Abstract
This study investigates the effects of adding whey protein powder and Bifidobacterium quadruplex live bacterial tablets to enteral nutrition on nutritional indicators, complications, and prognosis in neurological ICU patients. Between April 2022 and December 2023, 100 patients requiring enteral nutrition in our hospital’s Neurology ICU were randomly assigned to four groups (25 each): EN1 (enteral nutrition only), EN2 (enteral nutrition + Bifidobacterium), EN3 (enteral nutrition + Bifidobacterium + whey protein), and EN4 (enteral nutrition + whey protein). Nutritional indicators (albumin, total protein, prealbumin), complication rates (diarrhea, constipation, gastric issues), prognosis indicators (hospital stay, ventilator use, lung infections, antibiotic use), and APACHE II scores were compared. This study has been approved by the Ethics Committee of the Affiliated Hospital of Zunyi Medical University, NO: KLL-2021-112. We confirm that all experiments were performed in accordance with relevant guidelines and regulations. After 7 days, EN3 and EN4 groups showed significantly improved nutritional indicators compared to EN1, with EN3 outperforming EN2. Diarrhea and gastric mucosal bleeding were less frequent in EN2 and EN3 compared to EN1 and EN4. APACHE II scores improved significantly in EN3 and EN4 post-treatment. EN3 had the lowest pulmonary infection rate and reduced antibiotic use, but hospitalization time differences were not significant across groups. Metabolic indicators showed no significant differences between groups. Supplementing enteral nutrition with whey protein powder and Bifidobacterium quadruplex improves nutritional status, reduces gastrointestinal complications, and enhances prognosis in critically ill neurological patients.
Trial registration: ChiCTR2300079322, (30/12/2023); Website where it was obtained: https://www.chictr.org.cn/bin/home
Similar content being viewed by others
Introduction
Critically ill neurological patients, such as those with severe cerebrovascular disease, traumatic brain injury, brain tumors, encephalitis, status epilepticus, or severe myasthenia gravis, frequently require admission to the Neurological Intensive Care Unit (NICU). Malnutrition is highly prevalent in this population, primarily due to a hypermetabolic state triggered by acute neurological injury. This state is characterized by excessive secretion of endogenous catabolic hormones (e.g., glucocorticoids, catecholamines), resulting in hyperglycemia, elevated energy expenditure, immunosuppression, heightened infection risk, and prolonged ICU/hospital stays1,2,3. Furthermore, the gut microbiota modulates disease progression through the gut-brain axis, and dysbiosis may exacerbate nutritional deficiencies, potentially leading to multiple organ dysfunction syndrome4,5,6,7,8,9.
During the 2–4 weeks post-brain injury, nearly two-thirds of patients exhibit resting energy expenditure (REE) reaching 200% of baseline levels10. REE varies across disease types and can be influenced by NICU interventions such as barbiturate administration, sedation, and temperature management (normothermia/hypothermia). Concurrently, metabolic processes like glycogenolysis and gluconeogenesis contribute to hyperglycemia and accelerated protein catabolism. Inadequate nutritional intake may precipitate negative nitrogen balance, adversely affecting outcomes10,11. Thus, early nutritional risk assessment and timely intervention are imperative. The Nutritional Risk Screening 2002 (NRS 2002) and Nutrition Risk in Critically Ill (NUTRIC) scores effectively evaluate nutritional status and disease severity. An NRS 2002 score > 3 indicates nutritional risk, while ≥ 5 denotes high risk12, with demonstrated high sensitivity and predictive value in ICU populations13,14.
For critically ill neurological patients, enteral nutrition (EN) is the preferred support modality over parenteral nutrition (PN), given its advantages in preserving gut function, modulating microbiota balance, and ultimately lowering infection risks and ICU stays15,16,17,18. However, emerging evidence suggests early full feeding (particularly EN) may be harmful, though mechanisms remain unclear19. Current guidelines therefore recommend hypocaloric nutrition (≤ 70% of energy expenditure) during the acute phase (days 1–3), progressively increasing to 80–100% of measured expenditure thereafter, with protein targets of 1.2–2.0 g/kg/day. While standard EN formulations provide caloric support during acute illness, their low protein content limits calorie-to-nitrogen ratios. Early protein supplementation with adequate calorie-to-nitrogen ratios may improve outcomes. Whey protein powder, primarily composed of whey protein, contains a variety of essential amino acids and is easily digestible and absorbable. It has been shown to effectively improve patients’ nutritional status, promote wound healing, facilitate functional recovery, and maintain muscle mass. Several studies have reported that early combined use of enteral nutrition formulations and whey protein powder has achieved favorable outcomes in the treatment of severe stroke, acute severe pancreatitis, severe pneumonia, and sepsis20,21. However, there is still limited clinical research on its application during the acute phase of neurocritical illness.
While healthy individuals maintain balanced gut microbiota, critical illness—combined with antibiotics and suboptimal feeding—can disrupt this equilibrium, impairing nutrient absorption22,23. Probiotics (e.g., Bifidobacterium quadruple viable tablets) may restore microbial balance, enhance gastrointestinal function, and improve nutrient absorption rates24.
Given that our neurology department operates a dedicated neurological intensive care unit (NeuroICU) and has previously relied on a single EN1 enteral nutrition regimen, this study introduces a combined nutritional intervention. The intervention integrates enteral nutritional formulas, whey protein powder, and Bifidobacterium quadruple viable tablets to provide early nutritional support for neurocritical patients. We aim to evaluate the effects of this approach on patients’ nutritional status, gastrointestinal complications, protein metabolism, and overall prognosis. Additionally, we will compare the advantages and disadvantages of each nutritional regimen to identify simpler and more cost-effective enteral nutrition strategies for this patient population.
Methods
Study design
This study is a one-week parallel-group quadruple-blind randomized controlled trial (RCT) aimed at improving nutritional indicators and assessing prognosis in neuro-ICU patients using different nutritional protocols, with participants, researchers, data analysts, and care providers all being unaware of the treatment assignments. We used the CONSORT reporting guidelines25 and obtained written informed consent from each patient or their immediate family member. The study was approved by the Research Ethics Committee of the Affiliated Hospital of Zunyi Medical University (NO: KLL-2021-112). Due to influences such as the economic situation of patients’ families and the insufficiency of experimental equipment in the hospital, some indicators were not collected as planned in the protocol. Participants were randomly assigned according to the randomization table generated by SPSS 29.0. Blood samples were collected bedside from patients before enrollment and one week after starting nutritional support (Day 7). Throughout the treatment process, the occurrence of complications was monitored.
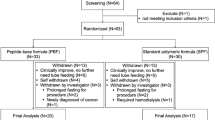
Participants
A total of 179 patients were selected from the affiliated hospital of Zunyi Medical University who were hospitalized in the neurological critical care unit and required enteral nutritional support treatment from April 2022 to December 2023. During the study, 34 cases had less than 7 days of enteral nutrition; 15 patients were excluded from the study as they or their families did not agree to enteral nutrition; 16 patients were not within the age range of 18 to 80 years; 12 patients had incomplete data; 2 patients were pregnant. Ultimately, a total of 100 patients were randomly divided into 4 groups (Group EN1: Enteral Nutrition Solution; Group EN2: Enteral Nutrition Solution + probiotics; Group EN3: Enteral Nutrition Solution + probiotics + Whey Protein Powder; Group EN4: Enteral Nutrition Solution + Whey Protein Powder), with 66 males and 34 females completing the study, Fig. 1.
Inclusion criteria
(1) Age between 18 and 80 years; (2) Body Mass Index (BMI) between 18.0 and 24.0 kg/m²; (3) Inability to eat independently or presence of consciousness disturbance upon hospital admission, with a Glasgow Coma Scale (GCS) score ≤ 12 points; (4) Nutrition Risk Screening 2002 (NRS 2002) score ≥ 3 points; (5) Acute Gastrointestinal Injury (AGI) classified as grade 0 to 1; (6) Duration of enteral nutrition implementation and supplementation with probiotics and whey protein powder exceeds one week.
Exclusion criteria
-
(1)
Patients with critical conditions, such as respiratory dysfunction (PaO2 < 60 mmHg and/or PaCO2 > 60 mmHg), cardiovascular dysfunction (blood pressure < 90/60 mmHg), hepatic and renal dysfunction (TBIL > 240 µmol/L, Cr > 500 µmol/L), lipid metabolism disorder (triglycerides > 4–5 mmol/L), acidosis (serum lactate > 3–4 mmol/L, pH < 7.2); (2) Patients with severe ischemic enteropathy, intestinal perforation, acute gastrointestinal hemorrhage, and intestinal obstruction; (3) Individuals who received albumin infusion before enrollment; (4) Patients allergic to whey protein; (5) Pregnant and lactating women.
Baseline survey
-
1.
Collect patient data such as gender, age, hypertension, diabetes, coronary heart disease, history of gastrointestinal ulcers, body weight, height, etc., obtained through a questionnaire survey.
-
2.
The degree of nutritional risk is assessed by the Nutritional Risk Screening (NRS2002) score.
-
3.
Prognosis is assessed by the Acute Physiology and Chronic Health Evaluation (APACHE II score).
-
4.
Laboratory examination related indicators: Albumin, Total Protein, Prealbumin, Urea, Creatinine, Creatinine Clearance, etc.
Experimental equipment
-
(1)
Nasogastric Tube: Nasogastric tube from Suzhou Wei Kang Medical Devices Co., Ltd., model and specification: Gastric tube silicone 5.33 mm (F16), medical device registration number: Suzhou Device Registration Approval 20,172,141,817.
-
(2)
Enteral Nutrition Pump: Shenzhen Maiketian Bio-Medical Technology Co., Ltd., registration number: Guangdong Device Registration Approval 20,192,140,403, model: EP60.
-
(3)
Enteral Nutritional Formula (1.0 Kcal/ml, each 500 ml contains 20.0 g of protein, 61.5 g of carbohydrates, 19.5 g of fat, 10 g of dietary fiber, manufactured by Nutricia Pharmaceutical Co., Ltd.). On the first day of enteral nutrition implementation, 1/2 to 1/3 of the total calories were given, and from 2 to 3 days to the full amount, with intravenous supplementation for any unmet caloric needs during the period.
-
(4)
Bifidobacterium Quadruple Viable Tablets (Silian Kang), manufactured by Hangzhou Yuanda Bio-Pharmaceutical Co., Ltd., specification: 0.5 g per tablet, usage: 3 tablets per time, 3 times per day, diluted with 20 ml of warm water and then administered through a nasogastric tube; the control group was given 20 ml of warm water placebo at the same time.
-
(5)
Whey Protein Powder: The product used is from Tomson Best Health, 450 g per can, containing approximately 320 kcal of calories, with 360 g of protein, mainly consisting of concentrated whey protein and soy protein isolate. National Food Health Number: G20140134. (Daily protein powder amount = actual protein requirement - protein provided by enteral nutritional formula, administered in 2 divided doses through a nasogastric tube, each diluted with 100 ml of warm water; the control group was given 100 ml of warm water placebo at the same time).
Nutrition implementation plan
EN1 Group: Enteral nutrition formula;
EN2 Group: Enteral nutrition formula + Bifidobacterium quadruple viable tablets;
EN3 Group: Enteral nutrition formula + Bifidobacterium quadruple viable tablets + Whey protein powder;
EN4 Group: Enteral nutrition formula + Whey protein powder;
On the first day of implementing enteral nutrition, administer 1/2 ~ 1/3 of the total caloric requirement, that is, during the acute phase (1–3 d), provide low-calorie nutrition (not exceeding 70% of energy expenditure); after 3 days, increase to 80–100%, and supplement through the intravenous route if the caloric goal is not met. Protein is supplemented at a rate of 1.2 ~ 2.0 g· kg-1·d-1. After one week all patients were given regular calories and protein for nutritional support according to their condition.
In the process of nutritional support, it is necessary to monitor the patient’s gastrointestinal tolerance during feeding, and according to the patient’s tolerance gradually increase the dose of nutritional solution, and gradually reach the patient’s need for the regular amount within 3 days. In order to reduce the risk of aspiration, the head of the bed was slightly elevated about 30°~40° during the nutritional support process; in order to maintain the smoothness and cleanliness of the nutritional tubes, the temperature and concentration of the nutritional solution should be appropriate, and before and after the treatment and at the time of the interruption and restarting, the tubes were rinsed by using 20 ~ 30 ml of lukewarm boiled water, and oral care was carried out. During the process, the nurses returned to pump the gastric residual fluid every 4 h to know the shape, colour and volume of the residual fluid, to monitor the complications of the feeding process; and checked the depth of the nutritional tube to avoid dislodging or excessive depth, as well as the head of the bed elevation, and the changes in the airbag pressure of the patients who were on the ventilator.
Observation content
Primary outcome
-
1.
Nutritional indicators: Before starting nutritional support and on the morning of the 7th day after starting nutritional support, fasting venous blood was sent for testing to determine the levels of Total Protein (TP), Albumin (ALB), and Prealbumin (PA).
-
2.
Complication-related indicators: During the nutritional support process, the incidence of related complications such as diarrhea, gastric retention, constipation, and gastrointestinal bleeding within 7 days was observed.
-
Gastric retention: Monitored every 4–6 h for Gastric Residual Volume (GRV), with GRV ≥ 250 ml considered as gastric retention.
-
Diarrhea: Currently, there is no unified recommendation for diarrhea, which is generally judged based on the frequency, consistency, and volume of bowel movements. The Critical Care Nutrition (CCN) defines it as having 3–5 bowel movements or a stool volume of ≥ 750 ml within 24 h.
-
Constipation: Defined as no bowel movement for more than 3 days or fewer than 3 bowel movements per week.
-
Gastrointestinal bleeding: Judged by the color of the patient’s stool, vomiting or aspiration of bloody material, positive results on gastric or fecal occult blood tests, etc.
-
-
3.
Prognosis-related indicators: Before starting nutritional support and on the 7th day after starting nutritional support, the APACHE II score was assessed; the number of cases with pulmonary infection and mechanical ventilation during the nutritional support period was recorded, along with the antibiotics used by each patient, the duration of mechanical ventilation, and the total hospital stay. For newly identified pulmonary infections, we will make a judgment based on the following criteria: a body temperature rise above 38 °C within 48 h after admission, accompanied by respiratory symptoms such as cough and sputum production, possible auscultatory findings of crackles in the lungs, and increased infection indicators in blood tests such as white blood cells, C-reactive protein, procalcitonin, etc., and new inflammatory lesions on chest CT scans compared to admission.
Secondary outcomes
Metabolic-related indicators: Before nutritional support and after 7 days, fasting venous blood was sent for testing to measure the levels of serum urea, creatinine, and endogenous creatinine clearance rate.
Management of complications
When the patient vomiting, abdominal distension, diarrhoea and other complications occur during the feeding process, the nurse first detects the gastric residual volume, if it is greater than 250 ml, slow down the rate of nutrient infusion, reduce the amount of nutrient solution, if there is no improvement, then give metoclopramide, montelukast for symptomatic treatment, if the GCV > 250 ml, suspension of the feeding, and according to the patient’s condition to restart the nutritional support; When constipation occurs, according to the patient’s condition, appropriate amount of water can be injected through the gastric tube, and if there is no relief, a emema glycerini or enema can be used to assist defecation; when abnormal colour of gastric residue is found in the retracted stomach, gastric fluid should be sent for examination to check the occult blood test, if the result suggests a positive result and there is the possibility of gastrointestinal haemorrhage, then the administration of proton pump inhibitors such as Pantoprazole enteric-coated tablets, Omeprazole enteric-coated tablets, etc., can be considered to protect the gastric mucous membrane. If the retracted gastric contents contain more than 100 ml of bloody material, EN should be discontinued; if the bloody contents are less than 100 ml, the feeding rate can be reduced to continue EN treatment until the possibility of gastrointestinal bleeding is ruled out before resuming the normal feeding rate.
Sample size Based on an estimated effect size of d = 0.80, alpha level = 0.05 (one-tailed as direction was hypothesised), power = 0.90, we estimated that we would require a total of n = 23 participants per group and therefore aimed to recruit 25 per group based on a 10% dropout rate.
Randomization and masking
Participants were randomized 1:1:1:1by SPSS29.0 to generate a corresponding random number, sort the random numbers in the order of smallest to largest, select the corresponding sample size in the order of the random numbers according to the pre-set sample size of each treatment group, randomly assign the research subjects to the different experimental groups according to the corresponding random numbers, and do a good job of grouping concealment.
Participant Blinding: Participants were informed that they would receive a standardized nutritional support protocol but were not provided with specific details about the treatment. To maintain blinding, all nutritional formulations were prepared in identical containers and labeled with codes that did not reveal the treatment group.
Caregiver Blinding: Nutritional formulations were prepared by nurses who were not involved in patient care, in a separate pharmacy unit. The formulations were delivered to caregivers in coded containers, ensuring that caregivers were unaware of the specific treatment being administered.
Researcher Blinding: Researchers responsible for data collection were kept unaware of the treatment assignments. All data collection forms and records used coded identifiers instead of specific treatment group names. This ensured that the researchers collecting the data remained unaware of the treatment allocation throughout the process.
Data Analyst Blinding: Data analysis was conducted by an independent statistical team that was unaware of the treatment assignments. All data provided to the data analysts were coded. The analysis was based on the coded data, ensuring that the analysts remained unaware of the specific treatments throughout the analysis process.
Quality control
-
1.
Selective bias: the enrolment of the study subjects was carried out by the neurology department responsible for the management of the neurointensive care unit level of primary care or above in strict accordance with the Na-exclusion criteria and exclusion criteria, and was reviewed by the deputy chief physician.
-
2.
Information collection bias: two attending neurologists with specialised training were selected to assess the NRS2002 score, APACH II score and other subjective indicators, and their mean values were calculated. If significant differences were found, a supervising physician would be asked to reassess.
-
3.
Each healthcare worker participating in this study must be trained in relevant nutritional support expertise, and the charge nurse remains unchanged during the patient’s nutritional support. The enteral nutrition patients need to be monitored every day, and the treatment team leader will be responsible for supervising the whole treatment and operation process.
Statistical methods
The database was constructed using Excel spreadsheet and statistically analysed using SPSS 29.0 with two-sided test, when p < 0.05, it indicated that the difference was statistically significant. For continuous data obeying normal distribution, they were described as mean ± standard deviation (‾x ± s), and multiple group comparisons were performed using one-way analysis of variance (ANOVA); while two-by-two comparisons were later performed using the LSD method. For non-normally distributed data, they were described as `median (interquartile spacing)’ and compared between groups using the Kruskal-Wallis H-test, followed by two-way comparisons using the Dunn-Bonferroni method. For count data, percentage calculations were performed, and between-group comparisons were made using the chi-square test, and then two-by-two comparisons were made using the chi-square split method. The experiment contained four groups and six tests were performed with a significance level of α = 0.05, so the significance level for the chi-square split was α = 0.00833.
Results
Participants’ characteristics
The baseline data of the four groups of patients, such as gender, age, weight, history of hypertension, history of coronary heart disease, history of diabetes, history of peptic ulcer, use of antibiotics, use of nasogastric tube, nasoenteric tube, type of disease, and basal nutritional status, were compared between the groups, and no significant differences were observed (P > 0.05), and the four groups of patients were comparable, Tables 1 and 2.
Analysis of nutritional indicators
Serum total protein, albumin, and prealbumin were compared between groups of patients before and after treatment using the Kruskall-Wallis H test, and the results showed that no significant difference was seen in the comparison between groups before treatment, which was not statistically significant (P = 0.205); the difference was statistically significant after 7 days of treatment (corrected P < 0.001), and the results were confirmed by the Dunn- Bonferroni test line two-by-two pairwise comparisons found that EN3 and EN4 groups were significantly higher than EN1 group, EN3 group was significantly higher than EN2 group (corrected P < 0.05), and the differences between EN2 and EN1, EN4 group, and EN3 and EN4 group were not statistically significant (corrected P > 0.05), Table 3; Fig. 2; Table 4; Fig. 3; Table 5; Fig. 4.
Complications occurring during nutritional support
The incidence of diarrhoea, constipation, gastric retention and gastric mucosal bleeding during the treatment period was compared among the four groups. The results showed that the incidence of gastric retention and constipation complications did not differ significantly between the groups (P > 0.05), whereas the incidence of diarrhoea and gastric mucosal haemorrhage differed statistically significantly between the groups (P < 0.05). A two-by-two comparison by the chi-square partition method revealed that the incidence of diarrhoea was significantly lower in the EN2 and EN3 groups relative to the EN1 and EN4 groups (P < 0.00833), the incidence of gastric mucosal bleeding was significantly lower in the EN2 group than in the EN1 group (P < 0.00833), the incidence of gastric mucosal bleeding was significantly lower in the EN3 group than in the EN1 and EN4 groups (P < 0.00833), while there was no statistically significant difference in diarrhoea and gastric mucosal haemorrhage between the EN1 and EN4 groups, EN2 and EN3 groups, and gastric mucosal haemorrhage between the EN2 and EN4 groups (P > 0.00833), Table 6.
Analysis of prognosis-related indicators
(1) Comparing the APACHE II scores of the patients in each group before and after treatment, the scores of the four groups decreased after treatment compared with those before treatment, and through one-way ANOVA, we found that there was no significant difference in the APACHE II scores before treatment among the different groups (P = 0.564); there was a significant difference in APACHE II scores after treatment among the four groups (P = 0.000), and after the LSD test, we found that that the scores of the EN3 and EN4 groups were significantly lower than those of the EN1 and EN2 groups (P < 0.05), while the differences between the EN1 and EN2 groups and between the EN3 and EN4 groups were not statistically significant (P > 0.05), Table 7, and Fig. 5.
(2)Comparing the time of mechanical ventilation and ventilator use in each group, we found no statistical significance between groups (P > 0.05). By comparing the chi-square test between multiple groups, we found that there was a significant difference in the rate of new-onset lung infections (P < 0.05), and after the chi-square partition method comparison between groups, the results showed that the rate of new-onset lung infections in the EN3 group was significantly lower than that in the EN1 and EN2 groups (P < 0.00833), while there was no statistically significant difference between the EN1 and EN2 groups, the EN1 and EN4 groups, the EN2 and EN4 groups, and the EN3 and EN4 groups were not statistically different from each other (P > 0.00833). Comparing the duration of antibiotic use and hospital between the four groups, the difference was found to be statistically significant by the Kruskall-Wallis H test (P < 0.05), and the duration of antibiotic use in the EN3 group was found to be significantly less than that in the EN1 and EN2 groups by the Dunn-Bonferroni test (P < 0.05), and there was no statistically significant difference between the EN1 vs. EN2 group, the EN1 vs. EN4 group, EN2 vs. EN4 group, and EN3 vs. EN4 group were not statistically different from each other (P > 0.05). In addition, the length of stay in the EN3 group was also significantly shorter than that in the EN1 group, but there were no statistical differences (corrected P > 0.05) between the EN2 group and the EN1, EN3 and EN4 groups, and between the EN4 group and the EN1 and EN3 groups, Table 8, and Fig. 6.
Comparison of the duration of antibiotic use and hospital after treatment in four groups of patients. Note Using the letter marking method, marking without the same letter indicates that the comparison of the two groups is P < 0.05, and having the same letter indicates that the comparison of the two groups is P > 0.05.
Comparison of metabolism-related indicators
Comparing the metabolic indexes: serum urea, creatinine, and endogenous creatinine clearance after treatment in the four groups of patients, the differences between the groups of serum post-treatment urea, creatinine, and endogenous creatinine clearance were not statistically significant when compared by the Kruskall-Wallis H-test (P = 0.22, P = 0.86, P = 0.84), Table 9.
Discussion
Research results and clinical significance
In the assessment of nutritional support efficacy, serum albumin, prealbumin, and total protein are commonly used as indicators. Several researchers have compared the effects of high-protein and non-high-protein diets on critically ill patients and found that patients in the high-protein nutrition group had higher nutritional indicators such as albumin and prealbumin compared to the non-high-protein group20,26,27. This is similar to the results of the current study, where the EN3 and EN4 groups added whey protein powder (> 1.2 g/kg/day). After seven days of nutritional support, it was found that the groups with added whey protein powder (EN3 and EN4) had significantly higher nutritional indicators than the groups without added whey protein powder (EN1 and EN2), with statistical differences. Furthermore, through the analysis of protein metabolism-related indicators, no statistical differences were found between the groups after seven days of nutritional support, further proving that whey protein powder can also improve the nutritional indicators of neurological critically ill patients and has a high safety profile.
In terms of gastrointestinal tolerance, the results of this study show that the incidence of diarrhea and gastric mucosal bleeding in the group supplemented with Bifidobacterium quadruple live bacteria tablets was significantly lower than in the non-supplemented group (P < 0.05), further indicating that Bifidobacterium quadruple live bacteria tablets can improve feeding complications in patients. Comparing the EN1 group with the EN4 group and the EN2 group with the EN3 group, that is, using protein powder as an observation indicator of whether it affects gastrointestinal tolerance, no statistical differences were found between the groups (P > 0.00833), indicating that the intake of protein powder does not significantly affect gastrointestinal complications. A double-blind, controlled, randomized, multicenter study on critically ill patients found that the incidence of complications such as gastric retention, vomiting, diarrhea, and constipation was statistically no different between the control group given a high-protein formula and the other groups28, which is similar to the results of the current study.
In terms of prognostic indicators, the results of this study show that the APACHE II scores of the EN3 and EN4 groups were significantly lower than those of the EN1 and EN2 groups (P < 0.05), suggesting that the combination of protein powder and Bifidobacterium quadruple live bacteria tablets may improve the prognosis of neurological critically ill patients. Looking at the incidence of new pulmonary infections, the duration of antibiotic use, and the length of hospital stay, the EN3 group was significantly less than the EN1 and EN2 groups, with no statistical difference between the EN3 and EN4 groups, further indicating that whey protein powder can improve the prognosis of neurological critically ill patients. The reason may be related to the high protein intake that can maintain a good nutritional status and muscle mass29, thereby enhancing immune function and promoting the recovery of neurological function.
Shortcomings and future directions
①Before initiating nutrition, it is necessary to train the NICU bedside nurses on the relevant precautions. They must strictly provide nutritional support according to the patient’s enrollment status and adjust the EN rate based on the patient’s tolerance during the process, making the nursing work cumbersome and the clinical implementation more challenging. ②In this study, whey protein powder was added to the EN process, which may have introduced errors during preparation. ③The sample size included in this study is relatively small. ④The duration of EN in this study was 7 days, which is relatively short. It is unknown whether extending the duration of EN support would have an impact on the results. We will consider longer intervention periods or follow-up phases in future studies to comprehensively evaluate the long-term effects of these nutritional interventions. ⑤Subgroup analyses by age, disease severity, or nutritional risk (e.g., NRS > 5) were not conducted. Such analyses may provide deeper insights into the study outcomes. Future studies should consider incorporating these factors into the design phase for subgroup analyses to more comprehensively assess the effects of nutritional interventions. ⑥Although this study employed a quadruple-blind design, perfect blinding is challenging to fully achieve in practice, especially due to the potential recognition of the physical characteristics of the nutritional formulations (such as color and odor). Future studies may consider using more advanced blinding techniques to further minimize bias.
Conclusion
For patients with neurological critical illness, the addition of Bifidobacterium quadruple live bacteria tablets to standard enteral nutrition formulas may reduce the incidence of enteral nutrition-related complications, such as diarrhea and gastric mucosal bleeding. Furthermore, the combination of whey protein powder and Bifidobacterium quadruple live bacteria tablets with standard enteral nutrition formulas may improve patients’ nutritional status, thereby contributing to improved prognosis.However, this study has some limitations, including the short intervention period and the limited sample size, which may affect the generalizability of the results. Future studies should consider longer intervention periods, larger sample sizes, and more detailed subgroup analyses to further validate these findings.
Data availability
The data used in this study has been made available,further inquiries can be directed to the corresponding author.
References
Carteron, L. et al. Semi-elemental versus polymeric formula for enteral nutrition in brain-injured critically ill patients: a randomized trial. (2021). Crit. care (Lond. Engl.) 25(1): 31 .
Helmy, A. et al. The cytokine response to human traumatic brain injury: Temporal profiles and evidence for cerebral parenchymal production . J. Cereb. Blood Flow. Metabol. Off. J. Int. Soc. Cereb. Blood Flow. Metabol. 31(2), 658–670 (2011).
Kurtz, P., Rocha, E. E. M. & Nutrition therapy glucose control, and brain metabolism in traumatic brain injury: A multimodal monitoring approach . Front. NeuroSci. 14, 190 (2020).
Hanscom, M., Loane, D. J. & Shea-donohue, T. Brain-gut axis dysfunction in the pathogenesis of traumatic brain injury . J. Clin. Investig., 131(12). (2021).
Sasso, J. M. et al. Gut Microbiome-Brain alliance: A landscape view into mental and Gastrointestinal health and disorders . ACS Chem. Neurosci. 14(10), 1717–1763 (2023).
Rusch, J. A., Layden, B. T. & Dugas, L. R. Signalling cognition: The gut microbiota and hypothalamic-pituitary-adrenal axis . Front. Endocrinol. 14, 1130689 (2023).
Bonaz, B. The gut-brain axis in parkinson’s disease . Rev. Neurol. 180(1–2), 65–78 (2024).
Erny, D. et al. Host microbiota constantly control maturation and function of microglia in the CNS . Nat. Neurosci. 18(7), 965–977 (2015).
Doroszkiewicz, J., Groblewska, M. & Mroczko, B. The role of gut microbiota and gut-Brain interplay in selected diseases of the central nervous system . Int. J. Mol. Sci., 22(18). (2021).
Abdullah, M, I. et al. Syed saadun tarek wafas W W,. Determination of calorie and protein intake among acute and sub-acute traumatic brain injury patients. Chin. J. Traumatol. Zhonghua Chuang Shang za Zhi, 23(5), 290-4. (2020).
Doley, J. Enteral nutrition overview. Nutrients, 14(11). (2022).
Singer, P. et al. ESPEN practical and partially revised guideline: Clinical nutrition in the intensive care unit . (2023). Clin. Nutr. Edinb. Scotl. 42(9), 1671–1689 .
Sheean, P. M. et al. Utilizing multiple methods to classify malnutrition among elderly patients admitted to the medical and surgical intensive care units (ICU) . (2013). Clin. Nutr. Edinb. Scotl. 32(5), 752–757 .
Lew, C. C. H. et al. Association between malnutrition and clinical outcomes in the intensive care unit: A systematic review [Formula: see text] . JPEN J. Parenter. Enter. Nutr. 41(5), 744–758 (2017).
Cadena, A. J. et al. The benefits of parenteral nutrition (PN) versus enteral nutrition (EN) among adult critically ill patients: what is the evidence? A literature review . J. Intensive Care Med. 35(7), 615–626 (2020).
Liu, F. et al. Comparison of two different threshold values for the measurement of gastric residual volume on enteral nutrition support in the neurocritically ill patients . Front. Nutr. 9, 871715 (2022).
Baiu, I. & Spain, D. A. Enteral nutrition. Jama, 321(20), 2040. (2019).
Quiroz-olguÍn, G. et al. The effect of enteral stimulation on the immune response of the intestinal mucosa and its application in nutritional support . Eur. J. Clin. Nutr. 75(11), 1533–1539 (2021).
Reintam Blaser, A., Rooyackers, O. & Bear, D. E. How to avoid harm with feeding critically ill patients: A synthesis of viewpoints of a basic scientist, dietitian and intensivist . (2023). Crit. Care (Lond. Engl.), 27(1), 258 .
Van ruijven, I. M. et al. High protein provision of more than 1.2 g/kg improves muscle mass preservation and mortality in ICU patients: A systematic review and meta-analyses. Clin. Nutr. (Edinb. Scotl.) 42(12), 2395–2403 (2023).
Suzuki, G. et al. Effect of high-protein nutrition in critically ill patients: A retrospective cohort study . Clin. Nutr. ESPEN. 38, 111–117 (2020).
Hillestad, E. M. R. et al. Gut bless you: The microbiota-gut-brain axis in irritable bowel syndrome . World J. Gastroenterol. 28(4), 412–431 (2022).
Zhou, P. et al. The gut-lung axis in critical illness: Microbiome composition as a predictor of mortality at day 28 in mechanically ventilated patients . BMC Microbiol. 23(1), 399 (2023).
Wan, G. et al. Effects of probiotics combined with early enteral nutrition on endothelin-1 and C-reactive protein levels and prognosis in patients with severe traumatic brain injury . J. Int. Med. Res. 48(3), 300060519888112 (2020).
Schulz, K. F., Altman, D. G., Moher, D. & for the CONSORT Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. PLoS Med. 7(3), e1000251 (2010).
Tedeschi-jockers, F. et al. A new high protein-to-energy enteral formula with a Whey protein hydrolysate to achieve protein targets in critically ill patients: A prospective observational tolerability study . Eur. J. Clin. Nutr. 76(3), 419–427 (2022).
Looijaard, W. et al. Achieving protein targets without energy overfeeding in critically ill patients: A prospective feasibility study . (2019). Clin. Nutr. (Edinb. Scotl.), 38(6): 2623–2631 .
Van Petit, A. R. H. & De waele, L. J, et al. Very high intact-protein formula successfully provides protein intake according to nutritional recommendations in overweight critically ill patients: a double-blind randomized trial . (2018). Crit. Care (Lond. Engl.), 22(1): 156 .
Mundi, M. S. et al. Current perspective for tube feeding in the elderly: From identifying malnutrition to providing of enteral nutrition . Clin. Interv. Aging. 13, 1353–1364 (2018).
Acknowledgements
ZX, SYH, and ZXJ designed research; CP and LZ conducted research; CP and YZB analyzed data; and CP, ZX and CY wrote the paper. ZGF optimizated of the grammatical structure and the revision of the manuscript. XZC, YBH and ZJ had primary responsibility for final content. All authors read and approved the final manuscript.
Funding
Guizhou Provincial Science and Technology Programme (NO: 202242940112230149).
Author information
Authors and Affiliations
Contributions
ZX, SYH, and ZXJ designed research; CP and LZ conducted research; CP and YZB analyzed data; and CP, ZX and CY wrote the paper. ZGF optimizated of the grammatical structure and the revision of the manuscript. XZC, YBH and ZJ had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
This study has been approved by the Ethics Committee of the Affiliated Hospital of Zunyi Medical University, NO: KLL-2021-112.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, X., Zhang, J., You, Zb. et al. Effects of enteral nutrition protocols on nutritional indicators and prognosis in neurological ICU patients: a randomized controlled trial. Sci Rep 15, 30916 (2025). https://doi.org/10.1038/s41598-025-12650-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-12650-y