Abstract
The primary objective of this study was to evaluate the influence of sociodemographic, clinical, and lifestyle factors on health-related quality of life (HRQoL) in older adults hospitalized with heart failure. A total of 210 patients (mean age 80.99 ± 8.32 years; 65.24% female) participated in the study. The standardized EQ-5D-5 L questionnaire was used as the main instrument to assess HRQoL.The average health status assessment on the EQ VAS scale in the study group of patients was 56.03 ± 18.81. Patients reported the greatest mobility problems, with 25.71% of them having severe walking problems and 7.62% of patients being unable to walk. 22.39% of respondents had serious problems with performing everyday activities or were unable to perform them at all. Nearly one fifth of patients experienced severe or extreme pain or discomfort (19.05%). Physical activity turned out to have a significant impact on motor skills (p < 0.001), self-care (p < 0.001), usual activities (p < 0.001) and anxiety/depression (p = 0.001). In conclusion, the quality of life of older patients hospitalized due to HF is reduced compared to the general population. The most prominent issues are pain/discomfort and anxiety/depression. A number of socioeconomic factors influence the quality of life of patients with HF.
Similar content being viewed by others
Introduction
Heart failure (HF) is one of the most important clinical problems, constituting a major public health challenge1. It is estimated that 64.3 million people live with heart failure worldwide2,3. The incidence of heart failure is estimated at between 2% and 4%, and this percentage increases to as much as 12% in the population of patients 65 years and older4,5. In Poland, HF occurs in 3,233/100,000 people, with an increasing trend observed both in the incidence and mortality due to HF6.
Today, due to a growing proportion of the aging population, the total number of patients with heart failure continues to increase. Nevertheless, more and more cases of HF are reported in younger people, which may be related to, among others, with the growing obesity epidemic. Other factors associated with the occurrence of HF include coronary artery disease, hypertension and diabetes, which often coexist and may interact, increasing the likelihood of developing HF7. Lifestyle factors are also associated with the development of HF8, in particular smoking4 and lack of physical activity9.
The high mortality rate among patients with HF is also disturbing, amounting to approximately 50% 5 years after diagnosis. This is particularly important given the progress in the treatment of this disease7.
In many cases, HF is associated with multiple diseases, requiring a holistic approach to treatment. The prevalence of HF creates the need for a multidimensional approach to the patient, including deeper research into the quality of life of this group of people10. Previous reports indicate that the health-related quality of life (HRQoL) in patients with HF is reduced compared to the general population11 and may be additionally determined by sociodemographic and lifestyle factors12. However, these factors are not widely described in the literature among the population of patients with HF13. The quality of life is an important aspect because it is considered a predictor of hospitalization and death among patients, including patients with HF. For this reason, it seems necessary to determine lifestyle-related factors that may determine the quality of life of patients with HF14.
Aim of the study
The main aim of the study was to assess the determinants of the health-related quality of life among older patients with heart failure. In the study, we also evaluated the relationship between patients’ quality of life and the following sets of parameters:
-
socio-demographic determinants: gender, age, pension amount, living with someone/alone;
-
lifestyle determinants: smoking cessation, overweight/obesity, physical activity, diet, number of medications taken, stressful events in the previous year, self-assessment of lifestyle;
-
disease-related determinants: type of heart failure and comorbidities (diabetes mellitus, COPD, hypertension).
Materials and methods
Patients and setting
The study was carried out between June 2022 and April 2024 among patients with heart failure hospitalized at the Department of Internal Medicine and Geriatric Cardiology, Centre of Postgraduate Medical Education.
The inclusion criteria for the study were:
-
Age > 18 years.
-
Hospitalization for heart failure.
The exclusion criterion was the lack of consent to participate in the study.
Ultimately, 210 patients participated in the study.
All methods were performed in accordance with the relevant guidelines and regulations. Consent to the study was given by the Bioethics Committee at the Centre of Postgraduate Medical Education of Warsaw (resolution No. 73/2022 of June 8, 2022).
Research tool
The basic research tool was the EQ-5D-5 L questionnaire - a standardized measure of health status developed by the EuroQol Group (Polish version). The questionnaire covers 5 dimensions of quality of life, including: mobility (MO), self-care (SC), usual activities (UA), pain/discomfort (PD), and anxiety/depression (AD). Each dimension is rated on a 5-point scale: 1 - no problems, 2 - slight problems, 3 - moderate problems, 4 - serious problems and 5 - extreme problems.
Health-related quality of life, as measured by the EQ-5D-5 L questionnaire, is represented through a combination of responses across five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension is rated on a five-point scale, and the resulting health state is expressed as a five-digit code—for example, “11111” indicates no problems in any dimension, while “55555” reflects extreme problems across all dimensions.
In addition to the descriptive system, the EQ-5D-5 L includes a visual analogue scale (EQ VAS), ranging from 0 to 100, on which patients rate their current overall health status—where 0 represents the worst imaginable health and 100 the best imaginable health.
Data analysis followed the guidelines outlined in the EQ-5D-5 L User Guide, Version 3.0 (September 2019)15. The study also collected data on patients’ sociodemographic characteristics, comorbidities, and lifestyle-related factors.
Data collection
Patients received a paper-and-pencil questionnaire to complete on their own. Responses to questions regarding demographic characteristics were collected using the computer-assisted personal interview (CAPI) technique.
Statistical analysis
Statistica 13.3 was used for statistical analysis [TIBCO Software Inc. (2017). Statistica (data analysis software system), version 13. http://statistica.io.]. The characteristics of the study group were made using numbers, percentages and descriptive statistics, such as mean, standard deviation, first and third quartiles, median, mode, minimum and maximum. Nonparametric statistics such as Spearman’s correlation coefficient, Mann-Whitney U test, and Kruskal-Wallis test were used due to the ordinal nature of most of the dependent variables. The significance level α was set at 0.05.
Results
Characteristics of the study group
The study sample consisted of 210 patients aged 39 to 97 years, with the vast majority (95.24%) being over the age of 65. Women accounted for a greater proportion of participants (65.24%) compared to men (34.76%). Most patients reported an average income (59.05%), and living arrangements were almost evenly split between those living with someone (49.52%) and those living alone (48.57%).
A history of smoking was reported by 100 patients, half of whom had smoked for at least 25 years; however, 81% of these individuals had successfully quit. Nearly half of the participants were overweight or obese (42.86%), and one-third (33.81%) reported no physical activity. The number of medications taken ranged from 0 to 12, with half of the patients using at least six.
Dietary modifications were common, including increased consumption of fruits and vegetables (50.0%), reduction in alcohol intake (48.57%), and limiting sugar consumption (48.10%). In terms of lifestyle self-assessment, nearly half of the patients (46.67%) rated their lifestyle as average, while over one-third (39.52%) considered it healthy.
The vast majority of patients were diagnosed with hypertension (83.81%), almost half with diabetes mellitus (43.33%), and one-tenth with COPD (10.95%). The most common type of heart failure in the study group was HFpEF (64.29%). The socio-demographic characteristics, lifestyle and health status of the patients are presented in Table 1.
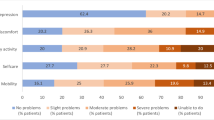
Quality of life scores in all domains
Table 2 shows the results of the EQ VAS and EQ-5D-5 L scale in all domains. The average health assessment on the EQ VAS scale in the study group of patients was 56.03 ± 18.81. Patients reported the greatest problems with mobility, including 25.71% of them had severe problems in walking about, and 7.62% of patients were unable to walk about, and only 26.19% had no problems with mobility. 22.39% of respondents had severe problems with daily activities or were unable to do them at all. Almost one fifth of patients experienced severe or extreme pain or discomfort (19.05%). On the other hand, most patients had no problems with washing or dressing (61.90%), and slightly less than half had no problems with usual activities (47.14%) and anxiety/depression (43.80%).
The data analysis showed that full health status (i.e. 11111) was indicated by 9.5% of respondents, including 13 women and 7 men. Patients in good health achieved an average EQ VAS score of 70.26. None of the patients reported the worst possible health condition (55555).
Of all patients, 22.86% were in health states of no problems or little problems on all dimensions (health states level 1 or 2 in all domains).
Determinants of health-related quality of life
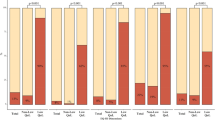
Table 3 shows the EQ-5D-5 L scores in all domains depending on the socio-demographic characteristics, lifestyle and health status of the examined patients. A weak, positive correlation was found between age (R = 0.20, p = 0.003), stressful events in the previous year (R = 0.210, p = 0.002) and number of medications taken (R = 0.147, p = 0.033) and the severity of problems with mobility. There was also a weak positive correlation between age and problems with self-care (R = 0.236, p = 0.001), usual activities (R = 0.182, p = 0.008), anxiety/depression (R = 0.159, p = 0.021). Moreover, the number of stressful events in the previous year influenced the severity of difficulties in usual activities (R = 0.143, p = 0.039), pain/discomfort (R = 0.279, p < 0.001) and anxiety/depression (R = 0.155, p = 0.025).
Females showed significantly greater severity of problems with pain/discomfort (p = 0.008) and anxiety/depression (p = 0.003). The Kruskal-Wallis test also showed significant differences in pain/discomfort (p = 0.045) and anxiety/depression (p = 0.042) depending on the pension amount, but Dunn’s post-hoc test only indicated a significantly more intense pain experience among people with low income compared to people with high income (p = 0.041). Physical activity turned out to have a significant impact on mobility (p < 0.001), self-care (p < 0.001), usual activities (p < 0.001) and anxiety/depression (p = 0.001), and Dunn’s post-hoc test indicated that patients with high physical activity, at least 5 times a week, experienced significantly fewer problems than patients with no or little physical activity, 1–2 times a week. Patients with obesity or overweight had significantly greater problems with mobility (p = 0.030), while reducing fats (p = 0.037), calories (p = 0.004) and sugar (p = 0.035) in the diet significantly increased the feeling of pain and discomfort. There are also statistically significant differences in mobility (p = 0.026), usual activities (p = 0.009) and anxiety/depression (p = 0.017) depending on self-assessment of lifestyle, and Dunn’s post-hoc test in particular indicates a significantly lower feeling of problems by patients leading a healthy lifestyle. Moreover, patients with hypertension have significantly fewer problems with daily activities (p = 0.028), and those with HFrEF have significantly more severe problems related to self-care (p = 0.037). In the case of the remaining analyses, the results turned out to be statistically insignificant.
There was a weak, negative correlation between age and self-assessment of health (R=-0.181, p = 0.011), as well as a weak, positive correlation between the number of diet changes and self-assessment of health (R = 0.158, p = 0.033). The correlation was not statistically significant in the case of years of smoking (p = 0.400), stressful events in the previous year (p = 0.165), or number of medications taken (p = 0.485).
Patients who did not show any physical activity (p < 0.001) and defined their lifestyle as unhealthy (p = 0.011) rated their health as the worst, while better health was observed in those who consumed fruit and vegetables (p = 0.018) and reduced sugar in diet (p = 0.027). However, there was no significant effect of age group (p = 0.926), gender (p = 0.812), pension amount (p = 0.968), living with someone/alone (p = 0.830), smoking cessation (p = 0.765), overweight/obesity (p = 0.211), diabetes mellitus (p = 0.055), COPD (p = 0.662), hypertension (p = 0.945) and type of heart failure (p = 0.372) on self-assessment of health. Data regarding self-assessment of health depending on selected variables are presented in Table 4.
Discussion
Our survey indicates that patients hospitalized for heart failure reported the most significant problems with mobility. One in four patients had serious difficulties walking, and nearly one in ten were unable to walk. Additionally, 60% of respondents reported problems in at least one dimension of the EQ-5D-5 L. More than 22% of patients experienced severe difficulties in performing daily activities or were unable to perform them at all. A similar proportion reported severe or extreme pain or discomfort.
The study further shows that limitations in mobility, daily activities, and the severity of pain/discomfort increased with age and the number of stressful events experienced in the previous year. Higher pain perception was also observed among individuals with lower income. Physical activity had a significant impact on mobility, self-care, usual activities, and anxiety/depression. A self-assessed healthy lifestyle was also strongly associated with better outcomes in these areas.
We compared the results of the EQ-5D-5 L questionnaire with population norms for Poland16. Research by Golicki et al. found that in the general Polish population, 38.5% of individuals report perfect health (‘11111’), with men more frequently than women. In contrast, our study among patients with heart failure shows that only 9.5% reported full health—more often women than men. In the self-reported data, at least one mild health limitation was indicated by 90.5% of respondents, compared to 61.5% in the general population. EQ-5D-5 L results in the Polish population are comparable to those from Germany and the United States in the dimensions of mobility and self-care, although U.S. respondents report more limitations in usual activities17.
When analyzing the individual dimensions of the EQ-5D-5 L questionnaire, it is noteworthy that in our self-reported study among patients with heart failure, the highest frequency of limitations was observed in the self-care and usual activities dimensions. In contrast, within the general population, the most commonly reported limitations were in the areas of pain/discomfort and anxiety/depression. These dimensions are also the lowest rated among older adults in the Polish population, particularly in the 65–74 and 75 + age groups16.
Interestingly, overall self-assessed health in the Polish population is lower than in Germany, especially in the dimensions of pain/discomfort and anxiety/depression18. Both in our study and in the general Polish population, limitations in these areas were more frequently reported by women. This finding has been confirmed in numerous studies, regardless of age or heart failure severity19. Furthermore, studies using other quality of life instruments have also identified female gender as a predictor of poorer overall, physical, and emotional quality of life20.
However, some research, such as the study by Gallagher AM et al. conducted in a heart failure outpatient clinic in the UK has found no clear association between patient demographics and HRQoL21. Studies from other countries also confirm that patients with heart failure have significantly lower quality of life compared to the general population22. For example, Boczor et al., in an observational study in Germany, demonstrated that HF patients experienced significant health limitations across all EQ-5D-5 L domains. The study also highlighted associations between HRQoL and sociodemographic factors such as employment status, living alone, and comorbidities23. Comorbid conditions in patients with HF particularly impacted mobility, usual activities, and pain/discomfort, as well as overall health status assessed via the EQ VAS. Consistent with our findings, other studies also emphasize the influence of age, psychological stress, and physical activity on HRQoL in this patient population24.
Differences in quality of life as measured by the EQ-5D-5 L questionnaire between patients with heart failure and the general population are also evident among younger individuals. A study by Tan YJ et al., involving HF patients with a mean age of 57 years, showed that nearly half of the respondents reported problems in the dimensions of mobility, usual activities, and pain/discomfort. Worse outcomes in these areas were observed among patients living alone, those with lower levels of education, and those who were unemployed due to poor health25.
Similarly, a prospective multicenter observational study focusing on patients with HFpEF (mean age 81 years) found significantly lower scores in the dimensions of mobility, usual activities, and self-care. Notably, these domains were identified as important predictors of mortality14.
It is also worth highlighting that self-assessed health status among patients with HF is poorer compared to individuals with other cardiovascular diseases. In our study, the mean EQ VAS score for HF patients was 56.03, whereas Chatzinikolaou A et al. reported an average score of 67.45 in a general cardiovascular patient population26. Literature suggests that self-rated health is strongly associated with factors such as education level, occupational status, household income, and living conditions, while differences by age and gender tend to be less pronounced27. In our study, however, EQ VAS scores were mainly differentiated by age and lifestyle-related variables.
While quantitative data provide essential information on HRQoL, qualitative research also plays a critical role in understanding the lived experience of patients with HF. A study by Saifan AR et al. revealed that HRQoL in HF patients is most affected by physical limitations, which influence daily functioning and contribute to symptoms such as fatigue and shortness of breath. These physical constraints also negatively impacted patients’ psychosocial and spiritual well-being, cognitive functioning, and capacity for employment, ultimately leading to increased levels of fear, anxiety, and social isolation28.
In conclusion, reduced health-related quality of life among patients with HF remains a significant clinical concern, as it is associated with poorer long-term outcomes and prognosis. Understanding the determinants of HRQoL in this population is therefore essential. Interestingly, studies also point to geographical disparities in HRQoL levels, with lower scores reported in Eastern Europe and Africa, and higher levels observed in Western European countries22.
Limitations of the study
The main limitation of the study was the inclusion of patients hospitalized in a large facility. This may have influenced the distribution of certain sociodemographic characteristics, particularly the place of residence. Additionally, by focusing solely on hospitalized patients, the study sample may overrepresent individuals with more severe health conditions and reduced quality of life, limiting the generalizability of the findings to the broader population of older adults with heart failure, especially those living in the community.
Another limitation is the cross-sectional design of the study, which does not allow for the assessment of changes in health-related quality of life over time or for establishing causal relationships between the examined variables. Furthermore, although the quantitative data provided a comprehensive overview of HRQoL determinants, the study lacked qualitative methods that could have enriched the interpretation of results by uncovering more nuanced patient experiences, emotional responses, and contextual factors.
We recognize these limitations and plan to address them in future research by expanding the study population to include community-dwelling patients and incorporating longitudinal and qualitative components.
Conclusions
Older patients hospitalized due to heart failure have a decreased quality of life compared to the general population. The greatest quality of life problems in these patients are related to pain/discomfort and anxiety/depression. Many socioeconomic, health and lifestyle factors may influence the assessed quality of life. In the studied population, these include, among others: gender, age, income, but especially lifestyle, including physical activity.
Data on quality of life, combined with socioeconomic and lifestyle variables, can be used to assess the health status and needs of specific populations. Combining them with medical data can be used to identify groups of people with potentially the lowest quality of life, which may help in making therapeutic decisions.
Therefore, during an interview with a patient with CHF, it is important to obtain not only medical information, but also information regarding the quality of life depending on the health condition, including the ability to function independently, which can be done using the EQ-5D-5 L.
Data availability
All data are available from the corresponding author.
Abbreviations
- CAPI:
-
Computer-assisted personal interviewing
- COPD:
-
Chronic obstructive pulmonary disease
- HF:
-
Heart failure
- HFpEF:
-
Heart failure with preserved ejection fraction
- HFrEF:
-
Heart failure with reduced ejection fraction
- HRQoL:
-
Health-related quality of life
References
Mendes, J. L., Santos, D., Sousa-Pinto, B. & C. M. & Assessment of patient-reported outcomes measures in heart failure: a systematic review. Heart Fail. Rev. 29, 853–867 (2024).
Luo, Z., Ruan, T., Xu, M., Ding, Y. & Zhu, L. Development and validation of the self-volume management behaviour questionnaire for patients with chronic heart failure. ESC Heart Fail. 11, 1076–1085 (2024).
Lippi, G. & Sanchis-Gomar, F. Global epidemiology and future trends of heart failure. AME Med. J. 5, 15 (2020).
Groenewegen, A., Rutten, F. H., Mosterd, A. & Hoes, A. W. Epidemiology of heart failure. Eur. J. Heart Fail. 22, 1342–1356 (2020).
van Riet, E. E. et al. Epidemiology of heart failure: the prevalence of heart failure and ventricular dysfunction in older adults over time. A systematic review. Eur. J. Heart Fail. 18, 242–252 (2016).
Leszek, P. et al. November. Real world heart failure epidemiology and outcome: a population-based analysis of 1,990,162 heart failure patients, European Heart Journal 41, Supplement 2, (2020).
Roger, V. L. Epidemiology of heart failure: A contemporary perspective. Circ. Res. 128, 1421–1434 (2021).
Aggarwal, M. et al. Lifestyle modifications for preventing and treating heart failure. J. Am. Coll. Cardiol. 72, 2391–2405 (2017).
Pandey, A. et al. Physical activity, fitness, and obesity in heart failure with preserved ejection fraction. JACC Heart Fail. 6, 975–982 (2018).
Kuan, W. C. et al. Validity and measurement equivalence of EQ-5D-5L questionnaire among heart failure patients in malaysia: a cohort study. J. Med. Econ. 27, 607–617 (2024).
Moradi, M. et al. Quality of life of chronic heart failure patients: a systematic review and meta-analysis. Heart Fail. Rev. 25, 993–1006 (2020).
Soleimani, M. A., Zarabadi-Pour, S., Motalebi, S. A. & Allen, K. A. Predictors of quality of life in patients with heart disease. J. Relig. Health. 59, 2135–2148 (2020).
Johansson, I. et al. Health-Related quality of life and mortality in heart failure: the global congestive heart failure study of 23 000 patients from 40 countries. Circulation 143, 2129–2142 (2021).
Seo, M. et al. The clinical relevance of quality of life in heart failure patients with preserved ejection fraction. ESC Heart Fail. 10, 995–1002 (2023). Osaka CardioVascular Conference (OCVC)-Heart Failure investigators.
EQ-5D-5L User Guide Version. 3.0. (2024). https://euroqol.org/publications/user-guides/
Golicki, D. & Niewada, M. EQ-5D-5L Polish population norms. Arch. Med. Sci. 13, 191–200 (2017).
Craig, B. M., Pickard, A. S. & Lubetkin, E. I. Health problems are more common, but less severe when measured using newer EQ-5D versions. J. Clin. Epidemiol. 67, 93–99 (2014).
Hinz, A., Kohlmann, T., Stobel-Richter, Y., Zenger, M. & Brahler, E. The quality of life questionnaire EQ-5D-5L: psychometric properties and normative values for the general German population. Qual. Life Res. 23, 443–447 (2014).
Faxén, U. L. et al. Patient reported outcome in hfpef: Sex-specific differences in quality of life and association with outcome. Int. J. Cardiol. 267, 128–132 (2018).
Tapia, J. et al. Psychosocial factors partially explain gender differences in health-related quality of life in heart failure patients. ESC Heart Fail. 10, 1090–1102 (2023).
Gallagher, A. M., Lucas, R. & Cowie, M. R. Assessing health-related quality of life in heart failure patients attending an outpatient clinic: a pragmatic approach. ESC Heart Fail. 6, 3–9 (2019).
Ventoulis, I. et al. Differences in Health-Related quality of life among patients with heart failure. Medicina (Kaunas). 60, 109 (2024).
Boczor, S. et al. Prognostic factors associated with quality of life in heart failure patients considering the use of the generic EQ-5D-5L™ in primary care: new follow-up results of the observational RECODE-HF study. BMC Fam Pract. 22, 202 (2021).
Boczor, S. et al. Quality of life assessment in patients with heart failure: validity of the German version of the generic EQ-5D-5L™. BMC Public. Health. 19, 1464 (2019).
Tan, Y. J. et al. Examining health-related quality of life in ambulatory adult patients with chronic heart failure: insights from Malaysia using EQ-5D-5L. Qual life res. Jun 5 (2024).
Chatzinikolaou, A., Tzikas, S. & Lavdaniti, M. Assessment of quality of life in patients with cardiovascular disease using the SF-36, macnew, and EQ-5D-5L questionnaires. Cureus 13, e17982 (2021).
Jensen, M. B. et al. Danish population health measured by the EQ-5D-5L. Scand. J. Public. Health. 5, 241–249 (2023).
Saifan, A. R. et al. Experiences on health-related quality of life of Jordanian patients living with heart failure: A qualitative study. PLoS One. 19, e0298893 (2024).
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization: UR and PJ; Methodology: UR and PJ; Formal Analysis: UR, MM and AB; Writing – Original Draft Preparation: UR, AS, WN, PC, KJ, MK-U, AD, MM, JP and PJ; Writing – Review & Editing: UR, AS, WN, PC, KJ, MK-U, AD, MM, JP and PJ; Visualization MM; Supervision: UR, JP and PJ. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethic approval and consent to participate
The study was approved by the Bioethics Committee at the Centre of Postgraduate Medical Education of Warsaw [resolution No. 73/2022 of June 8, 2022).
Informed consent
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Religioni, U., Sawicka, A., Niegowska, W. et al. Sociodemographic, disease-related and lifestyle determinants of health-related quality of life among older patients hospitalized with heart failure. Sci Rep 15, 31040 (2025). https://doi.org/10.1038/s41598-025-13881-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-13881-9