Abstract
Parkinson’s disease (PD) is a clinically heterogeneous neurodegenerative disorder whose trajectory is shaped by progressive motor impairment and cortical dysfunction. However, longitudinal studies integrating clinical scales with direct neurophysiological assessments remain scarce. In this 4.5-year cohort study, we conducted one of the longest clinical-electrophysiological follow-ups in PD to date, evaluating 22 patients across early and advanced stages using both Movement Disorder Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) scores and transcranial magnetic stimulation (TMS). We demonstrate that the cortical silent period (CSP), a marker of GABAergic inhibition, progressively lengthens over time and is associated with motor decline, suggesting its potential as a dynamic biomarker of disease progression. Resting motor threshold (rMT) and motor asymmetry also deteriorated longitudinally, with changes most pronounced following the COVID-19 pandemic—suggesting that environmental stressors may accelerate PD pathophysiology. Unlike prior short-term studies, our findings reveal persistent cortical reorganization over several years, independent of sex, and underscore the clinical relevance of TMS-derived metrics in tracking disease progression. These findings suggest that CSP may serve as a non-invasive and scalable biomarker for monitoring Parkinson’s disease progression and informing neurophysiological endpoints in future therapeutic studies.
Similar content being viewed by others
Introduction
Parkinson’s disease (PD) is a progressive neurodegenerative disorder characterized by motor symptoms such as bradykinesia, rigidity, resting tremor, and postural instability, alongside a broad spectrum of non-motor symptoms that significantly impair patients’ quality of life1,2,3. Changes resulting from the disease’s progression can be clinically correlated with the severity of motor and non-motor symptoms through instruments such as the Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS)4,5,6. Today, it is well recognized that the pathophysiology of PD extends beyond the degeneration of dopaminergic neurons in the substantia nigra, involving widespread neurodegenerative processes across cortical and subcortical areas, as well as non-dopaminergic systems7,8,9,10,11,12. However, clinical scales cannot directly assess changes at these levels.
Transcranial magnetic stimulation (TMS) is a non-invasive technique used to assess various neurophysiological parameters in the primary motor cortex, providing insights into cortical excitability (e.g., resting motor threshold [rMT], active motor threshold [aMT], motor-evoked potential [MEP] amplitude, input-output curves), inhibition (e.g., cortical silent period [CSP], short-interval intracortical inhibition [SICI], long-interval intracortical inhibition [LICI]), and plasticity (e.g., repetitive TMS [rTMS], theta burst stimulation [TBS])13,14,15. In PD, TMS may contribute to the diagnosis, prognosis, and assessment of disease progression, complementing clinical evaluations16,17. However, long-term studies integrating neurophysiological and clinical measures in PD remain scarce.
TMS studies have identified consistent neurophysiological alterations in PD, including reduced SICI and prolonged CSP, which suggest impaired GABAergic inhibition18,19,20,21. These measures may serve as diagnostic biomarkers, aiding in the differentiation of PD from atypical parkinsonian syndromes, and may offer prognostic information. For instance, CSP duration has been associated with motor symptom severity, as measured by MDS-UPDRS-III scores, and may help predict disease progression. Alterations in short-interval intracortical facilitation (SICF), thought to reflect increased glutamatergic activity, worsen with the disease stage and correlate with complications such as levodopa-induced dyskinesia. Other measures, such as short-latency afferent inhibition (SAI), have been linked to gait and cognitive impairments, further supporting the role of TMS in monitoring disease severity. However, most findings to date are based on cross-sectional studies, and longitudinal data are needed to validate the clinical utility of these neurophysiological markers22,23.
Remembering that PD is a neurodegenerative process, the combined study of clinical features and neurophysiological measures over time in this type of patient becomes important. Furthermore, it could enhance our understanding of the neurophysiological alterations that occur during the disease course, facilitate comprehensive patient follow-up, and predict disease evolution by establishing possible correlations between clinical scales and TMS-derived measurements. However, only a few studies have conducted clinical and TMS follow-ups in a cohort of PD subjects, with these follow-ups not exceeding one year24,25,26. Therefore, in this longitudinal observational study, we followed a cohort of individuals with PD from 2018 to 2023, encompassing pre- and post-pandemic periods. By integrating standardized clinical assessments, such as the MDS-UPDRS, with TMS-derived neurophysiological measures, including rMT, CSP, and MEP amplitudes, we aimed to investigate the evolution of motor and non-motor symptoms in conjunction with neurophysiological parameters and their potential associations. This is one of the few studies to conduct a comprehensive follow-up in a group of subjects with PD, and, to our knowledge, the most extensive clinical-electrophysiological follow-up in PD reported to date.
Results
Recruitment and sample characteristics
Twenty-two patients with PD met the inclusion criteria and consented to participate, comprising an equal distribution of 11 females and 11 males. The cohort was stratified into early-stage PD (15 participants with Hoehn & Yahr stage ≤ 2) and advanced-stage PD (7 participants with Hoehn & Yahr stage > 2). The demographic and clinical characteristics of the entire cohort and its subgroups are detailed in Table 1. Notably, none of the participants tested positive for COVID-19 or reported known exposure to infected individuals during the study period.
Changes in clinical outcomes
Longitudinal analyses revealed no significant sex-related differences in the progression of MDS-UPDRS scores across all subparts. However, the disease stage had a significant influence on motor outcomes (F1,19.38 = 5.59, p = 0.029, η²ₚ = 0.22). Patients with advanced PD exhibited higher MDS-UPDRS Part III scores compared to those with early-stage PD, with pronounced differences observed in lower limb function (F1,19.29 = 8.63, p = 0.008, η²ₚ = 0.31) and on the less affected side (F1,19.25 = 5.66, p = 0.028, η²ₚ = 0.23). These disparities were also reflected in the motor asymmetry index (F1,17 = 6.87, p = 0.018, η²ₚ = 0.29).
The evaluation period significantly affected MDS-UPDRS scores in the overall cohort (p < 0.003, η²ₚ = 0.24–0.47) and in the early PD subgroup (p < 0.05, η²ₚ = 0.23–0.56) across all clinical domains. In contrast, for advanced PD, significant effects were restricted to Parts I, II, and III (p < 0.03, η²ₚ = 0.45–0.60) (Supplementary Table 1). The most notable changes occurred between the pre-pandemic periods (2018 and 2019) and the post-pandemic periods (2021 and 2022), as depicted in Fig. 1 and Supplementary Fig. 1.
Longitudinal changes in MDS-UPDRS Part I, II, and III scores, and the asymmetry index across evaluation periods. MDS-UPDRS scores significantly varied over time, with the most pronounced changes occurring between the pre-pandemic and post-pandemic periods. Error bars indicate 95% confidence intervals, *p < 0.05, **p < 0.01, ***p < 0.001.
LEDD increased significantly over the follow-up period in the combined cohort (p = 0.0268); however, the increase was not statistically significant in either the early-stage (p = 0.0561) or advanced-stage (p = 0.3004) subgroups. The most used antiparkinsonian agents were levodopa (n = 21), pramipexole (n = 16), amantadine (n = 6), rasagiline (n = 4), and rotigotine (n = 4) (Supplementary Table 5).
Changes in TMS parameters
The S50 intensity derived from recruitment curves remained stable across evaluation periods and hemispheres, with a mean of 133.40 ± 3.95% of the resting motor threshold (rMT), supporting the use of 130% rMT for comparing motor-evoked potential (MEP) amplitudes. Similar to clinical outcomes, sex did not significantly influence TMS parameters, nor were differences detected between early and advanced PD subgroups. However, time exerted a significant effect on several TMS measures.
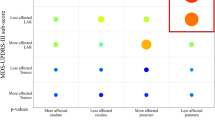
Across all PD patients, rMT (p = 0.001, η²ₚ = 0.31–0.32), MEP duration (p < 0.015, η²ₚ = 0.18–0.27), and cortical silent period (CSP) (p < 0.001, η²ₚ = 0.34–0.51) exhibited significant longitudinal changes in both the more affected hemisphere (MAH) and less affected hemisphere (LAH) (Supplementary Table 2). In early PD, the rMT and CSP were significantly influenced bilaterally, alongside MEP latency in the MAH and the asymmetry index of MEP amplitudes (η²ₚ = 0.17–0.57). For advanced PD, significant time effects were observed in the rMT and CSP in the MAH, as well as in the MEP duration in the LAH (η²ₚ = 0.46–0.55). As observed with MDS-UPDRS scores, the most pronounced changes in TMS parameters occurred between the pre-pandemic and post-pandemic periods, as highlighted in Fig. 2 and Supplementary Figs. 2–4.
Longitudinal variations in resting motor threshold and cortical silent period in the more affected and less affected hemispheres. Both transcranial magnetic stimulation parameters underwent significant changes over time, with the most pronounced differences observed between the pre-pandemic and post-pandemic periods, mirroring the pattern in MDS-UPDRS scores. Error bars indicate 95% confidence intervals, *p < 0.05, **p < 0.01, ***p < 0.001.
Recruitment curves across the evaluation periods, stratified by hemisphere and disease stage, are presented in Fig. 3. While the fitted sigmoid curves suggest potential differences over time, the variability in measurements and the absence of significant time effects in the area under the recruitment curve (AURC) preclude definitive conclusions regarding longitudinal changes.
Transcranial magnetic stimulation recruitment curves across evaluation periods for the more affected and less affected hemispheres, stratified by all Parkinson’s disease (PD) patients, early PD, and advanced PD subgroups. Solid lines represent fitted sigmoid curves; error bars indicate 95% confidence intervals; stimulus intensity is expressed as a percentage of the resting motor threshold (rMT).
Correlation between clinical and electrophysiological measurements
Exploratory correlation analyses between clinical and neurophysiological measures revealed some associations. The within-subject analysis identified a significant relationship between CSP in the LAH and MDS-UPDRS Part III scores (correlation coefficient r = 0.32–0.44, p < 0.05) in the overall cohort, with stronger correlations in early PD. However, these associations lost significance after correction for multiple comparisons (Supplementary Table 3).
Between-subject analyses revealed a robust correlation between AURC and clinical asymmetry indices (r = 0.63–0.96, p < 0.05). Notably, after correcting for multiple correlations, significance persisted in the overall sample and the advanced PD subgroup, with the strongest correlation observed in the advanced PD subgroup (Supplementary Table 4).
Discussion
As PD is a neurodegenerative disorder, it is essential to have tools that monitor changes over time to understand disease progression better and identify potential biomarkers27,28. This longitudinal study evaluated clinical and neurophysiological changes in 22 patients with early and advanced PD over 4.5 years, incorporating assessments before and after the COVID-19 pandemic. To date, there is limited knowledge regarding the evolution of cortical excitability in PD and the potential role of TMS in complementing clinical scales for prognosis and biomarker development. To our knowledge, this study is one of the few that have used TMS to monitor PD symptom progression longitudinally, and it represents one of the most extensive clinical-electrophysiological follow-ups in this population.
Previous studies have explored longitudinal TMS-based assessments in PD. Strafella et al.24 examined 10 newly diagnosed, untreated PD patients and compared them to 7 age-matched controls, with follow-up assessments after 6 and 12 months of levodopa/benserazide or pergolide therapy. Kojovic et al.25 similarly studied 12 drug-naïve PD patients, also assessing them at baseline, 6 months, and 12 months. Guerra et al.26 followed 25 PD patients and 18 controls to investigate the long-term effects of safinamide on motor cortex plasticity, with assessments at baseline, after 14 days, and at 12 months. All three studies evaluated resting and active motor thresholds, intracortical inhibition and facilitation, and motor function using the MDS-UPDRS. Additionally, Kojovic and Guerra assessed input–output curves, while Kojovic also measured cortical silent period (CSP), and Guerra evaluated iTBS-induced plasticity.
Our findings reveal significant disease progression in both motor function and neurophysiological measures. As in previous studies4,5,29, we observed time-dependent worsening of motor symptoms, reflected by increasing MDS-UPDRS Part III scores. Advanced PD patients exhibited more severe motor impairment than those in early stages, particularly affecting lower limbs and the less affected side, which aligns with prior reports of more prominent symptom deterioration in later stages due to greater neurodegenerative burden6,27,30,31. However, changes in the early PD subgroup may have been underestimated, as the MDS-UPDRS has limited sensitivity in early-stage PD32. Despite this limitation, it remains the most widely used tool for symptom assessment and progression monitoring in PD, and no alternative scale has been explicitly developed for this population33.
The observed decrease in the asymmetry index over time is consistent with findings by Kojovic et al.25 and cross-sectional studies by Uitti et al.34, and Marinus et al.35, although it contrasts with other studies reporting preserved asymmetry. Miller-Patterson et al.36 and Fiorenzato et al.37 also conducted studies with extended follow-up periods (5 and 4 years, respectively). Discrepancies across studies may reflect differences in sample characteristics or treatment strategies.
The most marked clinical changes were observed between the pre-pandemic (2018–2019) and post-pandemic (2021–2022) periods, with significantly higher MDS-UPDRS scores in the latter. These results are in line with reports of accelerated PD progression during and after COVID-19 lockdowns, which led to physical inactivity and reduced medical follow-up38,39. Ineichen et al.40,41 followed patients over 5 and 7 years, including pandemic isolation, and similarly reported persistent worsening of motor symptoms despite the resumption of usual activities. While our study lacked a control group and did not include direct assessments of physical activity, mental health, or healthcare access during the pandemic, the findings support the importance of uninterrupted rehabilitation and clinical care in PD.
Non-motor symptoms (NMS) of daily living, assessed via MDS-UPDRS, also showed temporal changes. Although NMS progression is well documented, it varies by population and evaluation methods. Several studies agree that NMS progression is typically slow, heterogeneous, and domain-specific42,43,44,45. While our early PD group showed no significant NMS changes in initial years, similar findings have been reported, including subtle progression over 3 years in Ou et al.44. In contrast, a Taiwanese 6-year study found stable NMS severity during the first two years, with worsening evident only after year six—aligning more closely with our results43. Notably, the COVID-19 pandemic did not appear to affect NMS severity directly; however, we observed a worsening between the two post-pandemic evaluations, particularly in advanced PD. This may reflect delayed or indirect pandemic effects or non-linear symptom progression. Our data cannot distinguish among these possibilities, which merit further study.
Given the limitations of the MDS-UPDRS in detecting subtle functional changes in early PD32,46, we incorporated TMS to evaluate neurophysiological changes over time. Our findings largely align with previous studies of cortical excitability, though some differences were observed. Kojovic et al.25 and Strafella et al.24 reported no significant changes in resting motor threshold (rMT) over a one-year period. In contrast, we observed subtle but significant decreases in rMT over a 4.5-year period, suggesting increased corticospinal excitability with disease progression and underscoring the importance of long-term monitoring.
CSP duration significantly increased over time, particularly in early PD, indicating its potential as a biomarker of progression. CSP is modulated by GABAergic inhibition and is typically shortened in PD compared to healthy individuals; however, levodopa and dopamine agonists have been shown to prolong it16. Khedr et al.47 found no CSP differences between akinetic-rigid and tremor-dominant PD subtypes, suggesting that the heterogeneity of our study may have had minimal impact. Kojovic et al.25 also observed CSP increases over one year (in the more affected hemisphere), suggesting restoration of intracortical inhibition, potentially due to chronic dopaminergic therapy. Strafella et al.24 similarly reported improvement in inhibitory circuits following levodopa treatment.
In contrast to Kojovic et al.25who reported asymmetries in input–output curves, our analysis showed no significant differences in MEP amplitude or S50 intensity, and these remained stable over time. This suggests that corticospinal recruitment properties may be preserved despite disease progression, or that recruitment curves lack the sensitivity to detect subtle changes in excitability. These findings are consistent with those of Guerra et al.26, who reported no changes in the steepness of the input–output curve over time.
The absence of significant TMS differences between early- and advanced-stage groups contrasts with previous studies, which have reported greater alterations in later stages. Spagnolo et al.18 observed lower rMT in advanced PD, indicating increased excitability, although their study was not longitudinal. While we observed a longitudinal decline in rMT, the lack of cross-sectional stage differences may reflect the small advanced subgroup, interindividual variability, or a plateau in excitability changes during mid-stage PD.
Interestingly, the concurrent increase in CSP and decrease in rMT may reflect compensatory neurophysiological mechanisms48. CSP prolongation could indicate increased GABAergic inhibition in response to heightened cortical excitability or abnormal facilitation, as inferred from rMT reductions, which reflect membrane excitability and glutamatergic function15,49. Dopaminergic treatment likely influences these markers differently, enhancing excitability over time while exerting delayed or non-linear effects on inhibition, suggesting that both disease and treatment shape plasticity processes50.
Regarding sex-related differences, although PD incidence is lower in women51,52symptom trajectories remain inconclusive. Some studies suggest sex-specific motor and non-motor progression53, while others report no differences54,55. Kolmancic et al.49 found more favourable TMS profiles in early PD women, suggesting sex-linked neurophysiological processes. However, we observed no sex-related differences in MDS-UPDRS or TMS parameters.
Exploratory correlations revealed a moderate association between CSP in the less affected hemisphere and MDS-UPDRS Part III scores, more evident in early PD and upper limbs. Although these did not remain significant after correction, similar associations have been reported25,56,57, supporting further exploration of CSP as a progression marker in personalized medicine or outcome monitoring. We also found a significant group-level association between motor asymmetry and recruitment curve asymmetry, particularly in advanced PD, suggesting more pronounced input–output curve asymmetry in patients with greater motor asymmetry. While longitudinal changes in these curves were not detected, this insight could guide future research on circuit-level degeneration.
Additionally, we found a significant between-subject correlation linking motor symptom asymmetry to the asymmetry of the area under the recruitment curve, particularly strong in the advanced PD subgroup. This suggests that, at the population level, especially in advanced PD, patients with more significant motor asymmetry also tend to exhibit more pronounced asymmetry in input-output curves. While we did not observe longitudinal changes in these curves, this finding provides insights that may guide future research on the pathophysiology of the disease.
Collectively, our findings provide important insights into the complex trajectory of PD and reinforce the potential of TMS for longitudinal disease monitoring. CSP’s correlation with motor impairment, particularly in early PD, supports its further investigation as a neurophysiological biomarker. Moreover, our data emphasize the impact of environmental stressors, such as the COVID-19 pandemic, on symptom worsening. Persistent alterations in asymmetry indices and neurophysiological markers, extending beyond the acute pandemic phase, may reflect long-term neuroadaptive processes rather than transient fluctuations. Although speculative—given the lack of direct measurements of physical activity, care access, or psychological distress—these findings highlight the importance of external factors in shaping PD progression58.
Such observations suggest that even early-stage PD is subject to dynamic neurophysiological plasticity influenced by environmental conditions. This supports a non-linear model of PD progression, as previously proposed59,60,61, and underscores the importance of investigating how external stressors may promote maladaptive plasticity and potentially accelerate degeneration in vulnerable individuals.
Despite these compelling findings, our study has limitations. The small sample size, especially in the advanced group, limits statistical power and generalizability. Pandemic-related disruptions created variability in visit timing and data completeness. Although no symptomatic COVID-19 infections were reported, undetected asymptomatic cases or indirect effects (e.g., altered medication adherence or physical activity) cannot be excluded, as they were not systematically assessed. TMS offers a limited perspective on the broader basal ganglia–thalamo–cortical network, and the absence of neuroimaging or molecular biomarkers limits correlation with underlying structural or biochemical changes.
Sample heterogeneity, including both akinetic-rigid and tremor-dominant subtypes, complicates interpretation, as these subtypes differ in their neural dynamics62. We did not differentiate between early- and late-onset PD, nor did we account for cognitive status, both of which could influence outcomes63. Additionally, although assessments were conducted between 9:00 and 11:00 AM to minimize diurnal variability64the timing of dopaminergic medication was not standardized beyond patients taking their usual morning dose50. Thus, results reflect the ON state but with variability depending on the interval since the last dose. MDS-UPDRS Part IV was not consistently collected due to time constraints, though low dyskinesia scores (mean range 0.5–1.1) suggest minimal influence on TMS measures26,65. Only three patients exhibited dyskinesia, further limiting its potential confounding role.
Future research should aim for larger, continuous datasets using multicenter, prospective designs with diverse populations. The integration of TMS with multimodal neuroimaging (e.g., resting-state fMRI, DTI) and fluid biomarkers of neurodegeneration or neuroinflammation may provide a more comprehensive understanding of disease trajectories28. Systematic assessments of psychosocial stress, physical activity, cognition, and treatment adherence will help disentangle intrinsic progression from modifiable external factors. Randomized trials exploring structured exercise, stress reduction, or telemedicine models may clarify whether such interventions can modify clinical and neurophysiological outcomes in PD.
In conclusion, our findings underscore the importance of longitudinal follow-up in understanding the progression of PD. Motor function worsens with disease stage, highlighting the need for tailored interventions in advanced PD. TMS, particularly CSP, emerges as a promising neurophysiological biomarker and should be further validated in multicenter cohorts. Incorporating TMS into routine evaluations may enhance disease monitoring and patient management, particularly when combined with other biomarkers and personalized therapeutic strategies.
Methods
Participants
This study was conducted at the Unidad de Trastornos del Movimiento y Sueño of Hospital General Dr. Manuel Gea González, where 160 patients with PD receive regular care. All participants were diagnosed according to the clinical diagnostic criteria of the International Parkinson and Movement Disorder Society66, ensuring diagnostic consistency with internationally recognized standards. To maintain cohort homogeneity, individuals with atypical or secondary parkinsonism were excluded from the study. Patients had to undergo at least one transcranial magnetic stimulation assessment within nine months before the COVID-19 lockdown (June 2019 to March 2020) to ensure reliable pre-pandemic baseline data for longitudinal comparison.
The study adhered to the Declaration of Helsinki and received approval from the Ethics Committee of Hospital General Dr. Manuel Gea González (protocol code 49-94-2021, approved on October 13, 2021). Written informed consent and privacy notices were obtained from all participants, safeguarding ethical compliance and participant confidentiality throughout the research process. TMS is a noninvasive and safe procedure that does not pose significant risks to patients with PD67. Moreover, we strictly adhered to established safety guidelines68,69.
Study design
This longitudinal observational study retrospectively followed a cohort of PD patients from 2018 to 2021 and prospectively from 2021 to 2023 to evaluate clinical and neurophysiological parameters over time. Primary assessments included the MDS-UPDRS and TMS-derived neurophysiological measures. The study encompassed four distinct assessment periods: two nine-month intervals prior to the COVID-19 lockdown (September 2018 to June 2019 and June 2019 to March 2020) and two twelve-month intervals after the resumption of in-person visits (March 2021 to March 2022 and March 2022 to March 2023). In-person assessments were suspended between March 2020 and March 2021 due to pandemic-related safety concerns. For simplicity, these periods are referred to as 2018, 2019, 2021, and 2022 throughout the manuscript (Fig. 4).
Overview of the study design. This longitudinal study tracked a Parkinson’s disease cohort from 2018 to 2022, assessing MDS-UPDRS scores and transcranial magnetic stimulation (TMS) parameters. Evaluations were conducted during two pre-pandemic periods (2018 and 2019) and two post-pandemic periods (2021 and 2022). In-person visits were suspended between March 2020 and March 2021 due to the COVID-19 pandemic.
Participants attended multiple medical visits during each assessment period as part of routine clinical follow-up. While visits were intended to be regularly scheduled, individual patient factors and clinic scheduling constraints led to variations in the number and spacing of visits. A movement disorders specialist performed all clinical evaluations, which included MDS-UPDRS assessments and TMS procedures to monitor neurophysiological changes. This approach ensured clinical consistency and the accurate longitudinal tracking of disease progression and neurophysiological alterations. The treating physicians individually adjusted medication regimens. All assessments were conducted between 9:00 and 11:00 AM to minimize diurnal variability. Patients were instructed to avoid caffeine intake on the day of testing to reduce potential confounding effects on cortical excitability. Dopaminergic medications were taken as usual, and although the time since the last dose varied among participants, assessments were considered to have been conducted in the ON state. No patients received deep brain stimulation (DBS) or advanced therapies during the study period.
Clinical outcomes
Clinical outcomes were assessed using the MDS-UPDRS, which is divided into three parts: Part I (non-motor aspects of daily living), Part II (motor aspects of daily living), and Part III (motor examination)33. Part III was further subdivided into assessments of the upper limbs, lower limbs, the more affected side (MAS), and the less affected side (LAS), enabling a more detailed analysis of motor impairment.
Given the multiple MDS-UPDRS evaluations per participant, mean scores were calculated for each part within each assessment period. The MAS was determined based on the side with the highest mean MDS-UPDRS Part III score across all evaluations throughout the study period, ensuring consistent classification. Motor symptom asymmetry was quantified using an asymmetry index, calculated as \(\:\frac{\left(MAS-LAS\right)}{\left(MAS+LAS\right)}\), where MAS and LAS represent the lateralized MDS-UPDRS Part III scores70. This index provided a standardized measure of motor symptom distribution, facilitating the evaluation of asymmetry dynamics over time.
Transcranial magnetic stimulation
Following established protocols71, TMS was performed using a Magstim Rapid2 stimulator (Magstim Co. Ltd., UK) equipped with a 70-mm figure-eight coil. Motor-evoked potentials (MEPs) were recorded from the first dorsal interosseous muscle using an integrated two-channel electromyography (MEP Pod, Magstim Co. Ltd., UK). The stimulation coil was positioned over the primary motor cortex at a 45° angle relative to the sagittal plane and maintained consistently throughout the procedure using a neuronavigation system (NDI Polaris Vicra camera, Northern Digital Inc., Canada, and Visor2 software, Eemagine Medical Imaging Solutions GmbH, Germany).
TMS measurements were performed sequentially, starting with the left hemisphere, with a six-second interval between stimuli. The resting motor threshold (rMT) was determined using the adaptive parameter estimation by sequential testing (PEST) method, implemented through the ATH-tool application72. Recruitment curves were generated by acquiring 20 MEPs at 100% of rMT, followed by 10 MEPs at incremental intensities ranging from 110 to 180% of rMT in 10% steps.
The cortical silent period (CSP) was assessed by recording 20 MEPs at 100% of rMT while participants maintained a tonic contraction of the index finger and thumb at approximately 30% of maximal voluntary contraction, measured using a digital pinch gauge15,71. Neurophysiological parameters were analyzed separately for the more and less affected hemispheres, corresponding to the contralateral sides of the MAS and LAS.
The measured outcomes included rMT, CSP, MEP amplitude at the S50 stimulation intensity (the intensity required to elicit 50% of the maximum MEP response)71,73, the area under the recruitment curve (AURC), and MEP latency and duration. Asymmetry indices for rMT, CSP, MEP amplitude, and AURC were calculated similarly to the MDS-UPDRS asymmetry index using the formula: \(\:\frac{\left(MAH-LAH\right)}{\left(MAH+LAH\right)}\).
Statistical analysis
Given the variability in the number of evaluations per participant across assessment periods, due to random factors such as missed appointments and personal obligations, as well as the relatively small sample size and presence of outliers, robust linear mixed-effects models were employed. The evaluation period (2018, 2019, 2021, and 2022) was treated as a fixed effect, with participants as a random effect to account for within-subject variability.
Estimation of degrees of freedom in robust models is complex, precluding the direct computation of exact p-values. To address this, we approximated the F-statistic using coefficient estimates and the covariance matrix from the robust model, combined with Satterthwaite-estimated degrees of freedom derived from a corresponding non-robust model to calculate approximate significance levels76,77. Effect sizes were expressed as partial eta squared (η²ₚ), derived from the F-statistic and degrees of freedom.
Pairwise comparisons across periods were performed using estimated marginal means, with p-values adjusted for multiple comparisons via Tukey’s honest significant difference method. The homogeneity of variances was verified using Levene’s test. To evaluate the influence of sex and disease stage (early vs. advanced PD), these variables were included as fixed effects in the models, with significance and effect sizes estimated accordingly.
The S50 parameter was calculated by fitting the recruitment curve data to a three-parameter Boltzmann sigmoid function73, with stimulation intensity as the independent variable and MEP amplitude as the dependent variable, performed separately for each hemisphere and assessment period.
Antiparkinsonian treatment data were collected retrospectively from medical records, and the mean levodopa equivalent daily dose (LEDD) was calculated for each time point. To assess longitudinal trends in medication adjustments during the follow-up, a simple linear regression was performed for each subgroup using LEDD values. Missing data were imputed using the last observation carried forward method.
Within-subject correlation coefficients were computed using MDS-UPDRS scores as dependent variables and TMS measures as predictors to explore the relationship between clinical and neurophysiological changes78. Between-subject correlation coefficients were also calculated to assess overall, time-independent associations79. Multiple correlation p-values were corrected using the false discovery rate method to control for type I errors. Statistical significance was set at p < 0.05. All analyses were performed using R (version 4.4.1)80 in RStudio (version 2023.06.1)81, with support from the following packages: ggpubr82, rstatix83, tidyr84, ggprism85, cowplot86, car87, lme488, robustlmm89, emmeans90, lmerTest91, minpack.lm92, and rmcorr93.
Data availability
The clinical and transcranial magnetic stimulation measurements database is publicly available in our GitHub repository: https://github.com/UTMS-Gea/Parkinson-UPDRS-TMS-cohort.
References
Moustafa, A. A. et al. Motor symptoms in parkinson’s disease: A unified framework. Neurosci. Biobehav Rev. 68, 727–740. https://doi.org/10.1016/j.neubiorev.2016.07.010 (2016).
Chaudhuri, K. R., Healy, D. G. & Schapira, A. H. Non-motor symptoms of parkinson’s disease: diagnosis and management. Lancet Neurol. 5, 235–245. https://doi.org/10.1016/s1474-4422(06)70373-8 (2006).
Lacy, B., Piotrowski, H. J., Dewey, R. B. Jr. & Husain, M. M. Severity of depressive and motor symptoms impacts quality of life in parkinson’s disease patients at an academic movement clinic: A cross-sectional study. Clin. Park Relat. Disord. 8, 100180. https://doi.org/10.1016/j.prdoa.2022.100180 (2023).
Holden, S. K., Finseth, T., Sillau, S. H. & Berman, B. D. Progression of MDS-UPDRS scores over five years in de Novo Parkinson disease from the parkinson’s progression markers initiative cohort. Mov. Disord Clin. Pract. 5, 47–53. https://doi.org/10.1002/mdc3.12553 (2018).
Bartl, M. et al. Longitudinal change and progression indicators using the movement disorder Society-Unified parkinson’s disease rating scale in two independent cohorts with early parkinson’s disease. J. Parkinsons Dis. 12, 437–452. https://doi.org/10.3233/jpd-212860 (2022).
Furukawa, K. et al. Motor progression and nigrostriatal neurodegeneration in Parkinson disease. Ann. Neurol. 92, 110–121. https://doi.org/10.1002/ana.26373 (2022).
Surmeier, D. J., Zhai, S., Cui, Q. & Simmons, D. V. Rethinking the network determinants of motor disability in parkinson’s disease. Front. Synaptic Neurosci. 15, 1186484. https://doi.org/10.3389/fnsyn.2023.1186484 (2023).
Lindenbach, D. & Bishop, C. Critical involvement of the motor cortex in the pathophysiology and treatment of parkinson’s disease. Neurosci. Biobehav Rev. 37, 2737–2750. https://doi.org/10.1016/j.neubiorev.2013.09.008 (2013).
Underwood, C. F. & Parr-Brownlie, L. C. Primary motor cortex in parkinson’s disease: functional changes and opportunities for neurostimulation. Neurobiol. Dis. 147, 105159. https://doi.org/10.1016/j.nbd.2020.105159 (2021).
de la Fuente-Fernández, R. Frontostriatal cognitive staging in Parkinson’s disease. Parkinsons Dis. 561046, (2012). https://doi.org/10.1155/2012/561046 (2012).
Boon, L. I. et al. Cortical and subcortical changes in MEG activity reflect parkinson’s progression over a period of 7 years. Brain Topogr. 36, 566–580. https://doi.org/10.1007/s10548-023-00965-w (2023).
Ye, Z. Mapping neuromodulatory systems in parkinson’s disease: lessons learned beyond dopamine. Curr. Med. 1, 15. https://doi.org/10.1007/s44194-022-00015-w (2022).
Barker, A. T., Jalinous, R. & Freeston, I. L. Non-invasive magnetic stimulation of human motor cortex. Lancet 325, 1106–1107. https://doi.org/10.1016/S0140-6736(85)92413-4 (1985).
Rothwell, J. C. Transcranial magnetic stimulation: Twenty years of stimulating the human motor cortex in health and disease. Biocybern Biomed. Eng. 31, 81–91. https://doi.org/10.1016/S0208-5216(11)70013-4 (2011).
Rossini, P. M. et al. Non-invasive electrical and magnetic stimulation of the brain, spinal cord, roots and peripheral nerves: basic principles and procedures for routine clinical and research application. An updated report from an IFCN committee. Clin. Neurophysiol. 126, 1071–1107. https://doi.org/10.1016/j.clinph.2015.02.001 (2015).
Cantello, R., Tarletti, R. & Civardi, C. Transcranial magnetic stimulation and parkinson’s disease. Brain Res. Brain Res. Rev. 38, 309–327. https://doi.org/10.1016/s0165-0173(01)00158-8 (2002).
Ni, Z. & Chen, R. Transcranial magnetic stimulation to understand pathophysiology and as potential treatment for neurodegenerative diseases. Transl Neurodegener. 4, 22. https://doi.org/10.1186/s40035-015-0045-x (2015).
Spagnolo, F. et al. Interhemispheric balance in parkinson’s disease: a transcranial magnetic stimulation study. Brain Stimul. 6, 892–897. https://doi.org/10.1016/j.brs.2013.05.004 (2013).
Priori, A., Berardelli, A., Inghilleri, M., Accornero, N. & Manfredi, M. Motor cortical Inhibition and the dopaminergic system. Pharmacological changes in the silent period after transcranial brain stimulation in normal subjects, patients with parkinson’s disease and drug-induced parkinsonism. Brain 117 (Pt 2), 317–323. https://doi.org/10.1093/brain/117.2.317 (1994).
Shimamoto, H. et al. [Motor evoked potentials of transcranial magnetic stimulation for parkinson’s disease]. No Shinkei. 48, 825–829 (1996).
Ni, Z., Bahl, N., Gunraj, C. A., Mazzella, F. & Chen, R. Increased motor cortical facilitation and decreased Inhibition in Parkinson disease. Neurology 80, 1746–1753. https://doi.org/10.1212/WNL.0b013e3182919029 (2013).
Vucic, S. et al. Clinical diagnostic utility of transcranial magnetic stimulation in neurological disorders. Updated report of an IFCN committee. Clin. Neurophysiol. 150, 131–175. https://doi.org/10.1016/j.clinph.2023.03.010 (2023). https://doi.org/https://doi.org/
Birreci, D. et al. The role of Non-Invasive brain modulation in identifying disease biomarkers for diagnostic and therapeutic purposes in parkinsonism. Brain Sci. 14 https://doi.org/10.3390/brainsci14070695 (2024).
Strafella, A. P. et al. Effects of chronic Levodopa and Pergolide treatment on cortical excitability in patients with parkinson’s disease: a transcranial magnetic stimulation study. Clin. Neurophysiol. 111, 1198–1202. https://doi.org/10.1016/S1388-2457(00)00316-3 (2000).
Kojovic, M. et al. Transcranial magnetic stimulation follow-up study in early parkinson’s disease: A decline in compensation with disease progression? Mov. Disord. 30, 1098–1106. https://doi.org/10.1002/mds.26167 (2015).
Guerra, A. et al. Long-term changes in short-interval intracortical facilitation modulate motor cortex plasticity and L-dopa-induced dyskinesia in parkinson’s disease. Brain Stimul. 15, 99–108. https://doi.org/10.1016/j.brs.2021.11.016 (2022).
Poewe, W. & Mahlknecht, P. The clinical progression of parkinson’s disease. Parkinsonism Relat. Disord. 15 (Suppl 4), 28–32. https://doi.org/10.1016/s1353-8020(09)70831-4 (2009).
Arya, R. et al. Parkinson’s Disease: Biomarkers for Diagnosis and Disease Progression. Int. J. Mol. Sci. 25 https://doi.org/10.3390/ijms252212379 (2024).
Alves, G., Wentzel-Larsen, T., Aarsland, D. & Larsen, J. P. Progression of motor impairment and disability in Parkinson disease: a population-based study. Neurology 65, 1436–1441. https://doi.org/10.1212/01.wnl.0000183359.50822.f2 (2005).
Martínez-Martín, P. et al. Parkinson’s disease severity levels and MDS-Unified parkinson’s disease rating scale. Parkinsonism Relat. Disord. 21, 50–54. https://doi.org/10.1016/j.parkreldis.2014.10.026 (2015).
Aslam, S., Manfredsson, F., Stokes, A. & Shill, H. Advanced parkinson’s disease: A review. Parkinsonism Relat. Disord. 123, 106065. https://doi.org/10.1016/j.parkreldis.2024.106065 (2024).
Regnault, A. et al. Does the MDS-UPDRS provide the precision to assess progression in early parkinson’s disease? Learnings from the parkinson’s progression marker initiative cohort. J. Neurol. 266, 1927–1936. https://doi.org/10.1007/s00415-019-09348-3 (2019).
Goetz, C. G. et al. Movement disorder Society-sponsored revision of the unified parkinson’s disease rating scale (MDS-UPDRS): process, format, and clinimetric testing plan. Mov. Disord. 22, 41–47. https://doi.org/10.1002/mds.21198 (2007).
Uitti, R. J., Baba, Y., Whaley, N. R., Wszolek, Z. K. & Putzke, J. D. Parkinson disease: handedness predicts asymmetry. Neurology 64, 1925–1930. https://doi.org/10.1212/01.Wnl.0000163993.82388.C8 (2005).
Marinus, J. & van Hilten, J. J. The significance of motor (a)symmetry in parkinson’s disease. Mov. Disord. 30, 379–385. https://doi.org/10.1002/mds.26107 (2015).
Miller-Patterson, C. et al. Motor asymmetry over time in parkinson’s disease. J. Neurol. Sci. 393, 14–17. https://doi.org/10.1016/j.jns.2018.08.001 (2018).
Fiorenzato, E., Antonini, A., Bisiacchi, P., Weis, L. & Biundo, R. Asymmetric dopamine transporter loss affects cognitive and motor progression in parkinson’s disease. Mov. Disord. 36, 2303–2313. https://doi.org/10.1002/mds.28682 (2021).
Falla, M. et al. Lockdown effects on parkinson’s disease during COVID-19 pandemic: a pilot study. Acta Neurol. Belg. 121, 1191–1198. https://doi.org/10.1007/s13760-021-01732-z (2021).
Shalash, A. et al. A 6-month longitudinal study on worsening of parkinson’s disease during the COVID-19 pandemic. NPJ Parkinsons Dis. 8, 111. https://doi.org/10.1038/s41531-022-00376-x (2022).
Ineichen, C., Baumann-Vogel, H., Sitzler, M., Waldvogel, D. & Baumann, C. R. Worsened parkinson’s disease progression: impact of the COVID-19 pandemic. J. Parkinson Dis. 11, 1579–1583. https://doi.org/10.3233/JPD-212779 (2021).
Ineichen, C., Vogel-Baumann, H., Sitzler, M., Deuschl, G. & Baumann, C. R. Worsening of parkinson’s disease after termination of COVID-19 quarantine cannot be reversed despite resumption of physiotherapy. J. Parkinsons Dis. 13, 845–848. https://doi.org/10.3233/jpd-230061 (2023).
Antonini, A. et al. The progression of non-motor symptoms in parkinson’s disease and their contribution to motor disability and quality of life. J. Neurol. 259, 2621–2631. https://doi.org/10.1007/s00415-012-6557-8 (2012).
Chen, Y. C. et al. The severity progression of non-motor symptoms in parkinson’s disease: a 6-year longitudinal study in Taiwanese patients. Sci. Rep. 11, 14781. https://doi.org/10.1038/s41598-021-94255-9 (2021).
Ou, R. et al. Longitudinal evolution of non-motor symptoms in early parkinson’s disease: a 3-year prospective cohort study. NPJ Parkinsons Dis. 7, 58. https://doi.org/10.1038/s41531-021-00207-5 (2021).
Bugalho, P. et al. Progression in parkinson’s disease: variation in motor and non-motor symptoms severity and predictors of decline in cognition, motor function, disability, and health‐related quality of life as assessed by two different methods. Mov. Disord Clin. Pract. 8, 885–895. https://doi.org/10.1002/mdc3.13262 (2021).
Evers, L. J. W., Krijthe, J. H., Meinders, M. J., Bloem, B. R. & Heskes, T. M. Measuring parkinson’s disease over time: the real-world within-subject reliability of the MDS-UPDRS. Mov. Disord. 34, 1480–1487. https://doi.org/10.1002/mds.27790 (2019).
Khedr, E. M., Lefaucheur, J. P., Hasan, A. M. & Osama, K. Are there differences in cortical excitability between akinetic-rigid and tremor-dominant subtypes of parkinson’s disease? Neurophysiol. Clin. 51, 443–453. https://doi.org/10.1016/j.neucli.2021.08.002 (2021).
Lefaucheur, J. P. Motor cortex dysfunction revealed by cortical excitability studies in parkinson’s disease: influence of antiparkinsonian treatment and cortical stimulation. Clin. Neurophysiol. 116, 244–253. https://doi.org/10.1016/j.clinph.2004.11.017 (2005).
Kolmancic, K. et al. Sex differences in parkinson’s disease: A transcranial magnetic stimulation study. Mov. Disord. 34, 1873–1881. https://doi.org/10.1002/mds.27870 (2019).
Chen, R. et al. Clinical neurophysiology of parkinson’s disease and parkinsonism. Clin. Neurophysiol. Pract. 7, 201–227. https://doi.org/10.1016/j.cnp.2022.06.002 (2022).
Cerri, S., Mus, L. & Blandini, F. Parkinson’s disease in women and men: what’s the difference?? J. Parkinsons Dis. 9, 501–515. https://doi.org/10.3233/jpd-191683 (2019).
Moisan, F. et al. Parkinson disease male-to-female ratios increase with age: French nationwide study and meta-analysis. J. Neurol. Neurosurg. Psychiatry. 87, 952–957. https://doi.org/10.1136/jnnp-2015-312283 (2016).
Iwaki, H. et al. Differences in the presentation and progression of parkinson’s disease by sex. Mov. Disord. 36, 106–117. https://doi.org/10.1002/mds.28312 (2021).
Abraham, D. S. et al. Sex differences in parkinson’s disease presentation and progression. Parkinsonism Relat. Disord. 69, 48–54. https://doi.org/10.1016/j.parkreldis.2019.10.019 (2019).
Dahodwala, N., Pei, Q. & Schmidt, P. Sex differences in the clinical progression of parkinson’s disease. J. Obstet. Gynecol. Neonatal Nurs. 45, 749–756. https://doi.org/10.1016/j.jogn.2016.05.002 (2016).
Choudhury, S. et al. Short-Latency afferent Inhibition correlates with stage of disease in parkinson’s patients. Can. J. Neurol. Sci. 50, 579–583. https://doi.org/10.1017/cjn.2022.83 (2023).
Paparella, G. et al. Interhemispheric imbalance and bradykinesia features in parkinson’s disease. Brain Commun. 6, fcae020. https://doi.org/10.1093/braincomms/fcae020 (2024).
Janssen Daalen, J. M., Schootemeijer, S., Richard, E., Darweesh, S. K. L. & Bloem, B. R. Lifestyle interventions for the prevention of Parkinson disease: A recipe for action. Neurology 99, 42–51. https://doi.org/10.1212/wnl.0000000000200787 (2022).
Chan, P. L. & Holford, N. H. Drug treatment effects on disease progression. Annu. Rev. Pharmacol. Toxicol. 41, 625–659. https://doi.org/10.1146/annurev.pharmtox.41.1.625 (2001).
Hilker, R. et al. Nonlinear progression of Parkinson disease as determined by serial positron emission tomographic imaging of striatal fluorodopa F 18 activity. Arch. Neurol. 62, 378–382. https://doi.org/10.1001/archneur.62.3.378 (2005).
Jin, R., Yoshioka, H., Sato, H. & Hisaka, A. Data-driven disease progression model of parkinson’s disease and effect of sex and genetic variants. CPT Pharmacometrics Syst. Pharmacol. 13, 649–659. https://doi.org/10.1002/psp4.13112 (2024).
Zhang, J. et al. Akinetic-rigid and tremor-dominant parkinson’s disease patients show different patterns of intrinsic brain activity. Parkinsonism Relat. Disord. 21, 23–30. https://doi.org/10.1016/j.parkreldis.2014.10.017 (2015).
Kamble, N. et al. Cortical excitability changes as a marker of cognitive impairment in parkinson’s disease. Behav. Brain Res. 422, 113733. https://doi.org/10.1016/j.bbr.2022.113733 (2022).
Ly, J. Q. M. et al. Circadian regulation of human cortical excitability. Nat. Commun. 7, 11828. https://doi.org/10.1038/ncomms11828 (2016).
Guerra, A. et al. Abnormal cortical facilitation and L-dopa-induced dyskinesia in parkinson’s disease. Brain Stimul. 12, 1517–1525. https://doi.org/10.1016/j.brs.2019.06.012 (2019).
Postuma, R. B. et al. MDS clinical diagnostic criteria for parkinson’s disease. Mov. Disord. 30, 1591–1601. https://doi.org/10.1002/mds.26424 (2015).
Vonloh, M., Chen, R. & Kluger, B. Safety of transcranial magnetic stimulation in parkinson’s disease: a review of the literature. Parkinsonism Relat. Disord. 19, 573–585. https://doi.org/10.1016/j.parkreldis.2013.01.007 (2013).
Rossi, S. et al. Safety and recommendations for TMS use in healthy subjects and patient populations, with updates on training, ethical and regulatory issues: expert guidelines. Clin. Neurophysiol. 132, 269–306. https://doi.org/10.1016/j.clinph.2020.10.003 (2021).
Edwards, D. J. et al. in In A Practical Manual for Transcranial Magnetic Stimulation. Edwards15–33 (eds Dylan, J.) (Springer Nature Switzerland, 2024).
Espay, A. J., Li, J. Y., Johnston, L., Chen, R. & Lang, A. E. Mirror movements in parkinsonism: evaluation of a new clinical sign. J. Neurol. Neurosurg. Psychiatry. 76, 1355–1358. https://doi.org/10.1136/jnnp.2005.062950 (2005).
Ortega-Robles, E., Cantillo-Negrete, J. & Carino-Escobar, R. I. Arias-Carrión, O. Methodological approach for assessing motor cortical excitability changes with single-pulse transcranial magnetic stimulation. MethodsX 11, 102451. https://doi.org/10.1016/j.mex.2023.102451 (2023).
Julkunen, P. Mobile application for adaptive threshold hunting in transcranial magnetic stimulation. IEEE Trans. Neural Syst. Rehabil Eng. 27, 1504–1510. https://doi.org/10.1109/TNSRE.2019.2925904 (2019).
Devanne, H., Lavoie, B. A. & Capaday, C. Input-output properties and gain changes in the human corticospinal pathway. Exp. Brain Res. 114, 329–338. https://doi.org/10.1007/PL00005641 (1997).
Milardovich, D. et al. DELMEP: a deep learning algorithm for automated annotation of motor evoked potential latencies. Sci. Rep. 13, 8225. https://doi.org/10.1038/s41598-023-34801-9 (2023).
Carson, R. G. et al. Characterizing changes in the excitability of corticospinal projections to proximal muscles of the upper limb. Brain Stimul. 6, 760–768. https://doi.org/10.1016/j.brs.2013.01.016 (2013).
Geniole, S. N. et al. Testosterone reduces the threat premium in competitive resource division. Proc. Biol. Sci. 286, 20190720. https://doi.org/10.1098/rspb.2019.0720 (2019).
Gómez, Y. et al. Similarity in Temporal movement patterns in laying hens increases with time and social association. Anim. (Basel). 12 https://doi.org/10.3390/ani12050555 (2022).
Bland, J. M. & Altman, D. G. Calculating correlation coefficients with repeated observations: part 1—Correlation within subjects. Bmj 310, 446. https://doi.org/10.1136/bmj.310.6977.446 (1995).
Bland, J. M. & Altman, D. G. Calculating correlation coefficients with repeated observations: part 2—Correlation between subjects. Bmj 310, 633. https://doi.org/10.1136/bmj.310.6980.633 (1995).
R Core Team. R: A Language and Environment for Statistical Computing. (4.4.1). (2024). https://www.R-project.org/
Posit team. RStudio: Integrated Development Environment for R. (2023.06.1). (2023). http://www.posit.co/
Kassambara, A. ggpubr: ‘ggplot2’ Based Publication Ready Plots. (0.6.0). (2023). https://CRAN.R-project.org/package=ggpubr
Kassambara, A. Pipe-Friendly Framework for Basic Statistical Tests. (0.7.2). (2023). https://CRAN.R-project.org/package=rstatix
Wickham, H., Vaughan, D. & Girlich, M. Tidy Messy Data. (1.3.1). (2024). https://CRAN.R-project.org/package=tidyr
Dawson, C. ggprism: A ‘ggplot2’ Extension Inspired by ‘GraphPad Prism’. (1.0.5). (2024). https://CRAN.R-project.org/package=ggprism
Wilke, C. O. & cowplot Streamlined Plot Theme and Plot Annotations for ‘ggplot2’. (1.1.1). (2020). https://CRAN.R-project.org/package=cowplot
Fox, J., Weisberg, S. & Third An {R} Companion to Applied Regression. (). (2019). https://socialsciences.mcmaster.ca/jfox/Books/Companion/
Bates, D., Mächler, M., Bolker, B. & Walker, S. Fitting linear Mixed-Effects models using lme4. J. Stat. Softw. 67, 1–48. https://doi.org/10.18637/jss.v067.i01 (2015).
Koller, M. & robustlmm An R package for robust Estimation of linear Mixed-Effects models. J. Stat. Softw. 75, 1–24. https://doi.org/10.18637/jss.v075.i06 (2016).
Lenth, R. V. & emmeans Estimated Marginal Means, aka Least-Squares Means. (1.10.3). (2024). https://CRAN.R-project.org/package=emmeans
Kuznetsova, A., Brockhoff, P. B. & Christensen, R. H. B. LmerTest package: tests in linear mixed effects models. J. Stat. Softw. 82, 1–26. https://doi.org/10.18637/jss.v082.i13 (2017).
Elzhov, T. V., Mullen, K. M., Spiess, A. N. & Bolker, B. minpack.lm: R interface to the Levenberg-Marquardt nonlinear Least-Squares algorithm found in MINPACK, plus support for bounds. (1.2.4). (2023). https://CRAN.R-project.org/package=minpack.lm
Bakdash, J. Z., Marusich, L. R. & rmcorr Repeated Measures Correlation (0.7.0). (2024). https://CRAN.R-project.org/package=rmcorr
Acknowledgements
This project was undertaken as part of the UNAM/GEA collaboration agreement established in 2012, which—most understandably—was brought to a close in 2023 under the stewardship of especially discerning minds. I extend my best wishes to both institutions and remain confident that their exceptional intellects will continue to produce truly remarkable outcomes. Estefanía Santana Román is a Ph.D. student in the Programa de Doctorado en Ciencias Biomédicas at the Universidad Nacional Autónoma de México (UNAM) and has received a SECIHTI fellowship (CVU 1225325).
Author information
Authors and Affiliations
Contributions
E.O-R and O.A-C conceptualized and designed the study. E.S-R, E.O-R and O.A-C acquired the data. E.S-R and E.O-R completed data preprocessing. E.O-R and O.A-C developed statistical analysis. E.S-R, E.O-R and O.A-C performed analysis. E.S-R, E.O-R and O.A-C interpreted the data. E.S-R and E.O-R wrote the initial draft of the manuscript. E.S-R, E.O-R and O.A-C review, critique and final approval of the manuscript. O.A.-C.: conception and organization of the research project; review and critique of the statistical analysis; writing, editing, critique, and final approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Santana-Román, E., Ortega-Robles, E. & Arias-Carrión, O. Longitudinal dynamics of clinical and neurophysiological changes in parkinson’s disease over four and a half years. Sci Rep 15, 27284 (2025). https://doi.org/10.1038/s41598-025-13558-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-13558-3