Abstract
This study aimed to assess the knowledge, attitudes, and practices (KAP) of patients with chronic obstructive pulmonary disease (COPD) regarding inhalation devices. A cross-sectional survey was conducted at Chongqing Hospital of Traditional Chinese Medicine from January to April 2024 among patients with COPD who had been using inhaled medications for at least one month, using a structured questionnaire. Inhaler adherence was evaluated with the Test of Adherence to Inhalers (TAI). A total of 518 COPD patients were enrolled. The average scores for knowledge, attitude, practice, and TAI were 22.82 ± 3.24, 51.79 ± 6.61, 33.08 ± 5.58, and 35.12 ± 11.01, respectively. Correlation analysis demonstrated significant positive relationships between knowledge and attitude (r = 0.490), knowledge and practice (r = 0.368), and knowledge and TAI scores (r = 0.118). Additionally, significant correlations were noted between attitude and practice (r = 0.602) and attitude and TAI scores (r = 0.310). The analysis showed that knowledge directly influenced both attitude and practice and indirectly affected practice through attitude. This study revealed that although COPD patients had adequate knowledge and positive attitude towards inhaler use, their adherence was poor. Tailored educational interventions are recommended to improve adherence to inhalation therapy.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a prevalent obstructive lung condition characterized by respiratory difficulties and airflow obstruction, primarily presenting as shortness of breath and expectoration1,2. It is primarily caused by cigarette smoking, air pollution, and dust exposure3 and has emerged as a critical public health challenge in China, where it is now the third leading cause of death4. Epidemiological studies reported a prevalence rate of 8.6% in 2015, affecting approximately 9.99 million individuals in China5.
Inhalation therapy is a cornerstone in the treatment of COPD. This modality requires only a fraction of the oral dose to elicit a therapeutic response, acts more quickly, and has fewer side effects than oral medications. Healthcare providers, including physicians, nurse assistants, and pharmacists, typically instruct patients on the proper use of inhaler devices. Correct utilization of these devices is crucial for successful treatment outcomes, as proper use at home without supervision significantly impacts COPD symptom scores and quality of life6,7.
Despite the availability of various treatments, COPD is often under-treated, which may be partially due to improper use of inhalers8. This misuse can lead to serious errors, limiting the dosage of medication delivered to the airways and consequently resulting in inadequate treatment. Even if patients adhere to prescribed treatment regimes, these errors can prevent them from achieving an adequate clinical response9. For instance, a study found that nearly half (45%) of patients had committed at least one error in using their inhalers, with 50% of these errors related to the device and 31% to inhalation technique10.
The Knowledge, Attitude, and Practice (KAP) model posits that individual behaviors are largely influenced by one’s knowledge and attitudes. In public health, this model is crucial for elucidating health-related behaviors, with behavioral practices often assessed alongside knowledge and risk perception through KAP surveys11,12,13,14,15. Understanding these components is particularly vital in conditions like COPD, where the correct use of inhalation devices is essential not only for effective treatment outcomes but also for significantly improving the quality of life of the patients. Although several studies have examined the knowledge and inhalation techniques of COPD patients16,17,18, comprehensive KAP studies remain limited, particularly among Chinese COPD patients. Addressing these gaps, this study aims to assess the knowledge, attitudes, and practices of COPD patients in China regarding inhalation device use.
Methods
Study design and patients
This cross-sectional observational study was conducted at the Chongqing Hospital of Traditional Chinese Medicine from January 28, 2024, to April 22, 2024. It targeted patients diagnosed with COPD19. The study was approved by the Ethics Committee of the Chongqing Hospital of Traditional Chinese Medicine (Approval No. 2024-IIT-KS-2), and informed consent was secured from all participants prior to their inclusion. All procedures were conducted in accordance with the ethical standards of the institutional research committee and with the principles outlined in the Declaration of Helsinki.
Inclusion Criteria: (1) Patients aged 18 years or older; (2) Patients who have been using inhaled medications for at least one month; (3) Patients with basic literacy skills and no communication barriers; (4) Patients who voluntarily agree to participate in the study. Patients were excluded if they had severe conditions involving the heart, brain, liver, kidneys, nervous system, mental health disorders, blood disorders, or malignancies.
Questionnaire
The questionnaire was developed with reference to the Chinese Expert Consensus on the Standard Application of Inhalation Devices in Stable Chronic Airway Disease Patients20, as well as previous literature16,17,18. Then, the questionnaire was submitted to a panel of 5 experts for review, including four respiratory medicine specialists and one statistician. A pilot study was conducted among 30 participants, yielding an overall Cronbach’s α value of 0.922, which indicated good internal consistency. During the pilot study, patients were encouraged to provide feedback on any items they found confusing or unclear, and no items were reported, thus confirming face validity.
The questionnaire was designed to evaluate participants across five dimensions and was presented in Chinese (Additional file 1. Questionnaire). The basic information section included 21 questions, such as gender, height, body weight, ethnicity, residence, education level, employment status, income level, marital status, medical insurance coverage, smoking history, duration of COPD, frequency of acute exacerbations, comorbidities, stage of COPD, pulmonary function assessment, current inhalation therapy, and the use of traditional Chinese medicine for COPD. The pulmonary function assessment was evaluated using the Global Initiative for Chronic Obstructive Lung Disease (GOLD) staging19. The severity of breathlessness was assessed using the modified Medical Research Council (mMRC) dyspnea scale21. The Body Mass Index (BMI) is calculated as the weight in kilograms divided by the square of the height in meters, with classifications of < 18.5 kg/m² as underweight, 18.5–23.9 kg/m² as normal weight, 24–27.9 kg/m² as overweight, and ≥ 28 kg/m² as obesity22.
The knowledge dimension included 16 items, with scoring options designed to reflect the accuracy of respondents’ understanding (e.g., correct answers were scored as 2 points, incorrect answers as 0 points, and “unfamiliar” responses as 1 point, with a total score ranging from 0 to 32 points). The attitude dimension consisted of 14 questions evaluated on a 5-point Likert scale, ranging from “strongly agree” (5 points) to “strongly disagree” (1 point), with total scores ranging from 14 to 70 points. The practice dimension comprised 8 items, also using a 5-point scale to assess the practical application of knowledge and attitudes in disease management, with scores ranging from 8 to 40 points. Adequate knowledge, positive attitudes, and proactive practices were defined as scoring above 70% of the maximum possible points in each respective dimension according to previous KAP studies23,24,25. Finally, inhaler adherence was assessed using the Test of Adherence to Inhalers (TAI)26. This scale employs a 5-point Likert scoring system, where 1 indicates “always” and 5 indicates “never.” A total score of ≤ 45 indicates low adherence, 46–49 represents medium adherence, and a score of 50 reflects high adherence.
Questionnaire distribution and quality control
An online questionnaire was created using the Wenjuanxing platform (https://www.wjx.cn/) and distributed through a QR code generated via WeChat for data collection. The QR code for the survey was provided to patients in the COPD outpatient clinic of our hospital. Participants scanned the QR code to access and complete the questionnaire. Participants accessed the questionnaire via a QR code, and study-related information—including objectives, anonymity, and data confidentiality—was displayed on the first page. Only those who confirmed informed and voluntary participation could proceed. Responses from those who declined were not recorded. To ensure the quality and completeness of the responses, each IP address was allowed only one submission, and all questions were mandatory. Trained research assistants explained the study’s purpose to participants and addressed any reported concerns without influencing their responses. Pulmonary function assessment and breathlessness severity were completed by members of the research team after reviewing the patients’ medical records to assist in providing accurate responses. Upon collection, data quality checks were conducted; questionnaires completed in less than 2 min, containing logical errors, or exhibiting repetitive answer patterns were considered invalid and excluded. All responses were reviewed by members of the research team for completeness, consistency, and validity.
Sample size
The minimum sample size was calculated based on a guideline recommending 10 times the number of demographic and KAP items for surveys27. Thus, considering a total of 38 items in the KAP dimensions, the required sample size was 380. To account for an estimated 20% of invalid questionnaires, the final required sample size was adjusted to 456.
Statistical analysis
Data analysis was conducted using SPSS 22.0 (IBM, Armonk, NY, USA). The internal consistency of the questionnaire was assessed by calculating Cronbach’s α coefficient. The Kolmogorov-Smirnov test was used to assess the normality of continuous data. Variables following a normal distribution were reported as means ± standard deviations (SD) and analyzed with Student’s t-test or ANOVA. For non-normally distributed data, medians (ranges) were presented, and the Wilcoxon-Mann-Whitney U-test or Kruskal-Wallis test was used for analysis. Categorical variables were expressed as counts (n) and percentages (%). Pearson correlation analysis was employed to explore relationships among the dimensions of KAP. Multivariate logistic regression analysis was conducted to identify independent factors associated with adequate knowledge, positive attitudes, and proactive practices, using 70% of the maximum possible points on the KAP score as the cut-off value. The variables with P < 0.05 in the univariable analyses were included in the multivariable analyses. Additionally, ordinal logistic regression was employed to examine independent factors related to inhaler adherence. Path analysis was conducted to explore the relationships between knowledge, attitudes, and practices. This approach was utilized to test the following hypotheses: (1) knowledge influences attitude, (2) knowledge affects practice, and (3) attitude impacts practice. A two-sided P-value less than 0.05 was considered statistically significant.
Results
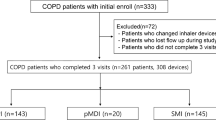
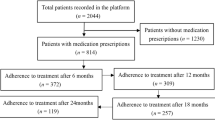
A total of 555 questionnaires were initially collected. After excluding 1 questionnaire with an abnormal age entry and 36 questionnaires with logical inconsistencies, 518 valid responses remained. In this study, 518 COPD patients who had been using inhaled medications for at least one month were included, with 369 (71.24%) being male and an average age of 68.21 ± 11.05 years. As shown in Table 1, most participants were of Han ethnicity (508, 98.07%) and lived in urban or suburban areas (291, 56.18%). The majority had a BMI within the range of 18.5–23.9 (291, 56.18%), and most had completed junior high school or below (278, 53.67%). Regarding employment status, 246 (47.49%) were retired. Additionally, 445 (85.91%) were married, and 514 (99.23%) had medical insurance. The highest proportion of participants had COPD for 3 years or more (251, 48.46%), with 187 (36.1%) experiencing 1 acute exacerbation in the past year. In terms of pulmonary function, the majority of patients were classified as GOLD stage 1 (24.9%) or GOLD stage 2 (45.75%), indicating mild or moderate airflow limitation. Assessment of breathlessness using the mMRC scale revealed that most participants experienced at least mild dyspnea, with 32.43% reporting grade 1 and 47.69% reporting grade 2 or above.
The mean scores for knowledge, attitude, practice, and TAI were 22.82 ± 3.24 (range: 0–32), 51.79 ± 6.61 (range: 14–70), 33.08 ± 5.58 (range: 8–40), and 35.12 ± 11.01 (range: 0–50), respectively. The response distribution of KAP dimensions was detailed in the Supplement Tables 1, 2 and 3.
Responses to the TAI dimension revealed that 16.22% always and 11.20% more than half the time forget to use inhaled medication on time (T1). Moreover, 11.39% would stop using inhalation medication on weekends or vacations (T4), when feeling anxious or depressed (T5), and when they felt it was not helping their condition (T6) (Supplement Table 4).
The correlation analysis revealed significant positive relationships between knowledge and attitude (r = 0.490, P < 0.001), knowledge and practice (r = 0.368, P < 0.001), and knowledge and TAI scores (r = 0.118, P = 0.007). Additionally, significant correlations were found between attitude and practice (r = 0.602, P < 0.001) as well as attitude and TAI scores (r = 0.310, P < 0.001). However, the correlation between practice and TAI was not significant (r = 0.071, P = 0.104) (Table 2).
The cut-off values of 70% of the maximum possible points were used for the knowledge, attitude, and practice dimensions. A total of 370 individuals (71.40%) scored above the cut-off for knowledge, 332 individuals (64.09%) for attitude, and 425 individuals (82.5%) for practice (Table 3).
Multivariate logistic regression showed that age (OR = 0.954, 95% CI: [0.930, 0.980], P = 0.001), with BMI of 18.5–23.9 kg/m2 (OR = 2.150, 95% CI: [1.070, 4.318], P = 0.032), with BMI of more than 27.9 kg/m2 (OR = 5.696, 95% CI: [1.616, 20.081], P = 0.007), with college education and above (OR = 0.377, 95% CI: [0.183, 0.776], P = 0.008), retired (OR = 2.204, 95% CI: [1.248, 3.894], P = 0.006), with monthly per capita income of 2000–5000 yuan (OR = 2.674, 95% CI: [1.454, 4.915], P = 0.002), with monthly per capita income of more than 5000 yuan (OR = 3.721, 95% CI: [1.714, 8.078], P = 0.001), had 3 times of acute exacerbations or more (OR = 6.095, 95% CI: [2.293, 16.204], P < 0.001), undergoing inhalation therapy (OR = 3.532, 95% CI: [1.503, 8.303], P = 0.004), and received TCM treatment (OR = 2.874, 95% CI: [1.462, 5.649], P = 0.002) were independently associated with adequate knowledge. Concurrently, knowledge score (OR = 1.390, 95% CI: [1.277, 1.514], P < 0.001), had 3 times of acute exacerbations or more (OR = 2.625, 95% CI: [1.021, 6.750], P = 0.045), GOLD 2 (OR = 0.183, 95% CI: [0.069, 0.485], P = 0.001), GOLD 3 (OR = 0.138, 95% CI: [0.044, 0.437], P = 0.001), GOLD 4 (OR = 0.097, 95% CI: [0.021, 0.439], P = 0.002), and received TCM treatment (OR = 2.937, 95% CI: [1.378, 6.262], P = 0.005) were independently associated with positive attitude. Furthermore, attitude score (OR = 1.244, 95% CI: [1.167, 1.325], P < 0.001), with BMI of more than 27.9 kg/m2 (OR = 15.520, 95% CI: [1.683, 143.144], P = 0.016), and undergoing inhalation therapy (OR = 4.555, 95% CI: [1.607, 12.914], P = 0.004) were independently associated with proactive practice (Table 4).
The ordinal logistic regression for TAI showed that attitude score (OR = 1.177, 95% CI: [1.114, 1.244], P < 0.001), with BMI of less than 18.5 kg/m2 (OR = 5.596, 95% CI: [1.362, 22.989], P = 0.017), with BMI of 23.9–27.9 kg/m2 (OR = 6.074, 95% CI: [1.627, 22.646], P = 0.007), unemployed (OR = 0.308, 95% CI: [0.130, 0.729], P = 0.007), grade 1 of breathlessness assessment (OR = 0.285, 95% CI: [0.098, 0.824], P = 0.020), and undergoing inhalation therapy (OR = 0.297, 95% CI: [0.121, 0.731], P = 0.008) were independently associated with inhaler adherence (Table 5).
The path analysis showed that knowledge directly influenced both attitude (β = 0.997, P = 0.002) and practice (β = 0.166, P = 0.016), and indirectly affected practice through attitude (β = 0.467, P = 0.002) (Supplement Table 5 and Fig. 1).
Discussion
This study revealed that while COPD patients demonstrated adequate knowledge, a positive attitude, and proactive practices toward inhaler use, their adherence to inhalation devices was poor. It is recommended that healthcare providers intensify educational interventions and support mechanisms that specifically target the enhancement of practical skills and adherence behaviors among COPD patients.
Our research findings illuminate the complex interplay between KAP regarding inhalation device use among COPD patients, as well as their TAI. The study shows that COPD patients have good knowledge and attitudes toward inhalation devices, but their adherence is poor, indicating a gap between awareness and adherence. This discrepancy suggests that while patients are aware of and appreciate the importance of their treatment devices, this knowledge does not fully translate into practical application. Significantly, gender differences were notable, with females demonstrating slightly better knowledge and practice scores than males. This aligns with previous research suggesting gender differences in health literacy and engagement in health-promoting behaviors28. Both the significant difference and logistic regression results support the importance of gender in understanding KAP related to COPD management, which may be influenced by societal roles and health communication strategies that differentially engage men and women.
Significant variances in age and BMI were observed. Advancing age may impair the ability to process health information and physically engage with healthcare practices, while patients within a normal BMI range demonstrated superior adherence, reflecting better overall health status and more effective disease management28,29. Higher educational levels were associated with improved knowledge but did not directly translate into better practices or adherence. This suggests that while educational interventions can augment knowledge, behavioral modification necessitates additional support and resources30,31. The frequency of acute COPD exacerbations was linked to better knowledge and attitudes, yet this did not consistently translate into improved practices or adherence. This pattern suggests that patients may adopt a reactive approach to disease management, adhering more closely to treatment protocols only during and following exacerbations32,33.
The direct and indirect effects analyses demonstrated that knowledge has a direct impact on both attitudes and practices and also indirectly affects practice through attitude. This pathway highlights the potential of educational interventions to not only improve knowledge directly but also to modify attitudes and, subsequently, practices. However, the limited translation of knowledge and attitudes into improved practices suggests that interventions should not only educate but also address practical barriers to adherence, such as physical limitations, complexity of inhalation devices, and psychological factors like fear of dependency or side effects34,35.
The distribution of responses in the knowledge dimension generally indicates a fair level of understanding among COPD patients regarding the disease and its management. Notably, the awareness that COPD can be exacerbated by factors like smoking and air pollution is relatively high. However, there are significant gaps in knowledge about the ongoing nature of COPD treatments and specific therapies like nebulized inhalation, where misconceptions are evident. For instance, only a small percentage of participants understood that COPD treatment regimens could be indefinite and that not all medications for nebulized inhalation are the same. To improve these areas, specific educational programs should be developed focusing on the chronic nature of COPD and the variability in treatment options, particularly nebulized therapies36,37. These programs could include detailed patient handouts, digital resources, and interactive workshops that reinforce the ongoing and individualized aspects of COPD management, as supported by literature indicating the effectiveness of comprehensive patient education in improving disease knowledge31,38.
In the attitude dimension, the majority of patients recognize the importance of inhalation therapy for managing COPD, yet there is a noticeable degree of neutrality or negative feelings towards its efficacy and safety. Particularly, a significant minority has reservations about the safety of inhalation therapy and the integration of traditional Chinese medicine with Western approaches. This reflects a broader hesitation which might be attributed to inadequate understanding or past negative experiences. Reflecting on the previous findings, which highlighted the positive correlation between adequate disease knowledge and favorable patient attitudes, enhancing educational outreach appears vital39,40. Specific recommendations could involve the creation of support groups and the incorporation of patient testimonials that address common concerns and misconceptions. Additionally, healthcare providers could offer regular counseling sessions to discuss and alleviate concerns about the safety and benefits of inhalation therapy41,42.
The practice dimension shows a moderate level of competency in handling inhalation devices and adherence to prescribed regimens. However, there are gaps in the correct operation and maintenance of inhalation therapy devices, and a portion of the patients displayed uncertainty about the procedures. Given the crucial role of proper technique in the effectiveness of inhalation therapy, these findings are concerning. Building on strategies that have been successful in other chronic disease contexts, such as diabetes management programs reported by previous studies, practical demonstrations, and hands-on training sessions could be particularly beneficial43,44. Healthcare providers should consider implementing regular device handling workshops and follow-up assessments to ensure that patients are competent in using their devices. Moreover, leveraging digital tools like instructional videos tailored to diverse patient groups could enhance understanding and retention of correct practices45,46.
This study has several limitations. First, the cross-sectional design restricts our ability to infer causal relationships between the observed factors and patient outcomes; longitudinal studies are needed to validate these findings over time. Second, the study sample is limited to patients from a single hospital in Chongqing, which may not be representative of COPD patients in other regions, potentially limiting the generalizability of the results. Third, self-reported measures were used to assess knowledge, attitudes, practices, and adherence, which may be subject to response biases, including social desirability and recall biases. Fourth, no practical assessment or monitoring of patients’ ability to handle inhalation devices was conducted, which may have led to an overestimation of their competence in device usage. Lastly, the study did not include a health literacy assessment, which is a crucial factor influencing patient understanding and adherence. Finally, longitudinal and multicenter studies with objective assessments of inhaler technique and adherence are warranted to further validate these findings and improve intervention strategies.
In conclusion, this study reveals a critical gap between the adequate knowledge and positive attitudes of COPD patients with at least one month of inhaled medication use, and their actual practices and adherence to inhalation device use, underscoring a complex interplay of educational, behavioral, and clinical factors that influence patient management. Clinicians should prioritize personalized patient education and regular monitoring of inhalation device use to improve adherence, particularly focusing on those with lower educational levels, higher body mass indexes, and complex clinical profiles to enhance overall disease management outcomes.
Data availability
All data generated or analysed during this study are included in this published article.
References
Graf, J. et al. Medical treatment of COPD. Dtsch. Arztebl Int. 155, 599–605 (2018).
Hou, W. et al. Cigarette smoke induced lung barrier dysfunction, EMT, and tissue remodeling: A possible link between COPD and lung Cancer. Biomed. Res. Int. 2025636 2019 (2019).
Soriano, J. B. et al. Temporal transitions in COPD severity stages within the GOLD 2017 classification system. Respir. Med. 142, 81–85 (2018).
Zhou, M. et al. Cause-specific mortality for 240 causes in China during 1990–2013: A systematic subnational analysis for the global burden of disease study 2013. Lancet 387, 251–272 (2016).
Wang, C. et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China pulmonary health [CPH] study): A National cross-sectional study. Lancet 391, 1706–1717 (2018).
Barbara, S., Kritikos, V. & Bosnic-Anticevich, S. Inhaler technique: Does age matter? A systematic review. Eur. Respir. Rev. 26 (2017).
Melzer, A. C. et al. Patient characteristics associated with poor inhaler technique among a cohort of patients with COPD. Respir. Med. 123, 124–130 (2017).
Grandmaison, G., Grobéty, T., Vaucher, J., Hayoz, D. & Suter, P. Prevalence of critical errors and insufficient peak inspiratory flow in patients hospitalized with COPD in a department of general internal medicine: A cross-sectional study. Chronic Obstr. Pulm Dis. 11, 406–415 (2024).
Wang, Y. H. et al. Diagnostic efficacy of CBCT, MRI and CBCT–MRI fused images in determining anterior disc displacement and bone changes of temporomandibular joint. Dentomaxillofac. Radiol. 51 (2022).
Lindh, A. et al. Errors in inhaler use related to devices and to inhalation technique among patients with chronic obstructive pulmonary disease in primary health care. Nurs. Open. 6, 1519–1527 (2019).
Hallit, S. et al. Knowledge, attitude and practice of Lebanese community pharmacists toward chronic obstructive pulmonary disease. J. Epidemiol. Glob Health. 10, 86–95 (2020).
Zhao, L. & Zhao, Q. Knowledge, attitude, and practice toward disease prevention among a high-risk population for chronic obstructive pulmonary disease: A cross-sectional study. Int. J. Nurs. Sci. 10, 238–244 (2023).
Aerts, C. et al. Understanding the role of disease knowledge and risk perception in shaping preventive behavior for selected vector-borne diseases in Guyana. PLoS Negl. Trop. Dis. 14, e0008149 (2020).
Liao, L., Feng, H., Jiao, J., Zhao, Y. & Ning, H. Nursing assistants’ knowledge, attitudes and training needs regarding urinary incontinence in nursing homes: A mixed-methods study. BMC Geriatr. 23, 39 (2023).
Mumena, W. A. Maternal knowledge, attitude and practices toward free sugar and the associations with free sugar intake in children. Nutrients 13 (2021).
Gregoriano, C. et al. Use and inhalation technique of inhaled medication in patients with asthma and COPD: Data from a randomized controlled trial. Respir Res. 19, 237 (2018).
Souza, M. L., Meneghini, A. C., Ferraz, E., Vianna, E. O. & Borges, M. C. Knowledge of and technique for using inhalation devices among asthma patients and COPD patients. J. Bras. Pneumol. 35, 824–831 (2009).
Dhand, R. et al. Results of a patient survey regarding COPD knowledge, treatment experiences, and practices with inhalation devices. Respir. Care. 63, 833–839 (2018).
Venkatesan, P. GOLD COPD report: 2023 update. Lancet Respir. Med. 11, 18 (2023).
Respiratory Rehabilitation Group & Chinese Chronic Obstructive Pulmonary Disease Coalition. Chinese expert consensus on standard application of inhalation device in stable chronic airway disease patients. Chin. J. Tuberc. Respir. Dis.. 42, 13 (2019).
Sunjaya, A., Poulos, L., Reddel, H. & Jenkins, C. Qualitative validation of the modified medical research Council (mMRC) dyspnoea scale as a patient-reported measure of breathlessness severity. Respir. Med. 203, 106984 (2022).
Pan, X. F., Wang, L. & Pan, A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 9, 373–392 (2021).
He, J. et al. Chinese pregnant women’s knowledge, attitude, and practice of self-protection against coronavirus disease 2019 during the post-pandemic period: A structural equation modeling-based survey. Int. J. Disaster Risk Reduct. 87, 103559 (2023).
Li, W. et al. Knowledge, attitude, and practice towards thyroid nodules and cancer among patients: A cross-sectional study. Front. Public. Health. 11, 1263758 (2023).
Xu, W., Li, Q., Mao, Y. & He, Y. Knowledge, attitude, and practice toward interstitial lung disease among patients: A cross-sectional study. Front. Med. (Lausanne). 11, 1397659 (2024).
Plaza, V. et al. Validation of the ‘test of the adherence to inhalers’ (TAI) for asthma and COPD patients. J. Aerosol Med. Pulm Drug Deliv. 29, 142–152 (2016).
Ni, P., Chen, J. L. & Liu, N. Sample size Estimation for quantitative studies in nursing research. 45, 378–380 (2010).
Li, P. et al. Cross-Verification of COVID-19 information obtained from unofficial social media accounts and associated changes in health behaviors: Web-Based questionnaire study among Chinese netizens. JMIR Public. Health Surveill. 8, e33577 (2022).
Hozawa, A. et al. Association between body mass index and All-Cause death in Japanese population: Pooled individual participant data analysis of 13 cohort studies. J. Epidemiol. 29, 457–463 (2019).
Gai, J. et al. Exploration of potential targets and mechanisms of naringenin in treating autism spectrum disorder via network Pharmacology and molecular Docking. Med. (Baltim). 101, e31787 (2022).
Panithanang, B. et al. The effect of health behavior modification program for liver fluke prevention among the risk group in rural communities, Thailand. Asian Pac. J. Cancer Prev. 19, 2673–2680 (2018).
Niu, C., Huang, X., Wang, L. & Liu, F. Effect of hospital, community and home care model on nursing and quality of life of patients after transurethral resection of benign prostatic hyperplasia. Am. J. Transl. Res. 13, 4959–4968 (2021).
Vandenberg, A. E., Echt, K. V., Johnson, T. M. & Bowling C. B. Patient discourse on chronic kidney disease monitoring: A qualitative study at a veterans affairs renal clinic. BMC Nephrol. 19, 183 (2018). 2.
Jung, T., Moorhouse, N., Shi, X. & Amin, M. F. A virtual reality-supported intervention for pulmonary rehabilitation of patients with chronic obstructive pulmonary disease: Mixed methods study. J. Med. Internet Res. 22, e14178 (2020).
Lewis, A., Conway, J., Middleton, J., Startup, C. K. & Wyatt, J. Playing the harmonica with chronic obstructive pulmonary disease. A qualitative study. Chron. Respir Dis. 19, 14799731221083315 (2022).
Fishwick, D., Barber, C. & Wiggans, R. Chronic obstructive pulmonary disease and work: The continuing narrative. Semin. Respir. Crit. Care Med. 44, 378–384 (2023).
Gloeckl, R., Schneeberger, T., Jarosch, I. & Kenn, K. Pulmonary rehabilitation and exercise training in chronic obstructive pulmonary disease. Dtsch. Arztebl Int. 115, 117–123 (2018).
Kaya, T., Atıcı, P., Karatepe, A. G. & Günaydın, R. Peer-led education or booklet for knowledge transfer about disease: A randomized-controlled trial with ankylosing spondylitis patients. Arch. Rheumatol. 36, 560–569 (2021).
Askari Tajabadi, N., Pakmanesh, H., Mirzaee, M. & Jahani, Y. The evaluation of survival rate in patients with prostate cancer by Bayesian Weibull parametric accelerated failure-time model. Iran. J. Public. Health. 51, 2108–2116 (2022).
Song, Y. L. & Park, J. H. Differences in body mass index trajectories and their classification, sociodemographic characteristics, and health behaviors between people with and without disabilities using Korea health panel survey data. Int. J. Environ. Res. Public. Health 19 (2022).
Blackstock, F. C. et al. Chronic obstructive pulmonary disease education in pulmonary rehabilitation. An official American thoracic society/thoracic society of Australia and new zealand/canadian thoracic society/British thoracic society workshop report. Ann. Am. Thorac. Soc. 15, 769–784 (2018).
Cornelison, S. D. & Pascual, R. M. Pulmonary rehabilitation in the management of chronic lung disease. Med. Clin. North. Am. 103, 577–584 (2019).
Cho, S. E., Kwon, M. & Kim, S. A. Influence of diabetes knowledge, self-stigma, and self-care behavior on quality of life in patients with diabetes. Healthcare (Basel) 10 (2022).
Sushko, K., Strachan, P., Butt, M., Nerenberg, K. A. & Sherifali, D. Understanding the self-management experiences and support needs during pregnancy among women with pre-existing diabetes: A qualitative descriptive study. BMC Pregnancy Childbirth. 23, 309 (2023).
Azkan Ture, D., Bhattacharya, S., Demirci, H. & Yildiz, T. Health literacy and health outcomes in chronic obstructive pulmonary disease patients: An explorative study. Front. Public. Health. 10, 846768 (2022).
van Beers, M., Janssen, D. J. A., Gosker, H. R. & Schols, A. Cognitive impairment in chronic obstructive pulmonary disease: Disease burden, determinants and possible future interventions. Expert Rev. Respir. Med. 12, 1061–1074 (2018).
Funding
1. Chongqing Kewei Joint Chinese Medicine Research Project (2023QNXM057). 2. Youth Top Talent Project of Chongqing Hospital of Traditional Chinese Medicine (CQSZYY2023016). 3. Chongqing Science and Technology Bureau (cstc2021ycjh-bgzxm0045). 4. Chongqing Education Commission (KJZD-K202215103). 5. Chongqing Research Institution Performance Incentive and Guidance Project (JXYN2021-1-14). 6. Chongqing famous Chinese medicine experts in Chongqing studio construction project (Fang Bangjiang).
Author information
Authors and Affiliations
Contributions
Qiu-ju Yao, Yadan Tu and Chenghu Wang carried out the studies, participated in collecting data, and drafted the manuscript. Yong Chen, Xuanhan Li and Bangjiang Fang performed the statistical analysis and participated in its design. Yadan Tu, Yi Ren and Yigang Wang participated in acquisition, analysis, or interpretation of data and draft the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This work has been carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association. The study was approved by the Ethics Committee of the Chongqing Hospital of Traditional Chinese Medicine (Approval No. 2024-IIT-KS-2), and informed consent was secured from all participants prior to their inclusion. The study was carried out in accordance with the applicable guidelines and regulations.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tu, Y., Yao, Q., Chen, Y. et al. Knowledge, attitudes, and practices of inhalation device use among patients with chronic obstructive pulmonary disease. Sci Rep 15, 26377 (2025). https://doi.org/10.1038/s41598-025-11852-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-11852-8