Abstract
We aimed to clarify the distribution of the spatiotemporal burden of Low physical activity (LPA)-related cardiovascular disease (CVD) at the global, regional, and national levels from 1990 to 2021. We systematically extracted Global Burden of Disease Study (GBD) 2021 data on CVD burden attributable to LPA from 1990 to 2021, stratified by Socio-demographic Index (SDI) quintiles and 21 GBD geographical regions. Three complementary metrics were employed: (1) Age-standardized death rate (ASDR) and (2) Disability-Adjusted Life Year (DALY) rate provided cross-sectional burden estimates, while (3) Estimated Annual Percentage Change (EAPC) quantified temporal trends in ASDR/DALY rates. The EAPC-derived trend patterns were further analyzed in conjunction with SDI levels and regional variations to identify disparities in physical inactivity-related CVD burden. The age-standardized DALY rate (EAPC = -1.30) and ASDR (EAPC = -1.41) for CVD attributable to LPA showed a decreasing trend from 1990 to 2021. The highest age-standardized DALY rate and ASDR per 100,000 population across all five SDI regions were observed in the Low-middle SDI region (111.53; 5.67). Among the 21 geographic regions and 204 countries, the highest age-standardized DALY rate and ASDR per 100,000 population for CVD attributable to LPA in 2021 were both reported in North Africa and the Middle East (211.62; 10.50), with Sudan having the highest rates (616.58; 24.56). The largest increase in the age-standardized DALY rate from 1990 to 2021 was observed in Southeast Asia (EAPC = 0.19), while the most substantial increase in ASDR was noted in Southern sub-Saharan Africa (EAPC = 0.44). Both the age- standardized DALY rate and ASDR increased the most in Lesotho (EAPC = 2.30; EAPC = 2.39). Although the global burden of CVD attributable to LPA has decreased from 1990 to 2021, the burden remains significant in low- and middle-income countries.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the leading cause of death worldwide and a major contributor to the global burden of disease. Over the past three decades, population aging, globalization, and increased pace of life have interacted with modifiable risk factors such as smoking, unhealthy diets, and physical inactivity to increase both new and recurrent CVD cases. The number of people living with CVD has almost doubled from 285 million in 1990 to an estimated 550 million in 20221. CVD is associated with a wide range of heterogeneous risk factors including metabolic, environmental, and lifestyle factors2. Several studies have shown that there is an inverse dose-response relationship between physical activity (PA) and CVD mortality3. It has been estimated that approximately 75% of CVD deaths could be prevented by appropriate lifestyle changes, particularly through increasing levels of physical activity.
Physical inactivity is the fourth leading cause of death according to the World Health Organization (WHO), but one quarter of adults worldwide do not meet the physical activity recommendations of the WHO4,5. LPA is a major contributor to metabolic risk factors that are associated with CVD. It is estimated that 23% of the world’s population is physically inactive and that 7.6% of CVD mortality can be attributed to this condition4. A large proportion of the world’s population is regularly exposed to low physical activity (LPA), which significantly contributes to the risk of cardiovascular disease (CVD), which places a heavy economic burden on healthcare systems6. LPA is the most important risk factor, accounting for 7.2% of all-cause mortality worldwide and 69% of deaths in middle-income countries4. Focusing on middle-income countries is crucial because these regions experience a disproportionate burden of deaths attributable to LPA. This is largely due to rapid urbanization, sedentary lifestyles, and limited public health infrastructure to promote physical activity7. Additionally, middle-income countries often face a double burden of disease, with persistent infectious diseases alongside rising noncommunicable diseases (NCDs) linked to LPA, such as CVDs and diabetes9. Addressing LPA in these regions can significantly reduce the global burden of mortality and morbidity. To address this growing public health problem, evidence-based guidelines on physical activity have been developed by WHO, United States, Canada, and China to increase physical activity levels and promote healthy lifestyles8,10.
The global burden of CVD and its risk factors can be obtained from the Global Burden of Disease (GBD) 2021 website. The burden and temporal trends of CVD related to metabolic risk factors, ambient particulate matter, and high body mass index (BMI) have been assessed in previous studies. However, previous studies have explored the global burden of CVD attributable to LPA, providing valuable insights into regional disparities and temporal trends. For instance, Lu et al. (2024)11 and Luo et al. (2024) analyzed spatiotemporal patterns of CVD burden attributable to LPA using GBD 2019 data12. However, these studies were limited to data up to 2019 and did not account for the potential impact of the COVID-19 pandemic on physical activity and CVD health.
The present study builds on this foundation by utilizing the most recent GBD 2021 dataset, which includes updated estimates for 2020–2021. Additionally, we shift the focus to LPA as an independent risk factor for CVD, offering a novel perspective on the interplay between renal health and cardiovascular outcomes. Our analysis provides a comprehensive assessment of temporal trends, regional disparities, and socioeconomic determinants of CVD burden attributable to LPA, offering new insights to inform public health policy and intervention strategies.
Methods
Research data sources
Data for this study were obtained from the Global Health Data Exchange website (http://ghdx.healthdata.org/gbdresults-tool). This site provides a visualization tool to display and analyze the data from the GBD 2021 study, which includes CVD mortality and disability due to LPA in seven super-regions, twenty-one regions, and two hundred and four countries between 1990 and 2021. The study explicitly lists the ICD-10 codes used to define CVDs in the Methods section (e.g., B33.2, I01-I01.9, I20-I25.9, etc.), CVD cases were identified using ICD-10 codes (full list provided in Supplementary Table 1)12. The Socio-Demographic Index (SDI) is a composite indicator that incorporates economic growth, education level, and fertility rate to measure the socio-economic development level of each country. Based on the SDI value, the 204 countries and territories are divided into five groups: Low SDI:≤0.45, Low-middle SDI: >0.45 to ≤ 0.60, Middle SDI: >0.60 to ≤ 0.75, High-middle SDI: >0.75 to ≤ 0.85, High SDI: >0.85. These SDI groups assist researchers in analyzing the impact of different levels of socio-economic development on health issues12. This study is based on a publicly available database and does not require ethical approval.
Attributable risk factors
The GBD Standardized Version 2021 questionnaire, a global physical activity assessment tool comprising the Global Physical Activity Questionnaire (GPAQ) and the International Physical Activity Questionnaire (IPAQ) was employed in this study13,14. The unit of energy expenditure used to measure the intensity of physical activity was metabolic equivalents (METs), where 1 MET is defined as 1 kcal of energy expenditure per kilogram of body weight per hour (i.e., sitting quietly).
The GPAQ and IPAQ were employed to quantify physical activity levels in terms of MET-minutes per week, a standardized unit of energy expenditure. Participants reported the frequency and duration of physical activities across different domains, allowing researchers to classify individuals into activity levels: LPA is defined as activities that result in < 4,000 MET-minutes/week, as per the GBD 2021 study, which categorizes physical activity levels based on metabolic equivalents (METs) using the GPAQ and IPAQ15.
These questionnaire-derived estimates of LPA prevalence were then integrated into the GBD comparative risk assessment framework. This framework uses population attributable fractions (PAFs) to estimate the proportion of CVD burden attributable to LPA. PAFs are calculated based on the relative risks of CVD associated with LPA, derived from meta-analyses of cohort studies, and the prevalence of LPA in each population group.
The PAF—the proportion of CVD burden attributable to LPA—is calculated using the formula:
where P is the prevalence of LPA and RR is the relative risk of CVD associated with LPA. This metric reflects how much CVD burden (e.g., deaths, DALYs) could theoretically be reduced if physical activity levels met recommended guidelines.
Statistical analysis
For the calculation of age-standardized rates (ASRs), a total of 1000 samples were utilized to ensure robust and reliable estimates. This sample size was chosen to minimize variability and enhance the precision of the ASRs. The ASRs were computed by applying age-specific rates to a standard population structure, allowing for meaningful comparisons across different regions and populations. Uncertainty intervals (UIs) were calculated to account for variability in the estimates. The estimated annual percentage changes (EAPCs) and their corresponding 95% confidence intervals (CIs) were used to measure the annual trends in Age-Standardized Death Rate (ASDR) and Disability-Adjusted Life Year (DALY) rates by fitting models. EAPC = 100 × (exp(β) − 1), where β is the direction of change in ASR. An increasing trend was defined as positive values for both EAPC and 95% CI, while a decreasing trend was defined as negative values for both. This method has been described in detail previously 16. All statistical analyses were performed using R software (version 4.1.3).
Results
Global burden of disease and trends in CVD due to LPAs
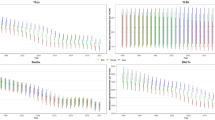
Globally, the 2021 DALYs and deaths due to LPA were 7,294,918.44 and 371,736.22, respectively. These values increased by 63.19% and 69.79%, compared with those in 1990. The age-standardized DALY rate and ASDR for LPA in 2021 were 85.95 (95% Uncertainty Interval: 35.25, 140.65) and 4.53 (95% UI: 1.52, 8.05), respectively, which were lower than those reported in 1990 by 36.35% and 2.23%, respectively. The age-standardized DALY rate for CVD caused by LPA decreased from 1990 to 2021 with an EAPC of − 1.30 (95% CI: − 1.36, −1.24). Similarly, the ASDR for LPA decreased from 1990 to 2021 with an EAPC of − 0.141 (95% CI: −1.47, −1.36). This study showed a downward trend in the global disease burden of LPA-induced CVD (Table 1; Fig. 1).
Trends by gender and age
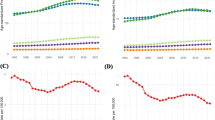
The age-standardized DALY rate and ASDR per 100,000 population with CVD attributable to LPA in 2021 were higher in females than males (age-standardized DALY rate: 92.49 vs. 77.20; ASDR: 4.91 vs. 3.96). From 1990 to 2021, the age-standardized DALY rate and ASDR attributable to LPA factors for CVD decreased in both sexes, with a more significant decrease observed in females (age-standardized DALY rate: male EAPC = − 1.00; female EAPC = − 1.42) (ASDR: male EAPC = − 0.99; female EAPC = − 0.99; female EAPC = − 1.42). In 2021, the mortality and DALY rates increased with age in both sexes, sharply increasing after the age of 60–64 and remaining high at ages 80+ (Table 1; Fig. 2, Supplementary Tables 2, 3).
SDI partition burden and super regions burden
As shown in Table 1; Fig. 1, the highest age-standardized DALY rate and ASDR per 100,000 CVDs attributable to LPA were found in Low-middle SDI region (age-standardized DALY rate: 111.53, 95% UI: 47.46, 180.69) (ASDR = 5.67, 95% UI: 2.02, 9.87) in 2021. The Middle SDI region had the second highest age-standardized DALY rate (104.39, 95% UI: 43.95, 170.88), while the High-middle SDI area had the second highest ASDR (5.65, 95% UI: 1.74, 10.62). The lowest age-standardized DALY rate and ASDR were found in High SDI (age-standardized DALY rate: 40.70, 95% UI: 16.23, 69.35) (ASDR = 2.06. 95% UI: 0.64, 3.83), with the largest decline in age-standardized DALY rate and ASDR observed in this region (EAPC = − 3.29; EAPC = − 3.76).
The age-standardized DALY rate and ASDR attributable to LPA decreased in all five SDI regions, with the decrease becoming more pronounced as the SDI increased (High SDI > High-middle SDI > Middle SDI > Low SDI > Low-middle SDI) (Table 1). The largest decrease was observed in the High SDI region (EAPC=−3.29; EAPC=−3.76). As the SDI value increased, the global age-standardized DALY rate and ASDR changed relatively smoothly until the SDI value reached approximately 0.5, after which both rates declined sharply as the SDI value increased. After an SDI value of 0.5, countries with an SDI value of approximately 0.2–0.4 (e.g., Central and Eastern Sub-Saharan Africa) had higher ASDR and age-standardized DALY rates than those with an SDI value of approximately 0.9 (e.g., Western Europe and High-income Asia Pacific) (Table 1; Figs. 1 and 3).
North Africa and Middle East had the highest age-standardized DALY rate and ASDR per 100,000 population with CVD attributable to LPA in 2021 (211.62 [95% UI: 91.41, 343.71] and 10.50 [95% UI: 4.07, 18.04], respectively). The second highest rates were found in Central Europe, Eastern Europe, and Central Asia. In contrast, Asia had an age-standardized DALY rate of 116.46 (95% UI: 43.76, 197.99) and an ASDR of 7.19 (95% UI: 2.15, 13.42). The regions with the lowest age-standardized DALY rates and ASDRs were all high-income areas (rate: 32.49 [95% UI: 11.99, 56.77]; ASDR: 1.73 [95% UI: 0.48, 3.24]) (Table 1).
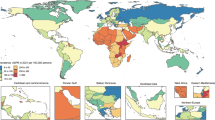
Geographic area burden
Among the 21 geographic regions, North Africa and Middle East had the highest age-standardized DALY and ASDR rate per 100,000 population with CVD due to LPA (211.62, 10.50) in 2021. Southern Latin America had the lowest age-standardized DALY rate and ASDR (19.47, 0.99). From 1990 to 2021, the age- standardized DALY rate increased most in Southeast Asia (EAPC = 0.19). The largest increase in ASDR is seen in Southern sub-Saharan Africa (EAPC = 0.44). Western Europe showed the largest decrease (EAPC = − 4.23) of age-standardized DALY rate Australasia (EAPC = − 4.47) has the largest decrease of ASDR (Table 1, Figs. 1AB, 4AB).
National burden
Sudan (616.58, 24.56) had the highest age-standardized DALY rate and ASDR per 100,000 population in 2021 for CVD due to LPA among the 204 countries, while Guatemala (15.60) had the lowest age-standardized DALY rate. The United Republic of Tanzania (0.60) had the lowest ASDR. Between 1990 and 2021, Lesotho had the most substantial increase in age-standardized DALY rate(EAPC = 2.30; male EAPC = 1.48; female EAPC = 2.48) and ASDR (total EAPC = 2.39; male EAPC = 1.35; female EAPC = 2.59), whereas Portugal had the most substantial decrease in age-standardized DALY rate (EAPC = − 5.37; male EAPC = − 5.20; female EAPC = − 5.52)and ASDR (total EAPC = − 5.52; male EAPC = − 5.46; female EAPC = − 5.57). (Supplementary Table 4, Figs. 3AB, 4AB).
Discussion
Over the period from 1990 to 2021, the absolute number of deaths and DALYs resulting from CVD attributable to kidney dysfunction increased significantly, with a rise exceeding 60%. This surge is largely attributable to global population growth and aging, highlighting the escalating public health challenge posed by CVD in an increasingly elderly population. Conversely, ASDR and age-standardized DALY rates showed a declining trend, indicating progress in reducing the relative burden of CVD. These improvements are likely due to advancements in healthcare, including better prevention, early diagnosis, and treatment strategies, particularly in high SDI regions. However, disparities persist, as low and low-middle SDI regions did not experience similar declines, underscoring the need to address global health inequalities. Together, these findings emphasize the dual challenge of managing both the absolute and relative burdens of CVD attributable to kidney dysfunction. In 2021, the most substantial burden of LPA-related CVD was observed in North Africa and the Middle East, Eastern Europe, and Southeast Asia. The most rapid growth in LPA-associated CVD was noted in Southern Sub-Saharan Africa and Southeast Asia. Notably, countries such as Portugal, Singapore, and Israel have seen a marked decline in ASDR and age-standardized DALY rates for LPA-related CVD over the past three decades. In contrast, Lesotho and Zimbabwe continue to witness escalating rates.
Several meta-analyses have examined the association between physical activity and CVD risk, revealing that different types of physical activity exert varying effects on CVD outcomes17. Physical activity is broadly categorized into leisure-time physical activity (LTPA), occupational physical activity (OPA), transportation-related activity, and domestic activity18. Among these, LTPA has been consistently highlighted as particularly beneficial for health promotion and disease prevention due to its association with reduced risks of CVD, improved endothelial function, and favorable impacts on metabolic and immune processes 19. In contrast, findings regarding OPA remain inconsistent, with some studies suggesting potential adverse health effects, possibly due to factors such as prolonged standing, repetitive movements, or insufficient recovery time20. Large population-based studies have demonstrated that engaging in moderate-intensity physical activity for a total of 150 min per week can significantly reduce the incidence of CVD by 17%, lower mortality by 23%, and decrease the risk of ischemic heart disease by 25%21. These findings underscore the critical role of physical activity, particularly LTPA, in mitigating major CVD risks. Additionally, physical activity contributes to obesity prevention, reduces atherosclerosis progression22,24, and induces beneficial biological effects on specific endocrine, immune, and metabolic pathways23. However, while the evidence supports the protective effects of LTPA, further research is needed to clarify the differential impacts of other activity types, such as OPA, which may not confer the same cardiovascular benefits and could even pose risks under certain conditions24. This nuanced understanding is essential for tailoring public health recommendations and interventions aimed at maximizing the cardiovascular benefits of physical activity.
Physical activity and exercise are well-established as key factors in improving cardiac capacity, reducing metabolic risk factors, and enhancing cardiac structure and function. However, the effects of physical activity can vary between women and men due to biological and physiological differences. For instance, women face unique clinical conditions such as pre-eclampsia, gestational diabetes mellitus, polycystic ovary syndrome, and menopause, which may predispose them to an increased risk of CVD25. Additionally, certain autoimmune diseases, which are more prevalent in women, further contribute to this elevated risk. Despite these challenges, women often demonstrate superior self-management skills, particularly in adhering to lifestyle modifications and medical interventions, which may mitigate some of the adverse outcomes associated with CVD. These gender-specific factors highlight the need for tailored approaches when designing exercise and health interventions for women compared to men.
Furthermore, aging introduces additional considerations, as both men and women experience changes in cardiovascular health over time. However, disparities in health outcomes are not solely attributed to biological factors; socioeconomic and geographic influences also play a significant role. For example, individuals in developed nations typically exhibit lower obesity rates and are less susceptible to metabolic risk factors such as hypercholesterolemia, hyperglycemia, and hypertension26,27. This trend may be attributed to better access to healthcare, higher health literacy, and environments that promote physical activity and healthier dietary habits. Conversely, individuals in low- and middle-income countries often face greater barriers to adopting healthy lifestyles, including limited resources, higher exposure to environmental stressors, and reduced access to preventive care. These disparities underscore the importance of considering both gender and regional contexts when addressing the global burden of CVD and promoting physical activity as a preventive strategy.
In line with previous studies and meta-analyses28,29, the age-standardized DALY rate and mortality due to CVD were significantly higher in low- and middle-income regions (Sub-Saharan Africa) than in Western Europe and High-income Asia Pacific regions. This difference may be related to the increasing adoption of Western diets and decreasing physical activity levels in low-income countries28. In contrast, high-income countries have a stronger focus on recreational physical activity, and people with higher socioeconomic status have more opportunities and resources to engage in such activities. However, low-income and low-education groups have a higher rate of inactivity and lack motivation29. The poor quality of primary health care services for screening and medical treatment of CVD further increases the disease burden. Therefore, mass media, community and public spaces, and fitness facilities should support global efforts to prevent LPA. Such support could increase physical activity levels and improve health outcomes.
There are substantial geographic variations in the ASDR and age-standardized DALY rate of CVD among countries and regions. These differences may be due to different exposure levels to risk factors. In 2021, North Africa and the Middle East region (including Sudan) had the highest ASDR and DALY rates for CVD. The region is undergoing a rapid demographic and economic transition, which is causing an epidemiological shift in disease burden. Obesity prevalence in this region was alarmingly high at 21.17%, with LPA being a major contributor to this increase. A recent meta-analysis showed that 49.2% of adults and 74.4% of adolescents in the region were not sufficiently physically active30. In Sudan, LPA was as high as 86.8%, with barriers to physical activity including insecurity, lack of interest, and time constraints. The Sudan war may have indirectly influenced the estimates of CVD) burden by exacerbating socioeconomic disparities, limiting access to healthcare, and increasing exposure to stress and malnutrition, all of which are significant risk factors for CVD30. Prolonged conflict often disrupts healthcare infrastructure, reduces availability of preventive care, and exacerbates poverty, further compounding CVD risks in affected populations 31. However, specific data linking the Sudan war directly to these estimates is not provided in the current analysis, highlighting a gap where further research could explore the intersection of conflict, socioeconomic instability, and CVD outcomes. Moreover, LPA was below the recommended level in Eastern Europe and Southeast Asia31, with more than 70% of the population not engaging in sufficient physical activity. Ambient air pollution, tobacco use, unhealthy dietary habits, and metabolic risk factors such as hypertension, hyperglycemia, hyperlipidemia, and diabetes mellitus are the main causes of the persistently high prevalence of CVD and mortality in these countries and regions32,33,34,35.
The age-standardized DALY rates and ASDR have increased substantially in Southern sub-Saharan Africa (Lesotho, Zimbabwe) between 1990 and 2021. Although the ASDR mortality rate is lower than that of high-income countries (HICs), absolute deaths have increased by more than 50%. The majority of these deaths occurred among younger populations, resulting in a higher number of DALYs. LPA may be influenced by local cultural and social values; overweight and obesity are considered desirable body images in some parts of Southern sub-Saharan Africa. In particular, being overweight or obese is still considered a symbol of health, wealth, well-being, and happiness among women36. Moreover, Sub-Saharan Africa faces unique challenges in addressing the rising burden of CVD. This region bears a disproportionate share of global health challenges, including infectious diseases such as HIV. Notably, approximately 70% of the global HIV population resides in Sub-Saharan Africa27. The intersection of HIV and CVD is becoming increasingly evident, as people living with HIV are at higher risk of developing CVD due to a combination of factors, including chronic inflammation, antiretroviral therapy side effects, and traditional CVD risk factors such as hypertension and dyslipidemia27. Compounding these issues is the region’s poor healthcare infrastructure and limited resources, which hinder effective prevention, diagnosis, and management of CVD37. As a result, the rising CVD burden in Sub-Saharan Africa is exacerbated by systemic healthcare disparities, creating an urgent need for targeted interventions and improved resource allocation.
This study assessed the spatial and temporal trends of LPA-associated CVD in 204 countries and 21 regions from 1990 to 2021. However, there are several limitations that should be considered. First, epidemiological data on CVD is not available for Southern Sub-Saharan Africa, which may result in biased or underestimated estimates. In Low SDI regions, underreporting of deaths due to weaker vital registration systems and limited access to healthcare may lead to underestimation of mortality rates. Additionally, the narrower UIs might stem from sparse or less variable data, which can result in overly precise estimates despite potential inaccuracies. These discrepancies highlight the need for cautious interpretation of GBD Second, most studies do not adjust for changes in the intensity and type of physical activity during follow-up38. Physical activity data are often collected using self-reports, which may not accurately reflect actual physical activity levels. Another key limitation is the scarcity of data points used in the GBD 2021 study to estimate exposure to LPA and its relative risk. The GBD 2021 study relied on only 261 studies from 131 countries to estimate LPA exposure and 100 data inputs from 17 countries to calculate the relative risk of LPA-related CVD. This limited data availability, particularly in low- and middle-income countries, may introduce uncertainty and potential bias in the global and national burden estimates, which could affect the precision of our findings15. Therefore, the results may be affected by misclassification of physical activity and measurement errors, which could affect the accurate assessment of the association between physical activity and health outcomes. Low-SDI regions often face challenges such as limited resources, incomplete health registries, and underreporting, which may introduce uncertainties into the LPA estimates. Regarding PAQ, it is unclear whether they were systematically obtained for all SDI regions, as the study relies on GBD data, which integrates multiple sources and may not uniformly apply PAQs across all regions. This heterogeneity in data sources could further affect the comparability and accuracy of LPA estimates across different SDI levels.
Conclusion
In conclusion, although the global burden of CVD attributable to LPA has declined from 1990 to 2021, it remains disproportionately high in certain regions and populations. Notably, the burden is particularly elevated in low- and middle-income regions, including North Africa and the Middle East, Southern sub-Saharan Africa, Southeast Asia, and Sudan, with Lesotho exhibiting a persistently high burden. Additionally, women continue to experience a higher relative burden compared to men, highlighting the need for targeted interventions to address these disparities.
The data underscores the critical importance of addressing LPA, a key contributor to a range of chronic health conditions. By implementing targeted prevention strategies, communities can reduce the burden of non-communicable diseases, improve overall well-being, and enhance quality of life. Furthermore, promoting science education is essential to fostering informed decision-making and empowering individuals to adopt healthier lifestyles. These combined efforts—LPA prevention and science education promotion—are vital to creating sustainable, long-term improvements in public health outcomes. Urgent action is required to mitigate the growing health challenges and ensure equitable access to resources that support healthier, more active populations.
Data availability
Data was publicly available from the Global Health Data Exchange website (http://ghdx.healthdata.org/gbdresults-tool) which provides a visualization tool to display and analyze the Global Burden of Disease data from the GBD 2021 study.
References
British Heart Foundation. Global heart & circulatory diseases factsheet. August (2022). https://www.bhf.org.uk/-/media/files/research/heart-statistics/bhf-cvd-statistics-global-fact sheet.pdf
US Preventive Services Task Force et al. Behavioral counseling interventions to promote a healthy diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: US preventive services task force recommendation statement. JAMA 324 (20), 2069–2075. https://doi.org/10.1001/jama.2020.21749 (2020).
Perry, A. S. et al. Physical activity over the lifecourse and cardiovascular disease. Circ. Res. 132 (12), 1725–1740. https://doi.org/10.1161/CIRCRESAHA.123.322121 (2023).
Katzmarzyk, P. T., Friedenreich, C., Shiroma, E. J. & Lee, I. M. Physical inactivity and non-communicable disease burden in low-income, middle-income and high-income countries. Br. J. Sports Med. 56 (2), 101–106. https://doi.org/10.1136/bjsports-2020-103640 (2022).
Guthold, R., Stevens, G. A., Riley, L. M. & Bull, F. C. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants [published correction appears in Lancet Glob Health. ;7(1):e36. doi: 10.1016/S2214-109X(18)30454-6]. Lancet Glob Health. 2018;6(10):e1077-e1086. (2019). https://doi.org/10.1016/S2214-109X(18)30357-7
Fletcher, G. F. et al. Promoting physical activity and exercise: JACC health promotion series. J. Am. Coll. Cardiol. 72 (14), 1622–1639. https://doi.org/10.1016/j.jacc.2018.08.2141 (2018).
Lee, I. M. et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. The Lancet, 380(9838), 219–229. 9. World Health Organization. (2018). Global action plan on physical activity 2018–2030: more active people for a healthier world. (2012). Retrieved from https://www.who.int/publications
World Health Organization. WHO guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 55 (3), 1–10. https://doi.org/10.1136/bjsports-2020-102955 (2020).
Tremblay, M. S. et al. Canadian 24-hour movement guidelines for adults aged 18–64 years and adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab. 45 (10), S57–S78. https://doi.org/10.1139/apnm-2020-0467 (2020).
Lu, Y. & Lan, T. Spatiotemporal trends of cardiovascular disease burden attributable to low physical activity during 1990–2019: an analysis of the global burden of disease study 2019. Public. Health. 228, 137–146. https://doi.org/10.1016/j.puhe.2024.01.008 (2024).
Luo, Y., Liu, J., Zeng, J. & Pan, H. Global burden of cardiovascular diseases attributed to low physical activity: an analysis of 204 countries and territories between 1990 and 2019. Am. J. Prev. Cardiol. 17, 100633 (2024). PMID: 38380078; PMCID: PMC10877163.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396 (10258), 1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9 (2020).
International Physical Activity Questionnaire (IPAQ) Group. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ). (2005). Retrieved from https://sites.google.com/site/theipaq/scoring-protocol
Global Physical Activity Questionnaire (GPAQ) Analysis Guide. World Health Organization. (2017). Retrieved from https://www.who.int/ncds/surveillance/steps/GPAQ_Analysis_Guide.pdf
GBD. methodology document (2021). https://www.healthdata.org/sites/default/files/methods_appendices/2021/lojustin_activity_writeup_gbd2020_AC_updated0131.pdf
Deng, Y. et al. Global burden of thyroid Cancer from 1990 to 2017. JAMA Netw. Open. 3 (6), e208759. https://doi.org/10.1001/jamanetworkopen.2020.8759 (2020). Published 2020 Jun 1.
de Lucena Alves, C. P., Crochemore-Silva, I., Lima, N. P., Coenen, P. & Horta, B. L. Prospective association of occupational and Leisure-Time physical activity with cardiovascular risk factors in early adulthood: findings from Pelotas (Brazil) 1982 birth cohort. J. Phys. Act. Health. 20 (9), 832–839. https://doi.org/10.1123/jpah.2022-0610 (2023). Published 2023 Jul 25.
Peeters, G., van Gellecum, Y. R., van Uffelen, J. G., Burton, N. W. & Brown, W. J. Contribution of house and garden work to the association between physical activity and well-being in young, mid-aged and older women. Br. J. Sports Med. 48 (12), 996–1001. https://doi.org/10.1136/bjsports-2012-091103 (2014).
Cheng, W. et al. Associations of leisure-time physical activity with cardiovascular mortality: A systematic review and meta-analysis of 44 prospective cohort studies. Eur. J. Prev. Cardiol. 25 (17), 1864–1872. https://doi.org/10.1177/2047487318795194 (2018).
Fontana, D., Ceron, R. & d’Errico, A. Occupational physical activity, all-cause mortality and incidence of cardiovascular diseases: results from three Italian cohorts. Int. Arch. Occup. Environ. Health. 97 (1), 81–100. https://doi.org/10.1007/s00420-023-02028-w (2024).
Wahid, A. et al. Quantifying the association between physical activity and cardiovascular disease and diabetes: A systematic review and Meta-Analysis. J. Am. Heart Assoc. 5 (9), e002495. https://doi.org/10.1161/JAHA.115.002495 (2016). Published 2016 Sep 14.
Acosta, S., Johansson, A. & Drake, I. Diet and lifestyle factors and risk of atherosclerotic cardiovascular Disease-A prospective cohort study. Nutrients 13 (11), 3822. https://doi.org/10.3390/nu13113822 (2021). Published 2021 Oct 27.
Khan, K. M. et al. Sport and exercise as contributors to the health of nations. Lancet 380 (9836), 59–64. https://doi.org/10.1016/S0140-6736(12)60865-4 (2012).
Holtermann, A. et al. The health paradox of occupational and leisure-time physical activity. Br. J. Sports Med. 55 (5), 235–236 (2021).
Smith, J. & Brown, A. Gender-specific risk factors for cardiovascular disease. J. Women’s Health. 29 (4), 123–130 (2020).
Lee, K. & Thompson, R. Global disparities in metabolic health: A comparative study. Int. J. Epidemiol. 48 (2), 456–467 (2019).
Zhang, L. & Martinez, D. Socioeconomic determinants of cardiovascular risk in developed and developing nations. Global Health Res. Policy. 6 (1), 89–102 (2021).
Saina, S., Senthil, P. & Prakash, O. Burden of illness, risk factor and physical activity in cardiovascular disease-A review[J]. Biomedicine 43 (4), 1080–1093 (2023).
Educational Status and Cardiovascular Risk Profile in Indians. Available online at: accessed July 25, (2022). https://pubmed.ncbi.nlm.nih.gov/17923677/ 25, 2022).
Njagi, P. et al. Financial costs of assisted reproductive technology for patients in low- and middle-income countries: a systematic review. Hum. Reprod. Open 2023(2):hoad007 (2023).
Alsaleh, E. & Baniyasin, F. Prevalence of physical activity levels and perceived benefits of and barriers to physical activity among Jordanian patients with coronary heart disease: A cross-sectional study. Front. Public. Health. 10, 1041428. https://doi.org/10.3389/fpubh.2022.1041428 (2023). Published 2023 Jan 4.
Institute for Health Metrics and Evaluation (IHME). GBD compare. Seattle, WA: IHME. University of Washington. (2015). available from http://vizhub.healthdata.org/gbd-compare. (Accessed [03/12/2022])).
Price, A. J. et al. Prevalence of obesity, hypertension, and diabetes, and cascade of care in sub-Saharan africa: a cross-sectional, population-based study in rural and urban Malawi. Lancet Diabetes Endocrinol. 6 (3), 208–222. https://doi.org/10.1016/S2213-8587(17)30432-1 (2018).
Tibazarwa, K. et al. A time bomb of cardiovascular risk factors in South africa: results from the heart of Soweto study heart awareness days. Int. J. Cardiol. 132 (2), 233–239. https://doi.org/10.1016/j.ijcard.2007.11.067 (2009).
UNAIDS & Global HIV & AIDS statistics — Fact sheet. (2023). Available from: https://www.unaids.org/en/resources/fact-sheet
Hsue, P. Y. & Deeks, S. G. HIV infection and cardiovascular disease: an update. Circul. Res. 129 (5), 561–576. https://doi.org/10.1161/CIRCRESAHA.121.318948 (2021).
Bloomfield, G. S. et al. Cardiovascular disease and cardiovascular risk factors in sub-Saharan africa: A systematic review. Global Heart. 15 (1), 1–14. https://doi.org/10.5334/gh.784 (2020).
Kazemi, A. et al. Leisure-time and occupational physical activity and risk of cardiovascular disease incidence: a systematic-review and dose-response meta-analysis of prospective cohort studies. Int. J. Behav. Nutr. Phys. Act. 21 (1), 45. https://doi.org/10.1186/s12966-024-01593-8 (2024). Published 2024 Apr 24.
Acknowledgements
We thank all authors for their contributions to the article.
Funding
This work was supported by the Key Technology R&D Program of Ningbo (2022Z149), Natural Science Foundation of Ningbo (No.2022J224), Funding of Natural Science Foundation of Ningbo (No.2024J296), partly funded by Key Laboratory of Precision Medicine for Atherosclerotic Diseases of Zhejiang Province, China (2022E10026) and Funding of the Plan of Science and Technology on Medical and Health in Zhejiang Province (No.2023KY1074) .
Author information
Authors and Affiliations
Contributions
Nan Wu and Jian Wang contributed to design of the study, Yingchu Hu and Tingsha Du contributed to data collection, Peng Shu contributed to analysis of the study, Caijie Shen and Xiaomin Chen write the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study is based on a publicly available database and does not require ethical approval.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Nan Wu and Jian Wang are co-first authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wu, N., Wang, J., Hu, Y. et al. Global burden of cardiovascular disease due to low physical activity, 1990–2021. Sci Rep 15, 25636 (2025). https://doi.org/10.1038/s41598-025-11329-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-11329-8