Abstract
Acute febrile illness (AFI) is a common cause of pediatric hospital visits in developing countries. Identifying the broad range of pathogens that can cause fever is critical to: improving AFI management, preventing unnecessary prescriptions, and guiding public health interventions. Between March 2020 and December 2021, 436 children in Mwanza, Tanzania were enrolled with acute fever lasting < 7 days. Malaria MRDT and microscopy, dengue rapid NSI antigen, dengue serology, chikungunya serology, urinalysis, blood and urine cultures were conducted. Multiplex reverse-transcriptase-polymerase-chain-reaction-ELISAs (m-RT-PCR-ELISA) were also performed for malaria, dengue virus type 1–4, Zika virus, chikungunya virus, yellow fever virus, Rift Valley fever virus, and West Nile virus. Nasopharyngeal swabs obtained from 77 children were used to identify respiratory pathogens using a multiplex PCR panel. Bacteria or viruses in the bloodstream, urinary and upper respiratory tracts were identified in 26/436 (6%), 47/436 (10.8%), and 33/77 (43%) of the participants, respectively. Pneumonia was diagnosed in 59/436 cases and confirmed in 8 by chest X-ray. The majority of isolates recovered from the bloodstream and upper respiratory tract were resistant to antibiotics commonly used clinically. Those organisms were most commonly found in cases of AFI. To conclude, there is an urgent need for point-of-care diagnostic assays for AFI that strengthen existing infection prevention interventions and evidence-based antimicrobial stewardship programs.
Similar content being viewed by others
Introduction
Two-thirds of 2.6 million pediatric infectious disease deaths occur annually in Sub-Saharan Africa (SSA)1. The majority are preventable with appropriate and timely management. Parasitic, bacterial and viral infections often present as acute febrile illness (AFI); fever is the most common symptom accounting for approximately one billion episodes annually worldwide2,3. The symptoms and differential diagnoses of these illnesses display significant similarities making accurate identification of the etiologic agent difficult without laboratory confirmation4,5. There has been a change in the epidemiology of AFI in African children compared to 15 years ago when malaria was the most likely cause4,5,6. Non-malarial febrile illnesses are important causes of morbidity and mortality even in areas where malaria is endemic7,8,9,10.
Co-infections along with multiple outbreaks of emerging and re-emerging arboviral infections in Africa have doubled the burden. Factors associated with this expanded burden include urbanization, global travel and, importantly, climate change11,12. Climate change plays an important role in the adaptation of disease-carrying organisms, and the expansion of vector-borne diseases, e.g., malaria, dengue, and Zika fever, into previously unaffected areas. This expansion has been attributed to a variety of factors that include environmental changes associated with increasing temperature, which affect mosquito physiology and the rate of mosquito growth, population size and survival13. Rainfall and humidity are also important factors14.
Given the diagnostic challenges in identifying the causes of AFI in children, the majority of cases are diagnosed clinically and provided empirical treatment with antibiotics or anti-malarial drugs4,10,15. The lack of diagnostic tools needed to provide timely and accurate results hinders a more targeted approach to treatment16. In the absence of specific diagnostic tests, empirical treatment must be guided in an effort to reduce morbidity and to prevent further development of antimicrobial resistance. Resistance is exacerbated by the limited capacity to perform laboratory analysis and sensitivity assays for common infections. Studies conducted in four African countries: Tanzania, Kenya, Uganda and Zambia, found adequate capacity was mainly present in tertiary and a few regional hospitals, but the availability of diagnostic tools was limited in many areas of Africa17.
Studies dedicated to the causes of AFI were conducted more than 10 years ago in Tanzania; these focused mainly upon hospitalized children below 5 years-of-age18,19,20. Reliable data for viral infections, and both emerging and reemerging diseases are lacking. This is especially true of data that consider a change in epidemiologic disease patterns due to climate change7,21. Information concerning the causes of fever, which is based upon diagnostic approaches that use both clinical presentation and laboratory confirmation, is critical for the correct management of these children.
Our recent study demonstrated that 80% of the study participants had neither malaria nor a dengue virus infection22. Investigating other causes of fever is paramount to providing epidemiological data that can guide empirical treatment of AFI. In the current study, blood and urine samples, dried blood spots, and nasal swabs were collected in an effort to identify potential AFI pathogens. The goal was to gain a better understanding of the epidemiological landscape of the relevant pathogens causing fever in children in the Lake Victoria region of Mwanza, Tanzania.
Methods
Study location
This study was conducted at Bugando Medical Centre (BMC), Sekou Toure Regional Referral Hospital (STRRH), Nyamagana District Hospital (NDH), Sengerema Designated District Hospital (SDDH), and Buzuruga Health Centre (BHC), all located within the Mwanza Region of Tanzania. Mwanza is the second largest urban metropolitan area, found in Northwestern Tanzania on the southern shores of Lake Victoria. According to the 2022 national census, Mwanza has a population of 3,104,521 people, a more detailed description of the study site was provided in our previous publication. BMC is the main teaching hospital of the Catholic University of Health and Allied Sciences (CUHAS), as well as for the Tertiary Referral Hospital for the Northwestern Tanzania, which serves ~ 18 million people. Approximately 60,000 children are seen annually by the pediatric departments on an inpatient (17,000) and outpatient (43,000) basis, ~ 40% present with acute fever in the Lake Victoria region. The children screened and included in this study came from the Mwanza Region, one of eight regions in northern Tanzania. Neonates, young infants ≤ 2 months-of-age and surgical patients were not included in this study. Participants were recruited during working hours on Mondays, Wednesdays and Fridays.
Study design and recruitment of the participants
This cross-sectional periodic prevalence and analytical study involving children ranging from 1 to ≤ 12 years-of-age was conducted between March 2020 and December 2021, a period that correlates with the disease seasonality. Arborvirus infections like dengue fever and acute respiratory infections tend to be more prevalent during rainy seasons in tropical areas. The study enrolled children who met presumptive malaria or dengue virus infections designated by WHO23,24. The children presented with an acute onset of high-grade fever (> 38 °C) lasting less than 7 days and at least one of the following symptoms: (1) vomiting, (2) headache, (3) rash or (4) joint pain. Patients with critical conditions that required intensive critical care, e.g., trauma or acute injury, or incomplete data (e.g., missing height/length or weight measurements) were excluded from the study (Fig. 1). The hospitals involved were divided into two groups during participant enrollment. The first group included higher tier hospitals: the tertiary and regional referral hospitals, i.e., BMC and STRRH, respectively. The second group was composed of lower tier hospitals that included two district hospitals and a health center: SDDH, NDH and BHC. All participants enrolled at the tertiary hospitals were inpatients admitted following collection of clinical samples. This study enrolled the same cohort of children who 80% had no known cause/correlation of acute fever episodes22. Screening was based upon the number of children seen at each of five study sites. Random sampling did not occur throughout the entire Mwanza region/lake Victoria region nor outside clinical pediatric settings (excluding neonatal and surgical clinics).
Flow diagram: study participants enrolled at five healthcare facilities in Mwanza, Tanzania. *Tests routinely available in this study. **Test obtained as part of the Provider initiated HIV Testing and Counseling (PITC) per Tanzania Guideline. Key: RDT, rapid diagnostic test; IgG, immunoglobulin G; IgM, immunoglobulin M; BS, blood microscopy; PCR, polymerase chain reaction; CHIKV, chikungunya virus; YFV, yellow fever virus; ZIKV, Zika virus, WNV, West Nile virus; RVFV, Rift Valley fever virus; ONN, O’nyong-nyong virus.
Specimen collection and laboratory procedures
Structured questionnaires were used to obtain social demographic characteristics, past medical history, and clinical information. Participant blood samples, urine samples, and nasal pharyngeal swabs were collected. Five milliliters of blood was collected from each child for malaria testing, m-RT-PCR-ELISA (arbovirus detection), blood culture and complete blood count; the malaria test was performed on site according to the manufacturer’s instructions. Complete blood counts were obtained using a Mindray hematology analyzer machine at the BMC laboratory as previously described.
Nasopharyngeal swabs were only obtained from 77 children who demonstrated fever, cough and flu-like symptoms. Swabs (Copan Diagnostics, Inc. CA, USA) were inserted straight back into one nostril along the floor of the nasal passage until reaching the nasopharynx25,26. The swabs were rotated gently for 5–10 s to loosen the epithelial cells and collect the sample. The samples were then transferred to viral transport medium and stored at − 80 °C at the CUHAS until transported to the University Medical Center of the Johannes Gutenberg University Mainz, Germany for processing. For transportation to Mainz, the samples were packed according to IATA regulations in cooling boxes suitable for medical samples. Specific cooling methods were based upon the transportation time. The nucleic acid was extracted using a High Pure Viral Nucleic Acid Kit (Roche; Mannheim, Germany) and isolated at Mainz using a protocol adapted from Puppe et al.26. Purified nucleic acid was eluted in 50 µl elution buffer; 4.5 µl was used as a template for m-RT-PCR-ELISA25,26.
A multiplex PCR panel capable of identifying 19 pathogens was used at Mainz to detect the pathogens that colonize or infect the upper respiratory tract. The following pathogens could be detected: enterovirus, influenza virus type A, influenza virus type B, respiratory syncytial virus, parainfluenza virus type 1, parainfluenza virus type 2, parainfluenza virus type 3, parainfluenza virus type 4, adenovirus, rhinovirus, human metapneumovirus, coronavirus, bocavirus, M. pneumoniae, C. pneumoniae, B. pertussis, B. parapertussis and L. pneumophila25,26.
Blood and urine culture
Brain heart infusion broth inoculated 1:10 with urine or blood samples was transported to the CUHAS Microbiology laboratory for bacterial culture and antimicrobial susceptibility testing (AST) following standard procedures. Briefly, inoculated blood culture bottles were pre-incubated for 18–24 h at 35 ± 2 °C before subculture on solid media, i.e., 5% sheep blood agar (SBA) and MacConkey agar (MCA) plates. Urine samples, on the other hand, were inoculated directly onto SBA and MCA plates within two hours following collection. All cultures were incubated aerobically at 35 ± 2 °C for 24 h. Morphology (e.g., size and color) and characteristics (e.g., hemolysis on SBA and lactose fermentation on MCA) were considered when interpreting positive and significant bacterial growth. For urine cultures, colony counts ≥ 105 CFU/ml were considered significant.
Biochemical identification testing
Pathogens isolated from blood and urine cultures were identified by biochemical identification tests prepared in-house27. Briefly, bacteria were categorized as either gram-positive cocci or gram-negative rods by Gram staining. Catalase, coagulase, novobiocin disc, bacitracin disc, optochin disc, and bile aesculin were subsequently used to identify gram-positive cocci. Gram-negative bacteria were identified by: sugar fermentation and the production of H2S and CO2 on triple sugar ion (TSI) agar; motility and the production of H2S and indole on sulfide, indole, motility (SIM) medium; utilization of sodium citrate as the sole source of carbon on Simmons citrate agar; production of urease on Christensen’s urea agar; and production of cytochrome c oxidase on oxidase test strips. Second blood and/or urine samples were collected for culture to rule out the possibility of contamination, e.g., skin microflora, S. epidermidis. A second positive culture consisting of the same bacterial species was considered significant.
Antimicrobial susceptibility testing (AST)
AST was performed by the Kirby-Bauer disc diffusion method28. Bacterial pathogens were suspended in sterile 0.9% saline, and the suspensions were adjusted to 0.5 McFarland turbidity standards. The suspensions were then spread over the entire surface of Mueller Hinton agar (MHA) plates to obtain an even lawn on which antibiotic discs were placed within 15 min. The MHA plates were incubated aerobically at 35 ± 2 °C for 18 h The diameter of the zones of inhibitions around the discs were measured in millimeters and interpreted as susceptible, intermediate or resistant according to the Clinical and Laboratory Standards Institute (CLSI) guidelines of 202029. The disc combination method using third-generation cephalosporins with or without clavulanic acid was used for phenotypic confirmation of extended-spectrum β-lactamase (ESBL) production by ceftriaxone-resistant Enterobacterales (CRO-RE)30. CRO-RE with a ≥ 5 mm difference in zones of inhibitions between third-generation cephalosporins with or without clavulanic acid confirmed a positive ESBL phenotype30. Briefly, ceftriaxone (30 µg CRO) and ceftazidime (30 µg CAZ) discs separated by 15 mm from a cefoxitin (30 µg FOX) disc were used for phenotypic confirmation of Amp-C β-lactamase production by CRO-RE with negative ESBL phenotypes30. A d-shaped zone of inhibition for CRO or CAZ on the side of FOX was interpreted as Amp-C β-lactamase positive29. All S. aureus strains exhibiting reduced susceptibility, i.e., zones < 22 mm around the cefoxitin disc, were interpreted as methicillin-resistant (MRSA).
Quality control measures
The questionnaire was cross-checked every day to ensure completeness and that data were entered into a data sheet. Sample collection, transportation and processing were conducted according to the standard protocol provided by the manufacturers and laboratory standard operating procedures. S. aureus (ATCC 25923), MRSA (ATCC 29213), E. coli (ATCC 25922), ESBL producing K. pneumoniae (ATCC 700603), and P. aeruginosa (ATCC 27853) were used as control bacterial strains to check the quality of media, discs and incubation conditions.
Malaria MRDT, dengue rapid NSI antigen, dengue and Chikungunya serology
Approximately 0.5 ml was used onsite to conduct malaria rapid diagnostic tests (MRDT, NADAL Malaria Pf/Pan Ag 4 Species Test; nal von minden GmbH, Regensburg, Germany) and dengue rapid IgM/IgG tests as reported in previous publications22,31. Dengue was diagnosed using the SD Bioline NSI IgM/IgG combo rapid test according to the manufacturer’s instructions (Standard Diagnostics, Inc., Suwon City, Korea)22,24. A dengue-positive rapid IgG test indicated past infection.
Identification of malaria and arbovirus infections by m-RT-PCR-ELISA
Multiplex-RT-PCR combined with a microwell hybridization assay (m-RT-PCR-ELISA) was used to identify mosquito-borne malaria and arbovirus pathogens. The following steps were taken: (1) multiplex PCR in which DIG-11 UTP was incorporated into the amplified strand when the targeted pathogen was present; (2) hybridization of the denatured DIG-labeled amplified strand to ELISA plates coated with the pathogen-specific complementary probe; (3) binding of peroxidase-conjugated digoxigenin-specific antibodies26,31. to hybridized, DIG-labelled DNA; (4) peroxidase catalyzed oxidation of ABTS substrate added to the well; and (5) detection of the green product using a microplate reader at 405 nm confirmed the presence of the targeted pathogen31.
Case definitions
Fever, core body temperature ≥ 38 °C; malaria, rapid test positive, microscopic visualization of parasites, positive genus-specific PCR; confirmed mosquito-borne disease, positive PCR result for arboviruses (dengue, chikungunya, yellow fever, Zika, West Nile, Rift Valley, O’nyong-nyong); presumptive acute mosquito-borne infection, positive rapid diagnostic test (RDT) results (dengue non-structural protein 1 (NS1) and/or detection of anti-arbovirus IgM by ELISA; bacteremia, bacteria in blood; bacteriuria, bacteria in urine; upper respiratory infection, presence of potential pathogens determined by multiplex PCR panel. Complete blood counts were interpreted as previously described32. Clinical diagnosis of pneumonia and gastroenteritis was defined according to the World Health guidelines of Integrated management of childhood illness (WHO/IMCI)33. Anemia was defined using the following WHO classifications. (a) children 6 to 59 months of age: normal 110, 100–110 g/l, moderate 80–109 g/l, severe > 80 g/l for; (b) children 5–11 years of age: normal ≥ 115, 110–114 g/l, moderate 80–109 g/l, severe > 80 g/l; and (c) children 12 to 14 years of age: normal ≥ 120, 110–119 g/l, moderate 80–109 g/l and severe > 80 g/l32,33.
Ethical approval and informed consent
Ethical approval was obtained from the National Institute of Medical Research of Tanzania (NIMR/HQ/R.8a/Vol. IX/2641). Ethical clearance was also obtained from the joint Catholic University of Health and Allied Sciences/Bugando Medical Centre review and Ethics Committee (CREC/455/2020). Permission was obtained from the administrations of: BMC, STRRH, BHC, NDH and SDDH. Written informed consent was obtained from a parent or guardian of each participating child. All participants diagnosed with malaria, dengue, bacteremia, bacteriuria, or the presence of viruses or fungi in the upper respiratory tract were treated according to the World Health guidelines23,24,33. The study was conducted in strict observance of the ethical standards adopted in the Declaration of Helsinki.
Data analysis
Data entry was conducted using Microsoft excel 10. The data were cleaned and analyzed using STATA version 15. Results were summarized using continuous variables described as the mean and standard deviation, or the median with interquartile range depending upon its distribution. Categorical data were summarized as proportions (%). The prevalence of bacteremia, bacteriuria, malaria or arbovirus infections was determined by calculating the number of children who tested positive in terms of the total number tested. The chi-square test was used to assess differences between proportions. Factors associated with the organisms identified in the urine and upper respiratory tract were determined by univariate, followed by multivariate logistic regression analyses. The odds ratio and 95% confidence interval were obtained. All factors with P-values < 0.05 were considered statistically significant.
Results
A total of 457 children were eligible to participate; 436 were enrolled in the final analysis (Fig. 1). All 436 children presented with fever; 38 °C was the lowest, 41 °C was the highest. The majority of children were less than 2 years-of-age (Table 1). Of 436 participants, 56.4% were male and 43.6% were female. Outpatient and inpatient children numbered 356 and 80, respectively. About 1.8% and 1.3% of the study participants suffered from severe wasting or stunting, respectively.
Clinical symptoms and vital signs of the study participants
Tachypnea and tachycardia were recorded in 235 and 179 children, respectively (Supplementary Table 1). Higher percentages of 6- to 12-year-old children exhibited elevated systolic and diastolic blood pressure, 30 mmHg and 80 mmHg, respectively.
Laboratory findings
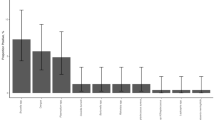
Bacteremia was observed in 6.2% of the study participants; 60% of those infections were due to gram-negative bacteria. Pathogens isolated in blood included Acinetobacter spp., K. pneumoniae, S. aureus (all were methicillin-resistant), Enterococcus spp., S. pyogenes, and S. epidermidis (Supplementary Fig. 1). 23% of these produced AmpC β-lactamase. Approximate 10% of the participants had bacteria in their urine; E. coli followed by K. pneumoniae were the most common organisms identified (Supplementary Fig. 2). Candiduria was detected in urine samples obtained from 8 patients. Thirty-four children (7.8%) were diagnosed with dengue virus infections by NSI-RDT. No arbovirus infections were detected by m-RT-PCR-ELISA (Table 2). Viruses were identified in the upper respiratory tract of 43% of 77 participants who provided nasopharyngeal swabs (Supplementary Fig. 3a). Rhinovirus followed by bocavirus were the most frequently identified in these selected patients (Supplementary Fig. 3b).
Etiology
Acute gastroenteritis and pneumonia diagnosed by WHO criteria were most commonly associated with AFI followed by laboratory analyses of bacteriuria and bacteremia (Fig. 2). The greatest prevalence occurred in children above 6 years-of-age (Fig. 3), and in more males than females (Supplementary Fig. 4). Diagnoses of gastroenteritis and pneumonia were higher in Nyamagana, Sekou Toure and Sengerema; dengue was most often seen in Bugando and Sengerema; bacteriuria was more common in Sekou Toure and Buzuruga (Supplementary Fig. 5).
Overlapping etiology
Potential overlapping causes of fever that occurred in non-malarial and non-dengue cases in this study were occasionally identified by laboratory tests. The overlap between bacteremia or bacteriuria and the presence of microorganisms in the upper respiratory tract was 0.2%; the overlap between bacteriuria and bacteremia was 1% (Fig. 4). Malaria and dengue virus coinfections were observed in 3.4% of patients in a previous study22.
Percent of antibiotic-resistant bacterial pathogens isolated from blood and urine samples
Gram-negative Acinetobacter spp. isolated from blood samples exhibited complete resistance to ceftriaxone, ceftazidime and meropenem (Supplementary Table 2). Similarly, Klebsiella pneumoniae demonstrated 100% resistance to amoxicillin-clavulanic acid, ceftriaxone, ceftazidime, ciprofloxacin and piperacillin-tazobactam. The following gram-positive bacteria isolated from blood samples exhibited significant antibiotic resistance: Staphylococcus spp. exhibited high resistance to gentamicin (50.0%), tetracycline (62.5%), erythromycin (100%) and trimethoprim-sulfamethoxazole (100%); Enterococcus spp. expressed 100% resistance to ampicillin, trimethoprim-sulfamethoxazole and vancomycin; and Streptococcus pyogenes displayed complete resistance to tetracycline, azithromycin, erythromycin, and trimethoprim-sulfamethoxazole.
Gram-negative E. coli isolated from urine samples demonstrated significant resistance to tetracycline, gentamicin, ciprofloxacin, ceftazidime and ceftriaxone (Supplementary Table 3). Klebsiella spp. exhibited elevated resistance to gentamicin, nitrofurantoin and ceftriaxone. Acinetobacter spp. displayed complete resistance to nitrofurantoin, ceftriaxone, and ceftazidime. Gram-positive S. epidermidis was 100% resistant to tetracycline; Enterococcus spp., on the other hand, exhibited 50% resistance to gentamicin, and 100% resistance to ciprofloxacin, ampicillin, erythromycin and trimethoprim-sulfamethoxazole.
Association between microorganisms, clinical symptoms of non-malarial AFI, and social demographics of child participants
Logistic regression analyses were undertaken to ascertain the association between the detection of microorganisms, clinical symptoms and the sociodemographic of children enrolled in the study. Univariate analysis showed an association between bacteremia and a decreased period of fever duration (1–3 days). Fever duration below three days, however, did not promote bacteremia in this cohort of children independent of other factors assessed (Supplementary Table 4a). Multivariate analysis revealed a significant association between bacteriuria and vomiting (Supplementary Table 4b). Multivariate analysis, however, failed to demonstrate a correlation between bacteremia, bacteriuria and any of the other clinical or sociodemographic factors examined. Similarly, multivariate analysis failed to detect an association between the presence of microorganisms in the upper respiratory tract and any of these same factors (Supplementary Table 4c).
Discussion
This study was conducted using diagnostic tests and definitions formulated by WHO/IMCI for the non-malarial etiology of AFI. Accordingly, acute gastroenteritis and pneumonia were documented in 16% (73/436) and 13% (59/436) of AFI cases. Bacteremia, bacteriuria, and human immunodeficiency virus infections were associated with 10%, 6% and 1.6% of the AFI cases occurring among the 436 participants, respectively. Upper respiratory tract infections or colonization was found among a selected group of patients with flu-like symptoms. A small proportion of those patients were infected with arboviruses; dengue virus infections were detected in 7.8% of children enrolled in our study reported previously22.
The present study, conducted in children attending five hospitals in a part of the country with a large catchment population, complements other studies conducted in Tanzania and Africa4,16,17,20. An approximate 30% of the cohort had clinical diagnoses; acute gastroenteritis and pneumonia were the leading causes. Acute gastroenteritis was more noticeable in children less than 2 years-of-age. The burden of acute gastroenteritis and pneumonia, the most preventable causes of AFI particularly in children, is well documented4,20,25,34. Most infections in young children are caused by viruses4,17,18,19. In 77 selected patients with flu-like symptoms whose nasopharyngeal passage was swabbed, rhinovirus, bocavirus and adenovirus were commonly identified most likely linked to colonization rather than a cause of the Upper respiratory tract infection. Common cold-like symptoms, particularly in the case of rhinovirus, have been linked to the exacerbation of asthma and chronic obstructive pulmonary disease, severe bronchiolitis and pneumonia in infants and children25,34,35. Accurate diagnosis of acute respiratory infections is a major challenge, however, especially using gold standard tools that differentiate viral and bacterial etiologies. Viral infections have been linked to the overuse of antibiotics in the absence of appropriate diagnostic tests to rule out bacterial infections leading to increased antimicrobial resistance in developing countries34,35,36,37. Nasopharyngeal swabs were only collected from children presenting with fever and respiratory symptoms in the current study. This introduces selection bias and fails to distinguish between colonization and infection. Thus, the elevated presence of viruses identified in the upper respiratory tract in our study must be interpreted with caution and should not be overestimated as definitive causes of fever cases rather than colonization. Other causes of upper respiratory infections such as acute ear infections and tonsilitis diagnosed by the clinical symptoms according to WHO are not within the scope of the current study.
Bacteremia was found in ~ 6% of AFI patients, 23% of those patients exhibited an alarming increase in number of bacterial isolates that were resistant to commonly used first- and second-line antibiotics. The isolates often produced AmpC β-lactamase. The most common pathogens isolated from the blood were A. freundii, S. aureus and K. pneumoniae. 8% of the multidrug resistant isolates in our study were obtained from tertiary and regional referral hospitals where most of the patients had previously received multiple antibiotics associated with the increased occurrence of antibiotic resistance pathogens. Similar findings reported in previous studies conducted in Uganda and Tanzania showed a varied patterns of antibiotic resistance dependent upon the healthcare facility in which the study was conducted17,38. Elevated resistance (6%) was reported in referral/tertiary hospitals while decreased resistance (1.7%) was reported in lower healthcare facilities38,39. Similar findings were reported in studies conducted in Ethiopia10. The prevalence of antibiotic resistance exhibited by most pathogens isolated in this study poses a major challenge to proper patient management. This is true for both hospital associated and community acquired infections. 20% of patients harboring drug resistance organisms came from district hospitals as outpatients where continued education of the community about the irrational use of antibiotics, e.g., buying without prescriptions and incomplete drug dosing, is advised.
An increase in global temperatures has fostered the development of antimicrobial resistance. Elevated temperature facilitates horizontal gene transfer and the exchange of resistance genes such as plasmid-borne extended-spectrum β-lactamases, as well as the direct uptake of free genetic material from the environment14,40. Higher temperatures also influence the spread of antimicrobial resistance by increasing bacterial growth rates, favoring selective pressure, and altering microbial communities and ecosystems13,14.
In 2019, the WHO reported that antimicrobial resistance (AMR) contributes to 4.95 million deaths and is directly responsible for 1.27 million deaths globally in that year41. The World Bank estimates that AMR could lead to 1 trillion US dollars in added healthcare costs by year 205042. As such, there is a critical need to strengthen the ability of healthcare systems to identify and differentiate between bacterial and viral pathogens, and to invest in rapid tests to detect infections and in diagnostic algorithms that will ensure appropriate antibiotics treatment. Studies conducted in 14 Sub-Saharan African countries reported that only 20% of 12 countries reported strengthening bacterial testing and the capacity for AMR detection according to the National Action plan43. Expanding and building the capacity for antimicrobial susceptibility testing by laboratory technicians at the district levels in Africa will reduce inappropriate antibiotics use and AMR.
Bacteriuria correlated with illness in a significant number of febrile children; 10.8% of the urine cultures in the current study were positive. This is low compared to 22% reported in a previous study that recruited both adults and children from the same area39. Participation in the current study depended upon presentation of a high temperature at the time of enrollment. The signs and symptoms of urinary tract infections were not screened. As such, the findings may indicate symptomatic or asymptotic urinary tract infections in the participants whose urine cultures tested positive. Notably, the finding of the current study is higher than other studies that reported positive urine cultures that ranged from 1.8 to 5.7% in febrile children under 5 years-of-age17,18. Gram-negative E. coli followed by K. pneumoniae were the dominant isolates in the present study. Conceivably, factors that include the interaction between microbial communities especially in gut and vagina, i.e., the ascending fecal-perineal-urethral route, contribute to the predominant occurrence of these organisms38,39. 20% of the children who tested positive for bacteriuria had extended-spectrum β-lactamase-producing Enterobacterales (ESBL-PE); 5% had AmpC β-lactamase-producing ESBL-PE. Another study conducted in the same area during the COVID-19 pandemic reported similar results39. These findings, as well as those related to bacteria in the bloodstream above, emphasize the critical need for enhanced surveillance of antimicrobial resistance, improved infection prevention measures, and strengthened antimicrobial stewardship programs that include the use of antibiogram to guide empirical treatment especially in this vulnerable group of children.
Studies conducted primarily in eastern Tanzania documented several outbreaks of dengue and chikungunya virus infections44,45. Others studies, including a recent systematic review and meta-analysis that demonstrated the existence of these pathogens in African children46. Another study in Tanzania found the arbovirus vector (Aedes aegypti) was abundant in the Dar es Salaam area47. A previous study by us documented the infrequent occurrence of dengue virus infections in febrile children; presumptive infections only occurred in 7.8% of children with fever22. IgM-positive serology and negative PCR results for dengue virus in the current study can be explained by a number of factors including a narrow window for virus detection, RNA instability, low virus shedding and rapid virus clearance6,44,45. There were no confirmed cases of other arbovirus infections (i.e., yellow fever virus, Zika virus, West Nile virus, Rift Valley fever virus or O’nyong-nyong virus). The low rate of arbovirus transmission and the probability that sampling did not occur during an outbreak when most cases of infection occur probably contributes to this finding43,44. Despite this, screening for arbovirus infections and neglected tropical diseases is crucial to improving case detection and management. Currently, there are no well-established epidemiological surveillance systems or laboratory diagnostic procedures. This contributes to a lack of information concerning the incidence and prevalence of arbovirus infections in children. In all probability, increased temperature associated with climate change will result in a net increase in the geographical distribution and a change in the life cycle of vectors, raising the potential for transmission of arbovirus infections in non-endemic area13.
Univariate analysis demonstrated that the cohort of patients that had a decreased period of fever duration (1–3 days) exhibited twice the odds of having bacteremia. Multivariate analysis, however, failed to support a correlation between bacteremia and decreased fever duration independent of other factors. Vomiting children were three times more likely to have bacteriuria compared to children without clinical signs of vomiting. Bacterial invasion of the urinary tract that triggers an inflammatory response in the vomiting center of the central nerve system could be an underlying factor. Co-existing conditions in the study areas may contribute to the lack of association between any of the other social demographic factors studied and bacteremia, bacteriuria or microbes detected in the upper respiratory tract. Additional studies that elucidate these relationships are warranted.
The study reported here has a number of limitations. First, PCR was only performed on nasopharyngeal swabs collected from children exhibiting a fever, cough and flu-like symptoms. Most children harbor respiratory viruses making it difficult to differentiate between colonization and infection. This may contribute to an overestimation and the elevated prevalence of viruses and bacteria in the upper respiratory tract34. The use of multiplex PCR for testing samples derived from the upper respiratory tract remains a challenge in low- and middle-income countries. A second limitation of this study is the failure to use PCR and stool culture as approaches to diagnosing patients with gastrointestinal infections caused by viral and bacterial pathogens. Conceivably, this results in underestimating the contribution of viral gastrointestinal infections to the prevalence of AFI. Third, collection of only a single blood sample reduces the possibility of isolating organisms present in bloodstream. Fourth, although participants were enrolled from both higher tier (Tertiary and Regional) and lower tier (Districts and Health Centre) hospitals, this was only true of the pediatric outpatient clinics and one tertiary pediatric ward. Random sampling did not occur throughout the entire Mwanza Region nor outside clinical pediatric settings excluding neonatal and surgical clinics. As such, selection bias associated with the facilities chosen undoubtedly occurred. Finally, the study lacks a healthy control group for comparison purposes. Despite of these limitations, the strength of this study lies in the effort to create better algorithms for selecting the best diagnostic tools to identify the pathogens associated with AFI in children who reside in a resource-limited setting.
In the current study, 1.6% of children were newly diagnosed with human immunodeficiency virus infections. Early diagnosis is important for the prompt enrollment of these children into care and treatment clinics. This demonstrate the importance of point-of-care counseling and testing both the mother and child upon entering the healthcare facility.
Laboratory analyses identified a substantial number of potential causative agents indicating their value in appropriate patient management. Implementing advanced diagnostic tools is a crucial next step in addressing any limitation. Among these tools, real-time PCR is an approach that can improve the accuracy of pathogen detection and reduce the time to diagnosis, thus supporting the ability of clinicians to make timely, informed decisions that result in better patient outcomes31,47. To overcome the challenges posed by current diagnostic approaches, future research should focus on the feasibility and effectiveness of integrating real-time PCR into routine practice in selected clinical settings48. Moreover, additional sample types such as stool specimens for the determination of gastrointestinal pathogens need to be included in future studies (Fig. 5).
Conclusion & recommendation
The findings presented herein demonstrate the ability to identify the causative agents in approximately 60% of children presenting with AFI when the appropriate tests are available together with WHO clinical algorithms. Prompt diagnosis and treatment should be tailored according to the diagnostic tools available locally; the increased use of supportive diagnostic tools (RDTs, microscopy, radiology, and microbiology laboratory point of care polymerase chain reactions) improve the clinical care of children living in Tanzania, as well as throughout Sub-Saharan Africa. An increase in multidrug resistant pathogens associated with bacteriuria and bacteremia was observed, highlighting the need to strengthen existing infection prevention and control interventions to include surveillance in order to ensure the rational use of antimicrobials. The results of this study should help inform decision makers and healthcare workers in planning and implementing interventions to improve the diagnosis, clinical management and prevention of neglected tropical febrile diseases. To strengthen these findings, the use of advanced diagnostic tools and the inclusion of a broader variety of specimen types should be explored.
Data availability
All datasets included in the manuscript are available upon request and almost provided within the manuscript. Requests should be made to the Director of research and Innovation, Catholic University of Health and Allied Sciences and corresponding author. All relevant materials used in this study are accessible upon request to ensure transparency and reproducibility of the research findings .
References
Reiner, R. C. et al. Diseases, injuries, and risk factors in child and adolescent health, 1990 to 2017: findings from the global burden of diseases, injuries, and risk factors 2017 study. JAMA Pediatr. 173 (6), e190337 (2019).
de Bont, E. G. et al. Workload and management of childhood fever at general practice out-of-hours care: an observational cohort study. BMJ Open. 5 (5), e007365 (2015).
McDonald, C. R., Weckman, A., Richard-Greenblatt, M., Leligdowicz, A. & Kain, K. C. Integrated fever management: disease severity markers to triage children with malaria and non-malarial febrile illness. Malar. J. 17, 1–7 (2018).
D’acremont, V. et al. Beyond malaria—causes of fever in outpatient Tanzanian children. N. Engl. J. Med. 370 (9), 809–817 (2014).
Villavicencio, F. et al. Global, regional, and National causes of death in children and adolescents younger than 20 years: an open data portal with estimates for 2000–21. Lancet Global Health. 12 (1), e16–e17 (2024).
Kading, R. C., Brault, A. C. & Beckham, J. D. Global perspectives on arbovirus outbreaks a 2020 snapshot. Trop. Med. Infect. Disease 5(3), 142 (2020).
Mordecai, E. A., Ryan, S. J., Caldwell, J. M., Shah, M. M. & LaBeaud, A. D. Climate change could shift disease burden from malaria to arboviruses in Africa. Lancet Planet. Health. 4 (9), e416–e423 (2020).
World Health Organization. World Health Statistics 2015 (World Health Organization, 2015). May 14.
Bassat, Q. et al. Causes of death among infants and children in the child health and mortality prevention surveillance (CHAMPS) network. JAMA Netw. Open. 6 (7), e2322494 (2023).
Shimelis, T. et al. Aetiology of acute febrile illness among children attending a tertiary hospital in Southern Ethiopia. BMC Infect. Dis. 20, 1–2 (2020).
Vogels, C. B. et al. Arbovirus coinfection and co-transmission: A neglected public health concern? PLoS Biol. 17 (1), e3000130 (2019).
Gubler, D. J. Dengue, urbanization and globalization: the unholy trinity of the 21st century. Trop. Med. Health. 39 (4SUPPLEMENT), S3–11 (2011).
Segala, F. V. et al. Insights into the ecological and climate crisis: emerging infections threatening human health. Acta Trop. 19, 107531 (2025).
Bellone, R. & Failloux, A. B. The role of temperature in shaping mosquito-borne viruses transmission. Front. Microbiol. 11, 584846 (2020).
Kissoon, N. & Uyeki, T. M. Sepsis and the global burden of disease in children. JAMA Pediatr. 170 (2), 107–108 (2016).
Novignon, J. & Nonvignon, J. Socioeconomic status and the prevalence of fever in children under age five: evidence from four sub-Saharan African countries. BMC Res. Notes. 5, 1–7 (2012).
Matee, M. et al. Mapping and gap analysis on antimicrobial resistance surveillance systems in kenya, tanzania, Uganda and Zambia. Bull. Natl. Res. Centre. 47 (1), 12 (2023).
Crump, J. A. et al. Etiology of severe non-malaria febrile illness in Northern tanzania: a prospective cohort study. PLoS Negl. Trop. Dis. 7 (7), e2324 (2013).
Mahende, C. et al. Aetiology of acute febrile episodes in children attending Korogwe district hospital in north-eastern Tanzania. PLoS One. 9 (8), e104197 (2014).
Elfving, K. et al. Omar rs,parola P, acute uncomplicated febrile illness in children aged 2–59 months in Zanzibar-aetiologies, antibiotic treatment and outcome. PloS One. 11 (1), e0146054 (2016).
Van de Vuurst, P. & Escobar, L. E. Climate change and infectious:a review of evidence and research trends. Infectioous Dis. Poverty 12(1), 51 (2023).
Kayange, N. M. et al. Malaria and dengue fever in febrile children entering healthcare facilities in Mwanza. Tanzan. Plos One. 19 (10), e0309613 (2024).
World Health Organization. Guidelines for the treatment of malaria. World Health Organ. Aug 13. (2015).
Dengue Guidelines for Diagnosis, Treatment, Prevention and Control: New Edition. WHO Guidelines Approved by the Guidelines Review Committee. Geneva (2009).
Kwiyolecha, E. et al. Patterns of viral pathogens causing upper respiratory tract infections among symptomatic children in Mwanza. Tanzan. Sci. Rep. 10 (1), 18490 (2020).
Puppe, W. et al. Validation of a multiplex reverse transcriptase PCR ELISA for the detection of 19 respiratory tract pathogens. Infection 41, 77–91 (2013).
Procop, G. W., Church, D. L., Hall, G. S. & Janda, W. M. Koneman’s Color Atlas and Textbook of Diagnostic Microbiology (Jones & Bartlett Learning, 2020).
Mu Hudzicki, J. Kirby-Bauer disk diffusion susceptibility test protocol. Am. Soc. Microbiol. 15, 1–23 (2009).
CLSI. (Clinical and Laboratory Standards Institute, Wyne, PA. (2020).
Tula, M. Y., Iyoha, O., Elisha, R., Filgona, J. & Aziegbemhin, S. Phenotypic detection of Extended-Spectrum β-lactamases (ESBLs) and aminopenicillin cephalosporinase (AmpC)-Producing bacterial isolates from surfaces of hospital fomites and hands of healthcare workers. J. Med. Microbiol. Infect. Dis. 11, 141–147 (2023).
Koliopoulos, P. et al. Multiplex-RT-PCR-ELISA panel for detecting mosquito-borne pathogens: plasmodium sp. preserved and eluted from dried blood spots on sample cards. Malar. J. 20, 1–6 (2021).
Abbam, G. et al. Complete blood count reference intervals for children aged less than 1 to 12 years in the Northern region of Ghana. Biomed. Res. Int. 2024 (1), 6607281 (2024).
World Health Organization. Pocket Book of Hospital Care for Children: Guidelines for the Management of Common Childhood Illnesses (World Health Organization, 2013).
Pratt, M. T. et al. Prevalence of respiratory viruses in community-acquired pneumonia in children: a systematic review and meta-analysis. Lancet Child. Adolesc. Health. 6 (8), 555–570 (2022).
Sirota, S. B. et al. Global, Regional, and National Burden of Upper Respiratory Infections and Otitis Media, 1990–2021: a Systematic Analysis from the Global Burden of Disease Study 2021 (The Lancet Infectious Diseases, 2024).
Turyasiima, M., Kiconco, G., Egesa, W. I., Twesigemukama, S. & Nduwimana, M. Prevalence and outpatient clinical diagnostic approaches for common acute respiratory tract infections in children under five years of age: A Cross-Sectional study. Pediatr. Health Med. Ther. 31, 49–57 (2024).
Huth, P. F. et al. Extensive antibiotic and antimalarial prescription rate among children with acute febrile diseases in the lake Victoria region, Tanzania. J. Trop. Pediatr. 67 (1), fmaa135 (2021).
Seni, J. et al. Deciphering risk factors for blood stream infections, bacteria species and antimicrobial resistance profiles among children under five years of age in North-Western tanzania: a multicentre study in a cascade of referral health care system. BMC Pediatr. 19, 1–1 (2019).
Silago, V. et al. Epidemiology and antimicrobial resistance trends of pathogens causing urinary tract infections in mwanza, tanzania: A comparative study during and after the implementation of the National action plan on antimicrobial resistance (2017–2022). Int. J. Infect. Dis. 147, 107208 (2024).
Warnes, S. L., Highmore, C. J. & Keevil, C. W. Horizontal transfer of antibiotic resistance genes on abiotic touch surfaces: implications for public health. MBio 3 (6), 10–128 (2012).
Talebi Bezmin Abadi, A., Rizvanovv, A. A., H Haertlé, T. & Blatt, N. L. World health organization report: current crisis of antibiotic resistance. BioNanoScience 9 (4), 778–788 (2019).
OBI, J., Berthe, A., Jean, F. C., Le Gall, F. G. & Marquez, P. V. Drug-resistant Infections : a Threat To our Economic Future (Vol. 2): Final Report (English). In: HNP/ Agriculture Global Antimicrobial Resistance Initiative (The World Bank, 2017).
Ondoa P, Kapoor G, Alimi Y, Shumba E, Osena G, Maina M, Batra D, Sow A, Matu M, Moreira M, Kebede Y. Bacteriology testing and antimicrobial resistance detection capacity of National tiered laboratory networks in sub-Saharan africa: an analysis from 14 countries. Lancet Microbe 6(1), 100976 (2025).
Mwanyika, G. O. et al. Circulationof dengueserotype1 viruses during the 2019 outbreakin Dar Es salaam, Tanzania. Pathog Glob Health. 115 (7–8), 467–475. https://doi.org/10.1080/20477724.2021 (2021).
Mboera, L. E. et al. Theriskofdengue virus transmission in Dar Es salaam, Tanzania during an epidemic period of 2014. PLoS Negl. Trop. Di. 10 (1), e0004313 (2016).
Kayange, N. et al. Seroprevalence of dengue and Chikungunya virus infections in children living in Sub-Saharan africa: systematic review and meta-analysis. Children 10 (10), 1662 (2023).
Ngingo, B. L. et al. Aedes aegypti abundance, larval indices and risk for dengue virus transmission in Kinondoni district, Tanzania. Trop. Med. Health. 50, 1–8 (2022).
Undrakonda, A. & Oroszi, T. Diagnostic and treatment strategies for acute febrile illnesses (AFIs). Advances in infectious diseases 14 (04), 793–809. https://doi.org/10.4236/aid.2024.144059 (2024).
Acknowledgements
The authors acknowledge the Catholic University of Health and Allied Sciences, Mwanza, Tanzania. We appreciate the hospital administration at Bugando Medical Centre Mwanza, Tanzania, and the Department of Pediatrics at the University Medical Center of Johannes Gutenberg University Mainz, Germany. We also appreciate the support provided by the Mwanza region commissioner and district medical officers of the Ilemela and Nyamagana districts. Additionally, we extend our gratitude to the medical officers in charges and staff of Buzuruga health center, Nyamagana district hospital, Sekou Toure Regional Referral hospital, Sengerema District hospital and Bugando Medical Centre. We would also like to thank the parents and children for their voluntary participation in this study. We are grateful for the research team: Dr. Gayo Mpalala, Mr. Peter Nandi, Mr. Frank Elias, and Dr. Evodia Chatila, We thanks also microbiology expert team Kilwa Patrick Mnibi and Vitus Silago. We especially thank Dr. Stephen H. Gregory (Providence, RI, USA) for his help writing, editing and reviewing this manuscript.
Funding
This study was supported by the Catholic University of Allied Health Sciences and Bugando Medica Centre Laboratories. Multiplex PCR-ELISA was supported by the European Virus Archive goes Global project, which received funding from the European Union’s Horizon 2020 research and innovation program under grant agreement No. 653316. The project was partially funded by the Else-Kröner Fresenius Stiftung Klinikpartnerschaften (Bad Homburg, Germany) Grant No. 1601079.
Author information
Authors and Affiliations
Contributions
N.K contributed to the conceptualization, design of the study, data collection, acquired funding and manuscript writing. OM conducted the literature review, developed methodologies and interpreting data. SS and BG performed molecular laboratory work. SG was responsible for results interpretation and critical revision of the manuscript . PK contributed to data curation and validation. SM was responsible for visualization and Coordination of research team supervising the project implementation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kayange, N.M., Malande, O.O., Scialaba, S. et al. Non-malarial etiology of acute febrile episodes in children attending five healthcare facilities in Mwanza, Tanzania years 2020–2021. Sci Rep 15, 34333 (2025). https://doi.org/10.1038/s41598-025-16723-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-16723-w