Abstract
The incidence of chronic limb-threatening ischemia, the most severe form of peripheral artery disease, is increasing. A considerable portion are deemed “no-option” patients and have high rates of limb loss and death, with even worse outcomes in underrepresented populations. This study aimed to delineate real-world, contemporary outcomes in an observational study of no-option chronic limb-threatening ischemia patients. The composite primary end point was amputation-free survival (defined as freedom from death and above-ankle amputation) at 1 year. A total of 180 patients with no-option chronic limb-threatening ischemia were included from 22 centers across the US. The median age was 70 years (IQR, 61–78 years), 33% were women, 39% were Black, and 11% were Hispanic/Latino. Comorbidities included 76% with diabetes, 33% with heart failure, and 25% with end-stage renal disease. At 1 year, the amputation-free survival rate was 37%, 45% had major amputation, and 33% died. Additionally, two-thirds of the remaining patients had persistent non-healing ulcers, 44% had minor amputation, and 83% required ambulatory assistance. In this severely diseased population, approximately half of patients underwent major amputation and one-third died within a year, highlighting the pressing need for innovative interventions for limb salvage.
Similar content being viewed by others
Introduction
There is a global epidemic of non-traumatic amputations primarily attributable to the rising prevalence of diabetes and peripheral artery disease1,2. These vascular diseases compromise lower limb blood flow and can lead to chronic limb-threatening ischemia, where progressive tissue necrosis and gangrene may necessitate amputation3. Advanced revascularization techniques can prevent the need for amputation by re-establishing perfusion to the leg; however, up to 20% of patients with advanced, end-stage chronic limb-threatening ischemia are ineligible for conventional revascularization techniques. These patients are termed “no-option” – either due to lack of arterial targets for open or endovascular intervention or non-responsiveness to revascularization attempts – and their limbs are considered unsalvageable4,5. A large meta-analysis revealed that a staggering one-third of patients face amputation within the year they are diagnosed with chronic limb-threatening ischemia, which is a significant concern given the associated mortality rates and detrimental socioeconomic consequences of amputation6,7,8,9.
The chronic limb-threatening ischemia population is heterogeneous in terms of risk factors, demographics, and socioeconomic variables, in addition to variability in providers, surveillance, and treatment strategies, making large cohort studies challenging to perform. Regardless of this inconsistency and given the increase in the incidence of patients with chronic limb-threatening ischemia, technologies and techniques have emerged to optimize limb salvage outcomes. However, there currently exists a gap in contemporary data on the natural progression of no-option chronic limb-threatening ischemia patients, making it challenging to accurately determine the impact of new therapies in truly decreasing amputation rates.
To address this need, a prospective, US-based, multicenter study was conducted to comprehensively capture real-world rates of amputation, survival, and limb salvage outcomes among no-option chronic limb-threatening ischemia patients.
Methods
Study design and patients
The CLariTI study is a prospective, multicenter, observational study in the USA, designed to track the clinical progression of chronic limb-threatening ischemia and the incidence of amputation-free survival, survival, and limb salvage over 1 year. The study protocol was approved by the Western Institutional Review Board (WIRB) and the institutional review board at each participating center and all patients provided written informed consent, and the study was executed following Good Practice Guidelines and the Declaration of Helsinki. The study teams at each center included specialists in vascular surgery, interventional cardiology, and podiatry.
To ensure real-world data in this natural history study, site selection was carefully considered. Half of the study sites were recruited utilizing epidemiological data from population-based amputation rates for peripheral artery disease to identify regions in which there was a significant burden of chronic limb-threatening ischemia patients10. The other half of study sites were recruited from those participating in the concurrently running PROMISE II trial of the transcatheter arterialization of the deep veins procedure (NCT03970538) in no-option chronic limb-threatening ischemia11.
Analyses were performed by North American Science Association (a contract research organization; Minneapolis, MN) and the sponsor. The authors were granted unrestricted access to the data; the first author drafted the initial version, and all authors contributed to the critical review of the manuscript. All authors affirm the accuracy, completeness of the data, and adherence to the study protocol.
Patients with no-option chronic limb-threatening ischemia and non-healing ulcers (Rutherford 5 or 6) were recruited and screened for eligibility based on lower-limb angiography and prespecified study inclusion and exclusion criteria (described in the Supplemental Material). The study population included no-option chronic limb-threatening ischemia patients with inadequate popliteal, tibial, or pedal revascularization target (Pathway 1: Lack of Target) or at least 2 revascularization attempts in the last 6 months that failed to resolve symptoms (Pathway 2: Non-responders) as determined by the revascularization provider caring for the patient. Enrolled patients were followed for 1 year or until they expired, with visits at 3, 6, and 12 months. Per protocol patients included those who completed the study without any major protocol deviations.
Outcomes
The composite primary endpoint of amputation-free survival was defined as freedom from both major, above-ankle amputation (limb salvage) and all-cause mortality. Secondary endpoints included change in Rutherford classification, which ranges from 0 to 6, with higher numbers indicating worse disease, and incidence of minor, below-ankle, amputations. The primary and secondary endpoint assessments were completed at 1 year follow-up. Other outcomes collected included wound assessment for presence of osteomyelitis, gangrene, or an open wound; ambulatory status; worsening comorbidities, and further attempts at conventional revascularization.
Statistical analysis
A sample size of 186 patients was estimated using a two-sided Fisher’s exact test with 80% power to detect a 15-percentage point difference in amputation-free survival. This rate was assumed to be 55% based on the upper bound of the 95% confidence interval of a risk-adjusted meta-analytic average6while considering possible attrition or incomplete data. Baseline categorical variables were summarized with descriptive statistics, including the number of observations and percentages. Continuous variables were summarized as medians with interquartile ranges. Kaplan-Meier estimates were used to calculate time-to-event variables.
Cox regression modeling was used to assess the baseline characteristics as predictors of mortality and major amputation through 1 year. For major amputation, the Cox regression model included race (White, non-White), BMI category (obese [≥ 30], overweight [25–29.9], healthy [18.5–24.9], underweight [< 18.5]), history of heart failure (yes, no), and baseline Rutherford classification (5, 6). For death, the model included age (years), history of diabetes (yes, no), and history of renal disease (yes, no).
Data preparation and statistical analyses were performed using SAS software, version 9.4 (SAS Institute, Cary, NC), and R version 4.3.2.
Results
Between February 2020 and March 2022, a total of 192 patients were enrolled in the study across 22 centers in the United States with 180 per protocol patients. The median age was 70 years (IQR, 61 to 78), 60 (33.3%) were women, 65 (38.9%) were Black, and 20 (11.4%) were Hispanic or Latino (Table 1). Preexisting conditions and risk factors associated with chronic limb-threatening ischemia were common, including diabetes (76.1%), hypertension (92.2%), dyslipidemia (79.7%), and history of smoking (60.0%). Over half of patients had a history of renal disease (51.1%), with 25.0% end-stage dialysis-dependent disease and 22.8% chronic kidney disease.
Many patients (75.0%) had undergone previous revascularization attempts in the target limb within the previous 6 months, which were deemed unsuccessful. Non-ambulatory status or ambulatory assistance, defined as minimal, walker, or wheelchair assistance, was required in 84.9%. Three-quarters of patients (73.7%) had an open wound and 18.4% presented with osteomyelitis. Most patients were in the South (53.3%), followed by the Northeast/Mid-Atlantic (32.2%) regions. Two-thirds (67.8%) of patients had established care with the treating physician, predominantly vascular surgeons (55.0%) or interventional cardiologists (42.8%). Study follow-up was completed in 169 (93.9%) patients at 1 year; 10 patients were lost to follow-up and 1 patient withdrew. A total of 57 patients died during follow-up.
Overall, amputation-free survival was 37.3%, limb salvage was 55.1%, and survival was 66.8% at 1 year (Fig. 1). Of the 72 patients with unsalvageable limbs who underwent major amputation, 8.0% died through 30 days (peri-amputation rate), while 29.4% died within 1 year. Within the patients in Pathway 1, amputation-free survival was 34.1%, limb salvage was 51.3%, and survival was 66.6% at 1 year. Within the patients in Pathway 2, amputation-free survival was 44.4%, limb salvage was 63.2%, and survival was 67.3%. When stratified by geographic region, amputation-free survival was 40.4% in the South and limb salvage was 62.3% in the West/Midwest region. All other rates were comparable to the overall population.
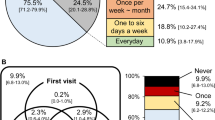
Figure 2A details the proportion of patients who either died, had a major amputation, or remained in a Rutherford classification of 5 or 6. In the patients who survived with their limbs, 67.7% remained in Rutherford classification of 5 or 6. Overall, an improvement of at least 1 Rutherford class was observed in 22.2% of patients at 6 months and 44.8% of patients at 1 year. In addition to major amputations, 44.3% of patients underwent a minor, below-ankle amputation (Supplementary Figure S1).
The proportion of patients with any wound or who had experienced major amputation or death was 90% at 3 months, 89% at 6 months, and 84% at 1 year (Fig. 2B). The proportion of patients needing wheelchair or walker assistance, were fully non-ambulatory, or who had experienced major amputation or death was 82% at 3 months and did not improve at 6 months and 1 year (Supplementary Figure S2). Overall, 83% of surviving patients with limbs needed some type of walking assistance at 1 year. At each follow-up point, approximately one-quarter of patients presented with worsening co-morbidities, most commonly kidney disease, hypertension, or diabetes (Supplementary Table S1). Further revascularization procedures were attempted on the target limb in 24.2% of patients between enrollment and 3 months follow-up, a further 12.1% between 3 and 6 months, and an additional 11.2% between 6 and 12 months. Of the revascularization procedures performed during the follow-up period, 90.7% were considered technically successful, but only 60.9% resulted in symptom relief. The most commonly performed intervention was angioplasty with uncoated balloons (Supplementary Table S2). Of note, within the revascularizations performed, 19 patients underwent 20 nonconventional endovascular revascularizations utilizing “off-label” deep vein arterialization with devices not approved or cleared for that indication by the FDA.
Cox regression modeling identified non-white race (HR: 2.31, 95% CI 1.34–3.98), history of heart failure (hazard ratio, 1.93; 95% CI 1.14–3.28), and a Rutherford 6 classification at baseline (hazard ratio 2.46; 95% CI 1.44–4.21) as independent predictors of increased rate of 1-year major amputation. Conversely, obese and overweight BMI (hazard ratio 0.49; 95% CI 0.27–0.92; hazard ratio 0.51, 95% CI 0.27–0.95) were found to have had a protective effect on major amputation. Age, diabetes, and renal disease were independent predictors of increased mortality at 1 year (Supplementary Table S1).
Discussion
This prospective study of no-option chronic limb-threatening ischemia demonstrates the poor outcomes of current standard of care despite significant technological advances for revascularization over the last decade. The patients in the study reflect a real-world scenario with the inclusion of underrepresented and geographically varied populations. Within 1 year, approximately a third of patients died and half underwent major amputation. Among those in whom amputation was performed, a further third died, underscoring the importance of limb salvage to prevent both morbidity and mortality. In the remaining patients, two-thirds had legs that remained ischemic with non-healing ulcers, despite standard care and additional revascularization attempts. As revascularization techniques advance to provide potential options to reduce amputation rates going forward, CLariTI will serve as an important benchmark for this patient population.
There are numerous challenges faced by clinicians and health systems that help explain the current outlook. While there is a major burden from chronic limb-threatening ischemia, the disease is characterized by heterogenicity in treatment practices, disease presentations, and patient demographics, which has made large, prospective studies challenging12. Furthermore, chronic limb-threatening ischemia studies historically have not had adequate enrollment of women or underrepresented minorities which is important given the major burden of this disease in these vulnerable populations13,14. The CLariTI study includes 33% women, nearly 40% Black, and 11% Hispanic or Latino patients, which represents real-world chronic limb-threatening ischemia populations. Amputation rates in peripheral artery disease vary by race and ethnicity, influenced by socioeconomic status, comorbidities, implicit biases, and disease severity15. Black, Hispanic, and Native American patients tend to fare worse in terms of amputation compared to White patients, even after adjusting for disease severity15,16,17. Similarly, CLariTI demonstrated that non-White race was predictive of major amputation at a rate twice that of White patients.
Recent research has highlighted disparities in care intensity preceding major amputation in chronic limb-threatening ischemia, wherein only 37% of patients undergo revascularization in the year leading up to amputation18. Additionally, regional disparities are evident, notably in the South where there exists a lower intensity of vascular care compared with other regions which is paired with higher amputation rates10. Notably, within CLariTI, eight centers in the South lacked the requisite personnel or infrastructure to partake in the study, despite being most affected by the amputation epidemic.
In the CLariTI study, the increased enrollment rates of minority participants compared to previous studies can be attributed to conscious efforts to recruit in regions with elevated amputation rates and limited vascular care. By engaging underrepresented groups who have historically had limited access to clinical trials, the study successfully increased minority participation, thus improving the generalizability and applicability of the study results10,19. The outcomes reported in the CLariTI study highlight the need for both dedicated chronic limb-threatening ischemia centers of excellence and standardization of care, as well as incorporating new tools and therapies to offer new options to these patients.
Finally, chronic limb-threatening ischemia patients commonly present with severe comorbidities. Diabetes is a major risk factor for peripheral artery disease, associated with up to 70% of lower-extremity amputations in the United States and was a common comorbidity in the CLariTI study2. Chronic kidney disease, often associated with diabetes and heart failure, also emerges as a significant risk factor for peripheral artery disease and subsequent amputation. The CLariTI data demonstrated established comorbidities that are associated with advanced chronic limb-threatening ischemia: 76% of patients had diabetes, 33% had heart failure, and 25% had end-stage renal disease. Other well-established risk factors for peripheral artery disease include smoking, hypertension, and dyslipidemia, which were prevalent in the enrolled patients of the CLariTI study.
Due to the aforementioned disparities, disease progression, and comorbidities, limited evidence exists regarding the outcomes of no-option chronic limb-threatening ischemia patients as these patients are commonly excluded from clinical trials. For perspective, even though not conducted to evaluate no-option chronic limb-threatening ischemia patients, for perspective, the BEST-CLI showed that amputation-free survival was 37–47% for patients with bypass or endovascular treatments, while BASIL-2 showed that it was 45–53%.13–14. Despite variations in the definition and severity of no-option chronic limb-threatening ischemia, a recent meta-analysis encompassing studies between 2006 and 2019 revealed an amputation-free survival rate of 33.3% at 1 year6. Together with CLariTI, these figures underscore the alarming prevalence of such outcomes despite the advancements and availability of state-of-the-art therapies in the United States.
In no-option chronic limb-threatening ischemia patients, treatment approaches include medical management, pain management, stem-cell therapies, hyperbaric oxygen, and intermittent pneumatic compression; these options have shown mixed results20. The imperative for more purposeful interventions has become apparent. Strategic arterialization of veins has emerged as a novel approach which offers the possibility of revascularization and limb salvage in many severely disadvantaged patients with no-option chronic limb-threatening ischemia21,22,23,24,25. Recent PROMISE I, II, and UK trials have demonstrated transcatheter arterialization of deep veins as a safe and viable option. The PROMISE I and UK trials reported 1-year amputation-free survival rates of 70% and 67%, respectively, in a very similar population, significantly higher than the 37% rate observed in CLariTI patients26,27. A recent propensity stratification analysis comparing 6 month outcomes from PROMISE II and CLariTI revealed a relative increase of 45% amputation-free survival rate among patients who underwent transcatheter arterialization of deep veins28. These findings, in conjunction with the meta-analysis, suggest that a subset of patients within CLariTI might have preserved their limbs had they been offered transcatheter arterialization of deep veins.
Limitations
The study has some limitations. This study was conducted during the COVID-19 pandemic, and related disruptions in healthcare access, staffing, and patient behavior may have influenced study enrollment and outcomes. As an observational study with enrollment determined by primary operators there was potential for selection bias. Sampling bias also may have occurred, given the involvement of 22 centers nationwide. However, the study design accomplishes the aim of capturing real-world factors influencing procedural outcomes. Given the real-world aspect of the study, there were variations in practice patterns and the required infrastructure to provide potential interventions. There was also an underrepresentation of hospitals in remote regions or among patients referred through alternative channels such as the emergency department. Finally, despite efforts to exclude patients with psychosocial conditions, there may have been unidentified psychosocial determinants of health influencing the study outcomes10.
Conclusions
CLariTI, a multicenter prospective observational registry, portrays the real-world outcomes faced by no-option chronic limb-threatening ischemia patients. Despite advancements in revascularization techniques, a significant portion of these individuals experience major amputation or mortality within a year, underscoring the urgent need for innovative solutions in advanced limb salvage.
Data availability
Data will be shared with bona fide researchers who submit a research proposal approved by an independent review board to the corresponding author.
References
Mokdad, A. H. et al. The continuing epidemics of obesity and diabetes in the united States. JAMA 286, 1195–1200. https://doi.org/10.1001/jama.286.10.1195 (2001).
Creager, M. A. et al. Reducing nontraumatic Lower-Extremity amputations by 20% by 2030: time to get to our feet: A policy statement from the American heart association. Circulation 143, e875–e891. https://doi.org/10.1161/CIR.0000000000000967 (2021).
Okazaki, J. et al. Analysis of wound healing time and wound-free period as outcomes after surgical and endovascular revascularization for critical lower limb ischemia. J. Vasc Surg. 67, 817–825. https://doi.org/10.1016/j.jvs.2017.07.122 (2018).
Sigvant, B., Lundin, F. & Wahlberg, E. The risk of disease progression in peripheral arterial disease is higher than expected: A Meta-Analysis of mortality and disease progression in peripheral arterial disease. Eur. J. Vasc Endovasc Surg. 51, 395–403. https://doi.org/10.1016/j.ejvs.2015.10.022 (2016).
Duff, S., Mafilios, M. S., Bhounsule, P. & Hasegawa, J. T. The burden of critical limb ischemia: a review of recent literature. Vasc Health Risk Manag. 15, 187–208. https://doi.org/10.2147/VHRM.S209241 (2019).
Ghare, M. I. et al. Outcomes among patients with chronic critical limb ischemia with no revascularization option: systematic review and Meta-Analysis. J. Crit. Limb Ischemia. 1, 2694 (2021).
Rowley, W. R. et al. : Insights from Yesterday, Today, and Future Trends. Popul Health Manag 20, 6–12. https://doi.org/10.1089/pop.2015.0181 (2017).
Norgren, L. et al. Inter-Society consensus for the management of peripheral arterial disease (TASC II). J. Vasc Surg. 45, 5–67. https://doi.org/10.1016/j.jvs.2006.12.037 (2007).
Jones, W. S. et al. High mortality risks after major lower extremity amputation in medicare patients with peripheral artery disease. Am. Heart J. 165, 809–815. https://doi.org/10.1016/j.ahj.2012.12.002 (2013).
Goodney, P. P. et al. Regional intensity of vascular care and lower extremity amputation rates. J. Vasc Surg. 57, 1471–1480. https://doi.org/10.1016/j.jvs.2012.11.068 (2013).
Shishehbor, M. H. et al. Transcatheter arterialization of deep veins in chronic Limb-Threatening ischemia. N Engl. J. Med. 388, 1171–1180. https://doi.org/10.1056/NEJMoa2212754 (2023).
Conte, M. S. et al. Global vascular guidelines on the management of chronic limb-threatening ischemia. J Vasc Surg 69, 3–125 e140. https://doi.org/10.1016/j.jvs.2019.02.016 (2019).
Bradbury, A. W. et al. A vein bypass first versus a best endovascular treatment first revascularisation strategy for patients with chronic limb threatening ischaemia who required an infra-popliteal, with or without an additional more proximal infra-inguinal revascularisation procedure to restore limb perfusion (BASIL-2): an open-label, randomised, multicentre, phase 3 trial. Lancet 401, 1798–1809. https://doi.org/10.1016/S0140-6736(23)00462-2 (2023).
Farber, A. et al. Surgery or endovascular therapy for chronic Limb-Threatening ischemia. N Engl. J. Med. 387, 2305–2316. https://doi.org/10.1056/NEJMoa2207899 (2022).
Jaramillo, E. A. et al. Racial and ethnic disparities in major adverse limb events persist for chronic limb threatening ischemia despite presenting limb threat severity after peripheral vascular intervention. J. Vasc Surg. 77, 848–857. https://doi.org/10.1016/j.jvs.2022.10.043 (2023).
Anjorin, A. C. et al. Racial and ethnic disparities in 3-year outcomes following infrainguinal bypass for chronic limb-threatening ischemia. J. Vasc Surg. 76, 1335–1346. https://doi.org/10.1016/j.jvs.2022.06.026 (2022).
Barnes, J. A., Eid, M. A., Creager, M. A. & Goodney, P. P. Epidemiology and risk of amputation in patients with diabetes mellitus and peripheral artery disease. Arterioscler. Thromb. Vasc Biol. 40, 1808–1817. https://doi.org/10.1161/ATVBAHA.120.314595 (2020).
Secemsky, E. A. et al. Impact of intensity of vascular care preceding major amputation among patients with chronic Limb-Threatening ischemia. Circ. Cardiovasc. Interv. 17, e012798. https://doi.org/10.1161/CIRCINTERVENTIONS.122.012798 (2024).
Schwartz, A. L., Alsan, M., Morris, A. A. & Halpern, S. D. Why diverse clinical trial participation matters. N Engl. J. Med. 388, 1252–1254. https://doi.org/10.1056/NEJMp2215609 (2023).
Farber, A. & Eberhardt, R. T. The current state of critical limb ischemia: A systematic review. JAMA Surg. 151, 1070–1077. https://doi.org/10.1001/jamasurg.2016.2018 (2016).
Ferraresi, R. et al. Hybrid foot vein arterialization in No-Option patients with critical limb ischemia: A preliminary report. J. Endovasc Ther. 26, 7–17. https://doi.org/10.1177/1526602818820792 (2019).
Kum, S. et al. Percutaneous deep venous arterialization in patients with critical limb ischemia. J. Cardiovasc. Surg. (Torino). 59, 665–669. https://doi.org/10.23736/S0021-9509.18.10569-6 (2018).
Saab, F. A. et al. Percutaneous deep venous arterialization: treatment of patients with End-Stage plantar disease. J. Soc. Cardiovasc. Angiography Interventions. 1, 100437. https://doi.org/10.1016/j.jscai.2022.100437 (2022).
Montero-Baker, M., Sommerset, J. & Miranda, J. A. Hybrid superficial venous arterialization and endovascular deep venous arterialization. J. Vasc Surg. Cases Innov. Tech. 9, 101160. https://doi.org/10.1016/j.jvscit.2023.101160 (2023).
Saini, N., Marrone, L., Desai, S., Herman, K. C. & Rundback, J. H. Comparison of outcomes of percutaneous deep venous arterialization in multiple practice settings. J. Vasc Surg. https://doi.org/10.1016/j.jvs.2024.05.051 (2024).
Clair, D. G. et al. PROMISE I: early feasibility study of the limflow system for percutaneous deep vein arterialization in no-option chronic limb-threatening ischemia: 12-month results. J. Vasc Surg. 74, 1626–1635. https://doi.org/10.1016/j.jvs.2021.04.057 (2021).
Zayed, H. et al. Transcatheter arterialization of the deep veins: 1-year outcomes of PROMISE-UK study. Br. J. Surg. 111, znae188. https://doi.org/10.1093/bjs/znae188 (2024).
Powell, R. J., Mullin, C. M., Clair, D. G., Shishehbor, M. H. & Dua, A. Comparison of transcatheter arterialization of deep veins to standard of care in patients with No-Option chronic limb threatening ischemia. Ann. Vasc Surg. 99, 50–57. https://doi.org/10.1016/j.avsg.2023.08.010 (2024).
Funding
The CLariTI study was sponsored by Inari Medical, Irvine, CA.
Author information
Authors and Affiliations
Contributions
AD, PAS, RJP, DC, MHS designed the study, researched data, had access to the study data, contributed to the discussion, and wrote the manuscript. SG wrote the first draft of the manuscript with input from AD. AD, ZND, ACL, NB, JLM, LFC, MCB, JLMT, SG, SSG recruited patients, contributed to the discussion, and reviewed and edited the manuscript. All authors approved submission of the final version of the manuscript and had access to the data. AD and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
AD: Educational consultant for Boston Scientific, Abbott, Penumbra, Gore. RJP: No disclosures. ACL: Advisory Board for FastWave Medical, Consultant for Abbott, BD, Cook Medical, Inari Medical. NB: No disclosures. JLM: Advisory Board for Xylocor and IsomAb. LFC: No disclosures. MCB: Consultant for Abbott Vascular, Shockwave Medical, Amgen, and Inari Medical; Institutional research support from Inari Medical and Johnson and Johnson. JLMT: No disclosures. SG: No disclosures. SSG: No disclosures. ZND: No disclosures. PAS has nothing to disclose. DC: Advisory and consultant for Boston Scientific, Bard Peripheral Vascular, Medtronic, and LimFlow. MHS: Advisory and consultant for Abbott Vascular, Medtronic, Terumo, Boston Scientific, Philips, ANT, Inquis Medical, and Inari Medical.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Dua, A., Powell, R.J., Lee, A.C. et al. Contemporary outcomes in no-option chronic limb-threatening ischemia. Sci Rep 15, 24446 (2025). https://doi.org/10.1038/s41598-025-09784-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-09784-4