Abstract
The global incidence and mortality rates of Mycobacterium avium–intracellulare complex pulmonary disease (MAC-PD) are increasing. We conducted a multicentre retrospective cohort study across 18 hospitals to develop a scoring system for predicting respiratory infection-related mortality in patients with MAC-PD. A total of 1,165 patients newly diagnosed with MAC-PD between 2010 and 2017 were enrolled and randomly allocated to a 4:1 ratio to derivation (n = 932) and validation (n = 233) groups. Among them, 656 patients (56.3%) received MAC-PD treatment within 5 years. During the observation period, all-cause mortality occurred in 183 patients (15.7%), and respiratory infection-related mortality occurred in 67 patients (5.8%). To identify the risk factors for respiratory infection-related mortality, Cox proportional hazards analysis was conducted in the derivation group, which informed the development and validation of the prognostic scoring model. Five independent risk factors were identified: age ≥ 65 years, male sex, interstitial pneumonia, albumin < 3.5 g/dL, and cavitary lesions. A prognostic score was developed by assigning 2 points to albumin < 3.5 g/dL and 1 point to each of the other factors. The score demonstrated good predictive performance, with areas under the receiver operating characteristic curves of 0.86 and 0.81 in the derivation and validation groups, respectively. Patients with scores ≥ 3 had significantly poorer prognoses than those with scores ≤ 2. The strength of this study lies in its multicentre validation and focus on respiratory infection-related mortality, providing a clinically useful risk stratification tool for MAC-PD.
Similar content being viewed by others
Introduction
Nontuberculous mycobacteria (NTM) are environmental microorganisms that cause chronic refractory respiratory infections. The global incidence of NTM pulmonary disease (NTM-PD) has been increasing with a concomitant increase in mortality rates1,2,3,4. The causative species of NTM-PD exhibit regional variation; however, Mycobacterium avium–intracellulare complex (MAC) accounts for 90% of NTM-PD cases in Japan5. The clinical course of MAC pulmonary disease (MAC-PD) is significantly heterogeneous. Some patients remain stable with watchful waiting alone, whereas others develop bronchiectasis or cavitation and succumb to respiratory failure despite multidrug therapy. Owing to the relatively high incidence of adverse events associated with multidrug therapy, treatment is not universally recommended at diagnosis6. The adherence rate to guideline-based treatment is low (4.3–41.9%), likely due to frequent adverse effects7. Consequently, prognostic evaluation at the time of diagnosis is crucial for determining disease severity. Nevertheless, determining which patients to treat and when remains challenging for clinicians8.
Systematic reviews have reported 5–42% 5-year mortality rates for MAC-PD9, identifying various risk factors, including male sex, comorbidities, advanced age, and presence of cavities. Mortality rates tend to be lower in Asian studies than in European or North American studies. In 2021, a Korean research group proposed the BACES score, which incorporates 5 components—body mass index (BMI), age, cavitation, elevated erythrocyte sedimentation rate (ESR), and male sex—as a prognostic factor for NTM-PD10. However, this scoring model is not specific to MAC-PD, as Mycobacterium abscessus complex (MABC), which is associated with poor prognosis, accounts for approximately 20% of the causative mycobacteria10. Furthermore, several variables, including male sex, age > 70 years, malignancy, BMI, lymphocyte count, albumin (Alb) levels, and fibrocavitary (FC) pattern, have been proposed in other prognostic score models for MAC-PD11. However, these models were developed in single tertiary care institutions, potentially including patients with more severe disease, and have not been validated in general healthcare environments. Furthermore, previous studies have focused on identifying prognostic factors for all-cause mortality, rather than those specific to respiratory infection-related death.
We conducted a multicentre retrospective cohort study of patients with NTM-PD in Kyushu, Japan, encompassing both tertiary care and community hospitals12. We aimed to develop and validate a prognostic scoring system to predict respiratory infection-related mortality in patients with MAC-PD.
Methods
Study design
This multicentre, retrospective, observational cohort investigation was conducted at 18 acute-care hospitals in Kyushu, Japan, as part of the Nagasaki, Fukuoka, Oita, Miyazaki, and Saga NTM study (NFOMS NTM study)12. The study population included patients aged ≥ 18 years with newly diagnosed NTM-PD who presented at the study centres between 1 January 2010 and 31 December 2017. Respiratory medicine specialists at each facility reviewed the medical records to collect data on patient characteristics, comorbidities, causative mycobacteria, laboratory findings, radiological features at the time of definitive NTM-PD diagnosis, treatment, and outcomes during the observation period. Patient follow-up continued until 31 December 2022. All data were collected using Research Electronic Data Capture (REDCap®). Data regarding the duration of oral corticosteroid (OCS) administration and the total dosage were not collected. Given the nature of multicentre retrospective studies, it is difficult to determine whether death was attributable solely to MAC-PD. MAC-PD is frequently associated with structural lung destruction, which may lead to respiratory failure or predispose patients to secondary infections caused by non-MAC pathogens—both of which can contribute to mortality. Therefore, we defined respiratory infection-related mortality as deaths in which MAC-PD was likely involved and evaluated the associated prognostic factors. Respiratory infection-related deaths were determined at the discretion of the attending physicians at each facility, based on their review of medical records.
To develop a scoring model for risk factors associated with respiratory infection-related mortality, eligible patients were randomly allocated to a 4:1 ratio to the derivation and validation groups. The risk factors for respiratory infection-related mortality were identified in the derivation group, and a scoring model was developed based on these factors to ensure consistency in the validation group. This study was conducted in accordance with the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (IRB) of Nagasaki University Hospital (approval number: 22121903). Verbal informed consent was obtained whenever possible, and an opt-out option was provided to the patients as this was a retrospective observational study. The IRB approved the waiver of informed consent.
Definitions for NTM-PD
The 2008 Japanese Society for Tuberculosis and Nontuberculous Mycobacteriosis (JSTNM) criteria were used to diagnose NTM-PD13. These diagnostic criteria were based on the 2007 official American Thoracic Society (ATS)/Infectious Diseases Society of America (IDSA)14. However, the JSTNM criteria do not include clinical symptoms, in contrast to the current 2020 ATS/European Respiratory Society/European Society of Clinical Microbiology and Infectious Diseases/IDSA guideline6. Identification methodologies for NTM species vary by institution and include PCR for M. avium and M. intracellulare, DNA–DNA hybridisation, and matrix-assisted laser desorption/ionisation-time-of-flight mass spectrometry. Radiological classification was conducted based on chest computed tomography and categorised by experts as nodular bronchiectasis (NB), NB with a cavity, or FC patterns.
Exclusion criteria
The primary objective of this study was to identify risk factors for respiratory infection-related mortality in patient with MAC-PD and develop a prognostic scoring model. Consequently, patients without MAC-PD were excluded. Further exclusion criteria included referral to other institutions for initial treatment.
Statistical analysis
Continuous variables were analysed using the Mann–Whitney U test, whereas categorical variables were examined using Fisher’s exact test. Cox proportional hazards analysis included variables that showed significant differences as assessed by experts, as well as those considered clinically relevant. A MAC-PD mortality prediction scoring model was developed based on Cox proportional hazards analysis results, and a receiver operating characteristic (ROC) curve was generated to evaluate the model’s performance. Cases with missing data were excluded from the multivariable analysis, and multicollinearity was assessed using the variance inflation factor (VIF), with a cutoff value of VIF > 5.
Survival analysis was performed using the log-rank test. All P values were two-sided, and P ≤ 0.05 were considered statistically significant. Group comparisons, multivariable analysis, and survival analysis were performed using GraphPad Prism ver. 10.4.2 (GraphPad Software, CA, USA), while the evaluation of ROC curves for the scoring model was conducted using JMP Pro ver. 18.1.0 (SAS Institute, Cary, NC, USA).
Results
Patients characteristics
During the study period, 1,317 patients were newly diagnosed with NTM-PD. The final analysis included 1,165 cases, with 139 cases excluded because of non-MAC-PD (Fig. 1). The mean age was 70.7 years, and 371 (31.8%) were male. M. avium and M. intracellulare were detected in 517 (44.4%) and 648 (55.6%) patients, respectively (Table 1). Within 5 years, 656 (56.3%) patients received treatment for MAC-PD. During the observation period, all-cause mortality occurred in 183 patients (15.7%), and respiratory infection-related mortality occurred in 67 patients (5.8%). In total, 932 and 233 patients were randomly allocated to the derivation and validation groups, respectively.
Risk factors for mortality
To identify the risk factors for respiratory infection-related mortality in MAC-PD, we evaluated the backgrounds, comorbidities, and laboratory findings at diagnosis of 932 patients in the derivation group. Univariate analysis revealed that age ≥ 65 years, male sex, BMI < 18.5, interstitial pneumonia (IP), chronic obstructive pulmonary disease (COPD), bronchial asthma, oral corticosteroid (OCS) use, inhaled corticosteroid use (ICS), Alb < 3.5 g/dL, elevated ESR (> 15 mm/h in male and 20 mm/h in female), lymphocyte count < 1,000/µL, M. intracellulare, cavity formation, and cavitary nodular bronchiectatic pattern were associated with an increased mortality risk (Table 2). Cox proportional hazards analysis was performed using the following variables: age ≥ 65 years, male sex, IP, COPD, ICS use, Alb < 3.5 g/dL, and cavitary lesions ≥ 2 cm in diameter (Table 2). Multicollinearity among these variables was assessed using the VIF, and all variables had VIF values below 3, indicating negligible multicollinearity. ESR was excluded because of missing data for 563 patients (60.4%). The results indicated that age ≥ 65 years, male sex, IP, Alb < 3.5 g/dL, and cavitary lesions ≥ 2 cm in diameter were independent risk factors for respiratory-infection related mortality (Table 2).
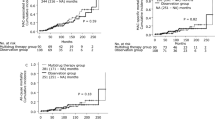
Overall, respiratory infection-related death occurred in 32 males (11.0%) and 19 females (3.0%). Male had a significantly higher respiratory infection-related mortality rate than female, as assessed by the log-rank test, with a crude hazard ratio of 5.12 (95% confidence interval [CI]: 2.63–9.99) (Fig. 2a). Age ≥ 65 years was significantly associated with respiratory infection-related mortality (HR 4.02, 95% CI: 2.18–7.44; Fig. 2b), as was IP (HR 5.32, 95% CI: 1.18–24.1; Fig. 2c). Hypoalbuminemia (Alb < 3.5 g/dL) demonstrated the strongest association (HR 8.69, 95% CI: 3.69–20.5; Fig. 2d), while cavitary lesions ≥ 2 cm in diameter were also significantly associated (HR 4.20, 95% CI: 1.56–11.3; Fig. 2e).
Kaplan–Meier analyses of patients in the derivation group. Male sex (a), age over 65 years (b), IP (c), hypoalbuminemia (d), and cavity formation (e) were associated with a significantly poorer prognosis. Without cavity ≥ 2 cm includes patients with no cavity or cavities < 2 cm. Cases with missing data were excluded from the analysis. IP, interstitial pneumonia.
Throughout the study, 33 patients (3.5%) in the derivation group and 6 patients (2.6%) in the validation group had coinfection with chronic pulmonary aspergillosis (CPA), either at diagnosis or during follow-up (Table 1). In a univariate analysis of respiratory infection-related mortality, the development of CPA was significantly associated with mortality, with a crude HR of 6.64 (95% CI: 3.0–13.0). Because CPA typically developed after the diagnosis of NTM-PD, it was not included as a variable in the Cox proportional hazards analysis.
Construction of the prognostic scoring model
We included 5 independent risk factors identified through multivariate analysis to develop a prognostic scoring model. Based on the adjusted hazard ratios from the Cox proportional hazards model in the derivation group, we developed a scoring system (MAC prognostic score) by assigning 2 points to Alb < 3.5 g/dL, and 1 point each to age ≥ 65 years, male sex, IP, and cavitary lesions ≥ 2 cm in diameter.
Among the 795 patients in the derivation group without missing scoring data, the area under the ROC curve (AUC) for the MAC prognostic score was 0.86 (Fig. 3a). To determine the optimal prognostic cutoff value for respiratory infection-related mortality within 5 years, we calculated the Youden index (sensitivity + specificity − 1) based on the ROC curve. A score of ≥ 3 yielded the highest index. At this cutoff, the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio, and negative likelihood ratio were 81.8%, 74.7%, 12.3%, 99.0%, 3.23, and 0.14, respectively. The treatment induction rates within 5 years of diagnosis were 75.0% (96/128) for score 0, 54.3% (242/447) for scores 1–2, 53.4% (99/185) for scores 3–4, and 62.9% (22/35) for scores 5–6. The Kaplan–Meier curves for the MAC prognostic score demonstrated significantly different prognoses for each score (Fig. 3b). The 5-year respiratory infection-related mortality rates were 0.0% (0/128) for score 0, 1.3% (6/447) for scores 1–2, 8.1% (15/185) for scores 3–4, and 34.3% (12/35) for scores 5–6. A higher score was associated with a poorer prognosis.
Receiver operating characteristic curve for MAC score and Kaplan–Meier analysis in the derivation group. (a) ROC curve of MAC score in the derivation group (n = 795). Cases with missing data were excluded from the analysis. The AUC was 0.86. The sensitivity and specificity were 81.8 and 74.7%, respectively, at a cutoff value of 3. (b) Kaplan–Meier analysis stratified by MAC score in the derivation group. MAC scores exceeding 3 points showed poor survival outcomes. AUC, area under the curve; ROC, receiver operating characteristic.
Validation of the MAC prognostic score
The MAC prognostic score was subsequently adapted for the validation group and evaluated. Figure 4a shows the ROC curve based on 196 patients without missing scoring data, with an AUC of 0.81. At a cutoff value of 3 points, the sensitivity, specificity, PPV, and NPV for respiratory infection-related mortality within 5 years were 76.9%, 73.8%, 17.2%, and 97.8%, respectively. The treatment induction rates within 5 years of diagnosis were 76.5% (26/34) for score 0, 54.8% (57/104) for scores 1–2, 47.8% (22/46) for scores 3–4, and 66.7% (8/12) for scores 5–6. The Kaplan–Meier curves also demonstrated different prognoses for each score in the validation group (Fig. 4b). The 5-year respiratory infection-related mortality rates were 0.0% (0/34) for score 0, 2.9% (3/104) for scores 1–2, 8.7% (4/46) for scores 3–4, and 25.0% (3/12) for scores 5–6. In the validation group, scores of 3 or higher were associated with a significantly worse prognosis compared to scores below 3.
Receiver operating characteristic curve for MAC score and Kaplan–Meier analysis in the validation group. (a) ROC curve of MAC score in the validation group (n = 196). Cases with missing data were excluded from the analysis. The AUC was 0.81. The sensitivity and specificity were 76.9 and 73.8%, respectively, at a cutoff value of 3. (b) Kaplan–Meier analysis stratified by MAC score in the validation group. MAC scores exceeding 3 points showed poor survival outcomes. AUC, area under the curve; ROC, receiver operating characteristic.
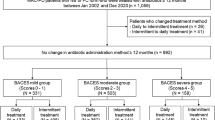
Comparison with the BACES score
The MAC prognostic scores were compared with the BACES scores. A total of 373 patients were included in the analysis, after excluding the cases lacking BMI data195 (16.7%), ESR data 698 (59.9%), or Alb data 173 (14.8%). The AUCs of the MAC prognostic score and BACES score were 0.82 and 0.88, respectively, with no statistically significant differences (Fig. 5a). The Kaplan–Meier curves for the MAC prognostic score and BACES score are presented (Figs. 5b, c). Compared with the BACES score, the MAC prognostic score demonstrated a non-inferior ability to identify the poor prognosis group.
Comparison of MAC and BACES scores. (a) ROC curves of MAC and BACES scores in the population without data loss (n = 373). The AUCs of the MAC and BACES scores were 0.82 and 0.88, respectively, with no significant differences. Kaplan–Meier curves for (b) the MAC score and (c) the BACES score showed comparable prognostic discrimination. AUC, area under the curve; ROC, receiver operating characteristic.
Discussion
In this study, we developed a prognostic scoring model to identify patients predicted to have poor prognosis in patients with MAC-PD. Multivariate analysis revealed that age ≥ 65 years, male sex, IP, albumin < 3.5 g/dL, and cavitary lesions ≥ 2 cm in diameter were independent prognostic factors. The MAC prognostic score demonstrated efficacy in identifying patients with poor prognosis.
BACES score is a prognostic tool for NTM-PD, and a separate prognostic score for MAC-PD has been reported in Japan10,11. The 5-year all-cause mortality rates in the derivation cohorts of these two reports were 21% and 20.5%, respectively, both higher than the 15.7% observed in the present study. The derivation cohorts in these reports were drawn from a single-centre study at a tertiary care hospital, which may have had a more severe case distribution than that in our report. In contrast, our study included 18 facilities with diverse backgrounds, ranging from tertiary care facilities to local hospitals12. A key strength of this study is its multicentre design, incorporating diverse hospitals, which enhances the generalizability of the findings to real-world clinical practice. Furthermore, while previous studies have investigated predictors of all-cause mortality, this study uniquely identified risk factors specifically associated with respiratory infection-related mortality.
When developing the scoring model, the variables were limited to those with a high-hazard ratio, those of clinical significance, or those whose data could be readily obtained in practice. This approach was necessary because of the small number of events in the derivation group (n = 51) and the need to develop a clinically applicable and efficient scoring model. In the present study, age ≥ 65 years, male sex, IP, albumin < 3.5 g/dL, and cavitary lesions ≥ 2 cm in diameter were identified as risk factors. Advanced age, male sex, hypoalbuminemia, and cavitary lesions have been identified as independent prognostic factors in several studies on NTM-PD10,11,15,16. IP has been identified as an independent risk factor for the development of NTM-PD, as demonstrated by a meta-analysis17. However, IP has not been clearly established as a prognostic factor for NTM-PD in large-scale studies. In the present study, we did not collect specific information on the subtypes of IP. However, several studies have suggested that the prognosis of patients with pleuroparenchymal fibroelastosis (PPFE), a distinct subtype of IP, complicated by NTM-PD, is extremely poor. For instance, radiological findings consistent with PPFE have been observed in 11.9% of patients with MAC-PD, and these patients exhibited significantly worse prognoses compared to those without such findings18. Moreover, the prognosis of NTM-PD patients with concomitant PPFE is poorer than that of patients with cavitary NB or FC types of NTM-PD19. In addition, respiratory infections such as NTM-PD have been suggested as potential causative factors in non-idiopathic PPFE20. These observations suggest a close association between PPFE and NTM-PD. Although the presence of PPFE could not be assessed in the present study, it is possible that the poor prognosis observed in patients with IP may have been influenced by factors related to PPFE. Consistent with previous reports, the present study also found that the coinfection of CPA during the disease course was associated with a poorer prognosis21,22,23,24. However, because CPA is generally not present at the time of MAC-PD diagnosis, it was not included as a variable in the multivariable analysis.
Despite the higher mortality risk associated with MAC prognostic scores of 5–6, treatment initiation rates were highest in patients with a score of 0 in both the derivation and validation groups. Multivariable analysis identified older age and dementia as negative predictors of treatment initiation, while connective tissue diseases, positive sputum acid-fast bacilli smear, and cavitary lesions were positive predictors (Table S1). As shown in Figure S1, treatment initiation rates declined with increasing age, suggesting that inclusion of age in the score may account for the lower treatment rates among high-score patients. A study involving older patients with MAC-PD reported lower treatment success rates and reduced prognostic impact of therapeutic interventions in those aged ≥ 80 years25, suggesting that the diminished benefit of treatment in this population may have contributed to the lower treatment initiation rates observed in our study.
The MAC prognostic score demonstrated remarkable prognostic predictive capabilities. Among the 991 patients with complete data, 27.7% (220/795) in the derivation group and 29.6% (58/196) in the validation group had scores ≥ 3, which were associated with higher rates of respiratory infection-related mortality. Compared to the BACES score, the MAC prognostic score exhibited non-inferior performance in predicting poor prognosis in patients with MAC-PD. Importantly, the BACES score is not directly comparable, owing to the inclusion of MABC in addition to MAC. Furthermore, while the BACES score evaluates all-cause mortality, our study assessed respiratory infection-related mortality, which more specifically reflects the prognosis directly attributable to MAC-PD.
This study has some limitations. First, due to the retrospective design, some patients had missing data. To ensure data integrity, these patients were excluded from the analysis, and this exclusion may have introduced selection bias. Second, this study was conducted in the Kyushu region of Japan and has not been validated in other regions. Third, although respiratory medicine specialists at each facility reviewed this multicentre study, no standardised validation of the radiological findings and disease type was performed. Furthermore, institutional variations in treatment regimen selection were not considered. In addition, the attribution of death to respiratory infection or other causes was based on the clinical judgment of the attending physicians, which may have introduced variability. Fourth, drug susceptibility test results were not evaluated, particularly macrolide resistance. Notably, a previous study reported a poor prognosis in patients with macrolide-resistant MAC-PD, with a 5-year mortality rate of 47%26, which was not assessed in the present study. Fifth, the association between treatment regimens and prognosis was not examined. Lastly, the scoring model demonstrated a relatively low PPV, possibly due to the relatively small number of deaths in this cohort compared with previous studies. Importantly, few studies have identified prognostic factors specifically associated with respiratory infection-related mortality in patients with MAC-PD. The findings of this multicentre study, therefore, provide valuable insights into disease-specific prognosis and have important implications for clinical risk stratification.
This study identified the following prognostic factors for MAC-PD: age ≥ 65 years, male sex, interstitial pneumonia, albumin < 3.5 g/dL, and cavitary lesions ≥ 2 cm in diameter. A prognostic model incorporating these factors effectively stratified patients by mortality risk. The strengths of this study include its multicentre design, which reflects diverse clinical settings, and the specific evaluation of respiratory infection-related mortality, offering a more disease-focused assessment. Further large-scale prospective studies are warranted to validate this model in other populations.
Data availability
The datasets analysed during the current study are not publicly available as data sharing was not approved by the IRB. However, reasonable requests for data access can be directed to the corresponding author. Upon receiving such a request, we will submit it for IRB review to assess whether data sharing is permissible under the approved ethical framework.
Abbreviations
- Alb:
-
albumin
- ATS:
-
American Thoracic Society
- AUC:
-
area under the curve
- BMI:
-
body mass index
- COPD:
-
chronic obstructive pulmonary disease
- CPA:
-
chronic pulmonary aspergillosis
- ESR:
-
erythrocyte sedimentation rate
- FC:
-
fibrocavitary
- ICS:
-
inhaled corticosteroid
- IDSA:
-
Infectious Diseases Society of America
- IP:
-
interstitial pneumonia
- IRB:
-
Institutional Review Board
- JSTNM:
-
Japanese Society for Tuberculosis and Nontuberculous Mycobacteriosis
- MABC:
-
Mycobacterium abscessus complex
- MAC:
-
Mycobacterium avium-intracellulare complex
- NB:
-
nodular bronchiectatic
- NPV:
-
negative predictive value
- NTM:
-
nontuberculous mycobacteria
- NTM-PD:
-
nontuberculous mycobacterial pulmonary disease
- OCS:
-
oral corticosteroid
- OS:
-
overall survival
- PPFE:
-
pleuroparenchymal fibroelastosis
- PPV:
-
positive predictive value
- ROC:
-
receiver operating characteristic
- VIF:
-
variance inflation factor
References
Adjemian, J., Olivier, K. N., Seitz, A. E., Holland, S. M. & Prevots, D. R. Prevalence of nontuberculous mycobacterial lung disease in U.S. Medicare beneficiaries. Am. J. Respir Crit. Care Med. 185, 881–886 (2012).
Namkoong, H. et al. Epidemiology of pulmonary nontuberculous mycobacterial disease, Japan. Emerg. Infect. Dis. 22, 1116–1117 (2016).
Dahl, V. N. et al. Global trends of pulmonary infections with nontuberculous mycobacteria: a systematic review. Int. J. Infect. Dis. 125, 120–131 (2022).
Harada, K. et al. Trends in the nontuberculous mycobacterial disease mortality rate in japan: a nationwide observational study, 1997–2016. Clin. Infect. Dis. 73, e321–e26 (2021).
Morimoto, K. et al. A laboratory-based analysis of nontuberculous mycobacterial lung disease in Japan from 2012 to 2013. Ann. Am. Thorac. Soc. 14, 49–56 (2017). (2017).
Daley, C. L. et al. Treatment of nontuberculous mycobacterial pulmonary disease: an official ATS/ERS/ESCMID/IDSA clinical practice guideline. Clin. Infect. Dis. 71, e1–e36 (2020).
Van Ingen, J. et al. Poor adherence to management guidelines in nontuberculous mycobacterial pulmonary diseases. Eur. Respir J. 49, 1601855 (2017).
Larsson, L. O. et al. Pulmonary disease by non-tuberculous mycobacteria - clinical management, unmet needs and future perspectives. Expert Rev. Respir Med. 11, 977–989 (2017).
Diel, R., Lipman, M. & Hoefsloot, W. High mortality in patients with Mycobacterium avium complex lung disease: a systematic review. BMC Infect. Dis. 18, 206 (2018).
Kim, H. J. et al. BACES score for predicting mortality in nontuberculous mycobacterial pulmonary disease. Am. J. Respir Crit. Care Med. 203, 230–236 (2021).
Kumagai, S. et al. Development and validation of a prognostic scoring model for Mycobacterium avium complex lung disease: an observational cohort study. BMC Infect. Dis. 17, 436 (2017).
Tanaka, Y. et al. Risk factors and Long-Term prognosis for coinfection of nontuberculous mycobacterial pulmonary disease and chronic pulmonary aspergillosis: A multicentre observational study in Japan. Mycoses 68, e70083 (2025).
Nontuberculous Mycobacteriosis Control Committee of the Japanese Society for T. Scientific assembly for I, tuberculosis of the Japanese respiratory S, international exchanging committee of the Japanese society for T. Guidelines for the diagnosis of pulmonary nontuberculous mycobacterial diseases–2008. Kekkaku 86, 37–39 (2011).
Griffith, D. E. et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am. J. Respir Crit. Care Med. 175, 367–416 (2007).
Hayashi, M. et al. Prognostic factors of 634 HIV-negative patients with Mycobacterium avium complex lung disease. Am. J. Respir Crit. Care Med. 185, 575–583 (2012).
Gochi, M. et al. Retrospective study of the predictors of mortality and radiographic deterioration in 782 patients with nodular/bronchiectatic Mycobacterium avium complex lung disease. BMJ Open. 5, e008058 (2015).
Loebinger, M. R. et al. Risk factors for nontuberculous mycobacterial pulmonary disease: A systematic literature review and Meta-Analysis. Chest 164, 1115–1124 (2023).
Aono, Y. et al. Prognostic significance of radiological pleuroparenchymal fibroelastosis in Mycobacterium avium complex lung disease: a multicentre retrospective cohort study. Thorax 78, 825–834 (2023).
Tanaka, H. et al. Distinctive clinical features of radiological pleuroparenchymal fibroelastosis with nontuberculous mycobacterial pulmonary disease: A multicenter retrospective cohort study. Int. J. Infect. Dis. 148, 107233 (2024).
Chua, F. et al. Pleuroparenchymal fibroelastosis. A review of clinical, radiological, and pathological characteristics. Ann. Am. Thorac. Soc. 16, 1351–1359 (2019).
Phoompoung, P. & Chayakulkeeree, M. Chronic pulmonary aspergillosis following nontuberculous mycobacterial infections: an emerging disease. J. Fungi (Basel). 6, 346 (2020).
Takeda, K. et al. The risk factors for developing of chronic pulmonary aspergillosis in nontuberculous mycobacteria patients and clinical characteristics and outcomes in chronic pulmonary aspergillosis patients coinfected with nontuberculous mycobacteria. Med. Mycol. 54, 120–127 (2016). (2016).
Furuuchi, K., Ito, A., Hashimoto, T., Kumagai, S. & Ishida, T. Risk stratification for the development of chronic pulmonary aspergillosis in patients with Mycobacterium avium complex lung disease. J. Infect. Chemother. 24, 654–659 (2018).
Takazono, T. et al. Risk factors and prognostic effects of aspergillosis as a complication of nontuberculous mycobacterial pulmonary disease: a nested case-control study. Mycoses 68, e70022 (2025).
Kim, J. Y., Kim, N. Y., Jung, H. W., Yim, J. J. & Kwak, N. Old age is associated with worse treatment outcome and frequent adverse drug reaction in Mycobacterium avium complex pulmonary disease. BMC Pulm Med. 22, 269 (2022).
Moon, S. M. et al. Clinical characteristics, treatment outcomes, and resistance mutations associated with macrolide-resistant mycobacterium avium complex lung disease. Antimicrob Agents Chemother. ; 60, 6758–6765 (2016). (2016).
Acknowledgements
The authors are grateful to Y. Ito, S. Koga, H. Ashizawa, K. Fukushima, N. Matsuo, S. Yoshioka, Y. Tanaka, D. Noritomi, Y. Fukushima, S. Kaneko, R. Morio, R. Mizuta, T. Inoue, T. Ikeda, A. Hara, D. Setoguchi, K. Mine, Y. Hirano, Y. Nagayoshi, R. Morishita, Y. Usui, K. Yoshiyama, S. Tomari, S. Doi, A. Umemura, Y. Umeyama, T. Miyamura, Ryosuke Ogata, Ryo Ogata, C. Iketani, K. Nemoto, M. Funada, Y. Isoshima, S. Shigemi, H. Kanda, M. Sumiyoshi, E. Kitamura, A. Kitamura, N. Matsumoto, A. Sano, A. Matsuo, E. Mitsutome, Y. Ideguchi, M. Yamasue, R. Takaki, and K. Tobino for their review of the medical records. We also thank R. Kawasaki and H. Yano of the Clinical Research Center, Nagasaki University Hospital, for building the electronic data capture system. Editage (www.editage.jp) was used for the English language editing. This work was partly supported by a nonprofit organisation aimed at supporting community medicine research in Nagasaki (3612) and the Joint Research Program of the Research Center for GLOBAL and LOCAL Infectious Diseases, Oita University (2023B15).
Funding
This work was partly supported by a nonprofit organisation supporting community medicine research in Nagasaki (3612) and the Joint Research Program of the Research Center for GLOBAL and LOCAL Infectious Diseases, Oita University (2023B15). The funds for this study were used to manage the electronic data capture system, statistical analyses, and English editing.
Author information
Authors and Affiliations
Contributions
K.T. wrote the main manuscript and prepared all figures and tables. K.T. and T.T. and S.I1. devised the concept of the study.T.T. and H.M. supervised the study.K.T., S.I1., M.Y., N.I., N.H., Y.T., S.I2., T.S1., T.M., A.K., T.K., Y.F., E.S., T.S2., Y.H., K.H., M.H., T.I., K.F., K.K., T.M. and K.Y1. investigated patient data. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
This study was conducted in accordance with the guidelines of the Declaration of Helsinki and approved by the appropriate Institutional Review Board of Nagasaki University Hospital (approval number: 22121903). Verbal informed consent was obtained whenever possible. As this was a retrospective observational study, an opt-out option was provided to the patients.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Takeda, K., Takazono, T., Ide, S. et al. Multicentre retrospective observational study for development and validation of MAC prognostic score model. Sci Rep 15, 28539 (2025). https://doi.org/10.1038/s41598-025-14348-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-14348-7