Abstract
To investigate the separate and combined associations of excess body weight (EBW), hypertension (HTN), and hypertriglyceridemia (HTG) with hyperglycemia among non-diabetic adults aged 60 years and above in regional China. In this cross-sectional study conducted in 2023, 26,769 non-diabetic individuals aged 60 years and older were selected from Nanjing municipality, China. Body weight and height, blood pressure, fasting plasma triglycerides, and glucose were objectively measured, while socio-demographic attributes, lifestyle and behaviors, and disease history were self-reported. The outcome variable was hyperglycemia. Independent variables included EBW, HTN, HTG, and their combinations. Mixed-effects logistic regression models were used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) to assess the separate and combined associations of EBW, HTN, and HTG with hyperglycemia. Among all participants, the prevalence of hyperglycemia was 16.3%, while 14.0%, 57.2%, and 27.8% had obesity, HTN, and HTG, respectively. After adjusting for potential confounders, individuals with EBW, HTN, or HTG were independently more likely to experience hyperglycemia compared to those without the corresponding condition. Participants with any two-factor combinations of these three conditions had a higher risk of hyperglycemia than those with only one. Moreover, individuals with the three conditions had substantially greater odds of hyperglycemia than those with any two-factor combinations. Obese adults with both HTN and HTG had 5.04-fold higher odds (95%CI = 4.31, 5.90), while overweight individuals with HTN and HTG had 3.20-fold higher odds (95%CI = 2.79, 3.67) of experiencing hyperglycemia, compared to those with normal body weight, blood pressure, and triglyceride levels. Among men, individuals with obesity who had HTN and HTG had 5.15-fold higher odds (95%CI = 4.02, 6.61), and overweight individuals with HTN and HTG had 3.27-fold higher odds (95%CI = 2.63, 4.05). Among women, individuals with obesity who had HTN and HTG had 5.36-fold higher odds (95%CI = 4.22, 6.82), and overweight individuals with HTN and HTG had 3.40-fold higher odds (95%CI = 2.74, 4.22) of hyperglycemia. EBW, HTN, and HTG jointly increased the risk of hyperglycemia among older adults, both men and women, aged 60 years and above in China. These findings have important public health implications, suggesting that personalized interventions targeting EBW, HTN, and HTG may serve as an effective strategy for the population-level prevention of hyperglycemia.
Similar content being viewed by others
Introduction
Diabetes and pre-diabetes have become major public health concerns worldwide1,2,3. In 2022, the global prevalence of diabetes was 14.0% among adults aged 18 years and older2. In 2021, the prevalence of impaired glucose tolerance and impaired fasting glycemia—the two main types of pre-diabetes—was 9.1% and 5.8%, respectively, among adults aged 20–79 years worldwide3. In the USA, the estimated prevalence of diabetes and pre-diabetes in 2021 was 11.6% and 38.0%, respectively, among individuals aged 18 years and older4. In China—the world’s most populous and rapidly developing country—the estimated prevalence of diabetes and pre-diabetes in 2018 was 12.4% and 38.1%, respectively, among adults aged 18 years and older5. Moreover, among those aged 60 years and older, the prevalence increased to 25.0% and 48.0%, respectively, in China5. These figures highlight the substantial burden of diabetes and pre-diabetes in the general population, particularly among older adults.
Pre-diabetes is typically characterized by elevated fasting blood glucose levels (hyperglycemia) that do not meet the diagnostic criteria for diabetes, placing affected individuals at high risk of progressing to diabetes1. As an intermediate state between normal glycemic levels and diabetes, pre-diabetes shares similar risk factors with diabetes1. Among the various forms of diabetes, type 2 diabetes (T2D) is the most common, accounting for approximately 90–95% of all cases, and primarily affects adults, particularly older individuals2,4. Prevention and treatment guidelines issued by the World Health Organization (WHO) and the American Diabetes Association (ADA) emphasize the management of hyperglycemia- or diabetes-associated risk factors, including excess body weight (EBW), hypertension (HTN), and hypertriglyceridemia (HTG)6,7,8. While each of these factors—EBW, HTN, and HTG—has been individually associated with hyperglycemia and T2D6,7,8, no study to date has investigated their combined associations with hyperglycemia or T2D.
To address this gap, we conducted a study to investigate the comprehensive associations of body weight, blood pressure (BP), and triglyceride (TG) with hyperglycemia among older adults aged 60 years and above who had no diagnosed T2D in regional China. Specifically, this study aimed to examine: (1) the separate associations of EBW, HTN, and HTG with hyperglycemia; (2) the joint associations of EBW and HTN, EBW and HTG, and HTN and HTG (two-factor combinations) with hyperglycemia, respectively; and (3) the combined association of all three factors—EBW, HTN, and HTG—with hyperglycemia among non-diabetic adults aged 60 years and above in Nanjing municipality, China.
Methods
Study design and participants
Nanjing municipality, a typical megacity in eastern China, comprised 12 administrative districts and had approximately 9.5 million registered residents at the end of 2022, with 19.5% aged 60 years and above9. A large-scale cross-sectional survey—Healthy Aging, Healthy Elders 2023 (HAHE-2023 study)—was conducted in 2023 among urban and rural residents aged 60 years and above in Nanjing municipality. As a periodical surveillance program, the HAHE-study was developed to: (1) investigate the prevalence of selected chronic conditions (primarily including diabetes, HTN, EBW, abnormal lipid profiles, elevated blood glucose); (2) collect information on lifestyle and behavior (including dietary consumption, physical activity [PA], smoking, and drinking); and (3) assess health-related quality of life among local registered residents aged 60 years and above in Nanjing. The first HAHE study was conducted in mid-201810, and the second, HAHE-2023 study, was implemented in mid-2023.
Individuals were eligible to participate in the HAHE study if they met the following criteria: (1) registered as a resident in Nanjing; (2) aged 60 years or older; (3) had no cognitive, psychiatric, or literacy-related problems. The sample size for the HAHE-2023 study was primarily based on the estimation used in the HAHE-2018 study, with additional consideration of the expected response rate. In China, the emergency containment measures against the COVID-19 epidemic were terminated on January 8 of 2023, after which regular prevention strategies were implemented11. As the HAHE-2023 study was conducted in the first year following the end of COVID-19 emergency measures in Nanjing, a conservative response rate was assumed. Additionally, the information collected in the HAHE-2023 study was intended to serve as reference data for future surveillance of chronic diseases and lifestyle/behavioral patterns among older residents in the post-COVID-19 context. Therefore, the overall sample size for the HAHE-2023 study was projected to exceed that of HAHE-2018 (N = 21000) to ensure adequate statistical power and population representativeness. Ultimately, the sample size for the HAHE-2023 study was determined to be approximately 30,000.
Participants were randomly selected from across the 12 districts in Nanjing municipality using a multi-stage sampling strategy10. First, the sub-sample size was calculated for each district based on its proportion of older residents (aged 60 years and above) relative to the municipality. Second, the number of participating households was estimated for each district, assuming that two eligible participants would be available per household. Third, 15 administrative communities or villages were randomly chosen from each district. Then, eligible households were randomly selected from each participating community based on the calculated number of households for each district. Finally, all eligible older residents within each selected household were invited to participate in the HAHE-2023 study. Consequently, 35,071 participants were recruited, and 32,735 (93.3%) successfully completed the survey.
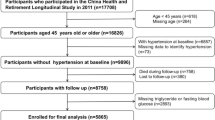
It is well-documented that individuals often seek clinical treatment and/or modify their lifestyle and behaviors to manage blood glucose levels following a diabetes diagnosis12,13. To ensure that blood glucose levels were not influenced by such diabetes-related clinical or behavioral interventions, it was scientifically necessary and appropriate to limit the analysis to individuals without a diagnosed diabetes condition. Therefore, all participants with diagnosed diabetes in the HAHE-2023 survey were excluded from the present study. This resulted in a final analytical sample of 26,769 non-diabetic individuals used to examine the combined associations of EBW, HTN, and HTG with hyperglycemia. Figure 1 presents the selection flowchart of participants included in the analysis.
Written informed consent was obtained from all participants prior to the survey. The Ethics Committee of Nanjing Medical University Affiliated Nanjing Municipal Center for Disease Prevention and Control approved the original data collection protocol. All methods used in this study adhered to the principles outlined in the Declaration of Helsinki. For the present analysis, only de-identified secondary data were used. Therefore, the Ethics Committee of Geriatric Hospital of Nanjing Medical University granted a waiver of ethical approval.
Data collection
For all participants, socio-demographic characteristics, lifestyle and behaviors, history of selected chronic diseases, and family history of diabetes were self-reported through a face-to-face questionnaire survey, while body weight, height, BP, fasting plasma glucose (FPG), and TG were objectively measured10,14. Information on socio-demographic characteristics included age, gender, residence, educational level, marital status, and health insurance. Lifestyle and behavioral factors in this study included PA, smoking, drinking, and meat and fruit consumption. Personal history of diabetes and HTN, as well as family history of diabetes, were also self-reported by each participant.
Body weight was measured to the nearest 0.1 kg and height to the nearest 0.01 m for each participant. Each measurement was taken twice, and the average was used to calculate body mass index (BMI), defined as body weight (kg) divided by height squared (m2)14. BP was recorded using a calibrated sphygmomanometer based on Korotkoff sounds, following the recommended procedure for measuring BP among Chinese adults15. For each participant, BP was measured at least twice and the average reading was used in the analysis15. A 5-ml fasting venous blood sample was collected from each participant at the survey site and sent to a designated laboratory for analysis. FPG and TG levels were assessed using a HITACHI 7180 analyzer (Hitachi Co., Japan), with detection kits provided by Shanghai Fosun Long March Medical Science Co., China.
Study variables
Outcome variable
The outcome measure was FPG status. In this study, a cutoff value of 6.1 mmol/L was used to categorize participants into either “normoglycemia (FPG < 6.1 mmol/L)” or “hyperglycemia (FPG ≥ 6.1 mmol/L)” for the analysis1,16. This FPG cutoff was recommended by the WHO for defining hyperglycemia1. Moreover, it has been officially adopted to identify hyperglycemia among older adults aged 60 years and above in China16.
Independent variables
There were three independent variables in the study: body weight, BP, and TG status. Body weight status was classified as “non-EBW (BMI < 24kg/m2),” “overweight (BMI: 24–27 kg/m2),” or “obesity (BMI ≥ 28 kg/m2)” with EBW referring to either overweight or obesity, according to BMI cutoffs recommended for Chinese adults14. Participants were categorized as having “HTN”, if they had previously been diagnosed with HTN by a physician or if their systolic/diastolic BP was ≥ 140/90 mmHg assessed during the survey15. Otherwise, participants were classified as having “normotension”. TG status was classified as “normal TG (< 1.7 mmol/L)” or “HTG (≥ 1.7 mmol/L)” according to the cutoff recommended for identifying elevated TG in Chinese populations17.
In addition to analyzing the separate associations of EBW, HTN, and HTG with hyperglycemia, participants were categorized into sub-groups based on two- and three-factor combinations to examine the joint associations with hyperglycemia. For the two-factor combinations: (1) Participants were grouped as non-EBW + normal BP (reference), non-EBW + HTN, overweight + normal BP, overweight + HTN, obesity + normal BP, or obesity + HTN (highest risk) to assess the combined association of EBW and HTN with hyperglycemia; (2) Participants were categorized as non-EBW + normal TG (reference), non-EBW + HTG, overweight + normal TG, overweight + HTG, obesity + normal TG, or obesity + HTG (highest risk) to evaluate the combined association of EBW and HTG with hyperglycemia; and (3) Participants were classified as normal BP + normal TG (reference), normal BP + HTG, HTN + normal TG, or HTN + HTG (highest risk) to assess the combined association of HTN and HTG with hyperglycemia.
Furthermore, for the three-factor combinations, participants were grouped as follows: non-EBW + normal BP + normal TG (reference), non-EBW + normal BP + HTG, non-EBW + HTN + normal TG, non-EBW + HTN + HTG, overweight + normal BP + normal TG, overweight + normal BP + HTG, overweight + HTN + normal TG, overweight + HTN + HTG, obesity + normal BP + normal TG, obesity + normal BP + HTG, obesity + HTN + normal TG, or obesity + HTN + HTG (highest risk) to investigate the three-factor combined associations with hyperglycemia.
Covariates
Potential influencing factors associated with hyperglycemia or diabetes—including socio-demographic attributes, lifestyle and behaviors, and family history of diabetes—were treated as covariates in the multivariate regression analysis. The socio-demographic factors adjusted for in analysis included age (60–69, 70–79, or 80 + years), sex (men or women), area of residence (urban or rural), educational level (≤ 6, 7–12, or 13 + years of schooling), marital status (single or with a spouse/partner), and type of health insurance (resident basic medical insurance [RBMI] or employee basic medical insurance [EBMI]).
Definitions of family history of diabetes, smoking, and drinking were adopted from those used in the official survey of Chinese chronic non-communicable disease and risk factor surveillance14. Participants were classified as having a positive family history of diabetes (“Yes”) if one of their parents had been diagnosed with diabetes. Otherwise, the participants were categorized as having a negative family history of diabetes (“No”)14. In addition, participants were classified as either “smoker” or “non-smoker”, and “drinker” or “non-drinker” in the analysis14.
PA level was measured using the validated Chinese version of the International Physical Activity Questionnaire (IPAQ-CHN)18,19. Participants were categorized as having “sufficient PA (≥ 150 min/week)” or “insufficient PA (< 150 min/week)” based on the total time spent in moderate PA plus twice the time spent in vigorous PA during the past 7 days20. Meat and fruit intake were assessed using a validated Chinese version of the Food Frequency Questionnaire (FFQ)21, which collected data on consumption frequency in the previous week. Based on weekly intake frequency recommendations for older Chinese adults from the Chinese Nutrition Society22, participants were classified as either “reached recommendation (Yes)” or “did not reach recommendation (No)” for meat and fruit intake, respectively. Participants with HTN or HTG were asked to report whether they were taking medications to manage these conditions. Accordingly, they were categorized as either “taking medications” or “not taking medications” in the analysis.
Data analysis
First, differences in selected participant characteristics (%) by sex and blood glucose status were examined separately using the Chi-square test. Then, mixed-effects logistic regression models were applied to calculate odds ratios (ORs) and 95% confidence intervals (CIs) for evaluating the separate and combined associations of EBW, HTN, and HTG with hyperglycemia among non-diabetic older adults. Model 1 was a univariate analysis, where body weight, BP, TG, or their combined measures served as the single independent variable, and the survey community was included as a random effect. Model 2 was a multivariate analysis, adjusting for age, sex (overall participants only), urban/rural residence, educational attainment, marital status, health insurance, PA, smoking, drinking, meat and fruit consumption, family history of diabetes, medication use for managing HTN or HTG, and—where applicable—body weight status, BP status, and TG status, in addition to the variable(s) considered in Model 1. The significance level was set at p < 0.05 (two-sided). EpiData version 3.1 (The EpiData Association, 2008, Odense, Denmark) and SPSS version 25.0 for Windows (SPSS Inc., Chicago, IL, USA) were used for data entry and analysis, respectively.
Results
Selected characteristics of participants
Among the 26,769 non-diabetic individuals analyzed in this study, 48.8% were men and 48.2% lived in urban areas, while 6.0% were aged 80 years or older and 8.6% had attained a college-level education. Additionally, 14.0%, 57.2%, and 27.8% of participants had obesity, HTN, and HTG, respectively (Table 1). The prevalence of hyperglycemia was 16.3% (95%CI = 15.8, 16.7), 17.6% (95%CI = 16.9, 18.3), and 15.0% (95%CI = 14.4, 15.6) among overall participants, men, and women, respectively (Table 2). Moreover, all the selected characteristics of participants differed significantly by sex and by hyperglycemia status.
Individual and two-factor combined associations of EBW, HTN, and HTG with hyperglycemia
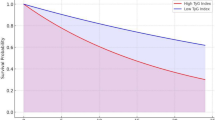
Figure 2a displays the individual and two-factor combined associations of EBW, HTN, and HTG with hyperglycemia among non-diabetic older adults aged 60 years and above in China. After adjusting for potential confounders, both individual and two-factor combined associations of EBW, HTN, and HTG with hyperglycemia were found to be statistically significant. Individually, overweight (adj.OR = 1.41, 95%CI = 1.31, 1.52) and obese (adj.OR = 2.07, 95%CI = 1.88, 2.28) participants had a higher likelihood of hyperglycemia compared to their non-EBW counterparts. Individuals with HTN were also at increased risk (adj.OR = 1.45, 95%CI = 1.32, 1.59) relative to normotensive participants. Furthermore, older adults with HTG were 1.73 times more likely (95%CI = 1.61, 1.86) to experience hyperglycemia compared to those with normal TG levels.
(a) The individual and two-factor combined associations of body weight, blood pressure and triglyceride with hyperglycemia among overall participants aged 60 + years in Nanjing, China (N = 26, 769). Footnotes: 1 Body weight status (non-excess: BMI < 24; overweight: BMI = 24–27; obese: BMI ≥ 28) was categorized based on recommendations for Chinese adults using body mass index (BMI). 2 Hypertension (HTN) referred to that either the objectively-measured systolic/diastolic blood pressure exceeded 140/90 mmHg or diagnosed hypertension. 3 Triglyceride status was classified as normal (< 1.7mmol/L) and hypertriglyceridemia (HTG) (≥ 1.7mmol/L) according to Chinese Guidelines for Lipid Management (2023). 4 Hyperglycemia was defined as objectively-assessed fasting venous blood glucose concentration ≥ 6.1mmol/L. 5 OR: odds ratios; 95%CI: 95% confidence interval. 6 Model 1 was a univariate analysis, where body weight, BP, TG, or their combined measures served as the single independent variable, and the survey community was included as a random effect. 7 Model 2 was a multivariate analysis, adjusting for age, sex (overall participants only), urban/rural residence, educational attainment, marital status, health insurance, PA, smoking, drinking, meat and fruit consumption, family history of diabetes, medication use for managing HTN or HTG, and—where applicable—body weight status, BP status, and TG status, in addition to the variable(s) considered in Model 1. (b) The individual and two-factor combined associations of body weight, blood pressure and triglyceride with hyperglycemia among men aged 60 + years in Nanjing, China (N = 13, 052). Footnotes : 1 Body weight status (non-excess: BMI < 24; overweight: BMI = 24–27; obese: BMI ≥ 28) was categorized based on recommendations for Chinese adults using body mass index (BMI). 2 Hypertension (HTN) referred to that either the objectively-measured systolic/diastolic blood pressure exceeded 140/90 mmHg or diagnosed hypertension. 3 Triglyceride status was classified as normal (< 1.7mmol/L) and hypertriglyceridemia (HTG) (≥ 1.7mmol/L) according to Chinese Guidelines for Lipid Management (2023). 4 Hyperglycemia was defined as objectively-assessed fasting venous blood glucose concentration ≥ 6.1mmol/L. 5 OR: odds ratios; 95%CI: 95% confidence interval. 6 Model 1 was a univariate analysis, where body weight, BP, TG, or their combined measures served as the single independent variable, and the survey community was included as a random effect. 7 Model 2 was a multivariate analysis, adjusting for age, sex (overall participants only), urban/rural residence, educational attainment, marital status, health insurance, PA, smoking, drinking, meat and fruit consumption, family history of diabetes, medication use for managing HTN or HTG, and—where applicable—body weight status, BP status, and TG status, in addition to the variable(s) considered in Model 1. (c) The individual and two-factor combined associations of body weight, blood pressure and triglyceride with hyperglycemia among women aged 60 + years in Nanjing, China (N = 13, 717). Footnotes : 1 Body weight status (non-excess: BMI < 24; overweight: BMI = 24–27; obese: BMI ≥ 28) was categorized based on recommendations for Chinese adults using body mass index (BMI). 2 Hypertension (HTN) referred to that either the objectively-measured systolic/diastolic blood pressure exceeded 140/90 mmHg or diagnosed hypertension. 3 Triglyceride status was classified as normal (< 1.7mmol/L) and hypertriglyceridemia (HTG) (≥ 1.7mmol/L) according to Chinese Guidelines for Lipid Management (2023). 4 Hyperglycemia was defined as objectively-assessed fasting venous blood glucose concentration ≥ 6.1mmol/L. 5 OR: odds ratios; 95%CI: 95% confidence interval. 6 Model 1 was a univariate analysis, where body weight, BP, TG, or their combined measures served as the single independent variable, and the survey community was included as a random effect. 7 Model 2 was a multivariate analysis, adjusting for age, sex (overall participants only), urban/rural residence, educational attainment, marital status, health insurance, PA, smoking, drinking, meat and fruit consumption, family history of diabetes, medication use for managing HTN or HTG, and—where applicable—body weight status, BP status, and TG status, in addition to the variable(s) considered in Model 1.
Compared to those with non-EBW and normal BP, participants with non-EBW and HTN (adj.OR = 1.54, 95%CI = 1.36, 1.75), overweight and normal BP (adj.OR = 1.50, 95%CI = 1.33, 1.69), overweight and HTN (adj.OR = 2.08, 95%CI = 1.84, 2.35), obesity and normal BP (adj.OR = 2.23, 95%CI = 1.87, 2.67), or obesity and HTN (adj.OR = 3.07, 95%CI = 2.67, 3.52) were more likely to experience hyperglycemia.
Relative to participants with non-EBW and normal TG, older adults with non-EBW and HTG (adj.OR = 1.89, 95%CI = 1.67, 2.13), overweight and normal TG (adj.OR = 1.48, 95%CI = 1.35, 1.62), overweight and HTG (adj.OR = 2.41, 95%CI = 2.17, 2.68), obesity and normal TG (adj.OR = 2.13, 95%CI = 1.88, 2.41), or obesity and HTG (adj.OR = 3.67, 95%CI = 3.22, 4.18) also had higher odds of experiencing hyperglycemia.
For the combined groups of BP and TG, participants with normal BP and HTG (adj.OR = 1.77, 95%CI = 1.57, 2.00), HTN and normal TG (adj.OR = 1.47, 95%CI = 1.32, 1.63), or HTN and HTG (adj.OR = 2.51, 95%CI = 2.23, 2.82) were at higher risk of hyperglycemia compared with their counterparts who had both normal BP and TG.
Three-factor combined associations of EBW, HTN, and HTG with hyperglycemia
Figure 3a presents the three-factor combined associations of EBW, HTN, and HTG with hyperglycemia among all non-diabetic older adults aged 60 years and above in China. Compared to participants whose body weight, BP, and TG were all normal, those who had: non-EBW and normal BP and HTG (adj.OR = 1.77, 95%CI = 1.46, 2.14), non-EBW and HTN and normal TG (adj.OR = 1.49, 95%CI = 1.29, 1.73), non-EBW and HTN and HTG (adj.OR = 2.93, 95%CI = 2.45, 3.49), overweight and normal BP and normal TG (adj.OR = 1.48, 95%CI = 1.28, 1.71), overweight and normal BP and HTG (adj.OR = 2.68, 95%CI = 2.26, 3.17), overweight and HTN and normal TG (adj.OR = 2.19, 95%CI = 1.90, 2.52), overweight and HTN and HTG (adj.OR = 3.40, 95%CI = 2.92, 3.96), obesity and normal BP and normal TG (adj.OR = 2.36, 95%CI = 1.88, 3.97), obesity and normal BP and HTG (adj.OR = 3.64, 95%CI = 2.80, 4.73), obesity and HTN and normal TG (adj.OR = 3.05, 95%CI = 2.58, 3.60), or obesity and HTN and HTG (adj.OR = 5.42, 95%CI = 4.56, 6.44) were more likely to experience hyperglycemia.
(a) The three-factor combined associations of body weight, blood pressure and triglyceride with hyperglycemia among overall participants aged 60 + years in Nanjing, China (N = 26, 769). Footnotes : 1 Body weight status (non-excess: BMI < 24; overweight: BMI = 24–27; obese: BMI ≥ 28) was categorized based on recommendations for Chinese adults using body mass index (BMI). 2 Hypertension (HTN) referred to that either the objectively-measured systolic/diastolic blood pressure exceeded 140/90 mmHg or diagnosed hypertension. 3 Triglyceride status was classified as normal (< 1.7mmol/L) and hypertriglyceridemia (HTG) (od pressure exceeded 140/90 mmHg Guidelines for Lipid Management (2023). 4 Hyperglycemia was defined as objectively-assessed fasting venous blood glucose concentration ≥ 6.1mmol/L. 5 OR: odds ratios; 95%CI: 95% confidence interval. 6 Model 1 was a univariate analysis, where body weight, BP, TG, or their combined measures served as the single independent variable, and the survey community was included as a random effect. 7 Model 2 was a multivariate analysis, adjusting for age, sex (overall participants only), urban/rural residence, educational attainment, marital status, health insurance, PA, smoking, drinking, meat and fruit consumption, family history of diabetes, medication use for managing HTN or HTG, and—where applicable—body weight status, BP status, and TG status, in addition to the variable(s) considered in Model 1. (b) The three-factor combined associations of body weight, blood pressure and triglyceride with hyperglycemia among men aged 60 + years in Nanjing, China (N = 13, 052). Footnotes : 1 Body weight status (non-excess: BMI < 24; overweight: BMI = 24–27; obese: BMI ≥ 28) was categorized based on recommendations for Chinese adults using body mass index (BMI). 2 Hypertension (HTN) referred to that either the objectively-measured systolic/diastolic blood pressure exceeded 140/90 mmHg or diagnosed hypertension. 3 Triglyceride status was classified as normal (< 1.7mmol/L) and hypertriglyceridemia (HTG) (≥ 1.7mmol/L) according to Chinese Guidelines for Lipid Management (2023). 4 Hyperglycemia was defined as objectively-assessed fasting venous blood glucose concentration ≥ 6.1mmol/L. 5 OR: odds ratios; 95%CI: 95% confidence interval. 6 Model 1 was a univariate analysis, where body weight, BP, TG, or their combined measures served as the single independent variable, and the survey community was included as a random effect. 7 Model 2 was a multivariate analysis, adjusting for age, sex (overall participants only), urban/rural residence, educational attainment, marital status, health insurance, PA, smoking, drinking, meat and fruit consumption, family history of diabetes, medication use for managing HTN or HTG, and—where applicable—body weight status, BP status, and TG status, in addition to the variable(s) considered in Model 1. (c) The three-factor combined associations of body weight, blood pressure and triglyceride with hyperglycemia among women aged 60 + years in Nanjing, China (N = 13, 717). Footnotes : 1 Body weight status (non-excess: BMI < 24; overweight: BMI = 24–27; obese: BMI ≥ 28) was categorized based on recommendations for Chinese adults using body mass index (BMI). 2 Hypertension (HTN) referred to that either the objectively-measured systolic/diastolic blood pressure exceeded 140/90 mmHg or diagnosed hypertension. 3 Triglyceride status was classified as normal (< 1.7mmol/L) and hypertriglyceridemia (HTG) (≥ 1.7mmol/L) according to Chinese Guidelines for Lipid Management (2023). 4 Hyperglycemia was defined as objectively-assessed fasting venous blood glucose concentration ≥ 6.1mmol/L. 5 OR: odds ratios; 95%CI: 95% confidence interval. 6 Model 1 was a univariate analysis, where body weight, BP, TG, or their combined measures served as the single independent variable, and the survey community was included as a random effect. 7 Model 2 was a multivariate analysis, adjusting for age, sex (overall participants only), urban/rural residence, educational attainment, marital status, health insurance, PA, smoking, drinking, meat and fruit consumption, family history of diabetes, medication use for managing HTN or HTG, and—where applicable—body weight status, BP status, and TG status, in addition to the variable(s) considered in Model 1.
Notably, the significant associations of EBW, HTN, and HTG with hyperglycemia were independent of each other among participants. Moreover, for both men and women, the pattern of individual, two-factor, and three-factor combined associations of EBW, HTN, and HTG with hyperglycemia were similar to those observed among overall participants in this study (Figs. 2b and c and 3b and c).
Discussion
In this large-scale population study, we aimed to explore the individual and combined associations of EBW, HTN, and HTG with hyperglycemia among non-diabetic individuals aged 60 years and above in regional China. It was observed that EBW, HTN, and HTG were each independently and positively associated with hyperglycemia. Moreover, joint associations were found for two- and three-factor combinations of EBW, HTN, and HTG with hyperglycemia. As expected, participants with all three conditions were at a higher risk of experiencing hyperglycemia compared to the two-factor combinations.
The findings regarding the individual associations of EBW, HTN, and HTG with hyperglycemia in this study are consistent with previous reports6,7,8. This may be partly explained by the fact that EBW, HTN, and HTG share some common risk factors—such as unhealthy diet and physical inactivity—with hyperglycemia8. Additionally, there are potential biological mechanisms underlying these associations: (1) The positive relationship between EBW and hyperglycemia may be due to the fact that EBW can cause insulin resistance and even early β-cell failure23. (2) The association between HTN and hyperglycemia may be attributed to the reduction in insulin delivery caused by decreased skeletal muscle blood flow and insulin sensitivity24. (3) The link between HTG and hyperglycemia may stem from the ability of HTG to reduce insulin sensitivity25 and stimulate insulin secretion26, which may progressively result in negative feedback on insulin production27,28.
Notably, EBW, HTN, and HTG can independently reduce insulin sensitivity and subsequently contribute to hyperglycemia23,24,25,26,27,28. Therefore, it is reasonable to infer that these conditions may act synergistically to reinforce insulin resistance and exert a compounded effect on hyperglycemia. In this study, individuals with any one of these conditions were more likely to experience hyperglycemia than those without. Moreover, participants with two conditions had a higher risk than those with only one, and those with all three conditions had the greatest risk of hyperglycemia.
Individuals living with obesity who had HTN and HTG were at the highest risk of hyperglycemia, a 5.42-fold increase in odds. Overweight adults with HTN and HTG were also 3.40 times more likely to experience hyperglycemia compared to those with normal body weight, BP, and TG. Importantly, the combined associations of EBW, HTN, and HTG with hyperglycemia were observed not only among the overall participants but also consistently among both men and women. This suggests that such combined associations may hold true for the general population of older adults aged 60 years and above in China. Therefore, the findings from this study provide solid epidemiological evidence of a joint relationship between EBW, HTN, HTG, and hyperglycemia among community-based, non-diabetic older individuals in China.
This study carries significant implications for population-level prevention of hyperglycemia. Based on the findings, the more conditions—EBW, HTN, and HTG—participants have, the higher their risk of developing hyperglycemia. For each individual, it is essential to identify the presence of these conditions as early as possible, self-evaluate the associated risk, and take personalized, targeted actions to prevent hyperglycemia, such as managing body weight, BP, and TG levels. From a public health perspective, it is equally important to implement individualized, combined intervention programs targeting EBW, HTN, and HTG to reduce the population-level burden of hyperglycemia.
This study had several strengths. First, the eligible participants were non-diabetic older residents aged 60 years and above, which ensured that their lifestyle and behaviors were unlikely to have been intentionally modified due to a diabetes diagnosis. Second, the sample size exceeded 26,000, and all participants were randomly selected from across the entire municipality of Nanjing. As such, the study population could be representative of the approximately 1.5 million older residents in the region. Third, body weight and height, BP, FPG, and TG levels were objectively measured using standardized procedures for each participant. Fourth, classical confounding factors associated with hyperglycemia and diabetes—including socio-demographic characteristics, lifestyle and behaviors, and family history of diabetes—were adjusted for in the analysis. Fifth, as many as 12 combinations of body weight, BP, and TG were used to assess joint associations with hyperglycemia. This approach may inform personalized intervention strategies targeting EBW, HTN, and HTG for the prevention of hyperglycemia. Finally, the combined associations of EBW, HTN, and HTG with hyperglycemia were identified not only among all participants but also within sex-specific subgroups, suggesting that the findings may be generalizable to the broader older adult population.
Several limitations should also be acknowledged. First, although residents with diagnosed diabetes were excluded from the study, it is still possible that some participants had undiagnosed diabetes. Second, data on family history of diabetes, lifestyle, and behaviors were self-reported by participants, which may have introduced recall bias. Third, the cross-sectional nature of the study limits the causal relationship between body weight, BP, TG, and hyperglycemia, although the lifestyles and behaviors of non-diabetic participants were assumed to be unaltered. Fourth, participants with HTN or HTG were only asked whether they were taking medications to manage their conditions, without details on specific medications. This limitation prevented adjustment for exact medication types in the analysis. Fifth, due to the non-normal distribution of meat and fruit intake frequencies and only binary classification (“recommendation reached” or “not reached”) recommended by the Chinese Nutrition Society, over-nutrition could not be adequately assessed using continuous or multi-level intake categories. It is worth noting that such binary classifications may not fully capture the potential influence of meat and fruit consumption on blood glucose metabolism in this diabetes-related study. Nevertheless, these factors were not primary explanatory variables but were included as covariates. In future research, longitudinal and/or intervention studies are recommended to explore the causal combined associations of EBW, HTN, and HTG with hyperglycemia among older adults and other age groups in China and globally.
Conclusions
In conclusion, EBW, HTN, and HTG were each independently and positively associated with hyperglycemia among older adults aged 60 years and above, including both men and women, in China. Furthermore, any combination of these conditions added incremental risk, with individuals who were obese and had both HTN and HTG facing the highest risk. These findings carry important public health implications, suggesting that personalized interventions targeting EBW, HTN, and HTG together may be an effective strategy for preventing hyperglycemia at the population-level.
Data availability
The data involved in this work are available upon reasonable request to corresponding author FX or WT.
References
World Health Organization. Global Report on Diabetes 2016. Geneva: World Health Organization (2024).
World Health Organization. Health topics. Diabetes. Fact sheets (2025, accessed 3 Jul 2025). https://www.who.int/news-room/fact-sheets/detail/diabetes.
Rooney, M. R. et al. Global prevalence of prediabetes. Diabetes Care. 46 (7), 1388–1394. https://doi.org/10.2337/dc22-2376 (2023).
Center for Disease Control and Prevention, Diabetes & Diabetes Data and Statistics. National Diabetes Statistics Report. Fast Facts on Diabetes (2024, accessed 3 Jul 2023). https://www.cdc.gov/diabetes/php/data-research/methods.html?CDC_AAref_Val=https://www.cdc.gov/diabetes/data/statistics-report/index.html.
Wang, L. et al. Prevalence and treatment of diabetes in china, 2013–2018. JAMA 326 (24), 2498–2506. https://doi.org/10.1001/jama.2021.22208 (2021).
World Health Organization. Health topic. Diabetes. Prevention and Treatment (2024, accessed 11 May 2024). https://www.who.int/health-topics/diabetes#tab=tab_3.
World Health Organization. Definition, Diagnosis, and Classification of Diabetes Mellitus and its Complications. Geneva: World Health Organization 1999. Report of a WHO Consultation (1999).
American Diabetes Association Professional Practice Committee. Diagnosis and classification of diabetes: standards of care in Diabetes-2024. Diabetes Care. 2 (S1), S20–S42. https://doi.org/10.2337/dc24-S002 (2024).
Nanjing Municipal Bureau of Statistics. Nanjing Statistical Yearbook (2023, accessed 17 Feb 2023). https://tjj.nanjing.gov.cn/material/njnj_2023/renkou/3-6.htm.
Zhang, G. et al. Meat, vegetable, and fruit consumption among urban and rural elders aged 60 + years in regional china: a population-level nutritional study. J. Nutr. Sci. 12, e120. https://doi.org/10.1017/jns.2023.104 (2023).
The Joint working team against COVID-19, The State Council of China. The overall plan for implementation of Class B management approaches for Class B infectious disease against COVID-19 : 144) (2022, accessed 17 Feb 2023). http://www.nhc.gov.cn/xcs/zhengcwj/202212/e97e4c449d7a475794624b8ea12123c6.shtml.
Uusitupa, M. et al. Prevention of type 2 diabetes by lifestyle changes: a systematic review and Meta-Analysis. Nutrients 11 (11), 2611. https://doi.org/10.3390/nu11112611 (2019).
Hansen, A. H., Wangberg, S. C. & Årsand, E. Lifestyle changes among people with type 2 diabetes are associated with participation in online groups and time since diagnosis. BMC Health Serv. Res. 21 (1), 688. https://doi.org/10.1186/s12913-021-06660-5 (2021).
Wang, L. et al. Scheme of the Chinese chronic non-communicable disease and risk factor surveillance. Chin. J. Prev. Med. 52, 191–194. https://doi.org/10.3760/cma.j.issn.0253-9624.2018.02.015 (2018).
Writing Group. The guidelines for the primary management of hypertension in China (2014 Edition). Chin. J. Health Manage. 9, 10–30. https://doi.org/10.3760/cma.j.issn.1674-0815.2015.01.004 (2015). (In Chinese).
Writing group. Clinical guidelines for prevention and treatment of type 2 diabetes in older Chinese people (2022 Edition). Chin. J. Diabetes. 30 (1), 2–51. https://doi.org/10.3969/j.issn.1006-6187.2022.01.002 (2022). (In Chinese).
Joint Committee on the Chinese Guidelines for Lipid Management. Chin. Circul. J. 38 (3), 237–271. https://doi.org/10.3969/j.issn.1000-3614.2023.03.001 (2023).
Qu, N. N. & Li, K. J. Study on the reliability and validity of international physical activity questionnaire. Chin. J. Epidemiol. 25, 265–268 (2004). (In Chinese).
Deng, H. B. et al. Reliability and validity of the IPAQ–Chinese: the Guangzhou biobank cohort study. Med. Sci. Sports Exerc. 40, 303–307. https://doi.org/10.1249/mss.0b013e31815b0db5 (2008).
Composing and Editorial Board of Physical Activity Guidelines for Chinese Physical activity guidelines for Chinese (2021). Chin. J. Epidemiol. 43 (1), 5–6. https://doi.org/10.1016/S1004-9541(22)00137-9 (2022). (In Chinese).
Liu, D. et al. Establishment and application of food frequency questionnaire method among Chinese. J. Hygiene Res. 47 (5), 744–755 (2018). (In Chinese).
Chinese Nutrition Society. China Elderly Dietary Guidelines (People’s medical publishing house, 2016).
Ruze, R. et al. Obesity and type 2 diabetes mellitus: connections in epidemiology, pathogenesis, and treatments. Front. Endocrinol. 14, 1161521. https://doi.org/10.3389/fendo.2023.1161521 (2023).
Sowers, J. R. Insulin resistance and hypertension. Am. J. Physiol. Heart Circ. Physiol. 286, H1597–H1602. https://doi.org/10.1152/ajpheart.00026.2004 (2004).
Baldi, S. et al. Influence of apolipoproteins on the association between lipids and insulin sensitivity: a cross-sectional analysis of the RISC study. Diabetes Care. 36 (12), 4125–4131. https://doi.org/10.2337/dc13-0682 (2013).
Natali, A. et al. RISC investigators. Plasma HDL-cholesterol and triglycerides, but not LDL-cholesterol, are associated with insulin secretion in non-diabetic subjects. Metabolism 69, 33–42. https://doi.org/10.1016/j.metabol.2017.01.001 (2017).
Mosser, R. E. et al. High-fat diet-induced β-cell proliferation occurs prior to insulin resistance in C57Bl/6J male mice. Am. J. Physiol. Endocrinol. Metab. 308 (7), E573–E582. https://doi.org/10.1152/ajpendo.00460.2014 (2015).
Sone, H. & Kagawa, Y. Pancreatic beta cell senescence contributes to the pathogenesis of type 2 diabetes in high-fat diet-induced diabetic mice. Diabetologia 48 (1), 58–67. https://doi.org/10.1007/s00125-004-1605-2 (2005).
Acknowledgements
Our special thanks go to all workers from local communities for their kind assistance in field data collection.
Funding
This present work was supported by Jiangsu Province Key R&D Plan Social Development Project (BE2023774; Recipient: Wei Tang).
Author information
Authors and Affiliations
Contributions
WT and FX conceived and designed the present study. XO, LG, TX TD and FX are responsible for data acquisition. FX analyzed the data. WT and FX obtained financial support. XO, LG, TX, TD, HX, YX, GA, WT and FX wrote and critically reviewed the manuscript. Each author approved the final version for submission and was also responsible for all aspects of the work presented in this manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Written informed consent was obtained from all participants prior to the survey. The Ethics Committee of Nanjing Medical University Affiliated Nanjing Municipal Center for Disease Prevention and Control approved the original data collection protocol. All methods used in this study adhered to the principles outlined in the Declaration of Helsinki. For the present analysis, only de-identified secondary data were used. Therefore, the Ethics Committee of Geriatric Hospital of Nanjing Medical University granted a waiver of ethical approval.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ouyang, X., Gu, L., Xu, T. et al. The combined associations of excess body weight, hypertension, and hypertriglyceridemia with hyperglycemia among nondiabetic older adults in regional China. Sci Rep 15, 30999 (2025). https://doi.org/10.1038/s41598-025-16879-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-16879-5