Abstract
Increased angiogenesis and vascular permeability are hallmarks of microvascular retinal diseases such as diabetic retinopathy and diabetic macular edema (DME). Periodic intravitreal injections of inhibitors of the vascular endothelial growth factor (VEGF) are first-line therapy, but their invasiveness and associated risks often lead to poor compliance and outcomes. Here, we investigate VIAN-c4551, a highly potent antiangiogenic cyclic heptapeptide, as a non-invasive topical ophthalmic alternative to the current standard of care for DME. VIAN-c4551 demonstrated high potency (IC50 = 137 pM) to inhibit the permeability of human umbilical vein endothelial cell monolayers induced by VEGF. VIAN-c4551 eye drops potently (0.005% minimum effective dose) prevented, for up to 24 h, the retinal vascular leakage induced by VEGF injected intravitreally and reversed the increased retinal vascular permeability due to diabetes in rats and mice. VIAN-c4551 exhibited high penetrability across MDCK epithelium and, after a single eye drop in rabbits, reached the vitreous and the retina-choroid at concentrations several orders of magnitude above its IC50 (Cmax ~239 nM and ~ 6.7 µM, respectively, after 6 h) that lasted at least 24 h. In conclusion, VIAN-c4551 is a non-invasive, once-a-day potential intervention for preventing and reversing retinal vascular leakage in DME and other vascular retinopathies and preserving sight.
Similar content being viewed by others
Introduction
Diabetes is a common cause of vision loss due to retinal microvascular complications in diabetic retinopathy (DR) and diabetic macular edema (DME). DME is present in 25% of persons with diabetes and 71% of patients with proliferative DR, and it is the clinical condition most closely associated with vision loss1. In DME, leakage from retinal capillaries causes the accumulation of extracellular fluid and proteins that alter the structure and function of the macula and may lead to blindness if untreated. Vascular endothelial growth factor (VEGF) is a major vascular permeability factor in DME2, and the intravitreal injection of agents blocking VEGF has become the first-line treatment for DME with vision loss3. However, intravitreal injections are invasive, and their repeated and long-term use, due to the chronic nature of DME, increases the chance of ocular complications and systemic adverse events4. Eye drops are a preferred therapeutic option because they are self-administered, non-invasive, and facilitate long-term therapy. However, reaching the back of the eye through eye drops is challenging due to the numerous ocular barriers5,6, and no eye-drop formulation has been approved by the FDA to treat posterior eye diseases, including DME.
VIAN-c4551 is a promising drug candidate for treating DME, DR, and other vascular retinopathies. VIAN-c4551 is an analog of vasoinhibin, an endogenous antiangiogenic protein with significant therapeutic potential. Vasoinhibin inhibits endothelial cell proliferation, migration, survival, and permeability in response to VEGF and other proangiogenic and vascular permeability factors (basic fibroblast growth factor, bradykinin, interleukin 1β )7,8. It helps restrict retinal angiogenesis under physiological conditions9, and the intravitreal administration of vasoinhibin reduces ischemia-induced retinal angiogenesis10 and prevents and reverses diabetes- and VEGF-induced increase in retinal vascular leakage in rodents11. In humans, the systemic and ocular levels of vasoinhibin are disrupted in retinopathy of prematurity12,13 and DR14, and a prokinetic medication (levosulpiride) that upregulates vasoinhibin levels in the vitreous of patients with proliferative DR15, improves visual acuity and structural retinal outcomes in patients with DME and vision loss16.
However, the direct use of vasoinhibin in the clinic is hampered by difficulties in its recombinant production17. These difficulties have been overcome by the development of VIAN-c4551, a vasoinhibin analog with improved pharmacological properties that conserves the efficacy and potency of vasoinhibin8. VIAN-c4551 inhibits VEGF-induced proliferation of endothelial cells with potency like vasoinhibin (IC50 = 150 pM) and is orally active to inhibit melanoma tumor growth and vascularization in mice8. The oral bioavailability of VIAN-c4551 demonstrates physiochemical properties (solubility, stability, permeability, and potency) that may help VIAN-c4551 overcome the anatomical and physiological barriers that prevent topically administered drugs from reaching the retina5,6. Here, we show the high potency and efficacy of VIAN-c4551 in eye drops to inhibit VEGF- and diabetes-induced retinal vascular leakage in rodents, the in vitro transit of VIAN-c4551 across epithelial cells, and the presence of VIAN-c4551 in the retina-choroid and vitreous at supra-therapeutic concentrations following eye drop administration in rats and rabbits.
Materials and methods
Reagents
VIAN-c4551(> 95% pure), VIAN-c4551 coupled to fluorescein-5-isothiocyanate (FITC), and recombinant human vascular endothelial growth factor-165 (VEGF) were from GenScript (Piscataway, NJ). Basic fibroblast growth factor (bFGF) from Scios, Inc., Mountain View, CA. Recombinant human vasoinhibin of 123 amino acids (Vi1-123) was produced as reported18. Eye drop vehicle (3% trehalose-0.15% sodium hyaluronate) was from Laboratories Théa (Clermont-Ferrand, France).
Cell culture
Human umbilical vein endothelial cells (HUVEC)19 were cultured in F12K medium supplemented with 20% fetal bovine serum (FBS), 100 µg mL− 1 heparin (Sigma Aldrich, St, Louis, MO), 25 µg mL− 1 endothelial cell growth supplement (ECGS) (Corning, Corning, NY), and 100 U mL− 1 penicillin-streptomycin, and authenticated by CD31 presence. HUVECs were used between passages 4 and 9. The Madin-Darby canine kidney (MDCK) epithelial cell line (ATCC, Rockville, MD) was cultured in 10% FBS-DMEM.
VEGF-induced endothelial cell permeability
HUVEC were seeded at 20,000 cells cm− 2 on a 6.5 mm transwell with a 0.4 μm pore to form a confluent monolayer. Transendothelial electrical resistance (TEER) was measured with the EVOM2 Volt/Ohm meter (World Precision Instruments, Sarasota, FL) as reported8. Monolayers were incubated with different concentrations of VIAN-c4551 or Vi1-123 for 1 h before adding PBS or 50 ng mL− 1 VEGF, and TEER measured over a 150-min period.
Immunofluorescence analysis of F-actin and CD31
HUVEC were seeded at 20,000 cells cm− 2 on 18 mm coverslips placed in a 12-well plate and cultured to confluence. Once the monolayer was established, cells were pretreated with or without 100 nM of VIAN-c4551 for 1 h prior to stimulation with 200 ng mL− 1 VEGF for 30 min. Cells were then washed, fixed with 4% paraformaldehyde (PFA) for 30 min, permeabilized with 0.5% Triton X-100 in PBS for 30 min, and blocked with 5% normal goat serum, 1% BSA, 0.05% Triton X-100 in PBS for 1 h at RT. Primary antibody incubation was performed overnight at 4 °C in a humidified chamber using anti-CD31 (1:100, Abcam) diluted in 1% BSA, 0.1% Triton X-100 in PBS. Following washes, cells were incubated for 2 h in darkness with goat anti-mouse Alexa Fluor 488-conjugated secondary antibody (1:500). F-actin was visualized by incubating cells with 160 nM TRITC (Tetramethylrhodamine)-phalloidin for 1 h in darkness (Thermo Fisher Scientific, Waltham, MA). Nuclei were counterstained with 5 µg mL− 1 Hoechst 33,342 (Sigma-Aldrich), and coverslips observed by fluorescence microscopy and merged images obtained using ImageJ-FIJI.
MDCK transit assay
MDCK cells were seeded (40,000 cells cm− 2) in 200 µL 10% FBS-DMEM on a 6.5 mm transwell with a 0.4 μm pore to form a confluent monolayer. Upon confluency, 0.4 nM and 4 nM VIAN-c4551 or Vi1-123 were added to the apical side of the monolayer for 2 h at 37 °C. 600 µL from the basolateral compartments were then collected and stored at -20 °C. VIAN-c4551 and Vi1-123 were quantified by means of their bioactive properties, as reported20. Recovery levels were expressed relative to those without MDCK cells, and the apparent permeability coefficient (Papp, cm s− 1) across the epithelial barrier was calculated as reported21.
Animals
Male and female Wistar rats (6–7 weeks old, 180–230 g), male CD-1 mice (8–10 weeks old, 20–25 g), and female New Zealand white rabbits (2–2.5 kg) were maintained and treated in adherence to the National Research Council’s Guide for the Care and Use of Laboratory Animals. The Bioethics Committee of the Instituto de Neurobiología (UNAM) approved all animal experiments. The authors confirm that the study is reported in accordance with the ARRIVE (Animal Research: Reporting of In Vivo Experiments) guidelines.
VEGF-induced retinal vascular permeability
One drop containing 0.5% [5 mg mL− 1 or 6.5 mM] VIAN-c4551 or vehicle was instilled in each eye of male mice (5 µL) and rats (10 µL) manually maintained still for 10 s to allow drop distribution on the ocular surface. After 1 h, animals were anesthetized with 60% ketamine and 40% xylazine (1 µL g− 1 body wt, i.p.) and injected intravitreally with 1 µL (mice) or 2 µL (rats) PBS or VEGF (250 ng) and two hours later, retinal vascular leakage was evaluated by the extravasation of albumin stained by the intravenously injected Evans blue dye, as reported22. For the qualitative microscopic imaging of retinal vascular leakage, a single eyedrop of VIAN-c4551 [0.5%] or vehicle was applied to the eye 4 h prior to intravitreal injection of VEGF (300 ng eye− 1) or PBS. One hour later, animals were anesthetized (ketamine/xylazine) and fluorescein isothiocyanate–labeled dextran (FITC-dextran, 50 mg mL− 1, MW 2 × 10⁶ Da; Sigma-Aldrich) was administered intravenously at a dose of 100 mg kg− 1. After allowing one h for systemic circulation, animals were euthanized by CO2 inhalation and retinas flat-mounted, fixed for 4 h in 4% PFA at room temperature, washed with PBS, mounted on glass slides using 50% glycerol in PBS, and observed under a fluorescence microscope.
Diabetes-induced retinal vascular permeability
Five daily i.p. injections of streptozotocin (STZ) (55 mg kg− 1; S0130, Sigma–Aldrich) and a single i.p. STZ injection (60 mg kg− 1) induced diabetes in male mice and male rats, respectively23,24. Blood glucose levels > 250 mg dL− 1 defined diabetes one week post-STZ. After 5 weeks, non-diabetic and diabetic animals received a daily eye drop of 0.5% VIAN-c4551 or vehicle per eye for 5 days. The Evans blue method evaluated retinal vascular leakage 24 h after the last eye drop.
Ocular pharmacokinetics
Female rats and rabbits were instilled with one eye drop (10 and 50 µL, respectively) containing 0.5% VIAN-c4551, VIAN-c4551-FITC (net peptide), or vehicle, and manually kept still for 10 s to allow drop surface distribution and euthanized by CO2 inhalation at different intervals for up to 24 h. Eyes were enucleated, and the vitreous, the retina from the rat, and the retina-choroid from the rabbit were collected, snap frozen in liquid nitrogen, and stored at -80 °C until analysis. Tissues were homogenized in RIPA buffer (10 mM Tris-HCl, 140 mM NaCl, 0.5% IGEPAL CA-630, 1mM EDTA, 0.5 mM EGTA, 1% triton X-100, 0.1% SDS, pH 7.4) supplemented with 1:100 protease inhibitor cocktail (Roche). Vitreous samples (125 ng µL− 1 protein) and retinas (150 ng µL− 1 protein) were added to HUVEC cultures to evaluate VIAN-c4551 levels through its bioactivity, as reported20. For fluorescence emission, a standard curve of VIAN-c4551-FITC from 0 to 100 pmol was prepared in a vitreous matrix (110 ng µL− 1 protein) for rat or rabbit or in a retina matrix (2.5 µg µL− 1 protein for rat or 750 ng µL− 1 protein for rabbit). Fluorescence emission of 100 µL from each standard dilution was quantified (Varioskan Flash, Thermo Fisher Scientific) at excitation and emission wavelengths of 490 nm and 520 nm, respectively, for 100 ms. Values were interpolated from standard curves in the respective matrix and pharmacokinetic analysis was performed using Plotly software25.
Ocular distribution of VIAN-c4551-FITC
Male Wistar rats (~ 285 g) received three eye drops (one per hour) of either vehicle or VIAN-c4551-FITC (0.5%). Six hours after the first dose, animals were euthanized by CO2 inhalation, perfused with PBS followed by 4% PFA. The eyes were postfixed in 4% PFA for 2 h, cryoprotected in 15% and 30% sucrose for 24 h each, embedded in TissueTek, and cryosectioned at 10 μm. Sections were mounted on gelatin-coated slides, washed with PBS, permeabilized (0.1% Triton X-100), counterstained with Sytox Red (S34859, Thermo Fisher Scientific, Waltham, MA), mounted in Vectashield, and observed under confocal microscopy (Zeiss LSM 780, Overkochen, Germany). Image analysis was performed in ImageJ-FIJI using Bio-Formats and hyperstacks. For each section, 5–7 optical slices were combined using maximum intensity projection.
Statistical analysis
Statistical analysis was performed using the GraphPad Prism version 10.2.2 for macOS, GraphPad Software (Boston, Massachusetts USA, www.graphpad.com). The threshold for significance was set at P < 0.05. For the analysis of two variables over time, we used two-way ANOVA with Dunnett’s post hoc test to compare treatment groups to the control at each time point. For grouped column comparisons involving two factors, we used two-way ANOVA with Sidak’s post hoc test for pairwise comparisons. For single-variable comparisons across multiple groups, we use one-way ANOVA with Dunnett’s post hoc, comparing each group to the control.
Results
VIAN-c4551 potently inhibits the VEGF-induced permeability of HUVEC monolayers
We evaluated the trans-endothelial electrical resistance (TEER) of HUVEC monolayers as an indicator of vascular permeability (Fig. 1a, b). VEGF rapidly decreased TEER values and kept them low throughout the 150-minute incubation period. VIAN-c4551 prevented the VEGF-induced reduction of TEER, and VIAN-c4551 alone showed no effect (Fig. 1a). TEER inhibition by VIAN-c4551 was dose-dependent with an IC50 of 137.3 pM, like that of the full-length vasoinhibin (Vi1-123) (IC50 = 163.2 pM) (Fig. 1b). Increased vascular permeability due to weakened endothelial cell junctions associates with the redistribution of the actin cytoskeleton that leads to cell contraction26. The actin cytoskeleton was therefore evaluated by the phalloidin-TRITC staining of F-actin in HUVEC monolayers co-stained for the endothelial cell marker CD31 and exposed to VEGF (Fig. 1c). VEGF altered the actin cytoskeleton as revealed by perinuclear actin stress fibers, contracted and rounded cell bodies, and lack of CD31 at the surface of cells. These changes were blocked by VIAN-c4551 (Fig. 1c). These findings visualize the protective effect of VIAN-c4551 against the loss of integrity of the endothelial barrier caused by VEGF and thereby confirm and complement TEER measurements.
VIAN-c4551 inhibits VEGF-induced permeability of HUVEC monolayers. (a) Changes in the trans-endothelial electrical resistance (ΔTEER) of HUVEC monolayers treated or not with 100 nM VIAN-c4551 throughout a 150-minute incubation period without (-) or with VEGF (50 ng mL− 1). Values are means ± SD, n = 3, *P < 0.006 vs. (-) for all time points except 0 (2-way ANOVA repeated measures, Dunnett’s). (b) Dose-response inhibition of the VEGF-induced reduction of ΔTEER at 90 min by different concentrations of VIAN-c4551 or Vi1-123. The IC50 of VIAN-c4551 and Vi1-123 are indicated. ΔTEER is relative to that of VEGF alone. Values are means ± SD, n = 9, and the curve represents a nonlinear regression analysis of four parameters (54 points, r2 ≥ 0.92). (c) Representative fluorescence of HUVEC monolayers stained for F-actin and CD31 pretreated with or without VIAN-c4551 for 1 h followed by VEGF (200 ng mL− 1) for 30 min. Nuclei were counterstained with Hoechst 33,342. Scale bar = 100 μm.
VIAN-c4551 exhibits high transit across epithelia
We analyzed the capacity of VIAN-c4551 to cross the MDCK epithelial cell monolayer, a well-established model to evaluate the paracellular and transcellular transport of drugs27,28. Around 50% of VIAN-c4551 in two concentrations (0.4 and 4 nM) crossed the monolayer after 2 h (Fig. 2a). VIAN-c4551 presented a high apparent permeability coefficient (Papp = 1.44 × 10− 5 cm s− 1) (Fig. 2b), like steroids29. The penetrability of Vi1-123 across the MDCK monolayer was negligible (Papp = 3.86 × 10− 7 cm s− 1).
VIAN-c4551 transit across MDCK epithelial cells. (a) Percentage of transit across an MDCK monolayer of two concentrations (0.4 and 4 nM) of VIAN-c4551 or Vi1-123 after 2 h relative to their transit of both compounds in the absence of MDCK monolayers. Bars indicate mean ± SD, n ≥ 6. Individual values are shown. (b) Permeability coefficient (Papp) of VIAN-c4551 and Vi1-123.
Given that VIAN-c4551 is highly potent to inhibit VEGF-induced vascular permeability and highly efficient to cross epithelia, we investigated the effect of VIAN-c4551 in eye drops on VEGF-induced retinal vascular permeability.
VIAN-c4551 eye drops prevent VEGF-induced retinal vascular permeability
A single eye drop containing 0.5% VIAN-c4551 or vehicle was administered one hour before intravitreal injection of VEGF or PBS, and two hours later the retinal vascular leakage was evaluated by the extravasation of albumin. VEGF induced a significant 2–fold increase in retinal vascular permeability relative to PBS, and VIAN-c4551 prevented this effect in both rats (Fig. 3a) and mice (Fig. 3b). The higher basal vascular permeability values in mice vs. rats may be attributed to the greater damage caused by the intravitreal injection given the smaller size of the mouse eye. VIAN-c4551 did not modify the retinal levels of the tracer in the absence of VEGF.
VIAN-c4551 eye drops potently inhibit VEGF-induced retinal vascular permeability for up to 24 h. Retinal vascular permeability in rats (a) and mice (b) treated with a single eye drop containing 0.5% VIAN-c4551 or vehicle administered one hour before the intravitreal injection of 250 ng of VEGF or PBS. (c) Dose-response inhibition of eye drops containing different concentrations of VIAN-c4551. (d) Duration of the effect of a single 0.5% VIAN-c4551 eye drop administered at different times before the intravitreal injection of VEGF. Quantification of Evans blue-stained albumin extravasation was performed two hours after VEGF administration. Values are means ± SD. Individual eye values are shown. Sample size (n) was 15–22 (a), 7–16 (b), 9–23 (c), and 5–27 (d). #P < 0.002 vs. no VEGF (-), *P < 0.033, **P < 0.002, ***P < 0.001 vs. Veh (-), 2-way ANOVA, Šidák’s (a, b), 1-way ANOVA, Dunnett’s (c, d).
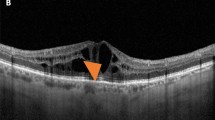
The efficacy of VIAN-c4551, profiled in rats, was dose-dependent, and the minimal effective dose was 0.005% (0.5 µg/eye drop) (Fig. 3c), confirming the high potency of VIAN-c4551. The duration of the effect was also profiled in rats by instilling 0.5% VIAN-c4551 or vehicle at different times before intravitreal injection of VEGF. The protective effect of VIAN-c4551 against the VEGF challenge was evident at 3 h, maximal at 12 h, and lasted up to 24 h after the eye drop (Fig. 3d). The effect of VIAN-c4551 eyedrops on retinal blood vessels was visualized by representative fluorescein angiography images of flat-mounted retinas from rats intravitreally injected with PBS or VEGF and evaluated 6 h after a single eyedrop containing vehicle or VIAN-c4551 (Fig. 4). VIAN-c4551 prevented the VEGF-induced leakage of retinal blood vessels, as evidenced by the reduced extravasation of FITC-dextran (arrows).
Visualization of VIAN-c4551 eye drop inhibition of VEGF-induced retinal vascular leakage. Representative fluorescein angiography images of flat-mounted retinas from rats treated with Veh or VIAN-c4551 eyedrops 4 h before intravitreal injection of PBS or VEGF and euthanized 2 h post-intravitreal injections. Retinal vasculature was visualized by FITC-dextran perfusion 1 h after intravitreal injection of VEGF and 1 h of circulation. Vascular leakage areas (arrowheads) and optic nerve (ON) are indicated. Scale bar = 1 mm.
The exceptional efficacy and 24–hour duration of VIAN-c4551 in eye drops suggested that VIAN-c4551 reaches the back of the eye at a high and sustained therapeutic concentration and warranted investigating its effect in the DME and DR rodent model induced by STZ, and its pharmacokinetic profile.
VIAN-c4551 in eye drops reverses diabetes-induced retinal vascular permeability
Excessive retinal vascular leakage is evident at 6 weeks of STZ-induced diabetes in rodents (Fig. 5)23. A single eye drop containing 0.5% VIAN-c4551 delivered once a day for the last five days suppressed the 2-fold increase in retinal vascular permeability due to diabetes in rats (Fig. 5a) and mice (Fig. 5b). The basal level of retinal vascular permeability in non-diabetic mice was smaller than that of non-diabetic rats, thereby, supporting our claim that the intravitreal injection by itself increases retinal vascular permeability in mice and not in rats (Fig. 3a, b).
VIAN-c4551 inhibits diabetes-induced retinal vascular permeability. Retinal vascular permeability in nondiabetic (NDB) and 6-week diabetic (DB) rats (a) and mice (b) treated daily for 5 days with a single eye drop containing 0.5% VIAN-c4551 or vehicle. The extravasation of Evans blue-stained albumin evaluated retinal vascular permeability 24 h after the last eye drop. Values are means ± SD. Individual eye values are shown. #P < 0.002 vs. NDB, **P < 0.002, ***P < 0.001 vs. Veh, (2-way ANOVA, Šidák’s).
The reduction of vascular leakage is indicative of the restoration of the blood-retinal barrier function and, thereby, proof-of-concept that VIAN-c4551 represents a potential, non-invasive therapy against DR and DME.
Ophthalmic instillation of VIAN-c4551 leads to high and sustained therapeutic concentration at the back of the eye
After a single eye drop, VIAN-c4551 reached the retina at levels ~ 10 and 30-fold greater than in the vitreous in rats and rabbits, respectively, and these amounts substantially exceeded the IC50 for inhibition of endothelial permeability (Fig. 6a, b). In rats, VIAN-c4551’s concentration in the retina was 32.8 µg g− 1 protein or ~ 4.3 µM, assuming a tissue density of 1 g mL− 1 and a retinal protein content of 10%30, and in the vitreous 300 ng mL− 1 or ~ 391 nM at 3 h post-dose (Fig. 6a). In rabbits, the pharmacokinetic (PK) profile defined a long absorption phase that peaked in the retina-choroid (Cmax 52 µg g− 1 protein or ~ 6.7 µM) and in the vitreous (Cmax 184 ng mL− 1 or ~ 239 nM) at 6 h and slightly declined thereafter (Fig. 6b). Even after 24 h, VIAN-c4551 exposure in retina-choroid (3.5 µg g− 1 protein or ~ 464 nM) and vitreous (10.6 ng mL− 1 or ~ 13.88 nM) were still ~ 3 and ~ 2 orders of magnitude higher than its IC50. PK parameters are summarized in Table 1. The PK profile was confirmed with VIAN-c4551-FITC. Despite that the FITC labeling reduced the transit of VIAN-c4551 across MDCK monolayers (Fig. 6c) and lowered its penetration to the retina-choroid and vitreous of rabbits (Fig. 6d), the kinetic profile of VIAN-c4551-FITC in both compartments was like that of the unlabeled compound, i.e., Cmax in retina-choroid was 1.3 µg g− 1 protein (~ 110 nM) at a Tmax of 6 h and maintained for 24 h at levels beyond IC50. Furthermore, VIAN-c4551-FITC was clearly visible in the retinal pigment epithelium of rats after its ophthalmic instillation (Fig. 7).
Ocular penetration and pharmacokinetics of VIAN-c4551. Concentration of VIAN-c4551 in the retina and vitreous of rats three hours after delivery of a single eye drop containing 0.5% VIAN-c4551 (a), and in the retina-choroid and vitreous of NZ rabbits at different time points after a 0.5% VIAN-c4551 eye drop (b). Values are mean ± SD, n ≥ 3; ng g− 1 protein is used for retina-choroid (left axis) and ng mL− 1 for vitreous (right axis). (c) Permeability coefficient (Papp) values of VIAN-c4551-FITC across MDCK epithelial cell monolayer compared to that of VIAN-c4551. (d) Concentration of VIAN-c4551-FITC in the retina-choroid and vitreous of rabbits at different time points after 0.5% VIAN-c4551-FITC eye drop instillation. Values are mean ± SD, n ≥ 3; ng g− 1 protein is used for retina-choroid (left axis) and ng mL− 1 for vitreous (right axis).
FITC-labeled VIAN-c4551 localizes in the retinal pigment epithelium of rats after eye drop administration. Representative confocal images of retinal sections from rats treated with 3 eye drops of Vehicle or 0.5% FITC-labelled VIAN-c4551 (VIAN-c4551-FITC) evaluated 6 h after the first eyedrop administration. VIAN-c4551-FITC accumulation is indicated (arrow heads). Retinal layers were stained with SytoxRed. Ganglion cell layer (GCL), inner nuclear layer (INL), outer nuclear layer (ONL), outer segment (OS), retinal pigment epithelium (RPE), choroid (CH), sclera (SCL). Scale bar = 100 μm.
Discussion
Excessive vascular leakage is a hallmark of retinal diseases with high prevalence, such as DME, DR, and age-related macular degeneration. The current therapy uses frequent anti-VEGF intravitreal injections, which are highly invasive, not always effective, cause complications, and associate with low compliance. Eye drop delivery is much more appealing as it is applied non-invasively by the patients themselves. However, topical administration faces delivery problems since only very low concentrations of drugs reach the retina6,31,32. Here, we report the eye drop delivery of VIAN-c4551, a small peptide derived from an endogenous protein that has outstanding anti-VEGF efficacy and pharmacokinetic properties, and has the potential to eliminate the need for repeated intravitreal injections.
VIAN-c4551 was developed as an effort to translate the anti-angiogenic vasoinhibin family of proteins (5.6 − 18 kDa) into an alternative therapeutic compound of 768 Da with improved pharmacological properties. In VIAN-c4551, the functional domain (His46-Gly47-Arg48) of vasoinhibin is contained within its 7 amino acid sequence (residues 45 to 51 of vasoinhibin) synthesized with D–amino acids in reverse order and cyclized to conserve potency and improve stability. VIAN-c4551 has the same vasoinhibin potency (IC50 = 150 pM) to inhibit VEGF-induced endothelial cell proliferation and is orally active to inhibit melanoma tumor growth and vascularization in mice8. Furthermore, the apoptotic, inflammatory, and fibrinolytic effects of vasoinhibin, which may be undesirable for antiangiogenic therapy, are in a different structural domain (residues 30 to 36) and, thereby, absent in VIAN-c455133.
Here, we report for the first time the inhibitory effect of VIAN-c4551 on excessive vascular permeability, another vascular action of vasoinhibin11,24. VIAN-c4551 blocked the VEGF-induced permeability of endothelial cell monolayers with the high potency (IC50 = 137 pM) of vasoinhibin. Such high potency is key for topical delivery to inhibit excessive retinal vascular leakage, as VIAN-c4551 needs to cross several ocular barriers and reach the retina at therapeutic concentrations. Overcoming ocular barriers depends on physicochemical properties, including size, charge, lipophilicity, solubility in water, stability, and permeability5,31. The oral bioavailability of VIAN-c4551 is indicative of its capacity to cross the intestinal system into the bloodstream and, thereby, of having adequate stability and permeability across epithelial barriers.
Aiming to develop the eye drop delivery of VIAN-c4551, we investigated its transit across MDCK cell epithelial monolayers. The MDCK cell system has been proposed as a model for predicting the penetration of drugs across the cornea27 and for studying the outer blood-retinal barrier28. VIAN-c4551 presented a high apparent permeability coefficient in MDCK cells, with values of magnitude over 10− 5 cm s− 1 and an average recovery of more than 50%. Therefore, VIAN-c4551 demonstrated the ability to cross a well-characterized epithelial barrier, and its transport across ocular epithelial barriers (corneal, conjunctiva, sclera, choroid, and retinal pigment epithelium) may not represent a relevant restriction for its eye drop absorption.
Encouraged by its high anti-VEGF potency and high penetrability, our efforts turned toward testing the in vivo efficacy of VIAN-c4551 in eye drops against the intravitreal injection of VEGF, a non-diabetic model of DME and DR34. A single eye drop containing 0.5% VIAN-c4551 prevented the increase in retinal vascular permeability induced by VEGF in rats and mice. The effect was dose-dependent and highly potent as the minimal effective dose was 0.005% (0.5 µg/eye/day). This dose is much lower than used for the ophthalmic instillation of antibodies (7.5 mg/eye/day), antibody fragments (0.2–0.5 mg/eye/day), or small molecules (0.3−1% /eye/day) in preclinical models of retinal microvascular diseases or clinical trials31,35,36. Moreover, the anti-VEGF effect of VIAN-c4551 lasted 24 h, suggesting a successful once-a-day topical ocular treatment.
VEGF is a major contributor to retinal vascular leakage in diabetes2. However, the pathologic cascade leading to DME and DR also involves other vasoactive substances like bradykinin37, bFGF38, and interleukin-1b39, all of which are inhibited by vasoinhibin7. By interacting with binding proteins (plasminogen activator inhibitor, urokinase, the urokinase receptor, and/or integrin α5β1)40,41 in endothelial cell membranes, vasoinhibin inhibits signaling pathways (Ras-Raf-MAPK, Ras-Tiam1-Rac1-Pac1, PI3K-Akt, and PLCg-IP3-eNOS) activated by several proangiogenic and vascular permeability factors (VEGF, bFGF, bradykinin, and interleukin 1β)7. Like vasoinhibin, VIAN-c4551 inhibits the proangiogenic and vasopermeability-inducing action not only of VEGF but also of other vasoactive factors such as bFGF and interleukin-1β [8], yet it does not bind to PAI-1, suggesting distinct or partially overlapping pathways33. In agreement with broad actions, vasoinhibin inhibits the increase in retinal vascular permeability induced by the intravitreal injection of vitreous from patients with DR42, and the ocular overexpression of vasoinhibin is more efficient than that of sFlt-1 (the secreted extracellular domain of the VEGF receptor 1) for blocking diabetes-induced retinal vascular permeability24. Addressing only the inhibition of VEGF action may, therefore, be of limited value, and the efficacy of VIAN-c4551 in diabetic conditions could exceed that of agents targeting only VEGF.
To investigate the broader benefit of the topical application of VIAN-c4551, we used the pharmacological induction of diabetes with STZ in rodents, one of the more commonly used DME and DR experimental models. In the STZ model of diabetes, increased retinal vascular permeability can occur as early as after 2 weeks of hyperglycemia34. Daily eye drops of 0.5% VIAN-c4551 for 5 days suppressed the retinal vascular leakage caused by 6 weeks of hyperglycemia in rats and mice. This result indicated that VIAN-c4551 in eye drops reverses the disruption of the blood-retinal barrier in diabetic rodents and, thereby, has potential curative properties in DME, DR, and other microvascular retinal diseases. The efficacy of VIAN-c4551 in the VEGF-non-diabetic model and the STZ-diabetic model is proof-of-concept that its topical delivery reaches the retina at therapeutic concentrations.
In agreement, VIAN-c4551 efficiently migrates to the back of the eye of rats and rabbits. A single 0.5% VIAN-c4551 eyedrop reached micromolar and nanomolar concentrations in the retina/choroid and vitreous, respectively, and the high levels were sustained for 24 h. The maximal concentrations in the retina/choroid (Cmax ~6.7 µM) and vitreous (Cmax ~239 nM) were 4 and 3 orders of magnitude higher, respectively, than the VIAN-c4551 IC50 (137.3 pM) to inhibit VEGF-induced endothelial cell permeability. These levels position VIAN-c4551 as the instilled compound with the highest measured concentration in the retina of rabbits (reviewed here6), the next one being dorzolamide hydrochloride, a glaucoma drug yielding a 2.8 µM retinal concentration after a 2% instillation dose6. However, pooling together the choroid and retina limits comparisons as it is difficult to conclude exposure in the retina. Along this line, confocal images demonstrated that, despite its low penetrability compared to the unlabeled peptide, VIAN-c4551-FITC eye drops effectively reached the retinal pigment epithelium of rats. Nevertheless, it should also be noted that albino animals confound the more general condition of pigmented animals, where binding to melanin can interfere with the ocular efficacy and distribution of drugs43.
A major question relates to the mechanisms mediating the exceptional ocular pharmacokinetic properties of VIAN-c4551. The fact that the concentration of VIAN-c4551 is lower in the vitreous than in the retina/choroid speaks in favor of migration through the conjunctiva-sclera-choroid-retina route and from the retina to the vitreous. This possibility is consistent with the hydrophilic nature of VIAN-c4551 and with absorption of hydrophilic compounds being facilitated by the larger paracellular pores and surface area of the non-corneal route31. However, VIAN-c4551 could also be absorbed through the cornea or through its clearance by the conjunctival blood vessels and subsequent retinal access via the retinal vasculature. Studies evaluating the ocular and systemic distribution of VIAN-c4551 following topical and intravenous delivery should help clarify these mechanisms. The physicochemical properties of VIAN-c4551 should also be addressed. Its small size, solubility in water, high permeability, and resistance to proteolysis very likely contribute to its efficient intraocular migration and 5-hour half-life in the inner ocular tissues. Finally, the relatively high retina and choroid levels of VIAN-c4551 after eye drop merit in-depth toxicological evaluation, including caspase-3 activation and the use of broader markers of cell death or inflammation to rule out putative off-target effects.
In summary, our findings suggest the feasibility of the topical self-administration of VIAN-c4551 in an outpatient setting that would represent a breakthrough in ophthalmology. Currently, no topical ocular formulations are available for treating microvascular retinal diseases. Several small molecules have undergone clinical trials but have not proceeded to the market despite having successful preclinical data6,44. The many reasons for failure include assuming the direct translation of positive results in rodents and rabbits to patients, which is limited by the anatomical and physiological differences between their eyes and the human eye31,45,46. However, the high concentrations of VIAN-c4551 achieved in the posterior segment of the eye indicate that its topical use for treating retinal diseases may be possible. This possibility is further acceptable due to the nature of VIAN-c4551 as an analog of vasoinhibin, an endogenous protein restraining the vascularity of ocular tissues9,47 that is downregulated in retinopathy of prematurity12, DR14, and DME15,16. Furthermore, the protective action of VIAN-c4551 against a broad range of vasoactive substances could benefit patients unresponsive to VEGF-therapy and its non-invasive route of administration offers the possibility of early intervention, a limitation of the anti-VEGF treatments typically reserved for the more severe stages of the disease48. Detailed physicochemical characterization, evaluation of safety profiles, and incorporation of large-scale production requirements warrant further research.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Cohen, S. R. & Gardner, T. W. Diabetic retinopathy and diabetic macular edema. Dev. Ophthalmol. 55, 137–146 (2016).
Nguyen, Q. D. et al. Vascular endothelial growth factor is a critical stimulus for diabetic macular edema. Am. J. Ophthalmol. 142, 961–969 (2006).
Cai, S. & Bressler, N. M. Aflibercept, bevacizumab or Ranibizumab for diabetic macular oedema: recent clinically relevant findings from drcr.net protocol T. Curr. Opin. Ophthalmol. 28, 636–643 (2017).
Falavarjani, K. G. & Nguyen, Q. D. Adverse events and complications associated with intravitreal injection of anti-VEGF agents: a review of literature. Eye 27, 787–794 (2013).
Boddu, S. H. S. et al. An update on strategies to deliver protein and peptide drugs to the eye. ACS Omega. 8, 35470–35498 (2023).
del Amo, E. M. Topical ophthalmic administration: can a drug instilled onto the ocular surface exert an effect at the back of the eye? Front Drug Deliv 2, (2022).
Clapp, C. et al. Regulation of blood vessels by prolactin and vasoinhibins. Adv. Exp. Med. Biol. 846, 83–95 (2015).
Robles, J. P. et al. The HGR motif is the antiangiogenic determinant of vasoinhibin: implications for a therapeutic orally active oligopeptide. Angiogenesis 25, 57–70 (2022).
Aranda, J. et al. Prolactins are natural inhibitors of angiogenesis in the retina. Invest. Ophthalmol. Vis. Sci. 46, 2947–2953 (2005).
Pan, H. et al. Molecular targeting of antiangiogenic factor 16K hPRL inhibits oxygen-induced retinopathy in mice. Invest. Ophthalmol. Vis. Sci. 45, 2413–2419 (2004).
Diaz-Lezama, N. et al. Diabetes enhances the efficacy of AAV2 vectors in the retina: therapeutic effect of AAV2 encoding vasoinhibin and soluble VEGF receptor 1. Lab. Invest. 96, 283–295 (2016).
Duenas, Z. et al. Prolactin in eyes of patients with retinopathy of prematurity: implications for vascular regression. Invest. Ophthalmol. Vis. Sci. 45, 2049–2055 (2004).
Zepeda-Romero, L. C. et al. Higher prolactin and vasoinhibin serum levels associated with incidence and progression of retinopathy of prematurity. Pediatr. Res. 81, 473–479 (2017).
Triebel, J., Huefner, M. & Ramadori, G. Investigation of prolactin-related vasoinhibin in Sera from patients with diabetic retinopathy. Eur. J. Endocrinol. 161, 345–353 (2009).
Nuñez-Amaro, C. D. et al. Levosulpiride increases the levels of prolactin and antiangiogenic vasoinhibin in the vitreous of patients with proliferative diabetic retinopathy. Transl Vis. Sci. Technol. 9, 27–27 (2020).
Núñez-Amaro, C. D. et al. Levosulpiride for the treatment of diabetic macular oedema: a phase 2 randomized clinical trial. Eye (Lond). 38, 520-528 (2024).
Moreno-Carranza, B. et al. Sequence optimization and glycosylation of vasoinhibin: pitfalls of Recombinant production. Protein Expr Purif. 161, 49–56 (2019).
Galfione, M. et al. Expression and purification of the angiogenesis inhibitor 16-kDa prolactin fragment from insect cells. Protein Expr Purif. 28, 252–258 (2003).
Baudin, B., Bruneel, A., Bosselut, N. & Vaubourdolle, M. A protocol for isolation and culture of human umbilical vein endothelial cells. Nat. Protoc. 2, 481–485 (2007).
Zamora, M. et al. Immunometric and functional measurement of endogenous vasoinhibin in human Sera. Front. Endocrinol. (Lausanne). 15, 1345996 (2024).
Sánchez, A. B., Calpena, A. C., Mallandrich, M. & Clares, B. Validation of an ex vivo permeation method for the intestinal permeability of different BCS drugs and its correlation with Caco-2 in vitro experiments. Pharmaceutics 11, 638 (2019).
Adán-Castro, E. et al. Sulpiride-induced hyperprolactinaemia increases retinal vasoinhibin and protects against diabetic retinopathy in rats. J. Neuroendocrinol. 34, e13091 (2022).
Ramirez-Hernandez, G. et al. Global deletion of the prolactin receptor aggravates Streptozotocin-Induced diabetes in mice. Front. Endocrinol. (Lausanne). 12, 619696 (2021).
Ramírez, M. et al. Vasoinhibin gene transfer by adenoassociated virus type 2 protects against VEGF- and diabetes-induced retinal vasopermeability. Invest. Ophthalmol. Vis. Sci. 52, 8944–8950 (2011).
Dash Gallery. Plotly: Noncompartmental Pharmacokinetics Analysis. (2021).
Dugina, V. B., Shagieva, G. S., Shakhov, A. S. & Alieva, I. B. The cytoplasmic actins in the regulation of endothelial cell function. Int. J. Mol. Sci. 22, 7836 (2021).
Rusinko, A., May, J., Liao, J., Namil, A. & Hellberg, M. A study of the enhanced corneal penetration of Moxifloxacin. Invest. Ophthalmol. Vis. Sci. 45, 4907 (2004).
Kadam, R. S., Scheinman, Robert, I. & Kompella, U. B. Pigmented-MDCK (P-MDCK) cell line with tunable melanin expression: an in vitro model for the outer Blood–Retinal barrier. Mol. Pharm. 9, 3228–3235 (2012).
Hellinger, E. et al. Comparison of brain capillary endothelial cell-based and epithelial (MDCK-MDR1, Caco-2, and VB-Caco-2) cell-based surrogate blood-brain barrier penetration models. Eur. J. Pharm. Biopharm. 82, 340–351 (2012).
Schimke, R. T. Effects of prolonged light deprivation on the development of retinal enzymes in the rabbit. J. Biol. Chem. 234, 700–703 (1959).
Löscher, M., Seiz, C., Hurst, J. & Schnichels, S. Topical drug delivery to the posterior segment of the eye. Pharmaceutics 14, 134 (2022).
Joussen, A. M. et al. The developing regorafenib eye drops for neovascular Age-related macular degeneration (DREAM) study: an open‐label phase II trial. Br. J. Clin. Pharmacol. 85, 347–355 (2019).
Robles, J. P. et al. Vasoinhibin’s apoptotic, inflammatory, and fibrinolytic actions are in a motif different from its antiangiogenic HGR motif. Endocrinology 165, bqad185 (2024).
Tang, L. H. C. et al. Animal Models of Diabetic Retinopathy (Part 2) in Experimental Animal Models of Human Diseases - An Effective Therapeutic Strategy (ed. Bartholomew, I.) https://doi.org/10.5772/intechopen.70589 (IntechOpen, 2017).
Csaky, K. G. et al. Clinical evaluation of pazopanib eye drops versus Ranibizumab intravitreal injections in subjects with neovascular age-related macular degeneration. Ophthalmology 122, 579–588 (2015).
Poor, S. H. et al. Topical VEGF receptor inhibitor, LHA510, did not demonstrate efficacy in a Proof-of-Concept study in patients with neovascular age-related macular degeneration (nv AMD). Invest. Ophthalmol. Vis. Sci. 59, 2394 (2018).
Gao, B. B. et al. Extracellular carbonic anhydrase mediates hemorrhagic retinal and cerebral vascular permeability through prekallikrein activation. Nat. Med. 13, 181–188 (2007).
Praidou, A. et al. Angiogenic growth factors and their inhibitors in diabetic retinopathy. Curr. Diabetes Rev. 6, 304–312 (2010).
Vincent, J. A. & Mohr, S. Inhibition of Caspase-1/Interleukin-1β signaling prevents degeneration of retinal capillaries in diabetes and galactosemia. Diabetes 56, 224–230 (2007).
Bajou, K. et al. PAI-1 mediates the antiangiogenic and profibrinolytic effects of 16K prolactin. Nat. Med. 20, 741–747 (2014).
Morohoshi, K., Mochinaga, R., Watanabe, T., Nakajima, R. & Harigaya, T. 16 kDa vasoinhibin binds to integrin alpha5 beta1 on endothelial cells to induce apoptosis. Endocr. Connect. 7, 630–636 (2018).
Garcia, C. et al. Vasoinhibins prevent retinal vasopermeability associated with diabetic retinopathy in rats via protein phosphatase 2A-dependent eNOS inactivation. J. Clin. Invest. 118, 2291–2300 (2008).
Rimpelä, A. K. et al. Implications of melanin binding in ocular drug delivery. Adv. Drug Deliv Rev. 126, 23–43 (2018).
Askew, B. C., Furuya, T., Edwards, D. S., Edwards, D. & & Ocular distribution and pharmacodynamics of SF0166, a topically administered αvβ3 integrin antagonist, for the treatment of retinal diseases. J. Pharmacol. Exp. Ther. 366, 244–250 (2018).
del Amo, E. M. et al. Pharmacokinetic aspects of retinal drug delivery. Prog Retin Eye Res. 57, 134–185 (2017).
Rodrigues, G. A. et al. Topical drug delivery to the posterior segment of the eye: addressing the challenge of preclinical to clinical translation. Pharm. Res. 35, 245 (2018).
Dueñas, Z. et al. Inhibition of rat corneal angiogenesis by 16-kDa prolactin and by endogenous prolactin-like molecules. Invest. Ophthalmol. Vis. Sci. 40, 2498–2505 (1999).
Antonetti, D. A., Silva, P. S. & Stitt, A. W. Current Understanding of the molecular and cellular pathology of diabetic retinopathy. Nat. Rev. Endocrinol. 17, 195–206 (2021).
Acknowledgements
The authors thank Fernando López Barrera, Xarubet Ruíz Herrera, Adriana González Gallardo, Alejandra Castilla, María A. Carbajo, and Martín García Servín for their excellent technical assistance.
Funding
This work was supported by the Secretaría de Educación, Ciencia, Tecnología e Innovación de la Ciudad de México (SECTEI/061/2023). JPR, MZ, EAC and LMSM receive postdoctoral fellowships from CONAHCYT.
Author information
Authors and Affiliations
Contributions
EAC and MZ designed, performed most research, and interpreted data. DGC, LMSM, JFGR, FM, and EA performed research. TB and JT contributed reagents. GME supervised and revised the study. JPR and CC conceived research, designed and supervised the study, interpreted the data, and wrote the manuscript. All authors reviewed and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
JPR, MZ, TB, JT, GME, and CC are inventors of a submitted patent application (WO/2021/098996), which is owned by the Universidad Nacional Autónoma de México (UNAM) and JT. JPR is the CEO and founder of VIAN Therapeutics Inc. MZ and CC are consultants for VIAN Therapeutics. Inc.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Adán-Castro, E., Zamora, M., Granados-Carrasco, D. et al. Topical ophthalmic administration of the antiangiogenic peptide VIAN-c4551 protects against experimental diabetic macular edema. Sci Rep 15, 26767 (2025). https://doi.org/10.1038/s41598-025-12331-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-12331-w