Abstract
Although the clinical importance of osteoporosis in middle-aged populations is widely recognized, the intricate relationships between body composition parameters, especially osteosarcopenic obesity, and bone health remain incompletely understood. This study aims to characterize the association between the skeletal muscle mass-to-visceral adipose tissue area ratio (SVR) and bone mineral density (BMD), while systematically evaluating potential variations by sex and menopausal status. Utilizing data from the National Health and Nutrition Examination Survey (2011–2018), we analyzed a cohort of 4,349 middle-aged adults (ages 40–59) with complete datasets on skeletal muscle mass (SMM), visceral adipose tissue area (VATA), and lumbar BMD. Dual-Energy X-ray Absorptiometry was employed for precise body composition analysis. Multivariate regression models were applied to analyze the relationships between SVR and BMD, with stratified analyses conducted to evaluate potential effect modifications by sex and menopausal status. Our findings revealed a significant positive correlation between SMM and BMD (β = 12.8, 95% CI: 11.2 to 14.4), while VATA exhibited an inverse relationship (β = -0.5, 95% CI: -0.6 to -0.4). Notably, men demonstrated a positive association between SVR and BMD (β = 342.4, 95% CI: 271.4 to 413.5), whereas premenopausal women displayed a non-linear, inverted U-shaped relationship between SVR and BMD, with a critical threshold identified at 0.31 kg/cm². This cross-sectional study highlights the association between SVR and lumbar BMD in middle-aged adults, revealing significant sex-specific differences. In men, higher SVR correlates with higher BMD, while in premenopausal women, BMD appears optimal when SVR falls within a specific range.
Similar content being viewed by others
Introduction
Bone mineral density (BMD) is a key biomarker for osteoporosis and fracture risk, gaining increasing relevance with population aging1,2. Once considered an inevitable aspect of aging, bone loss is now understood as a modifiable process, with middle age representing a critical window for intervention—before the accelerated skeletal decline of later life3,4. This period offers a strategic opportunity for proactive bone health management5. Identifying and targeting the physiological mechanisms underlying midlife bone metabolism could help mitigate age-related BMD deterioration, highlighting the importance of research in this demographic.
As metabolically active components of body composition, skeletal muscle and adipose tissue exhibit complex, often opposing interactions that significantly influence bone metabolism6,7. While skeletal muscle enhances bone formation via mechanical loading and myokine secretion8, adipose tissue disrupts bone homeostasis through pro-inflammatory cytokines and metabolic dysfunction8,9,10. Prior research has largely studied these tissues in isolation, overlooking their interdependent relationship. The skeletal muscle mass-to-visceral adipose tissue area ratio (SVR) provides a novel composite measure that reflects this physiological interplay, offering valuable insights into sarcopenic obesity and metabolic risk11,12. However, the association between SVR and BMD remains poorly understood, representing a key gap in our knowledge of body composition’s impact on bone health.
Sex hormones, particularly estrogen and testosterone, differentially regulate body composition and skeletal homeostasis13,14, introducing sex-specific variations in the muscle-fat-bone relationship. The menopausal transition, marked by rapid estrogen depletion, highlights a key knowledge gap regarding SVR’s influence on BMD, as current evidence lacks comprehensive sex- and menopause-stratified analyses. Using the National Health and Nutrition Examination Survey (NHANES) data with Dual-Energy X-ray Absorptiometry (DXA) -derived measurements, this study examines sex-specific associations between SVR and lumbar BMD in middle-aged adults.
Methods
Study design and population
NHANES is a comprehensive cross-sectional study conducted by the Centers for Disease Control and Prevention, offering a nationally representative assessment of the health and nutritional status of the U.S. population. Employing a rigorous methodology, NHANES integrates standardized household interviews with detailed physical examinations at Mobile Examination Centers, generating high-quality, multidimensional epidemiological data. In this investigation, we leveraged NHANES data from 2011 to 2018 to elucidate the intricate relationships between skeletal muscle mass (SMM), visceral adipose tissue area (VATA), and their compositional ratio with lumbar BMD among middle-aged adults. The research protocol received approval from the National Center for Health Statistics Research Ethics Review Board, with written informed consent obtained from all participants. This study was conducted in accordance with the ethical principles of the Declaration of Helsinki and reported following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines15.
From an initial cohort of 39,156 individuals, we implemented rigorous inclusion and exclusion criteria to optimize data quality and research precision. Participant selection criteria were meticulously defined: individuals aged 40–59 years with complete datasets encompassing SMM, VATA, and lumbar BMD. We systematically refined the sample by excluding participants with: incomplete covariate information, ambiguous menstrual status, and documented cancer history. Following comprehensive screening, the final analytical sample comprised 4,349 participants (Fig. 1).
Measurements of SVR and lumbar BMD
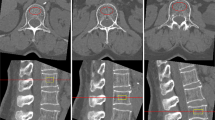
DXA was employed for body composition analysis, enabling precise quantification of SMM, VATA, and lumbar BMD. SMM was calculated by aggregating lean mass from all four extremities using whole-body DXA scan data. VATA was meticulously measured at the intervertebral space between L4 and L5 vertebrae. To ensure optimal data quality, all DXA examinations were conducted by radiologic technologists with specialized training and certification in precision imaging techniques.
Confounding variables
The analytical framework incorporated a multidimensional set of covariates, stratifying participants by demographic characteristics including age, sex (men, premenopausal and postmenopausal women), race/ethnicity (non-Hispanic White, non-Hispanic Black, Mexican American, and other), educational level (less than high school, high school, and more than high school), and marital status (married/living with partner, widowed/divorced/separated, and never married). Behavioral and physiological parameters were meticulously assessed, encompassing body mass index (BMI), sedentary lifestyle, hypertension and diabetes history, and serum biochemical markers (calcium, glucose, total protein, blood urea nitrogen, triglycerides, and total cholesterol). Demographic information was extracted from validated questionnaires. Sedentary status was determined through self-reported questionnaires, with participants classified as sedentary behavior if they reported no participation in either moderate or vigorous leisure-time physical activities. Menopausal status was classified based on self-reported absence of menstruation for ≥ 12 month. Hypertension and diabetes histories were systematically documented using specific questionnaire modules. Detailed methodological protocols are publicly accessible at wwwn.cdc.gov/nchs/nhanes/.
Statistical analyses
Descriptive statistics were expressed as mean ± standard deviation for continuous variables and percentages for categorical variables. Inter-group differences were rigorously evaluated using appropriate statistical tests: χ² tests for categorical data, one-way ANOVA for normally distributed continuous variables, and Kruskal-Wallis H tests for skewed distributions.
Multivariate linear regression analyses were employed to examine the correlations of SMM, VATA, and SVR with lumbar BMD, adhering to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines15. The analytical strategy comprised four progressive regression models: Model 1: unadjusted base model; Model 2: adjusted for age, sex, and race; Model 3: additional adjustment for BMI; Model 4: fully adjusted for all pre-screened covariates. Subgroup analyses were conducted using stratified linear regression models to explore potential effect modifications across demographic and clinical subpopulations. To comprehensively characterize the relationship, we applied advanced statistical techniques, including smooth curve fitting and generalized additive models, to investigate potential non-linear associations. We further employed a two-piecewise regression model to investigate the threshold effect of SVR on lumbar BMD. All statistical analyses were performed using R software (version 3.4.3) and EmpowerStats (X&Y Solutions, Inc., Boston, MA). Statistical significance was defined as two-sided P values less than 0.05.
Results
The characteristics of participants across sex and menopausal status are presented in Table 1. BMI progressively increased from men (28.8 ± 5.5) to premenopausal (29.8 ± 7.5) to postmenopausal women (30.1 ± 7.0), with postmenopausal women experiencing notably higher hypertension (40.8%) and diabetes (14.3%) prevalence. Men exhibited the highest SMM (26.8 ± 5.0 kg), significantly surpassing premenopausal (18.6 ± 4.4 kg) and postmenopausal women (18.1 ± 4.0 kg). VATA was correspondingly higher in men (129.5 ± 54.9 cm²) compared to premenopausal (105.2 ± 55.7 cm²) and postmenopausal women (125.2 ± 59.5 cm²). SVR stratification revealed highest values in men (0.24 ± 0.11 kg/cm²), followed by premenopausal (0.23 ± 0.17 kg/cm²) and postmenopausal women (0.18 ± 0.13 kg/cm²). Lumbar BMD demonstrated significant variations, with postmenopausal women showing the lowest values (976.4 ± 158.5 mg/cm²) compared to premenopausal women (1065.5 ± 148.3 mg/cm²) and men (1023.5 ± 164.3 mg/cm²).
Correlation analyses unveiled significant associations between body composition components and lumbar BMD. SMM demonstrated a positive correlation with BMD, whereas VATA exhibited an inverse relationship (Table 2). SVR exhibited a progressive and systematic increase across sequential multivariate regression models. These intricate associations were comprehensively validated through advanced statistical modeling and graphical representations (Fig. 2).
Subgroup analysis revealed pronounced sex-specific interactions in the associations between SMM, VATA, and SVR with lumbar BMD (Fig. 3). Postmenopausal women demonstrated a positive relationship with SMM (β = 15.3, 95% CI: 11.4–19.2), while men exhibited an inverse relationship with VATA (β = -0.7, 95% CI: -0.9 to -0.6). The SVR revealed significant sex differences, with men demonstrating a stronger association (β = 342.4, 95% CI: 271.4-413.5) than postmenopausal women (β = 156.6, 95% CI: 78.1-235.1). Notably, this association remained statistically non-significant in premenopausal women (β = 44.6, 95% CI: -11.6-100.8). In racial/ethnic subgroup analyses, the most pronounced association between SVR and BMD was observed in Mexican American participants (β = 305.9, 95% CI: 160.1-451.6).
Generalized additive models and smooth curve fittings substantiated these sex-stratified associations (Fig. 4), notably revealing an inverted U-shape relationship in premenopausal women between SVR and lumbar BMD. As initial linear regression analysis revealed no statistically significant association between SVR and BMD in premenopausal women, a two-piecewise linear regression model was conducted and identified a critical threshold at 0.31 kg/cm², demonstrating a significant positive association below this point (β = 360.48, 95% CI: 206.18-514.78) and a negative trend beyond it (β = -47.05, 95% CI: -116.66-22.55), with the log-likelihood ratio test confirming the model’s statistical significance (Table 3).
The correlations of skeletal muscle mass, visceral adipose tissue area and their ratio with lumbar bone mineral density. Age, sex, race, educational level, marital status, sedentary behavior, history of hypertension, history of diabetes, body mass index, total protein, blood urea nitrogen, serum calcium, serum glucose, triglycerides and total cholesterol were adjusted.
Subgroup analysis of the correlations of skeletal muscle mass, visceral adipose tissue area and their ratio with lumbar bone mineral density. Age, sex, race, educational level, marital status, sedentary behavior, history of hypertension, history of diabetes, body mass index, total protein, blood urea nitrogen, serum calcium, serum glucose, triglycerides and total cholesterol were adjusted. In the subgroup analysis, the model is not adjusted for the stratification variable itself. SMM: skeletal muscle mass VATA: visceral adipose tissue area SVR: skeletal muscle mass to visceral adipose tissue area ratio.
Sex-stratified smooth curve analysis of the the correlations of skeletal muscle mass, visceral adipose tissue area and their ratio with lumbar bone mineral density. Age, race, educational level, marital status, sedentary behavior, history of hypertension, history of diabetes, body mass index, total protein, blood urea nitrogen, serum calcium, serum glucose, triglycerides and total cholesterol were adjusted.
Discussion
Our investigation found distinct associations between body composition and lumbar BMD in middle-aged adults. SMM showed a strong positive correlation with BMD, whereas VATA displayed a significant inverse relationship. Most strikingly, the SVR-BMD association demonstrated marked sexual dimorphism: men exhibited a robust linear correlation, while premenopausal women showed a characteristic inverted U-shaped relationship.
Our findings aligned with and extend existing literature on the complex interplay between body composition and bone health. Previous research has consistently demonstrated the protective role of skeletal muscle on bone health, with studies revealing positive associations between muscle mass and BMD across diverse age groups, including both adults and adolescents16,17,18. Concurrently, visceral adipose has been substantiated as a negative predictor of BMD, reinforcing the detrimental metabolic impact of excess adiposity19,20. Our sex-stratified analyses revealed distinct sexual dimorphism in body composition-BMD relationships: postmenopausal women showed the strongest positive association between SMM and BMD, whereas men exhibited the most marked inverse relationship between VATA and BMD. These differential associations suggest fundamental sex-specific regulatory pathways in bone metabolism, supporting the implementation of sex-differentiated clinical approaches.
The innovative application of SVR as a composite metric addresses a critical limitation of isolated tissue analyses by revealing a sophisticated inverted U-shaped association in premenopausal women, thereby challenging the linear assumptions of previous models. Evidence suggests that increased visceral adiposity and decreased muscle mass are associated with various metabolic and cardiovascular risks, including dyslipidemia, insulin resistance, and metabolic syndrome21,22,23. We hypothesized that a moderate SVR optimizes the mechanical and metabolic synergy essential for bone health, while extremes may disrupt this equilibrium, potentially affecting bone health indirectly by altering metabolic pathways and hormonal balance24,25. The stronger association between SVR and BMD in men likely reflects their inherently greater muscle mass and lower estrogen levels, which enhance the relative contribution of mechanical loading to bone maintenance26,27. The threshold effect observed in premenopausal women indicates a dynamic interplay between anabolic muscle-driven and catabolic fat-driven signals, influenced by the hormonal stability characteristic of this phase28,29. Future studies should investigate whether interventions targeting SVR optimization can improve BMD in this population.
The intricate balance between SMM and VATA emerges as a pivotal determinant of optimal BMD. Robust SMM confers both mechanical and metabolic advantages that safeguard against osteoporosis, whereas excessive VATA precipitates adverse metabolic and inflammatory cascades detrimental to bone health. Mechanistically, skeletal muscle exerts direct mechanical forces on bone tissue, stimulating osteogenesis and remodeling processes essential for BMD maintenance30. Furthermore, myokines secreted by skeletal muscle, particularly irisin, play a crucial role in enhancing bone formation, with specific effects on cortical bone architecture31,32. Concurrently, skeletal muscle-derived adipokines, including leptin and adiponectin, modulate glucose metabolism and systemic inflammation, thereby indirectly influencing bone metabolism through complex endocrine pathways33,34. In contrast, visceral fat accumulation triggers the release of pro-inflammatory cytokines such as IL-6 and TNF-α, which disrupt bone homeostasis and promote osteoclastogenesis35,36. While animal and in vitro studies suggest that myokines and adipokines modulate bone metabolism, these biomarkers were not available in our dataset to directly test their roles. Thus, the observed associations may reflect broader muscle-fat-bone interactions warranting further investigation. Notably, the inverted U-shaped association in premenopausal women suggests a hormonally sensitive equilibrium. While moderate SVR optimizes the anabolic effects of muscle-derived mechanical loading on bone formation, excessively high SVR could disrupt endocrine homeostasis in this population. On the other hand, for clinical settings lacking DXA capabilities, SVR may be approximated using widely available tools such as bioelectrical impedance analysis for muscle mass assessment and waist circumference measurements for visceral fat estimation, though with acknowledged limitations in precision compared to DXA.
To the best of our knowledge, this is one of the first studies to employ the SVR metric for characterizing a non-linear, inverted U-shaped relationship between body composition and lumbar BMD in premenopausal women, while also highlighting sex-specific differences in middle-aged adults. The large sample size enhances the reliability of our findings and allows for meaningful statistical analyses. Furthermore, the standardized data collection process ensures high-quality and consistent measurements of the variables. However, several limitations should be noted. First, the study’s reliance on NHANES data precludes causal inference, as temporal relationships between SVR and BMD cannot be established. Longitudinal studies are required to delineate dynamic changes in body composition and bone health trajectories. Second, although we adjusted for several covariates, residual confounding may still exist due to unmeasured factors such as hormonal levels, measurements of key biomarkers (e.g., myokines, adipokines, inflammatory cytokines), dietary habits and genetic predispositions, which could modulate muscle-fat-bone interactions. Third, menopausal status was determined solely by self-reported menstrual history, which may misclassify women with irregular cycles. Fourth, our study, focused on middle-aged adults and excluding individuals with a history of cancer, enhances internal validity while inherently limiting the generalizability of the findings to younger and older populations, as well as cancer survivors, who may possess differing body composition and bone health profiles.
Conclusion
In conclusion, this study found significant associations between SVR and lumbar BMD in middle-aged adults, with notable sex-specific variations. Notably, men exhibitd a positive correlation between elevated SVR and higher BMD, whereas in premenopausal women, BMD appeared to peak within an specific SVR range. These results advocate for a personalized approach to osteoporosis prevention, emphasizing the importance of considering individual body composition profiles in clinical practice.
Data availability
The data of this study are publicly available on the NHANES website (https://wwwn.cdc.gov/nchs/nhanes/).
References
Anish, R. J. & Nair, A. Osteoporosis management-current and future perspectives - A systemic review. J. Orthop. 53, 101–113 (2024).
Ensrud, K. E. & Crandall, C. J. Osteoporosis. Ann. Intern. Med. 177 (1), Itc1–itc16 (2024).
Michalek, J. E. et al. Changes in total body bone mineral density following a common bone health plan with two versions of a unique bone health supplement: a comparative effectiveness research study. Nutr. J. 10, 32 (2011).
Wan, M., Gray-Gaillard, E. F. & Elisseeff, J. H. Cellular senescence in musculoskeletal homeostasis, diseases, and regeneration. Bone Res. 9 (1), 41 (2021).
Jamil, N. A., Dhanaseelan, J. & Buhari, N. A. Effectiveness of an e-Book on bone health as educational material for adolescents: Single-Group experimental Study. JMIR Pediatr. Parent. 7, e56611 (2024).
Fan, S. et al. Sarcopenic obesity and osteoporosis: research progress and hot spots. Exp. Gerontol. 195, 112544 (2024).
De Lorenzo, A. et al. Association between sarcopenia and reduced bone mass: is osteosarcopenic obesity a new phenotype to consider in weight management settings? Life (Basel) 14(1), 21 (2023).
Severinsen, M. C. K. & Pedersen, B. K. Muscle-Organ crosstalk: the emerging roles of Myokines. Endocr. Rev. 41 (4), 594–609 (2020).
Kawai, M., de Paula, F. J. & Rosen, C. J. New insights into osteoporosis: the bone-fat connection. J. Intern. Med. 272 (4), 317–329 (2012).
Deng, A. F. et al. Bone-organ axes: bidirectional crosstalk. Mil Med. Res. 11 (1), 37 (2024).
Kim, T. N. et al. Skeletal muscle mass to visceral fat area ratio is associated with metabolic syndrome and arterial stiffness: the Korean sarcopenic obesity study (KSOS). Diabetes Res. Clin. Pract. 93 (2), 285–291 (2011).
Xing, M. et al. The relationship between skeletal muscle mass to visceral fat area ratio and metabolic dysfunction-associated fatty liver disease subtypes in middle-aged and elderly population: a single-center retrospective study. Front. Nutr. 10, 1246157 (2023).
Subarajan, P., Arceo-Mendoza, R. M. & Camacho, P. M. Postmenopausal osteoporosis: A review of latest Guidelines. Endocrinol. Metab. Clin. North. Am. 53 (4), 497–512 (2024).
Yuan, W. & Song, C. Crosstalk between bone and other organs. Med. Rev. 2(4), 331–348 (2021).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370 (9596), 1453–1457 (2007).
Qin, X. et al. The association between appendicular skeletal muscle index and bone mineral density in children and adolescents with chronic kidney disease: A cross-sectional study. Med. (Baltim). 102 (50), e36613 (2023).
Lebrasseur, N. K. et al. Skeletal muscle mass is associated with bone geometry and microstructure and serum insulin-like growth factor binding protein-2 levels in adult women and men. J. Bone Min. Res. 27 (10), 2159–2169 (2012).
Han, C. S., Kim, H. K. & Kim, S. Effects of adolescents’ lifestyle habits and body composition on bone mineral density. Int. J. Environ. Res. Public. Health 18(11). (2021).
Zhang, P. et al. Visceral adiposity is negatively associated with bone density and muscle attenuation. Am. J. Clin. Nutr. 101 (2), 337–343 (2015).
Júnior, I. F. et al. The relationship between visceral fat thickness and bone mineral density in sedentary obese children and adolescents. BMC Pediatr. 13, 37 (2013).
Zhang, S. et al. Increased visceral fat area to skeletal muscle mass ratio is positively associated with the risk of cardiometabolic diseases in a Chinese natural population: A cross-sectional study. Diabetes Metab. Res. Rev. 39 (2), e3597 (2023).
Lim, H., Son, K. & Lim, H. Association between skeletal muscle mass-to-visceral fat ratio and dietary and cardiometabolic health risk factors among Korean women with obesity. Nutrients 15(7). (2023).
Liu, D. et al. Relationship between skeletal muscle mass to visceral fat area ratio and cardiovascular risk in type 2 Diabetes. Diabetes Metab. Syndr. Obes. 14, 3733–3742 (2021).
Liu, Y. et al. A comprehensive meta-analysis of risk factors associated with osteosarcopenic obesity: a closer look at gender, lifestyle and comorbidities. Osteoporos. Int. 35 (5), 759–773 (2024).
Conforto, R. et al. Advances in body composition and gender differences in susceptibility to frailty syndrome: role of osteosarcopenic obesity. Metabolism 161, 156052 (2024).
Garvey, M. E. et al. Age, sex, and race/ethnicity associations between fat mass and lean mass with bone mineral density: NHANES data. Int. J. Environ. Res. Public. Health 18(23) (2021).
Khosla, S. et al. Relationship of serum sex steroid levels to longitudinal changes in bone density in young versus elderly men. J. Clin. Endocrinol. Metab. 86 (8), 3555–3561 (2001).
Casale, M. et al. Lean mass and body fat percentage are contradictory predictors of bone mineral density in pre-menopausal Pacific Island women. Nutrients 8(8) (2016).
Li, L. & Wang, Z. Ovarian aging and Osteoporosis. Adv. Exp. Med. Biol. 1086, 199–215 (2018).
Turner, C. H. et al. Mechanobiology of the skeleton. Sci. Signal. 2 (68), pt3 (2009).
Storlino, G. et al. Irisin protects against loss of trabecular bone mass and strength in adult ovariectomized mice by stimulating osteoblast activity. Int. J. Mol. Sci. 24(12). (2023).
Colaianni, G. et al. The myokine Irisin increases cortical bone mass. Proc. Natl. Acad. Sci. U S A. 112 (39), 12157–12162 (2015).
Mohiti-Ardekani, J. et al. Relationships between serum adipocyte hormones (adiponectin, leptin, resistin), bone mineral density and bone metabolic markers in osteoporosis patients. J. Bone Min. Metab. 32 (4), 400–404 (2014).
Barbour, K. E. et al. The effects of adiponectin and leptin on changes in bone mineral density. Osteoporos. Int. 23 (6), 1699–1710 (2012).
Soare, I. et al. Body composition as a modulator of bone health changes in patients with inflammatory bowel disease. Life (Basel) 12(2). (2022).
Jin, X. et al. Pathophysiology of obesity and its associated diseases. Acta Pharm. Sin B. 13 (6), 2403–2424 (2023).
Acknowledgements
The authors appreciate the time and effort given by participants during the data collection phase of the NHANES project.
Funding
This study was supported by Zhejiang Province Traditional Chinese Medicine Science and Technology Program Project (No. 2023ZL136).
Author information
Authors and Affiliations
Contributions
FJ, STG and XCY contributed to data collection, analysis and writing of the manuscript. ZXZ contributed to study design, analysis, writing and editing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The ethics review board of the National Center for Health Statistics approved all NHANES protocols and written informed consents were obtained from all participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jin, F., Gao, S., Yao, X. et al. Sex-specific associations between muscle-fat ratio and bone density in middle-aged adults. Sci Rep 15, 29105 (2025). https://doi.org/10.1038/s41598-025-15069-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-15069-7