Abstract
Hepatitis B virus (HBV) infection is a major driver of hepatocellular carcinoma (HCC), yet the mechanisms by which HBV triggers HCC and how it interacts with the immune system remain largely undefined. In this study, 53 immune-related key genes involved in HBV-associated HCC progression were identified. By analyzing the mean C-index of 101 machine learning models, the optimal model—combining stepwise Cox regression (forward) with RSF—was developed to characterize the immune risk index. Patients in the high-risk group exhibited worse survival outcomes and increased infiltration of immunosuppressive cells. Integrating PPI analysis with machine learning, SPP1, GHR, and ESR1 emerged as promising druggable targets, with SPP1 notably overexpressed in tumors and linked to adverse outcomes. ScRNA-seq analysis revealed SPP1 was predominantly expressed in angio-TAMs, which may impair anti-tumor immunity by limiting T and NK cell infiltration. It also involved in tumor progression via angiogenesis and EMT pathways. Drug prediction and molecular docking identified small molecules such as myricetin and mefloquine that can target the aforementioned key immune genes, thereby modulating the immune landscape of HBV-HCC. Repurposing these established drugs represents a novel therapeutic avenue, offering both efficacy and expedited clinical translation for HBV-HCC.
Similar content being viewed by others
Introduction
Hepatocellular carcinoma (HCC), the most common subtype of liver cancer, ranks as the third most prevalent cancer globally1. Hepatitis B virus (HBV) infection is a primary risk factor for HCC2. Due to high recurrence rates, even patients who undergo surgical resection require additional treatments such as chemotherapy and immunotherapy3. However, immune checkpoint blockade (ICB) therapies show limited efficacy in HCC patients despite significant advancements4. Studies have shown that HBV-associated HCC exhibits a significantly immunosuppressive and exhausted tumor microenvironment (TME), which promotes immune escape, tumor progression, and resistance to immunotherapy5,6. Consequently, targeting the immune-suppressive TME in HBV-related HCC holds therapeutic promise.
Long-term HBV infection and liver damage from chronic inflammation contribute to the dysregulation of the immune microenvironment. On the other hand, suppressive immune cells and tumor cells drive the dysfunction of effector cells, further enhancing immunosuppression7. Macrophages, which are widely infiltrated into solid tumors, can be polarized into M1 or M2 states in response to signals from the TME, playing a dual role in the immune response. M1 macrophages are classically activated, while M2 macrophages are alternatively activated8. The balance between pro-inflammatory (M1-like) and anti-inflammatory (M2-like) macrophages determines the immune response within the TME. Therefore, understanding the molecular mechanisms underlying macrophage polarization could lead to the development of new therapeutic strategies.
SPP1 plays a critical role in cancer progression, including epithelial-mesenchymal transition (EMT), immune modulation and chemotherapy resistance9,10. Reports have indicated that SPP1 is aberrantly expressed in various cancers, including colorectal and lung cancer, where its high expression correlates with poor prognosis and enhanced immune suppression11,12. Furthermore, high expression of SPP1 is linked to the polarization of macrophages into the immunosuppressive M2 phenotype13. Thus, small molecule inhibitors targeting SPP1 may hold promise in reversing the immune suppressive phenotype in HBV-HCC, ultimately improving patient prognosis.
In our pursuit of identifying potential drug candidates, we utilized the DSigDB database, a comprehensive resource for associating compounds with their target genes14. Furthermore, molecular docking, renowned for predicting ligand-target interactions at the molecular level, has seen rising prominence in drug discovery15. This approach facilitates the identification of ligands with high binding affinity and favorable interaction characteristics, enabling the prioritization of drug targets for experimental validation and the refinement of drug candidate designs.
In this study, we developed and validated an immune risk index using machine learning algorithms, integrating differentially expressed immune-related genes in HBV-HCC. Our single-cell analysis identified a lower immune score in HBV-HCC and revealed increased infiltration of immunosuppressive SPP1 + angio-macrophages. Additionally, we identified ApoA and SPP1 signaling as key mediators of communication between SPP1 + macrophages and other cells. Our findings provide novel insights into the immune escape mechanisms in HBV-HCC and suggest that effective drug candidates targeting SPP1 may offer new therapeutic avenues for HBV-HCC.
Materials and materials
Data acquisition and identification of HBV-HCC related immune genes
The expression profiles of GSE12124816 (HBV-related HCC: normal = 37, tumor = 70) and TCGA-LIHC17 (HCC: normal = 50, tumor = 370) were retrieved from the GEO and TCGA databases, respectively. Differentially expressed genes (DEGs) from these two datasets were identified using the limma package, with the thresholds set at an adjusted p-value < 0.05 and |log2(fold change, FC)| > 1. To further explore the immune landscape within the HBV-HCC microenvironment, immunity-related genes (IRGs) were sourced from the ImmPort database18 (Supplementary Table S1). The intersecting genes between the IRGs and DEGs from both HBV-HCC datasets were then selected for further analysis. A protein-protein interaction (PPI) network was constructed using the STRING online platform, and key genes within the HBV-HCC disease network were identified using the cytoHubba plugin in Cytoscape. Simultaneously, we downloaded the GSE1452019, GSE7642720, GSE20206921, GSE5509222, GSE4407423 and GSE8314824 expression profiling datasets from the GEO database as validation sets. Additionally, a single-cell RNA sequencing dataset from HBV-related HCC and adjacent liver tissues was acquired from GSE202642 for further investigation. The detailed information of the datasets used in this study were included in Supplementary Table S6.
Construction and validation of the immune risk index based on HBV-HCC related immune genes
Recently, increasing number of prognostic signatures have been developed based on machine learning25,26. The intersection genes identified earlier were used as candidate genes to develop a robust prognostic immune risk index with high predictive accuracy. The TCGA-LIHC datasets served as training cohort, and ICGC-LIRI-JP, GSE14520, GSE76427 and GSE202069 as validation cohorts. A total of 101 combinations were generated using 10 machine learning algorithms, including Lasso, Ridge, stepwise Cox, CoxBoost, RSF, Enet, plsRcox, SuperPC, GBM, and survival-SVM25. For each model, the concordance index (C-index) was calculated across both the training and validation datasets. The model with the highest mean C-index was selected as the most robust and clinically relevant.
The optimal cutoff from the training cohort (determined via the “survminer” R package) was used to stratify both cohorts into high- and low-risk groups. Kaplan-Meier (KM) curve analysis was then performed using the ‘survminer’ R package to evaluate the survival probability in overall survival (OS), disease-free interval (DFI), progression-free interval (PFI), and disease-specific survival (DSS) between the two groups. Finally, ROC curve analysis using the ‘timeROC’ package was performed to evaluate the predictive accuracy of the immune risk index for OS in HBV-HCC patients.
Assessment of the independent prognostic value of the immune risk index and nomogram construction
Univariate and multivariate Cox regression analyses were conducted to evaluate the independent prognostic value of the immune risk index and clinical characteristics. We then developed a nomogram incorporating both the immune risk index and clinical factors to predict survival in HBV-HCC patients. Calibration curves were used to evaluate the nomogram’s predictive performance and determine its utility as an independent prognostic factor.
Exploration of immune status within HBV-HCC tumor microenvironment
To facilitate the exploration of immune status within the HBV-HCC tumor microenvironment, we first employed the ‘estimate’ R package to assess stromal levels, immune cell infiltration, and tumor purity. Additionally, the CIBERSORT algorithm was applied to quantify immune cell infiltration in both high- and low-risk groups. Spearman correlation analysis was then performed to examine the associations among prognostic-related immune genes, the immune risk index, and immune cell infiltration profiles.
Single-cell data processing
Low-quality cells were excluded based on specific criteria, including the presence of fewer than 200 or more than 6000 total detected genes, or a mitochondrial RNA content exceeding 20%. Normalization and dimensionality reduction were performed using the SCTransform, RunPCA, and RunUMAP functions of “Seurat” R package. Furthermore, the cell clusters were then artificially annotated according to classical cell markers. Subsequently, the FindMarkers function was applied to identify differentially expressed genes (DEGs). To further study macrophage subpopulations, we extracted macrophages from the samples and performed dimensionality reduction and clustering. Differential genes for each subpopulation were identified using the FindAllMarkers function. We then performed Gene Set Enrichment Analysis (GSEA) to investigate the enrichment of these genes in the Hallmark gene set, helping to reveal their biological functions. We also performed cell interaction analysis using the R package “CellChat”.
Drugs prediction and molecular Docking
Protein expression profiles of target genes in normal and tumor tissues of HCC were sourced from the HPA database (https://www.proteinatlas.org/). Potential drug candidates were predicted using the DSigDB database on the Enrichr platform (https://maayanlab.cloud/Enrichr/), with selection based on binding scores and reported drug efficacy. The PDB structure was selected based on the following criteria: high resolution (< 2.5 Å), presence of co-crystallized ligands to define the binding site, completeness of the active site residues, and biological relevance to the human homolog. Moreover, we referred to published literature and selected prioritized PDB entries that are functionally validated in previous studies. Protein 3D structures were downloaded from the PDB database, with PDB IDs: 1A22 (GHR), 3DSF (SPP1) and 1A52 (ESR1). And drug 3D structures were downloaded from the PubChem database, with PubChem IDs presented in Supplementary Table S1. Molecular docking was performed using PyMOL (v2.6.0) and AutoDockTools (v1.5.7) to prepare the ligands and proteins. Initially, water molecules were eliminated from both the proteins and ligands, and polar hydrogen atoms were added27. Grid boxes were then centered to cover the structural domains of each protein, enabling free molecular mobility28. Binding strength was assessed by Affinity (kcal/mol), where lower values indicated stronger ligand-receptor binding and finally visualized with PyMOL.
Statistics
All statistical analyses were performed using the R software version 4.3.1. Statistical significance was set at P < 0.05 unless specified otherwise.
Results
Identification of immune related genes involved in the onset and progression of HBV-HCC
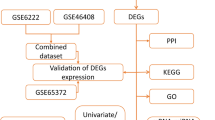
This study was conducted following the procedures shown in flow chart (Supplementary Fig. S1). The volcano plot analysis revealed 3,637 DEGs in tumor samples from the TCGA-LIHC dataset and 683 DEGs from the GSE121248 dataset (Fig. 1A, B, Supplementary Table S2, 3). By intersecting differentially expressed genes (DEGs) from both datasets with immunity-related genes (IRGs) from the ImmPort database, we identified 53 genes that were shared across all three gene sets, which further defined as immune-related genes involved in HBV-HCC progression (Fig. 1C, Supplementary Table S4). To determine their biological roles, GO and KEGG pathway enrichment analyses were performed29,30,31 (Fig. 1D, E). The key IRGs were primarily involved in cytokine-cytokine receptor interactions, chemokine signaling, and positive regulation of the MAPK cascade, which are closely linked to immune responses and tumorigenesis. A PPI network was then generated to further investigate the significance of these IRGs in the HBV-HCC disease network (Fig. 1F).
Identification of immune related genes involved in the onset and progression of HBV-HCC. (A) Volcano plot showing differential genes in TCGA-LIHC. (B) Volcano plot showing differential genes in GSE121248. (C) Intersecting genes of the DEGs of the above two datasets and immune related genes obtained from Immport. (D, E) GO (D) and KEGG (E) enrichment results for intersecting genes29,30,31. (F) PPI network constructed using 53 HBV-HCC related immune genes.
Construction and verification of a prognostic immune index for HBV-HCC and HBV infection
To identify pivotal genes and simplified immune risk index with high diagnostic value, the 53 intersection genes identified earlier were used as candidate genes. In the TCGA-LIHC training cohort, 101 prediction models were built using the LOOCV framework, and the C-index for each model was calculated across both the training and test datasets. Among these, the best-performing model combined stepwise Cox regression (forward) and RSF, yielding the highest average C-index of 0.706 (Fig. 2A). Fourteen prognostic genes were identified via forward stepwise Cox regression, and an immune risk score was constructed using a Random Survival Forest model (ntree = 1000, nodesize = 5, splitrule=‘logrank’) (Fig. 2B). Using the optimal threshold determined from the TCGA training cohort, the two cohorts were classified into high-risk and low-risk groups (Fig. 2C). Notably, higher immune scores were associated with significantly worse overall survival (OS) in the TCGA-LIHC training cohort (Fig. 2D) and external validation cohorts ICGC (Fig. 2E), GSE14520 (Supplementary Fig. S2A), GSE76427 (Supplementary Fig. S2B), and GSE202069 (Supplementary Fig. S2C). Time-dependent ROC curves further demonstrated the predictive sensitivity and specificity of the immune index for OS in the training cohort (Fig. 3A) and validation cohorts (Fig. 3B, Supplementary Fig. S2D–F). Consistent with this, heatmap revealed the high-risk group had elevated SPP1 expression and advanced tumor stages (Fig. 3C). The immune index also showed strong predictive value for DSS, PFI and DFI, with high-risk patients exhibiting poorer outcomes across these parameters (Fig. 3D-F, p < 0.05). To assess the diagnostic accuracy of the prognostic immune index in predicting the disease, ROC analyses were conducted and the results showed that immune index effectively distinguished between HBV-HCC (Supplementary Fig. S2G, H), HBV (Supplementary Fig. S2I) infection patients and their corresponding controls (AUC > 0.65).
Integrated machine learning framework develops immune risk index based on HBV-HCC related immune genes for HBV-HCC. (A) 101 different combinations of machine learning algorithms and each model’s c-index were calculated for training TCGA-LIHC and test ICGC-LIRI-JP datasets. (B) The number of trees for determining with minimal error and the importance of the 14 most valuable HBV-HCC related immune genes based on the RSF algorithm. (C) The optimal cutoff of training TCGA cohort. (D, E) Kaplan-Meier survival curve of OS between high- and low-risk group in the TCGA-LIHC (D) and ICGC-LIRI-JP datasets (E).
Validation the predictive performance of the immune risk index. (A, B) ROC curves of 1-year, 3-year, and 5-year OS in the training TCGA-LIHC (A) and test ICGC-LIRI-JP datasets (B). (C) Heatmap is presented to display the relationship of immune risk groups and clinical features, as well as the expression of the 14 most valuable HBV-HCC related immune genes in patients with HCC. (D-F) Kaplan-Meier survival curve predicted the survival probability for DSS (D), PFI (E) and DFI (F).
Establishment and validation of a nomogram combined immune index and clinical characteristics
To evaluate whether the immune index serves as an independent prognostic factor for HBV-HCC, we performed both univariate and multivariate Cox regression analyses using the TCGA-LIHC dataset. Our results revealed that the immune risk score is an independent prognostic factor in both analyses (HR > 1, p < 0.05), highlighting its strong prognostic value in HBV-HCC patients (Fig. 4A, B). To enhance the clinical utility and diagnostic accuracy, we developed a nomogram that integrates the immune risk score with clinical characteristics (Fig. 4C). The calibration curves indicated well consistency between the nomogram’s predicted outcomes and the actual observations (Fig. 4D).
Independent Clinical predictive value of the immune risk index. (A, B) Forest plot of univariable (A) and multivariable (B) Cox regression results for immune risk index and clinical parameters. (C) Nomogram to predict 1-, 3-, and 5-year survival. (D) Nomogram calibration curves for 1-, 3-, and 5-year OS. (E-G) Stromal (E), Estimate (F) and immune (G) score in the two immune risk groups.
Differentiating immune characteristics based on immune index
The immune infiltration status for different immune risk subgroups was assessed using the ESTIMATE algorithm. Notably, the high-risk group displayed significantly lower stromal (Fig. 4E), ESTIMATE (Fig. 4F), and immune scores (Fig. 4G). To further investigate differences in immune cell infiltration between high- and low-risk groups, we quantified the immune cell composition of each sample using the CIBERSORT algorithm. We observed that the high-risk group had a higher infiltration of M0 and M2 macrophages, but a lower presence of CD8 T cells (Fig. 5A). In addition, the immune score was positively correlated with pro-tumor M0 and M2 macrophages, and negatively correlated with anti-tumor M1 macrophages (Fig. 5B). Moreover, samples with higher levels of M2 macrophages exhibited lower T cell infiltration (p < 0.05, R = −0.8) (Fig. 5C). The comparison of immune risk scores revealed lower scores in the responder group, which further supports the notion that the low-risk group may be more responsive to immunotherapy (Fig. 5D). Immune checkpoint genes such as CD274, PDCD1LG2, BTLA, and CD96 were expressed at significantly lower levels in the high-risk group, indicating a poorer response to immune checkpoint inhibitors (ICI) (Fig. 5E). Furthermore, we found that 14 prognostic related IRGs included in the immune index were positively associated with the infiltration of immunosuppressive M2 macrophages (Fig. 5F).
The immune landscape associated with immune index score in HBV-HCC. (A) The abundance of immune infiltrated cell between high- and low-risk groups, quantified by the CIBESORT algorithm. (B) Correlation analysis between TME infiltrated cells and immune index score. (C) The correlation between the T cell proportion and M2 macrophages proportion. (D) Box plot illustrating the differences in estimated risk scores between non-responders and responders in the GSE202069 cohort. (E) The expression of immune checkpoints in high- and low-risk groups. (F) The correlation between the expression of the 14 key IRGs and immune cell abundance.
Heterogeneity of immune index scores in single-cell dataset
After conducting quality control and removing doublets, we opting for a resolution of 0.2 to partition all cells into 12 distinct clusters (Fig. 6A). Subsequently, we manually annotated 9 cell types based on established literature (Fig. 6B, C). Differentially expressed genes between HBV-HCC and normal tissues were also explored (Fig. 6D), and up-regulated DEGs in HBV-HCC exhibited enriched activity in MYC-targets, G2M checkpoint, mTORC1 pathways indicating a hyperproliferative state (Fig. 6E). Interestingly, cells from tumor tissues generally exhibit lower immune scores than those from normal tissues, suggesting that immunosuppression is prevalent in HBV-HCC (Fig. 6F, G).
Heterogeneity of immune index scores in single-cell dataset. (A) UMAP distribution of 12 clusters at a resolution of 0.2. (B) Expression of top markers corresponding to the 12 cell clusters. (C) UMAP distribution of 9 annotated cell types. (D) Volcano plot presented differential genes between HBV-HCC and normal tissues. (E) Bar chart displaying the up and down regulated hallmarker pathways in HBV-HCC. (F) Box plot of immune index scores of samples derived from HBV-HCC and normal tissues. (G) Box plot of immune index scores of different cells derived from HBV-HCC and normal tissues. (H, I) SPP1 expression levels in 9 annotated cell types.
SPP1 macrophages drive the formation of an immunosuppressive microenvironment
SPP1, identified as the most significant gene in the immune index score, is primarily expressed in macrophages (Fig. 6H, I). To further explore macrophage heterogeneity, we isolated the macrophage and re-clustered it into 5 subclusters using a resolution of 0.1 (Fig. 7A). Referring to the study on macrophage diversity by Ma, Ruo-Yu et al.32 and top differential marker genes (Fig. 7B), we annotated the five macrophage subtypes (Fig. 7C) and characterized their functional properties (Fig. 7E). SPP1 is predominantly expressed in angio-TAMs, which show higher levels of infiltration in HBV-HCC tissues compared to normal tissues (Fig. 7D). Functional enrichment analysis revealed that the SPP1⁺ angio-TAMs exhibited enhanced metastatic potential and immune suppressive characteristics, including activation of inflammatory response pathways, NF-κB signaling, and apoptotic regulation (Fig. 7E). Moreover, SPP1 + angio-TAM infiltration was negatively correlated with T and NK cell infiltration, but positively correlated with epithelial/cancer cell abundance (Fig. 7F). Patients with higher infiltration of SPP1 + angio-TAMs showed significantly worse overall survival, further supporting the prognostic relevance of SPP1 expression (Fig. 7G, H). This finding suggests that the increased infiltration of SPP1 + TAMs likely contribute to shaping an immunosuppressive microenvironment and promoting tumorigenesis in HBV-HCC.
Functional analysis of macrophage subsets. (A) Umap showed the distribution of macrophages subclusters. (B) Top5 marker genes of macrophages subclusters. (C). Annotated macrophages types based on top-ranked marker genes. (D) Proportion of main macrophages subtypes in tumor and normal tissue. (E) Hallmarker pathway enriched in different macrophages subsets. (F) Correlation analysis between angio-TAM infiltration and other immune cell populations. (G, H) Kaplan–Meier survival curves among patients with high and low Angio-TAM infiltration in the TCGA-LIHC and GSE14520 cohorts.
Cell-cell communication network between macrophage subgroups and other cells
Cell-cell communication is intricate and plays a pivotal role in HBV-HCC pathogenesis. Compared with the normal group, the HBV-HCC group exhibited more active intercellular communication (Fig. 8A), particularly with increased signaling interactions between SPP1⁺ angio-TAMs and other cell types (Fig. 8B). Among these interactions, the SPP1 and ApoA signaling pathways contributed the most to the overall communication strength of SPP1⁺ angio-TAMs (Fig. 8B, C). Therefore, we further focused on comparing SPP1 and ApoA signaling between HBV-HCC and normal tissues. We observed that in HBV-HCC tissues, SPP1 signaling was primarily transmitted from angio-TAMs to other cell types, whereas in normal tissues, it was mainly mediated by infla-TAMs (Fig. 8D). Additionally, ApoA signaling from epithelial/tumor cells to SPP1⁺ angio-TAMs was uniquely present in tumor tissues (Fig. 8E, F).
Cell-cell Communications analysis based on HBV-HCC single-cell RNA-sequencing. (A) The number and strength of cell interaction mediated by individual. signal pathways in normal and HBV-HCC groups. (B) Circle plots illustrate the changes in the number and strength of intercellular communications. Red indicates increased signaling in HBV-HCC compared to the normal group, while blue represents decreased signaling. (C) Heatmaps displayed the overall (both outgoing and incoming) signal flows of each cell population. (D) SPP1 signal pathway in normal and HBV-HCC groups. (E) ApoA signal pathway in normal and HBV-HCC groups. (F) Bubble map of cell–cell communication mediated by individual signaling axes, with the horizontal axis showing the cell class that initiates and receives the signal, and the vertical axis showing receptor-ligand pairs of the signaling pathway.
Identification of candidate drugs for the treatment of HBV-HCC based on the hub genes
Combining machine learning-selected prognostic immune-related genes (IRGs) with hub genes from the PPI network, we identified four promising druggable targets: SPP1, ESR1, GHR, and IL33. Among these, SPP1 was a risk factor, showing high expression in tumors, while ESR1, GHR, and IL33 were protective factors, exhibiting lower expression in the tumor microenvironment (Fig. 9A, B). To identify potential drug candidates, we used the DSigDB database on the Enrichr website to investigate drugs that target these genes (Supplementary Table S1). Following this, we performed molecular docking analysis to assess the binding strength between the candidate drugs and the four core target genes. Mefloquine (Fig. 9C), myricetin (Fig. 9D), withaferin (Fig. 9E), estramustine (Fig. 9F), formononetin (Fig. 9G) and apigenin (Fig. 9H) exhibited binding energies lower than − 5 kcal/mol, indicating strong binding affinities to their corresponding targets (Supplementary Table S5). Visible hydrogen bonding and strong electrostatic interactions enable each medication candidate to bind to its protein target.
Small molecule drug prediction and molecular docking verification. (A) Forest plot of univariable Cox regression results for the 14 key IRGs. (B) Immunohistochemical analysis of promising targets in HCC tumor and corresponding adjacent normal tissues. (C-H) Visualization of docking models using PyMOL (v2.6.0).
Discussion
Hepatocellular carcinoma (HCC) accounts for nearly 90% of primary liver cancers, with hepatitis B virus (HBV) infection being the predominant risk factor33,34. Chronic HBV infection plays a critical role in shaping a suppressive immune microenvironment, which facilitates tumor escape and accelerates tumor progression5. However, the specific molecular mechanisms underlying the formation of an immunosuppressive microenvironment in HBV-related HCC are yet to be fully elucidated.
More specifically, HBV infection drives the recruitment and accumulation of a large number of immunosuppressive cells, which significantly impair antitumor immune responses and contribute to a poor prognosis35. Specifically, we observed reduced infiltration of cytotoxic T lymphocytes, such as B cells, CD4 + T cells, and CD8 + T cells, which are essential for directly attacking and eliminating tumor cells36,37. In contrast, M2 macrophages, which promote immune suppression, were more abundant in the high-risk group. This imbalance between cytotoxic and immunosuppressive cells likely fosters an immunosuppressive tumor microenvironment, promoting tumor growth, metastasis, and resistance to therapies38,39. Moreover, single-cell RNA-seq analysis of HBV-HCC revealed a lower immune index in tumor tissues and downregulation of immune response pathways, reflecting the immunosuppressive landscape induced by HBV infection in HCC.
In this study, we identified hub genes involved in the pathogenesis of HBV-related HCC and immune regulation, constructing an immune index based on immune-related genes (IRGs) such as SPP1, ESR1, and GHR. We also observed that the abnormal expression patterns of these immune genes altered immune cell infiltration, which in turn mediated poor prognosis of HCC. SPP1 has been reported to be closely associated with tumorigenesis in various cancers, mediating tumor invasion, metastasis, and poor prognosis40,41,42. The risk gene SPP1, identified in our earlier transcriptomic analysis, was predominantly expressed in the angiogenesis-associated macrophage subpopulation (termed angio-TAMs), suggesting a potential role in tumor progression via promotion of angiogenesis and metastasis. SPP1⁺ angio-TAMs may impair anti-tumor immunity by limiting T and NK cell infiltration into the tumor microenvironment. In the HBV-HCC microenvironment, angio-TAMs exhibit significantly more active intercellular communication with other cell types, characterized by enhanced SPP1 and ApoE signaling interactions, which may promote tumor progression by fostering an immunosuppressive microenvironment, enhancing angiogenesis, and supporting tumor cell survival, invasion, and metastasis. ESR1 and GHR act as protective genes in HCC but are frequently downregulated through diverse mechanisms, involving epigenetics, transcriptional dynamics, hormone signaling imbalance, and microenvironmental factors. ESR1 DNA methylation increases in a time-dependent manner during HBV infection43with hypermethylation of the promoter region serving as a key mechanism for its downregulation44. Moreover, emerging evidence suggests that specific miRNAs suppress ESR1 or GHR expression by directly targeting their mRNAs for degradation or translational repression45.
To further investigate potential therapeutic options, we utilized the DSigDB database to predict small-molecule drugs targeting these key signaling axes. Molecular docking was then performed to assess the binding affinity between the compounds and their targets, where significant binding energy was considered effective. Two promising candidates, mefloquine and myricetin, were identified as potential drugs for reversing the immunosuppressive microenvironment and improving the prognosis of HBV-related HCC. Mefloquine, an existing drug with anticancer potential, has shown promise in enhancing the efficacy of PD-1 immunotherapy through ferroptosis induction46,47. Myricetin, which has been reported to inhibit HCC progression by inducing autophagy and reversing epithelial-mesenchymal transition48,49. However, the mechanism by which it reverses the immune-suppressive microenvironment in HBV-HCC remains unexplored. Discovering new applications for well-established, safe, and approved drugs significantly reduces the risk of failure due to adverse reactions. This approach accelerates the transition from preclinical findings to clinical research and eventual therapeutic application.
Conclusions
Our research stands out for its comprehensive approach to uncovering the immune mechanisms underlying HBV-HCC tumor progression. Through machine learning algorithms, we constructed an immune risk index model capable of effectively distinguishing immune status and prognosis. Single-cell analysis elucidates the mechanisms underlying the formation of the immunosuppressive microenvironment. Finally, targeting the immune-related oncogenic targets SPP1, GHR, and ESR1, we screened potential small molecules including myricetin, mefloquine, and withaferin. Molecular docking further enabled us to assess the binding affinity and interaction modes between the ligands and their respective targets.
Data availability
The bulk RNA-Seq data are available in the GEO database GSE121248, GSE14520, GSE76427, GSE202069, GSE55092, GSE44074 and GSE83148 (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi? acc=GSE121248) and TCGA-LIHC (https://www.cancer.gov/ccg/research/genome-sequencing/tcga). The scRNA-Seq data are available in the GEO database, GSE202642 (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi). Immunity-related genes (IRGs) were sourced from the ImmPort database 16. Further inquiries can be directed to the corresponding author.
References
Liu, Y. et al. Identification of a tumour immune barrier in the HCC microenvironment that determines the efficacy of immunotherapy. J. Hepatol. 78, 770–782. https://doi.org/10.1016/j.jhep.2023.01.011 (2023).
Yang, Y. et al. O-GlcNAcylation of YTHDF2 promotes HBV-related hepatocellular carcinoma progression in an N(6)-methyladenosine-dependent manner. Signal. Transduct. Target. Therapy. 8 https://doi.org/10.1038/s41392-023-01316-8 (2023).
Kudo, M. et al. Lenvatinib versus Sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet (London England). 391, 1163–1173. https://doi.org/10.1016/s0140-6736(18)30207-1 (2018).
Finn, R. S. et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N. Engl. J. Med. 382, 1894–1905. https://doi.org/10.1056/NEJMoa1915745 (2020).
Lim, C. J. et al. Multidimensional analyses reveal distinct immune microenvironment in hepatitis B virus-related hepatocellular carcinoma. Gut 68, 916–927. https://doi.org/10.1136/gutjnl-2018-316510 (2019).
Ho, D. W. et al. Single-cell RNA sequencing shows the immunosuppressive landscape and tumor heterogeneity of HBV-associated hepatocellular carcinoma. Nat. Commun. 12, 3684. https://doi.org/10.1038/s41467-021-24010-1 (2021).
Yin, D. et al. Novel insights into HBV-hepatocellular carcinoma at single-cell sequencing. 2, e60, https://doi.org/10.1002/mog2.60 (2023).
Toledo, B. et al. Deciphering the performance of macrophages in tumour microenvironment: a call for precision immunotherapy. J. Hematol. Oncol. 17 https://doi.org/10.1186/s13045-024-01559-0 (2024).
Kretschmer, C. et al. Identification of early molecular markers for breast cancer. Mol. Cancer. 10 https://doi.org/10.1186/1476-4598-10-15 (2011).
Lamort, A. S., Giopanou, I., Psallidas, I. & Stathopoulos, G. T. Osteopontin as a link between inflammation and cancer: the thorax in the spotlight. Cells 8 https://doi.org/10.3390/cells8080815 (2019).
Yu, S., Chen, M., Xu, L., Mao, E. & Sun, S. A senescence-based prognostic gene signature for colorectal cancer and identification of the role of SPP1-positive macrophages in tumor senescence. Front. Immunol. 14, 1175490. https://doi.org/10.3389/fimmu.2023.1175490 (2023).
Matsubara, E. et al. The significance of SPP1 in lung cancers and its impact as a marker for protumor Tumor-Associated macrophages. Cancers 15 https://doi.org/10.3390/cancers15082250 (2023).
Szulzewsky, F. et al. Glioma-associated microglia/macrophages display an expression profile different from M1 and M2 polarization and highly express Gpnmb and Spp1. PLoS One. 10, e0116644. https://doi.org/10.1371/journal.pone.0116644 (2015).
Yoo, M. et al. DSigDB: drug signatures database for gene set analysis. Bioinformatics 31, 3069–3071. https://doi.org/10.1093/bioinformatics/btv313 (2015).
Pinzi, L. & Rastelli, G. Molecular docking: shifting paradigms in drug discovery. Int. J. Mol. Sci. 20, 4331. https://doi.org/10.3390/ijms20184331 (2019).
Wang, S. M., Ooi, L. L. P. J. & Hui, K. M. Identification and validation of a novel gene signature associated Wit h the recurrence of human hepatocellular carcinoma. Clinical cancer Research: Official J. Am. Associa Tion Cancer Research 13, 6275–6283, https://doi.org/10.1158/1078-0432.CCR-06-2236 (2007).
Chang, K. et al. The Cancer genome atlas Pan-Cancer analysis project. Nat. Genet. 45, 1113–1120. https://doi.org/10.1038/ng.2764 (2013).
Bhattacharya, S. et al. ImmPort, toward repurposing of open access immunological assay data for translational and clinical research. Sci. Data. 5, 180015. https://doi.org/10.1038/sdata.2018.15 (2018).
Roessler, S. et al. A unique metastasis gene signature enables prediction of tumor relapse in early-stage hepatocellular carcinoma patients. Cancer Research 70, 10202–10212, https://doi.org/10.1158/0008-5472.CAN-10-2607 (2010).
Grinchuk, O. V. et al. Tumor-adjacent tissue co-expression profile analysis reveals pro-oncog enic ribosomal gene signature for prognosis of resectable hepatocellul ar carcinoma. Molecular Oncology 12, 89–113, https://doi.org/10.1002/1878-0261.12153 (2018).
Li, B., Cao, Y., Li, Y., Cheng, C. & Yu, D. Letter to the editor: the inflamed subclass predicts immunotherapy res ponse - external validations. Gut, gutjnl-2022-328130, https://doi.org/10.1136/gutjnl-2022-328130 (2023).
Melis, M. et al. Viral expression and molecular profiling in liver tissue versus microd issected hepatocytes in hepatitis B virus-associated hepatocellular Ca rcinoma. Journal Translational Medicine 12, 230, https://doi.org/10.1186/s12967-014-0230-1 (2014).
Ueda, T. et al. Gene expression profiling of Hepatitis B- and Hepatitis C-related Hepa Tocellular carcinoma using graphical Gaussian modeling. Genomics 101, 238–248, https://doi.org/10.1016/j.ygeno.2013.02.007 (2014).
Zhou, W. et al. Predictive model for inflammation grades of chronic hepatitis B: large -scale analysis of clinical parameters and gene expressions. Liver Int 37, 1632–1641, https://doi.org/10.1111/liv.13427 (2017).
Liu, Z. et al. Machine learning-based integration develops an immune-derived LncRNA signature for improving outcomes in colorectal cancer. Nat. Commun. 13, 816. https://doi.org/10.1038/s41467-022-28421-6 (2022).
Hong, W. et al. Deciphering the immune modulation through deep transcriptomic profiling and therapeutic implications of DNA damage repair pattern in hepatocellular carcinoma. Cancer Lett. 582, 216594. https://doi.org/10.1016/j.canlet.2023.216594 (2024).
Zhu, Y. et al. Comprehensive bioinformatics and experimental analysis of SH3PXD2B reveals its carcinogenic effect in gastric carcinoma. Life Sci. 326, 121792. https://doi.org/10.1016/j.lfs.2023.121792 (2023).
Cao, Y., Yang, Y., Hu, Q. & Wei, G. Identification of potential drug targets for rheumatoid arthritis from genetic insights: a Mendelian randomization study. J. Translational Med. 21 https://doi.org/10.1186/s12967-023-04474-z (2023).
Kanehisa, M., Furumichi, M., Sato, Y., Matsuura, Y. & Ishiguro-Watanabe, M. KEGG: biological systems database as a model of the real world. Nucleic Acids Res. 53, D672–d677. https://doi.org/10.1093/nar/gkae909 (2025).
Kanehisa, M. Toward Understanding the origin and evolution of cellular organisms. Protein Science: Publication Protein Soc. 28, 1947–1951. https://doi.org/10.1002/pro.3715 (2019).
Kanehisa, M. & Goto, S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 28, 27–30. https://doi.org/10.1093/nar/28.1.27 (2000).
Ma, R. Y., Black, A. & Qian, B. Z. Macrophage diversity in cancer revisited in the era of single-cell omics. Trends Immunol. 43, 546–563. https://doi.org/10.1016/j.it.2022.04.008 (2022).
Gao, Y. et al. Intratumoral stem-like CCR4 + regulatory T cells orchestrate the immunosuppressive microenvironment in HCC associated with hepatitis B. J. Hepatol. 76, 148–159. https://doi.org/10.1016/j.jhep.2021.08.029 (2022).
Péneau, C. et al. Hepatitis B virus integrations promote local and distant oncogenic driver alterations in hepatocellular carcinoma. Gut 71, 616–626. https://doi.org/10.1136/gutjnl-2020-323153 (2022).
Yang, P., Markowitz, G. J. & Wang, X. F. The hepatitis B virus-associated tumor microenvironment in hepatocellular carcinoma. Natl. Sci. Rev. 1, 396–412. https://doi.org/10.1093/nsr/nwu038 (2014).
Oh, D. Y. & Fong, L. Cytotoxic CD4(+) T cells in cancer: expanding the immune effector toolbox. Immunity 54, 2701–2711. https://doi.org/10.1016/j.immuni.2021.11.015 (2021).
Malyshkina, A., Brüggemann, A., Paschen, A. & Dittmer, U. Cytotoxic CD4(+) T cells in chronic viral infections and cancer. Front. Immunol. 14, 1271236. https://doi.org/10.3389/fimmu.2023.1271236 (2023).
Wang, K. et al. Identification of differentially expressed genes in non-small cell lung cancer. Aging 11, 11170–11185. https://doi.org/10.18632/aging.102521 (2019).
Lawal, B. et al. Multi-Omics data analysis of gene expressions and alterations, Cancer-Associated fibroblast and immune infiltrations, reveals the Onco-Immune prognostic relevance of STAT3/CDK2/4/6 in human malignancies. Cancers 13 https://doi.org/10.3390/cancers13050954 (2021).
Yi, X. et al. SPP1 facilitates cell migration and invasion by targeting COL11A1 in lung adenocarcinoma. Cancer Cell Int. 22 https://doi.org/10.1186/s12935-022-02749-x (2022).
Zhang, Z. et al. SPP1 could be an immunological and prognostic biomarker: from pan-cancer comprehensive analysis to osteosarcoma validation. FASEB Journal: Official Publication Federation Am. Soc. Experimental Biology. 38, e23783. https://doi.org/10.1096/fj.202400622RR (2024).
Zeng, B., Zhou, M., Wu, H. & Xiong, Z. SPP1 promotes ovarian cancer progression via integrin β1/FAK/AKT signaling pathway. OncoTargets Therapy. 11, 1333–1343. https://doi.org/10.2147/ott.S154215 (2018).
Kim, M. H., Kang, S. G., Park, J. H., Yanagisawa, M. & Kim, C. H. Short-Chain fatty acids activate GPR41 and GPR43 on intestinal epithelial cells to promote inflammatory responses in mice. Gastroenterology 145, 396–406e310. https://doi.org/10.1053/j.gastro.2013.04.056 (2013).
Hishida, M. et al. Estrogen receptor 1 gene as a tumor suppressor gene in hepatocellular carcinoma detected by triple-combination array analysis. Int. J. Oncol. 43, 88–94. https://doi.org/10.3892/ijo.2013.1951 (2013).
Ma, F. et al. miR-148a suppresses Estrogen-induced viability and migration of breast cancer cells via Inhibition of Estrogen receptor α expression. Experimental Therapeutic Med. 13, 2515–2522. https://doi.org/10.3892/etm.2017.4255 (2017).
Mudassar, F., Shen, H., O’Neill, G. & Hau, E. Targeting tumor hypoxia and mitochondrial metabolism with anti-parasitic drugs to improve radiation response in high-grade gliomas. J. Experimental Clin. cancer Research: CR. 39, 208. https://doi.org/10.1186/s13046-020-01724-6 (2020).
Tao, Q. et al. Mefloquine enhances the efficacy of anti-PD-1 immunotherapy via IFN-γ-STAT1-IRF1-LPCAT3-induced ferroptosis in tumors. J. Immunother. Cancer. 12 https://doi.org/10.1136/jitc-2023-008554 (2024).
Yang, W. et al. Myricetin induces autophagy and cell cycle arrest of HCC by inhibiting MARCH1-Regulated Stat3 and p38 MAPK signaling pathways. Front. Pharmacol. 12, 709526. https://doi.org/10.3389/fphar.2021.709526 (2021).
Wang, M. et al. Myricetin reverses epithelial-endothelial transition and inhibits vasculogenic mimicry and angiogenesis of hepatocellular carcinoma by directly targeting PAR1. Phytother. Res. 36, 1807–1821. https://doi.org/10.1002/ptr.7427 (2022).
Funding
This work was supported by 1.3.5 project for disciplines of excellence-Clinical Research Incubation Project, West China Hospital, Sichuan University (2021HXFH001); 1.3.5 project for Artificial Intelligence West China Hospital, Sichuan University (ZYAI24030); China Telecom Sichuan Company Biliary Tract Tumor Big Data Platform and Application Phase I R&D Project (312230752); National Natural Science Foundation of China for Young Scientists Fund (82203650, 82203782); Sichuan Natural Science Foundation (2024NSFSC0742, 2024NSFSC1949); Sichuan Science and Technology Program (2024YFFK0384, 2024YFFK0385); Science and Technology project of the Health planning committee of Sichuan (24QNMP031); Sichuan University-Sui Ning School-local Cooperation project (2022CDSN-18); the Postdoctor Research Fund of West China Hospital, Sichuan University (2024HXBH134); (Qilu) Clinical Research of Sichuan Anticancer Association (XH2023-032; XH2023-502); National Natural Science Foundation of China (62472069).
Author information
Authors and Affiliations
Contributions
Conceptualization, Fuyu Li, Haijie Hu, Antony Stalin and Yanjie Zhong; resources, Yanjie Zhong; methodology, Yanjie Zhong; software, Yushi Dai; formal analysis, Yanjie Zhong, Zhiqiang He and Ruiqi Zou; validation, Siqi Yang and Aoqiang Zhai; data curation, Yushi Dai; supervision, Antony Stalin, Fuyu Li and Haijie Hu; writing-original draft, Yanjie Zhong; writing-review and editing, Antony Stalin, Fuyu Li and Haijie Hu.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The data utilized in this study is exclusively obtained from publicly available sources, eliminating the need for ethical scrutiny.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhong, Y., Stalin, A., Dai, Y. et al. Integrating bulk and single cell sequencing data to identify prognostic biomarkers and drug candidates in HBV associated hepatocellular carcinoma. Sci Rep 15, 26038 (2025). https://doi.org/10.1038/s41598-025-10876-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-10876-4
Keywords
This article is cited by
-
Integrated Multi-Omics Analysis Reveals Cytokine Network Dynamics and Prognostic Signatures in Hepatitis B Virus-Associated Hepatocellular Carcinoma
Applied Biochemistry and Biotechnology (2026)