Abstract
This multicenter retrospective study analyzed 336 patients (236 adults, 100 children) who underwent liver transplantation (LT) for acute liver failure (ALF) between 2002 and 2019 across 14 centers in Türkiye. The aim was to evaluate pretransplant factors influencing short-term posttransplant survival. Median MELD and PELD scores were 31 and 30, respectively. The most common ALF etiologies were viral, indeterminate, and drug-induced causes. Living donor liver transplantation (LDLT) was more common in children (86.0%) than adults (57.2%). Mean posttransplant survival was 166±9 months in children and 117±6 months in adults. In adults, LDLT significantly improved survival compared to deceased donor LT (DDLT), with survival of 135 vs. 89 months (p=0.0012). Although pediatric LDLT recipients had longer mean survival than DDLT recipients (167 vs. 132 months), this difference was not statistically significant (p=0.5959). Three-month mortality was associated with low albumin and grade 4 hepatic encephalopathy (HE) in children. In adults, independent predictors of early mortality included DDLT, serum sodium >140 mEq/L, MELD >35, pH <7.3, and grade 4 HE. Our data suggest that LDLT may offer a survival advantage, particularly in adults with ALF. Identifying pretransplant risk factors is essential for improving early outcomes and guiding clinical decision-making.
Similar content being viewed by others
Introduction
Acute liver failure (ALF) is a rare, devastating condition characterized by acute severe liver injury, coagulopathy, and hepatic encephalopathy (HE) in patients with no known preexisting liver disease. Estimating the true burden of ALF is difficult due to its rarity, lack of comprehensive registries or population-based surveillance programs, and heterogeneity in the current ALF definitions1. It is thought to affect about 2000 persons per year in the United States2, while there is virtually no available data in Europe3. Significant geographical variations have been observed in the etiology, prognosis, and evolution of ALF3,4. Drug-induced liver injury (DILI) is the most common etiology in Western countries, whereas hepatotropic viruses, such as hepatitis A (HAV), hepatitis B (HBV), and hepatitis E viruses, are the leading causes of ALF in developing countries3,4,5.
ALF has a poor prognosis and a high short-term mortality rate. Spontaneous recovery is expected in 10–40% of patients6. The mortality rate of waiting-list patients ranges from 10 to 70%7,8. Liver transplantation (LT) is an effective treatment with favorable short-term survival rates, ranging from 68 to 84%9,10. The etiology of ALF and the availability of graft organs affect posttransplant outcomes.
Each country and center may have different allocation systems and policies for LT in ALF, although ALF patients have priority access to organs in most countries. Currently, Türkiye has one of the highest numbers of living donor liver transplantation (LDLT) in the world11. In contrast, a recent study reviewing the UNOS data has revealed LDLT constitutes 3.6% of all liver transplants for ALF12. In Türkiye, the experience of transplant centers and the annual number of LTs vary substantially. Considering these national distinctions and the limited global research comparing outcomes between living and cadaveric transplants for ALF patients, our objective was to evaluate the etiologies, donor types, outcomes, and survival metrics of LT conducted on pediatric and adult patients in Türkiye.
Materials and methods
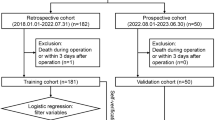
This was a multicenter study of adult and pediatric (< 18 years) ALF patients undergoing LT between January 2002 and November 2019. Turkish Association for the Study of the Liver (TASL) coordinated the Acute Liver Failure and Liver Transplantation Special Interest Group with the participation of 14 liver transplant centers across Türkiye. ALF was defined clinically, biochemically, and, when available, histologically according to international ALF guidelines13,14. All enrolled patients met the entry criteria for ALF and the data were retrieved from standardized electronic case reports from each center. The data was collected only for ALF patients who were transplanted, and included demographic information, date of transplantation, blood biochemistry within 24 h before transplantation. The information on pre-transplant treatments, such as administration of vasopressors, intracranial pressure monitoring, renal replacement therapy, or plasmapheresis was not reported. Given the rarity of ALF, all patients who received a diagnosis and subsequently underwent LT were included in the study. As such, no specific exclusion criteria were established. Patients with ALF who did not undergo LT were not included in this study, as data on non-transplanted ALF cases were incomplete and inconsistently recorded across participating centers. The study was approved by the Ethics Committee of the School of Medicine of Dokuz Eylül University. All methods were performed with the relevant guidelines and regulations. Specifically, the research was conducted in compliance with the Declaration of Helsinki. In this study, no transplanted livers were procured from prisoners. As this study is retrospective in nature, informed consent to participate was deemed unnecessary according to national regulations.
The etiologies were categorized based on detailed clinical, laboratory (within 24 h prior to LT), and imaging examinations and the evaluations included the following investigations as appropriate; serologic markers for viral etiologies (HAV, HBV, hepatitis C virus, hepatitis E virus, Epstein-Bar virus, cytomegalovirus, herpes simplex virus), autoantibodies for autoimmune liver diseases (anti-nuclear, anti-smooth muscle, and liver-kidney microsomal antibodies; if needed, anti-soluble liver antigen/liver-pancreas and anti-liver cytosol type 1 antibodies), tests for Wilson’s disease (ceruloplasmin, 24-hour urine copper level), metabolic screening (including tandem mass spectrometry, urine organic acid analysis, and serum lactate, pyruvate, and ferritin levels), and imaging investigations for Budd-Chiari syndrome (BCS). DILI was diagnosed by causality assessment of prescription drugs, over-the-counter medications, complementary/alternative medicines, dietary supplements, and illicit substance use after excluding other etiologies. Acute ischemic injury was diagnosed in the setting of (i) cardiac, circulatory, or respiratory failure; (ii) a dramatic increase in serum aminotransferase and lactic dehydrogenase enzyme levels; (iii) the exclusion of other common causes of hepatitis15. The diagnosis of pregnancy-related ALF was based on careful history, physical examination, laboratory, and imaging results for acute fatty liver of pregnancy and hemolysis, elevated liver enzymes, and low platelet count (HELLP syndrome). If no etiology could be established, ALF was classified as indeterminate. In the histological evaluation of the explanted livers, those having more than 90% necrosis were defined as massive hepatic necrosis, while livers exhibiting 15–90% necrosis were categorized as submassive hepatic necrosis16.
National Coordination Center under the Ministry of Health of Türkiye allocate the deceased liver donors nationwide by prioritizing according to listing status based on the model for end-stage liver disease (MELD) and Pediatric end-stage liver disease (PELD) scores. Patients with ALF were classified as United Network for Organ Sharing (UNOS) status 1b. In the case of the need for emergency LT, if a cadaveric liver graft was available, patients underwent deceased donor liver transplantation (DDLT); if not, the family was counseled about the need for a suitable living donor. The detailed protocol for the physical and psychological evaluation of potential living donors has been described previously17. All donors were under the age of 50. ABO-compatible graft livers were used in all patients. In LDLT, the right lobe of the liver was used for most adult cases, whereas the left lateral segments were used for pediatric cases. Patient management in intensive care units and post-transplant immunosuppression protocols were implemented according to the local protocol at each center. The patients were followed up in outpatient clinics at 1- to 3-month intervals. A physical examination and laboratory tests were performed at each visit.
The immunosuppressive protocols consisted of tacrolimus or cyclosporine and mycophenolate mofetil plus a steroid treatment. Tacrolimus or cyclosporine was administered with a therapeutic target level. Corticosteroids were gradually tapered and discontinued 6 months post-transplantation, except for cases with autoimmune etiologies. Alternative immunosuppressive agents, including sirolimus or everolimus, were used for some patients who were intolerant to calcineurin inhibitors or who had renal dysfunction.
The primary objective of this study was to estimate the short-term (3-month) and long-term (beyond 3 months) survival rates for both DDLT and LDLT. The secondary objectives were to identify the factors associated with the survival of pediatric and adult patients according to graft type.
Statistical analysis
Baseline measurable characteristics are presented as medians with corresponding 95% confidence intervals. For categorical variables, counts and percentages (%) were utilized. The Mann-Whitney U test was used to assess differences in continuous variables among children and adults, as well as between DDLT and LDLT groups, while the Chi-square test was applied to categorical variables. The survival rates at 3, 6, 12, and 24 months and 3, 5, and 10 years after LT were calculated using a life table analysis. Patient survival was assessed using the Kaplan-Meier estimator. Comparisons of survival curves between stratified subgroups were performed using the log-rank test. Because 81% of deaths occurred within the first three months, Cox regression was used to investigate the relationships between various parameters and 3-month survival. The investigated parameters were patient demographics, comorbid conditions, initial results of hospital blood tests (bilirubin, albumin, international normalized ratio [INR], creatinine, sodium, lactate, ammonia and pH values), MELD/PELD score before transplantation, etiology of ALF, waiting time until transplantation, type of transplant (LDLT or DDLT), degree of necrosis in the explanted liver, and HE grading. Variables found to be related to survival in univariate analysis were included in a multivariate analysis using a stepwise model. To evaluate whether specific cutoff values of continuous variables are more strongly associated with survival, receiver operating characteristic (ROC) analysis was performed and the Youden index was used to identify optimal thresholds for predicting 3-month mortality. These dichotomized variables were then compared to their continuous forms using Cox regression. Cutoff values for sodium (> 140 mEq/L) and arterial pH (< 7.3) showed a stronger association with 3-month survival than their continuous counterparts and were therefore included in the multivariable regression analysis. To mitigate the impact of baseline differences, propensity score matching was conducted between patients who underwent LDLT and DDLT, and subsequent survival analysis was performed on the matched cases. In all analyses, p < 0.05 was considered statistically significant. Missing data were addressed using a complete-case analysis approach, whereby only cases with available data for all variables included in a given model were analyzed. No data imputation was performed. This decision was based on the relatively low proportion of missing values and the intention to avoid assumptions inherent in model-based imputation techniques. We acknowledge that this approach may have resulted in a reduction in statistical power, particularly in multivariable models. The analyses were performed using IBM SPSS Statistics 22.0 (IBM, Armonk, NY, USA) for Windows and MedCalc 19.4 (MedCalc Software, Ostend, Belgium) for Windows.
Results
Among 6944 liver transplants performed in Türkiye between January 2002 and November 2019, 336 (4.8%) were ALF; these cases comprised the study cohort. The patient characteristics are shown in Table 1. There were 236 (70.2%) adults (female/male ratio: 143/93), and 100 (29.8%) children (female/male ratio: 48/52). The mean age at diagnosis was 37.0 ± 13.5 years for adults and 8.1 ± 5.5 years for children. The mean MELD and PELD scores were 31.1 ± 7.2 and 27.5 ± 9.6, respectively. 73% of the patients had HE grades 3–4. Adults exhibited poorer pretransplant levels of serum albumin, creatinine, and ammonia than children. The median waiting time from list to LT was 4 days (range: 0–34 days). The waiting time for transplantation was shorter in children (3 days) than in adults (4 days). LDLT was performed on 221 patients (65.8%), and DDLT was performed on 115 patients (34.2%). No living donor deaths were recorded. Massive necrosis was observed in 83.6% of the explanted livers.
In adults, viral hepatitis was the most common (32.2%) etiology of ALF. Other frequent etiologies in adults were 27.1% indeterminate causes and 18.6% DILI. The most frequent causes of ALF in children were 38.0% indeterminate causes, 24.0% DILI, 15.0% acute viral hepatitis, and 12.0% Wilson’s disease. The viruses leading to ALF were 88.2% HBV in adults, and 73.3% HAV in children. DILI was reported in 20.2% of the whole cohort (44 adults and 24 children). Twenty-three different agents, along with unknown drugs or herbal remedies, were thought to cause DILI-related ALF alone or in combination. The major ones were acetaminophen (11.8%), anti-tuberculosis drugs (8.8%), ornidazole (7.4%), and amoxicillin/clavulanate (7.4%).
Overall Survival
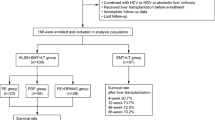
The mortality rate for the entire cohort was 30.1% with the highest rate within the first 3 months after LT (81%, n = 82). The mean overall survival (OS) was 140.9 (95% confidence interval [CI], 130.2-151.7) months, and the median follow-up period was 26.6 months (range, 1 day to 206.3 months). The cumulative survival rates at 3 months, 6 months, 1, 3, 5, and 10 years in pediatric and adult patients were 87.7%, 86.6%, 84.3%, 83.1%, 81.3%, 78.2%, and 69.7%, 68.4%, 66.9%, 63.4%, 63.4%, 62.0%, respectively (Fig. 1A-B). Cause-of-death data were available for 101 patients. The most common causes of mortality were multiorgan failure with or without sepsis (44%), acute or chronic rejection (19%), cardiac events (13%), intra-abdominal bleeding (11%), primary graft nonfunction (3%), cerebral events (1%), and other causes (9%). Three adult patients underwent retransplantation due to graft dysfunction, all of whom subsequently died.
Survival in pediatric patients
The mean OS in children was 165.7 (95% CI: 148.7-182.8) months. Out of 100 children, 18 children died during follow-up, and 12 of death were within first 3 months. Pre-transplant parameters associated with 3 months survival were shown in Table 2. In multivariate Cox regression analysis, serum albumin level (HR: 2.36) and grade 4 HE (HR: 3.37) were associated with 3 months mortality. No association was found between any pretransplant parameter and mortality beyond 3 months.
Survival in adults
The mean survival among adults was 117.3 months (95% CI: 105.6–129.0). Among the 83 recorded deaths during the follow-up period, 70 (84%) occurred within the initial 3 months. In multiple regression analysis, pre-transplant parameters including serum sodium level > 140 mEq/L (HR: 2.49), grade 4 HE (HR: 2.93), a MELD score higher than 35 (HR: 2.10), and an arterial pH lower than 7.3 (HR: 1.95), and having undergone DDLT (HR: 2.09) were found to be associated with 3-month mortality following transplantation (Table 2). Kaplan–Meier survival analyses illustrating the impact of these risk factors on 3-month survival are presented in Fig. 3, corroborating the findings from multivariable regression. When the patients were divided into hyponatremic (Na ≤ 130 mEq/L), normonatremic (Na = 131–145 mEq/L), and hypernatremic (Na > 145 mEq/L) groups, the mean survival times were 86.7 (95% CI: 67.6-105.8), 117.5 (95% CI:103.9-131.1), and 16.4 (95% CI: 4.9–27.9) months, respectively. Hypernatremic patients had significantly lower survival than others (p < 0.0001).
Kaplan–Meier survival curves demonstrating the association between 3-month post-transplant mortality and key predictors identified in multivariable regression analysis, including transplantation type (A), hepatic encephalopathy (B), MELD score (C), serum sodium level (D), and arterial pH (E). Log-rank tests were used to compare survival distributions across groups.
We developed a prognostic index incorporating five independent predictors of post-transplant mortality in ALF patients: transplantation type (DDLT vs. LDLT), HE grade, serum sodium level, MELD score, and arterial pH. This composite score demonstrated good discriminative ability (AUC = 0.823, p < 0.001), with sensitivity and specificity of 81.8% and 71.7%, respectively.
Survival in patients of various etiology was highly variable (Table 3). The patients transplanted for DILI had the best survival (140.1 months), whereas patients with mushroom poisoning had the shortest mean survival of 37.5 months. The multivariate analysis showed higher mortality beyond 3 months after LT in patients with grade 4 HE (HR: 5.71, 95% CI: 1.43–22.80) and in BCS (HR: 5.97, 95% CI: 1.47–24.2).
Survival in DDLT and LDLT patients
In the pediatric group, Kaplan-Meier analysis revealed mean survivals of 166.7 months (95%CI: 148.3-185.2) for LDLT and 131.8 months (95% CI: 93.6–170.0) for DDLT recipients (p = 0.5959), indicating comparable survival rates. No significant difference was observed in waiting time between the LDLT and DDLT groups. The 3 months mortality for children was 10.5% in the LDLT group (9 out of 86) and 21.4% in the DDLT group (3 out of 14), showing no significant statistical difference.
In the adult group, mean survival was 134.6 (95% CI: 120.6-148.6) months in patients who received LDLT and 88.6 (95% CI: 71.2–106.0) months in patients who received DDLT (p = 0.0012) (Fig. 2A). Within 3 months after transplantation, mortality rates were 21.5% (29 of 135 patients) for LDLT and 40.6% (41 of 101 patients) for DDLT (p = 0.0024).
Comparing pretransplant characteristics of LDLT and DDLT adult patients, DDLT patients were older and had higher creatinine, lower ammonia, and more grade 4 HE (Table 4). Since these characteristics might had an impact on survival, the survival analysis was repeated by matching the groups for age, creatinine, ammonia, and HE grade (Table 4). The survival advantage of LDLT persisted after the matching to make groups comparable in all baseline parameters (Fig. 2B).
Discussion
Türkiye is recognized as the country having one of the highest numbers of LDLTs globally. This national cohort study was coordinated by TASL - Acute Liver Failure and Liver Transplantation Special Interest Group and has evaluated the parameters associated with the survival of LDLT and DDLT in pediatric and adult patients transplanted for ALF. The type of graft affected the survival after LT for ALF in adults, but no significant association was found between graft type and survival in children. Adults with LDLT had a more favorable life expectancy than patients with DDLT.
Despite advances in the management of ALF, timely transplantation remains the only definitive life-saving intervention. In countries with limited deceased donor organ availability, such as Türkiye, LDLT plays a pivotal role in bridging this gap. Türkiye is recognized as one of the global leaders in LDLT volume. In our cohort, 86% of pediatric and 57% of adult ALF patients underwent LDLT. Notably, the proportion of LDLT among adults with ALF was lower than the national average for all liver transplants during the same period (70%), which is attributable to the prioritization of ALF patients in the national deceased donor allocation system.
The overall outcomes for liver transplant recipients with ALF remain poorer than those for patients with end-stage liver disease, primarily due to higher early post-operative mortality rates18. In our study, the 1-, 5-, and 10-year cumulative survival rates were 72%, 68%, and 66%, respectively—figures that are comparable to those reported in Western studies19,20,21. However, these Western studies predominantly involved DDLT. In contrast, LDLT is the predominant modality in most Asian countries, accounting for over 90% of all liver transplants9,22. In our cohort, the cumulative 1-, 5-, and 10-year survival rates for LDLT recipients were 78%, 76%, and 74%, respectively, aligning well with previously published Asian data, which report 1-year survival rates between 65 and 80%, 5-year rates between 65 and 74%, and 10-year rates between 65 and 73%9,23,24,25,26.
Few studies have evaluated post-transplant outcomes in pediatric ALF patients receiving either living or deceased donor grafts. Consistent with our findings, several reports demonstrated comparable overall survival between the two groups12,27,28,29. However, other studies suggest a potential advantage of LDLT in this setting. For instance, a Brazilian study reported significantly lower primary non-function rates (6.9% vs. 31.8%) and improved one-year survival (75.9% vs. 50%) among LDLT recipients30. Furthermore, a meta-analysis encompassing 1,622 LDLTs and 6,326 DDLTs in the broader pediatric population supported the survival benefit of LDLT, suggesting better outcomes in both patient and graft survival31.
Our findings suggest that LDLT may provide a survival advantage over DDLT in adult patients with ALF. Jin et al. reported outcomes of 160 adult ALF recipients who underwent either LDLT (n = 124) or DDLT (n = 36), and found similar 1- and 3-year survival rates between the groups (79.0% and 74.8% for LDLT vs. 77.8% and 74.1% for DDLT)25. Similarly, Urrunaga et al. reported comparable 1- and 5-year survival probabilities (79% and 71%, respectively) in a smaller cohort of ALF patients32. A recent meta-analysis including 2574 adult ALF patients found no statistically significant differences in short- or long-term survival between LDLT (n = 192) and DDLT recipients33. Similarly, an analysis of the UNOS/OPTN registry between 2002 and 2020 showed that while LDLT was rarely used in the context of ALF (3.6% overall), post-transplant survival was comparable between LDLT and DDLT in pediatric patients, and no independent survival advantage of LDLT was identified in adults12. Contrary to our findings, the lack of observed survival benefit of LDLT in adult ALF patients in prior studies may partially stem from limited sample sizes (raising the risk of type II error) as well as the low frequency of LDLT procedures performed in those centers, which may have hindered the manifestation of its potential advantages. In our cohort, the anticipated advantage of shorter waiting times for LDLT was not evident, as the median waiting time was 4 days for both LDLT and DDLT recipients. Nevertheless, the survival benefit of LDLT remained significant even after matching pre-transplant variables (Table 4). This advantage may be attributed to several factors, including the superior quality and optimal condition of living donor grafts, more controlled surgical planning, reduced cold ischemia time, lower rates of graft rejection, and the possibility of more meticulous perioperative management in LDLT recipients. Although LDLT offers several benefits, its use in ALF is constrained by the urgency of transplantation, which allows minimal time for donor evaluation and places considerable pressure on both donor candidates and medical teams. Additionally, technical complexity and donor risks, particularly with right lobe hepatectomy, remain important concerns.
Several pre-transplant parameters were associated with 3-month mortality in both pediatric and adult cohorts. The significant predictors of post-transplant survival were grade 4 HE and hypoalbuminemia for pediatrics, MELD score, serum sodium and the presence of acidosis for adults. The number of studies investigating early mortality predictors in pediatric ALF remains limited. Consistent with our findings, the Pediatric Acute Liver Failure Study Group34 reported that pediatric patients presenting with grade III–IV HE or exhibiting neurological deterioration had markedly increased 21-day mortality, underscoring the prognostic significance of encephalopathy severity and progression in pediatric ALF. Serum albumin is a component of the PELD score and this score has been evaluated in a few small-scale studies for its prognostic utility in pediatric ALF35,36,37. However, to date, no studies have specifically addressed the prognostic significance of pre-transplant serum albumin levels in predicting early post-transplant mortality in this population. Further large-scale, prospective studies are needed to clarify its potential role in risk stratification.
In our adult cohort, serum sodium levels showed an inverse relationship with post-transplant survival, consistent across subgroups stratified by age and gender. While several studies linked pretransplant hyponatremia with increased post-LT mortality, more recent large-scale analyses have suggested that hypernatremia, rather than hyponatremia, is associated with worse outcomes. For instance, in a study by Leise et al. involving over 19,000 patients, hypernatremia (Na > 145 mEq/L) was independently associated with higher in-hospital and 90-day mortality38. In our multivariable regression analysis, a pre-transplant serum sodium level exceeding 140 mEq/L was independently associated with increased 3-month post-transplant mortality (HR: 2.49). While this threshold lies within the conventional physiological range (135–145 mEq/L), it was identified through ROC analysis utilizing the Youden index as the optimal discriminator for early mortality in our cohort. Importantly, this cutoff does not represent a diagnostic threshold for hypernatremia per se, but rather a statistically derived marker of elevated risk. Although patients with serum sodium > 145 mEq/L exhibited the poorest survival outcomes in subgroup analysis, the 140 mEq/L threshold demonstrated superior sensitivity and model performance in the multivariable context, underscoring its clinical relevance for risk stratification in ALF. Potential mechanisms include fluid loss due to lactulose and suction, overcorrection to prevent cerebral edema, and iatrogenic hypernatremia from transfusions or resuscitation fluids. The prognostic utility of the MELD score in non-acetaminophen ALF has been previously demonstrated, with some studies suggesting its predictive performance is comparable to that of the King’s College Hospital criteria in this context39. Consistent with these findings, our analysis identified a MELD score > 35 as an independent predictor of 3-month post-transplant mortality. Acidosis (arterial pH < 7.3) is recognized as one of the prognostic markers in the King’s College Criteria for acetaminophen-induced ALF. It reflects severe metabolic decompensation and systemic compromise, often associated with multiorgan dysfunction. In our cohort, although the number of acetaminophen-related ALF cases was limited, acidosis emerged as an independent predictor of post-transplant outcome. The prognostic index we developed, incorporating five pretransplant variables (transplantation type, HE grade, serum sodium, MELD score, and arterial pH), demonstrated a high discriminative ability in predicting early post-LT mortality among ALF patients. This model, derived from routinely available clinical parameters, offers a practical tool for pretransplant risk stratification. While existing prognostic tools in ALF primarily focus on listing decisions (e.g., King’s College Criteria), our score uniquely targets outcomes after transplantation. Given its promising performance (AUC = 0.846), further validation in external, multicenter cohorts is warranted. If confirmed, this score may assist transplant teams in optimizing candidate selection, timing, and postoperative care strategies in this high-risk population.
While an association between pre-LT characteristics and early post-LT mortality is evident, elucidating the relationship between pre-LT variables and extended mortality is challenging. Yoon et al. found an association between pre-LT HE and long-term mortality after DDLT for chronic liver disease but did not propose an explanatory hypothesis40. The pre-transplant factors associated with survival beyond three months in adults were grade 4 HE and BCS. Due to the lack of posttransplant follow-up and treatment data, we do not have sufficient evidence to speculate on the association of BCS with mortality beyond three months.
This study has inherent limitations due to its retrospective design. Several clinically relevant variables, including the use of vasopressors, renal replacement therapy, transfusion requirements, ischemia times, donor and graft characteristics, and posttransplant complications, were either not recorded or inconsistently reported. As a result, we were unable to assess the impact of these factors on post-LT survival outcomes. In addition, the study included only patients who underwent LT; data on ALF patients who were listed but did not undergo transplantation—or were too critically ill to receive one—were not available across centers. Consequently, the proportion and outcomes of non-transplanted ALF cases remain unknown. Moreover, observed differences in survival outcomes between LDLT and DDLT may be confounded by structural variations in national transplant systems, including organ allocation frameworks, donor pool characteristics, and timing of transplantation—all of which differ across countries and were beyond the analytical scope of this study.
In conclusion, LDLT could represent a favorable option in terms of survival for adult ALF patients, but additional multicenter and prospective studies are needed to validate this observation. Early post-transplant mortality in adults was found to be associated with transplantation type, pre-transplant acidosis, grade 4 HE, serum sodium > 140 mEq/L, and high MELD score.
Data availability
The datasets used and analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- ALF:
-
Acute liver failure
- BCS:
-
Budd-Chiari syndrome
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- DDLT:
-
Deceased donor liver transplantation
- DILI:
-
Drug-induced liver injury
- HAV:
-
Hepatitis A virus
- HBV:
-
Hepatitis B virus
- HE:
-
Hepatic encephalopathy
- HELLP:
-
Hemolysis, elevated liver enzymes, and low platelets
- HR:
-
Hazard ratio
- INR:
-
International normalized ratio
- LDLT:
-
Living donor liver transplantation
- LT:
-
Liver transplantation
- MELD:
-
Model for end-stage liver disease
- OR:
-
Odds ratio
- OS:
-
Overall survival
- PELD:
-
Pediatric end-stage liver disease
- TASL:
-
Turkish Association for the Study of the Liver
- UNOS:
-
United Network for Organ Sharing
References
Wlodzimirow, K. A., Eslami, S., Abu-Hanna, A., Nieuwoudt, M. & Chamuleau, R. A. Systematic review: acute liver failure - one disease, more than 40 definitions. Aliment. Pharmacol. Ther. 35 (11), 1245–1256 (2012).
Lee, W. M. Acute liver failure. N Engl. J. Med. 329 (25), 1862–1872 (1993).
Wendon, J. et al. EASL clinical practical guidelines on the management of acute (fulminant) liver failure. J. Hepatol. 66 (5), 1047–1081 (2017).
Jayalakshmi, V. T. & Bernal, W. Update on the management of acute liver failure. Curr. Opin. Crit. Care. 26 (2), 163–170 (2020).
Stravitz, R. T. & Lee, W. M. Acute liver failure. Lancet 394 (10201), 869–881 (2019).
Reuben, A. et al. Outcomes in adults with acute liver failure between 1998 and 2013: an observational cohort study. Ann. Intern. Med. 164 (11), 724–732 (2016).
Russo, M. W., LaPointe-Rudow, D., Kinkhabwala, M., Emond, J. & Brown, R. S. Jr Impact of adult living donor liver transplantation on waiting time survival in candidates listed for liver transplantation. Am. J. Transpl. 4 (3), 427–431 (2004).
Bernal, W. et al. Outcome after wait-listing for emergency liver transplantation in acute liver failure: a single centre experience. J. Hepatol. 50 (2), 306–313 (2009).
Yamashiki, N. et al. Outcomes after living donor liver transplantation for acute liver failure in japan: results of a nationwide survey. Liver Transpl. 18 (9), 1069–1077 (2012).
Ostapowicz, G. et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the united States. Ann. Intern. Med. 137 (12), 947–954 (2002).
Global Observatory on Donation and Transplantation. International Report on Organ Donation and Transplantation Activities 2021 2021 [Available from: https://www.transplant-observatory.org/2021-global-report-5/
Moughames, E. et al. Recipient survival among living donor vs. Deceased donor liver transplants for acute liver failure in the united States. J. Clin. Med. ;13(6), 1729 (2024).
O’Grady, J. G., Schalm, S. W. & Williams, R. Acute liver failure: redefining the syndromes. Lancet 342 (8866), 273–275 (1993).
Squires, R. H. Jr. et al. Acute liver failure in children: the first 348 patients in the pediatric acute liver failure study group. J. Pediatr. 148 (5), 652–658 (2006).
Henrion, J. et al. Hypoxic hepatitis: clinical and hemodynamic study in 142 consecutive cases. Med. (Baltim). 82 (6), 392–406 (2003).
Hanau, C., Munoz, S. J. & Rubin, R. Histopathological heterogeneity in fulminant hepatic failure. Hepatology 21 (2), 345–351 (1995).
Kilic, M. et al. Live donor liver transplantation for acute liver failure. Transplantation 84 (4), 475–479 (2007).
Bernal, W. & Wendon, J. Liver transplantation in adults with acute liver failure. J. Hepatol. 40 (2), 192–197 (2004).
Germani, G. et al. Liver transplantation for acute liver failure in europe: outcomes over 20 years from the ELTR database. J. Hepatol. 57 (2), 288–296 (2012).
Farmer, D. G. et al. Liver transplantation for fulminant hepatic failure: experience with more than 200 patients over a 17-year period. Ann. Surg. 237 (5), 666–675 (2003). discussion 75 – 6.
Chan, G. et al. Long-term outcomes of emergency liver transplantation for acute liver failure. Liver Transpl. 15 (12), 1696–1702 (2009).
de Villa, V. H., Lo, C. M. & Chen, C. L. Ethics and rationale of living-donor liver transplantation in Asia. Transplantation 75 (3 Suppl), S2–5 (2003).
Pamecha, V. et al. Living donor liver transplantation for acute liver failure: donor safety and recipient outcome. Liver Transpl. 25 (9), 1408–1421 (2019).
Ikegami, T. et al. Living donor liver transplantation for acute liver failure: a 10-year experience in a single center. J. Am. Coll. Surg. 206 (3), 412–418 (2008).
Jin, Y. J. et al. Predicting survival after living and deceased donor liver transplantation in adult patients with acute liver failure. J. Gastroenterol. 47 (10), 1115–1124 (2012).
Yuan, D. et al. Adult-to-adult living donor liver transplantation for acute liver failure in China. World J. Gastroenterol. 18 (48), 7234–7241 (2012).
Szymczak, M. et al. Acute liver failure in children-Is living donor liver transplantation justified? PLoS One. 13 (2), e0193327 (2018).
Ogura, Y., Kabacam, G., Singhal, A. & Moon, D-B. The role of living donor liver transplantation for acute liver failure. Int. J. Surg. 82S, 145–148 (2020).
Uribe, M. et al. Living donor liver transplantation in pediatric patients with acute liver failure: safe and effective alternative. Transpl. Proc. 40 (9), 3253–3255 (2008).
Tannuri, A. C. et al. Pediatric acute liver failure in brazil: is living donor liver transplantation the best choice for treatment? Liver Transpl. 22 (7), 1006–1013 (2016).
Barbetta, A. et al. Living donor versus deceased donor pediatric liver transplantation: A systematic review and Meta-analysis. Transpl. Direct. 7 (10), e767 (2021).
UrrunagaNH, RachakondaVP, MagderLS & MindikogluAL Outcomes of living versus deceased donor liver transplantation for acute liver failure in the united States. Transpl. Proc. 46 (1), 219–224 (2014).
Shingina, A. et al. Adult-to-adult living donor liver transplantation in acute liver failure. Transpl. Rev. (Orlando). 36 (2), 100691 (2022).
Ng, V. L. et al. Outcomes of children with and without hepatic encephalopathy from the pediatric acute liver failure study group. J. Pediatr. Gastroenterol. Nutr. 63 (3), 357–364 (2016).
Sanchez, M. C. & D’Agostino, D. E. Pediatric end-stage liver disease score in acute liver failure to assess poor prognosis. J. Pediatr. Gastroenterol. Nutr. 54 (2), 193–196 (2012).
Núñez-Ramos, R. et al. Acute liver failure: outcome and value of pediatric End-Stage liver disease score in pediatric cases. Pediatr. Emerg. Care. 34 (6), 409–412 (2018).
Walabh, P. et al. Prognostic factors and scoring systems associated with outcome in pediatric acute liver failure. BMC Pediatr. 22 (1), 516 (2022).
Leise, M. D. et al. Effect of the pretransplant serum sodium concentration on outcomes following liver transplantation. Liver Transpl. 20 (6), 687–697 (2014).
Katoonizadeh, A. et al. MELD score to predict outcome in adult patients with non-acetaminophen-induced acute liver failure. Liver Int. 27 (3), 329–334 (2007).
Yoon, J. U. et al. The impact of pretransplant hepatic encephalopathy, model for end-stage liver disease (MELD) scale on long-term survival following deceased donor liver transplantation: a retrospective study. Ann. Palliat. Med. 10 (5), 5171–5180 (2021).
Acknowledgements
The authors wish to thank all members of the TASL- Acute Liver Failure and Liver Transplantation Special Interest Group and the entire team involved in the operation, follow-up, and the treatment of these patients.
Author information
Authors and Affiliations
Contributions
I.T., U.S.A, and R.I wrote the main manuscript text. U.S.A performed the statistical analysis. I.T., U.S.A, M.Al., M.H., S.Y., G.G., Ç.A., K.Y.P., F.Ö., M.Ak., T.Ü., Z.K., M.Z., H.G., M.A.K., E.B.B., A.Ç.K., D.B., M.D., H.A., D.D., H.D., M.T.G., F.G., E.D., Y.B., A.B.D., G.K., M.Aky., F.Gü., A.G., R.I. contributed to data collection and interpretation. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Grants and financial support
The authors received no funding for this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Turan, İ., Akarca, U.S., Aladağ, M. et al. Pre-transplant predictors of 3-Month survival following liver transplantation for acute liver failure in adult and pediatric patients in Türkiye. Sci Rep 15, 26221 (2025). https://doi.org/10.1038/s41598-025-11298-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-11298-y