Abstract
The prevalence of visual impairment (VI) increases with axial length (AL) and spherical equivalent (SE). This study aims to explore the prevalence and associated factors of myopia and AL-related VI in children and adolescents, including analysis of sex-specific differences. This cross-sectional survey included 2595 children and adolescents aged 4–18 years from nine educational institutions in a large municipality. The survey comprised a questionnaire, visual acuity examination, refractive screening and AL measurement. The prevalence of myopia and AL-related VI were 56.53% and 50.98% respectively and increased with age (P < 0.01). The myopia rate was higher in females than in males (60.23% vs. 52.71%, χ2 = 14.93, P < 0.05), with a significant difference observed in those aged 9 years and older. However, there was no sex difference between in the prevalence of AL-related VI (51.37% vs. 50.61%, χ2 = 0.15, P = 0.70). The research showed that older adolescent was a risk factor for both myopia (OR = 2.28, 95%CI = 2.06–2.53) and AL-related VI (OR = 2.49, 95%CI = 2.23–2.77). Having a myopic parent was also significantly associated with myopia (OR = 1.21, 95%CI = 1.12–1.32) and AL-related VI (OR = 1.25, 95%CI = 1.16–1.36). The prevalence of myopia and AL-related VI were high and increased with age in children and adolescents, with sex-specific differences in myopia but not in AL-related VI. Therefore, it is possible to predict the risk of myopia by considering age- and sex-specific factors.
Similar content being viewed by others
Introduction
Childhood visual impairment (VI) is a global public health challenge, particularly in low- and middle-income countries1. Globally, it is estimated that there are 19 million children under the age of 15 years old suffer from VI2, with uncorrected refractive error (RE) being the predominant cause1. The consequences of childhood VI extend far beyond visual deficits, potentially causing profound and sometimes irreversible impact on children’s psychological well-being, educational attainment, and social performance, which can persist into adulthood and affect individuals’ quality of life3.
Myopia is a type of refractive error in which the eye’s refractive system focuses parallel light rays in front of the retina rather than directly on it when in the relaxed state4. The World Health Organization (WHO) projects a staggering more than 3.36 billion cases of myopia by 2030, respresenting a 72.3% increase since 20105. The WHO also reported that the highest overall prevalence of myopia worldwide is in high-income countries in the Asia Pacific region (53.4%), followed by East Asian countries (51.6%)5. In East Asian countries, up to 80% of high school graduates have myopia and 10% have high myopia6. China exemplifies this growing crisis, with recent National Health Commission survey reporting the overall myopia prevalence of 51.9% among children and adolescents in 2022, which shows a trend of early onset and high incidence7. If without effective intervention, myopia might progress to high myopia,potentially causing permanent irreversible vision damage or other severe ocular complications8,9.
Cycloplegic refraction remains the gold standard for myopia detection10. However, the administration of cycloplegic eyedrops presents practical challenges in children, particularly in large-scale epidemiological studies where resources for cycloplegic refraction may be limited. Thus, non-cycloplegic refraction continues to be widely employed in population-based studies to assess the prevalence and severity of pediatric myopia11. Previous study suggested that combining non-cycloplegic refraction with visual acuity measurements significantly improves myopia detection accuracy compared to using non-cycloplegic refraction alone12. The approach endorsed by China for school-based myopia screening in children. Critically, AL elongation is the hallmark of myopia pathogenesis13. Axial myopia is diagnosed when the increase in AL surpasses the compensatory reduction in corneal and lenticular refractive power13. Current studies suggest that VI is more strongly associated with AL than with refractive error alone14, and excessive AL elongation gives precipitate vision-threatening complications including myopic retinopathy, retinal detachment, and glaucoma8,9. These clinical insights underscore the critical need to investigate risk factors associated with AL-related VI.
Although many previous studies have reported on the prevalence and risk factors of myopia and VI in school-aged children1,3,4,9,10,15,16,17,18. There remains a significant gap in research regarding the epidemiology of AL-related VI in children. Early myopia control clinical studies did not measure and monitor axial elongation, making refractive error the preferred outcome measure. More recently, the measurement of ocular biometric components of the eye has become more widely included and is a key measurement in myopia control clinics. The advantages of using axial elongation versus refractive error as the primary outcome measure relates to the direct relationship between the excessive growth of the myopic eye and the associated risk for posterior pole complications, although the two are strongly correlated19. Current evidence primarily focuses on refractive error as the primary metric for VI, with few population-based studies examining the burden and risk factors of AL-related VI20,21. Myopia-related VI is associated with structural changes of the retina and the globe because of elongation of the eye axis. Previous study demonstrated that VI is associated with AL and spherical equivalent (SE)22. This gap is critical given that excessive AL elongation precipitates vision-threatening complications (e.g., myopic maculopathy, retinal detachment) and is more strongly associated with irreversible vision loss than refractive error alone. The AL-VI might provide a missing link between anatomical change and functional vision loss, enabling targeted screening prior to refractive shift. The aims of this study were to assess the common causes of myopia and AL-related VI, and examine variations in prevalence rates by sex and age groups. The findings might inform the development of targeted ocular health care services for children in specific geographic regions.
Methods
Overview
This cross-sectional observational study constituted a sub-study of Beijing Children and Adolescents Health Cohort (BCHC) from 2022 to 202323. The parent BCHC is a prospective cohort study that enrolled 5579 children and adolescents from a demographically representative district of Beijing, characterized by urban-suburban integration and moderate socioeconomic status. At baseline, all participants underwent comprehensive assessments of exposure factors related to obesity, myopia, growth and development, physical activity, dietary patterns, sleep behaviors, and other behavioral determinants. For this sub-study, we employed a stratified cluster random sampling approach to select 2742 children and adolescents aged 4–18 years from nine educational institutions in Beijing.
Participants recruitment
All procedures were approved by the Institutional Review Board of the Capital Institute of Pediatrics prior to study commencement. We conducted a vision survey in which all students from nine educational institutions in Beijing (186 students from one kindergarten, 1452 students from five primary schools, 1394 students from two middle schools, and 664 students from one high school) who met the inclusion criteria were enrolled as study participants in 2022. The inclusion criteria were: (1) children and adolescents aged 4–18 years who were permanent residents of Beijing; (2) no history of ocular diseases, eye injuries, or ocular surgeries(except for refractive errors); (3) in good physical and mental health without congenital developmental abnormalities or systemic conditions that might affect vision or refractive examinations; (4) no wearing of corneal gas-permeable contact lenses within the previous month; and (5) willingness to cooperate by both children and their parents or guardians. In total, 2742 children and adolescents aged 4–18 years underwent comprehensive screening, including non-cycloplegic refraction, binocular uncorrected visual acuity testing, AL measurement. Standardized testing conditions were maintained by optimizing ambient illumination and minimizing potential visual distractions. A questionnaire survey was administered (completed by their parents for kindergarten children, and jointly by participants and their parents for school-age children). Following data quality control procedures involving logical verification and exclusion of inconsistent records, complete datasets were obtained for 2595 participants (effective response rate: 94.6%), as detailed in Fig. 1. The study participants were stratified into four age groups: 4–6 years (children), 7–9 years (children), 10–12 years (adolescents), and 13–18 years (adolescents).
Based on the reported myopia prevalence rate of 51.9% among children and adolescents in 20227, we estimated a similar rate of myopia in our target population. Allowing for an error of 2% level of significance (type 1 error), a 95% confidence interval, and a loss to follow-up rate less than 8%, a sample size of 2582 children and adolescents would be needed to achieve our study objectives.
Ethical considerations
We followed all Helsinki declaration and national ethical standards. All participants were ensured about the matter of confidentiality, written consent of the participants who was witnessed and formally recorded, was obtained before data collection. Identifiable information was removed from the collected data to ensure confidentiality, and access to these digital files was restricted to members of the research team. This study was approved by the Medical Ethics Committee of the Capital Institute of Pediatrics (SHERLL2022043). The guardian and/or their children provided informed consent and were willing to participate, and the investigation was approved by the local education bureau and school. To express our gratitude for their contributions, participants were given a Health check-up report which was promptly emailed to them following their interview.
Measurements and devices
This study evaluated visual acuity, refractive status, and AL in children and adolescents following standardized protocols. Visual acuity testing was performed using logarithmic visual acuity charts compliant with the GB/T 11,533–2011 standard for, which is a 5-mark record. Refractive status was assessed using a desktop autorefractor (KR-800; Topcon Corporation, Tokyo, Japan) that meets ISO 10,342 ophthalmic instrument standards for non-cycloplegic measurements. AL was measured using an optical biometer (IOL Master; ZEISS Group, Oberkochen, Germany). All instruments were validated and approved by regulatory authorities. Both autorefractors and biometers underwent simulated human eye calibration prior to use24. Participant screening followed the Guidelines for Appropriate Techniques for Myopia Prevention and Control in Children and Adolescents (Updated Version) issued by China’s National Health Commission25.
Myopia definition
Myopia in children aged 4–6 years: According to the Guidelines for Pediatric Eye Evaluations Preferred Practice Pattern (Updated Version) issued by the American Academy of Ophthalmology26, the criteria for determining myopia were that children aged 4–6 years with the sphere power(S) of <− 2.00 diopters(D) (detected using a computer refractometer in a noncycloplegic refraction state)26.
Myopia in children and adolescents aged ≥ 7 years: According to the International Myopia Institute (IMI)4 and the National Health Commission’s “Guidelines for Appropriate Techniques for Prevention and Control of Myopia in Children and Adolescents (Updated Edition)”25, the criteria for determining myopia eye the standard logarithmic visual acuity of the naked eye < 5.0 and SE < –0.50D.
While non-cycloplegic refraction is a practical approach, particularly in large-scale studies, it is predisposed to overestimating refractive error in younger children (versus cycloplegic gold-standard)27.The myopia prevalence in pre-school children and school-age children were defined respectively, and should be interpreted as screening indicators.
AL-related VI definition
According to the Expert Consensus on AL Reference Ranges for School-Aged children in 202228, and the average normal AL is 23.5 mm (range: 22–24.5mm). Clinically, AL is shorter than average in hyperopic eyes and longer than average in myopic eyes29. AL > 23.5 mm is generally regarded as indicative of abnormal axial elongation. In this study, we defined AL-related VI as AL measurement > 23.5 mm and uncorrected visual acuity < 5.0. Any participant meeting the definition in at least one eye was included in the total count of AL-related VI cases.
Data collection
We designed a self-administered questionnaire based on “the work plan of monitoring and intervention of common diseases and health effects among students” normative guidelines, and similar previous studies30,31. The questionnaire including demographic and behavioral data (e.g., sex, age, parental myopia, visual behaviors and environment, screen time, reading habits) were collected and administered by trained investigators. Both participants and their parents or legal guardians were imformed ahout the study, provided their consent and filled out questionnaires. Before completing the questionnaire, the survey or explained the significance of the survey, emphasized the confidentiality of the questionnaire, and any questions that were not understood would be explained by the investigator until the participants or their parents could understand the questions correctly in order to guarantee the credibility of the results. This approach aimed to enhance response reliability,though some degree of recall bias may still be present in the questionnaires.
Quality control
The on-site investigation was conducted by trained and qualified medical personnel using standardized vision examination methods and survey questionnaires30,31. The original data were collected and organized by the school as a unit.Designated personnel verified and entered the data. Health records were created for follow-up care and to notify participant of the results. Vision examinations adhered to national standards (using a standard light box), adhering to prescribed methodology, testing environment and viewing distance. In a semi-dark room, refractive testing of children in the natural state was performed to ensure that the system error was within a reasonable range. All examinations took place in a controlled environment with fixed conditions and appropriate lighting. The child’s seat was fixed within a radius of 50 cm, the head was kept upright, and the eyes were level with the instrument. The interocular distance between the right and left eyes was 35 cm. The average value of at least three consecutive readings from an autorefractor was used for analysis, and the average value of at least five consecutive readings from an axial biometric instrument was used for analysis.
Statistical analysis
The data were entered into an Excel 2007 spreadsheet. All statistical analyses were performed with R software 4.1.3. The Shapiro Wilk test was used to determine the normality of the data. Continuous variables were presented as mean ± standard deviation (mean ± SD). For skewed variables, non-parametric tests (Mann–Whitney U) were employed. Descriptive data are presented as frequency and percentage or mean with Wald 95% confidence interval (CI). Categorical variables are presented as frequency and percentage, and continuous variables are expressed as mean with standard deviation. These associations were tested using chi-square analyses or the correlation index, depending on the type of variables involved. Variables, which have a p-value of less than 0.05 in the univariate analysis of myopia, were selected and evaluated by multivariable logistic regression models. Our models demonstrated excellent discriminative power (AUC ≥ 0.70). The low VIF values (< 1.12) indicates no multicollinearity. Hosmer–Lemeshow P > 0.05 (adequate fit). The results of multivariable logistic regression are presented with odds ratio (OR) and 95%CI. Statistical significance was defined as P < 0.05.
Results
Basic information of myopia and AL-related VI among children and adolescents
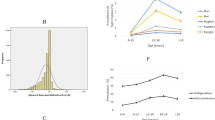
In total, 2595 children and adolescents were surveyed. The overall myopia rate was 56.53% (1467/2595),with a higher rate in females (60.23%) compared to males (52.71%) (χ2 = 14.93, P = 0.03). By age group, the myopia rate was 7.73% in children aged 4–6 years, 36.12% in children aged 7–9 years, 58.26% in adolescents aged 10–12 years, and 69.05% in adolescents aged 13–18 years. Sex difference in myopia rates between females and males were statistically significant in the 7–9 and 13–18 age groups (χ2 = 3.85, P = 0.05; χ2 = 12.37, P = 0.00). The rate of AL-related VI was 50.98% (1323/2595), with rates of 51.37% in boys and 50.61% in girls. By age group, the rate of AL-related VI was 5.31% in children aged 4–6 years, 26.68% in children aged 7–9 years, 51.42% in adolescents aged 10–12 years, and 64.79% in adolescents aged 13–18 years. In contrast to myopia, there was no statistically significant sex difference in AL-related VI rates (χ2 = 0.15, P = 0.70), as detailed in Table 1. Furthermore, the analysis revealed that the overall myopia rate was higher in females than in males, and this difference was significantly greater among females aged ≥ 9 years compared to males of the same age. Conversely, the overall AL-related VI rate was generally similar between males and females.However, it was significantly higher in males aged 10-12 years than in females of the same age group, as illustrated in Fig. 2.
Univariate analyses of factors associated with myopia and AL-related VI
The analysis of influencing factors for myopia and AL-related VI in children and adolescents revealed statistically significant differences associated with age, reading distance, long-distance reading time on electronics, near work time, children’s knowledge of the 20-20-20 rule, learning lighting, and parental myopia (all P < 0.05). Conversely, time spent on near screen using electronics, daily reading posture, and table arrangement were not significant influencing factors for either myopia or AL-related VI in this population (P > 0.05). Females were significantly more prone to developing myopia than males (χ2 = 14.93, P < 0.01). However, the difference in AL-related VI rates between females and males was not statistically significant (χ2 = 0.15, P = 0.70). Both myopia and AL-related VI showed a strong correlation with increasing age (χ2 = 330.91, P < 0.01; χ2 = 353.04, P < 0.01, respectively). Details are shown in Table 2.
Multivariable logistic regression analysis of myopia and AL-related VI
We applied multivariable logistic regression models to identify the effects of the investigated factors on Myopia and AL-related VI. A total of nine variables with P < 0.05 in the univariate analysis (Table 2) were entered into the initial multivariable logistic regression model for Myopia. Similarly, a total of eight variables with P < 0.05 in the analysis (Table 2) were entered into the initial multivariable logistic regression model for AL-related VI. In multivariable model, female sex, age and parental myopia were significantly associated with myopia. The survey shows that older age and parental myopia were significantly associated with AL-related VI. According to this analysis, each additional year of age was associated with a 2.28-fold higher risk for myopia (95% CI 2.06–2.53; P = 0.00), and a 2.49-fold higher risk for AL-related VI (95% CI 2.23–2.77; P = 0.00). Females were significantly more likely to have myopia (adjusted OR = 1.29, 95% CI 1.08–1.53; P = 0.005). Additionally, compared with the reference group (children with no myopic parents), participants with either one parent or both parents had myopia had a higher risk of both myopia and AL-related VI (adjusted OR = 1.21, 95% CI 1.12–1.32; P = 0.00; adjusted OR = 1.25, 95% CI 1.16–1.36; P = 0.00), as detailed in Table 3.
Discussion
Compared with other ocular structures, such as the cornea and crystalline lens, AL was the principal morphological factor related to refractive error progression22. In this study, we investigated the prevalence of myopia and its associated risk factors among children and adolescents in Beijing, with novel consideration of AL-related VI. The overall prevalence of myopia and AL-related VI were 56.53% and 50.98% among participants aged 4–18 years, respectively. It underscored the growing public health concern of VI in younger populations. Notably, our myopia prevalence exceeded national23 and global maxima7, despite methodological variations across studies16. Rigorous school-based sampling and standardized measurements enhance result validity.
The analysis reinforced the importance of age as a key predictor of both myopia and AL-related VI. The prevalence of myopia rose dramatically from 7.73% in the preschoolers to 69.05% in the high school adolescents, while AL-related VI increased dramatically from 5.31% to 64.79% across the same age groups. While our study used a fixed AL threshold (> 23.5 mm) to define AL-related VI, we acknowledged that AL varies with age during ocular development14,28,32. At younger ages, the range of AL across the population was narrow but progressively expanded with age. Influence of environmental risk factors would be minimal at younger ages, whereas the expanding range of AL may suggest greater influence of environmental risk factors at older ages14. The prevalence of myopia increased with age, and it increased particularly rapidly after 7 years old. The sharpest myopia acceleration occurred in children aged 7–9 years (from 7.73% to 36.12%), followed by adolescents aged 10–12 years. These findings were consistent with the previous surveys18,33.This trend aligns with evidence suggesting earlier myopia onset age and increasing progression rates17. The following are possible contributing factors. First, the irreversible nature of myopia might lead to cumulative prevalence in older adolescents. Second, children in China generally entered school around age 7 years old, and as their academic burden increased, they generally spent less time outdoors and more time engaged in near work such as close reading33. This prolonged near work might strain the ciliary muscles, increasing the risk of myopia development.
Sex differences were identified as an independent risk factor of myopia. Females showed higher prevalence of myopia than males (60.23% vs. 52.71%), particularlyfrom age 9 years onward, which was consistent with prior surveys18,34. This disparity might reflect behavioral differences, as males typically engage in more outdoor activities (a known protective factor)35, while females favor indoor near work tasks36. In contrast, the overall rate of AL-related VIwas similar between sexes (51.37% vs. 50.61%), although males aged 10-12 years showed elevated rates. The result might be related to the educational levels, near work time, outdoor activity and reach puberty by sex difference. It was possible that females who reach puberty earlier are also more likely to be heavier and taller than males of the same age and to develop myopia earlier37. However, the underlying mechanisms behind this sex difference remain unclear. These findings support initiating sex-specific myopia prevention before puberty. Thus, the early phases of puberty might be a sensitive period to control myopia in females. In this regard, special attention should also be paid to increase females’ outdoor physical activity and vision screening on myopia, and targeted measures should be formulated according to different genders to effectively protect the eye health of children and adolescents38.
Parental myopia was also identified an independent risk factor for both myopia and AL-related VI. Multivariable analyses confirmed that age, sex, and parental myopia as independently risk factors for myopia, while age and parental myopia as independently risk factors for AL-related VI. Hereditary influences align with prior studies39, although environmental modulators remain critical.
Univariate analyses identified additional significant risk factors for myopia and AL-related VI, including shorter reading distance, prolonged near-work time, inadequate learning lighting, and etc. These findings emphasized the role of environmental and genetic factors in the development of VI. While congenital factors are immutable, environmental factors and individual modifiable behaviors are critical intervention targets to prevention and control of myopia, such as visual habits, lifestyle, and outdoor activity. Detrimental eye habits associated with increased the risk of myopia include prolonged near work time exceeding 60 minutes continuously, reading distance less than 33 cm, incorrect reading and writing postures, excessive using screen time, and reading in bed or in moving vehicles40. In the past, it was believed that correct reading and writing posture should be maintained to achieve “one fist, one foot, and one inch”25,26. Different reading postures might affect reading comfort, but the main risk factors affecting the occurrence of myopia were reading distance and near work time41. The present study showed that a near learning time of > 60 min and reading distance of < 33 cm between the eyes and the book during reading were associated with myopia,which was consistent with the previous survey results42. Additionally, the 20-20-20 rule, which encouraged regular breaks during near-work activities, was an effective strategy for reducing digital eye strain and dry eye symptoms43. Its direct impact on myopia progression remains unproven. However, this study suggested that children and adolescents who were aware of the 20-20-20 rules had a significant association with myopia, suggesting that the 20-20-20 rule compliance might be a potential protective. Heredity played a role, but modifiable habits (adherence to the 20-20-20 rule in your daily eye habits might enhance visual health) were protective44. The 20-20-20 rule might help with eyestrain by allowing for intermittent distance viewing which may reduce accommodative lag. Previous studies have suggested a possible relationship between variability in accommodation and the development of myopia45.
Whether near screen time increased the risk of myopia remains controversial.A meta-analysis showed no significant correlation between screen use and myopia ocurrence46, aligning with our survey’s null result for near screen time, possibly attributable to parental restrictions limiting exposure47. This contrasts with established evidence linking prolonged near-vision work to elevated myopia risk, where each additional daily hour of digital screen time significantly increased odds ratios in prior studies47. Notably, our data revealed a paradoxical pattern, participants who used long-distance electronic devices for more than one hour per day had a lower prevance of myopia. The association remained insignificant for screen time exposure of up to one hour per day, suggesting a potential safety threshold47. The use of long-distance electronic products might reduce near work time and avoid high tension of the ciliary muscles and excessive lens flexion to a certain degree. In addition, many parents of children and adolescents with myopia required that the screen use did not exceed one hour per day. These factors might also contribute to reduce the risk of myopia.
Unexpectedly, we found that the combined use of both a fluorescent desk lamp and roof light was associated with myopic refraction, which was inconsistent with previous study48. Artificial natural light in the classroom of primary schools might result in reducing incidence rate of myopia49. In our study, combined traditional fluorescent lamp with low frequency of flicker and LED lamp on the desk increased risk, possibly due to fluorescent lamp with low frequency of flicker implicated in animal models to be capable of inducing myopia50. Whether this association attributed to the lamp characteristic remained unclear. Desk placement near windows showed no protective effect on myopia (P > 0.05), which was similar to prior study, though natural light exposure might offer indirect benefits on eyes51. Previous studies have shown that violet light with a wavelength of 360–400 nm might inhibit the progression of myopia by activating the secretion of retinal dopamine or regulating scleral fibroblasts, thereby inhibiting excessive axial elongation52. This might relate to the majority of windows glass block the violet light53, some children indoor seated near window could not exposure and get violet light enough.
This study provided some insights into the prevalence and risk factors of myopia and AL-related VI among children and adolescents. The high prevalence rates and strong association with age and parental myopia highlighted the need for targeted public health strategies, including promoting outdoor activities, optimizing learning environments, and strengthen beneficial eye behavior habits. Future research should explore longitudinal trends and the effectiveness of interventions to reduce the burden of VI in children and adolescents. This knowledge acquisition potentially facilitates self-regulated behavioral changes, such as maintaining optimal reading distance beyond 33 cm and complying with the 20-20-20 rule, which function as critical mediators buffering axial elongation progression. Notably, this cognitive-behavioral translation requires contextual reinforcement including parental supervision and school-based policy support, to achieve clinically significant protective effects42.
This study had two major strengths. First, we investigated the visual status of children and adolescents aged 4–18 years in a specific district of Beijing, covering a wide age range and providing intervention measures in children. The preschool-aged children were included, it would be useful to know how the younger children responded to the environmental change. Second, most previous studies used the equivalent spherical diopter to determine myopia, but the present study added AL-related VI to provide a more comprehensive and in-depth study.
This study had several limitations. First, the main limitation of the study was that a questionnaire survey was used to understand the influencing factors, and recall bias might be present as a result. Second, another limitation was that because this was a cross-sectional study in Beijing, the study design does not allow for causal inference or the determination of temporal sequences, which limits the interpretation of associations between risk factors and outcomes. Third, it must be noted that the 20-20-20 rule (visual break protocols) was based only on the subjective awareness rather than any objective behavioral measurements (complying with the 20-20-20 rule). Future studies should incorporate with electronic device monitoring (such as Clouclip) to quantify the actual implementation in future. Fourth, refractive error was assessed via non-cycloplegic autorefraction, which is a practical approach in large-scale studies, it might overestimate refractive error in younger children. Moreover, AL varies with age during ocular development. We will perform cycloplegic refraction and establish age-stratified AL criteria, which may result in more accurate results in future. Finally, our study was conducted in a certain district of Beijing and its generalizability was limited for other regions. We will perform multi-center, larger sample studies that were conducted by expanding the regional scope to further investigate and validate the conclusions.
Conclusion
This study highlights the high prevalence of myopia (56.53%) and AL-related VI (50.98%) among children and adolescents aged 4–18 years in Beijing, underscoring a significant public health concern. Key risk factors include older age, female sex, and parental myopia, with environmental influences such as prolonged near-work, inadequate lighting, and insufficient outdoor activity further exacerbating the burden. The findings call for targeted strategies, including early screening, promoting outdoor activities, optimizing learning environments, and sex-specific prevention programs. Future research should expand to multicenter, longitudinal studies to validate these findings and evaluate intervention efficacy in curbing myopia progression and AL-related VI.
Data availability
The data that support the findings of this study are available on request from the corresponding author upon reasonable request.
References
Yekta, A. et al. Global prevalence and causes of visual impairment and blindness in children: A systematic review and meta-analysis. J. Curr. Ophthalmol. 34(1), 1–15. https://doi.org/10.4103/joco.joco_135_21 (2022).
Kong, L., Fry, M., Al-Samarraie, M., Gilbert, C. & Steinkuller, P. G. An update on progress and the changing epidemiology of causes of childhood blindness worldwide. J. AAPOS. 16(6), 501–507. https://doi.org/10.1016/j.jaapos.2012.09.004 (2012).
Zou, M. et al. The burden, causes, and determinants of blindness and vision impairment in Asia: An analysis of the Global Burden of Disease Study. J. Glob. Health. 14, 04100. https://doi.org/10.7189/jogh.14.04100 (2024).
Flitcroft, D. I. et al. IMI—defining and classifying myopia: A proposed set of standards for clinical and epidemiologic studies. Invest. Ophthalmol. Vis. Sci. 60(3), M20–M30. https://doi.org/10.1167/iovs.18-25957 (2019).
WHO launches first World report on vision. https:/www.who.int/zh/news-room/detail/08-10-2019-who-launches-first-world-report-on-vision. Accessed 2019-10-11 (2019).
Tang, T. et al. A machine learning-based algorithm used to estimate the physiological elongation of ocular axial length in myopic children. Eye Vis. (Lond). 7, 50. https://doi.org/10.1186/s40662-020-00214-2 (2020).
The state council of the PRC. The National Center for Disease Control and Prevention actively promotes the prevention and control of myopia in children and adolescents, and the rate of myopia is showing a downward trend. https://www.gov.cn/lianbo/bumen/202403/content_6939270.htm. Accessed 2023-03-13 (2024).
Yan, X. et al. Research progress of fundus morphology in high myopia. Int. Eye Sci. 23(2), 212–216. https://doi.org/10.3980/j.issn.1672-5123.2023.2.06 (2023).
Tideman, J. W. L. et al. Axial length growth and the risk of developing myopia in European children. Acta. Ophthalmol. 96(3), 301–309. https://doi.org/10.1111/aos.13603 (2017).
Erratum in: IMI—defining and classifying myopia: A proposed set of standards for clinical and epidemiologic studies. Invest. Ophthalmol. Vis. Sci. 65(13), 19 (2024). https://doi.org/10.1167/iovs.65.13.19
National Health Commission of the PRC. Notice from the General Office of the National Health Commission on Issuing Guidelines for prevention and control of myopia in children and adolescents (2024 version). Accessed 2024-05-31. http://www.nhc.gov.cn/yzygj/s7653/202405/b6edbd0bf3a64ecc8cef30d72f80ed9e.shtml.
Wang, H. et al. Effect of school entrance age on myopia among primary schoolchildren using mixed-effect model: The Shantou Myopia Study (SMS). Asia Pac. J. Ophthalmol. (Phila). 13(6), 100121. https://doi.org/10.1016/j.apjo.2024.100121 (2024).
Li, S. M. et al. Corneal power, anterior segment length and lens power in 14-year-old Chinese children: The Anyang Childhood Eye Study. Sci. Rep. 6, 20243. https://doi.org/10.1038/srep20243 (2016).
He, X. et al. Normative data and percentile curves for axial length and axial length/corneal curvature in Chinese children and adolescents aged 4–18 years. Br. J. Ophthalmol. https://doi.org/10.1136/bjophthalmol-2021-319431 (2021).
Zhang, D. et al. Prevalence and associated factors of myopia among school students in Shenyang, China: A cross-sectional study. Front. Publ. Health. 11, 1239158. https://doi.org/10.3389/fpubh.2023.1239158 (2023).
Huang, Z., Song, D., Tian, Z., Wang, Y. & Tian, K. Prevalence and associated factors of myopia among adolescents aged 12–15 in Shandong Province, China: A cross-sectional study. Sci. Rep. 14(1), 17289. https://doi.org/10.1038/s41598-024-68076-5 (2024).
Arnoldi, K. Growing pains: The incidence and prevalence of Myopia from 1950 to 2050. J. Binocul. Vis. Ocul. Motil. 74(4), 118–121. https://doi.org/10.1080/2576117X.2024.2387379 (2024).
Guo, Z. et al. Analysis of influencing factors of screened myopia in primary school students in seven provinces. Chin. J. Sch. Health 41(12), 1872–1875. https://doi.org/10.16835/j.cnki.1000-9817.2020.12.027 (2020).
Wolffsohn, J. S. et al. IMI—clinical myopia control trials and instrumentation report. Invest. Ophthalmol. Vis. Sci. 60(3), M132–M160. https://doi.org/10.1167/iovs.18-25955 (2019).
Yahalom, C. et al. Childhood visual impairment and blindness: 5-year data from a tertiary low vision center in Israel. Eye (Lond). 36(10), 2052–2056. https://doi.org/10.1038/s41433-021-01743-3 (2022).
Anley, D. T. et al. Prevalence of visual impairment and associated factors among children in Ethiopia: Systematic review and meta-analysis. PLoS One. 17(7), e0271433. https://doi.org/10.1371/journal.pone.0271433 (2022).
Tideman, J. W. et al. Association of axial length with risk of uncorrectable visual impairment for Europeans with myopia. JAMA Ophthalmol. 134(12), 1355–1363. https://doi.org/10.1001/jamaophthalmol.2016.4009 (2016).
Liu, J. et al. Baseline characteristics analysis of the Beijing children and adolescents natural population cohort. Chinese J. Child Health Care 32(11), 1212–1231 (2024).
Xiang, K. D. et al. Refractive progression among students aged 4–14 in Shanghai and associated factors. Chin. J. Sch. Health. 43(9), 1309–1318. https://doi.org/10.16835/j.cnki.1000-9817.2022.09.008 (2022).
National Health Commission of the PRC. Appropriate technical guide-lines for prevention and control of myopia in children and adolescents (updated version) and interpretation. http://www.gov.cn/xinwen/2021-10/13/content_5642345.htm. Accessed 2022-03-02.
Arnold, R. W. et al. AAPOS uniform guidelines for instrument-based pediatric vision screen validation 2021. J. AAPOS. 26(1), 1.e1-1.e6. https://doi.org/10.1016/j.jaapos.2021.09.009 (2022).
Gu, F. et al. Effect of cycloplegia on refractive error measure in Chinese school students. Ophthalmic Epidemiol. 29(6), 629–639. https://doi.org/10.1080/09286586.2021.1999986 (2022).
Public Health Ophthalmology Branch of Chinese Preventive Medicine Association. Chinese expert consensus on the reference interval of ocular hyperopia reserve, axial length, corneal curvature and genetic factors in school-age children. Chinese J. Ophthalmol. 58(2):96–102 (2022).
Sen S, Tripathy K. Ultrasound biometry. In StatPearls. (StatPearls Publishing, Treasure Island (FL), 2024).
Wang, J., Li, S., He, S., Feng, Y. & Li, P. Regional disparities in the prevalence and correlated factors of myopia in children and adolescents in Gansu, China. Front. Med. (Lausanne). 11, 1375080. https://doi.org/10.3389/fmed.2024.1375080 (2024).
Shi, J. J. et al. Effects of school myopia management measures on myopia onset and progression among Chinese primary school students. BMC Publ. Health. 23(1), 1819. https://doi.org/10.1186/s12889-023-16719-z (2023).
Zhao, E. et al. Ocular biometrics and uncorrected visual acuity for detecting myopia in Chinese school students. Sci. Rep. 12(1), 18644. https://doi.org/10.1038/s41598-022-23409-0 (2022).
Aljaberi, H. A., Ali, I. R. & Noori, Z. T. M. Prevalence of refractive errors among school students in Iraq—a systematic review and meta-analysis. J. Optom. 18(1), 100534. https://doi.org/10.1016/j.optom.2024.100534 (2025).
Wang, J. et al. Normative value of hyperopia reserve and myopic shift in Chinese children and adolescents aged 3–16 years. Br. J. Ophthalmol. 108(7), 1024–1029. https://doi.org/10.1136/bjo-2023-323468 (2024).
Chen, J. et al. Smartwatch measures of outdoor exposure and myopia in children. JAMA Netw. Open. 7(8), e2424595. https://doi.org/10.1001/jamanetworkopen.2024.24595 (2024).
Bro, T. & Ludvigsson, J. Time spent outdoors in childhood related to myopia among young adults in the Swedish ABIS cohort. Acta. Ophthalmol. 103(2), 171–176. https://doi.org/10.1111/aos.16688 (2025).
Yip, V. C. et al. The relationship between growth spurts and myopia in Singapore children. Invest. Ophthalmol. Vis. Sci. 53(13), 7961–7966. https://doi.org/10.1167/iovs.12-10402 (2012).
Wang, J. et al. Puberty could regulate the effects of outdoor time on refractive development in Chinese children and adolescents. Br. J. Ophthalmol. 105(2), 191–197. https://doi.org/10.1136/bjophthalmol-2019-315636 (2021).
Yang, X. W. & Zhang, S. B. Current advance in the research of related influencing factors of myopia. Int. Eye Sci. 17(10), 1871–1873 (2017).
Yang, G. Y. et al. Associations between screen exposure in early life and myopia amongst Chinese preschoolers. Int .J. Environ. Res. Publ. Health. 17(3), 1056. https://doi.org/10.3390/ijerph17031056 (2020).
Ye, C. et al. Comparison of myopia-related behaviors among Chinese school-aged children and associations with parental awareness of myopia control: A population-based, cross-sectional study. Front. Publ. Health. 13, 1520977. https://doi.org/10.3389/fpubh.2025.1520977 (2025).
Pärssinen, O., Lassila, E. & Kauppinen, M. Associations of children’s close reading distance and time spent indoors with myopia, based on parental questionnaire. Children (Basel). 9(5), 632. https://doi.org/10.3390/children9050632 (2022).
Talens-Estarelles, C. et al. The effects of breaks on digital eye strain, dry eye and binocular vision: Testing the 20-20-20 rule. Cont. Lens. Anterior Eye. 46(2), 101744. https://doi.org/10.1016/j.clae.2022.101744 (2023).
Liu, Q. et al. A survey of public eye-care behavior and myopia education. Front. Publ. Health. 13, 1518956. https://doi.org/10.3389/fpubh.2025.1518956 (2025).
Harb, E., Thorn, F. & Troilo, D. Characteristics of accommodative behavior during sustained reading in emmetropes and myopes. Vis. Res. 46(16), 2581–2592. https://doi.org/10.1016/j.visres.2006.02.006 (2006).
Lanca, C. & Saw, S. M. The association between digital screen time and myopia: A systematic review. Ophthalmic Physiol. Opt. 40(2), 216–229 (2020).
Ha, A., Lee, Y. J., Lee, M., Shim, S. R. & Kim, Y. K. Digital screen time and myopia: A systematic review and dose-response meta-analysis. JAMA Netw. Open. 8(2), e2460026. https://doi.org/10.1001/jamanetworkopen.2024.60026 (2025).
Li, S. M. et al. Near work related parameters and myopia in Chinese children: The anyang childhood eye study. PLoS ONE 10(8), e0134514. https://doi.org/10.1371/journal.pone.0134514 (2015).
Cai, H. M. et al. Effect of artificial natural light on the development of myopia among primary school-age children in China: A three-year longitudinal study. Int. J. Ophthalmol. 17(5), 924–931. https://doi.org/10.18240/ijo.2024.05.18 (2024).
Tang, J. et al. Effects of 2 Hz flickering light on refractive state, fundus imaging and visual function of C57BL/6 mice. Exp. Eye Res. 246, 110014. https://doi.org/10.1016/j.exer.2024.110014 (2024).
Zhou, P. F., Tao, F. B. & Wu, X. Y. Light exposure and myopia in children and adolescents. Chin. J. Sch. Health 43(3), 467–471. https://doi.org/10.16835/j.cnki.1000-9817.2022.03.036 (2022).
Torii, H. et al. Violet light exposure can be a preventive strategy against myopia progression. EBioMedicine 15, 210–219. https://doi.org/10.1016/j.ebiom.2016.12.007 (2017).
Ullah, S., Umer, M. F. & Chandran, S. P. Violet light transmission through eyeglasses and its effects on myopic children: A systematic review and meta-analysis. Saudi J. Ophthalmol. 38(3), 235–242. https://doi.org/10.4103/sjopt.sjopt_146_24 (2024).
Acknowledgements
We would like to thank all the parents, children and data collectors who participated in this study. We also would like to thank the following individuals for their contribution and all of the medical workers and teachers involved in the study, for their enthusiasm, hard work and enduring support.
Funding
This project was supported by Public service development and reform pilot project of Beijing Medical Research Institute (BMR2021-3). The funding body had no role in the design, analysis or writing of this article.
Author information
Authors and Affiliations
Contributions
MC and ZH had full access to all the data, formulated the research question and made a design for the study; ZY, SL, JL, FC, XZ collected the data; MC have made substantial contributions to the interpretation and statistical analysis of the data; MC and ZH participated in the discussion and drafted the manuscript; TY and YG participated in the discussion. MC and ZH have made substantial contributions to the interpretation of data and substantively revised the manuscript. All authors have approved the submitted the final version and have agreed both to be personally accountable for the author’s own contributions and for ensuring that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, were appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The research was performed in accordance with the Declaration of Helsinki. This study was approved by the Ethics Committee of Capital Institute of Pediatrics under the code (NO.SHERLL2022043). Informed consent was obtained from children’s parents or guardians.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mingming, C., Zhou, Y., Shaoli, L. et al. Prevalence and associated factors of myopia and axial length-related visual impairment in children and adolescents aged 4–18 years. Sci Rep 15, 35277 (2025). https://doi.org/10.1038/s41598-025-18400-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-18400-4