Abstract
Subarachnoid hemorrhage (SAH) is a rare but serious stroke subtype that accounts for approximately 5% of all strokes. This study analyzed SAH epidemiology in Asia from 1990 to 2021 using the Global Burden of Disease (GBD) 2021 data. This study assessed the burden of SAH in Asia using four indicators: incidence, prevalence, mortality, and disability-adjusted life years (DALYs). An autoregressive integrated moving average (ARIMA) model was used to conduct a long-term trend analysis and forecast the changing trends of various indicators from 2022 to 2041. Between 1990 and 2021, the age-standardized incidence rates (ASIR) of SAH in Asia increased and then decreased, while the age-standardized prevalence rates (ASPR), age-standardized mortality rates (ASMR), and age-standardized disability-adjusted life years rates (ASDR) of SAH continued to decline. The Arima model predictions suggest that Asian age-standardized rates will typically show a decreasing trend over the next 20 years, except for the ASIR, which shows an increasing trend. Over the next 20 years, the ASIR of SAH in Asia is expected to increase. The ASPR, ASMR, and ASDR were expected to show decreasing trends. The burden of SAH in older patients remains high, highlighting the need to strengthen the health management of the older population.
Similar content being viewed by others
Introduction
Subarachnoid hemorrhage (SAH) is defined as bleeding in the subarachnoid space between the arachnoid and pia mater. It accounts for only 5% of all stroke cases and occurs at a relatively young age1. Despite its low incidence, when it does occur, the consequences can be extremely severe, resulting in very high rates of disability and mortality2. The most common clinical manifestation of spontaneous SAH is sudden onset of unexpected and intense headaches3. Survivors often have cognitive impairments. This significantly impacts their ability to engage in daily activities and social interactions, leading to a substantial decline in their quality of life. Many patients remain unable to resume their normal work and lifestyle even after receiving treatment. One study suggested that smoking and hypertension may influence the incidence of SAH4. These risk factors are prevalent in the population and, if left unchecked and unaddressed, will increase the risk of SAH for more individuals. SAH imposes an additional financial burden on the Health system, affecting the 50−60-year-old population, and leading to longer hospital stays5. This financial burden may divert medical resources away from other diseases, negatively impacting the operational efficiency of the entire healthcare system. This, in turn, has a cascading effect on the overall healthy development of society. In summary, SAH, a type of stroke associated with high rates of disability and mortality, presents a significant public health challenge due to its clinical manifestations, the influence of risk factors, and its economic burden. It is imperative that this issue receives widespread attention and focus from all sectors of the community, and that effective preventive and therapeutic measures are implemented to address this complex problem.
Existing studies have focused on the global burden of stroke6,7; however, the burden of SAH has not been adequately studied. This study utilized the latest Global Burden of Disease (GBD) database to assess the burden of SAH in Asia, with a focus on comprehensive regional-level analyses. It analyzes the incidence, prevalence, mortality, and disability-adjusted life years (DALYs) of SAH in Asia from 1990 to 2021, aiming to enhance understanding of its epidemiology and support authorities in identifying gaps in prevention, management, and intervention programs.
Methods
GBD began 30 years ago to provide timely, valid, and relevant assessments of key health outcomes. For continuous quality improvement, each annual GBD study re-estimates the entire time series by including all known advances in data, modelling, estimation methods, and health literacy, thereby ensuring that each GBD contains the most up-to-date estimates8.
The GBD 2021 indicators include estimates and their 95% uncertainty intervals (UI). According to the GBD algorithm, defined by the 25th and 975th ordered values of 1000 draws of the posterior distribution, all ratios were reported for every 100,000 persons9. UIs account for not only the variance in parameter estimation but also the uncertainty from data collection, model selection, and other sources of uncertainty under the parameter estimation process8.
We used the most recent data from the Global Health Data Exchange (https://vizhub.healthdat.sgbd-results/). Four Asian regions were extracted for the analysis of the burden of SAH: East Asia, South Asia, Southeast Asia, and Central Asia. In addition, we analyzed the burden of SAH in the high-income Asian Pacific.
DALYs represent the sum of years lived with disability (YLD) and years of life lost (YLL). ASPR were used to assess temporal trends in prevalence over the study period.
The autoregressive integrated moving average (ARIMA) (p, d, q) model was applied to forecast trends in the four age-standardized indicators of SAH in Asia from 2022 to 2041. The letters p, d, and q represent the order of autoregression, the degree of difference, and the order of moving average10. The best ARIMA (p, d, q) models were selected using the Akaike information criterion (AIC) and Bayesian information criterion (BIC) to predict SAH disease burden. The Ljung–Box Q test was used to determine whether the residuals of the selected models satisfied an independent normal distribution11.
This study used the R statistical program (version 4.2.2) for graphical analysis.
Results
Burden and Temporal trends of SAH in Asia
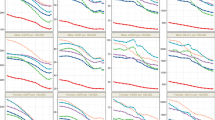
Table 1 shows the numbers and age-standardized rates of the four SAH indicators in Asia. As shown in Table 1; Fig. 1, the age-standardized incidence rate (ASIR), age-standardized prevalence rates (ASPR), age-standardized mortality rates (ASMR), and age-standardized disability-adjusted life years rate (ASDR) of SAH in Asia declined from 1990 to 2021 by 38.85%, 20.67%, 68.84%, and 64.87%, respectively. In Asia, the ASIR of SAH initially increased, then decreased, and eventually leveled off. The ASPR of SAH showed a flat and decreasing trend, while the ASMR and ASDR of SAH generally showed a sharp decline followed by a more gradual decrease. The ASMR and ASDR of SAH in Asia began to decline at an accelerated rate in 1995, indicating that disease management for SAH likely improved during that year.
In 2021, among the four regions of Asia, Southeast Asia had the highest ASIR, ASPR, ASMR, and ASDR of SAH in all four regions. East Asia had the lowest ASIR, ASPR, and ASDR of SAH, while South Asia had the lowest ASMR of SAH. The high-income Asia-Pacific region had a high ASIR and ASPR for SAH, and a low ASMR for SAH in 2021.
Trends of ASIR, ASPR, ASMR, and ASDR of SAH in Asia, Central Asia, East Asia, South Asia, Southeast Asia, and High-income Asia Pacific from 1990 to 2021. DALY: Disability-adjusted life year; ASIR: Age-standardized incidence rates; ASPR: Age-standardized prevalence rates; ASDR: Age-standardized DALY rates; ASMR: Age-standardized mortality rates.
Population distribution of SAH in Asia
Figure 2 shows that in 2021, the rates of SAH incidence in Asian women and men are generally similar, with Asian women having overall higher rates of SAH than men, and Asian women having slightly lower SAH mortality rates than men.
Overall, the incidence, prevalence, and mortality rates of SAH in Asia increased with age. For both men and women, the highest incidence and prevalence rates due to SAH are 95 years and over. The mortality rate occurs at ages 90–94 years for men and 95 years and over for women.
Regional distribution of SAH in Asia
Table 2 shows that among the four regions in Asia, Southeast Asia had the highest ASPR of 110.62 per 100,000 population (95% UI 101.73, 120.43), while East Asia had the lowest ASPR of 70.06 per 100,000 population (95% UI 62.78, 77.98). In the High-income Asia Pacific region, the ASPR is high, at 193.60 per 100,000 population (95% UI 175.43, 212.12).
Figure 3 shows the distribution of SAH in Asia in 2021. Table 2; Fig. 3 show that the Republic of Azerbaijan had the lowest age-standardized prevalence rate of 67.09 per 100,000 people (95% UI 61.95, 72.60), while the Solomon Islands had the highest age-standardized prevalence rate of 227.03 per 100,000 people (95% UI 213.74, 240.19).
To better describe the temporal trends in SAH prevalence in Asia, four more typical countries were selected for further analysis. Both China and India are populous developing countries. In contrast, Pakistan, though also a developing country, has a smaller population. Japan, however, is a developed Asian nation with a relatively small population. We consider these four countries to be representative examples. Figure 4 shows that between 1990 and 2021, the prevalence of SAH showed an increasing trend in all four countries. In China, the ASPR showed a decreasing trend, whereas in Japan, it showed a slow increasing trend. On the other hand, in India and Pakistan, the trend in ASPR has fluctuated slightly but has generally shown a slow decreasing trend. In China and Japan, the ASPR and number of SAH cases are higher in women than in men, whereas in India, the opposite trend is observed. In Pakistan, the ASPR of SAH in males is not significantly different from that in females, and the number of cases in males is slightly higher than that in females.
The Arima model predicts four age-standardized rates of SAH in Asia
This study used the ARIMA model to predict the trends in the ASIR, ASPR, ASMR, and ASDR of SAH in Asia over the next 20 years. The optimal model parameters, along with their corresponding AIC, BIC, and Ljung–Box test p-values, are presented in Table 3. The Ljung-Box test showed that the p-values were all greater than 0.05, indicating that the original hypothesis could not be rejected and that all models exhibited white noise residuals, indicating stability and a good fit to the data. Figure 5 presents the anticipated ASIR, ASPR, ASMR, and ASDR per 100,000 individuals for the period spanning from 2022 to 2041.
As illustrated in Fig. 5, from 2022 to 2041, the ASPR, ASMR, and ASDR of SAH in Asia showed a decreasing trend, while the ASIR showed an increasing trend. By 2041, the projected age-standardized rates are as follows: incidence, 10.51 per 100,000; prevalence, 86.97 per 100,000; deaths, 3.24 per 100,000; DALYs, 92.38 per 100,000.
Attributable risk factors for SAH dalys in 2021
In this study, an attributable risk analysis was conducted to evaluate the impact of 11 risk factors, including high systolic blood pressure, on SAH. As shown in the Fig. 6, high systolic blood pressure was the primary attributable risk factor in Asia and its various regions, accounting for over 50% of the total DALYs. The contributions of different risk factors varied across regions in Asia. In Asia, including Central Asia, East Asia, high-income Asia Pacific, and Southeast Asia, ambient particulate matter pollution and smoking are significant risk factors. And in South Asia, DALYs of SAH were more attributable to household air pollution from solid fuels (23.44%), ambient particulate matter pollution (15.88%), and diet low in fruits (15.58%), compared to other risk factors.
Discussion
This study provides the first comprehensive analysis of the burden of SAH in Asia and applies the ARIMA model to forecast changes in the age-standardized rates of SAH.
The results indicate that between 1990 and 2021, the ASPR, ASMR, and ASDR of SAH in Asia decreased, and the ASIR of SAH in Asia first increased and then decreased, suggesting a reduction in the burden of SAH in Asia. This declining incidence trend is consistent with the findings of a previous systematic review and meta-analysis4. It is possible that this change was due to the improved management of hypertension and cessation of smoking. The global incidence of SAH has been shown to decrease by 7.1% for every 1 mmHg reduction in systolic blood pressure, 11.5% for every 1 mmHg reduction in diastolic blood pressure, and 2.4% for every 1% reduction in smoking prevalence4. Feigin et al. also showed that smoking and systolic blood pressure are the most important risk factors for SAH in the Asia-Pacific region12. Attributable risk analyses also showed that high systolic blood pressure was the primary attributable risk factor in Asia and its various regions. The decreased mortality is most likely due to advances in follow-up and treatment in recent years13. Although the ASIR, ASPR, ASMR, and ASDR for SAH in Asia have generally declined, the burden of public health expenditures associated with SAH remains significant. During the acute phase of SAH, patients require both diagnostic assessments and urgent treatment, which can be expensive. A significant proportion of SAH patients necessitate long-term rehabilitation following the acute phase, further increasing the burden on public health resources. The death and disability resulting from SAH deprive many families of their primary source of income, while imposing a heavy economic burden on society. This situation adversely affects productivity and overall societal development.
Among the four Asian regions, Southeast Asia had the highest ASIR, ASPR, ASMR, and ASDR values for SAH. In the high-income Asia Pacific, ASIR and ASPR are higher, and ASMR is lower compared to other regions in Asia. This may be attributed to the more adequate healthcare resources available in high-income Asia Pacific regions, including advanced neuroimaging equipment, specialized neurosurgeons, and neurointensive care units. While these advancements have contributed to reduced mortality rates, the burden of SAH remains significant as the population continues to age.
In 2021, the ASIR for SAH in Asian men and women was essentially similar, with the ASPR for men being smaller than that for women and the ASMR slightly larger than that for women. Women are thought to be at greater risk of developing spontaneous SAH than men1. A systematic review and meta-analysis suggested that this sex difference was associated with estrogen deficiency and postmenopausal collagen depletion in women, especially after the age of 5014. However, some studies have reported that the incidence of SAH is higher in men than in women15. This finding suggests that the disease burden of SAH in Asia is influenced by factors other than sex.
In Asia, the ASIR, ASPR, and ASMR of SAH increased with age, and the burden of SAH was concentrated in older age groups. Population aging is accelerating and has become a major global challenge, and its burden is expected to increase further16. This suggests that in the course of social development, more attention should be paid to the health status of the older patients and that health-care services should prioritize their needs.
Countries such as China and India have fairly large populations, leading to a high prevalence of SAH. China has the highest prevalence rate in Asia. China has long been a populous country. In 2019, China had 18% of the world’s population, with 164.5 million Chinese citizens aged 65 years and over, and 26 million aged 80 years or over17. There are significant regional differences in the burden of cardiovascular and cerebrovascular diseases with respect to national demographics and the varying levels of population aging in Asia18. China, India, Japan, and Pakistan showed an increasing trend in the prevalence of SAH from 1990 to 2021. In China, the ASPR showed a decreasing trend; in Japan, it showed an increasing trend, whereas in India and Pakistan, the ASPR showed little change. In China and Japan, the burden of SAH is greater in women than in men; in India, it is greater in men than in women; and in Pakistan, there is little difference in the burden of the disease between men and women. Differences in the burden of SAH among these countries are complex and influenced by many factors, including the environment, lifestyle, racial and ethnic differences, level of medical care, and socioeconomic development.
The ARIMA model projections for the next 20 years in Asia showed that while ASPR, ASMR, and ASDR will continue to decline, ASIR is expected to increase. This suggests that we need to be concerned about the incidence of SAH in Asia and proactively adopt preventive strategies to reduce the future burden of this disease.
This study was limited by inherent limitations associated with the global burden of disease research, including the quality and accessibility of raw data. Problems with the GBD persist, such as poor data quality and incomplete coverage of certain regions or countries. The lack of stroke and SAH registries in certain underdeveloped countries may result in an underestimation of data, leading to inaccuracies. The predictions of the ARIMA model may not consider the complexity of real-world scenarios, thus limiting predictive accuracy, especially in the case of unforeseen future crises or sudden shifts. Future research could attempt to develop new forecasting models to improve accuracy.
Conclusion
This study analyzed the burden of SAH in Asia from 1990 to 2021 and forecasted potential trends for the period of 2022–2041. Currently, the disease burden of SAH in Asia remains high and poses a major threat to public health and economic development. There is a need to develop targeted policies and allocate health resources for the active prevention and treatment of SAH to reduce the burden of disease and mitigate the impact of SAH on countries, societies, and individuals.
Data availability
The datasets supporting the conclusions of this article are available in the Global Health Data Exchange (GHDx) query tool (https://ghdx.healthdata.org/gbd-2021).
Abbreviations
- SAH:
-
Subarachnoid hemorrhage
- GBD:
-
Global Burden of Disease
- DALYs:
-
Disability-adjusted life years
- YLD:
-
Years lived with disability
- YLL:
-
Years of life lost
- ASPR:
-
Age-standardized prevalence rates
- ARIMA:
-
Autoregressive integrated moving average
- ASIR:
-
Age-standardized incidence rates
- ASMR:
-
Age-standardized mortality rates
- ASDR:
-
Age-standardized disability-adjusted life years rate
References
Van Gijn, J., Kerr, R. S. & Rinkel, G. J. Subarachnoid haemorrhage. Lancet 369 https://doi.org/10.1016/S0140-6736(07)60153-6 (2007). 306 – 18.
Claassen, J. & Park, S. Spontaneous subarachnoid haemorrhage. Lancet 400, 846–862. https://doi.org/10.1016/S0140-6736(22)00938-2 (2022).
Perry, J. J. et al. Clinical decision rules to rule out subarachnoid hemorrhage for acute headache. JAMA 310, 1248–1255. https://doi.org/10.1001/jama.2013.278018 (2013).
Etminan, N. et al. Worldwide incidence of aneurysmal subarachnoid hemorrhage according to region, time period, blood pressure, and smoking prevalence in the population: A systematic review and Meta-analysis. JAMA Neurol. 76, 588–597. https://doi.org/10.1001/jamaneurol.2019.0006 (2019).
Hammer, A. et al. Impact of complications and comorbidities on the intensive care length of stay after aneurysmal subarachnoid haemorrhage. Sci. Rep. 10 https://doi.org/10.1038/s41598-020-63298-9 (2020).
He, Q. et al. Global, regional, and National burden of stroke, 1990–2021: A systematic analysis for global burden of disease 2021. Stroke 55, 2815–2824. https://doi.org/10.1161/STROKEAHA.124.048033 (2024).
GBD 2021 Stroke Risk Factor Collaborators. Global, regional, and National burden of stroke and its risk factors, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet Neurol. 23, 973–1003. https://doi.org/10.1016/S1474-4422(24)00369-7 (2024).
Golabi, P. et al. Burden of non-alcoholic fatty liver disease in asia, the middle East and North africa: data from global burden of disease 2009–2019. J. Hepatol. 75, 795–809. https://doi.org/10.1016/j.jhep.2021.05.022 (2021).
Rong, J., Cheng, P., Li, D., Wang, X. & Zhao, D. Global, regional, and National Temporal trends in prevalence for depressive disorders in older adults, 1990–2019: an age-period-cohort analysis based on the global burden of disease study 2019. Ageing Res. Rev. 100, 102443. https://doi.org/10.1016/j.arr.2024.102443 (2024).
Wei, J. et al. Time trends in the incidence of spinal pain in china, 1990 to 2019 and its prediction to 2030: the global burden of disease study 2019. Pain Ther. 11, 1245–1266. https://doi.org/10.1007/s40122-022-00422-9 (2022).
Wu, Y. et al. Disease burden and attributable risk factors of neonatal disorders and their specific causes in China from 1990 to 2019 and its prediction to 2024. BMC Public. Health. 23, 122. https://doi.org/10.1186/s12889-023-15050-x (2023).
Feigin, V. et al. Smoking and elevated blood pressure are the most important risk factors for subarachnoid hemorrhage in the Asia-Pacific region: an overview of 26 cohorts involving 306,620 participants. Stroke 36 (5), 1360. https://doi.org/10.1161/01.STR.0000170710.95689.41 (2005).
Cetinkaya, O. et al. Factors influencing the mortality of patients with subarachnoid haemorrhage in the intensive care unit: A retrospective cohort study. J. Clin. Med. 14, 1650. https://doi.org/10.3390/jcm14051650 (2025).
Vlak, M. H., Algra, A., Brandenburg, R. & Rinkel, G. J. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: A systematic review and meta-analysis. Lancet Neurol. 10, 626–636. https://doi.org/10.1016/S1474-4422(11)70109-0 (2011).
Harrison, C. H., Taquet, M., Harrison, P. J., Watkinson, P. J. & Rowland, M. J. Sex and age effects on risk of non-traumatic subarachnoid hemorrhage: retrospective cohort study of 124,234 cases using electronic health records. J. Stroke Cerebrovasc. Dis. 32, 107196. https://doi.org/10.1016/j.jstrokecerebrovasdis.2023.107196 (2023).
Beard, J. R. et al. The world report on ageing and health: a policy framework for healthy ageing. Lancet 387, 2145–2154. https://doi.org/10.1016/S0140-6736(15)00516-4 (2016).
Fang, E. F. et al. A research agenda for ageing in China in the 21st century (2nd edition): Focusing on basic and translational research, long-term care, policy and social networks. Ageing Res Rev. 64, 101174; (2020). https://doi.org/10.1016/j.arr.2020.101174
Zhang, X. et al. Analysis of ischemic stroke burden in Asia from 1990 to 2019: based on the global burden of disease 2019 data. Front. Neurol. 14, 1309931. https://doi.org/10.3389/fneur.2023.1309931 (2023).
Acknowledgements
The authors express their gratitude to the Institute for Health Metrics and Evaluation for sharing valuable GBD data.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by grants from the Natural Science Foundation of Heilongjiang Province (LH2022H081).
Author information
Authors and Affiliations
Contributions
LYT: Writing – original draft. WMM: Writing – review & editing. ZLW: Writing – review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, Y., Wu, M. & Zhu, L. Burden of subarachnoid hemorrhage in Asia and ARIMA model prediction trends from 1990 to 2021. Sci Rep 15, 33407 (2025). https://doi.org/10.1038/s41598-025-18756-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-18756-7