Abstract
Denture defects affect patients’ aesthetic appearance and masticatory function, thus reducing their quality of life. There are many ways to repair denture defects, among which removable partial dentures are a basic and widely used method. The purpose of this study was to compare the clinical performance of Bio-HPP and Vitallium frameworks in the restoration of free-end removable partial dentures. 80 patients with free-end removable partial dentures treated at the Stomatology Hospital of Xi’an jiaotong university from January 2022 to March 2023 were randomly divided into two groups. 40 patients in the control group received Vitallium frameworks and 40 patients in the observation group received Bio-HPP frameworks. The abutment tooth mobility, gingival index, and patient satisfaction after one year of restoration were compared and analyzed between the two groups using an Independent T-test. P < 0.05 was considered significant. All our experiments were carried out in accordance with relevant standards and regulations of Stomatology Hospital of Xi 'an Jiaotong University. After 1-year follow-up, in terms of aesthetics, comfort, and patient satisfaction, Bio-HPP was significantly superior to Vitallium frameworks, whereas the opposite was true for denture stability (P < 0.05). Besides, there were no significant differences in the mobility of abutment teeth and gingival index between Bio-HPP and Vitallium frameworks (P > 0.05). Both Bio-HPP and Vitallium frameworks can be used in restoring free-end removable partial dentures and the performance of the restorations was clinically acceptable. However, Bio-HPP has unique advantages in terms of aesthetics and comfort.
Similar content being viewed by others
Introduction
Dentition defect refer to the varying degrees of tooth loss in different segments of the upper or lower dentition, constituting a prevalent clinical condition. Multiple factors contribute to dental defects, notably caries, periodontitis, and dental trauma, ultimately resulting in tooth loosening and eventual loss. These defects significantly impact the patient’s chewing function, speech articulation, and aesthetic appearance1,2. Currently, various methods are employed for repairing dentition defect, including fixed bridge, implant, and removable partial dentures restoration (RPDs). For patients who do not meet the criteria for fixed bridge and implant restoration, RPDs frequently serve as the sole viable option3,4,5.
RPDs are a type of dental appliance that utilizes the remaining natural teeth, mucous membranes, and alveolar ridge as support and retention mechanisms, restoring the functionality of missing teeth through the use of artificial teeth6. These dentures can be categorized into Kennedy Class I, Kennedy Class II, Kennedy Class III and Kennedy Class IV based on the Kennedy classification7. Given the varying strengths, hardness, and toughness of denture materials, dental researchers have conducted extensive studies to evaluate the restoration effects of each material8. Traditionally, cobalt–chromium (Co–Cr) alloys has been the primary material used for denture frameworks. However, with advancements in materials science, newer options such as Bego Partial Denture (BPD) perfect stand, Vitallium, and pure titanium denture frameworks have emerged9. Some studies comparing Vitallium with pure titanium and Co–Cr alloy in clinical analysis have found that Vitallium RPDs achieve higher overall satisfaction. The reason is that Co–Cr alloy have relatively lower elasticity, resulting in poorer comfort, while pure titanium RPDs are prone to breakage due to manufacturing defects. However, the drawback of Vitallium RPDs is that they are heavier and have poor biocompatibility compared to pure titanium frameworks10.
Therefore, researchers discovered a new type of material for dental restoration. Polyetheretherketone (PEEK) is a polymeric thermoplastic material that a polymer with excellent biological and mechanical performance and an elastic modulus close to the bone11. PEEK mixed with carbon fiber (PEEKc) shows a high toughness, strength, and chemical resistance12. Besides, PEEK with glass fiber (PEEKg) can improve the tensile modulus and strength by 75%13. Unlike metals, PEEK has biocompatibility and a naturally tooth-colored appearance. Therefore, PEEK is widely used in fixed prostheses, implants, provisional abutments, maxillary obturator prostheses, and RPDs. In addition to being shock-absorbing during mastication, PEEK frameworks provide significant resistance to degradation and abrasion. Despite the considerable strength of metals, resilience, and patient comfort are also major concerns14,15,16,17,18,19.
In recent years a new type of material called Polyether Ether Ketone-Based Ceramic-Reinforced High-Performance Polymer (Bio-HPP) has emerged. It is an enhanced PEEK with 20% ceramic molecules of aluminum oxide and zirconia oxide nanoparticles which has a high-performance polymer possessing good elasticity, chemical resistance, thermal stability, mechanical properties, and biocompatibility20,21. According to studies by Tannous et al., indicated that high-quality prostheses are produced using Bio-HPP due to their correctability, ideal polishing ability, good stability, and aesthetics. For patients with high aesthetic demands, Bio-HPP has immense potential as a framework material and is a promising alternative to Cr-Co frameworks. To date, not many studies have been done to understand the clinical performance of Bio-HPP in the field of dentistry, particularly in the construction of denture frameworks for dental restoration22,23. And there are few studies comparing Bio-HPP with Vitallium RPDs. Consequently, it is necessary to conduct randomized clinical trials to compare and evaluate the clinical success of Bio-HPP and Vitallium. Therefore, the purpose of this study is to compare the clinical effects of two highly elastic scaffolds, Bio-HPP and Vitallium to assess their performance in free-end RPDs. Preliminary results of this study revealed that both the Bio-HPP and Vitallium RPDs can be clinically acceptable, however in terms of aesthetics and comfort, Bio-HPP has greater advantages over Vitallium RPDs. The null hypothesis of this study is that the overall satisfaction with Bio-HPP RPDs is higher than that of Vitallium RPDs.
Materials and methods
Study design
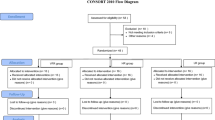
The denture materials used in this study are listed in Table 1. The sample size was calculated using the G-Power statistical software and also in the present research24, the requisite sample size was 40 for each group. A total of 80 patients (aged between 42 and 70 years; a mean age of 60 ± 5 years; 44 men, 36 women) with free-end dentition defects, were admitted to the stomatological hospital of Xi’an Jiaotong University between January 2022 and March 2023, were randomly assigned to receive either Bio-HPP or Vitallium dentures by using randomization software (www. Randomizer.org). Forty patients received Bio-HPP RPDs and forty received Vitallium RPDs. All dentures were designed by two operators with more than 10 years of experience. The processing plant of the denture used in this article is Shanxi Lianmei denture technology. All our experiments were carried out in accordance with the relevant standards and regulations of the Stomatology Hospital of Xi 'a Jiaotong University. This study was approved by the hospital Medical Ethics Committee (ethics approval number XJKQIEC-030-002). Informed consent was obtained from all subjects or their legal guardian(s).
Patient recruitment
The inclusion criteria for the study were as follows: (1) Patients exhibiting dentition defects with missing free ends (Kennedy Class I or Kennedy Class II) and abutment loosening of ≤II degree; (2) Abutment teeth devoid of caries or fillings; (3) Alveolar bone absorption in the abutment area not exceeding half of the root length; (4) Good oral hygiene practices or periodontitis that has been effectively managed; (5) Patients providing informed consent. Conversely, the exclusion criteria encompassed: (1) Patients with allergies to stent materials; (2) The presence of oral mucosal diseases; and (3) the Inability to wear dentures independently and maintain regular clinic visits. All dentures were designed and partially fabricated by the same clinician, with the remaining processing handled by a consistent technician.
Clinical procedures
Two clinicians with more than 10 years of clinical experience in prosthetic dentistry. (1) Prior to the repair process, a thorough oral examination is conducted to evaluate the condition of the remaining teeth and administer necessary dental and periodontal treatments. (2) Subsequently, digital impression and model creation are undertaken. This involves selecting appropriate abutments and preparing the teeth by removing excessive concavities, lacunar grooves, and support pits. The 3shape digital intraoral scanner is employed to capture intraoral impressions, which are then used to print models, fabricate individual trays, and obtain precise impressions for subsequent denture design. (3) The relationship between the jaw and its position is then determined. (4) Following this, the model design and processing phase commences. (5) A base wax pattern is crafted. (6) The denture support is then cast. (7) Wax teeth are formed and positioned. (8) The oral support is tried in for fit and comfort. (9) The denture undergoes embedding, heat treatment, grinding, and polishing to achieve the desired finish. (10) Finally, a dental and clinical index examination is performed to ensure the quality and functionality of the denture.
Clinical evaluation
Two independent prosthodontists with more than 10 years of clinical experience performed the evaluation of restorations which was mentioned in other articles25,26. Evaluations were performed before the restorative procedures as baseline and at 1 year according to the modified FDI (World Dental Federation) criteria as following aspects16: (1) Abutment Loosening Degree: The assessment encompassed three degrees of loosening. Degree I entailed buccolingual loosening only. Degree II was characterized by both buccolingual loosening alongside proximal and distal loosening. Lastly, Degree III comprised buccolingual, proximal-distal, and vertical loosening. (2) Gingival index: This index only looks at the gingival condition, checking the color and quality of the gingival change, as well as bleeding tendency. The score was 0= gum health; 1= mild gingival inflammation: the gingival color has a slight change and edema, no bleeding; 2= moderate gingival inflammation: red gingival color, edema bright, probing bleeding; 3= Severe inflammation of the gums: the gums are obviously red, swollen or ulcerated, and spontaneous bleeding. (3) Patient satisfaction: The two groups of patients were investigated in terms of denture comfort, aesthetics, chewing and language function. Language function includes (1) Pronunciation Clarity: Patients may feel discomfort and mild difficulty in pronunciation initially due to the new denture. This is mainly because the base may cover part of the oral mucosa, affecting tongue movement. Unnatural actions may also impact pronunciation. (2) Speech Fluency: Patients may feel unfluent initially. This is due to the need to adapt pronunciation. (3) Impact on Language Understanding: Dentures usually don’t directly affect understanding. However, pronunciation difficulties may indirectly affect communication, so accuracy and clarity are crucial. Satisfied (+), not satisfied (-).
Statistical analysis
The statistical analysis of the data was conducted using IBM SPSS version 26.0, adhering to rigorous academic standards. The counting data were presented in the form of the number of cases, accompanied by percentages, and subjected to the Chi-square test for statistical evaluation. On the other hand, the measurement data were expressed as the mean value ± standard deviation (x±s) and analyzed using the two independent samples T-test. Statistical significance was set at P < 0.05, indicating that any observed differences with this threshold were considered to be statistically meaningful.
Results
The clinical comparison photographs of the two groups of RPDs, pre- and post-restoration, are presented respectively in Figs. 1 and 2. These images provide a visual representation of the RPDs’ condition before and after the restoration process, allowing for a direct comparison of their initial and final states. Upon thorough analysis of the data, it becomes evident that no statistically significant difference was observed in the levels of abutment looseness and gingival index between the Bio-HPP and Vitallium RPDs one-year following implantation (P > 0.05), as detailed in Tables 2 and 3. This finding suggests that both stent types maintain comparable levels of stability and gingival health over time.
In terms of patient satisfaction, a more nuanced comparison reveals that the Bio-HPP RPD emerged as the preferred option (P < 0.05). Patients reported superior performance in both comfort and aesthetics when compared to the Vitallium group as outlined in Table 4 (P < 0.05). Interestingly, the two groups showed opposite results in terms of denture stability, with Vitallium being more stable than Bio-HPP (P < 0.05). However, when comparing the two groups in terms of pronunciation clarity, no discernible differences were identified (P > 0.05).
Discussion
The present study aimed to compare RPDs with different materials, one of which was a modified PEEK(Bio-HPP) and the other was the Vitallium material. The null hypothesis of this study is that the overall satisfaction with Bio-HPP RPDs is higher than that of Vitallium RPDs. The clinical success of PEEK has been tested in clinical studies comparing these materials with cobalt-chromium alloy (Co–Cr), which indicated that compared with the Co–Cr clasp, the PEEK clasp underwent less fatigue deformation, which makes it feasible for clinical applications27,28. However, there is no study evaluating the clinical performance of Bio-HPP and Vitallium RPDs.
The main components of Vitallium are 60% cobalt, 28% ~ 32% chromium, 5% ~ 7% molybdenum and 1% manganese and silicon. Notably, the enhanced molybdenum content imparts superior toughness and elasticity to this alloy material. Lots of studies have shown that Vitallium scaffolds exhibit superior corrosion resistance and excellent mechanical properties compared to conventional cobalt-chromium alloys. Several studies have demonstrated that the Vitallium stress-interrupt design concept can diminish alveolar bone resorption in free-end abutment teeth, thereby offering significant clinical value29,30. However, the biocompatibility of Vitallium is poor, and there are some defects such as allergy and easy corrosion. In contrast, Bio-HPP, as a new material, shows significant advantages in the application of dentures.
Bio-HPP represents a refined version of PEEK material, a semi-crystalline, thermoplastic, ceramic-reinforced, high-performance polymer that boasts remarkable hardness, surface polish, and elasticity. Bio-HPP has been applied in clinical practice for the processing of fixed dentures, removable dentures and implant abutments28,31. For example, Zoidis P has reported that the clinical use of a Bio-HPP RDP framework is presented as an alternative for the treatment of a distal extension case32. Bio-HPP is more advantageous for being anti-allergic in nature, excellent polishing properties, non-metallic in taste, low plaque affinity and good wear resistance. When combined with conventional acrylic dentures and denture base materials, it can also serve as an alternative material for RPD framework applications33,34,35.
Rauch et al. demonstrated that PEEK fixed partial dentures (FPDs) exhibit significantly shorter manufacturing time and lower material weight compared to zirconia-based restorations in clinical applications. While acknowledging that zirconia demonstrates superior aesthetic outcomes relative to veneered PEEK prostheses, the authors noted that both materials meet clinically acceptable aesthetic standards36,37. In the field of dental implantology, comparative studies of three implant material assemblies—carbon fiber-reinforced PEEK, zirconia, and titanium—showed no statistically significant differences in biomechanical performance or osseointegration potential. Notably, clinical trials involving PEEK implants have reported no implant failure rates, suggesting promising biocompatibility characteristics38,39,40.
In this study, Bio-HPP with its low specific weight can be used to construct extremely lightweight prostheses, offering high patient satisfaction and comfort which showed similar results with other studies11,41,42. Our findings revealed there is no statistically significant differences in gingival index or abutment loosening between the two materials with one-year following up. This may be due to the fact that this study was limited to observational cases and a short investigation period. Therefore, the long-term efficacy of Bio-HPP in making removable local dentures needs to be further studied. Some factors representing inflammatory response in the gingival crevicular fluid can be detected, which will provide better clinical guidance.
Nevertheless, it is noteworthy that despite the absence of statistical significance, we observed that in one patient with multiple missing free ends repaired using Bio-HPP, the abutment transitioned from a non-loose state to a degree of III looseness. This observation may be attributed to the heightened elasticity of Bio-HPP, which, in the case of concave abutments, can exert a substantial force during denture removal. Consequently, to balance the elasticity and retaining force of the denture, modifications to the abutment concavity and augmentation of the Bio-HPP clasp thickness are recommended to optimize patient outcomes.
In terms of patient satisfaction, the findings of this study showed that Bio-HPP RPDs were significantly better than Vitallium RPDs in aesthetics and comfort. This advantage stems from the fact that Bio-HPP exhibits a significantly lighter weight compared to Vitallium, and its opalescent color is more aesthetically pleasing to patients with anterior tooth restoration. Furthermore, the utilization of CAD/CAM cutting technology in the fabrication of Bio-HPP brackets has resulted in enhanced adhesion, surpassing the traditional manufacturing process employed for Vitallium processing. Despite these positive attributes, it is noteworthy that four patients with Bio-HPP RPDs expressed dissatisfaction with the aesthetics. Upon investigation, it was discovered that Bio-HPP materials were easy to stain by the presence of tea or coffee on the surface. Consequently, meticulous selection of Bio-HPP materials for these patients is imperative.
In terms of denture stability, Vitallium RPDs demonstrated a statistically significant higher stability than Bio-HPP RPDs. This disparity can be attributed to the high elasticity of Bio-HPP, which renders it less stable during mastication, particularly in large stents with missing free ends, such as those with double free-end spans. Clinically, we can improve the stability by modifying the abutment shape, increasing the thickness of the Bio-HPP clasp and the depth of entering the concave, and increasing its retaining force, which is sufficient to meet the clinical use of Bio-HPP. Furthermore, advanced Bio-HPP framework modifications including double rest design with lingual bracing arm, major connector thickness optimization, and T-Scan computerized occlusal analysis implementation for support fossae morphology refinement and lateral force minimization, along with biomimetic hybrid material combinations, present viable solutions for achieving optimal stability parameters in Bio-HPP prosthodontic applications43,44,45.
With the limitation of the study, it would be possible to increase the sample size and extend the duration of clinical follow-up. Evaluations of Bio-HPP RPDs based on factors such as Kennedy classification and denture design will be considered for further study, in order to provide evidence for the widespread clinical use of Bio-HPP materials.
Conclusion
Bio-HPP and Vitallium frameworks can be used in restoring free-end RPDs and the performance of the restorations was clinically acceptable. However, Bio-HPP shows unique advantages in aesthetics and comfort. In addition, the application of Bio-HPP in the field of stomatology requires further study in clinical practice to determine its feasibility and long-term performance. These studies will help promote the deeper application of Bio-HPP in the field of oral medicine, so as to bring more breakthroughs in oral clinical treatment.
Patient consent statement
We have been fully informed about the nature and purpose of the study in which we are participating. We understand that my personal information and any related images may be used in a scientific publication by the researchers. We consent to the use of our data and images for the stated purposes, and we are aware that this consent is irrevocable once the material has been published. We also confirm that we have been treated with respect throughout the process and that our privacy has been protected in accordance with the relevant laws and regulations.
Data availability
The datasets used or analysed during the current study available from the corresponding author on reasonable request.
References
Kurosaka, H. et al. Development of dentition: From initiation to occlusion and related diseases. J. Oral Biosci. 64(2), 159–164. https://doi.org/10.1016/j.job.2022.02.005 (2022).
Brook, A. H., Jernvall, J., Smith, R. N., Hughes, T. E. & Townsend, G. C. The dentition: The outcomes of morphogenesis leading to variations of tooth number, size and shape. Aust. Dent. J. 59(Suppl 1), 131–142. https://doi.org/10.1111/adj.12160 (2014).
Peng, K. et al. The effect of denture restoration and dental implant restoration in the treatment of dentition defect: A systematic review and meta-analysis. Ann. Palliat. Med. 10(3), 3267–3276. https://doi.org/10.21037/apm-21-421 (2021) (PMID: 33849111).
Saeed, F. et al. Prosthodontics dental materials: From conventional to unconventional. Mater. Sci. Eng. C Mater. Biol. Appl. 106, 110167. https://doi.org/10.1016/j.msec.2019.110167 (2020) (Epub 2019 Sep 7. PMID: 31753414).
Tavelli, L., Barootchi, S., Rasperini, G. & Giannobile, W. V. Clinical and patient-reported outcomes of tissue engineering strategies for periodontal and peri-implant reconstruction. Periodontol 2000 91(1), 217–269. https://doi.org/10.1111/prd.12446 (2023).
Patel, J., Jablonski, R. Y. & Hodson, T. M. Removable partial dentures: Part 1. Br. Dent. J. 237(7), 537–542. https://doi.org/10.1038/s41415-024-7893-7 (2024) (Epub 2024 Oct 11. PMID: 39394297).
Pun, D. K., Waliszewski, M. P., Waliszewski, K. J. & Berzins, D. Survey of partial removable dental prosthesis (partial RDP) types in a distinct patient population. J. Prosthet. Dent. 106(1), 48–56. https://doi.org/10.1016/S0022-3913(11)60093-0 (2011) (PMID: 21723993).
Melo Neto, C. L. M., Turcio, K. H., Dos Santos, D. M. & Goiato, M. C. Removable partial denture—Functional impression techniques: Review. Prague Med. Rep. 124(4), 380–391. https://doi.org/10.14712/23362936.2023.29 (2023) (PMID: 38069644).
Sun, B., Wang, Y. Q., Xu, Y., Shi, P. & Zhou, Q. Clinical study of Vitallium removable partial denture with dual major connector in Kennedy I and II dentition defect. Shanghai Kou Qiang Yi Xue. 27(5), 518–521 (2018) (Chinese. PMID: 30680398).
Gao, S. & Miao, Y. Comparative Study on cast support of Vitallium 2000, Pure Titanium and Diamond Chromium Alloy. Dis. Surveill. Control 9(11), 775–776 (2015).
Bathala, L., Majeti, V., Rachuri, N., Singh, N. & Gedela, S. The role of polyether ether ketone (Peek) in dentistry—A review. J. Med. Life 12(1), 5–9. https://doi.org/10.25122/jml-2019-0003 (2019).
Khan, H. A. et al. Carbon fiber-reinforced PEEK spinal implants for primary and metastatic spine tumors: A systematic review on implant complications and radiotherapy benefits. J. Neurosurg. Spine 39(4), 534–547. https://doi.org/10.3171/2023.5.SPINE23106 (2023).
Zhang, R., Chen, L., Xie, K., Liu, K. & Wu, Z. Compression properties and constitutive model of short glass fiber reinforced poly-ether-ether-ketone (PEEK). Sci. Rep. 13(1), 19206. https://doi.org/10.1038/s41598-023-46078-z (2023).
Abdulfattah, N. et al. Ultrasonic welding of polyetheretherketone for dental applications. J. Mech. Behav. Biomed. Mater. 130, 105225. https://doi.org/10.1016/j.jmbbm.2022.105225 (2022) (Epub 2022 Apr 5 PMID: 35405522).
Zheng, J., Aarts, J. M., Ma, S., Waddell, J. N. & Choi, J. J. E. Fatigue behavior of removable partial denture cast and laser-sintered cobalt-chromium (CoCr) and polyetheretherketone (PEEK) clasp materials. Clin. Exp. Dent. Res. 8(6), 1496–1504. https://doi.org/10.1002/cre2.645 (2022) (Epub 2022 Aug 8. PMID: 35938907; PMCID: PMC9760146).
Wang, B. et al. PEEK in fixed dental prostheses: Application and adhesion improvement. Polymers (Basel) 14(12), 2323. https://doi.org/10.3390/polym14122323 (2022).
Elashmawy, Y., Aboushelib, M. & Elshahawy, W. Retention of different CAD/CAM endocrowns bonded to severely damaged endodontically treated teeth: An in vitro study. J. Indian Prosthodont. Soc. 21(3), 269–275. https://doi.org/10.4103/jips.jips_91_21 (2021).
Roy, M. et al. Photofunctionalization effect and biological ageing of PEEK, TiO2 and ZrO2 abutments material. Mater. Sci. Eng. C Mater. Biol. Appl. 121, 111823. https://doi.org/10.1016/j.msec.2020.111823 (2021).
Papathanasiou, I., Kamposiora, P., Papavasiliou, G. & Ferrari, M. The use of PEEK in digital prosthodontics: A narrative review. BMC Oral Health 20(1), 217. https://doi.org/10.1186/s12903-020-01202-7 (2020) (PMID: 32741366; PMCID: PMC7398079).
de Almeida, M. V. R. et al. Dental implant and abutment in PEEK: Stress assessment in single crown retainers on anterior region. Clin. Oral Investig. 28(6), 336. https://doi.org/10.1007/s00784-024-05722-2 (2024).
Guo, L. et al. Attachment and osteogenic potential of dental pulp stem cells on non-thermal plasma and UV light treated titanium, zirconia and modified PEEK surfaces. Materials 15(6), 22–25. https://doi.org/10.3390/ma15062225 (2022).
Au, A. R., Lechner, S. K., Thomas, C. J., Mori, T. & Chung, P. Titanium for removable partial dentures (III): 2-year clinical follow-up in an undergraduate programme. J. Oral Rehabil. 27(11), 979–985. https://doi.org/10.1046/j.1365-2842.2000.00576.x (2000) (PMID: 11106989).
Paul, S. M., Anitha, K. V. & Balasubramaniam, M. Effect of different agents on preload force of dental implants with bio high-performance poly-ether-ether-ketone abutments. J. Oral Biol. Craniofac. Res. 14(6), 756–760. https://doi.org/10.1016/j.jobcr.2024.10.004 (2024) (Epub 2024 Oct 17).
Luo, C. et al. PEEK for oral applications: Recent advances in mechanical and adhesive properties. Polymers 15(2), 386. https://doi.org/10.3390/polym15020386 (2023).
Hobbi, P. et al. Clinical performance of 3D printed resin composite posterior fixed dental prosthesis: A permanent solution?. Eur. J. Prosthodont. Restor. Dent. https://doi.org/10.1922/EJPRD_2796Hobbi10 (2024) (Epub ahead of print. PMID: 39535404).
Hickel, R. et al. FDI world dental federation: Clinical criteria for the evaluation of direct and indirect restorations—Update and clinical examples. Clin. Oral Investig. 14, 349–366. https://doi.org/10.1007/s00784-010-0432-8 (2010).
Wu, S., Qian, C., Jiao, T. & Sun, J. Comparison of the retention and fit of polyether ether ketone clasps during fatigue circulation tests. Heliyon 9(9), e19959. https://doi.org/10.1016/j.heliyon.2023.e19959 (2023) (PMID: 37809567).
Vaddamanu, S. K. et al. Retentive forces and deformation of fitting surface in RPD clasp made of polyether-ether-ketone (PEEK). Polymers (Basel) 15(4), 956. https://doi.org/10.3390/polym15040956 (2023) (PMID: 36850239).
Kurokawa, H., Takamizawa, T., Rikuta, A., Tsubota, K. & Miyazaki, M. Three-year clinical evaluation of posterior composite restorations placed with a single-step selfetch adhesive. J. Oral Sci. 57, 101–108. https://doi.org/10.2334/josnusd.57.101 (2015).
Sadek, S. A. & Elawady, D. Impact of removable partial denture type on patient satisfaction and abutment survival rate-RCT. Open Access Maced. J. Med. Sci. 7(15), 2513–2519. https://doi.org/10.3889/oamjms.2019.668 (2019).
Qian, C., Wu, X., Zhang, F. & Yu, W. Electrochemical impedance investigation of Ni-free Co-Cr-Mo and Co-Cr-Mo-Ni dental casting alloy for partial removable dental prosthesis frameworks. J. Prosthet. Dent. 116(1), 112–118. https://doi.org/10.1016/j.prosdent.2015.12.001 (2016).
Zoidis, P. & Papathanasiou, I. Modified PEEK resin-bonded fixed dental prosthesis as an interim restoration after implant placement. J. Prosthet. Dent. 116(5), 637–641. https://doi.org/10.1016/j.prosdent.2016.04.024 (2016).
Parate, K. P., Naranje, N., Vishnani, R. & Paul, P. Polyetheretherketone material in dentistry. Cureus 15(10), e46485. https://doi.org/10.7759/cureus.46485 (2023) (PMID: 37927628; PMCID: PMC10624419).
Zol, S. M. et al. Description of poly(aryl-ether-ketone) materials (PAEKs), polyetheretherketone (PEEK) and polyetherketoneketone (PEKK) for application as a dental material: A materials science review. Polymers (Basel) 15(9), 2170. https://doi.org/10.3390/polym15092170 (2023) (PMID: 37177316; PMCID: PMC10180673).
Zhao, K., Wu, S., Qian, C. & Sun, J. Suitability and trueness of the removable partial denture framework fabricating by polyether ether ketone with CAD-CAM technology. Polymers 16, 1119. https://doi.org/10.3390/polym16081119 (2024).
Tanner, J. et al. Zirconia single crowns and multiple-unit FDPs-An up to 8-year retrospective clinical study. J. Dent. 79, 96–101. https://doi.org/10.1016/j.jdent.2018.10.012 (2018).
Ahmad, F., Nimonkar, S., Belkhode, V. et al. Role of polyetheretherketone in prosthodontics: A literature review. Cureus. 16(5) (2024).
Mahalakshmi, G., Gasthi, A., Hosain Almansour, H. M., Babaji, P., Madhusudhana Rao, U., Haseeb, S. A. & Venkata Ramaiah, V. Evaluation of stress and deformation in bone with titanium, CFR-PEEK and zirconia ceramic implants by finite element analysis. Dent. Res. J. (Isfahan). 20–57 (2023).
Zhang, Y., Zhang, W., Yang, M. et al. Comprehensive review of polyetheretherketone use in dentistry. J. Prosthodont. Res. JPR_D_24_00142 (2025).
Mishra, S. K., Bhasmey, S. R. & Chowdhary, R. Complete-arch implant-supported fixed dental prostheses fabricated with PEEK and PEKK framework: A systematic review. Evid. Based Dent. 24, 193. https://doi.org/10.1038/s41432-02300928-x (2023).
Alexakou, E. et al. PEEK high performance polymers: A review of properties and clinical applications in prosthodontics and restorative dentistry. Eur. J. Prosthodont. Restor. Dent. 27(3), 113–121. https://doi.org/10.1922/EJPRD_01892Zoidis09 (2019) (PMID: 31433133).
Zoidis, P., Papathanasiou, I. & Polyzois, G. The use of a modified poly-ether-ether-ketone (PEEK) as an alternative framework material for removable dental prostheses. A clinical report. J. Prosthodont. 25(7), 580–584. https://doi.org/10.1111/jopr.12325 (2016).
Vaddamanu, S. K. et al. Retentive forces and deformation of fitting surface in RPD clasp made of polyether-ether-ketone (PEEK). Polymers (Basel) 15, 956. https://doi.org/10.3390/polym15040956 (2023) (PMID:36850239).
Hussein, M. Biomechanical pPerformance of PEEK and graphene-modified PMMA as telescopic removable partial denture materials: A nonlinear 3D f inite element analysis. Int. J. Prosthodont. 35, 793–800. https://doi.org/10.11607/ijp.8177 (2022) (PMID:36125879).
Ding, L., Lu, W., Zhang, J., Yang, C. & Wu, G. Preparation and performance evalua tion of duotone 3D-printed polyetheretherketone as oral prosthetic mate rials: A proof-of-concept study. Polymers (Basel) 13, 1949. https://doi.org/10.3390/polym13121949 (2021) (PMID:34208259).
Acknowledgements
This work was supported by grants from the Natural Science Basic Research Program of Shaanxi (Program No. 2024JC-YBQN-0969)
Funding
This work was supported by grants from the Natural Science Basic Research Program of Shaanxi (Program No. 2024JC-YBQN-0969).
Author information
Authors and Affiliations
Contributions
TongZhai, Mengting Li, Yu Zhen and Zhenzhen Wang contributed to the conceptualization of this work. All the authors made substantial intellectual contributions to refining, finalizing, and approving the manuscript for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhai, T., Li, M., Zheng, Y. et al. Evaluate the clinical performance of Bio-HPP and Vitallium frameworks in free-end removable partial dentures. Sci Rep 15, 28777 (2025). https://doi.org/10.1038/s41598-025-11370-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-11370-7