Abstract
Airway mucus plugs are frequently observed on chest computed tomography (CT) scans in patients with chronic obstructive pulmonary disease (COPD). However, the association between the presence of mucus plugs and the risk of lung cancer in COPD patients has not been thoroughly investigated. This study aimed to determine whether mucus plugs are associated with an increased risk of lung cancer in COPD patients. We conducted a retrospective cohort study of COPD patients treated at a teaching hospital between 2004 and 2020. The primary outcome was the incidence of lung cancer, with secondary outcomes including lung cancer histologic subtypes. Among 616 COPD patients, 256 (41.7%) had mucus plugs, while 360 (58.4%) did not. Over a median observation period of 66 months, 56 patients developed lung cancer. Mucus plugs were significantly associated with an increased risk of lung cancer (adjusted HR = 2.281 [95% CI = 1.192–4.363], P-value = 0.013). Notably, this association was significant even in patients who did not meet conventional lung cancer screening criteria. Patients with mucus plugs also had a significantly higher incidence of squamous cell carcinoma (P-value = 0.001), but not adenocarcinoma. In COPD patients, the presence of mucus plugs is associated with a higher incidence of lung cancer, particularly squamous cell carcinoma.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a major global health burden and a leading cause of death, characterized by persistent airflow limitation, chronic inflammation of the airways, and mucus dysfunction1,2,3. COPD patients are at higher risk for several comorbidities, with lung cancer being one of the leading causes of death4,5. Regardless of smoking history, age, or sex, individuals with COPD have a markedly increased risk of developing lung cancer, with a four- to six-fold higher incidence compared to the general population6. The majority of lung cancers in COPD patients are diagnosed at advanced stages, resulting in poor survival rates7. Consequently, early detection of lung cancer has been considered a critical issue in COPD patients.
Lung cancer screening with low-dose computed tomography (LDCT) has demonstrated significant mortality reduction in high-risk populations8,9,10. The United States Preventive Services Task Force (USPSTF) 2021 guideline recommended annual LDCT screening for individuals aged 50 to 80 years with a significant smoking history11. However, even COPD patients who do not meet the current LDCT screening criteria remain at substantial risk for lung cancer12. Therefore, it is crucial to identify promising biomarkers that can more precisely predict the future risk of lung cancer development in COPD patients.
Imaging biomarkers, including mucus plugs, have gained attention in COPD patients13,14. Mucus plugs are found in 25–67% of COPD patients during chest CT scans15,16. They are linked to worse clinical outcomes, including higher mortality, more frequent exacerbations, and faster decline in lung function. Given the observed association between mucus plugs and cancer-related mortality in COPD patients, it is plausible that mucus plugs could be linked to the development and progression of lung cancer in this population17. The presence of mucus plugs, which correlate with a worsened prognosis and are commonly associated with chronic inflammation, lung function impairment, and tissue damage, may create a microenvironment favorable to carcinogenesis. This potential connection suggests that mucus plugs could serve as valuable biomarkers for identifying COPD patients at elevated risk of lung cancer development.
Therefore, our study aims to elucidate the association between mucus plugs detected in medium- to large-sized airways on chest CT scans and the incidence of lung cancer in COPD patients.
Methods
Study design and participants
This retrospective cohort study evaluated patients who were consistently followed for COPD management at a teaching hospital between January 2004 and December 2020. The diagnosis of COPD was confirmed by pulmonologists using electronic medical records, based on the identification of chronic respiratory symptoms, relevant risk factors, and non-fully reversible airflow obstruction, defined as a post-bronchodilator forced expiratory volume in 1 s (FEV1)/forced vital capacity (FVC) ratio of less than 0.7.
Patients were included if they met the following criteria: (1) a baseline chest computed tomography (CT) scan was performed within three months of the initial COPD diagnosis to ensure accurate assessment of airway and parenchymal abnormalities at the time of diagnosis; (2) a minimum clinical follow-up duration of one year with at least two outpatient visits per year, which allowed for adequate longitudinal monitoring of disease course and clinical events; and (3) at least one follow-up chest CT scan conducted after the baseline CT, enabling reliable evaluation of incident lung cancer throughout the observation period.
Patients were excluded under the following conditions: (1) baseline chest CT findings were suggestive of pre-existing lung cancer (e.g., spiculated nodules, lobulated masses, or mediastinal lymphadenopathy), as such features would confound the evaluation of mucus plug–related cancer risk; (2) no follow-up chest CT was available during the observation period, which precluded reliable assessment of newly developed lung cancer; and (3) a concurrent diagnosis of current asthma or interstitial lung disease at baseline, in order to minimize diagnostic overlap and ensure a homogeneous COPD cohort.
The eligible patients were divided into two groups based on the presence of mucus plugs. In addition, patients were further stratified by mucus plug scores into three groups: 0, 1–3, and ≥ 4. These cut-offs were determined based on findings from our exploratory pilot analyses. The eligible patients were categorized into subgroups based on age, pack years, smoking history, and established lung cancer screening criteria, including National Lung Screening Trial (NLST), Nederlands-Leuvens Longkanker Screenings Onderzoek (NELSON) and 2021 USPSTF criteria (Supplementary S1)8,9,11.
Variables
At the time of COPD diagnosis, we collected baseline demographic and clinical information, including age, sex, body mass index (BMI), smoking status, pack-years, Charlson comorbidity index, presence of comorbid conditions, dyspnea severity using the Modified Medical Research Council (mMRC) grade, complete blood count results, lung function parameters (post-bronchodilator FEV1, FVC, FEV1/FVC ratio, and FEF25 − 75%), as well as prescribed inhaled treatments.
Mucus plug measurements
The assessment of mucus plugs was performed according to a standardized visual scoring protocol adapted from a previously published study18. Mucus plugs were defined as complete luminal occlusion of segmental bronchi with diameters of approximately 2–10 mm on axial CT images, with preserved visibility of distal airways. A total of 18 bronchopulmonary segments were evaluated per patient, with the lingula considered a separate lobe. The number of involved segments was recorded as the mucus plug score, ranging from 0 to 18.
The initial screening for mucus plugs was conducted at the bronchopulmonary segmental level on baseline chest CT scans by thoracic radiologists. Following this, two investigators (KNJ and HWL) evaluated the mucus plug scores across the entire CT scan. Calibration was achieved by reviewing 100 randomly selected scans with mucus plugs and 100 without, ensuring the inter-reader agreement’s correlation coefficient reached 0.9 or greater. Discrepancies in the assessment of mucus plug scores during calibration were resolved through discussion between the investigators. The reliability of the final analysis for mucus plug presence and scores was evaluated using Cohen’s Kappa coefficient and the correlation coefficient.
Outcomes
The primary outcome was the incidence of histologically confirmed lung cancer. Lung cancer was identified through routine clinical evaluations and follow-up imaging studies, with subsequent pathological confirmation obtained via biopsy. The secondary outcome was lung cancer histologic subtypes, including non-small cell lung cancer (NSCLC) subtypes such as squamous cell carcinoma and adenocarcinoma, as well as other histologic subtypes. Sensitivity analysis was conducted using landmark analysis, defining time points at 3 and 5 years after the baseline CT to evaluate whether the cumulative incidence of lung cancer is consistently higher in the mucus plug group after each time point.
Statistical analysis
Baseline characteristics were compared between groups using the chi-square test or Fisher’s exact test for categorical variables and Student’s t-test or Wilcoxon rank sum test for continuous variables. Time to lung cancer incidence was analyzed using Kaplan-Meier survival curves and the log-rank test. The hazard of lung cancer incidence was assessed using Cox proportional hazards models. The multivariable Cox regression model included covariates that showed statistical significance in the univariable analysis. The proportional hazards assumption was assessed using the Schoenfeld residuals test, with non-significant P-values indicating that the assumption was not violated. A significance threshold of P-value < 0.05 was applied to all tests, with results reported alongside 95% confidence intervals. Statistical analyses were conducted using R software (version 4.3.3; R Foundation, Vienna, Austria).
Ethics
Our study was conducted in compliance with the ethical standards outlined in the Declaration of Helsinki. The Institutional Review Board of Seoul Metropolitan Government-Seoul National University (SMG-SNU) Boramae Medical Center granted approval for this study (IRB no. 30-2024-1), and waived the requirement for written informed consent.
Results
A total of 1,012 patients with COPD who underwent baseline chest CT scan were reviewed. Among them, 7 were excluded due to suggestive of lung cancer in baseline CT, 368 patients due to lack of any chest CT scan following the baseline scan, 11 due to radiologic findings suggestive of ILD, and 10 due to concurrent asthma treatment. Consequently, 616 patients were deemed eligible (Fig. 1). Of these, 256 patients (41.7%) had mucus plugs on their baseline CT scans, while 360 patients (58.4%) did not. The distribution of mucus plug scores is depicted in Supplementary Fig. S2. The inter-reader agreement for the presence of mucus plugs, as measured by Cohen’s Kappa coefficient, was 0.87 (95% CI, 0.84–0.90), and the correlation coefficient for mucus plug scores was 0.83.
Baseline characteristics
The demographic and clinical characteristics of the patients are summarized in Table 1. Notable differences were identified between the mucus plug and no mucus plug groups. Patients in the mucus plug group were older, had a lower BMI, and a higher pack-year among ever-smokers. This group also exhibited a greater prevalence of respiratory comorbidities such as bronchiectasis and chronic bronchitis. In terms of dyspnea severity, the mucus plug group had higher patients with mMRC ≥ 2. Blood tests revealed a higher neutrophil count in the mucus plug group. Pulmonary function tests showed significantly lower post-bronchodilator FEV1, FEV1/FVC ratio, and FEF25 − 75% in the mucus plug group.
Mucus plugs and lung cancer
During the observation period of median 66 (interquartile range [IQR] = 36–103) months, we identified 56 cases of histologically confirmed lung cancer. Demographic and clinical characteristics were evaluated according to the incidence of lung cancer (Supplementary Table S1). Mucus plugs were more frequently observed (38.4% vs. 73.2%, P-value < 0.001) and mucus plug score was higher (0 ([0–2] vs. 2 [0–4], P-value < 0.001) in the baseline CT of patients who developed lung cancer. Kaplan-Meier curves indicated that time to lung cancer incidence was shorter in individuals with mucus plugs or a higher mucus plug score (Fig. 2 and Supplementary Fig. S2). Landmark analysis model showed that the time to lung cancer incidence significantly differed after the 3-year and 5-year landmark point (log-rank P-value < 0.001 and 0.002, respectively; Supplementary Fig. S3).
In the univariable Cox regression model, the presence of mucus plugs and higher mucus plug scores were significantly associated with an increased risk of lung cancer, with unadjusted hazard ratios (uHRs) of 3.220 (95% confidence interval [CI] = 1.736–5.972, P-value < 0.001) and 1.115 (95% CI = 1.038–1.197, P-value = 0.003), respectively (Supplementary Table S2).
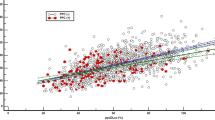
In the multivariable Cox regression model, the presence of mucus plugs was significantly associated with an increased risk of lung cancer (adjusted HR [aHR] = 2.281 [95% CI = 1.192–4.363], P-value = 0.013) (Table 2). Notably, several subgroups demonstrated significant findings, including those who did not meet conventional lung cancer screening criteria. Patients aged ≥ 75 years had an aHR of 4.709 (95% CI = 1.283–17.290, P-value = 0.019). Individuals with less than 30 pack-years of smoking history exhibited a substantially elevated risk, with an aHR of 11.490 (95% CI = 2.023–65.243, P-value = 0.006). Additionally, never smokers or ex-smokers had an aHR of 3.108 (95% CI = 1.286–7.511, P-value = 0.012). The presence of mucus plugs also significantly increased the risk of lung cancer among participants who did not meet the NLST (aHR = 4.236, 95% CI = 2.005–8.951, P-value < 0.001), NELSON (aHR = 4.068, 95% CI = 1.919–8.622, P-value < 0.001) and 2021 USPSTF (aHR = 4.601, 95% CI = 1.974–10.720, P-value < 0.001) screening criteria. Furthermore, there was a trend of increasing HRs with higher mucus plug scores, with the adjusted model indicating a more pronounced risk at higher scores (Fig. 3). Particularly, a significant linear trend was observed in the risk of lung cancer for mucus plug scores ranging from ≥ 2 to ≥ 6, with an increasing adjusted hazard ratio (P-value for trend = 0.034, Supplementary Table S3).
The association between mucus plug score with lung cancer incidence. Adjusted hazard ratios were calculated by controlling for covariables such as age, sex, smoking history, pack-years, Charlson comorbidity index, history of asthma, history of pulmonary tuberculosis, blood neutrophil (%), and post-bronchodilator FEV1/FVC.
Mucus plugs and histology subtypes
The incidence of lung cancer across different histological subtypes was analyzed in patients with and without mucus plugs (Fig. 2). The mucus plug group demonstrated a significantly higher incidence of squamous cell carcinoma (P-value = 0.001) and other histological subtypes (P-value = 0.003), but not adenocarcinoma, compared to the group without mucus plugs.
In Cox regression analyses, the presence of mucus plugs was significantly associated with an increased risk of non-small cell lung cancer in the unadjusted model (HR = 2.594, 95% CI = 1.370–4.911, P-value = 0.003) (Table 3). However, this association lost statistical significance after multivariable adjustments. In contrast, the presence of mucus plugs was consistently and significantly associated with an increased risk of squamous cell carcinoma across both univariable (uHR = 3.757, 95% CI = 1.596–8.841, P-value = 0.002) and multivariable models (aHR = 2.985, 95% CI = 1.207–7.383, P-value = 0.018). There was no statistically significant association found between mucus plugs and adenocarcinoma in either model.
Discussion
In this study, the presence of mucus plugs identified on baseline chest CT scans was significantly associated with an increased risk of lung cancer in COPD patients. Specifically, patients with mucus plugs had a higher incidence of lung cancer, with a more pronounced risk observed in those with a greater mucus plug burden. The association was particularly significant for squamous cell carcinoma, while no significant relationship was observed with adenocarcinoma. These findings persisted even after adjusting for multiple potential confounders. Notably, the increased risk of lung cancer was also evident in COPD patients who did not meet conventional lung cancer screening criteria. Our findings suggest that mucus plugs could serve as an important imaging biomarker for identifying COPD patients at higher risk of lung cancer, beyond the traditionally recognized high-risk groups.
In recent years, significant efforts have been made to identify biomarkers for the early detection of lung cancer. Traditionally, various molecular biomarkers have been explored, including DNA methylation patterns, circulating tumor DNA, exhaled breath, and specific protein markers, all of which have demonstrated varying degrees of sensitivity and specificity19. Functional biomarkers, such as the rate of lung function decline, have also proven useful in identifying individuals at high risk for lung cancer who may benefit from screening20. Several radiologic features have been evaluated as potential imaging biomarkers for predicting the future development of lung cancer. Among these, a meta-analysis revealed a significant association between emphysema, particularly centrilobular emphysema, and the development of lung cancer21. A novel aspect of our study is that it is the first to examine the association between the presence of mucus plugs in medium- to large-sized airways and lung cancer incidence in COPD patients. Notably, significant associations were observed in several subgroups, including those who did not meet conventional lung cancer screening criteria. Consequently, the detection of mucus plugs may warrant chest CT follow-up, potentially increasing early detection of lung cancer in COPD patients.
The potential mechanisms underlying the association between mucus plugs and lung cancer can be explained by several hypotheses. First, chronic inflammation in COPD may be a potent driver of lung cancer development. An increase in mucus plugs detected on chest CT was associated with a higher frequency of neutrophilic inflammation-dominant exacerbations in COPD18. Since chronic airway inflammation is a known risk factor for lung cancer, it is plausible that the presence of mucus plugs indicates sustained inflammation, which in turn may be associated with a higher risk of lung cancer22. Mucus plugs can exacerbate infection and inflammation by creating an environment conducive to microbial growth23. Aberrant cytokine signaling in chronic inflammation can further stimulate cell growth, differentiation, and apoptosis24. This chronic inflammation in COPD can lead to lung damage and increased cell division, thereby raising the risk of mutations and carcinogenesis25. Second, hypoxic conditions in COPD patients, which may be exacerbated by mucus plugs, could also contribute to lung cancer development. Hypoxia triggers the activation of the transcription factor hypoxia-inducible factor 1-alpha, which is similarly activated in cancer cells due to the local hypoxic environment. This factor promotes glycolysis, supports cellular immortalization through telomerase activation, inhibits differentiation, and can prevent apoptosis, all of which are processes involved in cancer development26. Third, oxidative stress plays a critical role in the promotion and progression of lung cancer through mechanisms such as DNA damage27. Reactive oxygen species (ROS) are produced due to airway obstruction and inflammation caused by mucus plugs. Mitochondria, being the primary source of ROS within cells, contribute to oxidative stress, and the mitochondrial dysfunction observed in COPD could be linked to the development of lung cancer28. Fourth, genetic mutations may explain the relationship between mucus plugs and lung cancer. In fact, the oncogenic P53 mutant protein is associated with increased mucus production and the prolonged survival of metaplastic bronchial mucus cells29.
As discussed above, chronic inflammation and oxidative stress may be major driving mechanisms leading to lung cancer in COPD patients27. This suggests that anti-inflammatory or antioxidant agents might have potential for lung cancer prevention. N-acetylcysteine (NAC), erdosteine, and ambroxol are mucolytic agents that also possess anti-inflammatory and antioxidant properties30. Given the significant role of oxidative stress and inflammation, these therapies might benefit patients by reducing the incidence of lung cancer. However, this view has been challenged due to inconsistent results from antioxidant treatments in COPD. NAC treatment was associated with lung cancer progression by disrupting the ROS-p53 axis in mouse and human lung tumor cells31. However, NAC promoted the development of lung adenocarcinoma in mice, while it decreased lung oxidative damage and cell senescence and protected against lung emphysema32. Although ambroxol may have anti-inflammatory effects, it does not directly inhibit lung tumor development in rodent models33. Therefore, while mucus plugs in COPD patients may represent a potential treatable trait, there are currently no medications proven to prevent lung cancer development. While our study focused on radiologic assessment of mucus plugs, the integration of molecular biomarkers may enhance prognostic precision in future research34.
The present study has several limitations. First, as a retrospective observational study, it cannot establish a causal relationship between the presence of mucus plugs and the development of lung cancer. Second, the study population was exclusively Asian, which may limit the generalizability. Third, our study assessed mucus plugs that were found in medium- to large-sized airways, which may underestimate the true extent of mucus plugs. Fourth, CT scans were acquired over a 15-year period, during which technological advancements likely introduced variability in image resolution and slice thickness, potentially affecting the detection of mucus plugs and early-stage cancers. Fifth, functional assessment data regarding bronchial resistance (e.g., impulse oscillometry or body plethysmography) were not routinely available due to the retrospective design and variable pulmonary function test protocols over the study period. Future prospective investigations incorporating standardized bronchial resistance measurements may better clarify the physiological implications of mucus plug burden and strengthen its role as a potential imaging biomarker.
In conclusion, the presence of mucus plugs in medium- to large-sized airways is associated with an increased risk of lung cancer, particularly squamous cell carcinoma, in COPD patients. Notably, this association was significant even in patients who did not meet conventional lung cancer screening criteria, highlighting the potential of mucus plugs as a valuable imaging biomarker for early lung cancer detection. These findings suggest that incorporating mucus plug assessment into routine COPD management may help identify patients at higher risk for lung cancer, warranting further prospective studies to confirm and expand upon these results.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- ILD:
-
Interstitial lung disease
- LDCT:
-
Low-dose computed tomography
- NAC:
-
N-Acetylcysteine
- NELSON:
-
Nederlands-Leuvens Longkanker Screenings Onderzoek
- NLST:
-
National Lung Screening Trial
- ROS:
-
Reactive oxygen species
- USPSTF:
-
The United States Preventive Services Task Force
References
World Health Organization (WHO) website. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (Accessed August 2024).
Celli, B. et al. Definition and nomenclature of chronic obstructive pulmonary disease: time for its revision. Am. J. Respir Crit. Care Med. 206, 1317–1325. https://doi.org/10.1164/rccm.202204-0671PP (2022).
Diaz, A. A. et al. Airway-Occluding mucus plugs and mortality in patients with chronic obstructive pulmonary disease. Jama 329, 1832–1839. https://doi.org/10.1001/jama.2023.2065 (2023).
Miller, J. et al. Comorbidity, systemic inflammation and outcomes in the ECLIPSE cohort. Respir Med. 107, 1376–1384. https://doi.org/10.1016/j.rmed.2013.05.001 (2013).
Labaki, W. W. et al. Causes of and clinical features associated with death in tobacco cigarette users by lung function impairment. Am. J. Respir Crit. Care Med. 208, 451–460. https://doi.org/10.1164/rccm.202210-1887OC (2023).
Young, R. P. et al. COPD prevalence is increased in lung cancer, independent of age, sex and smoking history. Eur. Respir J. 34, 380–386. https://doi.org/10.1183/09031936.00144208 (2009).
Tanoue, L. T., Tanner, N. T., Gould, M. K. & Silvestri, G. A. Lung cancer screening. Am. J. Respir Crit. Care Med. 191, 19–33. https://doi.org/10.1164/rccm.201410-1777CI (2015).
Aberle, D. R. et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl. J. Med. 365, 395–409. https://doi.org/10.1056/NEJMoa1102873 (2011).
de Koning, H. J. et al. Reduced Lung-Cancer mortality with volume CT screening in a randomized trial. N Engl. J. Med. 382, 503–513. https://doi.org/10.1056/NEJMoa1911793 (2020).
Henschke, C. I. et al. Survival of patients with stage I lung cancer detected on CT screening. N Engl. J. Med. 355, 1763–1771. https://doi.org/10.1056/NEJMoa060476 (2006).
Krist, A. H. et al. Screening for lung cancer: US preventive services task force recommendation statement. Jama 325, 962–970. https://doi.org/10.1001/jama.2021.1117 (2021).
Park, H. Y. et al. Chronic obstructive pulmonary disease and lung cancer incidence in never smokers: a cohort study. Thorax 75, 506–509. https://doi.org/10.1136/thoraxjnl-2019-213732 (2020).
Morgan, L., Choi, H., Reid, M., Khawaja, A. & Mazzone, P. J. Frequency of incidental findings and subsequent evaluation in Low-Dose computed tomographic scans for lung cancer screening. Ann. Am. Thorac. Soc. 14, 1450–1456. https://doi.org/10.1513/AnnalsATS.201612-1023OC (2017).
Regan, E. A. et al. Identifying Smoking-Related disease on lung cancer screening CT scans: increasing the value. Chronic Obstr. Pulm Dis. 6, 233–245. https://doi.org/10.15326/jcopdf.6.3.2018.0142 (2019).
Dunican, E. M. et al. Mucus plugs and emphysema in the pathophysiology of airflow obstruction and hypoxemia in smokers. Am. J. Respir Crit. Care Med. 203, 957–968. https://doi.org/10.1164/rccm.202006-2248OC (2021).
Okajima, Y. et al. Luminal plugging on chest CT scan: association with lung function, quality of life, and COPD clinical phenotypes. Chest 158, 121–130. https://doi.org/10.1016/j.chest.2019.12.046 (2020).
Mettler, S. K. et al. Airway-occluding mucus plugs and Cause-specific mortality in chronic obstructive pulmonary disease. Am. J. Respir Crit. Care Med. 209, 1508–1510. https://doi.org/10.1164/rccm.202401-0121LE (2024).
Jin, K. N. et al. Mucus plugs as precursors to exacerbation and lung function decline in COPD patients. Arch. Bronconeumol. https://doi.org/10.1016/j.arbres.2024.07.017 (2024).
Seijo, L. M. et al. Biomarkers in lung cancer screening: achievements, promises, and challenges. J. Thorac. Oncol. 14, 343–357. https://doi.org/10.1016/j.jtho.2018.11.023 (2019).
Lee, H. W. et al. Rapid FEV(1) decline and lung cancer incidence in South Korea. Chest 162, 466–474. https://doi.org/10.1016/j.chest.2022.03.018 (2022).
Yang, X. et al. Association between chest CT-defined emphysema and lung cancer: A systematic review and Meta-Analysis. Radiology 304, 322–330. https://doi.org/10.1148/radiol.212904 (2022).
Adcock, I. M., Caramori, G. & Barnes, P. J. Chronic obstructive pulmonary disease and lung cancer: new molecular insights. Respiration 81, 265–284. https://doi.org/10.1159/000324601 (2011).
Worlitzsch, D. et al. Effects of reduced mucus oxygen concentration in airway Pseudomonas infections of cystic fibrosis patients. J. Clin. Invest. 109, 317–325. https://doi.org/10.1172/jci13870 (2002).
Dranoff, G. Cytokines in cancer pathogenesis and cancer therapy. Nat. Rev. Cancer. 4, 11–22. https://doi.org/10.1038/nrc1252 (2004).
Caramori, G. et al. Unbalanced oxidant-induced DNA damage and repair in COPD: a link towards lung cancer. Thorax 66, 521–527. https://doi.org/10.1136/thx.2010.156448 (2011).
Kobliakov, V. A. Mechanisms of tumor promotion by reactive oxygen species. Biochem. (Mosc). 75, 675–685. https://doi.org/10.1134/s0006297910060015 (2010).
Durham, A. L. & Adcock, I. M. The relationship between COPD and lung cancer. Lung Cancer. 90, 121–127. https://doi.org/10.1016/j.lungcan.2015.08.017 (2015).
Schetter, A. J., Heegaard, N. H. & Harris, C. C. Inflammation and cancer: interweaving microrna, free radical, cytokine and p53 pathways. Carcinogenesis 31, 37–49. https://doi.org/10.1093/carcin/bgp272 (2010).
Chand, H. S. et al. A genetic variant of p53 restricts the mucous secretory phenotype by regulating SPDEF and Bcl-2 expression. Nat. Commun. 5, 5567. https://doi.org/10.1038/ncomms6567 (2014).
Barnes, P. J. Oxidative stress-based therapeutics in COPD. Redox Biol. 33, 101544. https://doi.org/10.1016/j.redox.2020.101544 (2020).
Sayin, V. I. et al. Antioxidants accelerate lung cancer progression in mice. Sci. Transl Med. 6, 221ra215. https://doi.org/10.1126/scitranslmed.3007653 (2014).
Breau, M. et al. The antioxidant N-acetylcysteine protects from lung emphysema but induces lung adenocarcinoma in mice. JCI Insight 4. https://doi.org/10.1172/jci.insight.127647 (2019).
Yoshida, S. et al. Effects of the expectorant drug ambroxol hydrochloride on chemically induced lung inflammatory and neoplastic lesions in rodents. J. Toxicol. Pathol. 31, 255–265. https://doi.org/10.1293/tox.2018-0012 (2018).
D’Ascanio, M. et al. Surfactant protein B plasma levels: reliability as a biomarker in COPD patients. Biomedicines 11. https://doi.org/10.3390/biomedicines11010124 (2023).
Author information
Authors and Affiliations
Contributions
H.W.L. have full access to all data in the study, supervised the study, and take responsibility for the integrity of the data and accuracy of analysis. H.W.L. and S.J.K contributed to protocol design, data collection and analysis, and writing of the manuscript. H.J.L. and H.M.P. contributed to data collection. J.K.L., E.Y.H., K.N.J. and D.K.K contributed to the data collection and interpretation of data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Reporting checklist
The authors have completed the STROBE reporting checklist.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, S.J., Park, H., Lee, H.J. et al. Mucus plug and lung cancer incidence in patients with COPD. Sci Rep 15, 30193 (2025). https://doi.org/10.1038/s41598-025-13501-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-13501-6