Abstract
In this paper, the problem of a magnetically actuated robotic catheter landing on a beating heart surface for the robotic catheter ablation procedure is addressed. A landing control strategy that optimizes the catheter tip trajectories, leading to a stable tip-tissue contact and a safe ablation force level for a successful catheter ablation procedure is proposed. Specifically, an ablation phase analysis is presented that investigates the optimal catheter tip configuration and the timing of the landing, preparing for a stable and safe ablation force throughout the ablation phase. A reference trajectory generation algorithm and a decoupled landing control optimization are then proposed for respectively generating a series of desired tip trajectories and achieving the optimal tip configurations in a desired landing period. The simulation results using in vivo heart motion data are presented to demonstrate the feasibility and effectiveness of the proposed methods.
Similar content being viewed by others
Introduction
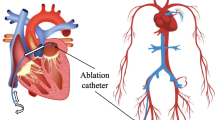
Catheter ablation has become one of the most common and effective procedures for treating cardiac arrhythmia, such as atrial fibrillation (AF)1,2. During the catheter ablation, the catheter is inserted into the femoral vein and guided through the right atrium. A transseptal puncture is created on the atrial septum and the catheter is guided into the left atrium until the tip of the catheter reaches the desired area, such as the ostia of the left pulmonary veins. The catheter tip then applies radio frequency energy to the tissue and creates lesions to achieve isolation of the pulmonary veins and restore sinus rhythm1 of the heart. The accuracy of catheter tip position and the catheter tip-tissue contact force quality have become the most critical factors in creating a gap-free transmural lesions for an effective lesion formation and a successful ablation outcome.
In the paradigm proposed in this paper, a novel magnetic resonance imaging (MRI)-actuated robotic intravascular catheter3,4 is used to perform the catheter ablation procedure. The MRI-actuated robotic catheter is operated inside the bore of an MRI scanner and is actuated by multiple sets of electromagnetic micro-coils that deflect the catheter using the Lorentz force under the static magnetic field of the MRI scanner. This actuation method enhances the catheter’s flexibility and maneuverability when targeting ablation sites. Compared to existing robotic catheter systems, which uses the X-ray fluoroscopy for imaging, our system does not expose patient and medical staff to radiation. In addition, MRI provides superior soft-tissue visualization which could significantly improve the ablation outcome and efficiency in ventricular arrhythmia scenarios. This paper addresses the problem of the MRI-actuated robotic catheter landing on a beating heart surface for robotic catheter ablation. The goal of the catheter tip landing is to establish an accurate, smooth, and stable tip-tissue contact, ensuring a safe ablation force and a successful lesion formation. Specifically, two phases of the robotic catheter ablation process are discussed, i.e., a free landing phase and an ablation phase. During the free landing phase, the catheter tip approaches the beating heart surface towards the desired ablation position. During the ablation phase, the catheter tip first makes contact with the tissue surface and the tip-tissue contact force reaches the desired force levels for the lesion creation and retains safe and stable contact with the tissue until the lesion is formed.
Force sensing-based feedback control strategies5,6,7 have been proposed for robotic catheter ablation. However, MRI-compatible force sensors are usually difficult and costly to manufacture. In this paper, a feed-forward landing control method for landing the MRI-actuated robotic catheter on the beating heart surface is proposed. In the proposed method, first, an ablation phase analysis is performed to determine the optimal timing of the landing during the heart cycle and the optimal tip configuration at the target landing point for achieving a safe normal force level within the desired force range and a stable tip-tissue contact without slippage during the ablation phase. This is followed by the free landing phase, where a tip reference trajectory generation algorithm is proposed to generate the desired tip trajectory that achieves the optimal landing timing and tip configuration. A decoupled landing control optimization is then performed, optimizing the control inputs that track the tip reference trajectories. Finally, a robotic catheter ablation planner employing the proposed landing control strategy is presented. The effectiveness of the proposed methods is evaluated in four case studies using the prerecorded in vivo heart motion data under regular heartbeat motions, varying heartbeat motions, and arrhythmia motions in the simulation environment.
Related studies
Robotic catheter ablation technologies8,9,10,11 have shown to improve the efficacy and safety of the ablation procedure due to the precise positioning and dexterous manipulation of the catheter tip. Several motion planning and control methods5,6,7,12,13,14,15,16 have been proposed for robotic catheter manipulations and catheter-tissue interaction under heart motion disturbances. There have been studies on robotic catheter ablation and force control using feedback-based control schemes5,6,7,16. However, few studies have focused on ensuring safe and stable catheter-tissue contact during ablation procedures, particularly in scenarios where real-time sensing feedback (e.g., force sensing under MR-imaging) is difficult to obtain. To the best of the authors’ knowledge, this is the first study to investigate a feedforward-based control strategy for robotic catheter to make contact with beating heart surface that optimizes catheter-tissue contact stability and safety.
Zhang et al.6 propose a decoupled feedback controller for a tendon-driven robotic catheter where the catheter insertion and bending inputs are controlled independently. The controller solves the control inputs as well as the contact force as a quadratic programming (QP) problem where the catheter is modeled using the finite element method. Greigarn et al.12 propose a task space motion planner for a MRI-actuated robotic catheter modeled by the pseudo-rigid body model. The catheter shape and contact force are estimated by minimizing the potential energy of the robotic catheter. Bajo and Simaan13 propose a hybrid position/force controller of a multi-backbone tendon-driven continuum robot. The controller calculates the joint-space control inputs using a model-based actuation compensation method. Yip and Camarillo14 propose a model-less hybrid position/force controller for tendon-driven continuum robots through Jacobian estimation. Jayender et al.15 propose an augmented hybrid impedance controller for catheter insertion. This controller uses an outer loop that generates desired position and force profiles and an inner loop that computes the joint space control inputs.
Yuen et al.5 developed a motion compensation system with feed-forward normal directional contact force control under the beating heart motions. This system utilizes a miniature uni-axial force sensor for contact force sensing inside the heart. The positional heart motion trajectory used for the feed-forward motion compensation is estimated using the extended Kalman filter based on the sensing information obtained from the 3D ultrasound. Kesner et al.7 propose a 3D ultrasound image-guided robotic catheter system with a force-sensing end-effector. Friction compensation is included in the feed-forward force controller. This system can maintain a 1 N force on a moving motion target. Yip et al.16 develop a model-less approach for generating contiguous lesions on the beating heart tissue. An adaptive Jacobian estimation is proposed for the force and position control of a tendon-driven catheter under heart motion disturbances, where a force sensor is employed to regulate the contact force.
This paper focuses on how the catheter tip should establish the tip-tissue contact to guarantee a stable contact and a safe ablation force for an effective ablation procedure. The main contribution of this paper is twofold: (1) A reference trajectory generation strategy that achieves the optimal landing timing and landing tip configuration for establishing an effective and safe catheter-tissue contact. (2) The robotic catheter is kinematically redundant, i.e., one tip configuration can be achieved through multiple actuation inputs. To reduce the redundancy of the trajectory planning and guarantee a smooth insertion trajectory by avoiding frequent overshoot and retraction of the catheter insertion inputs, a decoupled feed-forward control optimization method is proposed to track the reference landing trajectory, which optimizes the catheter insertion inputs and catheter deflection inputs independently.
Problem formulation
In this paper, two phases of the robotic catheter ablation process, i.e. a free landing phase and an ablation phase, are studied. As presented in Fig. 1, during the free landing phase, the robotic catheter is actuated towards the target ablation point before the tip of the robotic catheter makes a “touchdown” against the tissue surface. A touchdown is defined as the instantaneous moment where the tip of the robotic catheter makes initial contact with the tissue surface with a zero contact force. After the touchdown at a desired ablation point, the robotic catheter tip then applies a desired ablation force against the tissue surface during the ablation phase. This paper investigates two sub-problems: 1) how the catheter should approach the tissue surface for a safe and stable landing during the free landing phase, and 2) how to control the catheter-tissue contact force for an effective ablation during the ablation phase.
The two phases of the catheter ablation problem for the robotic catheter ablation procedure: a free landing phase and an ablation phase. S denotes the spatial frame of the robotic catheter. \(P_i\) denotes the instantaneous contact point established between the catheter tip and the tissue surface at time \(t_i\), where \(P_1\) denotes the “touchdown” motion point.
Modeling of the MRI-actuated robotic catheter
The MRI-actuated robotic intravascular catheter3,4 is magnetically actuated by the magnetic torques generated by the electromagnetic micro-coils embedded on the catheter tubing placed under the static magnetic field of the MRI scanner. Each set of micro-coils (or actuators) contains one axial coil, and two orthogonal side coils4, as shown in Fig. 2. The deflection of the catheter is controlled by the currents passing through the coils. The insertion of the catheter is controlled using a friction-based drive mechanism. Specifically, let \(z = [\zeta ^T, l]^T \in \mathbb {R}^{N_z \times 1}\) denote the control inputs of the robotic catheter, where \(\zeta \in \mathbb {R}^{N_c} \times 1\) is the vector of actuation currents and \(N_c\) denotes the number of the actuation coils and \(l \in \mathbb {R}\) is the inserted length of the catheter. Let \(\zeta _i \in \mathbb {R}^3\) denote the actuation currents of the i-th actuation coil, the magnetic moment \(\mu _i\) generated by the i-th actuator is then given as
where the \(^\wedge\) operator maps a vector in \(\mathbb {R}^3\) to so(3). \(N_i\) and \(A_i\) are 3 by 3 diagonal matrices whose diagonal elements are the number of winding turns and the cross-sectional area of the i-th actuator, respectively. The static magnetic field \(B_s\) of the MRI scanner expressed in the body frame of the i-th actuator is given as \(B_i = R_{i}^T B_s\), where \(R_{i}\) denotes the rotation matrix of the frame attached to the i-th actuator relative to the spatial frame.
In this paper, two types of catheter models, a tip position constraint quasi-static Cosserat-Rod model (CRM), and a time-discretized dynamic Cosserat-Rod model are employed for modeling the robotic catheter at the ablation phase and the free landing phase, respectively. In the dynamic model, the robotic catheter is modeled as a series of flexible and rigid segments (actuation coils). Let \(N_r\) denote the number of actuation coils, the state variables of the actuation coils are given as:
where \(v_i\), \(w_i\), \(p_i\) and \(R_i\) denote the linear velocity, angular velocity, position and rotation matrix of the i-th actuation coil, respectively. The state variables of the catheter tip are given as:
where \(p_{c}\), \(R_{c}\), and \(u_{c}\) are respectively the position, rotation matrix, and curvature at the catheter tip. The time-discretized dynamic model of the MRI-actuated robotic catheter is denoted as
where z(t) is the control inputs and \(\Delta t\) is the step size of the time discretization. The readers are referred to17 for a complete discussion of the dynamic models for the MRI-actuated robotic catheter.
Let \(p_d\) denote the contact point on the given surface and \(p_{c}\) denote the tip position returned from the free tip forward kinematics modelFootnote 1 under the actuation inputs z and the tip contact force \(f_{c}\), the catheter tip position under non-sliding contact is constrained as
The tip contact position-constrained model solves the catheter configuration under the tip position constraint by solving the following optimization problem
The readers are referred to18 for a complete discussion of the tip contact position-constrained CRM model. The tip contact position-constrained CRM model is denoted as
in the rest of this paper, where \(X_0 = [p_0, R_0]\) denote the entry point state variable, where \(p_0\) and \(R_0\) respectively denote the initial position and rotation matrix.
Landing on a beating heart surface
In this section, we investigate the optimal landing strategy to establish a stable tip-tissue contact with appropriate ablation force for the MRI-actuated robotic catheter ablation. The ablation phase analysis is first presented, where the timing of the touchdown, and the optimal catheter tip configuration at the touchdown position for achieving a stable tip-tissue contact with the desired ablation force range, are discussed. A landing control approach, including a reference trajectory generation method and a receding horizon landing control optimization, is then proposed, ensuring a smooth landing process within a desired time period.
Ablation phase analysis
In the ablation phase analysis, we investigate the optimal tip configuration at the touchdown point and touchdown timing that establishes a safe and stable initial contact between the catheter tip and the tissue surface, ensuring an effective and safe ablation process. We define a touchdown angle \(\alpha _{d}\) as the relative angle between the catheter tip normal \(n_c\) and the heart surface normal \(-n_s\) at the touchdown point, as shown in Fig. 3. In the ablation phase analysis, the optimal timing \(t_d\) of the touchdown and the optimal touchdown angle \(\alpha _{d}\) for a safe and effective catheter tip landing are investigated.
The touchdown angle \(\alpha _d\) is defined as the angle between the catheter tip normal \(n_c\) and the surface normal \(-n_s\) for a given surface configuration. \(\Psi\) denotes the instantaneous heart surface frame. \(\beta _d\) is the rotation angle with respect to the z axis of the surface frame. 90 sampled catheter configurations are used for touchdown motion analysis with touchdown angles \(\alpha _d\) from \(0^ \circ \sim 30 ^\circ\) and tangential angles \(\beta _d\) from \(0^ \circ \sim 360 ^\circ .\).
In this analysis, the in vivo heartbeat motion data of two points-of-interest (POIs), namely, the target ablation points, on the left ventricle (LV)19 are employed for the ablation phase analysis, as shown in Fig. 4. The two-coil catheter prototype presented in20 is used in this analysis. The contact force model defined in21 is employed for modeling catheter tip-tissue contact. Specifically, suppose the contact between the catheter and the surface is non-conforming, the origin of the contact frame is located at the contact point with the z-axis of the contact frame pointing in the outward surface normal direction. The friction cone FC for the catheter tip-tissue contact is defined as:
where \(\sigma _s\) is the static friction coefficient between the catheter tip and the tissue surface. \(\lambda _c\), \(\lambda _{f_x}\) and \(\lambda _{f_y}\) respectively denote the normal and the two tangential components of the contact force \(f_c = [\lambda _{f_x}, \lambda _{f_y}, \lambda _c]\).
Let \(\sigma \in \mathbb {R}\) denote the contact ratio between frictional force and normal force, and
where \(\lambda _{f} = [{\lambda _{f}}_x, {\lambda _{f}}_y]\). The catheter tip-tissue contact is considered stable (i.e., no slippage between the tip and target ablation point on the surface) if the contact force is inside the friction cone FC, or equivalently, \(0 \le \sigma \le \sigma _s\). The internal wall of the heart is relatively smooth and well-lubricated due to the presence of blood22. In23, the static friction coefficient of a silicone catheter against porcine aorta is reported as 0.1, where distilled water is used as lubricant. In24, the static friction coefficients of a silicone catheter against aorta and superior vena cava are reported as 0.67 and 0.56, respectively, where blood is used as lubricant for both cases. For ablation under blood, a static friction coefficient under the reported values of 0.56 suffices for this analysis. In this paper, a relatively conservative value of \(\sigma _s = 0.2\) as the static friction coefficient between the robotic catheter and the heart surface, is used, as reported in our previous studies in20,21.
For the safety of the ablation procedure, the normal contact force between the catheter tip and heart tissue should be limited within a desired force range \(\lambda _c \in [\lambda _{min}, \lambda _{max}]\). Several studies25,26,27 suggest that for an effective and safe tip-tissue contact, the desired normal contact force should be limited within the range from 10 g to 25 g (0.1 N\(\sim\)0.25 N).
(a) The distance between the POI and origin of the spatial frame, i.e., the entry point of the catheter using the first POI heart motion data. The optimal touchdown period is marked in red lines. (b) Percentage of the number of the contact force samples that violate the desired normal force range \([\lambda _\textrm{min}, \ \lambda _\textrm{max}]\), averaged over the tangential rotation angles \(\beta _d\), for the first cycle of the first POI heart motion data. (c) Percentage of the number of contact force samples that violate the friction cone FC, averaged over the tangential rotation angles \(\beta _d\), for the first cycle of the second POI heart motion data. (d) The distance between the POI and the origin of the spatial frame using heart motion data of the second POI. The optimal touchdown periods are marked in red lines. (e) Percentage of the number of the contact force samples that violate the desired normal force range \([\lambda _\textrm{min}, \ \lambda _\textrm{max}]\), averaged over the tangential rotation angles \(\beta _d\), for the first cycle of the second POI heart motion data. (f) Percentage of the number of contact force samples that violate the friction cone FC, averaged over the tangential rotation angles \(\beta _d\), for the first cycle of the second POI heart motion data.
For the analysis of the optimal touchdown angle, a tip orientation control algorithm is proposed, as presented in Algorithm 1. The tip orientation control algorithm iteratively updates the control input until the desired tip normal is reached for a given contact point and surface configuration.
Specifically, the proposed algorithm takes the inputs of an initial control input \(z_0\) and a desired tip normal \(n_d\). In Line 3, the catheter tip normal \(n_j\) is calculated using the free tip quasi-static CRM model. In Line 5, The normal component of the kinematic Jacobian \({J_{n}}_j \in \mathbb {R}^{3xN_z}\) that relates the catheter tip normal to the control inputs is calculated as
where \((R_{c})_3\) denotes the z-directional component of tip rotation matrix \(R_{c}\). The readers are referred to18 for details of the analytical derivation of the kinematic Jacobian. The incremental change of the catheter normal \(dn_j\) is then calculated in Line 6, where \(k_n\) denotes the step size of the update speed. The desired incremental change of the control input \(dz_j\) is calculated in Line 7, where \({J_{n}^{\dag }}_j = ({{J_{n}}_j }^T {J_{n}}_j )^{-1}{{J_{n}}_j }^T\) denotes the pseudo-inverse of the Jacobian \({J_{n}}_j\). The control input \(z_{j+1}\) is then updated in Line 8. The iteration continues until the calculated tip normal error \(|n_d - n_{j}|\) is within the error threshold \(\epsilon\).
In this analysis, the catheter tip-tissue contact is deemed safe if the catheter tip-tissue contact force is within a safe normal force range \([\lambda _{min}, \lambda _{max}]\), and the catheter tip-tissue contact is deemed stable if the catheter tip-tissue contact force is within the friction cone FC. The first cycle of the heart motion data is used to analyze the safety and stability of the catheter tip-tissue contact under different landing timing and landing tip configurations. For determining the optimal touchdown timing \(t_d\), 26 motion points are uniformly sampled as the touchdown point along the first cycle of the heart motions. At each sampled touchdown point, the tip of the catheter is in contact with the target motion point with zero/negligible normal contact force. Additionally, for determining the optimal catheter tip configuration at the touchdown point, let \(\beta _d\) denote the rotation angle about the z-direction of the surface frame in the tangential plane of the tissue surface, as shown in Fig. 3, a tip normal \(n_d\) can be specified by the touchdown angle \(\alpha _d\) and tangential angle \(\beta _d\) in the spatial frame as
where \(R_{s \Psi }\) is the rotation matrix of the surface frame \(\Psi\) relative to the spatial frame. A set of desired tip normals \(\{n_d\}_{1:N_t}\) are sampled such that the touchdown angle varies in \([0^\circ , 30^\circ ]\)Footnote 2 with the tangential rotation angle \(\beta _d\) varies in \([0^\circ , 360^\circ ]\), where \(N_t = 90\) is the number of sampled tip normals. A set of actuation inputs \(\{z\}_{1:N_t}\) are collected using Algorithm 1 to achieve the desired tip normals. The actuation inputs \(\{z\}_{1:N_t}\) are applied to the robotic catheter at a constant level for one cycle of the heart motion. The percentage of contact forces that violate the safe normal force range \([\lambda _{min}, \lambda _{max}]\) and the percentage of contact forces that violate the friction cone, i.e., \(\sigma > \sigma _s\), during one cycle of the two POI data sets are collected, as present in Fig. 5.
The percentage of the violations of the desired force range and friction cone, averaged over the tangential rotation angle \(\beta _d\), for the two POI data sets are presented in Fig. 5a-c and d-f, respectively. Fig. 5a and d show the Euclidean distance between the POIs and the catheter entry point during the first cycle of heart motion data sets. In Fig. 5b, the average number of violations for the normal force samples drop below 40\(\%\) for the touchdown timing \(t_d \in [0.6 s,\ 0.75 s]\) and touchdown angle \(\alpha _{d} \in [0^\circ ,\ 25^\circ ]\). In Fig. 5c, the number of violations for the contact ratio \(\sigma\) samples drop below 30\(\%\) for the touchdown timing \(t_d \in [0.4 s,\ 0.8 s]\) and touchdown angle \(\alpha _{d} < 7^\circ\). In Fig. 5 (e), the numbers of violations for the normal force samples drop below 40\(\%\) for the touchdown timing \(t_d \in [0.65 s,\ 0.75 s] \cup [0.9 s,\ 1 s]\) and touchdown angle \(\alpha _{d} \in [0^\circ ,\ 20^\circ ]\). In Fig. 5f, the number of violations for the contact ratio \(\sigma\) samples drop below 40\(\%\) for the touchdown timing \(t_d \in [0.65 s,\ 1 s]\) and touchdown angle \(\alpha _{d} < 7^\circ\).
Fig. 5 indicates that, along the heart motion cycle, a touchdown point with a large spatial distance to the catheter entry point results in less normal force and contact ratio violations over the heart motion data. Consider the case when the touchdown motion point is furthest from the catheter base, the catheter is first compressed with increasing contact force and then rebounded with contact force reduced back to near zero. On the contrary, when the touchdown motion point is closest to the catheter entry point, the catheter tip tends to lose contact with the tissue surface when the tissue surface first moves away from and then moves down towards the catheter. In the first case, the contact force fluctuates in a certain force range, while in the second case, the lost of contact between the catheter tip and tissue surface causes significant violations of the desired force range. In addition, as shown in Fig. 5 (c) and (f), the contact ratio violation decreases when a touchdown angle is close to \(0^\circ\), indicating that a catheter tip normal that is perpendicular to the heart surface results in a stable catheter tip-tissue contact.
Based on this analysis, the touchdown motion point will be chosen as the furthest motion point during the next cycle of the predicted heart motion and a touchdown tip normal will be chosen perpendicular to the heart surface in the rest of this paper. To further optimize the tip-tissue contact force and reduce the force fluctuation during the ablation phase, the catheter is actuated at a desired sample control rate of 20 Hz to achieve a desired normal force and a stable tip contact with the heart tissue surface using the receding horizon contact force control method with adaptive filter-based prediction as presented in21.
Reference landing trajectory generation
In this section, the proposed reference landing trajectory generation method, generating the desired tip configuration trajectory to land on the target ablation POI location at the desired landing time with the desired tip configuration, is presented. The proposed method generates the reference tip configuration trajectory based on the intrinsic Tau-G guidance strategy28,29 by employing predicted heartbeat motions. In this paper, the generalized adaptive filter-based heart motion prediction proposed in19 is used to provide the predicted POI positions for the reference tip trajectory generation.
Let \({\tilde{p}}\) and \({\tilde{n}}\) denote the predicted POI motion and the tissue surface normal, respectively, we define the closest heart motion point as the point along the POI trajectory that has the smallest Euclidean distance to the entry point of the catheter and the furthest motion point as the point along the POI trajectory that has the largest Euclidean distance to the entry point of the catheter. The heart cycle is then divided into two motion periods, i.e., an approaching period and a departing period. The approaching period is defined as the period where the POI is moving towards the catheter tip from the furthest motion point to the closest motion point. The departing period is then defined as the period where the POI moving from the closest motion point towards the furthest motion point. Given a desired landing period, the reference tip trajectory generation algorithm generates a series of catheter tip trajectories such that the catheter tip approaches the closest heart motion point without collision with the heart surface during the approaching period then chases the POI towards the furthermost motion point during the departing period until a touchdown at the POI is achieved at the furthermost motion point.
In this paper, the intrinsic Tau-G guidance strategy28,29 is employed to generate the tip reference trajectories given the predicted heart motion for a desired landing period. Let \(\chi _x(t) \in \mathbb {R}\) denote the x directional temporal distance gap between the catheter tip and the target POI motion position, Tau \(\tau\) is defined as the time-to-closure of the distance gap and is calculated as28:
The intrinsic Tau-G guidance strategy assumes that the movements to close the distance gap are intrinsically guided by a free fall motion28. Specifically, the intrinsic Tau-G guidance strategy generates temporal reference trajectories that are guided by coupling the distance gap \(\chi _x(t)\) onto an intrinsically generated guiding motion \(G_x(t)\)28,29 and
where \({G_0}_x\) denotes the initial intrinsic motion gap at \(t = 0\), and \({V_G}_x\) denotes the initial velocity of the catheter tip. \(g=9.8 m/s^2\) is the gravitational acceleration. Let T denote the total duration of the landing process, x(T) and \({\dot{x}}(T)\) denote the x-directional target catheter tip position and target velocity at the touchdown point, and let \(x(0) \in \mathbb {R}\) and \({\dot{x}}(0) \in \mathbb {R}\) denote the initial catheter tip position and tip velocity in x-direction. The initial intrinsic motion gap \({G_0}_x\) and initial velocity \({V_G}_x\) can be computed as29
where \({\chi _0}_x = \chi _x(T) - \chi _x(0) - {\dot{\chi }}_x(T) T\). The desired x directional catheter tip motion x(t) can then be computed as
where \(k_x \in [0, 0.5]\) is a constant ratio.
The y and z directional tip position reference trajectories, and the tip normal reference trajectories can then be computed similarly by specifying the y and z directional, and the tip normal initial and target motions in (14) and (15).
Let \(p_r(t)\) denote the temporal reference tip position at time t and \(n_r(t)\) denote the temporal reference tip normal at time t, the approaching period reference trajectories \(\{p_r(t)\}_{t=0:T_a}\) and \(\{n_r(t)\}_{t=0:T_a}\) are given as follows:
where \(T_a\) is the duration of the approaching period, and \(p_0\) and \({n}_0\) denote the catheter tip position and tip normal at \(t=0\). \({\tilde{p}}_{closest}\) and \({\tilde{n}}_{closest}\) denote the target position and surface normal of the predicted closest POI motion point at time \(t=T_a\). A small distance vector \(\epsilon =[\epsilon _x, \epsilon _y, \epsilon _z]^T\) is added to the target tip position at the end of the approaching period \(t = T_a\) in order to leave a gap between the catheter tip and the tissue surface to avoid a premature landing, where \(\epsilon ^T {\tilde{n}} >0\). The TauGuidance function takes the input of the initial and target states of the catheter tip, and generates the approaching tip reference trajectories using (12-15).
Let \(T_d\) denote the duration for the departing period and \(T = T_a + T_d\) denote the total landing duration. The departing period reference trajectories \(\{p_r(t)\}_{t=T_a:T}\) and \(\{n_r(t)\}_{t=T_a:T}\) are given as
where \({\tilde{p}}_{furthest}\) and \({\tilde{n}}_{furthest}\) denote the target touchdown position and surface normal of the predicted furthermost POI motion point. \(\dot{{\tilde{p}}}_{furthest}\) and \(\dot{{\tilde{n}}}_{furthest}\) denote the velocity of the position and the tip normal of the predicted furthermost POI motion point. The overall tip reference landing trajectories \(\{p_r(t)\}_{t=0:T}\) and \(\{n_r(t)\}_{t=0:T}\) are given as the concatenated trajectories of the approaching and departing periods:
Let \(\{{\tilde{p}}(t), {\tilde{n}}(t)\}_{t=0:{T}}\) denote the predicted POI motion over the landing duration T, the tip reference landing trajectory generation is denoted as:
in the rest of this paper, where \(\{{\tilde{p}}(t), {\tilde{n}}(t)\}_{t=0:{T}}\) denote the predicted heart motion over the landing horizon T. \({\tilde{p}}\) and \({\tilde{n}}\) are respectively the predicted POI position and tissue surface normal.
A decoupled free-landing control optimization
In this section, a decoupled free-landing control optimization method is presented to generate the control input trajectory that tracks the reference tip trajectories \(\{p_r(t)\}_{t=0:T}\) and \(\{n_r(t)\}_{t=0:T}\). The decoupled control optimization strategy of the insertion inputs and magnetic actuation inputs is employed to improve global optimality under different control limits between the insertion and magnetic actuation and avoid frequent overshoot and retraction of the catheter insertion inputs.
The decoupled free-landing control optimization iteratively optimizes the insertion input \(l \in \mathbb {R}\) and magnetic actuation inputs \(\zeta \in \mathbb {R}^{N_c}\) independently using a rollout strategy that solves two multistep lookahead minimization problems. The first optimization problem optimizes the magnetic actuation inputs over the desired planning horizon \(T_h\) given an initial insertion input l, where the iterative Linear Quadratic Regulator (iLQR) is employed for optimizing the magnetic actuation \(\zeta\). In the second optimization problem, the catheter insertion input l is optimized by simulating the landing trajectory with the optimized magnetic actuation inputs over the desired planning horizon. At each optimization iteration i, the magnetic actuation inputs \(\zeta _{i}(t= t_0:T_h)\) for a given catheter insertion input \(l_i(t)\) are optimized using the iLQR planner. The catheter insertion inputs \(l_{i}(t= t_0:T_h)\) is then iteratively optimized such that the quadratic cost function at the end of the planning horizon is minimized.
First, the iLQR-based trajectory optimization of the magnetic actuation \(\zeta\) is presented. We consider the following discrete-time dynamic system:
where the control variable of the system \(\Delta \zeta (t) \in \mathbb {R}^{N_z}\) is the displacement of the magnetic actuation inputs. \(z(t) = [\zeta (t), l]\) is the total actuation input for a given insertion length l. The system output state \(O(t) = [X_{coil}(t), X_{tip}(t)]^T\) is the concatenated vector of the catheter rigid segment dynamic states \(X_{coil}(t)\) and the tip states \(X_{tip}(t)\) as computed in the CRM dynamics function (4).
Let \(y(t) = [p_{c}(t), n_{c}(t)]^T \in \mathbb {R}^6\) denote the tip position and tip normal components of the system output O(t), for a given initial state \(\zeta (t_0)\) and the target reference tip configuration \({y_r}({T_h}) = [{p_r}({T_h}), {n_r}({T_h}) ]^T\) at \(T_h\). The iLQR controller iteratively solves the following multistep lookahead minimization problem:
where \(c_t\) denotes the cost function at time step t, and \(\zeta ({T_h})\) denotes the terminal state. \(t_0\) denotes the initial planning time. The cost function weighting matrices \(Q_{T_h},\ Q\) and R are symmetric positive semi-definite, and \(Q_{T_h} \in \mathbb {R}^{6 \times 6}\), \(Q, \ R \in \mathbb {R}^{N_c \times N_c}\).
The iLQR controller iteratively optimizes the control inputs through a backward pass and a forward pass30. In the backward pass, a cost-to-go function \(V(\zeta , \Delta \zeta )\) is first defined as:
Let \(\delta \zeta\) and \(\delta \Delta \zeta\) denotes the small changes around \(\zeta\) and \(\Delta \zeta\), the value function S in (22) can be approximated as30:
and
where the subscripts \(_\zeta\) and \(_{\Delta \zeta }\) denote the partial derivatives with respect to the state variable \(\zeta\) and the control variable \(\Delta \zeta\), respectively. \(V'(t)\) and \(V''(t)\) denote the partial derives of the cost-to-go function with respect to the state variable \(\zeta\) where
The cost-to-go function V can be optimized iteratively by updating \(V'(t)\) and \(V''(t)\) subject to the boundary conditions:
where \(J^{*}_{T_h}\in \mathbb {R}^{6\times 6}\) is the positional and normal components of the kinematic Jacobian which is calculated as18
At each iLQR iteration, the optimal policy of the control variable \(\Delta \zeta _t\) is updated by30:
Let \(k(t) = -{{S}_{\Delta \zeta \Delta \zeta }(t)}^{-1} {S}_{\Delta \zeta }(t)\) and \(K(t) = -{{S}_{\Delta \zeta \Delta \zeta }(t)}^{-1} {S}_{\Delta \zeta \zeta }(t)\), \(V'\) and \(V''\) are updated in the backward pass as:
The new state trajectory \(\{{\hat{\zeta }}(t)\}_{t=t_0:{T_h}}\) is then propagated given the optimal control policy \(\{\Delta {\hat{\zeta }}(t)\}_{t=t_0:{T_h}}\) from (28) in the forward pass as:
The backward and forward passes are repeated iteratively until convergence. The algorithm returns the optimized magnetic actuation input trajectory \(\zeta (t)_{t=t_0:T_h}^*\) over the planning horizon \(T_h\).
The magnetic actuation optimization (22)-(30) at a given insertion length l is denoted as
where \(y({T_h})\) is the catheter tip state at the end of the planning horizon \(T_h\), as computed in (20). For each optimization iteration, the catheter insertion input l(t) at time step t is optimized by minimizing a quadratic cost function over the desired planning horizon \(T_h\) as:
where \(l^*({t})\) denotes the optimized insertion length. \(Q^l_{T_h} \in \mathbb {R}^{6\times 6}\) is a symmetric positive semi-definite weight matrix. The proposed landing control planner applies the optimized actuation inputs \(z^*(t) = [\zeta ^*(t), l^*({t})]^T\) at the servo control rate and optimizes the magnetic cost function (21) and insertion cost function (32) over the given tip reference waypoint until last tip reference configuration \(y_r(T)\) is reached.
Ablation control planner
In the rest of this paper, the decoupled free landing control algorithm given by (21-32) to calculate the optimized control input trajectory \(\{z^*(t)\}_{t=0:T}\) for an initial actuation input z(0) will be denoted as
The overall catheter ablation planner based on the proposed landing control approach is presented in Algorithm 2. The planner takes as inputs that desired landing time duration T, the entry point state variables \(X_0\), initial catheter configurations \(X_{coil}(0)\), \(X_{tip}(0)\), and actuation input z(0), and the predicted POI motions \(\{{\tilde{p}}(t), {\tilde{n}}(t)\}_{t=0:{T}}\) over the desired landing period T. In Line 1, the planner first generates the reference trajectories \(\{p_r(t)\}_{t=0:T}\) and \(\{n_r(t)\}_{t=0:T}\) as given in (19). In Line 2, the optimized control input trajectory is generated as given in (33). In Line 4, the initial catheter tip configuration is initialized with \(O(0) = [X_{coil}(0), X_{tip}(0)]^T\). Before the tip-tissue contact is established, the planner applies the free landing control inputs \(\{z^*(t)\}_{t=0:T}\) at the sample control rate, as in Lines 11-12. In Line 7, when a tip contact is detected, the catheter configuration is estimated using the tip position constraint forward kinematics in (7), and the estimated tip contact force is calculated. In Line 8, the planner proceeds to optimize the control input z(t) over the predicted heart motion over the control horizon using the receding horizon contact force controller with adaptive filter-based prediction (RHCAF)21 and update the control inputs at the servo control rate. If the tip contact is never made within the maximum time duration \(T_{max}\), a re-planning can be performed by adjusting the approaching time \(T_a\) for a more feasible landing timing, and adjusting parameters of the control optimization, such as increasing \(Q_{T_h}\) for larger end state costs.
Simulation-based validation studies
Simulation environment setup
The robotic catheter prototype used in this paper has two rigid segments (actuation coil sets) and three flexible segments, as shown in Fig. 2. The lengths of the proximal and distal coil sets are 16 mm. The Young’s modulus and shear modulus of the flexible segments are 8.22 MPa and 1.76 MPa, respectively. The initial inserted length \(l =\) 79 mm with the lengths of the tip flexible segment and the second flexible segment are 26 mm and 15 mm, respectively. The most proximal flexible segment has varied length given different insertion inputs. In this study, a stiff contact between the catheter tip and the heart tissue surface is assumed21 as the stiffness of the heart tissue \(k_s \approx 423.3\) N/m21 is significantly greater than the stiffness of the robotic catheter \(k_c = 11.6\) N/m at the configuration used in the validation studies under the desired ablation force of 0.20 N27.
Four types of in vivo heart motion data combined with respiratory motion are employed to evaluate the performance of the proposed landing method. First, two 62.5 s long regular heart rate POI motions collected at a 249 Hz sampling rate on the left ventricular (LV) of a free-beating heart from a swine model19, are used. The first POI, which is located at 1 cm laterally from the left anterior descending coronary artery and 8 cm cranially from the LV apex. The second POI is located at 5 cm laterally from the left anterior descending coronary artery and 10 cm cranially from the LV apex. The two POI motions are referred to as top and side POI motions in the rest of this paper. In addition, a 128 s long heart motion data with arrhythmia and a 200 s long varying heart rate motion data are used for evaluating the performance of the proposed landing control algorithms under the presence of arrhythmia motions and varying heart rate motions31. The arrhythmia and the varying heart rate motion data are sampled at a 404.5 Hz sampling rate. In this simulation analysis, the servo control sampling period of 48 ms, approximately matching the target servo control rate of 20 Hz of the prototype catheter system32, is used.
Simulation results
In this section, the performance of the decoupled free-landing control optimization and the overall landing control planner are evaluated in the simulation environment. First, the landing position and landing orientation accuracy using the decoupled free-landing control optimization method are evaluated at given landing locations. Additionally, the landing accuracy of an inverse Jacobian-based free-landing controller is presented for performance evaluation against the proposed decoupled free-landing control optimization. Finally, the landing accuracy, landing timing, and ablation safety and stability using the proposed ablation control planner are evaluated under the regular heart rate motion data, varying heart motion data, and arrhythmia motion data, are presented.
Simulation results of the decoupled free-landing control optimization
In this section, the landing performance of two types of landing control strategies, namely, the proposed decoupled free-landing control optimization and an inverse Jacobian-based free-landing control method, are presented and analyzed.
To evaluate the accuracy of the proposed decoupled free-landing control optimization approach, we uniformly sampled 25 target landing points over the first cycle of each of the heart motion data sets. The free-landing controller first generates the reference trajectories using (19) for each sampled target landing position, and the set of actuation trajectories \(\{z\}_{1:T}\) over the desired landing period \(T= 1\) s are generated using the decoupled landing control optimization. The tip position errors \(||{\tilde{p}}(T) - p(T)||\) between the desired touchdown point \({\tilde{p}}(T)\) and the tip position p(T) and the touchdown angles \(\alpha _d\) are calculated at the end of the actuation trajectories. The mean and variance of the tip positional errors and the touchdown angles for the 100 sampled landing motion points of the two regular heart rate POI motions, arrhythmia motion, and varying heart rate motion are presented in Table 1. The average positional error of the 100 sampled touchdown points is 2.18 mm with an average touchdown angle \(\alpha _d = 3 ^\circ\) over an average free landing distance of 11.34 mm.
An inverse Jacobian-based positional landing control is implemented for the performance comparison. Specifically, given the reference trajectories \(\{p_r(t)\}_{t=0:T}\), the controller calculates the desired control update dz(t) using a PD controller as:
where \(e_p(t) = p_r(t) - p(t)\) is the error between the reference position and the actual catheter tip position. \(K_p\) and \(K_d\) are the proportional and derivative coefficients, respectively. \(J_p \in \mathbb {R}^{3\times Nz}\) is the positional component of the kinematic Jacobian \(J^*\) in (27). The controller then iteratively updates the control inputs as
until the end point of the reference trajectory is reached.
The simulation results using the inverse Jacobian-based free-landing control of the 100 sampled target tip positions over the 4 heart motion data sets are presented in Table 2. The average positional error of the 100 sampled touchdown points is 5.25 mm. The large positional error of the inverse Jacobian-based free-landing control is caused by the different control scales of the insertion input and the magnetic actuation. The inverse Jacobian-based free-landing controller has difficulty correcting the steering of the catheter tip when the x and y directional position error is large. The decoupled free-landing controller is able to correct the steering efficiently by optimizing the insertion and magnetic actuation independently over the expected control horizon. The inverse Jacobian-based free-landing controller is also prone to instability when the catheter configuration is close to singularity.
Simulation results of the landing control planner
The effectiveness of the proposed landing strategy for robotic catheter ablation are evaluated using the four types of heart motion data. The robotic catheter ablation planner proposed in Algorithm 2 is then applied to the 4 in vivo heart motion data sets. The first cycle of the heart motion is used for the tip reference trajectory generation in (19). The desired approaching period \(T_a\), departing period \(T_d\) and the overall desired landing period \(T^*\) for the 4 types of heart motion data are given in Table 3. The actual free landing time period \(T'\), the positional error \(||{\tilde{p}}(T')-p(T')||\) and the touchdown angle \(\alpha _d\) at the touchdown point are presented in Table 4. In addition, the average normal contact force \(f_n\) and average contact ratio \(\sigma\) over 3 cycles of the heart motion after establishing the tip-tissue contact, are presented.
In Table 4, the touchdown timing errors \(|T^*-T'|\) for the top and side regular heart rate motions, varying heart rate motion, and the arrhythmia motion are 0.1 s, 0.3 s, 0.1 s, and 0.3 s, respectively. The touchdown positional error \(||{\tilde{p}}(T')-p(T')||\) for the side regular heart rate motion is 4.1 mm, with a larger average contact ratio \(\sigma =0.19\), compared to the top POI regular heart rate motion, varying heart rate motion, and the arrhythmia motion sets, is due to the larger average motion variations, as shown in Table 5.
The landing process for the top POI regular heart rate motion at 6 sample time stamps are presented in Fig. 6. In Fig. 6 (a)-(c), the robotic catheter and the heart surface configuration during the free landing process at \(t=\) 0 s, 0.5 s, and 1.1 s, are shown. The catheter tip reached the touchdown motion point at \(t=\) 1.1 s. Fig. 6d shows the catheter configuration at \(t=\) 1.5 s where the catheter tip-surface contact is established with a normal contact force \(f_n =\) 0.20 N and a contact ratio \(\sigma =\) 0.11. Figure 6e shows the catheter configuration at \(t=\) 3.1 s with a normal contact force \(f_n =\) 0.16 N and a contact ratio \(\sigma =\) 0.09. Finally, Fig. 6f shows the catheter configuration at \(t=\) 4.1 s after 3 heart motion cycles with a normal contact force \(f_n =\) 0.16 N and a contact ratio \(\sigma =\) 0.08. The friction cone FC and the contact force \(f_c\) (marked by the red arrow) are also shown in (d)-(f).
(a)-(c) The configurations of the robotic catheter and the heart surface during the free landing process at \(t =\) 0, 0.5, 1.1 s. At \(t=\) 1.1 s, the catheter tip reached the touchdown motion point. (d) The robotic catheter is in contact with the surface during the ablation phase at \(t=\) 1.5 s, with normal contact force \(f_n =\) 0.20 N and contact ratio \(\sigma =\) 0.11. The friction cone FC and the contact force \(f_c\), marked by the red arrow, are also presented. (e) The robotic catheter at \(t=\) 3.1 s, with normal contact force \(f_n =\) 0.16 N and contact ratio \(\sigma =\) 0.09. (f) The robotic catheter at \(t=\) 4.1 s, with normal contact force \(f_n =\) 0.16 N and contact ratio \(\sigma =\) 0.08.
Discussion and conclusion
In this paper, a landing control method for an MRI-actuated robotic catheter landing on a beating heart surface is proposed. An ablation phase analysis is first presented to investigate the optimal catheter tip configuration at the touchdown point for achieving a stable and safe tip-tissue contact during the ablation. A free landing control algorithm that generates a desired tip reference trajectory given the predicted heart surface motion, is proposed. A decoupled landing control optimization algorithm to generate the control input trajectories that guide the catheter tip to the desired touchdown configuration, is proposed. Finally, a robotic catheter ablation planner based on the proposed landing control strategy is presented. The robotic catheter ablation planner employs the proposed free landing controller that drives the catheter tip to the target touchdown position and optimizes the catheter-tip tissue contact using the receding horizon contact force controller proposed in21 during the ablation phase. The simulation-based studies provide an evaluation of the proposed landing control strategy and the robotic catheter ablation planner, which paves the way for hardware implementation and validation of the proposed landing control methods in future research.
The simulation results show that the decoupled landing controller achieves better accuracy and stability for the free-landing process of the MRI-actuated robotic catheter, compared to an inverse Jacobian-based landing controller. The robotic catheter ablation planner based on the decoupled landing controller is able to establish stable contact quickly for the given heart motions and provide appropriate normal force levels for the ablation procedure. The contact ratios for the side POI motion during the ablation phase exceed the static friction coefficient due to the large-scale motion variations. It’s important to note that the motion variations of the left ventricle heart motion are significantly larger than the motion variations of the left atrium, where the ablation procedure is performed. The additional landing results for the top, side regular heartbeat motions, varying heartbeat motions, and arrhythmia motions are provided in the supplementary video.
The presented simulation results indicate that the proposed landing control method is able to achieve a stable and safe tip-tissue contact, towards an automated robotic catheter ablation procedure. Although the simulation results demonstrate the feasibility of the proposed landing control method, several limitations of the proposed methods are identified. In this work, the variation of the heart surface orientation during the heartbeat motion is ignored, since the proposed landing control method emphasizes on the landing performance under the positional change of the heart motions, although the ablation phase analysis method proposed in Sect. 5.1 is applicable to the heart surface motions with simultaneous positional and orientation variations. A potential avenue for future work is to include the variations of the heart surface orientations as an additional optimization objective. The approaching and departing periods \(T_a\) and \(T_d\) are determined by predicted heart motion and the desired landing period T. However, in cases where the desired tip position is not reachable within the given landing periods, the calculated control inputs can lead to instability of the catheter configurations. In this case, the landing periods \(T_a\) and \(T_d\) require extra tuning to guarantee the desired tip position is reachable within the given time period. Blood flow disturbances are ignored during the landing process as this work emphasizes on the catheter landing process under the effect of the disturbances caused by the beating heart motions.
The tip-constrained Cosserat-Rod models, and the dynamic model of the catheter are implemented in C/C++ on Ubuntu 22.04 operating system. The proposed landing control method is implemented in MATLAB ®. The computer is equipped with Intel® CoreTM i9-11900 CPU @ 2.50 GHz and 31.0 GB memory. MATLAB’s constrained optimization function fminbnd is employed for the optimization of the inserted length l in (32). The landing control algorithm achieves an average computation time of approximately 42.40 seconds per case study, demonstrating practical feasibility and computational efficiency for preprocedural planning of the catheter ablation. The computation time can be further reduced with a fully optimized C/C++ implementation. Additionally, the proposed ablation control planner achieves catheter tissue contact forces within the desired safe range, with positional accuracy ranging from 1.7 mm to 4.1 mm under regular heart rate, varying heart rate, and arrhythmia motions, highlighting its effectiveness in optimizing both contact safety and control accuracy.
As part of our future works, the effect of the blood flow disturbances and heart surface orientation variations will be incorporated into the proposed landing control method. Our future work will also focus on the hardware implementation and validation of the proposed landing control algorithms. The experimental validation of the proposed methods on hardware is the next step once the real-time tracking algorithms of the robotic catheter system and the tissue surface from intra-operative MRI imaging are available. The analysis results and landing strategy provided by the proposed methods will be experimentally validated using a prototype of our MRI-actuated robotic catheter system as part of the subsequent research. The experimental validation will be performed once the real-time tracking of the robotic catheter system and the real-time tissue surface from intra-operative MRI imaging are available. These algorithms are currently under development as part of a parallel research study in our research group.
Data availability
All data generated or analyzed during this study are included in this published article (and its Supplementary Information files)
Notes
The readers are referred to18 for a detailed discussion of the free tip forward kinematics model.
In this study, we use a static coefficient of friction of 0.2, which implies that the touchdown angle must be smaller than 11.3 to ensure stable catheter tip tissue contact. For validation, we analyze touchdown angles within the range of 0 to 30 .
References
Marrouche, N. F. et al. Catheter ablation for atrial fibrillation with heart failure. N. Engl. J. Med. 378, 417–427 (2018).
Dewire, J. & Calkins, H. State-of-the-art and emerging technologies for atrial fibrillation ablation. Nat. Rev. Cardiol. 7, 129 (2010).
Liu, T. et al. Modeling and validation of the three-dimensional deflection of an MRI-compatible magnetically actuated steerable catheter. IEEE Trans. Biomed. Engineering 63, 2142–2154 (2016).
Greigarn, T. Kinematics, Planning, and Perception for Magnetically-Actuated MRI-Guided Continuum Robots. Ph.D. thesis, Case Western Reserve University (2018).
Yuen, S.G. et al. Robotic force stabilization for beating heart intracardiac surgery. In International Conference on Medical Image Computing and Computer-Assisted Intervention, 26–33 (Springer, 2009).
Zhang, Z., Dequidt, J., Back, J., Liu, H. & Duriez, C. Motion control of cable-driven continuum catheter robot through contacts. IEEE Robotics Autom. Lett. 4, 1852–1859 (2019).
Kesner, S. B. & Howe, R. D. Robotic catheter cardiac ablation combining ultrasound guidance and force control. Int. J. Robot. Res. 33, 631–644 (2014).
Kanagaratnam, P. et al. Experience of robotic catheter ablation in humans using a novel remotely steerable catheter sheath. J. Interv. Card. Electrophysiol. 21, 19–26 (2008).
Ernst, S. Robotic approach to catheter ablation. Curr. Opin. Cardiol. 23, 28–31 (2008).
Rillig, A. et al. Manual versus robotic catheter ablation for the treatment of atrial fibrillation: The man and machine trial. JACC: Clinical Electrophysiol.3, 875–883 (2017).
Hlivák, P. et al. Robotic navigation in catheter ablation for paroxysmal atrial fibrillation: midterm efficacy and predictors of postablation arrhythmia recurrences. J. Cardiovasc. Electrophysiol. 22, 534–540 (2011).
Greigarn, T., Poirot, N. L., Xu, X. & Cavusoglu, M. C. Jacobian-based task-space motion planning for MRI-actuated continuum robots. IEEE Robotics and Automation Letters (2018).
Bajo, A. & Simaan, N. Hybrid motion/force control of multi-backbone continuum robots. Int. J. Robot. Res. 35, 422–434 (2016).
Yip, M. C. & Camarillo, D. B. Model-less hybrid position/force control: a minimalist approach for continuum manipulators in unknown, constrained environments. IEEE Robot. Autom. Lett. 1, 844–851 (2016).
Jayender, J., Patel, R. V. & Nikumb, S. Robot-assisted active catheter insertion: Algorithms and experiments. Int. J. Robot. Res. 28, 1101–1117 (2009).
Yip, M. C., Sganga, J. A. & Camarillo, D. B. Autonomous control of continuum robot manipulators for complex cardiac ablation tasks. J. Med. Robot. Res. 2, 1750002 (2017).
Hao, R., Tuna, E.E., Itsarachaiyot, Y. & Çavuşoğlu, M. C. Free-space dynamic modeling of an mri-actuated robotic catheter. IEEE Transactions on Mechatronics (under review) (2024).
Itsarachaiyot, Y., Hao, R. & Çavuşoğlu, M.C. Analytical computation of the contact force jacobian for mri-actuated robotic catheter. In 2023 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS) (IEEE, 2023).
Tuna, E. E. et al. Heart motion prediction based on adaptive estimation algorithms for robotic-assisted beating heart surgery. IEEE Trans. Rob. 29, 261–276 (2012).
Liu, T., Poirot, N., Greigarn, T. & Cavusoglu, M. Design of an MRI-guided magnetically-actuated steerable catheter. ASME Journal of Medical Devices, Special Issue on Cardiovascular Device Development and Safety Assessment using Computational and/or Experimental Approaches11 (2017).
Hao, R., Erdem Tuna, E. & Çavuşoğlu, M. C. Contact stability and contact safety of a magnetic resonance imaging-guided robotic catheter under heart surface motion. J. Dyn. Syst. Meas. Control143 (2021).
Ho, S. Y., Cabrera, J. A. & Sanchez-Quintana, D. Left atrial anatomy revisited. Circulation: Arrhythmia Electrophysiol.5, 220–228 (2012).
Kazmierska, K., Szwast, M. & Ciach, T. Determination of urethral catheter surface lubricity. J. Mater. Sci. - Mater. Med. 19, 2301–2306 (2008).
Prokopovich, P. et al. Frictional properties of light-activated antimicrobial polymers in blood vessels. J. Mater. Sci. - Mater. Med. 21, 815–821 (2010).
Andrade, J. G. et al. Pulmonary vein isolation using contact force ablation: the effect on dormant conduction and long-term freedom from recurrent atrial fibrillation a prospective study. Heart Rhythm 11, 1919–1924 (2014).
Williams, S.E. et al. The effect of contact force in atrial radiofrequency ablation: electroanatomical, cardiovascular magnetic resonance, and histological assessment in a chronic porcine model. JACC: Clinical Electrophysiology1, 421–431 (2015).
Thiagalingam, A. et al. Importance of catheter contact force during irrigated radiofrequency ablation: evaluation in a porcine ex vivo model using a force-sensing catheter. J. Cardiovasc. Electrophysiol. 21, 806–811 (2010).
Kendoul, F. Four-dimensional guidance and control of movement using time-to-contact: Application to automated docking and landing of unmanned rotorcraft systems. Int. J. Robot. Res. 33, 237–267 (2014).
Yang, Z., Fang, Z. & Li, P. Decentralized 4d trajectory generation for uavs based on improved intrinsic tau guidance strategy. Int. J. Adv. Rob. Syst. 13, 88 (2016).
Li, W. & Todorov, E. Iterative linear quadratic regulator design for nonlinear biological movement systems. In ICINCO (1), 222–229 (Citeseer, 2004).
Tuna, E. E. et al. Towards active tracking of beating heart motion in the presence of arrhythmia for robotic assisted beating heart surgery. PLoS ONE 9, e102877 (2014).
Tuna, E.E. et al. Analysis of dynamic response of an MRI-guided magnetically-actuated steerable catheter system. In Proceedings of the IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), 4927–4934 (2018).
Acknowledgements
This work was supported in part by the National Science Foundation under grants CISE IIS-1524363, CISE IIS-1563805, ENG IIP-1700839, and the National Heart, Lung, and Blood Institute of the National Institutes of Health under grant R01 HL153034.
Author information
Authors and Affiliations
Contributions
Ran Hao wrote the main manuscript text and and M. Cenk Cavusoglu edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Information 1.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hao, R., Cavuşoğlu, M.C. Landing control of a magnetically actuated robotic catheter on beating heart surface. Sci Rep 15, 34581 (2025). https://doi.org/10.1038/s41598-025-18054-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-18054-2