Abstract
Multidrug-resistant diarrheagenic Escherichia coli (MDR-DEC) increasingly complicates treatment of pediatric infections, largely due to β-lactamase-mediated resistance. Despite their clinical relevance, the evolutionary diversity, functional mechanisms, and therapeutic targeting of β-lactamase enzymes in DEC remain poorly defined. This study addresses that gap by evaluating the prevalence of β-lactamase genes in DEC isolates and exploring their molecular interactions with key antibiotics. This study aims to detect and characterize β-lactamase-producing diarrheagenic Escherichia coli (DEC) isolates from children suffering from diarrhea, and to investigate the underlying drug-target interactions contributing to antimicrobial resistance. A total of 120 E. coli isolates were obtained from pediatric diarrheal, non-diarrheal, and healthy groups. Molecular screening for β-lactamase genes was performed using RT-PCR. Structural modeling, phylogenetic analysis, and molecular docking were used to evaluate evolutionary patterns and drug interactions with ceftriaxone and amoxicillin. β-lactamase enzymes in DEC strains exhibited varying thermal stability and were frequently co-produced. Molecular docking revealed that while amoxicillin had stronger binding affinity for certain enzymes, ceftriaxone demonstrated greater inhibitory potency across key targets. Resistance genes such as bla_TEM, bla_SHV, and bla_CTX-M were central in the resistance network. Additional mechanisms, including efflux pump activity and DNA repair pathways, contributed to the multidrug-resistant phenotype. This study highlights the multifactorial resistance landscape of DEC, driven by diverse β-lactamase variants and supporting mechanisms such as efflux and DNA repair. The differential drug interaction profiles of amoxicillin and ceftriaxone underscore the importance of structure-guided antibiotic selection. These insights may inform more targeted therapeutic strategies and support molecular surveillance efforts to monitor and combat MDR-DEC in pediatric settings.
Similar content being viewed by others
Introduction
The rise of β-lactamase-producing multidrug-resistant (MDR) Escherichia coli strains is a significant public health concern, particularly in vulnerable populations such as children under five years of age1. E. coli is a leading cause of diarrheal diseases in children, and the emergence of strains that produce β-lactamase enzymes has severely limited treatment options, making these infections more difficult to manage2,3. lactamases enzymes, including extended spectrum β-lactamases (ESBLs), metallo-β-lactamases (MβLs), and AmpC β-lactamases, confer resistance to a wide range of β-lactam antibiotics, such as penicillin’s and cephalosporins, by hydrolyzing the β-lactam ring, thereby neutralizing the efficacy of the antibiotics4.
In recent years, there has been a notable increase in the prevalence of MDR diarrheagenic E. coli (DEC) in children, complicating treatment strategies and posing a significant threat to child health5. The β-lactamase-producing strains are of particular concern because they not only resist standard treatments but also often carry additional resistance genes on plasmids, which can spread rapidly through bacterial populations through horizontal gene transfer (HZT)6. This situation is exacerbated in pediatric populations, where therapeutic options are limited due to the need for careful dosing and the restricted use of certain antibiotics7,8.
Amoxicillin, a commonly used penicillin derivative, and ceftriaxone, a third-generation cephalosporin, are often prescribed for treating bacterial infections in children due to their broad-spectrum activity and safety profiles9,10,11,12. However, the effectiveness of these antibiotics is increasingly compromised by the presence of β-lactamase-producing DEC, which degrade these drugs before they can effectively eliminate the infection13. The ability of these pathogens to resist amoxicillin and ceftriaxone is particularly concerning in the context of diarrheal diseases, which remain a leading cause of morbidity and mortality in young children globally14,15,16.
The broad clinical use and varied activity spectra of amoxicillin and ceftriaxone make them penicillin and cephalosporins, respectively11. Unlike other antibiotics, these drugs are frequently targeted by key β-lactamase enzymes, making them ideal for studying resistance mechanisms11. Amoxicillin and ceftriaxone are frequently targeted by β-lactamase enzymes due to their widespread use and structural vulnerability. Amoxicillin is easily hydrolyzed by common β-lactamases, while ceftriaxone is a key target of ESBLs like CTX-M. Their frequent use, especially without β-lactamase inhibitors, creates strong selective pressure, promoting resistance. Additionally, their distinct chemical structures allow for a comparative analysis of how structural differences influence binding and resistance, providing broader insights that might be gained from other antibiotics11,12.
This study is relevant for detecting and characterizing β-lactamase-producing diarrheagenic Escherichia coli (DEC) isolates from children with diarrhea, as well as for exploring the underlying drug-target interactions that contribute to antimicrobial resistance. By employing molecular docking studies to analyze the interactions between β-lactamase enzymes and key antibiotics such as amoxicillin and ceftriaxone, this research aims to uncover the structural features that contribute to drug resistance. The study also correlates these molecular interactions with the broader MDR mechanisms, providing a comprehensive understanding of how these enzymes play a central role in the resistance network.
This research is crucial for developing targeted interventions to combat MDR E. coli infections in children, particularly in resource-limited settings where the burden of diarrheal diseases is highest17. Understanding the specific mechanisms of resistance in this age group will help in designing better therapeutic approaches and in implementing more effective antibiotic stewardship programs to preserve the efficacy of existing drugs. Ultimately, this study aims to contribute to reducing the incidence and severity of diarrheal diseases caused by MDR DEC in young children, thereby improving health outcomes in this vulnerable population.
Materials and methods
Study group
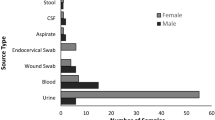
The study population consisted of three groups of children under 5 years of age. Group 1 included 40 children with acute diarrhea who were not receiving any antibiotics. Group 2 comprised 40 hospitalized children receiving antibiotic (oral/I/v) for reasons other than diarrhea admitted to NICU/Ward for the past 72-hour duration (to distinguish the impact of antibiotic exposure from the presence of diarrhea itself on the development, spread and pattern of antimicrobial resistance). Group 3 consisted of 40 healthy children who were not suffering from diarrhea or any other disease. While children with known immunological disorders, chronic gastrointestinal disorders and receiving/received probiotic for the last seven days were excluded from the study. The samples were collected for a period of two years from June 2014 to June 2016.
Ethics
Stool samples were collected after obtaining informed consent from the parents or guardians of the participants. The study was approved by the “institutional ethics committee—human research (IEC-HR) university college of medical sciences, University of Delhi, New Delhi in accordance with WHO guidelines.
Processing of samples
Fecal samples were processed using standard biochemical tests for distinguishing E. coli from other enteric bacteria18. Antimicrobial susceptibility testing was conducted using the Kirby-Bauer disc diffusion method for β-lactamase production using a phenotypic method19, and subsequently confirmed by quantitative polymerase chain reaction (qPCR) following DNA extraction. The list of primers used for β-lactamase production in this study is presented in Table 1.
Quantitative PCR (qPCR)
SYBR Green-based qPCR was conducted in a 96-well white opaque plate (Roche), with each well containing a total volume of 20 µL. The reaction mixture included 10 µL of SYBR Green I master mix (2X), 1 µL of each primer (forward and reverse), and 3 µL of DNA. DNA amplification was carried out using the Roche LightCycler 480-II, starting with a pre-incubation step at 94 °C for 7 min, followed by 35 cycles of amplification with an annealing at 60 °C for 30 s, and concluding with cooling at 40 °C.
Sequencing
DNA sequencing of selected PCR products was performed using the same set of primers mentioned in our previous studies to verify the authenticity of the gene24,25. The sequencing was conducted at Helix Biosciences in Delhi. The sequences have been deposited in genbank, and accession numbers were obtained.
Molecular docking
To predict the binding poses of the selected β-lactamase gene products with drugs exhibiting minimal resistance or high sensitivity, molecular docking was conducted using AutoDock 4.2 and analyzed with Discovery Studio Visualizer 2021, following the general approach described by Reddy et al.26,27. The 3D structures of the target drugs were retrieved from the PubChem database28, and ligand preparation was carried out using the LigPrep module (version 2.8, Schrödinger Suite)29,30, with energy minimization applied via the OPLS_2005 force field to generate low-energy conformers.
The β-lactamase protein structures were prepared by removing water molecules, adding polar hydrogens, and assigning Kollman charges, following standard AutoDock protocols26. The docking grid was centered on active site residues identified through structural analysis, with dimensions set to 60 × 60 × 60 Å and a grid spacing of 0.375 Å, consistent with established docking procedures26. Docking was executed using AutoDock’s Lamarckian Genetic Algorithm, with 100 independent runs, a population size of 150, 2.5 million energy evaluations per run, and mutation and crossover rates of 0.02 and 0.8, respectively27. Binding poses were ranked by binding energy, and the top-scoring conformations were selected for analysis.
While docking scores offer a useful approximation of ligand–receptor interaction strength, they are limited by simplified scoring functions that neglect key thermodynamic factors, such as enthalpy and entropy13. Therefore, docking in this study was primarily used for posing prediction and comparative assessment.
Comprehensive genomic and functional analysis
To perform a comprehensive functional analysis, genes associated with MDR-DEC were retrieved from the NCBI database31. Various analyses were then conducted using these sequences. Gene interaction network analysis was carried out using STRING32 and Cytoscape software33 to elucidate the interactions and functional relationships between these genes. For functional annotation, gene ontology (GO) enrichment analysis34 was performed to determine the biological processes, cellular components, and molecular functions associated with the identified genes. Additionally, KEGG pathway analysis was utilized to map these genes into relevant biochemical pathways, providing insights into their roles in metabolic and signaling pathways35. For phylogenetic analysis, multiple sequence alignments of the identified genes were conducted using Clustal W, and phylogenetic trees were constructed using MEGA software36 to explore evolutionary relationships and divergence among the gene sequences. These combined analyses provided a comprehensive understanding of the genetic basis of MDR in DEG.
Statistical analysis
Statistical analysis was performed to compare the prevalence of MDR-DEG among the three study groups. Data from antimicrobial susceptibility testing and β-lactamase production assays were analyzed using the Fisher’s exact test to determine significant differences in resistance patterns between groups. For continuous variables, such as zone of inhibition measurements and temperature stability values, one-way ANOVA followed by Tukey’s post-hoc test was employed to assess group-wise differences. The qPCR data, including gene expression levels, were analyzed using the 2^−ΔΔCt method for relative quantification. Differences in gene expression levels among groups were assessed using one-way ANOVA followed by Bonferroni’s post-hoc test.
To evaluate potential predictors associated with multidrug resistance, multiple logistic regression analysis was conducted using SPSS version 25.0, adjusting for relevant clinical and demographic covariates. Phylogenetic analysis was performed using the Maximum Likelihood (ML) method with bootstrap analysis (1,000 replicates) to assess the statistical robustness of tree topologies. Gene interaction network analysis, along with Gene Ontology (GO) and KEGG pathway enrichment analysis37,38, was statistically evaluated using hypergeometric tests and corrected for multiple testing using the Benjamini-Hochberg false discovery rate (FDR) method to control for type I error. All statistical analyses were performed using SPSS software version 25.0 or relevant bioinformatics tools, and a p-value of < 0.05 was considered statistically significant.
Results
Thermal stability of different β-lactamase genes: qPCR melting curve analysis
The average melting temperature (Tm) for each tested β-lactamase gene is presented in Fig. 1.
The OXA gene had the highest average melting temperature at 90 °C, indicating it may have the most stable structure under thermal conditions. The SHV gene had the lowest average melting temperature at 81.92 °C, suggesting it may be the least stable under thermal conditions. Most genes exhibited average melting temperatures around the mid to high 80 s °C, with varying degrees of standard deviations, reflecting different levels of structural stability. The standard deviations were relatively small for most genes, indicating consistent melting temperature measurements across replicates.
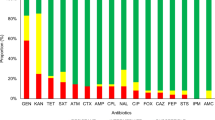
Distribution of β-lactamase production
A comparative distribution of β-lactamase production (ESBL, MBL, and AmpC) by phenotypic and genotypic methods is depicted in Table 2. Among the total isolates, 76 were identified as ESBL producers (27 from Group 1, 27 from Group 2, and 22 from Group 3). The most prevalent ESBL genes were TEM (40.83%) and SHV (32.5%), followed by CTX-M (19.16%) and OXA (19.16%). Overall, while co-production of specific β-lactamase genes was common, the complete co-occurrence of all relevant ESBL, MBL, or AmpC genes in a single isolate was not observed, indicating distinct patterns of resistance gene distribution within the bacterial populations studied (Table 2).
Prevalence and co-production patterns of β-lactamase enzymes
The distribution of β-lactamase production either alone or in combination within isolates is depicted in Table 3. Out of 120 clinical isolates examined, 99 (82.5%) were positive for β-lactamase production, indicating a high prevalence of resistance mechanisms within the sample population. Group 1 showed the highest overall rates of β-lactamase co-production, suggesting a significant burden of MDR strains within this group. These findings highlight the complexity and diversity of resistance mechanisms in clinical isolates, underlining the challenges in treating infections caused by these MDR bacteria39.
Age-related association of β-lactamase infections in pediatric patients
Table 4 presents a multivariable logistic regression analysis comparing the odds of β-lactamase infections (ESBL, MBL, and AmpC) between two age groups (< 36 months and 36–60 months), using group 3 as the reference. The odds of having an ESBL infection in group 1 were 3.612 times higher compared to group 3, and in group 2, the odds were 0.527 times lower than in group 3. However, these differences were not statistically significant (p > 0.05), the reason for this maybe lies in the fact that group 2 was hospitalized and likely received antibiotics for other bacterial infections. This prior or ongoing antibiotic exposure could influence microbial resistance patterns or colonization rates, making their microbial profile different from that of healthy community controls, group 2 may have been exposed to selective pressure due to antibiotic treatment, leading to an increased likelihood of carrying resistant organisms and it might also be due to insufficient sample size or variability within the group, which limits the power to detect a real difference even if it exists.
Overall, this logistic regression analysis reveals that, generally, there is no statistically significant association between age and β-lactamase infections (ESBL, MBL, and AmpC) in the two age groups analyzed, except for ESBL-negative cases in group 1, where younger children were more likely to be ESBL-negative.
Age as a significant predictor of β-lactamase production in pediatric patients
Table 5 presents a multivariable logistic regression analysis identifying age as a significantly associated with β-lactamase production in pediatric patients. Children under 3 years were significantly associated with increased odds of producing ESBL (odds ratio = 10.19), MBL (odds ratio = 8.4), and AmpC β-lactamases (odds ratio = 13.82) compared to those aged 3 to 5 years (p < 0.0001 for all). Gender did not significantly predict β-lactamase production, although a non-significant trend was observed for higher MBL production in males. These results underscore the critical role of age in β-lactamase production among young children.
Phylogenetic analysis and evolutionary relationships of β-lactamase genes in diverse bacterial strains
A phylogenetic tree was constructed using the maximum likelihood method in MEGA 11.0, following multiple sequence alignment with Clustal W (Fig. 2). Sequences generated in this study were deposited in the NCBI GenBank, with accession numbers including KX941097.1, KY753820.1 (TEM), KY883445.1 (SHV), KY753817, KY883447.1, KY883448.1, KY883449.1, KY883450.1 (CTX), KY913604.1 (OXA), KY753818.1 (NDM-1) and KY753819.1 (CMY). The DEC isolates sequenced in this study are indicated with red diamonds in Fig. 2 and represent various β-lactamase genes associated with multidrug resistance (Table S1).
This phylogenetic tree represents the evolutionary relationships among various β-lactamase genes associated with multidrug resistance from different bacterial strains. The tree is derived from multiple sequence alignments and constructed using MEGA software. Each branch corresponds to a specific gene sequence, with labels indicating the gene name and the bacterial strain. Red diamonds highlight the DEC specifically focused on in this study. The tree provides insights into the genetic diversity and evolutionary lineage of β-lactamase genes (Table S1), illustrating the clustering of similar gene sequences within and across different bacterial species.
The phylogenetic tree demonstrates that these β-lactamase genes are distributed among distinct clades, reflecting both sequence divergence and horizontal gene transfer events. Clustering of similar β-lactamase variants across different bacterial species indicates frequent inter-species gene exchange, contributing to the dissemination of resistance mechanisms. To further validate the functional conservation of these genes, INTERPROSCAN analysis was performed. This revealed that all β-lactamase gene sequences shared ≥ 98% similarity with known β-lactamase family domains. This high degree of domain conservation, across diverse phylogenetic clusters, supports the evolutionary stability and functional importance of β-lactamase activity despite sequence variability. Together, the phylogenetic and domain analyses suggest that these resistance genes are both evolutionarily conserved and selectively retained, underscoring their central role in antibiotic resistance.
Structural insights into the binding interactions of amoxicillin and ceftriaxone with β-lactamase proteins
In this study, we analyzed the interactions between amoxicillin and ceftriaxone and β-lactamase proteins (TEM, SHV, CTX-M, OXA, NDM-1, and AmpC), which are key mediators of antibiotic resistance in bacterial pathogens, using active site prediction and molecular docking techniques (Figs. 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14).
Docking interactions of amoxicillin with the TEM β-lactamase protein. (A) 2D Interactions: Depicts the molecular interactions of amoxicillin with active site residues of the TEM β-lactamase protein, highlighting hydrogen bonds, hydrophobic interactions, and other non-covalent interactions critical for binding. Generated using Discovery Studio Visualizer. (B) 3D Interactions: Shows the spatial conformation of amoxicillin within the active site of the TEM protein, providing insights into its orientation and proximity to critical residues. Generated using PyMOL for 3D visualization of the docked complex. (C) Surface Area Interactions: Highlights the binding pocket topology, including hydrophilic and hydrophobic regions, showcasing how amoxicillin interacts with the enzyme’s surface. Created using AutoDock Tools for docking results and PyMOL for surface visualization. (D) Protein Structure with Binding Site: Demonstrates the location of the binding pocket within the overall tertiary structure of the TEM protein. Generated using PyMOL to integrate the docking results into the protein structure.
Active site prediction
The active sites of the β-lactamase proteins were meticulously identified and compared with their respective template structures to pinpoint conserved binding regions (Figs. 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14). The analysis revealed that sites 1 and 2 were highly conserved across most of the proteins, although each enzyme exhibited distinct patterns of amino acid residues at these active sites. For the TEM β-lactamase, key residues such as PHE135, THR120, and MET19 were crucial for binding interactions with inhibitors. In the SHV enzyme, residues like ALA60, GLU121, and THR163 played significant roles in facilitating interactions with beta-lactam antibiotics. The CTX-M β-lactamase’s active site included critical residues such as MET38, LEU15, and ARG12, essential for the enzyme’s function and its binding to inhibitors. Similarly, the OXA enzyme exhibited important conserved residues, including VAL23, TRP134, and MET19, which were vital for its activity. The NDM-1 enzyme’s active site was characterized by residues like TRP134, LEU83, and ILE86, which are key for inhibitor binding. Finally, in the AmpC β-lactamase, residues such as TYR48, GLY121, and SER22 were identified as integral to the enzyme’s resistance mechanism. These findings highlight the importance of these conserved residues in the functionality and interactions with inhibitors of β-lactamase enzymes.
Molecular docking interactions
Following the prediction of active sites, molecular docking studies were conducted to evaluate the binding interactions of amoxicillin and ceftriaxone with the identified β-lactamase proteins. The docking results provided detailed insights into the structural and molecular interactions within the active sites, as visualized in Figs. 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14. For the TEM protein (Fig. 3 and 4), amoxicillin interacted within a site volume of 330 cubic Å, forming hydrogen bonds and other molecular interactions with residues such as SER56, GLN62, and ARG57, while ceftriaxone engaged with residues like MET129, GLY130, and LYS16 within the same site volume, highlighting distinct binding profiles. In the SHV protein (Figs. 5 and 6), amoxicillin docked within a larger site volume of 486 cubic Å, interacting with residues like PHE35, PRO36, and MET38, whereas ceftriaxone showed binding interactions with residues such as GLY14, LEU15, and ILE16, demonstrating a different orientation within the same active site. The CTX-M protein (Figs. 7 and 8) exhibited a site volume of 259 cubic Å for both drugs, with amoxicillin interacting with ALA47, PRO63, and VAL54, and ceftriaxone binding to residues like THR51, VAL54, and VAL27, further illustrating differences in binding orientation. For the OXA protein (Figs. 9 and 10), amoxicillin occupied a site volume of 234 cubic Å, interacting with residues such as PHE82, LEU83, and ILE86, while ceftriaxone engaged with residues like SER22, GLN79, and MET19 within the same volume, showcasing distinct interaction profiles. The NDM-1 protein (Figs. 11 and 12), with a site volume of 264 cubic Å, showed that amoxicillin interacted with residues like ILE16, GLU17, and MET18, whereas ceftriaxone bound to residues such as GLN79, LYS119, and THR120, reflecting potential differences in inhibitory effectiveness. Lastly, in the AmpC protein (Figs. 13 and 14), amoxicillin docked within a site volume of 313 cubic Å, interacting with residues like MET38, VAL13, and PRO152, while ceftriaxone showed interactions with residues such as PHE82, LEU83, and ILE86, demonstrating how each drug occupies and interacts with the active site differently.
Docking interactions of ceftriaxone with the TEM β-lactamase protein. (A) 2D Interactions: Depicts the molecular interactions of ceftriaxone with active site residues of the TEM β-lactamase protein, including hydrogen bonds, van der Waals forces, and other critical non-covalent interactions. Generated using Discovery Studio Visualizer. (B) 3D Interactions: Shows the spatial conformation of ceftriaxone within the active site of the TEM protein, highlighting the orientation and spatial proximity to key amino acid residues. Created using PyMOL. (C) Surface Area Interactions: Displays the surface topology of the TEM protein binding pocket, emphasizing hydrophilic and hydrophobic interactions with ceftriaxone. Generated using AutoDock Tools and visualized in PyMOL. (D) Protein Structure with Binding Site: Demonstrates the position of the binding pocket in the overall 3D structure of the TEM protein, providing a holistic view of the docking interaction. Visualized using PyMOL.
Docking interactions of amoxicillin with the SHV-1 β-lactamase protein. (A) 2D Interactions: Displays the molecular interactions of amoxicillin with the active site residues of the SHV-1 β-lactamase protein, including hydrogen bonds, van der Waals forces, and other critical interactions stabilizing the drug-enzyme complex. Generated using Discovery Studio Visualizer. (B) 3D Interactions: Illustrates the spatial orientation of amoxicillin within the active site, highlighting its proximity to key amino acid residues and the structural compatibility of the molecule within the binding pocket. Visualized using PyMOL. (C) Surface Area Interactions: Reveals the topological features of the SHV-1 protein’s binding pocket, emphasizing the interactions of amoxicillin with hydrophilic and hydrophobic regions. Generated using AutoDock Tools and visualized in PyMOL. (D) Protein Structure with Binding Site: Demonstrates the location of the amoxicillin binding pocket within the overall tertiary structure of SHV-1, providing a comprehensive view of the interaction. Visualized using PyMOL.
Docking interactions of ceftriaxone with the SHV-1 β-lactamase protein. (A) 2D Interactions: Highlights the molecular interactions of ceftriaxone with key active site residues of the SHV-1 β-lactamase protein, including hydrogen bonds, van der Waals interactions, and other non-covalent interactions. These interactions stabilize the ceftriaxone-enzyme complex. Generated using Discovery Studio Visualizer. (B) 3D Interactions: Shows the spatial orientation of ceftriaxone within the SHV-1 active site, illustrating its interaction with critical residues and the structural fit within the binding pocket. Created using PyMOL. (C) Surface Area Interactions: Depicts the binding pocket topology of the SHV-1 protein, emphasizing the hydrophilic and hydrophobic interactions between ceftriaxone and the enzyme surface. Visualized using AutoDock Tools and PyMOL. (D) Protein Structure with Binding Site: Presents the overall structure of the SHV-1 β-lactamase protein with the binding pocket highlighted, providing a holistic view of the ceftriaxone binding interaction. Visualized using PyMOL.
Docking interactions of amoxicillin with the CTX-M-14 β-lactamase protein. (A) 2D Interactions: Shows the molecular interactions of amoxicillin with active site residues of CTX-M-14, including hydrogen bonds, van der Waals forces, and other key non-covalent interactions. These interactions play a crucial role in stabilizing the drug-enzyme complex. Generated using Discovery Studio Visualizer. (B) 3D Interactions: Illustrates the spatial orientation of amoxicillin within the active site of CTX-M-14, highlighting its proximity to critical residues and the structural compatibility of the molecule with the binding pocket. Visualized using PyMOL. (C) Surface Area Interactions: Depicts the binding pocket topology of CTX-M-14, emphasizing hydrophilic and hydrophobic regions involved in the interaction with amoxicillin. Generated using AutoDock Tools and visualized with PyMOL. (D) Protein Structure with Binding Site: Provides an overview of the CTX-M-14 β-lactamase protein’s tertiary structure, showcasing the binding pocket location and the interaction of amoxicillin with surrounding residues. Visualized using PyMOL.
Docking interactions of ceftriaxone with the CTX-M-14 β-lactamase protein. (A) 2D Interactions: Depicts the molecular interactions of ceftriaxone with key active site residues of CTX-M-14, including hydrogen bonds, van der Waals interactions, and other stabilizing forces that contribute to the drug’s binding. Generated using Discovery Studio Visualizer. (B) 3D Interactions: Highlights the spatial conformation of ceftriaxone within the CTX-M-14 active site, showing its orientation and proximity to critical residues involved in drug binding. Created using PyMOL. (C) Surface Area Interactions: Displays the binding pocket topology, showcasing hydrophilic and hydrophobic regions and their interactions with ceftriaxone. Generated using AutoDock Tools and visualized in PyMOL. (D) Protein Structure with Binding Site: Provides an overview of the CTX-M-14 β-lactamase protein’s tertiary structure, pinpointing the binding pocket and illustrating the interactions of ceftriaxone with key residues. Visualized using PyMOL.
Docking interactions of amoxicillin with the OXA-1 β-lactamase protein. (A) 2D Interactions: Illustrates the molecular interactions between amoxicillin and the active site residues of OXA-1, including hydrogen bonds, van der Waals forces, and other stabilizing interactions that support binding. Generated using Discovery Studio Visualizer. (B) 3D Interactions: Depicts the spatial conformation of amoxicillin within the OXA-1 active site, highlighting its orientation and interaction with key residues critical for binding. Visualized using PyMOL. (C) Surface Area Interactions: Highlights the binding pocket topology, showing hydrophilic and hydrophobic regions and their interaction with amoxicillin. Generated using AutoDock Tools and visualized with PyMOL. (D) Protein Structure with Binding Site: Provides a structural overview of the OXA-1 β-lactamase protein, identifying the binding pocket and its interaction with amoxicillin within the overall tertiary structure. Visualized using PyMOL.
Docking interactions of ceftriaxone with the OXA-1 β-lactamase protein. (A) 2D Interactions: Highlights the molecular interactions between ceftriaxone and the active site residues of OXA-1, including hydrogen bonds, van der Waals forces, and other stabilizing interactions crucial for binding. Generated using Discovery Studio Visualizer. (B) 3D Interactions: Depicts the spatial conformation of ceftriaxone within the OXA-1 active site, showing its orientation and proximity to key residues involved in the binding process. Visualized using PyMOL. (C) Surface Area Interactions: Displays the binding pocket topology of OXA-1, emphasizing the hydrophilic and hydrophobic interactions between ceftriaxone and the enzyme’s active site. Generated using AutoDock Tools and visualized with PyMOL. (D) Protein Structure with Binding Site: Provides a structural overview of the OXA-1 β-lactamase protein, identifying the binding pocket location and illustrating the interactions of ceftriaxone with key residues in the tertiary structure. Visualized using PyMOL.
Docking interactions of amoxicillin with the NDM β-lactamase protein. (A) 2D Interactions: Highlights the molecular interactions between amoxicillin and the active site residues of NDM, including hydrogen bonds, van der Waals forces, and π-alkyl interactions. These interactions are essential for stabilizing the drug-enzyme complex. Generated using Discovery Studio Visualizer. (B) 3D Interactions: Shows the spatial conformation of amoxicillin within the NDM active site, illustrating its binding orientation and proximity to key residues involved in stabilizing the complex. Visualized using PyMOL. (C) Surface Area Interactions: Depicts the binding pocket topology of NDM, emphasizing hydrophilic and hydrophobic interactions between amoxicillin and the enzyme. Generated using AutoDock Tools and visualized with PyMOL. (D) Protein Structure with Binding Site: Provides an overview of the NDM β-lactamase protein’s tertiary structure, pinpointing the location of the binding pocket and illustrating the interactions of amoxicillin with the surrounding residues. Visualized using PyMOL.
Docking interactions of ceftriaxone with the NDM β-lactamase protein. (A) 2D Interactions: Highlights the molecular interactions between ceftriaxone and the active site residues of NDM, including hydrogen bonds, van der Waals forces, and π-alkyl interactions. These interactions are critical for stabilizing the drug-enzyme complex. Generated using Discovery Studio Visualizer. (B) 3D Interactions: Depicts the spatial conformation of ceftriaxone within the NDM active site, illustrating its binding orientation and proximity to key residues involved in stabilizing the complex. Visualized using PyMOL. (C) Surface Area Interactions: Shows the topology of the NDM binding pocket, emphasizing hydrophilic and hydrophobic interactions between ceftriaxone and the enzyme. Generated using AutoDock Tools and visualized with PyMOL. (D) Protein Structure with Binding Site: Provides a structural overview of the NDM β-lactamase protein, identifying the binding pocket location and illustrating the interactions of ceftriaxone with key residues in the tertiary structure. Visualized using PyMOL.
Docking interactions of amoxicillin with the AmpC β-lactamase protein. (A) 2D Interactions: Illustrates the molecular interactions between amoxicillin and the active site residues of AmpC, highlighting hydrogen bonds, van der Waals forces, and π-alkyl interactions that stabilize the drug-enzyme complex. Generated using Discovery Studio Visualizer. (B) 3D Interactions: Depicts the spatial conformation of amoxicillin within the AmpC active site, showing its binding orientation and interaction with critical residues. Visualized using PyMOL. (C) Surface Area Interactions: Shows the topology of the AmpC binding pocket, emphasizing hydrophilic and hydrophobic interactions between amoxicillin and the enzyme. Generated using AutoDock Tools and visualized with PyMOL. (D) Protein Structure with Binding Site: Provides an overview of the AmpC β-lactamase protein, identifying the location of the binding pocket and illustrating amoxicillin’s interactions with surrounding residues in the tertiary structure. Visualized using PyMOL.
Docking interactions of ceftriaxone with the AmpC β-lactamase protein. (A) 2D Interactions: Depicts the molecular interactions between ceftriaxone and active site residues of AmpC, including hydrogen bonds, van der Waals forces, π-alkyl interactions, and other stabilizing forces. These interactions play a key role in forming the drug-enzyme complex. Generated using Discovery Studio Visualizer. (B) 3D Interactions: Highlights the spatial orientation of ceftriaxone within the AmpC active site, showing its proximity to key residues involved in stabilizing the binding interaction. Visualized using PyMOL. (C) Surface Area Interactions: Shows the binding pocket topology of AmpC, emphasizing hydrophilic and hydrophobic regions that interact with ceftriaxone. Generated using AutoDock Tools and visualized with PyMOL. (D) Protein Structure with Binding Site: Provides an overview of the AmpC β-lactamase protein, pinpointing the binding pocket and illustrating the interactions of ceftriaxone with surrounding residues in the tertiary structure. Visualized using PyMOL.
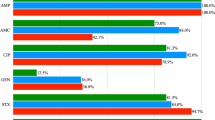
Molecular docking analysis reveals differential affinities of amoxicillin and ceftriaxone for β-lactamase genes in MDR DEC bacteria
To know the affinity between the selected β-lactamase genes and drugs that showed minimum resistance or high sensitivity as in our study of amoxicillin and ceftriaxone, molecular docking was performed26. The binding energy between drugs and ligands were obtained in K.cal/mol (Fig. 15).
Docking results of amoxicillin and ceftriaxone with β-lactamase genes. This figure illustrates the binding energy (K.cal/mol) and predicted IC50 values (nM/µM) for various drug targets when interacted with two compounds: amoxicillin and ceftriaxone. The bar plot represents the binding energy, with lighter blue bars for amoxicillin and darker blue bars for ceftriaxone. The line plot overlaying the bars represents the predicted IC50 values on a logarithmic scale, with a blue line for amoxicillin and a dark blue line for ceftriaxone. The x-axis lists the drug targets (TEM-1, SHV-1, CTX-M, OXA-1, NDM-1, and AmpC), while the y-axes display the binding energy on the left and the predicted IC50 values on the right. This dual representation allows for a comprehensive comparison of the binding affinity and inhibitory concentration of the two drugs across different targets.
Binding affinity
Docking results indicate that amoxicillin shows stronger predicted binding (more negative binding energy) than ceftriaxone to several β-lactamase targets, including TEM-1 (−8.41 kcal/mol), OXA-1 (−7.85 kcal/mol), and NDM-1 (−6.98 kcal/mol). Ceftriaxone shows stronger binding to SHV-1 (−6.69 kcal/mol), CTX-M (−5.95 kcal/mol), and AmpC (−7.92 kcal/mol), which may contribute to differences in resistance profiles among β-lactamase-producing bacteria. However, while these docking predictions suggest ceftriaxone can still bind NDM-1, they do not fully account for the clinical observation that NDM-1 producers exhibit high resistance to amoxicillin but remain moderately susceptible to ceftriaxone. This discrepancy highlights that binding affinity alone cannot predict resistance, as catalytic efficiency (kcat/Km) and other factors like permeability and expression levels also play crucial roles (Table 6)4,13,40,41.
Inhibitory potency (IC50 values)
Despite generally weaker predicted binding affinities, ceftriaxone consistently showed lower IC50 values across all β-lactamase targets, indicating stronger inhibitory potency. For example, the IC50 values for ceftriaxone against TEM-1 and AmpC were 19.81 nM and 1.56 µM, respectively, compared to 686.08 nM and 4.29 µM for amoxicillin. These results suggest that ceftriaxone is more effective at inhibiting these enzymes, particularly in the context of multidrug-resistant strains.
Comprehensive analysis of MDR mechanisms: distribution, enrichment, and network interconnections in DEC
In this work, we examined important MDR genes, particularly those connected to DEC, to comprehend their functions in DEC-mediated MDR when combined with ceftriaxone and amoxicillin (Table 7). Using these genes, we conducted a series of analyses to explore the distribution of gene functions, pathway enrichment, and network interactions. These analyses reveal the interconnected mechanisms through which these genes contribute to MDR, providing insights into the complexity and challenges of combating resistant bacterial strains.
Distribution and diversity of MDR mechanisms in MDR-DEC
Analysis of resistance gene functions in MDR-DEC revealed that multidrug efflux pumps and β-lactamase enzymes were the most prevalent, highlighting their dominant roles in resistance (Fig. S1, Table 7). Other mechanisms included antibiotic-modifying enzymes (e.g., aminoglycoside acetyltransferase), target site modification genes, and regulators of biofilm formation. This functional diversity illustrates the complex, multifactorial basis of resistance in DEC isolates59.
Enriched pathways in MDR
Pathway enrichment analysis revealed significant involvement of efflux pump systems and membrane integrity pathways, suggesting their critical role in antibiotic evasion (Fig. S1 and S2). Additional enriched pathways included DNA repair mechanisms, topoisomerase activity, and glycosyltransferase-related processes, reflecting bacterial strategies to survive under antimicrobial pressure.
Network analysis of DEC-MDR genes
Network mapping of resistance genes showed that bla_TEM, bla_SHV, and bla_CTX-M genes were central hubs, with high connectivity to other resistance-related genes (Fig. S3). Efflux-related genes such as acrA, acrB, EmrE, and tolC also exhibited strong network integration. These gene clusters indicate co-expression or co-occurrence patterns that may enhance resistance and support horizontal gene transfer (Fig. 2), which may facilitate the spread of these resistance traits across different bacterial species60.
Interconnected pathways in MDR
The pathway network diagram highlights the interconnectedness of the key pathways involved in MDR (Fig. S4). Notably, glycosyltransferase pathways form a dense cluster, indicating their critical role in modifying bacterial structures like cell walls to resist antibiotic action. Efflux pump and membrane-associated pathways also form a significant cluster, showcasing their importance in actively expelling antibiotics from bacterial cells, thereby reducing drug efficacy. Additionally, pathways related to topoisomerase activity and DNA repair are closely linked, emphasizing their role in maintaining DNA integrity and helping bacteria survive antibiotic-induced stress. The strong interactions between these pathways suggest a coordinated effort by bacteria to employ multiple resistance mechanisms simultaneously, enhancing their overall survival against various antibiotics61.
Discussion
The findings of this study provide valuable insights into the thermal stability, distribution, and co-production patterns of β-lactamase enzymes in DEC, highlighting the complex mechanisms underlying antibiotic resistance in the MDR DEC strains.
The thermal stability analysis revealed significant variations in the Tm of different β-lactamase genes, with the OXA gene exhibiting the highest stability (Tm = 90 °C) and the SHV gene the lowest (Tm = 81.92 °C) (Fig. 1). This variation in thermal stability is crucial as it suggests that enzymes like OXA, with higher Tm, may be more resilient under various thermal conditions62,63.
The distribution analysis of β-lactamase production revealed a high prevalence of resistance genes among the clinical isolates (Table 2). ESBL production was notably the most common, identified in 63.3% of the isolates, with TEM and SHV genes being the most prevalent. The study also uncovered significant co-occurrence patterns, particularly between the TEM and SHV genes, which were 4.394 times more likely to co-occur than the CTX-M and OXA genes (Table 3). However, despite the frequent co-production of multiple β-lactamase genes, no single isolate harbored all relevant ESBL, MBL, or AmpC genes simultaneously. This may suggest that despite the common co-production of resistance genes, the complete co-occurrence of all resistance mechanisms within a single bacterial strain is not rare, which may require a combination of antibiotics to treat MDR strains39,64.
The logistic regression analysis indicated that age is a significant association of β-lactamase production in pediatric patients (Tables 4 and 5). Children under 3 years were significantly more likely to produce ESBL, MBL, and AmpC β-lactamases compared to those aged 3 to 5 years (p < 0.05). This increased prevalence in younger children may be attributed to their underdeveloped immune systems, higher frequency of hospital visits or admissions, and greater exposure to broad-spectrum antibiotics, often prescribed empirically for recurrent infections such as pneumonia, otitis media, and diarrhea. Additionally, infants and toddlers are more susceptible to colonization with resistant bacteria due to immature gut microbiota and close contact with caregivers, which may facilitate the horizontal transmission of resistance genes65,66. However, specific data comparing the prevalence between children under 3 years and those aged 3 to 5 years remain limited. This age-related association underscores the vulnerability of younger children to MDR infections, necessitating careful monitoring and targeted treatment strategies in this demographic.
The phylogenetic analysis revealed substantial genetic variation among the DEC strains, with multiple β-lactamase genes (blaTEM, blaSHV, blaCTX-M, blaOXA-1) detected across various subgroups (Fig. 2). The phylogenetic tree highlights the clustering of specific β-lactamase genes within DEC, emphasizing their role in conferring multidrug resistance. Closely related genes, such as blaCTX-M variants, may share similar enzymatic properties and resistance profiles, offering valuable clues for therapeutic targeting. By grouping β-lactamase genes, the tree facilitates the identification of potential targets for β-lactamase inhibitors, as genes within the same clade are likely to respond similarly to inhibitors. The red-highlighted DEC serves as a specific focus, enabling comparative analyses of their β-lactamase genes against those from other species and shedding light on unique or shared resistance mechanisms (Table S1)40,67.
The detailed exploration of β-lactamase-mediated resistance mechanisms in DEC uncovers the complex interactions between antibiotics and resistance enzymes, particularly through molecular docking studies and comprehensive analysis of MDR mechanisms.
The molecular docking studies provide crucial insights into the binding interactions between key β-lactamase enzymes and the antibiotics amoxicillin and ceftriaxone, which are commonly used in clinical settings to combat bacterial infections11. The docking results revealed distinct differences in the way these antibiotics interact with the active sites of various β-lactamase proteins (Figs. 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14).
Amoxicillin demonstrated a stronger binding affinity for several β-lactamase enzymes, including TEM-1, OXA-1, and NDM-1 (Fig. 4). This strong binding, characterized by more negative binding energy values, suggests that amoxicillin is effectively recognized and bound by these enzymes68,69.
Overall, the combination of active site prediction and molecular docking provided a comprehensive understanding of how amoxicillin and ceftriaxone interact with β-lactamase proteins. The distinct binding profiles observed in the docking studies, visualized in Figs. 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, reflect the unique interaction mechanisms of each antibiotic with different β-lactamase enzymes. These findings illustrate the significance of considering specific active site residues and binding interactions when designing inhibitors to counteract antibiotic resistance in bacteria70.
Ceftriaxone’s ability to inhibit the growth of β-lactamase-producing bacteria is not related to its ability to bind to β-lactamase or lower IC50 value. β-lactams work by inhibiting PBPs, thus inhibiting peptidoglycan biosynthesis71. This difference in binding and inhibition profiles between amoxicillin and ceftriaxone may highlight the significance of their binding affinity; as they are β-lactam antibiotics; they don’t inhibit β-lactamases instead the substrates for β-lactamases68,72.
The comprehensive analysis of MDR mechanisms in DEC isolates sheds light on the intricate network of resistance strategies employed by these bacteria (Table 7; Fig. 5A and D). The study identified key resistance genes, including those encoding β-lactamase enzymes and multidrug efflux pumps, as central players in the MDR phenotype observed in these isolates.
The gene interaction network revealed that β-lactamase genes such as bla_TEM, bla_SHV, and bla_CTX-M are highly interconnected with other resistance genes, indicating their pivotal role in conferring resistance to β-lactam antibiotics. These genes not only facilitate the hydrolysis of β-lactam antibiotics, rendering them ineffective but also contribute to a broader resistance network by co-occurring with other resistance mechanisms, such as efflux pumps and target site modifications41,73. This network of interactions underscores the complexity of bacterial resistance, where multiple mechanisms work synergistically to protect the bacterial cell from the effects of antibiotics74.
Efflux pumps, particularly those encoded by genes such as acrA, acrB, and tolC, play a critical role in actively expelling antibiotics from the bacterial cell, reducing the intracellular concentration of the drug and thereby diminishing its efficacy75. This active expulsion mechanism is crucial for maintaining resistance, especially in combination with β-lactamase production, which further neutralizes the antibiotic threat75,76,77.
Moreover, the pathway enrichment analysis highlighted the involvement of additional resistance mechanisms, such as DNA repair pathways and glycosyltransferase activity. These pathways contribute to the survival and adaptation of DEC strains in the presence of antibiotics by repairing drug-induced damage and modifying bacterial cell structures to prevent drug binding78,79. The interconnectedness of these pathways suggests a coordinated response by the bacteria to antibiotic pressure, enhancing their ability to survive and proliferate despite treatment80.
Conclusion
This study offers significant contributions beyond its immediate findings on β-lactamase-mediated resistance in DEC isolates. For researchers, the integration of molecular docking with microbiological and genotypic analysis provides a robust framework to investigate resistance mechanisms at both molecular and phenotypic levels. It sets a precedent for applying computational tools to predict antibiotic-enzyme interactions, which can accelerate the identification of potential drug candidates or structural vulnerabilities in pathogens. The observed cross-resistance patterns and enzyme-substrate dynamics in DEC may guide further research into resistance evolution and horizontal gene transfer, especially in community-acquired infections among pediatric populations.
For clinicians, the study highlights the limitations of commonly used antibiotics like amoxicillin and ceftriaxone in the face of widespread β-lactamase activity. By correlating binding affinity with enzymatic degradation, it emphasizes the importance of using molecular insights to inform empirical treatment choices, particularly in settings with high rates of multidrug resistance. The findings may influence antibiotic selection, dosing decisions, and the prioritization of alternative therapies or combination regimens involving β-lactamase inhibitors.
From a public health and infection control perspective, the high prevalence of MDR strains in children under 36 months points to urgent needs for targeted interventions—such as surveillance programs, early diagnostics, and pediatric-specific antibiotic stewardship strategies. The study’s methodological approach—combining in silico, molecular, and phenotypic data—can be adopted by diagnostic labs or hospital surveillance units to monitor resistance trends in other pathogens like Klebsiella, Salmonella, or Pseudomonas, many of which harbor similar resistance determinants.
Overall, the study bridges clinical microbiology, computational biology, and public health, offering a scalable model for investigating resistance in diverse contexts. Its implications extend to drug discovery, policy-making, and clinical practice—making it a valuable reference for a wide range of stakeholders working to combat antimicrobial resistance.
Limitations of the study
While the findings of this study offer valuable insights into β-lactamase-mediated resistance in DEC isolates, several limitations were present. First, the study was conducted on a relatively limited number of clinical isolates from a specific pediatric population, which may affect the generalizability of the results to broader or more diverse patient groups. Expanding the sample size and including isolates from different geographic regions and age groups could provide a more comprehensive understanding of resistance patterns.
Second, the study focused primarily on β-lactamase enzymes and did not comprehensively assess the role of other resistance mechanisms, such as efflux pumps, porin mutations, or plasmid-mediated gene transfer, which may also contribute significantly to the MDR phenotype. A more holistic approach integrating genomic, transcriptomic, and proteomic data would provide a deeper understanding of the multifactorial nature of resistance. Addressing these limitations in future research will help refine our understanding of antimicrobial resistance and support the development of more targeted and effective therapeutic interventions.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Lin, F. C. et al. Characterization of young infants with fecal carriage of multidrug-resistant Escherichia coli in Southern Taiwan. Pediatr. Neonatol. 65, 138–144 (2024).
Zhou, Y. et al. Characteristics of diarrheagenic Escherichia coli among children under 5 years of age with acute diarrhea: a hospital based study. BMC Infect. Dis. 18, 63 (2018).
Shahbazi, G. et al. Characteristics of diarrheagenic Escherichia coli pathotypes among children under the age of 10 years with acute diarrhea. Gene Rep. 25, 101318 (2021).
Kaderabkova, N. et al. The biogenesis of β-lactamase enzymes. Microbiology (Reading) 168. (2022).
Uzodi, A. S., Lohse, C. M. & Banerjee, R. Risk factors for and outcomes of Multidrug-Resistant Escherichia coli infections in children. Infect. Dis. Ther. 6, 245–257 (2017).
Coleman, J. P., Smith, C. J. M. & Resistance In: XPharm: the Comprehensive Pharmacology Referencepp. 1–3 (Elsevier, 2007).
Yu, D. et al. Antimicrobial resistance in pediatric infectious diseases: antimicrobial resistance, resistance mechanisms and antimicrobial use. Front. Cell. Infect. Microbiol. 13, 1287051 (2023).
Romandini, A. et al. Antibiotic Resistance in Pediatric Infections: Global Emerging Threats, Predicting the Near Future. Antibiotics (Basel) 10. (2021).
Wang, C. Y., Lu, C. Y., Hsieh, Y. C., Lee, C. Y. & Huang, L. M. Intramuscular ceftriaxone in comparison with oral amoxicillin-clavulanate for the treatment of acute otitis media in infants and children. J. Microbiol. Immunol. Infect. 37, 57–62 (2004).
Biner, B. et al. The comparison of single-dose ceftriaxone, five-day azithromycin, and ten-day amoxicillin/clavulanate for the treatment of children with acute otitis media. Turk. J. Pediatr. 49, 390–396 (2007).
Guz, D. et al. Ceftriaxone versus ampicillin for the treatment of community-acquired pneumonia. A propensity matched cohort study. Clin. Microbiol. Infect. 29, 70–76 (2023).
Cusumano, J. A. et al. Penicillin plus ceftriaxone versus ampicillin plus ceftriaxone synergistic potential against clinical Enterococcus faecalis blood isolates. Microbiol. Spectr. 10, e0062122 (2022).
Bush, K. & Bradford, P. A. β-Lactams and β-Lactamase Inhibitors: An Overview. Cold Spring Harb Perspect Med 6. (2016).
World Health. Organization Diarrhoeal Disease (2024).
Kowalski, M. et al. Antimicrobial resistance in enterobacterales infections among children in sub-Saharan africa: a systematic review and meta-analysis. EClinicalMedicine 70, 102512 (2024).
Kotloff, K. L. et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the global enteric multicenter study, GEMS): a prospective, case-control study. Lancet 382, 209–222 (2013).
Ingle, D. J., Levine, M. M., Kotloff, K. L., Holt, K. E. & Robins-Browne, R. M. Dynamics of antimicrobial resistance in intestinal Escherichia coli from children in community settings in South Asia and sub-Saharan Africa. Nat. Microbiol. 3, 1063–1073 (2018).
Koneman, E. W. A.S.J.W.Mycology. In Color Atlas and Textbook of Diagnostic Microbiology, in: n.d.
CLSI Performance Standards for Antimicrobial. Disk Susceptibility Tests, (2024).
Kim, J. et al. Rapid detection of extended spectrum β-Lactamase (ESBL) for Enterobacteriaceae by use of a multiplex PCR-based method. Infect. Chemother. 41, 181 (2009).
Naas, T., Ergani, A., Carrër, A. & Nordmann, P. Real-time PCR for detection of NDM-1 carbapenemase genes from spiked stool samples. Antimicrob. Agents Chemother. 55, 4038–4043 (2011).
Dallenne, C., Da Costa, A., Decré, D., Favier, C. & Arlet, G. Development of a set of multiplex PCR assays for the detection of genes encoding important beta-lactamases in Enterobacteriaceae. J. Antimicrob. Chemother. 65, 490–495 (2010).
Manoharan, A. et al. Phenotypic & molecular characterization of AmpC β-lactamases among Escherichia coli, Klebsiella spp. & Enterobacter spp. From five Indian medical centers. Indian J. Med. Res. 135, 359–364 (2012).
Singh, T. et al. Changing paradigm of antibiotic resistance amongst Escherichia coli isolates in Indian pediatric population. PLoS One. 14, e0213850 (2019).
Singh, T. et al. Transcriptome analysis of beta-lactamase genes in diarrheagenic Escherichia coli. Sci. Rep. 9, 3626 (2019).
Reddy, S. V., Reddy, K. T., Kumari, V. V. & Basha, S. H. Molecular Docking and dynamic simulation studies evidenced plausible immunotherapeutic anticancer property by Withaferin A targeting indoleamine 2,3-dioxygenase. J. Biomol. Struct. Dyn. 33 (12), 2695–2709 (2015).
Yuan, C. & Hao, X. Antibacterial mechanism of action and in Silico molecular Docking studies of Cupressus funebris essential oil against drug-resistant bacterial strains. Heliyon 9(8), e18742 (2023).
Kim, S. et al. PubChem 2019 update: improved access to chemical data. Nucleic Acids Res. 47, D1102–D1109 (2019).
Schrödinger, L. LigPrep, Version 2.8 (Schrödinger, LLC, 2013).
Schrödinger, L. Glide, Version 6.1 (Schrödinger, LLC, 2013).
Sayers, E. W. et al. Database resources of the National center for biotechnology information. Nucleic Acids Res. 50, D20–D26 (2022).
Szklarczyk, D. et al. The STRING database in 2023: protein-protein association networks and functional enrichment analyses for any sequenced genome of interest. Nucleic Acids Res. 51, D638–D646 (2023).
Shannon, P. et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 13, 2498–2504 (2003).
The Gene Ontology Consortium The Gene Ontology Resource. 20 years and still going strong. Nucleic Acids Res. 47, D330–D338 (2019).
Kanehisa, M., Sato, Y., Kawashima, M., Furumichi, M. & Tanabe, M. KEGG as a reference resource for gene and protein annotation. Nucleic Acids Res. 44, D457–D462 (2016).
Tamura, K., Stecher, G. & Kumar, S. MEGA11: molecular evolutionary genetics analysis version 11. Mol. Biol. Evol. 38, 3022–3027 (2021).
Barido-Sottani, J., Chapman, S. D., Kosman, E. & Mushegian, A. R. Measuring similarity between gene interaction profiles. BMC Bioinform. 20, 435 (2019).
Chen, L. et al. Prediction and analysis of essential genes using the enrichments of gene ontology and KEGG pathways. PLoS One. 12, e0184129 (2017).
Prestinaci, F., Pezzotti, P. & Pantosti, A. Antimicrobial resistance: a global multifaceted phenomenon. Pathog Glob Health. 109, 309–318 (2015).
Baquero, F. et al. Evolutionary pathways and trajectories in antibiotic resistance. Clin. Microbiol. Rev. 34, e0005019 (2021).
Munita, J. M. & Arias, C. A. Mechanisms of antibiotic resistance. Microbiol Spectr. 4. https://doi.org/10.1128/microbiolspec.vmbf-0016-2015 (2016).
Smith, B. L., Fernando, S. & King, M. D. Escherichia coli resistance mechanism AcrAB-TolC efflux pump interactions with commonly used antibiotics: a molecular dynamics study. Sci. Rep. 14, 2742 (2024).
Nolivos, S. et al. Role of AcrAB-TolC multidrug efflux pump in drug-resistance acquisition by plasmid transfer. Science 364, 778–782 (2019).
Chaudhary, M. K., Jadhav, I. & Banjara, M. R. Molecular detection of plasmid mediated blatem, blaCTX-M,and BlaSHV genes in extended spectrum β-Lactamase (ESBL) Escherichia coli from clinical samples. Ann. Clin. Microbiol. Antimicrob. 22, 33 (2023).
Ramirez, M. S., Nikolaidis, N. & Tolmasky, M. E. Rise and dissemination of aminoglycoside resistance: the aac(6’)-Ib paradigm. Front. Microbiol. 4, 121 (2013).
Ramírez-Bayard, I. E. et al. Prevalence of Plasmid-Associated Tetracycline resistance genes in Multidrug-Resistant Escherichia coli strains isolated from environmental, animal and human samples in Panama. Antibiotics (Basel) 12, 280 (2023).
Malek Jamshidi, M. R., Zandi, H. & Eftekhar, F. Correlation of quinolone-resistance, Qnr genes and integron carriage in multidrug-resistant community isolates of Klebsiella spp. Iran. J. Basic. Med. Sci. 22, 1387–1391 (2019).
Pourahmad Jaktaji, R. & Mohiti, E. Study of mutations in the DNA gyrase GyrA gene of Escherichia coli. Iran. J. Pharm. Res. 9, 43–48 (2010).
Ortega-Balleza, J. L. et al. G.; Bocanegra-García, V. Genomic Analysis of Multidrug-Resistant Escherichia coli Strains Isolated in Tamaulipas, Mexico. Trop Med Infect Dis 8. (2023).
Karczmarczyk, M., Abbott, Y., Walsh, C., Leonard, N. & Fanning, S. Characterization of multidrug-resistant Escherichia coli isolates from animals presenting at a university veterinary hospital. Appl. Environ. Microbiol. 77, 7104–7112 (2011).
Xiang, Y. et al. Sun, Y. A new plasmid carrying MphA causes prevalence of Azithromycin resistance in enterotoxigenic Escherichia coli serogroup O6. BMC Microbiol. 20, 247 (2020).
Potrykus, J. & Wegrzyn, G. Chloramphenicol-sensitive Escherichia coli strain expressing the Chloramphenicol acetyltransferase (cat) gene. Antimicrob. Agents Chemother. 45, 3610–3612 (2001).
Li, W., Ma, J., Sun, X., Liu, M. & Wang, H. Antimicrobial resistance and molecular characterization of gene cassettes from class 1 integrons in Escherichia coli strains. Microb. Drug Resist. 28, 413–418 (2022).
Yan, C. H. et al. The transcription factor CsgD contributes to engineered Escherichia coli resistance by regulating biofilm formation and stress responses. Int. J. Mol. Sci. 24, 13681 (2023).
Ochoa, S. A. et al. Multidrug- and extensively Drug-Resistant uropathogenic Escherichia coli clinical strains: phylogenetic groups widely associated with integrons maintain high genetic diversity. Front. Microbiol. 7, 2042 (2016).
Shrestha, R. et al. Extended spectrum β-lactamase producing uropathogenic Escherichia coli and the correlation of biofilm with antibiotics resistance in Nepal. Ann. Clin. Microbiol. Antimicrob. 18, 42 (2019).
Qin, J. et al. Conserved FimH mutations in the global Escherichia coli ST131 multi-drug resistant lineage weaken interdomain interactions and alter adhesin function. Comput. Struct. Biotechnol. J. 20, 4532–4541 (2022).
Wang, Y., Liu, B., Grenier, D. & Yi, L. Regulatory mechanisms of the LuxS/AI-2 system and bacterial resistance. Antimicrob. Agents Chemother. 63, e01186-19 (2019).
Zenebe, T. et al. Distribution of ß-Lactamase genes among Multidrug-Resistant and Extended-Spectrum ß-Lactamase-Producing diarrheagenic Escherichia coli from Under-Five children in Ethiopia. Infect. Drug Resist. 16, 7041–7054 (2023).
Wang, Q., Wei, S., Silva, A. F. & Madsen, J. S. Cooperative antibiotic resistance facilitates horizontal gene transfer. ISME J. 17, 846–854 (2023).
Wallace, V. J., Sakowski, E. G., Preheim, S. P. & Prasse, C. Bacteria exposed to antiviral drugs develop antibiotic cross-resistance and unique resistance profiles. Commun. Biol. 6, 837 (2023).
Li, W. et al. Association between antibiotic resistance and increasing ambient temperature in china: an ecological study with nationwide panel data. Lancet Reg. Health West. Pac. 30, 100628 (2023).
Hecky, J. & Müller, K. M. Structural perturbation and compensation by directed evolution at physiological temperature leads to thermostabilization of beta-lactamase. Biochemistry 44, 12640–12654 (2005).
Worthington, R. J. & Melander, C. Combination approaches to combat multidrug-resistant bacteria. Trends Biotechnol. 31, 177–184 (2013).
Tola, M. A., Abera, N. A., Gebeyehu, Y. M., Dinku, S. F. & Tullu, K. D. High prevalence of extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae fecal carriage among children under five years in addis ababa, Ethiopia. PLoS One. 16, e0258117 (2021).
Mansouri, S., Savari, M., Malakian, A. & Abbasi Montazeri, E. High prevalence of multidrug-resistant enterobacterales carrying extended-spectrum beta-lactamase and AmpC genes isolated from neonatal sepsis in ahvaz, Iran. BMC Microbiol. 24, 136 (2024).
Toprak, E. et al. Evolutionary paths to antibiotic resistance under dynamically sustained drug selection. Nat. Genet. 44, 101–105 (2011).
Hain, E., Adejumo, H., Anger, B., Orenstein, J. & Blaney, L. Advances in antimicrobial activity analysis of fluoroquinolone, macrolide, sulfonamide, and Tetracycline antibiotics for environmental applications through improved bacteria selection. J. Hazard. Mater. 415, 125686 (2021).
Safdari, H. et al. Potent and selective inhibitors of class A β-lactamase: 7-prenyloxy coumarins. J. Antibiot. (Tokyo). 67, 373–377 (2014).
Yang, K. B. et al. High-resolution landscape of an antibiotic binding site. Nature 622, 180–187 (2023).
Laws, M., Shaaban, A. & Rahman, K. M. Antibiotic resistance breakers: current approaches and future directions. FEMS Microbiol. Rev. 43, 490–516 (2019).
Soothill, J. S., Ward, R. & Girling, A. J. The IC50: an exactly defined measure of antibiotic sensitivity. J. Antimicrob. Chemother. 29, 137–139 (1992).
Huemer, M., Mairpady Shambat, S., Brugger, S. D. & Zinkernagel, A. S. Antibiotic resistance and persistence-Implications for human health and treatment perspectives. EMBO Rep. 21, e51034 (2020).
Li, Y., Feng, T. & Wang, Y. The role of bacterial signaling networks in antibiotics response and resistance regulation. Mar. Life Sci. Technol. 4, 163–178 (2022).
Jang, S. AcrAB-TolC, a major efflux pump in gram negative bacteria: toward Understanding its operation mechanism. BMB Rep. 56, 326–334 (2023).
Gaurav, A., Bakht, P., Saini, M., Pandey, S. & Pathania, R. Role of bacterial efflux pumps in antibiotic resistance, virulence, and strategies to discover novel efflux pump inhibitors. Microbiology (Reading) 169. (2023).
Hernández-Durán, M. et al. Inside-out, antimicrobial resistance mediated by efflux pumps in clinical strains of acinetobacter baumannii isolated from burn wound infections. Braz. J. Microbiol. 55(4), 3629–3641 (2024).
Revitt-Mills, S. A. et al. Defects in DNA double-strand break repair resensitize antibiotic-resistant Escherichia coli to multiple bacteriodddal antibiotics. Microbiologyopen 11, e1316 (2022).
Yakovlieva, L., Fülleborn, J. A. & Walvoort, M. T. C. Opportunities and challenges of bacterial glycosylation for the development of novel antibacterial strategies. Front. Microbiol. 12, 745702 (2021).
Deter, H. S., Hossain, T. & Butzin, N. C. Antibiotic tolerance is associated with a broad and complex transcriptional response in E. coli. Sci. Rep. 11, 6112 (2021).
Acknowledgements
The Council of Scientific and Industrial Research (CSIR), Pusa, New Delhi, India is acknowledged for providing Fellowship [08/532(0007)/2011-EMR-I] to Dr. Taru Singh. The authors wish to thank all the children and their parents for providing the samples.
Funding
No funding was available to conduct the study.
Author information
Authors and Affiliations
Contributions
TS and SD conceived and designed the study, analysed/interpreted results. TS, and CS collected the samples. TS, CS, SS, and SD collected the data. TS, and CS performed experiments and analyzed the data. TS, and SS carried out the literature search. TS, CS, and SS wrote the manuscript. SD performed manuscript editing. TS, SS, and SD supervised the study and revised the final version of the manuscript. All authors read and approved of the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the “Institutional Ethics Committee—Human Research (IEC-HR) University College of Medical Sciences, University of Delhi, New Delhi in accordance with WHO guidelines.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Singh, T., Shekhar, C., Singh, S. et al. Integrating computational approaches to uncover β-lactamase-associated resistance in diarrheagenic Escherichia coli from pediatric patients. Sci Rep 15, 30921 (2025). https://doi.org/10.1038/s41598-025-16122-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-16122-1