target network diagram. (D) GO enrichment analysis results of common targets. (E) KEGG enrichment analysis results of common targets.
Construction of drug-active ingredient-target network diagram
A total of 11 herbal medicines and 247 active ingredients were identified in CMC by querying the TCMSP database, HERB database, and literature. These included 1 species of Mylabris, 22 species of ginseng, 20 species of Hedysarum Multijugum Maxim, 19 species of Eleutherococcus senticosus, 5 species of Sparganii Rhizoma, 29 species of Scutellariae Barbatae Herba, 3 species of zedoary, 20 species of Cornus Officinalis Sieb, 13 species of Glossy Privet, 23 species of Bear Bile Powder, and 92 species of licorice. After eliminating duplicate ingredients, a total of 1,053 drug targets were obtained. Subsequently, an intersection of DLBCL target genes and CMC targets yielded 50 common targets (Fig. 4B). These common targets and active ingredients were imported into Cytoscape software to construct a network diagram of drug-active ingredient-target interactions (Fig. 4C), comprising 259 nodes and 927 edges. Based on DC values, the top five ranked major active ingredients of CMC for DLBCL treatment were identified as sitosterol, 3’-Methoxyglabridin, quercetin, kaempferol, and isorhamnetin.
GO and KEGG enrichment analyses
Enrichment analysis of CMC-DLBCL common targets revealed that BP were mainly involved in G1/S transition of mitotic cell cycle, cell cycle G1/S phase transition, positive regulation of cell cycle, regulation of cell cycle phase transition, and cell cycle checkpoint. The CC analysis mainly displayed associations with chromosomal region, cyclin-dependent protein kinase holoenzyme complex, serine/threonine protein kinase complex, chromosome, telomeric region, and protein kinase complex. MF analysis indicated the key activities are primarily related to protein serine/threonine kinase activity, histone kinase activity, cyclin-dependent protein serine/threonine kinase activity, cyclin-dependent protein kinase activity, and magnesium ion binding (Fig. 4D). The KEGG enrichment analysis showed significant associations with pathways such as the cell cycle, p53 signaling pathway, cellular senescence, FoxO signaling pathway, and PI3K-Akt signaling pathway (Fig. 4E).
Expression and distribution of common targets
Expression analysis of the GSE32018 dataset revealed significant upregulation of the 50 common targets previously identified in DLBCL (Fig. 5A). Validation with the TCGA dataset demonstrated significant upregulation of 45 out of these common targets in DLBCL, except for C5AR1, FPR2, IRAK4, MCL1, and PFKFB3 (Fig. 5B). Single-cell RNA-seq data from seven DLBCL patients were analyzed. Following stringent quality control and batch effect correction, high-quality cell data were obtained (Fig. 5C). We clustered the data into nine cell clusters using UMAP dimensionality reduction, with the clustering tree resolution set to 0.8 and the principal component number to 30 (Fig. 5D). The UMAP plot displayed the characteristic marker genes for each cell cluster (Fig. 5G), thereby further confirming the clustering results. We annotated these clusters into seven cell types, including DLBCL cells, NK cells, CD4+ T cells, CD8+ T cells, monocytes, plasma cells, and others, using marker genes from the CellMarker database (Fig. 5E). We employed the FindAllMarkers function in Seurat to identify marker genes for each cell population. A heatmap was subsequently generated to depict the gene expression patterns across each cell cluster, thereby revealing the characteristic gene types for each cluster (Fig. 5F). Further, GSEA pathway enrichment analysis of marker genes in the B cell tumor cell subpopulation revealed the activation of pathways related to MYC targets, G2M checkpoint, and E2F targets. Conversely, pathways including apical junction, complement, TNF-α signaling via NF-κB, IL2-STAT5 signaling, and KRAS signaling UP were observed to be suppressed (Fig. 5H-J), which is consistent with previous DEG enrichment results. Additionally, we used the AUCell package to score the expression of the previously identified 50 common CMC-DLBCL targets at the single-cell level (Fig. 5K). This analysis revealed that these targets were predominantly expressed in the tumor cell subpopulation .
Expression of 50 CMC-DLBCL common target genes in DLBCL transcriptome data and single-cell data. (A,B) Expression of 50 common target genes in GSE32018 and TCGA. (C) Quality control of single-cell data. (D) Clustering dendrogram. (E) UMAP clustering plot showing annotated clusters of different cell types. (F) Heatmap of annotated cell subpopulation marker expressions. (G) Expression of annotated cell subpopulation markers. (H) Hallmark pathway enrichment analysis of feature expression genes in merged B cell subpopulations. (I,J) Pathways activated and inhibited in B cell subpopulations. (K) Expression levels of 50 common targets after single-cell clustering.
Construction of the PPI network and identification of key genes
The 50 common CMC-DLBCL targets were uploaded to the String online database for the construction of a PPI network (Fig. 6A). The network consisted of 43 nodes and 236 edges, where each node represented a protein and the edges indicated interaction relationships. Notably, larger nodes corresponded to higher DC values. The interaction data was exported as a TSV file and subsequently imported into Cytoscape. Based on DC values, the top five key genes were identified as CDK1, CDK2, TOP2A, CHEK1, and CDC25C (Fig. 6B).
Screening, diagnosis and prognosis analysis of key genes. (A) PPI interaction network diagram. (B) Identification of key genes using Cytoscape software. (C,D) Expression of key genes in the GSE32018 and TCGA datasets. (E) ROC analysis of key genes. (F) Univariate Cox regression analysis and overall prognosis analysis of key genes in the GSE181063 dataset.
Expression, diagnostic and prognostic functions of key genes
Across the GSE32018 and TCGA datasets, the five key genes (CDK1, CDK2, TOP2A, CHEK1, CDC25C) were generally highly expressed in DLBCL. ROC analysis confirmed their good diagnostic value (Fig. 6C–E). A univariate Cox regression analysis was conducted on the GSE181063 dataset to assess the prognostic value of these genes. The results revealed that CDK1 (CDC2), TOP2A, CHEK1, and CDC25C were highly expressed and correlated with poor prognosis (P < 0.05). However, despite high expression, CDK2 did not show a significant correlation with prognosis. Multivariate Cox regression analysis further indicated that the collective high expression levels of these five key genes were significantly associated with poor prognosis (P < 0.001) (Fig. 6F). Hence, CDK1, CDK2, TOP2A, CHEK1, and CDC25C could potentially serve as crucial targets in DLBCL progression.
Molecular docking
We used MOE 2019 software to perform molecular docking, aiming to investigate the interactions between small molecular active ingredients and protein targets. The results suggested that sitosterol and 3’-Methoxyglabridin could penetrate the binding domains of the target proteins CDK1, CDK2, TOP2A, CHEK1, and CDC25C. The docking energy values ranged from − 5.8674 to -7.6058 kcal/mol (Fig. 7A–J). Of these, four docking groups demonstrated strong binding activity, and six groups exhibited good binding activity (Generally, docking energy values less than − 4.25 kcal/mol suggest some binding activity, values less than − 5.0 kcal/mol imply good binding activity, and those less than − 7.0 kcal/mol denote strong binding activity). These findings offer crucial insights for future drug design and development.
Molecular docking of major active ingredients with key genes. (A) Sitosterol-CDK1. (B) 3’-Methoxyglabridin-CDK1. (C) Sitosterol-CDK2. (D) 3’-Methoxyglabridin-CDK2. (E) Sitosterol-TOP2A. (F) 3’-Methoxyglabridin-TOP2A. (G) Sitosterol-CHEK1. (H) 3’-Methoxyglabridin-CHEK1. (I) Sitosterol-CDC25C. (J) 3’-Methoxyglabridin-CDC25C.
Molecular dynamics simulation
Initially, we assessed the equilibrium of the complexes using RMSD analysis. Figure 8A demonstrates that almost all complexes achieved equilibrium after 95 ns. 3’-Methoxyglabridin, compared to sitosterol, displayed more stable binding to the five target proteins. The CDK1/3’-Methoxyglabridin complex, in particular, demonstrated the lowest RMSD, with fluctuations around 3 Å. This observation signifies high stability of 3’-Methoxyglabridin when bound to CDK1. Further analysis indicated that 3’-Methoxyglabridin forms hydrogen bonds with CDK1. The Rg and SASA values of the complex remained stable throughout the simulation, suggesting a consistently compact structure (Fig. 8B-D). Figure 8E further substantiates the stability of their interaction by showing a low RMSF value for the 3’-Methoxyglabridin/CDK1 complex. In summary, the binding of 3’-Methoxyglabridin to CDK1 exhibits the highest stability, implying it may exert its effects by directly inhibiting the target protein.
Molecular dynamics simulation of 3’-Methoxyglabridin and sitosterol with target protein. (A) RMSD values of the five complexes. (B) Number of hydrogen bonds in the five complexes. (C) Radius of gyration (Rg) values of the five complexes. (D) Solvent-accessible surface area (SASA) values of the five complexes. (E) Root mean square fluctuation (RMSF) values of the five complexes.
In vitro experiments to evaluate the role of major active ingredients
In order to evaluate the effect of sitosterol on DLBCL cells, two cell lines Pfeiffer and U2932 were selected for in vitro experiments. The results of CCK-8 experiment showed that sitosterol inhibited the growth of both cell lines in a dose-dependent manner. It was further calculated that the half maximal inhibitory concentration (IC50) was 14 ng/mL and 6 ng/mL respectively (Fig. 9A,F). In order to further verify the pro-apoptotic effect of sitosterol on DLBCL cells, apoptosis rate was detected by Annexin V/PI double staining. Pfeiffer and U2932 cells were treated with a concentration gradient of sitosterol. Flow cytometry results showed that sitosterol induced concentration-dependent apoptosis in DLBCL cells, with the apoptosis rate increasing proportionally with the treatment concentration (**P < 0.01 or ***P < 0.001, n = 3, Fig. 9B–E, G–J).
Effects of sitosterol on viability and apoptosis of DLBCL cells. (A,F) The IC50 values of sitosterol treatment for Pfeiffer and U2932 cells were 14 ng/mL and 6 ng/mL respectively. (B–D) The results of flow cytometry for Pfeiffer cells in the PBS and sitosterol treatment group. (G–I) The results of flow cytometry for U2932 cells in the PBS and sitosterol treatment group. (E,J) Sitosterol induced concentration-dependent apoptosis in Pfeiffer and U2932 cells, with apoptotic rates escalating proportionally to treatment concentrations (**P < 0.01 or ***P < 0.001).
Discussion
DLBCL, a highly aggressive and heterogeneous form of NHL, has treatment outcomes and prognosis that are influenced by a variety of factors. Immunotherapy, chemotherapy, radiotherapy, autologous hematopoietic stem cell transplantation (ASCT), and Chimeric Antigen Receptor T-Cell Immunotherapy (CAR-T) are the primary treatment options for DLBCL10,11,12. Nonetheless, after standard first-line treatment, 30-40% of patients undergo disease progression or relapse13. Consequently, seeking effective treatment strategies is of paramount importance. CMC, an anti-tumor drug, comprises 11 traditional Chinese medicines, including Mylabris, ginseng, Hedysarum Multijugum Maxim, Sparganii Rhizoma, Scutellariae Barbatae Herba, zedoary, Cornus Officinalis Sieb, Glossy Privet, licorice, Eleutherococcus senticosus, and Bear Bile Powder5. However, its role in the context of DLBCL remains unclear. This study aims to elucidate the mechanism and potential targets of CMC in DLBCL treatment, leveraging bulk RNA sequencing datasets, single-cell RNA-seq datasets, and network pharmacology. Validation is achieved through molecular docking and molecular dynamics simulation.
Initially, we obtained bulk RNA sequencing datasets for DLBCL from the GEO database and identified DEGs. Further analysis indicated activation of DEGs in pathways like MYC targets, DNA repair, cell cycle, and purine metabolism, while pathways such as KRAS signaling and cell adhesion molecules (CAMs) were inhibited. Subsequently, we identified 50 common targets of CMC and DLBCL through WGCNA and network pharmacology analysis. GO and KEGG enrichment analyses demonstrated significant involvement of these common targets in biological processes, including the cell cycle, p53 signaling pathway, cellular senescence, FoxO signaling pathway, and PI3K-Akt signaling pathway. In human DLBCL cell lines, the PI3K/AKT signaling pathway is continuously activated. PI3K inhibition can induce apoptosis in the majority of DLBCL cells14. Studies indicate that low-dose lenalidomide, when combined with PI3K/mTOR inhibitors, hinders DLBCL progression by inhibiting CDK2 phosphorylation and reducing the number of S phase cells15. Transcriptomic and whole-genome analyses have uncovered that copy number alterations (CNA) in DLBCL result in diminished p53 activity, which in turn disrupts cell cycle regulation. In DLBCL patients exhibiting CNA in the p53 and cell cycle pathways, there is a decrease in the expression of p53 target genes, while the expression of E2F target genes and the Ki67 proliferation marker increases. The CNA of the CDKN2A-TP53-RB-E2F axis underpins DLBCL proliferation and could serve as a potential predictor of treatment efficacy and a feasible therapeutic target. Among DLBCL subtypes, patients carrying TP53 mutations (Mut-p53) display adverse prognostic characteristics, attributed to the dysregulation of the p53 signaling pathway and activation of the PI3K signaling pathway16. The nuclear export protein 1 (exportin 1, XPO1) inhibitor, Selinexor, is approved for treating relapsed/refractory DLBCL. However, resistance is noted in DLBCL patients with Mut-p5317. Investigating effective treatment strategies for DLBCL patients exhibiting dysregulation of the p53 signaling pathway could yield further insights into DLBCL therapy. The FoxO transcription factor family, by regulating gene expression, participates in physiological processes including apoptosis, cell cycle control, glucose metabolism, oxidative stress resistance, and lifespan extension. FoxO1 expression in DLBCL acts as a response molecule for PI3K/AKT inhibitors and could serve as a predictive marker for resistance to these inhibitors18. Thus, these findings align with our enrichment analysis results.
We further constructed a PPI network utilizing 50 common targets in CMC-DLBCL and pinpointed key genes based on DC values, namely CDK1, CDK2, TOP2A, CHEK1, and CDC25C. CDK1, a cyclin-dependent kinase, plays a vital role in cell cycle regulation. It is found to be overexpressed in DLBCL, and this overexpression is positively correlated with poor prognosis19,20. CDK2, another cyclin-dependent kinase, contributes to the cell cycle progression. Research suggests that apigenin can curtail DLBCL cell proliferation by downregulating CDK2 levels, and CDK2 expression is closely linked to survival in DLBCL patients21,22. TOP2A, a multifunctional nuclease, plays a significant role during cell division and DNA replication23. Chemotherapeutic strategies for DLBCL often encompass targeted agents against TOP2A, which can interact with TOP2A within DNA repair enzyme complexes to mitigate DLBCL progression24. CHEK1, a serine/threonine protein kinase, maintains genomic stability by activating various cell cycle checkpoints. Its involvement in the progression of multiple cancers is closely tied to prognosis25,26,27. Valentina et al. established that inhibiting CHEK1 expression levels could serve as a therapeutic strategy for DLBCL28. CDC25C, a member of the CDC25 family of cell cycle regulators, was found in a study involving 99 DLBCL patients to be expressed alongside CHEK1 in approximately half of the patients, marking DNA damage response activation. Utilizing inhibitors to target these pathways may serve as a therapeutic strategy for DLBCL29. The study’s results reveal significantly elevated expression levels of CDK1, CDK2, TOP2A, CHEK1, and CDC25C in DLBCL patients compared to the control group. These markers, consistent with previous findings, possess high diagnostic and prognostic value.
We conducted an expression analysis on 50 common targets between CMC and DLBCL using a single-cell RNA-seq dataset to validate the stability of these common targets. These genes, our results revealed, were primarily expressed in the DLBCL cell subgroups. In the GSE32018 and TCGA datasets, we observed significantly higher expression levels of CDK1, CDK2, TOP2A, CHEK1, and CDC25C in DLBCL patients compared to the normal group. Simultaneously, our ROC analysis indicated a promising diagnostic value for these genes. Our subsequent survival analysis, utilizing the GSE181063 dataset, identified CDK1, TOP2A, CHEK1, and CDC25C as independent risk factors for poor DLBCL prognosis. Moreover, a multivariate Cox regression analysis revealed these five key genes collectively contribute to a poor prognosis in DLBCL. The findings suggest that the key genes identified in this study present high feasibility as therapeutic targets for DLBCL, demonstrating both diagnostic and prognostic significance.
The assembly of the drug-active ingredient-target network disclosed the top five principal active ingredients: sitosterol, 3’-Methoxyglabridin, quercetin, kaempferol, and isorhamnetin. Studies have identified sitosterol as a plant sterol, abundantly found in cereals, nuts, and seeds, exhibiting anti-inflammatory and antioxidant properties30. Sitosterol and β-sitosterol are different names for the same ingredient, exhibits anti-cancer effects against various cancers including leukemia, lung, stomach, and liver cancer. It operates by interfering with cell proliferation, cell cycle arrest, apoptosis, angiogenesis, inflammation, and other signaling pathways31,32. He et al. discovered that β-sitosterol induces apoptosis in DLBCL cells, and can amplify the anti-DLBCL efficacy of rituximab by modulating the acid sphingomyelinase/Ceramide signal transduction33. 3’-Methoxyglabridin, a derivative of licorice, exhibits diverse pharmacological effects, including antioxidant, anti-inflammatory, and antibacterial properties34. Currently, there are no research reports on its role in DLBCL. Quercetin, widely found in fruits and vegetables, exerts anti-cancer effects by inhibiting cell proliferation, inducing cell apoptosis, and impeding the invasion and metastasis of cancer cells35,36. Research indicates that quercetin can significantly impede DLBCL cell proliferation, induce cell apoptosis, and enhance the condition of rituximab-resistant DLBCL37,38. Kaempferol exhibits diverse pharmacological properties, primarily encompassing antibacterial, anti-inflammatory, antioxidant, and anti-cancer activities. It can counteract cancers such as breast and cervical cancer by intervening in cell apoptosis and cell cycle arrest39,40. Zhan et al. discovered that kaempferol can significantly curtail the proliferation of DLBCL cells and induce cell apoptosis37. Isorhamnetin, an active ingredient in traditional Chinese medicine found in sea buckthorn and ginkgo leaves, exhibits a broad spectrum of medicinal effects, including cardiovascular and cerebrovascular protection, anti-tumor, and anti-inflammatory activities41. Research has identified that isorhamnetin can significantly suppress the proliferation and migration of breast cancer cells, and enhance the anti-tumor efficacy of doxorubicin against breast cancer cells both in vitro and in vivo42.
In DLBCL, CDK1/2 overexpression is associated with aggressive tumor behavior43,44,45.Our enrichment analysis highlights the involvement of cell cycle pathways in CMC’s mechanism of action. Sitosterol, a key phytosterol in CMC, has been reported to has an inhibitory effect on the activity of various cyclin–CDK complexes, such as cyclin D and CDK2, 4, and 6 which plays a pivotal role in DLBCL progression46.While a previous study showed that β-Sitosterol treatment increased p53 expression and its phosphorylation at Ser15. Studies have shown that sitosterol can contribute to the treatment of colorectal cancer via CDK1 and TOP2A interactions47. β-sitosterol can interact with CDK2, contributing to the treatment of breast cancer-related anxiety and Acute Gouty Arthritis48,49. Furthermore, Zhou and Li et al. discovered that β-sitosterol serves as an effective active ingredient for liver cancer treatment, associated with TOP2A and CHEK150,51. In this study, through molecular docking and molecular dynamics simulation, we demonstrated that sitosterol and 3’-Methoxyglabridin possess strong binding affinity with the five key genes, aligning with previous research findings. This implies that CMC could potentially serve as a pivotal drug in the treatment of DLBCL. In addition, we verified that sitosterol inhibited the growth and induces apoptosis of DLBCL cells in a dose-dependent manner through in vitro experiments. These results suggested that sitosterol might inhibit the proliferation of DLBCL cells by inducing apoptosis. As there is no extract of 3’-Methoxyglabridin in the market at present, this study only evaluates its effect on the bioinformatics level, and do not further evaluate its effect on DLBCL cells through experiments.
The multi-component nature of TCM implies that the bioavailability and compositional variability of CMC may significantly influence their therapeutic efficacy and toxicity profiles. To address these factors, comprehensive evaluations—including animal experiments and mass spectrometry-based analyses—are warranted. In particular, the pharmacokinetic properties of key bioactive components such as sitosterol and 3’-methoxyglabridin require validation through in vivo studies to assess their clinical feasibility.
CMC demonstrates promising CDK inhibitory effects, with potential advantages over existing inhibitors; however, these claims require experimental validation. Leveraging single-cell RNA sequencing data from DLBCL patients, our team will expand the dataset to explore CMC’s impact on drug resistance-associated genes and pathways. These efforts aim to establish a robust foundation for future research and clinical translation.
Conclusion
To summarize, CMC manifests anti-tumor effects in DLBCL by modulating targets like CDK1, CDK2, TOP2A, CHEK1, and CDC25C. These targets influence MYC targets, cell cycle, E2F targets, TNF-α signaling via NF-κB, IL2-STAT5 signaling, and KRAS signaling. Furthermore, the study affirmed the pivotal roles of two major active ingredients in CMC—sitosterol and 3’-Methoxyglabridin (the principal active ingredient of licorice) in DLBCL. This furnishes crucial research evidence supporting the use of CMC and licorice as standalone herbs in the treatment of DLBCL.
Data availability
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
References
Li, S., Young, K. H. & Medeiros, L. J. Diffuse large B-cell lymphoma. Pathology 50, 74–87. https://doi.org/10.1016/j.pathol.2017.09.006 (2018).
He, M. Y. & Kridel, R. Treatment resistance in diffuse large B-cell lymphoma. Leukemia 35, 2151–2165. https://doi.org/10.1038/s41375-021-01285-3 (2021).
Liu, Y. et al. Traditional Chinese medicine for Cancer treatment. Am. J. Chin. Med. 52, 583–604. https://doi.org/10.1142/S0192415X24500253 (2024).
Wang, K. et al. Anticancer activities of TCM and their active components against Tumo metastasis. Biomed. Pharmacother. 133, 111044. https://doi.org/10.1016/j.biopha.2020.111044 (2021).
Liu, Y. et al. Fufang Banmao capsule, a traditional Chinese medicinal formulation, enhances the survival of patients with hepatocellular carcinoma and Vp3-4 portal vein tumor thrombosis undergoing supportive treatment. J. Altern. Complement. Med. 26, 956–965. https://doi.org/10.1089/acm.2019.0334 (2020).
Liu, K. et al. Seven oral traditional Chinese medicine combined with chemotherapy for the treatment of non-small cell lung cancer: a network meta-analysis. Pharm. Biol. 62, 404–422. https://doi.org/10.1080/13880209.2024.2351940 (2024).
Bi, D., Chai, X. Y., Song, Y. L., Lei, Y. & Tu, P. F. Novel bile acids from bear bile powder and bile of geese. Chem. Pharm. Bull. (Tokyo). 57, 528–531. https://doi.org/10.1248/cpb.57.528 (2009).
Jo, S., Kim, T., Iyer, V. G. & Im, W. CHARMM-GUI: a web-based graphical user interface for CHARMM. J. Comput. Chem. 29, 1859–1865. https://doi.org/10.1002/jcc.20945 (2008).
Mark, P. & Nilsson, L. Structure and dynamics of the TIP3P, SPC, and SPC/E water models at 298 K. J. Phys. Chem. A. 105, 9954–9960. https://doi.org/10.1021/jp003020w (2001).
Stephens, D. M. et al. Continued risk of relapse independent of treatment modality in Limited-Stage diffuse large B-Cell lymphoma: final and Long-Term analysis of Southwest oncology group study S8736. J. Clin. Oncol. 34, 2997–3004. https://doi.org/10.1200/JCO.2015.65.4582 (2016).
Mounier, N. et al. High-dose therapy and autologous stem cell transplantation in first relapse for diffuse large B cell lymphoma in the rituximab era: an analysis based on data from the European blood and marrow transplantation registry. Biol. Blood Marrow Transpl. 18, 788–793. https://doi.org/10.1016/j.bbmt.2011.10.010 (2012).
Schuster, S. J. et al. Tisagenlecleucel in adult relapsed or refractory diffuse large B-Cell lymphoma. N Engl. J. Med. 380, 45–56. https://doi.org/10.1056/NEJMoa1804980 (2019).
CoiffierB & SarkozyC Diffuse large B-cell lymphoma: R-CHOP failure-what to do? Hematol. Am. Soc. Hematol. Educ. Program. 2016, 366–378. https://doi.org/10.1182/asheducation-2016.1.366 (2016).
Uddin, S. et al. Role of phosphatidylinositol 3’-kinase/AKT pathway in diffuse large B-cell lymphoma survival. Blood 108, 4178–4186. https://doi.org/10.1182/blood-2006-04-016907 (2006).
Jin, Z. et al. Low dose of Lenalidmide and PI3K/mTOR inhibitor trigger synergistic cytoxicity in activated B cell-like subtype of diffuse large B cell lymphoma. J. Exp. Clin. Cancer Res. 35, 52. https://doi.org/10.1186/s13046-016-0327-x (2016).
Shen, R. et al. Simplified algorithm for genetic subtyping in diffuse large B-cell lymphoma. Signal. Transduct. Target. Ther. 8, 145. https://doi.org/10.1038/s41392-023-01358-y (2023).
Deng, M. et al. XPO1 expression worsens the prognosis of unfavorable DLBCL that can be effectively targeted by Selinexor in the absence of mutant p53. J. Hematol. Oncol. 13, 148. https://doi.org/10.1186/s13045-020-00982-3 (2020).
Szydlowski, M. et al. FOXO1 activation is an effector of SYK and AKT Inhibition in tonic BCR signal-dependent diffuse large B-cell lymphomas. Blood 127, 739–748. https://doi.org/10.1182/blood-2015-06-654111 (2016).
Zhao, X. F. & Gartenhaus, R. B. Phospho-p70S6K and cdc2/cdk1 as therapeutic targets for diffuse large B-cell lymphoma. Expert Opin. Ther. Targets. 13, 1085–1093. https://doi.org/10.1517/14728220903103833 (2009).
Dai, L. et al. Single-cell and Spatial transcriptomics reveal a high Glycolysis B cell and tumor-associated macrophages cluster correlated with poor prognosis and exhausted immune microenvironment in diffuse large B-cell lymphoma. Biomark. Res. 12, 58. https://doi.org/10.1186/s40364-024-00605-w (2024).
Huang, S. et al. Apigenin and abivertinib, a novel BTK inhibitor synergize to inhibit diffuse large B-cell lymphoma in vivo and vitro. J. Cancer. 11, 2123–2132. https://doi.org/10.7150/jca.34981 (2020).
Faber, A. C. & Chiles, T. C. Inhibition of cyclin-dependent kinase-2 induces apoptosis in human diffuse large B-cell lymphomas. Cell. Cycle. 6, 2982–2989. https://doi.org/10.4161/cc.6.23.4994 (2007).
Nitiss, J. L. DNA topoisomerase II and its growing repertoire of biological functions. Nat. Rev. Cancer. 9, 327–337. https://doi.org/10.1038/nrc2608 (2009).
Jain, N. et al. Targeting nucleolin for better survival in diffuse large B-cell lymphoma. Leukemia 32, 663–674. https://doi.org/10.1038/leu.2017.215 (2018).
Ma, C. X., Janetka, J. W. & Piwnica-Worms, H. Death by releasing the breaks: CHK1 inhibitors as cancer therapeutics. Trends Mol. Med. 17, 88–96. https://doi.org/10.1016/j.molmed.2010.10.009 (2011).
Yin, Y. et al. Chk1 Inhibition potentiates the therapeutic efficacy of PARP inhibitor BMN673 in gastric cancer. Am. J. Cancer Res. 7, 473–483 (2017).
Liu, X. P. et al. Strong correlation between the expression of CHEK1 and clinicopathological features of patients with multiple myeloma. Crit. Rev. Eukaryot. Gene Expr. 30, 349–357. https://doi.org/10.1615/CritRevEukaryotGeneExpr.2020027084 (2020).
Restelli, V. et al. Inhibition of CHK1 and WEE1 as a new therapeutic approach in diffuse large B cell lymphomas with MYC deregulation. Br. J. Haematol. 181, 129–133. https://doi.org/10.1111/bjh.14506 (2018).
Derenzini, E. et al. Constitutive activation of the DNA damage response pathway as a novel therapeutic target in diffuse large B-cell lymphoma. Oncotarget 6, 6553–6569. https://doi.org/10.18632/oncotarget.2720 (2015).
Singh, A. Sitosterol as an antioxidant in frying oils. Food Chem. 137, 62–67. https://doi.org/10.1016/j.foodchem.2012.10.008 (2013).
Chen, Y. et al. Beta-Sitosterol suppresses hepatocellular carcinoma growth and metastasis via FOXM1-regulated Wnt/beta-catenin pathway. J. Cell. Mol. Med. 28, e18072. https://doi.org/10.1111/jcmm.18072 (2024).
Nandi, S. et al. Anticancer activity and other biomedical properties of beta-sitosterol: bridging phytochemistry and current Pharmacological evidence for future translational approaches. Phytother Res. 38, 592–619. https://doi.org/10.1002/ptr.8061 (2024).
He, G. et al. Beta-Sitosterol inhibits tumor growth and amplifies rituximab sensitivity through acid sphingomyelinase/ceramide signaling in diffuse large B-Cell lymphoma. J. Agric. Food Chem. 72, 16177–16190. https://doi.org/10.1021/acs.jafc.4c00014 (2024).
Luo, Z. et al. Action mechanism underlying improvement effect of Fuzi Lizhong Decoction on nonalcoholic fatty liver disease: a study based on network Pharmacology and molecular Docking. Evid. Based Complement. Alternat Med. 2022, 1670014. https://doi.org/10.1155/2022/1670014 (2022).
Wang, M. et al. The targeting of noncoding RNAs by Quercetin in Cancer prevention and therapy. Oxid. Med. Cell. Longev. 2022, 4330681. https://doi.org/10.1155/2022/4330681 (2022).
Kasiri, N., Rahmati, M., Ahmadi, L., Eskandari, N. & Motedayyen, H. Therapeutic potential of Quercetin on human breast cancer in different dimensions. Inflammopharmacology 28, 39–62. https://doi.org/10.1007/s10787-019-00660-y (2020).
Zhan, X. Z. et al. Determination and mechanism of Xiao-Ai Jie-Du Decoction against diffuse large B-cell lymphoma: in Silico and in vitro studies. J. Ethnopharmacol. 319, 117271. https://doi.org/10.1016/j.jep.2023.117271 (2024).
Zhao, Q. et al. Biomarkers and coptis chinensis activity for rituximab-resistant diffuse large B-cell lymphoma: combination of bioinformatics analysis, network Pharmacology and molecular Docking. Technol. Health Care. 32, 2091–2105. https://doi.org/10.3233/THC-230738 (2024).
Imran, M. et al. Kaempferol: a key emphasis to its anticancer potential. Molecules 24 https://doi.org/10.3390/molecules24122277 (2019).
Wang, X., Yang, Y., An, Y. & Fang, G. The mechanism of anticancer action and potential clinical use of Kaempferol in the treatment of breast cancer. Biomed. Pharmacother. 117, 109086. https://doi.org/10.1016/j.biopha.2019.109086 (2019).
Gong, G. et al. Isorhamnetin: a review of Pharmacological effects. Biomed. Pharmacother. 128, 110301. https://doi.org/10.1016/j.biopha.2020.110301 (2020).
Yang, T. et al. Isorhamnetin induces cell cycle arrest and apoptosis by triggering DNA damage and regulating the AMPK/mTOR/p70S6K signaling pathway in doxorubicin-resistant breast cancer. Phytomedicine 114, 154780. https://doi.org/10.1016/j.phymed.2023.154780 (2023).
Zhao, M. Y. et al. Phospho-p70S6K/p85S6K and cdc2/cdk1 are novel targets for diffuse large B-cell lymphoma combination therapy. Clin. Cancer Res. 15, 1708–1720. https://doi.org/10.1158/1078-0432.CCR-08-1543 (2009).
Chen, Q. et al. CDK1 inhibitor RO-3306 enhances BTKi potency in diffuse large B-cell lymphoma by suppressing JAK2/STAT3 signaling. Int. J. Biol. Macromol. 297, 139893. https://doi.org/10.1016/j.ijbiomac.2025.139893 (2025).
Chen, Q. et al. Prognostic significance of CDK1 expression in diffuse large B-Cell lymphoma. BMC Cancer. 25, 20. https://doi.org/10.1186/s12885-024-13388-y (2025).
Wang, H., Wang, Z., Zhang, Z., Liu, J. & Hong, L. β-Sitosterol as a promising anticancer agent for chemoprevention and chemotherapy: mechanisms of action and future prospects. Adv. Nutr. 14, 1085–1110. https://doi.org/10.1016/j.advnut.2023.05.013 (2023).
Islam, M. A. et al. Exploring core genes by comparative transcriptomics analysis for early diagnosis, prognosis, and therapies of colorectal cancer. Cancers (Basel) 15. https://doi.org/10.3390/cancers15051369 (2023).
Li, Z. H., Yang, G. H. & Wang, F. Molecular mechanisms of Baihedihuang Decoction as a treatment for breast cancer related anxiety: a network Pharmacology and molecular Docking study. World J. Clin. Cases. 10, 12104–12115. https://doi.org/10.12998/wjcc.v10.i33.12104 (2022).
Fan, Y. et al. Integrated molecular Docking with network Pharmacology to reveal the molecular mechanism of Simiao powder in the treatment of acute gouty arthritis. Evid. Based Complement. Alternat Med. 2021, 5570968. https://doi.org/10.1155/2021/5570968 (2021).
Zhou, X., Tan, F., Zhang, S., Wang, A. & Zhang, T. A strategy based on bioinformatics and machine learning algorithms reveals potential mechanisms of Shelian capsule against hepatocellular carcinoma. Curr. Pharm. Des. 30, 377–405. https://doi.org/10.2174/0113816128284465240108071554 (2024).
Li, C. et al. Identification of Formononetin as the active compound of CR-SR in hepatocellular carcinoma treatment: an integrated approach combining network pharmacology and weighted gene co-expression networks. Chem. Biol. Drug Des. 103, e14363. https://doi.org/10.1111/cbdd.14363 (2024).
Funding
This study was supported by Natural Science Foundation of Xinjiang Uygur Autonomous (2022D01D21) and the National Natural Science Foundation of China (82360037).
Author information
Authors and Affiliations
Contributions
CCW: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing—original draft. JTW: Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing—original draft. JY: Conceptualization, Data curation, Investigation, Methodology, Software, Visualization, Writing—original draft. NF: Investigation, Software, Visualization. RZ: Formal analysis, Investigation, Validation. JJM: Software, Validation. HXG: Formal analysis, Visualization. GDZ: Conceptualization, Project administration, Supervision, Writing—review & editing. XXL: Conceptualization, Funding acquisition, Project administration, Supervision, Writing—review & editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, C., Wang, J., Yu, J. et al. Multi-omics and experimental validation reveal mechanism of compound mylabris capsules in treating diffuse large B-cell lymphoma. Sci Rep 15, 23856 (2025). https://doi.org/10.1038/s41598-025-09767-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-09767-5