Abstract
The nutritional support program for malnourished pregnant and lactating mothers has been implemented to improve the health of both pregnant women and their infants and reduce their mortality rates. The aim of this retrospective field trial was to compare the effects of the food basket program and the cash transfer program to support pregnant and lactating mothers in needy suffering from malnutrition in Iran. The participants recruited from health centers were divided into 4 groups: food basket (n = 241), cash transfer (n = 213), eligible non-supported (n = 438), and non-needy control (n = 439). Information collected includes age, body mass index before pregnancy, mother’s weight gain and hemoglobin in the 4th and 8th months, the infants’ weight and head circumference at birth, and the weighing trend. The pre-pregnancy weight of the non-needy control group was significantly higher (p < 0.001). The average hemoglobin was significantly decreased in all 4 groups in the 8th month of pregnancy (p < 0.001). The weight gain of mothers improved significantly from the fourth to the eighth month of pregnancy in the food basket group (p < 0.001). The weight of infants in the eligible unsupported group at 2 and 4 months was significantly lower and in the cash transfer group was more than the food basket group (p < 0.001). It seems that the cash transfer method is more effective on weighing infants during the first 4 months after birth than the food basket approach, while the food basket had a more significant effect on the weight gain of mothers during pregnancy.
Similar content being viewed by others
Introduction
Pregnancy is a vital period in a woman’s life and nutrition during pregnancy affects her and her child’s future health1. Proper nutrition can prevent birth defects and the risks of adverse pregnancy outcomes, including cesarean section, severe anemia and postpartum hemorrhage for the mother and the birth of premature or low birth weight (LBW) infants2 and respiratory diseases, which can be lead to reducing obesity and osteoporosis and diabetes in adults3. If women suffer from malnutrition due to poor nutrition, this can increase the risk of adverse pregnancy outcomes4.
The prevalence rate of maternal malnutrition ranges between 10 and 19% worldwide, which is more common among poor populations5.The rate of malnutrition among pregnant women living in low- and middle-income countries (LMIC) is unacceptably high despite extensive global economic growth in recent decades6. Moreover, the results of a study performed in Iran on pregnant women showed that underweight during pregnancy was 7.4%, and the prevalence of LBW in infants of this population of mothers was 5.1%. In addition, 9.7% of underweight women had underweight infants7. Therefore, a large-scale intervention to improve the nutritional status of malnourished pregnant women in order to prevent the birth of LBW infants could have a great impact on the health and productivity of individuals and communities8. In this regard, many countries have support programs for malnourished pregnant women and their babies after birth to improve health indicators. Among these programs, we can point out the Healthy Start program of England9, women, infants and children (WIC) of the United States10, Canada Prenatal Nutrition Program (CPNP)11 and One Full Meal (OFM) program in India12.
Healthy Start is the UK government’s food voucher program for low-income pregnant women and young children. Covered mothers are given weekly vouchers, which they can use for any combination (one or more) of fruit and vegetables, plain cow’s milk, or infant formula, and fresh, dried, and canned beans. In addition, according to this program, eligible families are also entitled to receive the vitamins needed for the mother and baby for free9. A study conducted on the Healthy Start showed that covered mothers reported that food stamps provided to buy foods increased the quantity of their fruit and vegetable intake and improved the quality of their family’s diet13.
The WIC program, whose main purpose is to provide support services for pregnant women, infants and children to minimize the risk of adverse health outcomes at birth, has three main components: nutritional supplements and the provision of food packages, nutrition counseling, and referrals to health and social care services10. Another study reported that for every dollar spent on WIC during pregnancy, savings for Medicaid costs during the first 60 days of life ranged from $1.77 to $3.1314.
The OFM program aims to improve maternal nutrition and health across India by providing hot meals cooked at one location to pregnant and lactating women with other services including daily iron and folic acid (IFA) and calcium administration. Antimalarial medication, gestational weight gain monitoring, newborn weight and height monitoring and health and nutrition counseling have been implemented in poor states since 201315. A review of this program showed that the OFM program could to be used as an effective platform to provide combined services to pregnant women, which can be essential for both fetal growth and maternal health12.
In Iran, in order to improve the health of both pregnant women and their infants and reduce their mortality rates, the nutritional support program for malnourished pregnant and lactating mothers has been implemented for more than 12 years; however, no evaluation of this program has been done so far. Therefore, this study aims to compare the effects of the food basket program and the cash transfer program on the weight gain of pregnant mothers and their infants’ birth weight, the anemia status of mothers, and the growth rate of infants (up to 6 months) of breastfeeding mothers.
Methods
Study design and setting
This is a retrospective field trial study in 2023. Since these two programs were executed one after the other and there was no simultaneous data about them, it was conducted on data collected from 2018 to 2019 for the food basket program and data from 2021 to 2022 for the cash transfer program.
Its main objective was to examine the comparing the effects of the food basket program and the cash transfer program on the weight gain of pregnant mothers and their infants’ birth weight, the anemia status of mothers, and the growth rate of infants (up to 6 months) of breastfeeding mothers, in deprived pregnant and lactating mothers with malnourished in the four provinces of Ardabil, Jiroft, Kerman and Abadan.
The support program for needy pregnant and lactating mothers suffering from malnutrition in the provinces of Iran was started by the Ministry of Health (Community Nutrition Improvement Office), the Alavi Foundation and the Center for Population Youth, Family Health and Schools since 2007. The support program was first started only in rural areas by providing food baskets, and after 4 years, the outskirts of the cities were also included in the program.
According to the instructions of this program, if the pregnant woman met one of the criteria listed in the manual and was in financial need, she entered the program from the fourth month of pregnancy and until the 6th month after giving birth, she received a food basket once every two months, that is, a total of 6 times, three times during pregnancy and three times during breastfeeding, and also this food basket was received by the mother referred to the health center.
The criteria to be covered by the support program included weight less than 45 kg, hemoglobin level less than 11 g/dL, multiple births, unfavorable weight gain during pregnancy based on the table of weight gain according to BMI, body mass index (BMI) less than 18.5 kg/m2 and to be in need. The mother’s neediness in the food basket program was confirmed by the search of the healthcare provider of the Health House. Having chronic diseases does not disqualify individuals from being covered by these support programs. However, mothers who are contraindicated for any reason during pregnancy and meet the eligibility criteria for these programs, as outlined in the guidelines, will not be included in this program.
All women who received food baskets were required to receive a care card and participate in relevant training sessions and follow all the recommendations of health workers.
The contents of the food basket included rice 10 kg, 4 packs of enriched or normal pasta of 700 g each, chickpeas 1 pack 900 g, 2 packs of lentils 900 g, cobs 1 pack 900 g, 4 packs of soybeans 250 g each, pinto beans 1 pack 900 g, dates 2 packs 900 g, oatmeal 1 pack 900 g, 3 one-liter bottles of liquid oil, 7 kg of frozen chicken, 1 package of red beans of 900 g, and 2 molds of 450 g of cheese.
Since 2019, due to management changes, it was decided to change this type of support from providing food baskets to providing cash deposits, but food baskets are still being provided in some areas.
As with the conditions for providing food baskets, in the cash transfer program, eligible mothers who met the above criteria also entered the program from the fourth month of pregnancy and received a cash transfer in the amount of 250 thousand tomans ($21) every two months until 6 months after giving birth for 6 times (three times during pregnancy and three times during breastfeeding) through the credit card issued in the name of the mother. The mother’s neediness was determined by the income decile, if a mother’s income is up to the fifth decile in the information system of Iranians of the Ministry of Welfare, the program covers her.
In addition to providing this food support, mothers were required to participate in nutrition training sessions held by nutrition experts, in which they are taught what foods to buy with this deposit money to meet their nutritional needs. Of course, for how to spend this money, there is no deposit for recipient mothers.
For several decades in Iran’s health care system, free prenatal care is provided to mothers in health centers, and after applying and filing an electronic file in the integrated health system (SIB), all the measures taken for the pregnant mothers were registered in the system every month according to the instructions of the Ministry of Health.
The data for the study that was extracted from the SIB included the mother’s name and surname, age, mother’s education level, head of the household, spouse’s occupation, BMI before pregnancy, mother’s weight gain in the 4th and 8th or 9th months of pregnancy, hemoglobin level in the 4th and 8th month of pregnancy, birth weight and head circumference of the infant at the time of birth, weighing trend and the type of feeding of the infant at 2, 4 and 6 months.
Sample size
The provinces were selected based on the availability of the required information in them and the cities in clusters and based on the presence of mothers covered by the program in comprehensive health service centers or health houses. Covered mothers were included in the study at four provinces of Ardabil, Abadan, Jiroft, and Kerman.
To calculate the sample size, birth weight was used as the most important variable. Based on the following formula, taking into account the minimum difference of 100 g and the standard deviation of 300 g, with alpha equal to 0.05 and beta equal to 0.15, the required sample size was 162 people per group:
In order to consider the possibility of defects in the files, 15% was added to the sample size, and as a result, the final sample size was determined to be at least 185 people per group.
Inclusion criteria included the availability of complete medical records for mothers and their infants at health centers during the specified years, receiving a food basket at least twice during pregnancy and breastfeeding in the food basket program intervention group, and charging the mother’s card at least twice in the pregnancy and breastfeeding intervention group within the cash transfer program. Since the study was retrospective, there were no exclusion criteria.
Sampling of mothers
This support program is implemented in 61 regions of the country to cover pregnant and lactating mothers. We conducted correspondence with all regions to find study samples and asked them to announce the list of mothers covered by this program (intervention group) along with complete information on the mother’s registered care during pregnancy and information on their neonates up to six months of age. Four provinces of Jiroft, Ardabil, Kerman, and Abadan announced a complete list of covered mothers and we selected these regions as the sample for this study. Therefore, the selection of the sampling regions was not random.
Each region has between 60 and 180 health centers and we extracted a list of mothers’ names from all centers covered by each region and included then a certain number of mothers in the program in proportion to the size of the population covered by the health centers.
The number of mothers in the food basket intervention group was 85 in Jiroft, 65 in Ardabil, 46 in Abadan, and 45 in Kerman. The number of mothers in the cash transfer intervention group was 46 in Jiroft, 47 in Ardabil, 47 in Abadan, and 73 in Kerman. These numbers were randomly selected from all mothers covered by the programs and eligible non-supported mothers.
The eligible non-supported group mothers were selected from the same areas who met the criteria for entering the support program and were similar in terms of livelihood and cultural status to the intervention group but were not covered by the program due to the lack of program quotas, proportional to the size of the population covered by the health centers. The number of eligible non-supported group mothers was 109 in Jiroft, 111 in Ardabil, 91 in Abadan and 117 in Kerman.
Mothers in the non-needy group were also selected from the same areas, whose livelihood and cultural status were similar to the intervention group. These mothers did not have any nutritional and economic problems, and the number of this group was proportional to the population covered by the health centers. The number of non-needy group mothers from Jiroft was 107, Ardabil 117, Abadan 90 and Kerman 124.
This study divided mothers in each region into four groups:
-
Food basket group (Intervention group): Qualified mothers who participated in the program and received food baskets.
-
Cash Transfer group (Intervention Group): Eligible mothers who participated in the program and had their credit cards charged.
-
Eligible non-supported group (Control Group): Eligible mothers who, based on the program’s criteria, were not enrolled due to the limited program quotas.
-
Non-needy control: mothers who did not have necessary conditions and only went to comprehensive health service centers or health centers for monthly pregnancy care.
Statistical analysis
The collected data were entered into the computer after checking. For descriptive report, quantitative variables were presented as mean and standard deviation, and qualitative variables were expressed as absolute and relative frequency.
All statistical analysis was performed by using SPSS version 23. Chi-square test was used to determine the significant difference in the frequency of qualitative variables, and ANOVA with Bonferroni post hoc test was used to assess the difference of the mean values in the four study groups. Paired-t test was used to compare the quantitative variables before and after the intervention in each of the investigated groups. Since the maternal hemoglobin level was measured twice and the baby’s weight was measured more than twice during the study, repeated measures ANOVA was used to compare data at multiple times as a multivariate model with fixed and random effects. This procedure analyzes groups of related dependent variables that represent different measurements of the same attribute while adjusting other variables. In a doubly multivariate repeated measures design, the dependent variables represent measurements of more than one variable for the different levels of the within-subjects’ factors. A p-value less than 0.05 was considered significant.
Results
One thousand three hundred and twenty-one pregnant women were included in the four intervention groups: food basket group (n = 241), cash transfer group (n = 213), eligible non-supported group (n = 438), and non-needy control group (n = 439) from the areas covered by four provinces: Kerman, Ardabil, Jiroft, and Abadan. The characteristics of the study participants were presented in Table 1. There was a significant difference between the four groups in terms of education level, and the frequencies of illiteracy in the food basket group and primary education level in the eligible non-supported group were significantly higher than those in the other groups. There was a significant difference among the groups in terms of occupation of the head of household, and higher occupations were reported in the non-needy control group than the other three groups. The frequency of non-male headed households was very small.
The relative frequency of mothers in the four groups of food basket, cash transfer, eligible non-supported, and non-needy control, separated by the investigated regions, is shown in Fig. 1.
Figure 1- Relative frequency of food basket, cash transfer, eligible non-supported, and non-needy control groups in the four investigated medical sciences universities.
The mean and standard deviation of maternal characteristics including age, weight, and BMI before pregnancy in addition to hemoglobin less than 11 g/dL are shown in Table 2. The average BMI before pregnancy in all 4 groups was within the normal range (between 23 and 25 kg/m2). The weight and BMI of the non-needy control group were significantly higher than the other three groups. The frequencies of BMI less than 18.5 kg/m2, weight below 45 kg, and hemoglobin below 11 g/dL in the eligible non-supported group was higher than those in other groups, and the lowest was observed in the non-needy control group (p < 0.001). Three cases of twins were observed in pregnant women receiving food baskets, and one case of triplets was found in the eligible non-supported group.
Table 3 shows the changes in hemoglobin level, the prevalence of anemia and weight gain of the participants in the four groups. The average hemoglobin levels in all four groups were significantly decreased in the 8th month of pregnancy compared to the 4th month of pregnancy, but the decrease was the same in all four groups. The prevalence rate of anemia was significantly increased in all four groups in the 8th month compared to the 4th month of pregnancy, and the increase in the eligible non-supported group was more than that in the other three groups.
The characteristics of anthropometric indices and the infants’ type of feeding in the four groups are shown in Table 4. There was a significant difference among the four groups in birth weight. The head circumference of infants in the non-needy control group was significantly higher than that of the cash transfer and eligible non-sponsored groups. The weight of infants in the eligible non-supported group at 2 months of age was significantly less than that of the other three groups, and it was more in the cash transfer group than the food basket group. In addition, the weight of infants at 4 months in the non-needy control group was significantly higher than that of the other three group (p < 0.001). The lowest frequency of infants born weighing less than 2,500 was found in the non-needy control group and the highest in the eligible non-supported group (p < 0.001).
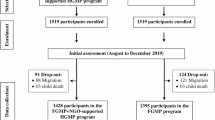
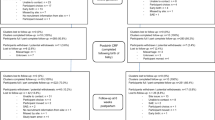
Based on the repeated measures ANOVA analysis as shown in Figs. 2 and 3, the interaction of time and group during the study period on infant weight gain was not significant. In other words, the infant’s weight similarly increased during the study period in different groups, while the changes of maternal hemoglobin levels in different groups were significantly different (p < 0.001). The non-needy control group had the highest increase in the infant weight and mother’s hemoglobin levels in inter-group comparisons. Also, the occupation of head of household was the only socio-economic variable that had a significant effect on both the infant’s weight gain and mother’s hemoglobin level (p < 0.05). Maternal education level was shown to be effective only on hemoglobin changes (p < 0.001).
Figure 2: ANOVA analysis of infant weight at birth, 2, 4, and 6 months adjusted for age, mother’s education, and household head’s occupation (p Time < 0.001, p Group < 0.001, p Time*Group = 0.0.210, Intra-class correlation (ICC) = 0.810).
Figure 3: Repeated Measurement ANOVA analysis for mother’s hemoglobin in the 4th and 8th months of pregnancy adjusted for age, mother’s education and household head’s occupation (p Time = 0.214, p Group < 0.001, p Time*Group = 0.010, ICC = 0.689).
Discussion
The results of this study showed that the distribution of food baskets significantly increased weight in pregnant women and birth weight in infants, while in women who were supported by cash transfer, the prevalence of iron deficiency anemia at the eighth month of pregnancy was less and the weight gain of children in the first 4 months after birth was more favorable. Several studies have investigated the effect of cash transfer on weight gain in pregnant and lactating women and infants, as well as the prevalence rate of anemia in them16,17,18,19.
The weight gain of mothers during the study period before the intervention in the fourth month to the end of the eighth month of pregnancy showed an increasing trend in the average weight gain of women in the food basket, cash transfer and eligible non-supported groups. In addition, by comparing food basket and cash transfer groups, it was observed that the weighting process of women in the food basket group was better than that in the cash transfer group. Moreover, the assessment of mothers who gained less than optimal weight showed that in all groups, except for the non-needy control group, the frequency of mothers with less-than-optimal weight gain significantly decreased after the intervention. By comparing the food basket and cash transfer groups, it was observed that the frequency of mothers with less-than-optimal weight in the food basket group decreased more than the cash transfer group. In this way and based on the findings of this study, food basket intervention can be more effective than cash transfer in increasing the maternal weight gain, although this weight gain is not always desirable and in some cases it may be associated with an increase in the prevalence rate of obesity in mothers, as observed in a study in Guatemala by Leroy et al.17. This study showed that the PROCOMIDA food transfer program led to an increase in BMI after childbirth among women led to an improvement in weight gain in mothers, but considering the prevalence rate of obesity in women in this region, which was not desirable17. Previous studies have shown that the use of cash or voucher transfer with behavior change communication (BCC) in food support programs can help improve nutritional outcomes, without leading to unintended negative consequences, such as increasing women’s BMI and the prevalence rate of obesity in them18,20.
Therefore, the design of food transfers programs and methods of intervention, evaluation and management of the implementation of these programs should be done carefully and based on the conditions of the target group in each area. In cases where women’s weight gain is undesirable, such as in situations where female underweight is high and the prevalence rate of overweight and obesity is low, cash transfers targeting women, and controlling the use of transfers to achieve their goal are important18,21,22,23.
According to the findings of this study, the average hemoglobin levels decreased in all four groups at the eighth month of pregnancy compared to the fourth month of pregnancy, and the prevalence rate of anemia significantly increased. The average hemoglobin level in the cash transfer group was higher than that in the food basket group before the intervention, but its decrease in the eighth month of pregnancy was significantly higher than the food basket group and reached a value lower than the average hemoglobin level in the food basket group in the eighth month. This difference may be related to the effect of hemoglobin at the beginning of the study, not to the intervention. This finding is consistent with the results found by some previous studies. A review of the Tubaramure program - an integrated food-assisted health and nutrition program in Burundi - reported that, despite a decrease in hemoglobin level and a significant increase in anemia from the start of the program to its two-year follow-up, Tubaramure had a significant beneficial effect on mothers who had given birth the three last month’s16. The program followed women and their children in the first 1,000 days of life (from pregnancy to the child’s second birth) and included four interventions to reduce anemia, including the distribution of fortified food, preventive health care like promoting the use of bed nets to prevent malaria. In endemic areas, behavior change strategies were aimed at promoting optimal nutrition and child health and hygiene practices16.
The Tubaramure is a program model that combines food distribution with a package of Maternal and Child Health and Nutrition (MCHN) interventions. This program has been widely used in low- and middle-income countries with the aim of reducing the persistent problems of maternal and child malnutrition intended to highlight the importance of intervention during this critical period to achieve sustainable improvements in maternal and child nutrition24. However, there is little evidence of the effect of this program on reducing the prevalence rate of anemia25.
In contrast to the effects observed in the Tubaramure program, a recent review found that none of the voucher and food transfer programs examined in this study had a significant effect on improving women’s hemoglobin levels or reducing the prevalence rate of anemia18. The review showed that although food transfer programs with enriched foods compared to cash transfer programs might increase women’s blood hemoglobin concentration and lead to a reduction in the prevalence rate of anemia; this may vary based on the type of program and the outcome evaluated18. In any case, there is little evidence about the effectiveness of various nutritional support programs, and the design of programs, training, or the method of controlling the use of these services and changing behavior carried out in some of these programs, may also affect the consequences of the program and their effectiveness.
The findings of the present study showed that the birth weight of the babies among the four groups and the head circumference of the babies in the non-needy control group were significantly different from the cash transfer and eligible non-supported groups. Based on this study, it seems that the food basket intervention may have a greater effect on the birth weight of babies than cash transfer may, but the effect of both interventions on the head circumference of babies at birth is the same.
This shows that the cash transfer method may have more effects on the weight gain of infants during the first 4 months after birth than the food basket method. On the other hand, by examining the interaction of time and group in food basket and cash transfer groups, it seems that the weight changes in the two groups were similar, indicating the same effect of the two interventions of food basket and cash transfer on infant’s weight gain. Few studies have compared the effects of two approaches of food transfer and cash transfer. According to Olney et al., food provision has a greater positive effect on children’s weight-for-height Z-score (WHZ) compared to cash transfer. However, the effectiveness of the approaches may vary based on the type of program and outcome evaluated18.
In any case, it is necessary to have more evidence about the method of transmission, control and use of the service to make the decision to choose the food support approach and how to implement it easier (21). On the other hand, based on previous studies, cash transfer has a long-term positive effect on growth outcomes and mortality rates caused by malnutrition in children aged 0 to 5, especially in vulnerable households26,27,28,29.
In these studies, the strategy of food distribution and transportation has not been investigated. On the other hand, some studies have shown that the combination of these two strategies can be led to better results. Based on the findings of a prospective study performed by Langendorf et al. in rural areas in Nigeria, a combination of food aid and cash transfer has a better preventive effect on moderate acute malnutrition (MAM) than strategies that rely on cash transfer or food transfer alone, had severe acute malnutrition (SAM) and improved weight or mid-upper arm circumference (MUAC)30.
In any case, cash transfer, as a preventive strategy, while strengthening the food security of vulnerable households; if it is combined with the behavior change communication approach, it gives the family enough purchasing power to have a suitable and balanced diet. In addition, cash transfers can help access health services, maintain good health standards, and invest in food production tools for the growth and development of children in families18.
Currently, there is little evidence on the effectiveness of cash transfers combined with behavior change approaches, and more research is necessary to evaluate the effectiveness of these strategies, especially regarding the choice of food support intervention method in different settings. On the other hand, market access is another factor that can be effective in choosing the intervention method. In areas where food is marketed and stackable, cash transfers or vouchers may be as effective as or even more effective than food transfers in achieving nutritional outcomes even. While in an area with poor or unstable market access, the food transfer or food basket method is likely to be more effective18.
Food support is considered as a suitable strategy to maintain or improve the food security of households, and thus prevent acute malnutrition in households involved with food insecurity31. Limited physical access and financial problems are the causes of lack of access to food31.
While food aid is effective on dietary consumption and improves food insecurity, it can free up money spent on providing food to cover other costs such as housing, water, electricity, medicine, and transportation32.
Interventions based on providing food packages or coupons and cash transfers, as food aid, are suitable options for increasing household access to food31. Which method is most appropriate to achieve the best response in household food security is of great importance, and re-evaluating nutritional strategies of support programs will help choose strategies that have better cost-effectiveness. Therefore, it is necessary to examine the value of energy, composition and different packaging in various programs of food transportation in different countries, as well as their control and distribution method, and process evaluation should be included in the studies of the effectiveness of support programs.
This is the first comparative study considering the two support programs of food basket and cash transfer in Iran. The large sample size and wide geographic distribution of these two programs are considered the strong points of the program.
Limitations
The lack of systematic monitoring of the way food packages are consumed or how cash transfer is spent is a limitation of this study. On the other hand, this study may have underrepresented the results due to the brief intervention period. The research was conducted in provinces that had adequate and relevant data, while many provinces were excluded because of insufficient documentation and data recording. The incompleteness of the raw data and the absence of a national database for the food basket program resulted in the loss of significant data across various regions of the country.
Recommendations
Due to the limited resources and the high cost of cash transfers, it is necessary to conduct more studies on the cost-effectiveness of the type of intervention and the method of implementation, as well as the method of systematic control and monitoring of the consumption of the provided food or the cost of cash and behavior control. beneficiaries and results of the program to choose the most feasible option in terms of implementation as well as more effective in terms of improving the nutritional outcomes of vulnerable women and children and sustainable food security of households.
It is advisable that the effects of variables such as maternal age and education, household size, number of children, access to health care during pregnancy or childbirth, geographical region and ethnicity, use of iron supplements, and the method and quantity of their use, which may skew the results of the association between receiving nutritional support and outcomes, be taken into account in future studies.
Conclusion
Nutritional support is a well-known strategy to improve nutritional outcomes in pregnancy, and according to the existing conditions and needs of the society, it is necessary to choose an appropriate approach that is more effective. Interventions based on providing food packages or cash transfers are two food support approaches that can lead to increasing household access to food. In the current study comparing these two intervention methods in the support program for pregnant and lactating women suffering from malnutrition in 4 provinces of Ardabil, Jiroft, Kerman and Abadan in Iran, it was found that the cash transfer method was effective in weighing infants during the first 4 months after birth than the food basket method, while the food basket had a more significant effect on maternal weight gain during pregnancy. Taking the interaction of time and group into account, the two methods had the same effects on infant’s weight gain. Few studies have compared the impacts of different nutrition support approaches, such as providing food, vouchers or cash, or a combination of these, on nutritional improvement outcomes, and limited and sometimes conflicting evidence exists on the impact of these approaches on different nutritional outcomes, particularly for mothers and children. It seems that despite the advice of die-hard supporters of the food basket, who believe that the nutritional needs of pregnant women and their babies are more likely to be met with this method and that cash payments may be used for other non-food expenses, there is no significant difference in the outcome of the two methods in Iran. However, more studies are necessary to choose the most appropriate solution in different populations.
Data availability
“The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.”
Abbreviations
- LBW:
-
low birth weight
- LMIC:
-
low- and middle-income countries
- WIC:
-
women, infants and children
- CPNP:
-
Canada Prenatal Nutrition Program
- OFM:
-
One Full Meal
- IFA:
-
Iron and folic acid
- BMI:
-
Body mass index
- BCC:
-
Behavior change communication
- WHZ:
-
Children’s weight-for-height Z-score
- SAM:
-
Severe acute malnutrition
- MUAC:
-
Mid-upper arm circumference
References
Dolati, S. et al. Pregnancy outcomes in obese women who gave birth during the outbreak of the Covid-19 and before it. Ethiop. J. Reproductive Health, 16(1). (2024).
Gebre, B. et al. Determinants of malnutrition among pregnant and lactating women under humanitarian setting in Ethiopia. BMC Nutr. 4, 1–8 (2018).
Harvey, L. B. & Ricciotti, H. A. Nutrition for a healthy pregnancy. Am. J. Lifestyle Med. 8 (2), 80–87 (2014).
Moran-Lev, H. et al. Nutrition and the use of supplements in women during pregnancy: A cross-sectional survey. FoodNutr. Bull. 40 (2), 231–240 (2019).
Victora, C. G. et al. Revisiting maternal and child undernutrition in low-income and middle-income countries: Variable progress towards an unfinished agenda. Lancet 397 (10282), 1388–1399 (2021).
Habtu, M. et al. Effect of Integrated nutrition-sensitive and nutrition-specific Intervention Package on Maternal Malnutrition among Pregnant Women in Rwanda18p. e13367 (Maternal & Child Nutrition, 2022). 3.
Salem, Z. et al. The prevalence of malnutrition and its association with pregnancy outcome among pregnant women in rafsanjan, Iran, in 2016. J. Occup. Health Epidemiol. 6 (2), 106–113 (2017).
Kuma, M. N. et al. Effect of nutrition interventions before and/or during early pregnancy on low birth weight in Sub-Saharan africa: a systematic review and meta-analysis. FoodNutr. Bull. 43 (3), 351–363 (2022).
Ohly, H. et al. A realist review to explore how low-income pregnant women use food vouchers from the UK’s healthy start programme. BMJ Open. 7 (4), e013731 (2017).
Di Noia, J. et al. Feasibility of a farm-to-WIC intervention. Public Health. Nutr. 22 (18), 3405–3415 (2019).
Mildon, A. et al. Effect on breastfeeding practices of providing in-home lactation support to vulnerable women through the Canada prenatal nutrition program: Protocol for a pre/post intervention study. Int. Breastfeed. J. 16, 1–9 (2021).
Kachwaha, S. et al. Improving maternal nutrition in India through integrated hot-cooked meal programs: a review of implementation evidence. (2021).
McFadden, A. et al. Can food vouchers improve nutrition and reduce health inequalities in low-income mothers and young children: a multi-method evaluation of the experiences of beneficiaries and practitioners of the healthy start programme in England. BMC Public. Health. 14, 1–13 (2014).
Kogan, K. et al. A Quasi-Experimental assessment of the effect of the 2009 WIC food package revisions on breastfeeding outcomes. Nutrients 15 (2), 414 (2023).
Leroy, J. L., Olney, D. & Ruel, M. Tubaramure, a food-assisted integrated health and nutrition program in burundi, increases maternal and child hemoglobin concentrations and reduces anemia: A theory-based cluster-randomized controlled intervention trial. J. Nutr. 146 (8), 1601–1608 (2016).
Leroy, J. L., Olney, D. K. & Ruel, M. T. PROCOMIDA, a food-assisted maternal and child health and nutrition program, contributes to postpartum weight retention in guatemala: A cluster-randomized controlled intervention trial. J. Nutr. 149 (12), 2219–2227 (2019).
Olney, D. K. et al. Social assistance programme impacts on women’s and children’s diets and nutritional status. Matern. Child Nutr. 18 (4), e13378 (2022).
Torres, T. F. et al. A study on the effect of the Brazilian conditional cash transfer program on child nutrition. Int. J. Soc. Econ., (2025).
Olney, D. K. et al. Nutrition-sensitive social protection programs within food systems. (2021).
Iruhiriye, E., Heckert, J., Olney, D. K., Leroy, J. L. & Ruel, M. Tubaramure, a Food-Assisted integrated health and nutrition program, improves maternal health and nutrition knowledge in Burundi. FASEB J. 30, 669–618 (2016).
Leroy, J. L. et al. Tubaramure, a food-assisted maternal and child health and nutrition program in burundi, increased household food security and energy and micronutrient consumption, and maternal and child dietary diversity: A cluster-randomized controlled trial. J. Nutr. 150 (4), 945–957 (2020).
Leroy, J. L., Olney, D. & Ruel, M. Tubaramure, a food-assisted integrated health and nutrition program, reduces child stunting in burundi: A cluster-randomized controlled intervention trial. J. Nutr. 148 (3), 445–452 (2018).
Black, R. E. et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 382 (9890), 427–451 (2013).
Lentz, E. C. & Barrett, C. B. The economics and nutritional impacts of food assistance policies and programs. Food Policy. 42, 151–163 (2013).
Fernald, L. C., Gertler, P. J. & Neufeld, L. M. Role of cash in conditional cash transfer programmes for child health, growth, and development: An analysis of mexico’s oportunidades. Lancet 371 (9615), 828–837 (2008).
Gertler, P. Do conditional cash transfers improve child health? Evidence from PROGRESA′ s control randomized experiment. Am. Econ. Rev. 94 (2), 336–341 (2004).
Paes-Sousa, R., Santos, L. M. P. & Miazaki, É. S. Effects of a conditional cash transfer programme on child nutrition in Brazil. Bull. World Health Organ. 89, 496–503 (2011).
Sridhar, D. & Duffield, A. A Review of the Impact of Cash Transfer Programmes on Child Nutritional Status and some Implications for Save the Children UK Programmes (Save the Children UK, 2006).
Langendorf, C. et al. Preventing acute malnutrition among young children in crises: A prospective intervention study in Niger. PLoS Med. 11 (9), e1001714 (2014).
Doocy, S. et al. Cash-based assistance and the nutrition status of pregnant and lactating women in the Somalia food crisis: A comparison of two transfer modalities. PloS One. 15 (4), e0230989 (2020).
Berkowitz, S. A. et al. I was able to eat what I am supposed to eat--patient reflections on a medically-tailored meal intervention: A qualitative analysis. BMC Endocr. Disorders. 20, 1–11 (2020).
Acknowledgements
In this study, we would like to thank the colleagues in the Nutrition Department of the Deputy Health Department of Kerman, Jiroft, Ardabil and Abadan Universities for their cooperation in data collection.
Funding
Theis’ research was approved and supported by Faculty of Nutrition and Food sciences, Tabriz.
Author information
Authors and Affiliations
Contributions
S .D., A .B., F .M-N. and M. A. designed the study and developed data collection tools. S. D., F. M-N. and M. A. performed material preparation, data collection, and data analysis. S .D., A .B., F. M-N., M. A., and R. K-Z. contributed to developing the study proposal and drafting the manuscript. S .D., A .B., F. M-N. and M. A. wrote the paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was conducted on existing data in the provincial and central departments of community nutrition in primary health care system of Iran according to the guidelines laid down in the Declaration of Helsinki. Because the study was conducted on the available data, it was not possible to obtain informed consent from the participants. All procedures involving research study participants were approved by the research ethics committee of Tabriz University of Medical Sciences. (IR.TBZMED.REC.1401.1078). Considering the retrospective nature of the study, the ethics committee of Tabriz University of Medical Sciences, while approving it, did not consider the consent of the participants necessary.
Consent for publication
Due to retrospective nature of the study Informed consent was waived by the ethics committee of Tabriz University of Medical Sciences - IR.TBZMED.REC.1401.1078”.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Dolati, S., Barzegar, A., Mohammadi-Nasrabadi, F. et al. Comparing the effectiveness of food baskets and cash transfers to support pregnant and lactating mothers in needy suffering from malnutrition in Iran. Sci Rep 15, 25684 (2025). https://doi.org/10.1038/s41598-025-09824-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-09824-z