Abstract
Transcutaneous auricular vagus nerve stimulation (taVNS) is a promising technique that potentially influences cortical activity, mainly increasing electroencephalography (EEG) power spectrum activity in low-frequency oscillations, and demonstrates potential therapeutic benefits for various pathologic conditions, like depression and chronic pain. To learn further about taVNS brain mechanisms, the present study investigated how using a single taVNS session can affect brain oscillations in healthy subjects. 44 healthy participants were included in this randomized, double-blind, sham-controlled trial. Participants were divided into the active and sham taVNS groups. Resting-state EEG power was analyzed across the frontal, central, and parietal regions in both hemispheres. Our findings demonstrated that active taVNS modulates low-frequency oscillations in the frontal areas of healthy subjects. After the intervention, the average delta power at the frontal region increased in the active group compared to the sham group. These changes were also observed with an increase in delta asymmetry (towards the right hemisphere) in the active group compared to the sham group. In healthy subjects, active taVNS selectively induces changes in the resting-state frontal brain oscillations. Our results suggest that taVNS increases homeostatic low-frequency oscillatory activity mainly over the right frontal hemisphere. Active taVNS induces activation of the fronto-vagal network, which has a therapeutic potential to generate salutogenic and balanced brain activity.
Similar content being viewed by others
Introduction
Transcutaneous auricular vagus nerve stimulation (taVNS) is a non-invasive neuromodulation technique in which electrodes are placed on the tragus or concha of the ear. Delivered through a portable device, taVNS is more accessible and poses as a less risky approach to patients in comparison to the surgically implanted vagus nerve stimulators1. Stimulation of vagal afferents through taVNS can influence several brain structures. For instance, the locus coeruleus (LC), a crucial adrenergic center, receives inputs from the vagus nerve and is linked to the nucleus of the solitary tract (NST)2. The frontal and parietal cortex, thalamic nucleus, and hippocampal regions are among the cortical and subcortical structures that receive projections from the locus coeruleus; therefore, modulation of these areas forms the basis for the potential mechanisms of taVNS1.
The taVNS field has grown exponentially in the last few years, although most studies have focused on possible clinical applications across several health conditions3. There is still much to discuss about taVNS mechanisms and its effects on biological processes. Studying taVNS physiological effects must, ideally, include neurophysiological markers, indicative of the vagus nerve stimulation pathways and its impact on the different brain structures and functions. This approach would make it possible for more extensive exploration and insightful understanding of the mechanisms and therapeutic effects of taVNS. So far, potential biomarkers are under investigation, including autonomic nervous system activation, functional neuroimaging, and brain electrical activity4,5,6,7. Despite some progress, more mechanistic studies involving healthy participants remain scarce.
Electroencephalography (EEG) has emerged as a promising taVNS biomarker, due to its cost-effective and non-invasive nature to assess cortical activity from the target areas activated during or after taVNS. Resting state EEG captures the spontaneous brain oscillation networks and top-down or endogenous regulation activities of sensory, cognitive, and motor functions, which can be predictive of health outcomes8. Previous studies on invasive VNS in epileptic subjects demonstrated that it acutely alters brain network activity by changing slow EEG oscillation activities in a dose-dependent manner, that is, the delta-theta spectra9,10. Preliminary sham-controlled resting-state EEG studies in healthy adults have pointed out potential short-term effects of taVNS on brain oscillations that need further investigation6. They showed taVNS increased delta spectral power over several scalp areas and attenuated occipital alpha power11,12. Furthermore, a prior systematic review demonstrated that taVNS could induce spectral power changes in low-frequency bands (delta and theta)13. However, more robust, well-designed studies on the effects of taVNS on brain activity are necessary to overcome the substantial degree of heterogeneity in preliminary studies.
Another promising EEG metric is oscillations asymmetry, which reflects interhemispheric functional differences in resting brain activity throughout different health conditions, especially in psychopathology14. The clinical and physiological implications of asymmetrical relationships in brain oscillations are still being discussed. However, it is suggested that asymmetries may reflect the role of different cortical areas in sensory, motor, and psychological function14. Yet, in the context of taVNS, this metric has not been explored.
Based on the premise that quantitative EEG can be used to evaluate how taVNS affects brain activity and based on preliminary results, we expected increases in resting-state lower frequency oscillations after stimulation, although other metrics in the spectrum of the alpha band might also change. Therefore, the primary objective of our study was to investigate acute changes in resting state EEG oscillations, with focus on low frequency bands, after taVNS in healthy adults, and secondarily to assess whether taVNS can induce interhemispheric asymmetries in EEG oscillations activity.
Results
Participants
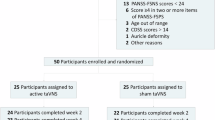
A total of 44 healthy subjects were included in this study from a total of 204 subjects screened (Figs. 1 and 2) between May and September 2023. 160 participants were excluded during the screening process, and 6 participants dropped out before randomization. The final sample included 22 subjects allocated to the active taVNS group, and 22 subjects allocated to the sham taVNS group. There were no dropouts after randomization.
Demographic and clinical characteristics
We collected information regarding age, gender, ethnicity, race, education, fatigue, and mood levels. Further clinical variables and sample characteristics are provided in Table 1.
Brain oscillations and asymmetry findings
All 44 participants were included in the EEG analysis, divided into the sham group or active group. The resting-state EEG power unadjusted findings of the frontal, central, and parietal regions are provided in Tables 2, 3 and 4, respectively, presenting results for the sham group and active group. Moreover, we presented topographic distributions of absolute power in delta (Fig. 3), theta, alpha, and beta (Fig. 4). An increased activity was observed qualitatively in the topographic plots, especially in the delta band.
Topographic distribution of scalp plots in resting-state EEG: (a) theta power (4 to 7.9 Hz, range 35 to 40 dB, 10 x log10); (b) alpha power (8 to 12.9 Hz, range 35 to 40 dB, 10 x log10); and (c) beta power (13 to 29.9 Hz, range 23 to 29 dB, 10 x log10). The y-axis represents the groups: sham (top) and active (bottom). The x-axis represents the timeline: pre-intervention (left) and post-intervention (right).
No significant differences were found between the baseline EEG measurements. We used the differences of the EEG metrics (post minus pre) to calculate the intervention effects. Frontal delta power showed a medium positive effect of active taVNS compared to sham (Cohen’s d = 0.60, 95% CI [–0.01 to 1.20]), corresponding to an adjusted model demonstrating a significant increase in the active taVNS compared to sham (β = 0.085; CI [0.011, 0.159]; p = 0.025). This increase was present predominantly in the right hemisphere with the largest and most consistent effect (Cohen’s d = 0.82, 95% CI [0.20 to 1.44]) and adjusted model between-group difference (β = 0.107; CI [0.035, 0.180]; p = 0.004). Left frontal delta changes were smaller (Cohen’s d = 0.46, 95% CI [–0.15 to 1.06]) and did not reach statistical significance in the adjusted model (β = 0.075; CI [− 0.011, 0.161]; p = 0.084). No significant changes were observed in the relative power of other frequency bands (theta, alpha, and beta). Additionally, when analyzing the possible effect modification of subgroups such as age, biological sex, race (white vs. non-white), or adequate mood levels at baseline, this revealed no significant effect modification (model interaction p-values: 0.26, 0.84, 0.37, 0.13, respectively), which suggests a homogenous effect across subgroups.
The linear mixed-effects model analyses revealed region-specific effects of group, time, and their interaction on delta band power, confirming the directions observed in our linear regression models. In the frontal region, the group x time interaction demonstrated an increase in delta oscillations in the active group compared to the sham group (β = 0.074, 95% CI [0.003, 0.145], p = 0.042). In the right frontal region, we also observed in group x time interaction (β = 0.097, 95% CI [0.028, 0.166], p = 0.006), indicating that delta power increased in the active group post-intervention compared to the sham group. In contrast, the left frontal region showed no significant effects. Age and gender were not significant predictors of delta power in any region (p > 0.26). Intercepts in all models were significant (p < 0.001), reflecting the baseline delta power levels. Overall, these results suggest a stronger modulation of delta activity in the right frontal cortex, particularly in response to the active intervention.
Our asymmetry findings demonstrate an increase in delta power in the right frontal area as compared to the delta power in the left frontal area, as illustrated in Fig. 3. Consequently, our regression analysis (see Table 5) indicates a notable increase in delta asymmetry (favoring the right hemisphere) within the active group compared to the sham group (β = 0.042; CI [0.001, 0.089]; p = 0.045). However, statistical significance was not observed in the theta bands. Yet, the changes between delta and theta bands asymmetry demonstrate significant results (β = 0.040; CI [0.002, 0.078]; p = 0.041). Table 5 presents the alterations in delta and theta asymmetry observed in the frontal region, with results adjusted for age, gender, and fatigue. Despite our supplementary analysis, no statistically significant differences in FAA between the two groups were found post-intervention (β=-0.206; CI [-0.645, 0.232]; p = 0.347). Supplementary Table S2 displays the mean values of log frontal alpha power, followed by SD and p-value for each hemisphere pre- and post-intervention.
Adverse events and successful blinding
No serious or unanticipated negative events occurred. One participant in the active group reported transient tingling behind the left ear at the start of the stimulation, which resolved within five minutes. The session ended as scheduled. There were no significant group differences (sham taVNS: 0%, active taVNS: 4.55%, p = 0.31).
Regarding blinding efficacy, after the intervention, participants were asked to guess their group allocation. In total, 91% guessed incorrectly, and only 9% (n = 4) guessed correctly, indicating successful blinding. This result confirms that participants could not reliably distinguish between the interventions, which were identical in appearance and procedure to the active taVNS stimulation but delivering no current. The blinding process was further supported by the use of a team member, not involved with any assessments, who was only in charge of preparing and delivering the appropriate device to the blinded experimenter.
Discussion
The primary objective of our study was to investigate the effect of taVNS on resting-state brain oscillations and, secondarily, to assess whether it would cause an asymmetric increase in brain oscillations between the left and right hemispheres. Our main results showed an increase in frontal delta power and interhemispheric differences, favoring the right hemisphere, following active taVNS. No significant changes were observed in the power of other high-frequency bands. These findings reinforce over the safety of a bilateral taVNS, as no relevant adverse effects were reported. Smaller studies investigating taVNS and EEG have yielded mixed results on taVNS effects on EEG, and high levels of heterogeneity in study designs, outcomes, and experimental paradigms13. Based on the findings of previous studies, we decided to perform a bilateral taVNS study to modulate the neural activity in the afferent fibers of both vagus nerves for 60 min. This approach aimed to enhance the effectiveness and safety of this technique.
Our results showed that after taVNS intervention, the average delta power at the frontal region increased in the active group compared to the sham, and this increase was present predominantly in the right hemisphere. The observed increase in delta power is aligned with previous studies investigating the mechanism of action of VNS, both in healthy and epileptic individuals9,10,11. The stimulation intensity is an important metric for treatment response, but the direct association between taVNS intensity and delta oscillations has been poorly investigated in the literature, due to the high heterogeneity between studies13. This is one of the strengths of this pilot trial, as we could observe the effect of 1.5 mA of bilateral taVNS over resting low-frequency bands. Part of the taVNS effects might indirectly activate deep brain structures via thalamus, resulting in changes in cortical activity15. Thus, brain oscillations, as measured by EEG, may provide relevant metrics that can be used to measure and understand the mechanisms of taVNS, both to ensure the stimulation of the vagus nerve pathway and to measure its effects16,17.
Interestingly, Chen et al.18 observed widespread increases in pre-post stimulation resting state (eyes open) delta, theta, and alpha bands in an experiment aimed to measure the effect of taVNS on motor planning during a motor task. In contrast, our sham-controlled, eyes closed protocol in 44 healthy individuals, only frontal delta power changed because of the concomitant vagal stimulation. This may suggest that taVNS, even during dynamic tasks, can increase delta power, stressing the stability of this brain oscillation across different experimental paradigms, which is crucial should delta activity be a biomarker of taVNS.
Delta oscillations are related to the activity of the most ancient parts of the brain, associated with global processing modes, which influence the integration of different cortical areas and other faster brain oscillations19. While delta activity is recognized as the most prominent aspect of the non-rapid eye movement sleep produced in the cortex, its activity can increase in awake states during meditative practices, as observed by Yordanova et al.20suggesting a series of large-scale states present during meditation, serving as the source of top-down influences for the next state. Also, the widely distributed increase in delta seen during meditation indicates that the delta band is the primary frequency linked to the large-scale integrative mechanisms that support all subsequent states of meditation21,22,23. Studies on hemisphere asymmetries, both using neuropsychological and neuroimaging data, have demonstrated that the right hemisphere is biased in emotional and attentional functions24. For example, frontal alpha asymmetry at the resting state is thought to be predictive of future emotional behavior specificity or psychopathology25,26,27.
This latter characteristic associates delta activity with synaptic efficacy and sleep-dependent plasticity, suggested by several studies15,28,29. Alternatively, increases in delta activity have been associated with pathological deviations after subcortical damage, although similar findings were also found in healthy subjects30,31. These findings provide credence to the hypothesis that subcortical deep centers generate delta oscillations in the human brain, which play basic homeostatic roles and the integration of brain networks as a background brain activity32. Subcortical activation of brainstem nuclei connected to the vagus nerve and with serotonergic properties (NST, LC, raphe nuclei) may, therefore, account for the increase in resting-state EEG delta activity observed after taVNS33.
Considering these findings, an increase in delta oscillations in the frontal area and the absence of other brain oscillation increments, as observed in this trial, could indicate that taVNS can create a state in which more complex cerebral activity, such as higher cognitive processing, may decrease, giving room for more basic background processes, such as homeostatic and autonomic processing. In this context, asymmetries have been understood in terms of reallocating attentional resources to important stimuli that pose risks in terms of executive control during rest and stressful situations, both at baseline and under stress scenarios34,35 (i.e., whereas right-lateralized control limits processing of positive distractions, left-lateralized executive control would inhibit processing of negative distractions). For example, Razumnikova and Khoroshavtseva36 investigated the differences in brain activity between the resting state and the retrieval of good or negative emotional memories utilizing EEG in six frequency ranges, from delta to beta. They found alpha desynchronization at the posterior cortex accompanied memory retrieval, irrespective of the emotional valence, and showed a positive correlation between positive scores and beta oscillations at the left anterior temporal location, while negative emotion scores showed a positive correlation with the right temporal zone. On the other hand, their results could not find any correlations with delta oscillations.
Regarding the interhemispheric differences observed in delta band power, our study seems to be the first one to demonstrate that taVNS can modulate frontal delta asymmetrically. However, the meaning of this asymmetry remains hypothetical, as no previous evidence has demonstrated that the relationships of left-right frontal alpha asymmetry also apply for delta oscillations or if it is a consequence of lateralized natural physiological processes. observed in the brain for a bunch of functions that increase across the lifespan37. However, these possible explanations are not exclusive, as they may coexist with the possibility that taVNS asymmetrically modulates delta activity. Here we demonstrated that the observed effects were not dependent on mood, race, age, or sex. Therefore, further research should explore the clinical implications of asymmetrical modulation of delta activity and the proposed hypotheses.
In case of being a result of the neuromodulation, delta modulation (and asymmetrical delta modulation) perhaps could explain how taVNS alleviates psychophysical burden caused by emotional dysregulation, depression, anxiety, central fatigue, and chronic pain38,39,40proclaiming researchers to include delta oscillation asymmetry (and other EEG asymmetries) in VNS studies to explore the relationships between these oscillations asymmetries and response to treatment. Based on the functional roles attributed to delta oscillations in the human brain, it can be further hypothesized that for the mentioned conditions, taVNS may optimize frontal brain networks and the underlying brain states necessary for reducing excessive input and neural processing overloads, thereby improving homeostatic function41.
While our study presents valuable insights, it is essential to acknowledge certain intrinsic limitations, first the use of only one session of taVNS in a healthy population, challenges in capturing the long-term effects of the intervention, or the investigation of dose-dependent effects. The absence of multiple EEG follow-up sessions restricts our ability to observe sustained changes or fluctuations in the observed alterations in brain oscillations. Second, the homogeneity of our sample limits the generalizability of our findings to more diverse populations. Third, these findings should be viewed as hypothesis-generating, particularly for the observed right-lateralized delta modulation, rather than as definitive evidence. Despite these limitations, our study successfully demonstrated detectable changes in brain oscillations after a single taVNS session.
Future research should aim to incorporate more diverse participant groups and implement a longitudinal study design to provide a more comprehensive understanding of the intervention’s impact over time, should whether delta oscillations change should be considered a marker of taVNS. In summary, we suggest that active taVNS induces selective changes in the frontal areas by acutely increasing delta oscillatory activity and that this effect is asymmetrical between brain hemispheres.
Methods
Study design
In this clinical trial, we recruited 44 healthy participants for this randomized, double-blind, sham-controlled trial, divided into two groups (active taVNS group or sham taVNS group) at a 1:1 allocation ratio at Spaulding Rehabilitation Hospital, Cambridge, MA, USA (06/04/2023, NCT05801809).
Participants
Healthy participants over the age of 18 who were new to taVNS stimulation were included in this study. Patients with unstable medical conditions, past six months of alcohol or drug abuse, and any contraindication to taVNS, such as metal in the skull or implanted cardiac or cranial devices, were excluded. Additionally, subjects scoring higher than 30 on the Beck Depression Inventory (BDI) were excluded. All participants provided their consent by signing an online informed consent form via the secure REDCap web platform. The study was conducted in compliance with the Declaration of Helsinki.
Interventions
Utilizing a Healaon Transauricular Vagus Nerve Stimulation device (Neurive Inc., Gimhae, South Korea), we applied stimulation bilaterally to the auricular concha of the ears using an ear set with conductive ear tips (see Fig. 1). Specific details about the device are displayed in Supplementary Table S1. A stimulator was used to connect electrodes, and for 60 min, continuous active stimulation was applied to both auricular concha of the ears while the subjects remained sitting at resting, at the following parameters frequency of 30 Hz, 250 us, ~ 1.5 mA, considered safe and effective, with no risk on cardiac rhythm, as showed in previous studies42. Likewise, the sham and active devices were visually identical in every aspect, such as device model and electrode type, but the only difference between them was that the sham device was programmed to deliver no electrical current to the participant. Blinding was achieved by having a research staff member not involved in data collection or analysis handle the devices for the experimenter after the participants were randomized. To ensure the blinding, we explained to the participants that as the stimulation intensity from the device is low, the stimulation could be indistinguishable by the patients, which maintained uncertainty expectations about their allocation. At the end of the stimulation, adverse events were assessed using a 4-point scale questionnaire (none, mild, moderate, and severe), addressing the most commonly reported side effects in the literature42such as ear pain, headache, or tingling, as well as any other adverse event not listed.
Electroencephalography (EEG) assessment
EEG data were recorded using a high-density 64-channel EGI system (EGI, Eugene, United States of America), with Cz as the reference. Electrode impedances were kept below 50 kΩ throughout the recording session. During acquisition, a hardware high-pass filter at 0.3 Hz, a low-pass filter at 200 Hz, and a notch filter at 60 Hz were applied, using the NetStation software, as previously described in our studies43. We recorded the resting-state EEG with eyes closed for five minutes before and after the intervention. The EEG was recorded without any cognitive or motor tasks to better understand the role of brain oscillations during the resting state.
EEG preprocessing
Using EEGLab45 in MATLAB (MATLAB R2014b, The MathWorks Inc. Natick, MA, 2000), the original data were preprocessed to correct any biological or nonbiological artifact that compromised the analyses. More details about the methodology can be found in our MATLAB Pipeline for EEG preprocessing manuscript46. This method was also applied in our previous studies47,48. We performed the EEG signal processing following the steps described below: i) filtering; (ii) downsampling; (iii) artifact correction; (iv) Independent Component Analysis (ICA); (v) re-referencing, and (vi) frequency band calculation. The details of each step are described below. We followed Makoto’s pipeline49 using the Darbeliai EEGLAB plugin: (i) Band Pass filter of 1 Hz (High Pass) and 50 Hz (Low Pass); (ii) down sampling from 1000 Hz to 250 Hz; (iii) channels were re-referenced by the average of the electrodes; (iv) 60 Hz powerline noise correction (frequency in the USA). We then eliminated the channels that (i) were flat for longer than three seconds, (ii) showed high-frequency noise more significant than two standard deviations, and (iii) showed correlation with neighboring channels less than 0.8 using the Clean_rawdata EEGLAB plugin (v2.2). A visual inspection and rejection of periods containing artifacts was carried out prior to performing the ICA and re-referencing. The remaining channels were once more fed into the Infomax ICA calculation using the Darbeliai plugin. This analysis demonstrates higher efficiency in identifying components and it successfully identifies artifacts50,51. Using the ICLabel toolbox52components associated with heart rate, blinking, muscle noise, and eye movement were eliminated. The EEG preprocessing and analysis were conducted by a blinded assessor.
Resting-state EEG analysis
After completing the preprocessing steps previously outlined, the pop_spectopo EEGLab function was used to process the artifact-free data, applying a Fast Fourier Transformation with two-second windows, 50% overlap, Hamming Window, and a frequency resolution of 0.5 Hz. We included the following oscillations: Delta (1–3.9 Hz), Theta (4–7.9 Hz), Alpha (8–12.9 Hz), and Beta (13–29.9 Hz), as well as the sub-oscillations Low Alpha (8–9.9 Hz), High Alpha (10–12.9 Hz), Low Beta (13–19.9 Hz), and High Beta (20–29.9 Hz), and determined the relative power (power in a specific frequency range/total power from 1 to 29.9 Hz) for all the bands. We calculated the average of the channels selected from the regions as demonstrated in our protocol53.
To determine the frontal asymmetry, we first calculated the relative power of the frontal right hemisphere minus the left hemisphere for pre- and post-intervention. First, the delta, theta, and alpha relative powers of the frontal left, and right hemisphere electrodes were natural log-transformed, and we estimated the asymmetry score by subtracting the value of the left from the right hemisphere (for instance, natural log-transformed spectral power of frontal alpha right - natural log-transformed spectral power of frontal alpha left) for pre and post-intervention.
Sample size
Considering the primary outcome domains in EEG that we hope to test in our study and some of the calculated smallest effect sizes, we opted for a more conservative approach. We made the following assumptions: the power of 80%, type I error of 5% (alpha), type II error of 20% (beta). Considering this scenario, we therefore estimated a sample size of 36 participants. To account for a conservative attrition rate and boost power for secondary outcome analysis, we increased the sample size by 20%. Therefore, we included 44 subjects in each group, resulting in 22 subjects.
Randomization and blinding
We generated a randomization list with a 1:1 allocation ratio using the online tool http://randomization.com and stored it in sealed envelopes. Randomization was then conducted by a research team member who was not involved in delivering the intervention, conducting assessments, or involved in the data process. This staff member opened the sealed randomization envelope and handed the corresponding device (active or sham taVNS device) to the blinded experimenter. The experimenter applied the device without knowing the allocation. The sham and active setups were identical in appearance, duration, and electrode placement, with the sole difference being that in the sham condition, the device delivered no electrical current. This process ensured blinding of both participants and all investigators involved in assessments.
Statistical analysis
Given the exploratory nature of this study and a priori hypotheses about low-frequency bands modulation by taVNS, we prioritized the analysis in delta and theta oscillations in the frontal region (primary outcomes) based on previous findings in the literature13. Outcomes are reported as hypothesis-generating. Secondary analyses examined relative power across the predefined three regions of interest (frontal, central, parietal) and four bands (delta, theta, alpha, beta) and frontal asymmetry.
After performing a detailed descriptive statistical analysis, we reported means (or percentages) and standard deviations for continuous variables (like age) and frequencies for categorical variables (like gender and ethnicity) related to participant characteristics. We used STATA® 17.0 for all statistical analyses. To ensure that randomization was adequate, we also looked at baseline differences between the taVNS and sham groups. We performed a t-test to identify significant differences in EEG power band baselines between the two groups. We also calculated Cohen’s d as a standardized mean difference for the change scores (post – pre) between active and sham groups for the frontal delta outcomes (overall, left hemisphere, and right hemisphere), with positive values indicating greater increases in the active group relative to sham, and 95% CI were reported.
We used a generalized linear model in regression analysis to assess the effects between taVNS and sham groups. The dependent variables were the changes in relative power (delta) of the three predefined regions (frontal, central, and parietal) and each frequency band. We used linear regression models since we treated the EEG power as a continuous variable, including the regression coefficients with the accompanying 95% confidence intervals, as well as the p-values. The primary independent variable was the intervention group (taVNS vs. sham). We predefined the variables approach (age, biological sex, fatigue levels at baseline), and we created the models for the linear multivariate analyses by combining theoretical relevance. A few participants were excluded from some analyses due to missing data in some specific channels or locations (see Tables 6, 7 and 5). Diagnostic plots, residual analysis, and statistical tests were used to evaluate the model assumptions.
In addition to standard regression, we used linear mixed-effects models (LMMs) specifically for the delta band relative power to account for repeated measures. These models included fixed effects for group (active vs. sham), time (post vs. pre), and the group × time interaction, as well as age and gender. A random intercept for subject was included to account for within-subject correlation. Model fit was evaluated using likelihood ratio (LR) tests comparing each mixed-effects model to its corresponding linear model. Statistical significance was defined as p < 0.05.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Ben-Menachem, E., Revesz, D., Simon, B. J. & Silberstein, S. Surgically implanted and non-invasive vagus nerve stimulation: a review of efficacy, safety and tolerability. Eur. J. Neurol. 22, 1260–1268. https://doi.org/10.1111/ene.12629 (2015).
Mandalaneni, K. & Rayi, A. in StatPearls (2024).
Johnson, R. L. & Wilson, C. G. A review of vagus nerve stimulation as a therapeutic intervention. J. Inflamm. Res. 11, 203–213. https://doi.org/10.2147/jir.S163248 (2018).
Yoshida, Y. et al. Effects of transcutaneous auricular vagus nerve stimulation on hemodynamics and autonomic function during exercise stress tests in healthy volunteers. Circ. Rep. 7, 315–322. https://doi.org/10.1253/circrep.CR-24-0136 (2025).
de Oliveira, H. M. et al. Transcutaneous auricular vagus nerve stimulation in insomnia: A systematic review and Meta-Analysis. Neuromodulation https://doi.org/10.1016/j.neurom.2025.04.001 (2025).
An, S., Oh, S. J., Noh, S., Jun, S. B. & Sung, J. E. Enhancing cognitive abilities through transcutaneous auricular vagus nerve stimulation: findings from prefrontal functional connectivity analysis and virtual brain simulation. Neuroimage 311, 121179. https://doi.org/10.1016/j.neuroimage.2025.121179 (2025).
Jelinčić, V. et al. Continuous transcutaneous auricular vagus nerve stimulation increases Long-Latency neural processing in multiple sensory modalities. Psychophysiology 62, e70048. https://doi.org/10.1111/psyp.70048 (2025).
Smith, E. E. et al. Frontal theta and posterior alpha in resting EEG: A critical examination of convergent and discriminant validity. Psychophysiology 57, e13483. https://doi.org/10.1111/psyp.13483 (2020).
Lanzone, J. et al. Vagal nerve stimulation cycles alter EEG connectivity in drug-resistant epileptic patients: A study with graph theory metrics. Clin. Neurophysiol. 142, 59–67. https://doi.org/10.1016/j.clinph.2022.07.503 (2022).
Germany Morrison, E. et al. Characterization of vagus nerve stimulation (VNS) dose-dependent effects on EEG power spectrum and synchronization. Biomedicines 12, (2024). https://doi.org/10.3390/biomedicines12030557
Ricci, L. et al. Transcutaneous vagus nerve stimulation modulates EEG microstates and delta activity in healthy subjects. Brain Sci. 10 https://doi.org/10.3390/brainsci10100668 (2020).
Sharon, O., Fahoum, F. & Nir, Y. Transcutaneous vagus nerve stimulation in humans induces pupil dilation and attenuates alpha oscillations. J. Neurosci. 41, 320–330. https://doi.org/10.1523/jneurosci.1361-20.2020 (2021).
Gianlorenco, A. C. L. et al. Electroencephalographic patterns in taVNS: A systematic review. Biomedicines 10, (2022). https://doi.org/10.3390/biomedicines10092208
Metzen, D. et al. Frontal and parietal EEG alpha asymmetry: a large-scale investigation of short-term reliability on distinct EEG systems. Brain Struct. Funct. 227, 725–740. https://doi.org/10.1007/s00429-021-02399-1 (2022).
Adair, D. et al. Electrical stimulation of cranial nerves in cognition and disease. Brain Stimul. 13, 717–750. https://doi.org/10.1016/j.brs.2020.02.019 (2020).
Fidalgo, T. M. et al. Biological markers in noninvasive brain stimulation trials in major depressive disorder: a systematic review. J. Ect. 30, 47–61. https://doi.org/10.1097/YCT.0b013e31828b34d8 (2014).
Biomarkers and surrogate. Endpoints: preferred definitions and conceptual framework. Clin. Pharmacol. Ther. 69, 89–95. https://doi.org/10.1067/mcp.2001.113989 (2001).
Chen, Y., Yang, H., Wang, F., Lu, X. & Hu, L. Modulatory effects of transcutaneous auricular vagus nerve stimulation (taVNS) on attentional processes. Gen. Psychiatr. 36, e101176. https://doi.org/10.1136/gpsych-2023-101176 (2023).
Knyazev, G. G. EEG delta oscillations as a correlate of basic homeostatic and motivational processes. Neurosci. Biobehav Rev. 36, 677–695. https://doi.org/10.1016/j.neubiorev.2011.10.002 (2012).
Yordanova, J. et al. Common and distinct lateralised patterns of neural coupling during focused attention, open monitoring and loving kindness meditation. Sci. Rep. 10, 7430. https://doi.org/10.1038/s41598-020-64324-6 (2020).
in Psychology of Meditation. Psychology of Emotions, Motivations and Actions. 147–166 (Nova Science, Hauppauge, NY, US, (2014).
Tononi, G. & Edelman, G. M. Consciousness and complexity. Science 282, 1846–1851. https://doi.org/10.1126/science.282.5395.1846 (1998).
Varela, F., Lachaux, J. P., Rodriguez, E. & Martinerie, J. The brainweb: phase synchronization and large-scale integration. Nat. Rev. Neurosci. 2, 229–239. https://doi.org/10.1038/35067550 (2001).
Hartikainen, K. M. Emotion-Attention interaction in the right hemisphere. Brain Sci. 11, 1006 (2021).
Gatzke-Kopp, L. M., Jetha, M. K. & Segalowitz, S. J. 56 73–85 (Wiley, US, (2014).
Papousek, I., Reiser, E. M., Weber, B., Freudenthaler, H. H. & Schulter, G. Frontal brain asymmetry and affective flexibility in an emotional contagion paradigm. Psychophysiology 49, 489–498. https://doi.org/10.1111/j.1469-8986.2011.01324.x (2012).
Smith, E. E., Reznik, S. J., Stewart, J. L. & Allen, J. J. Assessing and conceptualizing frontal EEG asymmetry: an updated primer on recording, processing, analyzing, and interpreting frontal alpha asymmetry. Int. J. Psychophysiol. 111, 98–114. https://doi.org/10.1016/j.ijpsycho.2016.11.005 (2017).
Quercia, A., Zappasodi, F., Committeri, G. & Ferrara, M. Local Use-Dependent sleep in wakefulness links performance errors to learning. Front. Hum. Neurosci. 12, 122. https://doi.org/10.3389/fnhum.2018.00122 (2018).
Capone, F. et al. Transcutaneous vagus nerve stimulation combined with robotic rehabilitation improves upper limb function after stroke. Neural Plast. 2017 (7876507). https://doi.org/10.1155/2017/7876507 (2017).
Coutin-Churchman, P. et al. Quantitative spectral analysis of EEG in psychiatry revisited: drawing signs out of numbers in a clinical setting. Clin. Neurophysiol. 114, 2294–2306. https://doi.org/10.1016/s1388-2457(03)00228-1 (2003).
Bates, A. T., Kiehl, K. A., Laurens, K. R. & Liddle, P. F. Low-frequency EEG oscillations associated with information processing in schizophrenia. Schizophr Res. 115, 222–230. https://doi.org/10.1016/j.schres.2009.09.036 (2009).
Nariai, H. et al. Ictal high-frequency oscillations at 80–200 hz coupled with delta phase in epileptic spasms. Epilepsia 52, e130–134. https://doi.org/10.1111/j.1528-1167.2011.03263.x (2011).
Chen, Y., Lu, X. & Hu, L. Transcutaneous auricular vagus nerve stimulation facilitates cortical arousal and alertness. Int. J. Environ. Res. Public. Health. 20 https://doi.org/10.3390/ijerph20021402 (2023).
Grimshaw, G. M. & Carmel, D. An asymmetric Inhibition model of hemispheric differences in emotional processing. Front. Psychol. 5, 489. https://doi.org/10.3389/fpsyg.2014.00489 (2014).
Adolph, D., von Glischinski, M., Wannemüller, A. & Margraf, J. The influence of frontal alpha-asymmetry on the processing of approach- and withdrawal-related stimuli-A multichannel psychophysiology study. Psychophysiology 54, 1295–1310. https://doi.org/10.1111/psyp.12878 (2017).
Razumnikova, O. & Khoroshavtseva, E. Imbalance between emotionally negative and positive life events retrieval and the associated asymmetry of brain activity. Behav. Sci. (Basel). 10 https://doi.org/10.3390/bs10010018 (2019).
Lubben, N., Ensink, E., Coetzee, G. A. & Labrie, V. The enigma and implications of brain hemispheric asymmetry in neurodegenerative diseases. Brain Commun. 3, fcab211. https://doi.org/10.1093/braincomms/fcab211 (2021).
Parente, J. et al. Anti-inflammatory, and clinical effects of transauricular vagus nerve stimulation in major depressive disorder: A systematic review. Int. J. Neuropsychopharmacol. https://doi.org/10.1093/ijnp/pyad058 (2023). Neural.
Tarn, J., Legg, S., Mitchell, S., Simon, B. & Ng, W. F. The effects of noninvasive vagus nerve stimulation on fatigue and immune responses in patients with primary sjögren’s syndrome. Neuromodulation 22, 580–585. https://doi.org/10.1111/ner.12879 (2019).
Chakravarthy, K., Chaudhry, H., Williams, K. & Christo, P. J. Review of the uses of vagal nerve stimulation in chronic pain management. Curr. Pain Headache Rep. 19, 54. https://doi.org/10.1007/s11916-015-0528-6 (2015).
Costa, V. et al. Transcutaneous vagus nerve stimulation effects on chronic pain: systematic review and meta-analysis. Pain Rep. 9, e1171. https://doi.org/10.1097/pr9.0000000000001171 (2024).
Kim, A. Y. et al. Safety of transcutaneous auricular vagus nerve stimulation (taVNS): a systematic review and meta-analysis. Sci. Rep. 12, 22055. https://doi.org/10.1038/s41598-022-25864-1 (2022).
Marques, L. M. et al. Motor event-related synchronization as an inhibitory biomarker of pain severity, sensitivity, and chronicity in patients with knee osteoarthritis. Neurophysiol. Clin. 52, 413–426. https://doi.org/10.1016/j.neucli.2022.09.006 (2022).
Farmer, A. D. et al. International consensus based review and recommendations for minimum reporting standards in research on transcutaneous vagus nerve stimulation (Version 2020). Front. Hum. Neurosci. 14 https://doi.org/10.3389/fnhum.2020.568051 (2021).
Delorme, A. & Makeig, S. EEGLAB: an open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J. Neurosci. Methods. 134, 9–21. https://doi.org/10.1016/j.jneumeth.2003.10.009 (2004).
Murrins Marques, L. et al. PIPEMAT-RS: development and validation of a standardized MATLAB pipeline for Resting-State EEG preprocessing. J. Vis. Exp. 220 https://doi.org/10.3791/68350 (2025).
Lacerda, G. J. M. et al. EEG oscillations as neuroplastic markers of neural compensation in spinal cord injury rehabilitation: the role of Slow-Frequency bands. Brain Sci. 14, 1229 (2024).
Camargo, L., Pacheco-Barrios, K., Marques, L. M., Caumo, W. & Fregni, F. Adaptive and compensatory neural signatures in fibromyalgia: an analysis of resting-state and simulus-evoked EEG oscillations. Biomedicines 12, 1428 (2024).
Miyakoshi, M. Makoto’s preprocessing pipeline, < (2020). https://sccn.ucsd.edu/wiki/Makoto’s_preprocessing_pipeline
Delorme, A., Sejnowski, T. & Makeig, S. Enhanced detection of artifacts in EEG data using higher-order statistics and independent component analysis. Neuroimage 34, 1443–1449. https://doi.org/10.1016/j.neuroimage.2006.11.004 (2007).
Onton, J. & Makeig, S. Information-based modeling of event-related brain dynamics. Prog Brain Res. 159, 99–120. https://doi.org/10.1016/s0079-6123(06)59007-7 (2006).
Pion-Tonachini, L., Kreutz-Delgado, K., Makeig, S. & ICLabel An automated electroencephalographic independent component classifier, dataset, and website. Neuroimage 198, 181–197. https://doi.org/10.1016/j.neuroimage.2019.05.026 (2019).
Gianlorenco, A. C. et al. Understanding the effects of non-Invasive transauricular vagus nerve stimulation on EEG and HRV. J. Vis. Exp. 203 https://doi.org/10.3791/66309 (2024).
Acknowledgements
VC is a fellow of the Institutional Internationalization Program (CAPES/PrInt/UFScar) funded by the Brazilian Federal Agency for Support and Evaluation of Graduate Education (CAPES)/Ministry of Education of Brazil.
Author information
Authors and Affiliations
Contributions
FF, HC, and JS conceived and planned the experiments. LC, AG, and KP conducted the study and conducted subject recruitment, data collection, and data analysis. EP conducted the study and subject recruitment. VC analyzed data. All the authors contributed to the writing. FF supervised all the steps of the study and critically revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
HC and JS are affiliated with neuromodulation company Neurive Co. This company develops neuromodulation technology (e.g., taVNS) to treat common brain disorders. FF is funded by a research grant from Neurive to Spaulding Rehabilitation Hospital. The other authors declare no conflict of interest.
Ethics declaration
This trial (Protocol number: 2022P003200) was approved by the Mass General Brigham Human Research Committee. The clinical trial was first posted on 06/04/2023 (NCT05801809), and before the study began, all participants provided their consent by signing an online informed consent form via the secure REDCap web platform. The study was conducted in compliance with the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Camargo, L., Gianlorenço, A.C., Pacheco-Barrios, K. et al. The effects of non-invasive transcutaneous auricular vagus nerve stimulation on resting-state delta oscillation: a randomized, double-blinded, sham-control trial. Sci Rep 15, 34531 (2025). https://doi.org/10.1038/s41598-025-17821-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-17821-5