Abstract
Brucellosis, a significant zoonotic infectious disease caused by Brucella spp., necessitates the development of efficient, rapid, accurate, and cost-effective diagnostic methods. This study evaluated the diagnostic value of Brucella Type IV secretion proteins VirB1, VirB5, and VirB6 for human brucellosis serological diagnosis. A total of 100 positive serum samples, 96 negative serum samples, and 27 serum samples from patients with fever caused by other pathogens were collected. Recombination VirB1 (rVirB1), rVirB5, and rVirB6 were expressed using prokaryotic expression systems, while VirB2 and VirB7 were synthesized as peptides. An indirect ELISA method was established using purified proteins and synthetic peptides, with sensitivity, specificity, AUC, and cut-off values determined through ROC analysis. The study successfully prepared rVirB1 (~ 36 kD, purity 90.6%), rVirB5 (~ 32 kD, purity 90.3%), and rVirB6 (~ 28 kD, purity 94.9%). These proteins exhibited sensitivity and specificity exceeding 0.9500 and 0.9271, respectively, comparable to traditional LPS antigens. Cross-reactivity assessments revealed that rVirB1 exhibited cross-reactivity with Pseudomonas putrida, while rVirB5 and rVirB6 showed no cross-reactivity. In contrast, LPS exhibited 14 instances of cross-reactivity. This study successfully developed an indirect ELISA diagnostic method using rVirB1, rVirB5, and rVirB6, demonstrating high diagnostic accuracy comparable to traditional LPS antigen detection techniques. Although some cross-reactivity was observed, the method presents a promising new candidate for the serological diagnosis of brucellosis. Future research should focus on optimizing this method to enhance diagnostic specificity and reliability.
Similar content being viewed by others
Introduction
Brucellosis is a significant zoonotic infectious disease caused by Brucella spp1. This disease is transmitted to humans through direct contact with infected animals or their secretions and excretions, or by ingesting contaminated animal products2. Globally, brucellosis is widely distributed, particularly in developing countries, posing a substantial challenge to public health3. The clinical manifestations of brucellosis are diverse and nonspecific, complicating diagnosis4. Common symptoms in humans include prolonged fever, sweating, fatigue, joint pain, hepatosplenomegaly, and lymphadenopathy5. Additionally, the reproductive system may be affected, with male patients experiencing orchitis or epididymitis, which is characterized by testicular pain and swelling and can severely impact fertility6. Female patients may experience menstrual irregularities, amenorrhea, or pelvic inflammatory disease7. Since the symptoms of brucellosis resemble those of other diseases, such as tuberculosis and rheumatism, misdiagnosis or delayed diagnosis is common8. Therefore, enhancing the diagnostic process for brucellosis is crucial. This not only facilitates the timely detection and treatment of cases, reducing disease transmission, but also contributes to public health security and socio-economic stability.
Traditional diagnostic methods for brucellosis primarily include serological tests, molecular techniques, and bacterial culture9,10. Serological tests identify Brucella antibodies in patient serum to assist in diagnosis11, while bacterial culture is considered the “gold standard” for confirming Brucella infection12. However, bacterial culture is complex; it requires specialized culture media and can take several weeks to produce results, which limits its widespread application in clinical practice13. Given these limitations, the development of an efficient, rapid, accurate, and cost-effective diagnostic method is essential.
VirB proteins are crucial components of the Brucella Type IV secretion system (T4SS)14. The T4SS is a complex structure composed of multiple proteins, and the VirB protein family includes members from VirB1 to VirB12, which work closely together in both structure and function15. Although VirB proteins play a significant role in the pathogenesis and biological functions of Brucella, research on their potential application in the serological diagnosis of human brucellosis is relatively limited. A systematic analysis of the potential of VirB proteins in serological diagnosis not only aids in the development of new diagnostic tools but also offers innovative strategies for the prevention and control of brucellosis. Therefore, conducting in-depth research on the immunological characteristics of VirB proteins and their application in serological diagnosis holds great scientific and practical significance.
In previous studies16, we utilized proteomics to identify six proteins (VirB3-4, 8–11) that are highly expressed in wild-type Brucella abortus strains, demonstrating their potential value in the serological diagnosis of human brucellosis. However, other T4SS proteins, which exhibited no expression differences between wild-type and vaccine strains, were not investigated. Therefore, this study aims to evaluate the remaining VirB proteins using indirect enzyme-linked immunosorbent assay (ELISA), providing a reference for the development of serological diagnostic antigens for brucellosis.
Materials and methods
Serum samples
A total of 100 brucellosis positive serum samples and 96 brucellosis negative serum samples were obtained from the Xuzhou Center for Disease Control and Prevention. All samples were confirmed as positive or negative using the standard tube agglutination test. Additionally, 27 serum samples from patients with fever (non-brucellosis) caused by other pathogens were utilized to evaluate the cross-reactivity of the developed methods.
Preparation of Recombinant T4SS proteins
The amino acid sequences of the VirB proteins were selected based on relevant literature17 and the NCBI protein database. The sequences of VirB1, VirB2, VirB5, VirB6, and VirB7 were analyzed using the UniProt website (https://www.uniprot.org/uniprotkb), and transmembrane regions, signal peptides, and hydrophobic regions were removed. Following a comprehensive evaluation, VirB1, VirB5, and VirB6 were expressed using prokaryotic expression systems, while VirB2 and VirB7 were synthesized as peptides (see Table 1).
Peptide synthesis
Peptide synthesis was outsourced to a professional peptide synthesis company (Beijing Protein Innovation Co., Ltd.). During the synthesis process, reaction conditions—including temperature, reaction time, and reagent concentration—were meticulously controlled. After each synthesis step, the purity of the peptides was assessed using high-performance liquid chromatography (HPLC, Agilent 1260, USA) to ensure a purity level exceeding 90%. The synthesized VirB2 and VirB7 peptides were then conjugated with keyhole limpet hemocyanin (KLH, Sigma) as a carrier. Following conjugation, unreacted reagents and impurities were removed through dialysis to obtain the final VirB2-KLH and VirB7-KLH conjugates.
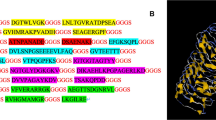
Prokaryotic expression
Based on the amino acid sequences of VirB1, VirB5, and VirB6 listed in Table 1, linkers (“GGGS”) were incorporated between adjacent sequences. Codon optimization was conducted to facilitate prokaryotic expression, and a 6xHis tag was appended to the 3’ end for subsequent protein purification. The recombinant protein genes were synthesized by Beijing Protein Innovation Co., Ltd. These synthesized genes were then cloned into the pET30a expression vector and transformed into BL21 cells for IPTG-induced expression. The specific steps were as follows: BL21 competent cells, stored at −80 °C, were thawed on ice and mixed with pET30a(+) before being incubated on ice for 30 min. The mixture underwent a heat shock at 42 °C for 90 s, followed by immediate cooling on ice for 2 min. Subsequently, 800 µL of LB medium (L113084, Aladdin, USA) was added, and the mixture was incubated at 37 °C for 45 min. The cells were centrifuged at 5000 rpm for 3 min, and most of the supernatant was discarded, leaving approximately 100–150 µL to resuspend the cells. The suspension was plated on an LB agar plate containing the 50 µg/mL of Kanamycin and cultured overnight at 37 °C. The cultured bacterial suspension was then transferred to 250 mL of LB liquid medium containing the corresponding antibiotics and incubated at 37 °C with shaking at 200 rpm until the optical density at 600 nm (OD600) reached 0.6–0.8. The cells were induced with 0.5 mM IPTG (16758, Sigma, Germany) at 37 °C for 4 h. Following this, the cells were collected by centrifugation at 8000 rpm for 6 min, and the pellet was resuspended in 20–30 mL of 10 mM Tris-HCl (pH 8.0) solution and sonicated (500 W, 180 cycles, with each cycle consisting of 5 s on and 5 s off). A 100 µL aliquot of the lysed bacterial suspension was centrifuged at 12,000 rpm for 10 min, and 50 µL of the supernatant was transferred to another EP tube. The pellet was resuspended in 50 µL of 10 mM Tris-HCl (pH 8.0) solution. A 12% SDS-PAGE (P0012AC, Beyotime, Shanghai, China) was performed to determine whether the target protein was present in the supernatant or the pellet for subsequent purification.
The nickel column (Ni Sepharose 6 Fast Flow, GE Healthcare) was washed with deionized water until the pH reached 7.0, and then equilibrated with approximately 100 mL of 10 mM Tris-HCl (pH 8.0, T3253, Sigma, Germany). The chromatography column was further equilibrated with about 50 mL of a 10 mM Tris-HCl (pH 8.0) solution containing 0.5 M NaCl (A501218-0001, Sangon Biotech, Shanghai, China). The sample containing the target protein was diluted and loaded onto the column. After loading, the column was washed with a 10 mM Tris-HCl (pH 8.0) solution containing 0.5 M NaCl. Proteins were eluted using 10 mM Tris-HCl (pH 8.0) solutions containing 15 mM, 60 mM, and 300 mM imidazole (with 0.5 M NaCl). Protein peaks were collected and analyzed for purification efficiency using 12% SDS-PAGE. Protein quantification was performed using a BCA protein assay kit (P0010, Beyotime). It is important to note that no dialysis was performed during the purification process, as the proteins were expressed in a soluble form.
The purified protein was verified using Western blot (WB), following these steps: First, the samples were mixed with Loading Buffer at a 1:1 ratio and heated at 95 °C for 5 min to denature the proteins. Next, a 10% SDS-PAGE gel was prepared using the One-Step Fast PAGE Gel Casting Kit (G2177-50T), and the gel was run at 200 V for 35 min in SWE Rapid High-Resolution Electrophoresis Buffer after loading the protein samples and Prestained Protein Marker IV (8-200 kDa, G2083-250UL). Following electrophoresis, the gel was transferred to a membrane using Ice-free Rapid Transfer Buffer at a constant current of 400 mA for 25 min. The membrane was then washed three times with TBS-T for 5 min each. Afterward, the membrane was blocked with 5% skim milk in TBS-T at room temperature for 1 h and washed again with TBS-T three times for 5 min each. Subsequently, the membrane was incubated with Recombinant Anti-His Tag antibody (Mouse mAb, GB151251-100) diluted according to the manufacturer’s instructions (typically 1:1000-1:5000) at 4 °C overnight or at room temperature for 2 h, followed by three 5-minute washes with TBS-T. Next, the membrane was incubated with HRP-conjugated Goat anti-Mouse IgG (typically 1:5000-1:10000, GB23301) at room temperature for 1 h and washed three times with TBS-T for 5 min each. Finally, the membrane was placed in Substrate Solution for color development in the dark for 5–10 min, and the reaction was terminated with water to observe the bands. All reagents were purchased from Wuhan Servicebio Technology Co., Ltd (China).
Establishment of indirect ELISA for serum detection
The indirect enzyme-linked immunosorbent assay (iELISA) was performed as follows: Purified proteins and synthetic peptides were diluted to a concentration of 10 µg/mL in carbonate buffer solution (CBS, pH 9.6), and 100 µL of this solution was added to each well of a 96-well microplate (Corning, USA). The plate was incubated overnight at 4 °C. After washing the wells three times with PBST, 300 µL of blocking solution (5% skim milk in PBS) was added to each well and incubated at 37 °C for 2 h. The plate was washed again with PBST, and human serum diluted in PBS (1:200) was added, followed by incubation at 37 °C for 1 h. After three additional washes with PBST, 100 µL of HRP-conjugated rabbit anti-human IgG (diluted 1:10,000, A18903, Thermo Fisher Scientific, USA) was added to each well and incubated at 37 °C for 1 h. The plate was washed three times with PBST, and tetramethylbenzidine (TMB, T2573, TCI, Japan) substrate solution was added, followed by incubation in the dark for 10 min to allow color development. The reaction was terminated with 2M H2SO4, and the optical density at 450 nm (OD450) was measured using a microplate reader (Versa Max Microplate Reader, Molecular Devices, USA).
In the iELISA assay, the positive controls used were serum samples from patients previously confirmed to be positive for brucellosis by standard tube agglutination tests. The negative controls were serum samples from healthy individuals who had no history of brucellosis or exposure to Brucella spp. Additionally, LPS (provided by the Chinese Animal Health and Epidemiology Center, 3 mg/mL) served as a positive antigen control. Each serum sample was measured in triplicate using the same procedure. Sensitivity, specificity, area under the curve (AUC), and cut-off values were determined through receiver operating characteristic (ROC) analysis.
Assessment of Cross-Reactivity via indirect ELISA
The cross-reactivity of the Brucella T4SS recombinant proteins was assessed using serum samples from patients with fever who did not have brucellosis, in comparison to LPS. Cross-reactivity was evaluated via iELISA as above and based on the cutoff values determined by the ROC curve.
Statistical methods
Dot plots and ROC curve analyses were performed using GraphPad Prism version 6.05. Statistical analyses were conducted using unpaired Student’s t-tests, with a significance level set at P < 0.05.
Results
Expression and purification of Recombinant T4SS proteins
The rVirB1 (molecular weight ~ 36 kDa, purity 90.6%), rVirB5 (~ 32 kDa, purity 90.3%), and rVirB6 (~ 28 kDa, purity 94.9%) were successfully expressed and purified, with all proteins achieving a purity exceeding 90% (Fig. 1 and Supporting material 1).
Results of iELISA
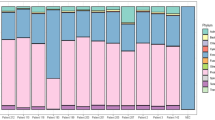
Based on the ROC curve, the cut-off values for the three proteins were calculated using the Youden index. The diagnostic accuracy of the proteins, ranked from highest to lowest, was as follows: rVirB1, rVirB5, and rVirB6. The AUC values for these proteins were 0.9948, 0.9855, and 0.9808, respectively, while the AUC for LPS was 0.9999. And rVirB1 demonstrated a sensitivity of 0.9900 (95% CI: 0.9455 to 0.9997) and a specificity of 0.9479 (95% CI: 0.8838 to 0.9776); rVirB5 showed a sensitivity of 0.9500 (95% CI: 0.8882 to 0.9785) and a specificity of 0.9375 (95% CI: 0.8703 to 0.9710); rVirB6 had a sensitivity of 0.9500 (95% CI: 0.8882 to 0.9785) and a specificity of 0.9271 (95% CI: 0.8571 to 0.9642); LPS had a sensitivity of 0.9900 (95% CI: 0.9455 to 0.9997), and a specificity of 1.000 (95% CI: 0.9623 to 1.000). Although the sensitivity and specificity of the three proteins were slightly lower than those of LPS, they still demonstrated good performance in diagnosing brucellosis. The results are presented in Table 2; Fig. 2 and Supporting material 2.
IELISA Analysis of Human Serum Samples. (A) Dot plot of human serum samples showing optical density (OD) values from the indirect ELISA. Positive samples are in red, and negative samples are in blue. The cut-off value (dashed line) is determined using the Youden index from the ROC analysis. (B) ROC analysis of human serum samples illustrates the diagnostic performance of recombinant VirB proteins, with AUC values of 0.9948 for rVirB1, 0.9855 for rVirB5, and 0.9808 for rVirB6. The ROC curve demonstrates high sensitivity and specificity in distinguishing positive from negative samples, with the cut-off value marked and sensitivity and specificity values listed in the table below.
Additionally, we synthesized two peptides, VirB2 and VirB7, to evaluate their potential as diagnostic antigens. However, preliminary analysis using 16 positive and 16 negative serum samples showed that the AUC values for VirB2 and VirB7 were 0.6445 and 0.5898, respectively. These results indicated that these peptides did not demonstrate sufficient diagnostic value to distinguish between positive and negative serum samples. Therefore, further testing on additional samples was not pursued for these peptides. The partial serum test results for VirB2 and VirB7 are provided in Supporting material 2.
Cross-Reactivity assessment
Using the iELISA method and the established cut-off values, cross-reactivity was assessed with rVirB1, rVirB5, and rVirB6 in 27 serum samples from patients with fever who did not have brucellosis. The results indicated 1, 0, and 0 cases of cross-reactivity, respectively. Notably, rVirB1 exhibited cross-reactivity with Pseudomonas putrida, while rVirB5 and rVirB6 showed no cross-reactivity. Additionally, cross-reactivity with LPS was observed in 11 cases, which included 5 instances of Escherichia coli, 1 case each of Klebsiella pneumoniae, Enterococcus faecalis, Haemophilus influenzae, Moraxella osloensis, Pseudomonas aeruginosa, and Staphylococcus aureus (Supporting material 2).
Discussion
Indirect ELISA is a cost-effective method compared to advanced techniques like PCR or next-generation sequencing, making it suitable for resource-limited areas where brucellosis is endemic. This straightforward method can be scaled for high-throughput screening, benefiting large-scale epidemiological studies and public health surveillance. Unlike bacterial culture, which poses biohazard risks from live pathogens, indirect ELISA uses purified proteins or peptides, reducing infection risks. It can also be adapted for multiplexing, allowing simultaneous detection of antibodies against multiple antigens, enhancing diagnostic accuracy. In this study, we developed an indirect ELISA using recombinant VirB proteins (rVirB1, rVirB5, and rVirB6) for diagnosing human brucellosis. Indirect ELISA offers rapid results-typically within hours-compared to the weeks needed for bacterial culture, making it crucial for timely diagnosis and treatment in clinical settings.
The T4SS is a vital virulence factor of Brucella, consisting of 12 protein complexes (VirB1 to VirB12) encoded by the VirB region18,19. Research has explored the potential of VirB proteins for vaccine development and serological diagnosis. For instance, Yin et al.20 identified antigenic epitopes of VirB8 and VirB10 using immunoinformatics, screening for various T and B cell epitopes to develop a multi-epitope vaccine. However, studies primarily focus on individual VirB proteins and lack a comprehensive analysis of their role in brucellosis diagnosis.
In our previous study16, we analyzed six highly expressed VirB proteins (VirB3, VirB4, VirB8, VirB9, VirB10, and VirB11) in wild-type Brucella strains for diagnosing human brucellosis. Recombinant forms were prepared and evaluated using an indirect ELISA method, showing high sensitivity and specificity with AUC values over 0.95. rVirB3 and rVirB4 had the highest accuracy, with AUCs of 0.9979 and 0.9914, respectively, comparable to traditional tests. In this study, we prepared three additional recombinant proteins (rVirB1, rVirB5, and rVirB6) and synthesized two peptides (VirB2 and VirB7). The recombinant proteins showed high diagnostic performance, while the peptides lacked sufficient value, possibly due to structural issues and a limited sample size (16 positive and 16 negative serum samples), resulting in low AUCs (0.6445 for VirB2 and 0.5898 for VirB7). These results indicate that recombinant VirB proteins are promising diagnostic antigens, while the peptides need optimization. Future research should focus on improving peptide structure or exploring other VirB antigens. Our findings suggest rVirB3 is the most effective for serological diagnosis, followed by rVirB1 and rVirB4, all exceeding AUCs of 0.9. Despite slightly lower performance than traditional tests, these proteins are valuable diagnostic tools reflecting Brucella infection status with significant clinical potential. As key components of the Brucella T4SS, VirB proteins enhance the pathogen’s virulence and host cell interaction21,22, making them valuable diagnostic antigens that accurately reflect Brucella infection status and hold significant clinical potential.
This study found differences in the diagnostic performance of various VirB proteins. rVirB1 had the highest accuracy, while rVirB5 and rVirB6 showed slightly lower sensitivity, likely due to their specific roles and expression levels in the Brucella lifecycle23. Antigenicity may also be affected by amino acid sequences, spatial conformation, and glycosylation modifications24,25. Future research should explore the antigenic epitopes of these proteins and optimize their structures for improved diagnostic performance. In prior experiments, we assessed six proteins: rVirB3, rVirB4, rVirB9, rVirB8, rVirB11, and rVirB10. The diagnostic performance of rVirB1, rVirB5, and rVirB6 in identifying human brucellosis was comparable to or superior to that of the initial six proteins, indicating potential limitations in the TMT proteomics method for selecting diagnostic antigens, which requires further verification and optimization.
Cross-reactivity is vital for evaluating the specificity of diagnostic antigens26. In this study, rVirB1 showed some cross-reactivity, but its frequency and intensity were lower than LPS. In contrast, rVirB5 and rVirB6 exhibited no cross-reactivity in 27 serum samples from febrile patients without brucellosis, indicating high specificity. The cross-reactivity of rVirB1 may result from shared antigenic epitopes with other pathogens, leading to false positives. Conversely, rVirB5 and rVirB6 have unique epitopes specific to Brucella. Variations in expression levels and post-translational modifications can also affect antigenicity; rVirB1 may have modifications that increase cross-reactivity. Thus, VirB proteins may help minimize cross-reactivity as diagnostic antigens. However, broader assessments are necessary to evaluate their specificity in practical applications.
TMT proteomics studies have shown no significant differences in the expression levels of VirB1, VirB2, and VirB5-VirB7 between the vaccine strain Brucella abortus A19 and the wild-type strain Brucella abortus DT21. However, further investigation into the diagnostic potential of these proteins in human brucellosis is essential. This study provides strong evidence that T4SS proteins are critical to the infection process and offers a foundation for developing new diagnostic antigens. Additional research is needed for the clinical application of VirB proteins. In summary, VirB proteins demonstrate significant potential for serological diagnosis of brucellosis, and future studies should explore their antigenicity and diagnostic efficacy to improve diagnostic methods.
Despite these advantages, our study has several limitations. The sample size was relatively small, which may limit the generalizability of our findings. Additionally, cross-reactivity observed with rVirB1 highlights the need for further optimization of the purification process and antigen selection to enhance diagnostic specificity. The presence of residual Escherichia coli proteins in the purified samples, despite achieving over 90% purity, could contribute to non-specific binding and cross-reactivity. Future studies should aim to further optimize the purification process to minimize the presence of contaminating proteins and reduce cross-reactivity. A broader and more diverse set of samples should be used to thoroughly evaluate the specificity of these proteins in practical applications.
Conclusion
This study successfully developed an indirect ELISA method using recombinant VirB proteins (rVirB1, rVirB5, and rVirB6) for the serological diagnosis of human brucellosis. The method demonstrated high diagnostic accuracy, comparable to traditional LPS antigen detection techniques. While our results are encouraging, the study’s limitations, including the small sample size and observed cross-reactivity, suggest that further validation is needed. Future research should focus on optimizing the method to enhance diagnostic specificity and reliability. The development of this method represents a promising step forward in the serological diagnosis of brucellosis.
Data availability
No datasets were generated or analysed during the current study.
References
Qureshi, K. A. et al. Brucellosis: epidemiology, pathogenesis, diagnosis and treatment-a comprehensive review. Ann. Med. 55, 2295398 (2023).
Khurana, S. K. et al. Bovine brucellosis - a comprehensive review. Vet. Q. 41, 61–88 (2021).
Jin, M. et al. Research progress on complications of brucellosis. Front. Cell. Infect. Microbiol. 13, 1136674 (2023).
Liu, Z., Gao, L., Wang, M., Yuan, M. & Li, Z. Long ignored but making a comeback: a worldwide epidemiological evolution of human brucellosis. Emerg. Microbes Infect. 13, 2290839 (2024).
Moriyón, I., Blasco, J. M., Letesson, J. J., De Massis, F. & Moreno, E. Brucellosis and one health: inherited and future challenges. Microorganisms 11, 2070 (2023).
Ma, X. et al. Brucellosis infection complicated with myelitis: a case report and literature review. Front. Cell. Infect. Microbiol. 14, 1378331 (2024).
Liu, B. et al. Epidemiology, clinical manifestations, and laboratory findings of 1,590 human brucellosis cases in ningxia, China. Front. Microbiol. 14, 1259479 (2023).
Shi, Q. N. et al. Incidence and warning signs for complications of human brucellosis: a multi-center observational study from China. Infect. Dis. Poverty. 13, 18 (2024).
Franco, M. P., Mulder, M., Gilman, R. H. & Smits, H. L. Human brucellosis. Lancet Infect. Dis. 7, 775–786 (2007).
Legesse, A. et al. Comparative evaluation of RBPT, I-ELISA, and CFT for the diagnosis of brucellosis and PCR detection of Brucella species from Ethiopian sheep, goats, and cattle Sera. BMC Microbiol. 23, 216 (2023).
Loubet, P. et al. Diagnosis of brucellosis: combining tests to improve performance. PLoS Negl. Trop. Dis. 18, e0012442 (2024).
Kiambi, S. G., Fèvre, E. M., Omolo, J., Oundo, J. & de Glanville, W. A. Risk factors for acute human brucellosis in ijara, north-eastern Kenya. PLoS Negl. Trop. Dis. 14, e0008108 (2020).
Edao, B. M. et al. Whole genome sequencing of Ethiopian Brucella abortus isolates expands the known diversity of an early branching sub-Saharan African lineage. Front. Microbiol. 14, 1128966 (2023).
Xiong, X. et al. The virb system plays a crucial role in Brucella intracellular infection. Int. J. Mol. Sci. 22, 13637 (2021).
Rouot, B. et al. Production of the type IV secretion system differs among Brucella species as revealed with VirB5- and VirB8-specific antisera. Infect. Immun. 71, 1075–1082 (2003).
Wu, Q. et al. Preparation and evaluation of Brucella T4SS Recombinant proteins in serodiagnosis of human brucellosis based on TMT-based proteomics technology. Front. Cell. Infect. Microbiol. 14, 1514046 (2025).
Borghesan, E. et al. A Brucella effector modulates the Arf6-Rab8a GTPase cascade to promote intravacuolar replication. EMBO J. 40, e107664 (2021).
Yin, Y., Tian, M., Zhang, G., Ding, C. & Yu, S. A novel Brucella T4SS effector RS15060 acts on bacterial morphology, lipopolysaccharide core synthesis and host Proinflammatory responses, which is beneficial for Brucella melitensis virulence. Microbiol. Res. 292, 128015 (2025).
Jiao, H. et al. The mechanism of facultative intracellular parasitism of Brucella. Int. J. Mol. Sci. 22, 3673 (2021).
Yin, Z. et al. Design of multi-epitope vaccine candidate against Brucella type IV secretion system (T4SS). PLoS One. 18, e0286358 (2023).
Potemberg, G. et al. Genome-wide analysis of Brucella melitensis genes required throughout intranasal infection in mice. PLoS Pathog. 18, e1010621 (2022).
Wang, J. et al. Upregulation of TREM2 expression in M2 macrophages promotes Brucella abortus chronic infection. Front. Immunol. 15, 1466520 (2024).
Li, C. et al. The Brucella effector BspI suppresses inflammation via Inhibition of IRE1 kinase activity during Brucella infection. J. Immunol. 209, 488–497 (2022).
Costa, T. R. D. et al. Type IV secretion systems: advances in structure, function, and activation. Mol. Microbiol. 115, 436–452 (2021).
Jakob, S. et al. The virulence regulator virb from Shigella flexneri uses a CTP-dependent switch mechanism to activate gene expression. Nat. Commun. 15, 318 (2024).
Chan, K. R. et al. Serological cross-reactivity among common flaviviruses. Front. Cell. Infect. Microbiol. 12, 975398 (2022).
Funding
This work was supported by Xuzhou Science and Technology Bureau (Grant number KC23306), the Medical Research Program of Jiangsu Commission of Health (Grant number Z2023080), QingLan Project of Jiangsu Province (2024). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
LW, SZ and DY conceived and designed the study. SZ and MY performed the assays and drafted the manuscript. XQ, QP and YC were analyzed the data. LW and DY reviewed and made improvements for the manuscript. All authors approved the final version of the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval statement
All methods were carried out in accordance with the Declaration of Helsinki. The study was reviewed and approved by the Ethics Committee of Xuzhou Medical University (approved number: xzhmu-2024Z052) and informed consent was obtained from all subjects.
Supplementary Information
Supporting material 1. Original images for Fig. 1.
Supporting material 2. Raw data for I-ELISA.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, L., Zhao, S., Qi, X. et al. Application of Brucella type IV secretion proteins VirB1, VirB5, and VirB6 in the serological diagnosis of brucellosis. Sci Rep 15, 31389 (2025). https://doi.org/10.1038/s41598-025-16590-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-16590-5