Abstract
By exploring the factors that influence treatment failure in tuberculosis, the study aimed to provide references for the treatment and management of tuberculosis. The study data were derived from the National Tuberculosis Specialized Reporting System. Univariate analysis was used to test individual characteristic variables related to tuberculosis treatment failure. A three-level model was conducted to estimate the risk of tuberculosis treatment failure from both temporal and spatial levels, as well as from the individual level. Analysis revealed that demographic characteristics, such as older age (50 years and above) and male sex, were independent risk factors for tuberculosis treatment failure. Among diagnostic and treatment factors, the type of tuberculosis diagnosis contributed the most to treatment failure, followed by positive result for Mycobacterium tuberculosis detection, a history of previous drug therapy and treatment delays of more than one month. After excluding the effects of individual factors, there was also a spatiotemporal effect of treatment failure. Besides the effect of the individual factors, macro factors such as the socioeconomic development level and the quality of tuberculosis management might also play an important role in treatment failure. The study on the spatiotemporal effect provided a reference for objectively evaluating the quality of work in different regions.
Similar content being viewed by others
Introduction
Tuberculosis is caused by the bacillus Mycobacterium tuberculosis, which is spread when people who are sick with tuberculosis expel bacteria into the air (e.g. by coughing)1. The World Health Organization (WHO), in its Global Tuberculosis Report 2024, stated that in 2023, tuberculosis has probably returned to being the world’s leading cause of death from a single infectious agent (replacing COVID-19), and 8.2 million new cases of tuberculosis were diagnosed globally1. China, as the second-largest tuberculosis high-burden country globally, has consistently ranked second in the number of reported pulmonary tuberculosis cases among Class A and Class B notifiable infectious diseases (which are categorized based on their severity and transmission risk) in China., and the number of deaths ranked in the top three legally reported infectious diseases2.
Tuberculosis is a preventable and treatable infectious disease. According to the Global Tuberculosis Report 2024 of WHO, the treatment success rate for drug-sensitive tuberculosis patients worldwide was 88% in 2022, while the treatment success rate for multidrug-resistant tuberculosis (MDR-TB) and rifampicin-resistant tuberculosis (RR-TB) patients was 68%1. Treatment failure of tuberculosis leads to retreatment for patients. Previous studies have shown that the direct medical costs for retreatment patients are 2.24 times higher than those for initial treatment patients, the indirect costs are 3.10 times higher, and the socioeconomic burden is 2.78 times greater3,4. The heavy economic burden undoubtedly increases the incidence of poverty due to illness and the recurrence of poverty due to illness. Treatment failure of tuberculosis also causes the pathogen to persist in the patient’s body, increasing the risk of spreading it to others. Therefore, studying the risk factors for tuberculosis treatment failure is not only of positive significance for improving treatment success rates and effectively controlling the spread of tuberculosis, but also providing a basis for public health departments to allocate medical resources reasonably.
This study provided references for tuberculosis treatment and management from both spatiotemporal and individual perspectives.
Materials and methods
Ethics statement
The data for the study were obtained from the registration system of tuberculosis management. This was an observational study rather than an experimental study. There were no human subjects or human tissue samples involved, nor were there any experimental animals. Moreover, the data used in the study have been anonymized to remove any information that could identify the patients, such as names, identification numbers, medical record numbers, addresses, phone numbers, and dates of birth. The participants have provided informed consent. The study was approved by the Medical Ethics Committee of Hangzhou Center for Disease Control and Prevention (Hangzhou Health Supervision Institution)(2025-64). The study adhered to the Declaration of Helsinki.
Materials
This study collected relevant information from 38,385 tuberculosis cases under treatment management in Hangzhou from 2015 to 2021 registered in the National Tuberculosis Specialized Reporting System5. After excluding 22 cases diagnosed with non-tuberculosis mycobacterial infections and 5,097 cases lost to follow-up/death, a total of 33,266 study subjects were included. The vast majority of the cases were from 13 districts of Hangzhou (99.4%, 33,071/33,266, including Binjiang/BJ, Chunan/CA, Fuyang/FY, Gongshu/GS, Jiande/JD, Linan/LA, Linping/LP, Qiantang/QT, Shangcheng/SC, Tonglu/TL, Xihu/XH, Xiaoshan/XS, Yuhang/YH), only a few came from outside Hangzhou (0.6%, 195/33,266, including economically developed regions /ED, economically underdeveloped regions /EU). Due to some adjustments made to the tuberculosis reporting system between 2015 and 2021, certain registration items were newly added after these adjustments. As a result, data for these items were missing for the period before the adjustments. Therefore, items with data missing for more than 20% were not included in the analysis of the study.
Study design
All definitions involved in the study meet the requirements of “Technical specifications for Tuberculosis prevention and Control in China (2020 edition)”6. Multidrug-resistant tuberculosis (MDR-TB) refers to resistance to at least two first-line anti-tuberculosis drugs, including isoniazid and rifampicin. Rifampicin-resistant tuberculosis (RR-TB) refers to resistance to rifampicin, regardless of resistance to other anti-tuberculosis drugs. Criteria for judging the treatment outcome of tuberculosis patients based on sputum smear or culture examination: (1) Cured: Patients who are smear- or culture-positive complete the prescribed course of treatment. At the end of the last month of treatment, and in the most recent sputum smear or culture, the results are negative. (2) Completed Treatment: Patients who are smear- or culture-negative complete the prescribed course of treatment, with a negative sputum smear or culture result at the end of the treatment course, or no detection of the pathogen. Patients who are smear- or culture-positive complete the prescribed course of treatment, with no sputum examination results available at the end of the treatment course, but the most recent sputum smear or culture result is negative. (3) Treatment Failure: The sputum smear or culture result is positive at the end of the fifth month of treatment or at the end of the treatment course. (4) Death: Death due to any cause before or during the treatment course. (5) Lost to Follow-Up: Failure to start treatment or interruption of treatment for two months or more. (6) Other: Outcomes not falling into the above five categories. The standard also stipulates that both “cured” and “completed treatment” are classified as successful treatment outcomes; patients who discontinue treatment due to adverse reactions are classified as lost to follow-up. In the study, the treatment outcome was used as an effect indicator, with treatment failure defined as a positive event and treatment success as a negative event. The treatment failure rate (%) = number of treatment failure cases / total number of treated cases × 100%. The study proposed a hypothesis: If there were differences in tuberculosis treatment failure rates across different regions and times, were these differences due to variations in patient composition across regions and over time, or were they caused by other factors related to geography and time? We called the factors related to geography and time “macro factors,” which were in contrast to patients’ factors. Based on the hypothesis, first, we would analyze whether there were temporal trends and regional differences in treatment failure rates. Second, we would examine the impact of individual characteristics on treatment failure. Finally, we would conduct a comprehensive analysis to determine whether temporal and spatial effects still exist after controlling for the influence of these individual characteristics. This approach would provide a full description of the risk factors for tuberculosis treatment failure from both population and individual perspectives.
Statistical analyses
According to the study design, univariate analysis was used to test individual characteristic variables related to treatment failure. The tested factors included demographic characteristics and factors related to the diagnosis and treatment, i.e., age (< 25 years, 25–49 years, ≥ 50 years), sex (female, male), nationality (Han nationality, other), occupation (worker, farmer/migrant worker, clerks/service industry, healthcare worker/teacher/student, retired/unemployed), registered residence (local city, other city), source of cases (self-initiated consultation, active screening, recommended referral), HIV (negative, positive), time delayed in treatment(≤ 30 days, > 30 days), region of management (including 13 districts of Hangzhou and 2 regions outside Hangzhou), current management organization (hospital, CDC), etiology (negative, positive), comorbidities (none, pneumoconiosis, diabetes/chronic disease), registration classification (new case, initial treatment failure, relapse), use of Fixed-dose combination (FDC) (yes, no), and comorbidity with other tuberculosis (none, one type, two or more types). Diagnostic classification included hematogenous dissemination type, secondary type, and other types (such as primary pulmonary tuberculosis, tuberculous pleuritis, and extrapulmonary tuberculosis). The Cochran-Armitage Trend Test was used to analyze whether there was a temporal trend in the tuberculosis treatment failure rate. The Chi-square test was applied to examine whether there were differences in the treatment failure rate across different regions. These significant variables were then used as independent variables in a three-level logistic model, with region of case management as the three-level unit, treatment year as the two-level unit, and case as the one-level unit7. The three-level logistic model was different from the general logistic model. In the general logistic model, the total variation of the dependent variable was one-dimensional. However, in the three-level logistic model, the total variation of the dependent variable was three-dimensional, and these three dimensions had a hierarchical structure from high to low. The sources of the total variation in the three-level model were composed of three aspects: 1. The attribute variables of the management area; 2. The temporal characteristics of the treatment period; 3.The individual variables among patients. We used the MLwiN 2.02 statistical software for three-level statistical modeling. The model was constructed with a scale parameter of one, the connection function was logit, and the parameter estimation method chosen was the two-step Predictive Quasi-likelihood (PQL) algorithm. The selection of independent variables used the forward stepwise method, with a probability for stepwise entry of 0.05 and removal of 0.10. The basic structure of the model was as follows:
In the equation, i represented the patient (i.e., the one-level unit); j represented the treatment year (i.e., the two-level unit); k represented the region of patients management (i.e., the three-level unit); \(\:{{\upbeta\:}}_{0\text{jk}}\) was the intercept; \(\:{{\upbeta\:}}_{1}\) was the effect parameter of the independent variables, also known as the fixed effect parameter; \(\:\:{\text{v}}_{0\text{k}}\) was the residual for three-level unit, also known as the random effect at three-level, and its variance \(\:{{\upsigma\:}}_{{\text{v}}_{0}}^{2}\) was referred to as the random parameter, which reflected the differences in the ratios across regions (three-level unit); \(\:{\text{u}}_{0\text{jk}}\) was the residual for two-level unit, also known as the random effect at two-level, and its variance \(\:{{\upsigma\:}}_{{\text{u}}_{0}}^{2}\) reflected the differences in the ratios across years (two-level unit). A p value of < 0.05 indicated statistical significance at the 0.05.
Results
General characteristics of the study population
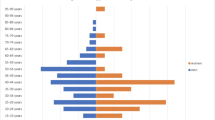
Among the 33,266 study subjects, the male-to-female ratio was 1.9:1 (21,917/11,349), with average age of 47.5 ± 20.5 years. The proportion of cases aged 50 years and above was 46.4% (15,430/33,266). The predominant occupation was farmers/migrant workers (47.2%, 15,252/32,337). Mycobacterium tuberculosis - positive cases constituted 40.3% (13,392/33,266). The proportion of primary pulmonary tuberculosis was very low, at only 0.03% (9/33,266). The majority of cases were newly diagnosed (92.0%, 30,621/33,266), while retreatment cases accounted for 8.0% (2,645/33,266).
Temporal trends and regional variations in treatment failure rates for tuberculosis
From 2015 to 2021, the average tuberculosis treatment failure rate in this region was 6.6% (2181/33266). The failure rate was the lowest in 2015 (5.8%, 316/5439) and the highest in 2018 (7.6%, 351/4599). Trend analysis showed that the tuberculosis treatment failure rate had an increasing trend from 2015 to 2021 (Z = 3.563, P = 0.0004) (Fig. 1a). There were differences in the treatment failure rates among different regions (χ2 = 364.872, P < 0.001). The highest rate was in JD (13.4%, 289/2,159), while the lowest rates were in BJ and QT (both 3.3%, 33/1,000, 69/2,086). The failure rate in the economically underdeveloped regions (EU) outside Hangzhou was significantly higher than that in the economically developed regions (ED) (8.6% vs. 3.6%, 5/58, 5/137) (Fig. 1b), suggesting that the tuberculosis treatment failure rate may be influenced by spatial and temporal factors. However, whether the spatial and temporal effects were due to differences in case composition across regions or macro factors (e.g., differences in socio-economic development and work quality) remained to be further explored through multivariable and multilevel analysis.
Univariate analysis of demographic characteristics and diagnostic and treatment factors
Univariate analysis (Table 1) identified the following demographic characteristics associated with treatment failure: age, gender, occupation, and registered residence. Patients over the age of 50 had a treatment failure risk 3.2 times higher than those under 25 (95% CI 2.7, 3.8). Men had a treatment failure risk twice as high as women (95% CI 1.8, 2.2). Among occupations, farmers/migrant workers had a higher risk of treatment failure, with a risk 1.8 times that of workers (95% CI 1.5, 2.1). Patients with registered residence on the other city had a lower risk of treatment failure compared to those with local city (0.7 times, 95% CI 0.6, 0.7).
In terms of diagnostic and treatment-related factors (Table 1), cases who undergo active screening had a lower risk of treatment failure compared to those who sought treatment independently (RR: 0.7, 95% CI 0.6, 0.9). Treatment delays of more than one month increased the risk of treatment failure by 40% (RR: 1.4, 95% CI 1.3, 1.5). Among the various types of tuberculosis, hematogenous disseminated tuberculosis had the highest risk of treatment failure, being 31.6 times higher than that of other types (including primary pulmonary tuberculosis, tuberculous pleuritis, and extrapulmonary tuberculosis) (95% CI 14.6, 68.4). Cases with positive etiology results had a treatment failure risk 12.7 times higher than those with negative results (95% CI 11.1, 14.5). Cases with either comorbid pneumoconiosis or diabetes/chronic illness had a corresponding increased risk of treatment failure (former RR: 2.8, 95% CI 1.1, 7.1; latter RR: 2.6, 95% CI 2.3, 2.9). Cases with treatment failure in their initial course of treatment had a 3.9 times higher risk of treatment failure compared to new cases (RR: 4.9, 95% CI 4.0, 6.1).
Three-level analysis of treatment failure
The three-level logistic null model was created with region of case management at the three-level unit, treatment year at the two-level unit, and cases at the one-level unit. The results showed that the random parameter for the three-level unit (region of case management) \(\:{\sigma\:}_{v}^{2}\) was 0.202 (three-level logistic null model: P = 0.018), and for the two-level unit (treatment year) \(\:{\sigma\:}_{u}^{2}\) was 0.064 (three-level logistic null model: P = 0.0004). This indicated that there was a spatial effect of the region of case management and a temporal effect of the treatment year in the treatment failure rate.
Based on the null model, variables with statistical significance from the univariate analysis were incorporated into the three-level logistic model for tuberculosis treatment failure rate (Table 2). The results showed that factors such as occupation, registered residence, source of cases, and comorbidities were not statistically significant (three-level logistic model: P > 0.05). As can be seen from the fixed parameter section of Table 2 (the upper part of Table 2), cases over 50 years old had a 1.4-fold higher risk of treatment failure compared with cases aged 25–49 years (95% CI 1.2, 1.5), and 1.6 times higher in men than in women (95% CI: 1.4, 1.8). Among the factors related to tuberculosis diagnosis and treatment, the tuberculosis diagnostic type had a greater impact on treatment failure, in which the risk of treatment failure was greatest for hematogenously disseminated tuberculosis, which was 14.3 times higher than that of other types( including primary pulmonary tuberculosis, tuberculous pleuritis, and extrapulmonary tuberculosis) (95% CI 5.1, 39.9), and secondary tuberculosis, which was 9.6 times higher than that of other types (95% CI 4.5, 20.8), followed by the risk of treatment failure for cases with Mycobacterium tuberculosis positive, which was 7.9 times (95% CI 6.8, 9.2) higher than that of negative cases. In addition, the case’s previous treatment history also had an impact on the current treatment failure, e.g., the risk of re-treatment failure in cases who failed the initial treatment was 2.6 times higher than that in new cases (95% CI 2.1, 3.4), and the risk of re-treatment failure in cases with relapse was 2.2 times higher than that in new cases (95% CI 1.9, 2.5). Treatment delay was another factor to consider, with studies showing that delays of more than one month were associated with a 20% (95% CI 1.0, 1.3) increased risk of treatment failure.
The random parameter section of Table 2 (at the bottom of Table 2) showed that the P-value for the random parameter \(\:{\sigma\:}_{v}^{2}\) of the three-level unit was 0.071 in the three-level logistic model, which was close to 0.05. Combined with Fig. 2a, it could be seen that the residual distributions of JD and LA were both above the zero scale line, indicating that the difference in failure rates between these two regions was statistically significant. Meanwhile, the P-value for the random parameter \(\:{\sigma\:}_{u}^{2}\) of the two-level unit was 0.011 in the three-level logistic model, which indicated that there was a temporal effect on the treatment failure rate. Therefore, based on the fixed and random parameters in Table 2, it could be concluded that, after controlling for the aforementioned individual characteristic factors: (1) There were differences in the treatment failure rate among management regions, with JD having the highest treatment failure rate (a higher rank indicates a higher treatment failure rate), followed by LA (Fig. 2a); (2) The treatment failure rate within the same region of case management varied across different years (Fig. 2b). From the cumulative rank figure of tuberculosis treatment failure rates (Fig. 2c), it could be observed that JD consistently had a higher treatment failure rate, while SC showed an abnormal increase in treatment failure rates in 2020 and 2021.
By comparing the regional ranks in Figs. 1b and 2a, which showed the situation before and after controlling for individual characteristics, it was evident that JD maintained the highest rank both before and after control. In contrast, CA’s rank changed significantly, falling from fifth before control to fourteenth after control.
High level effect estimation of tuberculosis treatment failure rate. a Residual of tuberculosis treatment failure rate and its 95% CI ranking in different areas of case management, b the residual of tuberculosis treatment failure rate and its 95% CI ranking in different years’ areas of case management, c cumulative rank of tuberculosis treatment failure rate in different years in different areas of case management.
Discussion
The study showed that in a city in Eastern China, the tuberculosis treatment failure rate had shown an increasing trend since 2015, with variations in treatment failure rates across different regions. Among the demographic characteristics, age (50 years and older) and male sex were independent risk factors for tuberculosis treatment failure, which may be related to the decline in physiological functions of organs, decreased immune function, poor tolerance of drugs in the elderly cases8, and the lower treatment adherence in males compared to females9. Among the factors related to the diagnosis and treatment of tuberculosis, the classification of tuberculosis diagnosis had the greatest impact on treatment failure. Hematogenous disseminated pulmonary tuberculosis had the highest risk of treatment failure, followed by secondary pulmonary tuberculosis. The classification of tuberculosis diagnosis reflects the clinical characteristics of different types of tuberculosis. Primary pulmonary tuberculosis usually presents with mild clinical symptoms, and most patients have a self-limiting course. This may also be one of reasons for the relatively low number of primary pulmonary tuberculosis cases in the study. In contrast, most cases of hematogenous disseminated pulmonary tuberculosis are acute in onset, with severe acute intoxication symptoms clinically. Secondary pulmonary tuberculosis is the most common type of pulmonary tuberculosis in adults, and its clinical manifestations vary widely10. One of the important factors affecting the success or failure of treatment was the microbiological result, which was consistent with the findings of other similar studies11. A positive microbiological result indicates that the Mycobacterium tuberculosis is actively multiplying in the case’s body, suggesting that the infection is in an active phase and indirectly reflecting a weakened immune response. Initial treatment failure could indicate the presence of factors that reduce sensitivity to chemical drugs, and during re-treatment, the limited choice of drugs increases the risk of treatment failure. As for relapsed cases, although initial treatment is successful, it does not mean that the Mycobacterium tuberculosis is completely eradicated, it is likely that the bacteria merely entered a dormant state under the pressure of drugs and the immune system, when the immune system is weakened, the bacteria can become active again, so previous history of chemical drug treatment increases the risk of drug resistance during relapse. Studies have already confirmed that bacterial resistance is a significant factor contributing to treatment failure12,13. Treatment delays not only increase the risk of transmission, but also exacerbate the proliferation of Mycobacterium tuberculosis and cause more extensive and deeper damage to the body14, which highlights the necessity of early treatment.
It was worth mentioning that, based on controlling for the individual characteristic factors affecting tuberculosis treatment failure, the study also revealed the existence of spatiotemporal effect in treatment failure. Specifically, the macro factors of the case management region influenced treatment failure, and this impact varied with time. The existence of this spatiotemporal effect had been confirmed by the high-level random effects in the three-level model (Fig. 2). We speculated that the possible reasons were: 1.The level of socioeconomic development in the current administrative region. The connection had already been confirmed in previous studies15,16. In terms of regional ranking, regions with lower socioeconomic development levels tended to have higher tuberculosis failure rates, such as JD vs. BJ and EU vs. ED, which were examples of this trend. 2. The quality of management in the current administrative regions, such as the quality of tuberculosis diagnosis and treatment, case management and supervision, and laboratory testing technology. For over two decades, tuberculosis prevention and control strategy in China has employed a three-tier management pattern involving disease prevention and control institutions (CDCs), hospitals (designated tuberculosis hospitals and non-designated hospitals), and primary healthcare institutions. The CDCs are responsible for tuberculosis prevention and control within their jurisdictions, providing technical guidance, management, and assessment to hospitals and primary healthcare institutions. tuberculosis designated hospitals are in charge of diagnosing and treating patients, while non-designated hospitals are responsible for referring patients. Primary healthcare institutions are tasked with regularly following up on patient treatment (every ten days during the intensive phase and monthly during the consolidation phase), encouraging and guiding patients to adhere to standardized treatment. It was reasonable to speculate that the quality of management in the current administrative regions may have a certain degree of common impact on local patient treatment. The comparison between JD and CA counties in the study provided a clue: JD and CA are two adjacent counties with relatively underdeveloped economies. Both are high-incidence areas for tuberculosis in Hangzhou, and both have a higher proportion of elderly patients than the average level of 46.4% (JD: 73.1%, CA: 76.4%). However, the two counties showed completely different rank changes before and after controlling for individual factors. This indicated that the reasons for the high treatment failure rates in the two counties were entirely different. Specifically, the high failure rate in CA was largely due to the individual characteristics of the patients (such as the majority being elderly patients), while in JD, macro factors could play a more significant role. It could be inferred that this macro factor, in addition to the relatively low level of economic development, was another factor that had a substantial impact on the treatment outcomes of tuberculosis, such as poor tuberculosis management quality. It can be seen that the spatiotemporal effects of treatment failure rates help administrative departments to exclude the interference caused by patient factors when evaluating the quality of work in different regions, making the evaluation results more objective and fair. At the same time, it also provides a scientific basis for the management department to identify areas that need to be prioritized for improvement in the future. Based on the results of the study, JD should be listed as a key county for improving the quality of tuberculosis management in Hangzhou. As for the abnormal increase in the treatment failure rate in SC in 2020 and 2021, it might have been affected by the COVID-19 pandemic, as in many other countries and regions17,18.
The limitations of the study lie in the insufficient collection of work indicators from the current management areas, which prevents an in-depth analysis of the specific causes of the spatiotemporal effects. Additionally, since this is an observational study rather than an experimental one, the completeness of data collection is limited by objective conditions. Of course, the advantage of the study is that it confirms the existence of spatiotemporal effects beyond the role of individual characteristics, which may provide a basis for the quality evaluation of tuberculosis management departments.
Conclusion
Old age (50 years and above) and male sex were independent risk factors for tuberculosis treatment failure. The classification of tuberculosis diagnosis had the greatest impact on treatment failure, followed by Mycobacterium tuberculosis positivity, history of previous drug treatment, and treatment delay of more than one month, all of which also affected tuberculosis treatment failure. In addition, the macro factors such as the socioeconomic development level and the quality of tuberculosis management might also play an important role in treatment failure.
Data availability
All relevant data was contained within the manuscript, further inquiries could be directed to the corresponding author.
References
WHO. Global Tuberculosis Report 2024(World Health Organization) 1–2 (Geneva, 2024).
National Center for Disease Control and Prevention. Overview of the National epidemic situation of notifiable infectious diseases in 2023. Chin. J. Viral Dis. 14, 600 (2024).
He, T. N. The analysis and comparison of family and social economic burden of initial treat and retreat tuberculosis case. Mod. Prev. Med. 33, 2134–2135 (2006).
Chen, L. X. & Wu, Y. L. Investigation on economic burden of tuberculosis patients in sanmenxia City. Prev. Med. Trib. 13, 869–871 (2007).
Chinese, C. D. C. China information system for disease control and prevention. 10.249.6.18:8881/cdc (2004).
Chinese, C. D. C. Chinese Technical Code of Practice for Prevention and Control of Tuberculosis (Edition) 27(2020). (2020).
Yang, M. & Li, X. S. Common Multilevel Statistical Models in Medical and Public Health Research (1st edition) 6–25 (Peking University Medical Press, 2007).
Wen, Y. & Zhou, L. F. Analysis on the factors of the treatment failure of smear-positive pulmonary tuberculosis patients after the implementation of DOTS program in Beihai City. J. Clin. Pulm. Sci. 15, 1452–1453 (2010).
Du, Y. H., Lu, C. Y. & Chen, Q. C. Analysis on the factors that influence the treatment failure and death of smear-positive pulmonary tuberculosis patients in Guangzhou City. J. Chin. Defense Consum. 29, 226–229 (2007).
Li, L. J. & Ren, H. Infectious Diseases (8th edition) 212 (Beijing: People’s Medical Publishing House, 2015).
Sindhu, S., Mandeep, W. & Rakesh, L. K. Factors associated with treatment failure in childhood tuberculosis. Indlan Pediatrics. 45, 769–771 (2008).
Du, J. et al. Factors influencing the failure of initial and furthertreatment of pulmonary tuberculosis in patients treated with standard short-course chemotherapy. J. Pathogen Biol.. 7, 523–526 (2012).
Sun, X. X. et al. Analysis of the causes of tuberculosis treatment failure caused by non-compliance behavior. Chin. J. Nurs. 35, 478–480 (2000).
Almeida, S. J., Soares, P., Leite, A., Duarte, R. & Nunes, C. Patient and healthcare delays in critical and non-critical pulmonary tuberculosis incidence areas in portugal: are there differences? Public Health. 201, 41–47 (2021).
Guy, H., Marcia, C. & Castro A. Spatial analysis of social and economic determinants of tuberculosis in Brazil. Health Place 25, 56–67 (2014).
David, R. et al. Identification of spatial and cohort clustering of tuberculosis using surveillance data from British columbia, canada, 1990–2013. Soc. Sci. Med. 168, 214–222 (2016).
Bentum-Micah, G., Lianyu, C. & Ahoto, A. T. Observation of covid-19 safety protocols by persons with chronic health conditions in ghana: the influence of health belief model. Acta Psychol. (Amst). 236, 103928 (2023).
Hanson, C. L. et al. Protection motivation during COVID-19: a cross-sectional study of family health, media, and economic influences. Health Educ. Behav. 48, 434–445 (2021).
Funding
This study was funded by the Public Welfare Technology Research Program in Zhejiang Province (No. LGF21H190002), Zhejiang General Research Project on Medical Health and Science Technology Plan (No.2020KY238 and No.2021KY951).
Author information
Authors and Affiliations
Contributions
C.P. Huang &L. Zhang contributed to the study conception and design. Material preparation, data collection and analysis were performed by Q.L. Chen, Q.C. Li, M. Lu, Y.F. Wu. The first draft of the manuscript was written by C.P. Huang and L. Zhang. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, C., Wu, Y., Cheng, Q. et al. A multilevel analysis on spatiotemporal and individual-level determinants of tuberculosis treatment failure in China. Sci Rep 15, 30140 (2025). https://doi.org/10.1038/s41598-025-15797-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-15797-w