Abstract
Carpal tunnel syndrome (CTS) presents with pain, numbness, and occasional weak hand grip. Diagnosis is predominantly clinical, with initial management involving conservative measures; surgery is considered for non-responsive cases. The Boston Carpal Tunnel Questionnaire (BCTQ), an efficient patient-reported outcome measure, is increasingly utilized for objective treatment assessment. Our study aimed to apply the BCTQ in patients who underwent carpal tunnel release surgery, contributing to the growing use of this effective assessment tool, and utilizing it in assessing patient-reported outcomes after carpal tunnel release surgery in Jordanian population. A retrospective cohort study design was utilized, enrolling 681 patients who underwent carpal tunnel release surgery. Inclusion criteria encompassed patients undergoing open primary carpal tunnel release surgery within a 5-year period (2018–2022), excluding cases of revision surgery, endoscopic surgery, surgery site trauma or fracture, peripheral neuropathies, and those with lost follow-up. In our study (n = 681), patients had a mean age of 52.0 years. Females comprised 77.2%. Diabetes and hypertension were prevalent, with 67.8% and 38.5% of patients, respectively. The mean self-reported functional disability score was 7.2. On BCTQ analysis, females exhibited a significantly higher mean S score compared to males (3.27 vs. 2.9, p = 0.002). We found significantly higher S score differences in patients reporting pain (-1.78 vs. -1.02, p < 0.001), paresthesia (-1.77 vs. -0.77, p < 0.001), nocturnal symptoms (-1.83 vs. -1.05, p < 0.001. Similarly, F score differences were statistically significant for pain (-1.32 vs. -0.080, p < 0.001), and nocturnal symptoms (-1.33 vs. -0.97, p = 0.003). In our cohort, females showed greater symptomatic and functional improvements than males. Smoking and comorbidities had no clear impact on BCTQ scores. Patients with night symptoms, paresthesia, disabling pain, and subjective weak grip displayed significant BCTQ score improvements.
Similar content being viewed by others
Introduction
Carpal Tunnel Syndrome (CTS) manifests as a clinical syndrome resulting from the compression of the median nerve within the carpal tunnel of the wrist1,2. It is characterized by pain and paresthesia affecting the three and a half radial digits3,4. Primary interventions for CTS encompass the administration of analgesics, utilization of night splints, and the application of steroid injections. Surgical release of the carpal tunnel is considered in cases where patients do not exhibit improvement with conservative management strategies5,6,7.
Patients diagnosed with carpal tunnel syndrome may manifest a spectrum of symptomatology, spanning from mild hand pain and paresthesia to severe, incapacitating symptoms, particularly during nocturnal periods8,9. This array of symptoms has the potential to significantly impact the patient’s capacity to execute routine activities of daily living10,11,12. Consequently, individuals seek medical intervention to mitigate the disabling manifestations associated with this condition13,14.
The assessment of treatment effectiveness in carpal tunnel syndrome increasingly relies on patient-reported outcomes (PROs)15. Functional disability levels in individuals with this condition are gauged using scoring systems, facilitating the objective translation of perceived symptom severity into clinically reliable measures16. One noteworthy scoring system is the Boston Carpal Tunnel Questionnaire (BCTQ)17, introduced in 1993, serving as a pivotal clinical instrument for quantifying symptom severity on a standardized scale. This questionnaire proves valuable for precisely evaluating the impact of carpal tunnel syndrome on patients’ functional well-being18,19,20,21,22,23.
The Boston Carpal Tunnel Questionnaire (BCTQ) is widely acknowledged as a reliable clinical tool for evaluating patient-reported outcomes in individuals undergoing carpal tunnel release surgery. Its efficacy stems from its comprehensive nature, covering various aspects related to both the severity of the disease and its functional implications on patients24,25. Notably, previous research has not explored the use of the BCTQ in assessing carpal tunnel surgery outcomes in Middle Eastern countries, making this study particularly valuable in shedding light on the outcomes of a common surgical procedure within this population context.
The primary objective of this research is to evaluate patient-reported outcome measures using the BCTQ in individuals who have undergone open carpal tunnel release surgery. Through examining the differences between preoperative and postoperative scores, our objective is to reveal associations that contribute to both favorable and unfavorable surgical outcomes, thereby offering deeper insights into the determinants of surgical success.
Patients and methods
Study design and research objectives
In this study, we utilized a retrospective cohort study design to examine the outcomes of carpal tunnel release surgery, focusing on the perspectives and patient-reported experiences.
Our primary objective was to investigate these outcomes using the Boston Carpal Tunnel Questionnaire (BCTQ). Specifically, we aimed to measure the BCTQ scores before and after surgery, as well as determine the difference between the pre and postoperative scores.
Additionally, we sought to explore secondary outcomes, including the patients’ health profiles, medical comorbidities, disease presentations, and treatment modalities used. We then aimed to analyze these factors alongside the BCTQ score differences to identify any potential associations.
Participants and setting of the study
In this study, we examined a total of 681 patients who underwent carpal tunnel release surgery at two leading hospitals in Jordan over a period of five years, from January 2018 to December 2022. These patients were diagnosed with carpal tunnel syndrome through clinical examination, and confirmation of the diagnosis was achieved using electrodiagnostic studies.
Inclusion and exclusion criteria
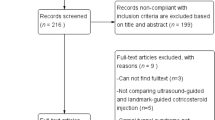
The inclusion criteria for this study consisted of patients who underwent isolated open carpal tunnel release surgery between January 2018 and December 2022. However, patients who underwent combined procedures during the carpal tunnel release surgery, had endoscopic surgery, or underwent revision surgery were excluded from the study. Additionally, patients who refused to participate, had incomplete health records, had previous surgery on the operated hand, had previous hand trauma or fractures on the operated hand, or had systemic or peripheral neuropathies were also excluded from the study.
Study sample and sample size
A convenience sampling method was employed for patient recruitment in this study. The selected sample size of 681 patients was deemed sufficient for the purpose and objectives of our research and was determined based on several considerations. Firstly, a review of prior studies on this topic indicated that the majority of them utilized sample sizes that were comparable to, or smaller than, ours, thereby suggesting the adequacy of our chosen sample size. Moreover, the selection of 681 patients was also influenced by practical considerations, particularly the operational capacity and resources available within the two hospitals included in our study. By aligning our sample size with the feasibility and logistical capabilities of the study sites, we ensured the smooth and efficient conduct of data collection within the designated timeframe.
Outcome variable definitions
In this study, the primary outcome variable of interest was the Boston Carpal Tunnel Questionnaire (BCTQ). Levine et al. introduced the BCTQ in 199317, which includes two distinct sections.
The first section, known as the Symptom Severity Scale, is composed of 11 questions aimed at evaluating the severity of symptoms associated with carpal tunnel syndrome. Each question is scored on a scale of 1 to 5, where a lower score indicates a more favorable condition (1 indicates the least severe symptoms and 5 indicates the most severe).
The second section, the Functional Status Scale, assesses the patient’s functional status through 8 items, each scored similarly on a scale of 1 to 5. Here, a lower score again denotes a better condition (with 1 being the least impairment and 5 being the most impairment).
After completing the BCTQ, the average scores for both symptom severity and functional status scales were calculated. Our study included evaluating pre- and post-surgery BCTQ scores and determining the score differences, thus offering a comprehensive assessment of each patient’s condition.
Study protocol
We included patients diagnosed with carpal tunnel syndrome through clinical evaluation and confirmed with electrodiagnostic studies who underwent carpal tunnel release surgery between January 2018 and December 2022. Following the application of specific inclusion and exclusion criteria, 681 patients were deemed eligible for analysis. The surgical procedures were conducted by skilled orthopedic surgeons using a standardized technique at day-case surgery centers within two hospitals. All patients underwent assessment using the Boston Carpal Tunnel Questionnaire (BCTQ) within one week before surgery, and BCTQ was subsequently re-assessed postoperatively during clinic follow-up visits, interviews, and phone calls with patients.
Ethical consideration
This study received approval from the Institutional Review Board (IRB) at Jordan University’s Medical Research Office, with IRB number 2023/25,128. Prior to enrollment, all participants provided informed consent, and strict measures were implemented to safeguard patient confidentiality and privacy throughout the study. The research adhered to the Code of Ethics outlined by the World Medical Association (Declaration of Helsinki).
Data collection and analysis
The data collected in this study is organized into three main categories. Firstly, it includes an examination of patients’ health profiles and medical comorbidities, encompassing variables such as age, gender, smoking habits, and the presence of comorbidities. Secondly, the dataset contains information related to patients’ symptomatology, including aspects such as pain, paresthesia, and nocturnal symptoms. Lastly, the study incorporates patient-reported outcome variables, specifically the Boston Carpal Tunnel Questionnaire (BCTQ).
Data were collected and analyzed using the Statistical Package for Social Science (SPSS), version 23. The data collection process involved postoperative follow-up visits, phone calls, and authorized access to patients’ health records. Descriptive statistics were utilized to summarize patient characteristics and patient-reported outcomes (PROs), with a statistical significance level set at p < 0.05 to determine significant findings.
Quantitative variables such as age, weight, height, and BMI were analyzed using descriptive statistics, with means and standard deviations calculated. The relationship between mean differences in pre- and postoperative BCTQ scores was assessed using Student’s t-test.
Figure 1 illustrates the Boston Carpal Tunnel Questionnaire, and Fig. 2 presents a concise flowchart summarizing our study methodology.
Results
Our cohort comprised a total of 681 patients who underwent open carpal tunnel release surgery. The average age was 52.0 years, with a mean body mass index of 31.4 kg/m2. The average duration of symptoms was 1.5 years (19 months). In terms of gender distribution, over two-thirds of the cohort were females (526 patients, 77.2%). Of the surgeries performed, 421 (61.8%) were for the right hand, and 260 (28.2%) were for the left hand. The majority of the cohort (82.1%) were non-smokers. In terms of comorbidities, 219 patients (67.8%) had diabetes, 262 (38.5%) had hypertension, 93 (13.7%) had cardiovascular disease, and 65 (9.5%) had cerebrovascular disease. (Table 1).
Examination of patients’ clinical presentations revealed that 590 individuals (86.6%) reported complaints predominantly centered around pain, 645 patients (96.0%) experienced paresthesia, 591 patients (86.6%) reported disabling nocturnal symptoms, and 532 patients (78.1%) reported weakened grip strength. Regarding received treatments within our cohort, 99 patients (14.5%) received steroid injections, 238 patients (34.9%) utilized night splints, and 167 patients (24.5%) were administered gabapentin. The mean pre-operative self-reported functional disability, measured on a Likert scale of 10, was 7.2, and the average time taken to achieve full recovery was 1.7 months. (Table 2).
Analysis of patient variables in relation to the Boston Carpal Tunnel Questionnaire (BCTQ) yielded insights into certain individuals exhibiting elevated levels of symptom severity and functional disability. The BCTQ comprises two distinct components, namely the symptom severity scale (referred to as the S score) and the functional status scale (referred to as the F score). The S score encompasses 11 items, while the F score consists of 8 elements. Each item in both scales is graded on a scale of 1 to 5, with higher values indicating a more severe status.
To evaluate the impact of the surgical intervention, we computed the differences between the preoperative and postoperative S scores and F scores, denoted as S score differences and F score differences, respectively. Negative scores indicate improvement, as postoperative scores were lower than preoperative scores. Moreover, the magnitude of the difference reflects the extent of improvement.
To further investigate the relationship between these score changes and patient variables, statistical analysis utilizing student t-test was employed. This allowed for comparisons of how different patient characteristics were associated with changes in the S scores and F scores. Notably, a greater difference in scores indicates a more significant improvement in symptoms and functional status following the intervention.
In our patient cohort, females exhibited a higher mean S score compared to males (3.27 vs. 2.9, p = 0.002), while both genders demonstrated nearly equal levels of functional disability (1.46 vs. 1.44 for males, p < 0.001). The S score differences were assessed for patients based on specific characteristics: smokers (-1.63 vs. -1.43 for non-smokers, p = 0.28), individuals with diabetes (-1.68 vs. -1.75 for non-diabetics, p = 0.39), those with hypertension (-1.74 vs. -1.72 for non-hypertensive, p = 0.75), cardiovascular diseases (-1.85 vs. -1.71, p = 0.81), cerebrovascular disease (-1.72 vs. patients without cerebrovascular disease − 1.72, p = 0.81), and patients with renal disease (-1.64 vs. non-renal disease − 1.74, p = 0.22). (Table 3)
Differences in the F score was more pronounced in females compared to males (-1.3 vs. -1.0, p < 0.001). When considering smoking status, non-smokers exhibited slightly higher F score differences than smokers (-1.30 vs. -1.20, p = 0.33). Patients with diabetes, hypertension, cardiovascular, cerebrovascular, and renal diseases displayed comparable F score differences, with p-values of 0.86, 0.75, 0.59, 0.75, and 0.15, respectively. (Table 3)
Moreover, in analyzing patient symptomatology, we found significantly higher S score differences in those reporting predominant pain symptoms (-1.78 vs. -1.02, p < 0.001), paresthesia (-1.77 vs. -0.77, p < 0.001), nocturnal symptoms (-1.83 vs. -1.05, p < 0.001), and weak grip (-1.85 vs. -1.28, p < 0.001). Similarly, F score differences were statistically significant for pain (-1.32 vs. -0.080, p < 0.001), paresthesia (-1.31 vs. -0.77, p = 0.013), nocturnal symptoms (-1.33 vs. -0.97, p = 0.003), and weak grip (-1.46 vs. -0.66, p < 0.001). (Table 3).
Discussion
In the context of this investigation involving patients with carpal tunnel syndrome, females exhibited a higher likelihood of experiencing severe symptoms compared to their male counterparts, while demonstrating comparable levels of functional disability. Notably, medical comorbidities did not appear to influence either symptoms severity or functional status in these patients. Furthermore, individuals presenting with pain as a predominant feature, substantial paresthesia, nocturnal symptoms, and those with subjective weak grip strength exhibited a higher likelihood of experiencing notable improvement in both symptoms and functional status following surgical intervention.
Carpal tunnel syndrome (CTS), a clinical syndrome typically observed in late adulthood, exhibits a higher prevalence in females, particularly those aged over 55, as reported by Lam et al.28. Other identified risk factors include obesity, elevated BMI, and increasing age, as highlighted by Becker et al.29. Notably, Karpitskaya et al. observed a lower prevalence of smoking among CTS patients compared to the general population30. Our study, encompassing a cohort with a mean patient age of 52 years, a mean BMI of 31.4 kg/cm2, and a composition of more than two-thirds females and non-smokers, aligns consistently with these established patterns in the existing literature.
Carpal tunnel syndrome (CTS) is frequently associated with comorbidities such as diabetes mellitus (DM), hypertension (HTN), and obesity, potentially influencing its severity, as reported by Nazish et al.31. Pourmemari et al. further highlighted that diabetic patients are more prone to developing carpal tunnel syndrome32. Tharwat et al. reported an elevated risk of carpal tunnel development in individuals with renal impairments undergoing hemodialysis, attributed to a reduced carpal tunnel cross-sectional area33. Consistent with these observations, our study reveals a similar prevalence of comorbidities, with diabetes, hypertension, and cardiovascular disease being among the most prevalent conditions.
Previous studies have addressed the mediating influence of medical comorbidities on symptoms severity and functional impairment in individuals with carpal tunnel syndrome. Yucel et al. linked symptoms severity in carpal tunnel syndrome patients to diabetes, night symptoms, and chronic fatigue syndrome34. Similarly, Sharief et al. highlighted associations between symptoms severity and comorbid conditions such as diabetes, hypertension, and thyroid disorders35. You et al. stratified symptoms severity based on preoperative electrophysiologic studies36. Additionally, Newington et al. correlated the severity of patients’ symptoms with the presence of night symptoms and discomforting paresthesia37. In our study, the presence of diabetes, hypertension, cardiovascular, and renal disease exhibited a slight increase in symptoms severity scores and functional impairment.
Numerous studies have explored factors predicting favorable outcomes following carpal tunnel release surgery. Fakhouri et al. found younger age and absence of hand grip weakness to be associated with improved outcomes38, while Gong et al. and Wintman et al. identified greater improvement in patients with nocturnal pain and no hand grip weakness39,40. Calderón et al. emphasized depression’s significance in predicting patient satisfaction post-surgery41. Conversely, Sonohata et al. reported younger age, milder pain, and absence of nocturnal pain as negative prognostic factors42. Our study supports the significance of night symptoms and paresthesia as a good indicator for postoperative improvement.
While acknowledging certain limitations in our study, we maintain that they do not compromise the validity of our findings. The retrospective design introduces potential limitations in data collection and analysis but proves valuable for exploring associations and generating hypotheses. Our study concentrated on prevalent comorbidities such as diabetes, hypertension, and renal disease, excluding factors like psychiatric illness and socioeconomic status due to their lower endemicity and representation in our patient sample. Despite these constraints, our research offers valuable insights and establishes a basis for future investigations in this domain.
Conclusion
In our patient cohort, females and non-smokers constituted the majority, with diabetes and hypertension emerging as the most prevalent medical comorbidities. Females exhibited a higher likelihood of experiencing both symptomatic and functional status improvements compared to males. Smoking and medical comorbidities did not exert discernible effects on patients’ pre- and postoperative Boston Carpal Tunnel Questionnaire (BCTQ) scores. Notably, patients presenting with night symptoms, paresthesia, disabling pain, and weak grip demonstrated statistically significant improvement in BCTQ scores.
Clinical implication
Based on the study’s findings, the authors wish to emphasize the following clinical implications and physician recommendations.
-
1.
Functional Disability Assessment:
The mean self-reported functional disability of 7.2 on a Likert scale of 10 signifies a significant impact of carpal tunnel syndrome on patients’ functional well-being. The average time taken to achieve full recovery at 1.7 months provides clinicians with a timeframe expectation for postoperative recovery, aiding in patient counseling and expectation management.
-
2.
Gender Disparities and Comorbidity Management:
Given the gender disparities observed, with females exhibiting higher symptom severity, clinicians should tailor interventions considering potential gender-specific factors. Additionally, the study highlights the influence of comorbidities such as diabetes, hypertension, cardiovascular, and renal disease on symptoms severity and functional impairment. An integrated approach considering both specific symptoms and comorbidities is essential for comprehensive patient care.
-
3.
Symptomatology and Surgical Outcomes:
Patients presenting with specific symptomatology, including pain, paresthesia, nocturnal symptoms, and weak grip, demonstrated statistically significant improvements in BCTQ scores postoperatively. This highlights the potential prognostic value of symptomatology in predicting surgical outcomes.
-
4.
Boston Carpal Tunnel Questionnaire (BCTQ) as a Clinical Tool:
The Boston Carpal Tunnel Questionnaire (BCTQ) emerges as a crucial clinical tool for objectively assessing symptom severity and functional impairment. Incorporating BCTQ scores into routine assessments provides clinicians with valuable insights into the impact of carpal tunnel syndrome on patients’ lives, aiding in treatment planning and outcome evaluation.
Data availability
The data that support the findings of this study are available upon appropriate request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Abbreviations
- CTS:
-
Carpal tunnel Syndrome
- BCTQ:
-
Boston carpal tunnel questionnaire
References
Sevy, J. O., Varacallo, M. & Syndrome, C. T. Accessed: Sep. 02, 2023. [Online]. (2022). Available: https://www.ncbi.nlm.nih.gov/books/NBK448179/
Genova, A., Dix, O., Saefan, A., Thakur, M. & Hassan, A. Carpal tunnel syndrome: A review of literature. Cureus 12 (3), 316–320. https://doi.org/10.7759/CUREUS.7333 (2020).
Orhurhu, V. et al. Carpal tunnel release Surgery- A systematic review of open and endoscopic approaches. Anesthesiol Pain Med. 10, 1–12. https://doi.org/10.5812/AAPM.112291 (2020).
El Miedany, Y., Ashour, S., Youssef, S., Mehanna, A. & Meky, F. A. Clinical diagnosis of carpal tunnel syndrome: old tests-new concepts. Jt. Bone Spine. 75 (4), 451–457. https://doi.org/10.1016/J.JBSPIN.2007.09.014 (2008).
Chammas, M. Carpal tunnel syndrome. Chir. Main. 33 (2), 75–94. https://doi.org/10.1016/J.MAIN.2013.11.010 (2014).
Keith, M. W. et al. Treatment of carpal tunnel syndrome. J. Am. Acad. Orthop. Surg. 17 (6), 397–405. https://doi.org/10.5435/00124635-200906000-00008 (2009).
Duncan, S. F. M., Bhate, O. & Mustaly, H. Pathophysiology of carpal tunnel syndrome. Neurosciences 20 (1, p. 4, ). https://doi.org/10.1007/978-3-319-57010-5_3 (2015).
Assmus, H., Antoniadis, G. & Bischoff, C. Carpal and cubital tunnel and other, rarer nerve compression syndromes. Dtsch. Arztebl Int. 112 (14), 1–2. https://doi.org/10.3238/ARZTEBL.2015.0014 (2015).
Ahn, D. S. Hand elevation: A new test for carpal tunnel syndrome. Ann. Plast. Surg. 46 (2), 120–124. https://doi.org/10.1097/00000637-200102000-00005 (2001).
Patel, A. et al. The negative effect of carpal tunnel syndrome on sleep quality. Sleep. Disord. 2014, 1–7. https://doi.org/10.1155/2014/962746 (2014).
Patel, J. N., McCabe, S. J. & Myers, J. Characteristics of sleep disturbance in patients with carpal tunnel syndrome. Hand (N Y). 7 (1), 55. https://doi.org/10.1007/S11552-011-9373-1 (2012).
Ma, H. & Kim, I. The diagnostic assessment of hand elevation test in carpal tunnel syndrome. J. Korean Neurosurg. Soc. 52 (5), 472–475. https://doi.org/10.3340/jkns.2012.52.5.472 (2012).
Steinberg, D. R. Surgical release of the carpal tunnel. Hand Clin. 18 (2), 291–298. https://doi.org/10.1016/S0749-0712(01)00011-7 (2002).
Sanati, K. A. et al. Surgical techniques and return to work following carpal tunnel release: a systematic review and meta-analysis. J. Occup. Rehabil. 21 (4), 474–481. https://doi.org/10.1007/S10926-011-9310-8 (2011).
Mertz, K., Lindsay, S. E., Morris, A. & Kamal, R. N. Outcome metrics in the treatment of carpal tunnel syndrome: A systematic review. Hand (N Y). 17 (4), 659. https://doi.org/10.1177/1558944720949951 (2022).
Liao, C. D., Abdou, S. A., Daar, D. A., Lee, Z. H. & Thanik, V. Patient-Centred outcomes following open carpal tunnel release: A systematic review of the current literature. J. Hand Surg. Asian-Pacific Vol. 27 (3), 430–438. https://doi.org/10.1142/S2424835522500424 (2022).
Levine, D. W. et al. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J. Bone Joint Surg. Am. 75 (11), 1585–1592. https://doi.org/10.2106/00004623-199311000-00002 (1993).
Atroshi, I., Johnsson, R. & Sprinchorn, A. Self-administered outcome instrument in carpal tunnel syndrome: reliability, validity and responsiveness evaluated in 102 patients. Acta Orthop. Scand. 69 (1), 82–88. https://doi.org/10.3109/17453679809002363 (1998).
Sezgin, M. et al. Assessment of symptom severity and functional status in patients with carpal tunnel syndrome: reliability and validity of the Turkish version of the Boston questionnaire. Disabil. Rehabil. 28 (20), 1281–1286. https://doi.org/10.1080/09638280600621469 (2006).
Mody, G. N. et al. Carpal tunnel syndrome in Indian patients: use of modified questionnaires for assessment. J. Hand Surg. Eur. Vol. 34 (5), 671–678. https://doi.org/10.1177/1753193409101469/ASSET/IMAGES/LARGE/10.1177_1753193409101469-FIG3.JPEG (2009).
Park, D. J. et al. Cross-Cultural adaptation of the Korean version of the Boston carpal tunnel questionnaire: its clinical evaluation in patients with carpal tunnel syndrome following local corticosteroid injection. J. Korean Med. Sci. 28 (7), 1095–1099. https://doi.org/10.3346/JKMS.2013.28.7.1095 (2013).
Lue, Y. J., Lu, Y. M., Lin, G. T. & Liu, Y. F. Validation of the Chinese version of the Boston carpal tunnel questionnaire. J. Occup. Rehabil. 24 (1), 139–145. https://doi.org/10.1007/S10926-013-9438-9/METRICS (2014).
Bougea, A. et al. Reliability and validation of the Greek version of the Boston carpal tunnel questionnaire. Hand 13 (5), 593–599. https://doi.org/10.1177/1558944717725379/SUPPL_FILE/HAN725379_SUPPLEMENTAL_TABLES.DOCX (2018).
Leite, J. C. D. C., Jerosch-Herold, C. & Song, F. A systematic review of the psychometric properties of the Boston carpal tunnel questionnaire. BMC Musculoskelet. Disord. 7 (1), 1–9. https://doi.org/10.1186/1471-2474-7-78/TABLES/3 (2006).
Bakhsh, H., Ibrahim, I., Khan, W. S., Smitham, P. & Goddard, N. Assessment of validity, reliability, responsiveness and bias of three commonly used patient-reported outcome measures in carpal tunnel syndrome. Ortop. Traumatol. Rehabil. 14 (4), 335–340. https://doi.org/10.5604/15093492.1005085 (2012).
Thomas, M., Hinton, A., Heywood, A., Shirley, R. & Chan, J. K. K. Peripheral nerve decompression in the upper limb in spinal cord injury: experiences at the National Spinal Injuries Centre, UK, Spinal Cord Ser. Cases vol. 7, no. 1, pp. 1–7, 2021, (2021). https://doi.org/10.1038/s41394-021-00423-4
BCTQ. accessed 09, (2023). https://www.gettingitrightfirsttime.co.uk/wp-content/uploads/2021/12/BCTQ.pdf
Lam, N. & Thurston, A. Association of obesity, gender, age and occupation with carpal tunnel syndrome. Aust N Z. J. Surg. 68 (3), 190–193. https://doi.org/10.1111/J.1445-2197.1998.TB04743.X (1998).
Becker, J. et al. An evaluation of gender, obesity, age and diabetes mellitus as risk factors for carpal tunnel syndrome. Clin. Neurophysiol. 113 (9), 1429–1434. https://doi.org/10.1016/S1388-2457(02)00201-8 (2002).
Karpitskaya, Y., Novak, C. B. & Mackinnon, S. E. Prevalence of smoking, obesity, diabetes mellitus, and thyroid disease in patients with carpal tunnel syndrome. Ann. Plast. Surg. 48 (3), 269–273. https://doi.org/10.1097/00000637-200203000-00007 (2002).
Nazish, S. et al. Electrophysiologic severity of carpal tunnel syndrome in diabetic patients of the Saudi population. Neurosciences 24 (1), 22. https://doi.org/10.17712/NSJ.2019.1.20180217 (2019).
Pourmemari, M. H. & Shiri, R. Diabetes as a risk factor for carpal tunnel syndrome: a systematic review and meta-analysis. Diabet. Med. 33 (1), 10–16. https://doi.org/10.1111/DME.12855 (2016).
Tharwat, S. & Nassar, M. K. Clinical and ultrasonographic screening for carpal tunnel syndrome in Hemodialysis patients. Kidney Res. Clin. Pract. 39 (2), 213. https://doi.org/10.23876/J.KRCP.20.011 (2020).
Yucel, H. Factors affecting symptoms and functionality of patients with carpal tunnelsyndrome: a retrospective study. J. Phys. Ther. Sci. 27 (4), 1097. https://doi.org/10.1589/JPTS.27.1097 (2015).
Sharief, F., Kanmani, J. & Kumar, S. Risk factors, symptom severity and functional status among patients with carpel tunnel syndrome. Neurol. India. 66 (3), 743–746. https://doi.org/10.4103/0028-3886.232351 (2018).
Relationships between clinical. symptom severity scales and nerve conduction measures in carpal tunnel syndrome - You – 1999 - Muscle & Nerve - Wiley Online Library. Accessed Dec 10, (2023). https://onlinelibrary.wiley.com/doi/10.1002/(SICI)1097-4598(199904)22:4%3C497::AID-MUS11%3E3.0.CO;2-T
Newington, L., Harris, E. C. & Walker-Bone, K. Carpal tunnel syndrome and work. Best Pract. Res. Clin. Rheumatol. 29 (3), 440–453. https://doi.org/10.1016/J.BERH.2015.04.026 (2015).
Fakhouri, F., Alsukhni, R. A., Altunbi, B., Hawoot, Z. & Dabbagh, R. Factors correlated with unfavorable outcome after carpal tunnel release surgery. Asian J. Neurosurg. 12 (04), 670–673. https://doi.org/10.4103/AJNS.AJNS_3_15 (2017).
Gong, H. S. et al. Clinical features influencing the patient-based outcome after carpal tunnel release. J. Hand Surg. Am. 33 (9), 1512–1517. https://doi.org/10.1016/J.JHSA.2008.05.020 (2008).
Carpal tunnel release. Correlations with preoperative symptomatology - PubMed. accessed Dec. 10, (2023). https://pubmed.ncbi.nlm.nih.gov/8620634/.
Lozano Calderón, S. A., Paiva, A. & Ring, D. Patient satisfaction after open carpal tunnel release correlates with depression. J. Hand Surg. Am. 33 (3), 303–307. https://doi.org/10.1016/J.JHSA.2007.11.025 (2008).
Sonohata, M. et al. The effect of carpal tunnel release on neuropathic pain in carpal tunnel syndrome. Pain Res. Manag. 2017 https://doi.org/10.1155/2017/8098473 (2017).
Acknowledgements
We acknowledge the cooperation of the IT office to facilitate the collection of data from electronic and archived files.
Author information
Authors and Affiliations
Contributions
Dawod conceptualized the study, supervised the research, performed data analysis, and drafted the manuscript. Alswerki contributed to study design, coordinated data collection, and critically reviewed the manuscript. Alelaumi handled data acquisition and preliminary analysis, while Alqawasmi and Khasawneh supported the literature review, data validation, and editing. Alrayes and Hamadeen assisted with clinical records, data entry, and formatting. Alqudah and Al-Amer contributed to data organization, formatting, and proofreading. Khanfar provided oversight of surgical methodology and approved the final manuscript. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics and consent to participate
This study was approved by the Jordan University Hospital IRB (IRB number 2023/25128). Participants gave informed consent, and strict confidentiality measures were maintained. The research followed the World Medical Association’s Declaration of Helsinki ethics code.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Dawod, M.S., Alswerki, M.N., Alelaumi, A.F. et al. Patient-reported outcomes and functional recovery after carpal tunnel surgery in a developing health care system: insights from clinical practice. Sci Rep 15, 34224 (2025). https://doi.org/10.1038/s41598-025-16058-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-16058-6