Abstract
Injury and violence is a global public health concern, implicated in 4.4 million deaths annually. The most common cause of preventable death is haemorrhage in the out-of-hospital setting. Haemorrhagic shock patients are at risk of disseminated intravascular coagulation, global myocardial ischemia, and death. This risk is heightened among the young, older adults, or polytraumatised. The definitive standard of care is to stop the bleeding and to replace the lost haemoglobin whilst supplementing oxygen. There is paucity in emergency blood transfusion research in the out-of-hospital setting. It is not out-of-hospital standardised practice. This novel research conducted in Western Cape, South Africa, determined the viability of blood in transit by evaluating haemolysis and oxidative stress in Packed Red Blood Cells (PRBC) on public ambulances. A relatively new statistical method (generalised additive model with smooth term) was used to model non-linearity in the haemolysis trend. In a designed experiment, the viability of blood was determined by placing PRBC in temperature-controlled refrigerators at ambulance bases (maintained at 1–6 °C) as a ‘Control’. The ‘Treatment’ PRBC were transported in cooler-boxes with 2 eutectics (icepacks). The cold-chain was monitored against the recommended transportation temperature range of 1–10˚C. The PRBC was assessed weekly for haemolysis and at the end of the study for lipid peroxidation, both threats to PRBC viability following environmental exposure (to transit temperatures and movement). The PRBC placed on ambulances indicated that they were < 0.8% haemolysis threshold after day 35. Three packs in the treatment group were > 0.8% on day 42, along with one in the control group (which was deemed an outlier). Transported PRBC remained between 1–10˚C for the most part. Conjugated dienes and thiobarbituric acid reactive substances showed no statistically significant changes and aligned with colorimetric assessment. The blood viability on ambulances remained within the acceptable ≤ 0.8% haemolysis level until the PRBC expiry, on day 42. PRBC remained within the transportation temperature reference range for South Africa and no significant oxidative stress or cellular degradation was documented. This evidence supports PRBC viability when transported in ambulances conditional to the use of eutectics in closed cooler boxes and has relevance in low- and middle-income countries or in humanitarian contexts.
Similar content being viewed by others
Introduction
According to the World Health Organisation (WHO) injury from violence is said to be one of the most prominent public health concerns globally, where injuries account for approximately 4.4 million deaths annually1. The most common cause of potentially preventable death is pre-hospital haemorrhage, associated with traumatic injury2,3. Recent studies suggest that early administration of Packed Red Blood Cells (PRBC) has been documented to reduce mortality in haemorrhaging patients4.
Cape Town is known as ‘stab capital of South Africa’5, with a township in Cape Town, Nyanga, referred to as the ‘murder capital of South Africa’6. With a high burden of penetrating trauma in Cape Town, patients are at high risk of experiencing exsanguinating haemorrhage, whether it is en-route to the emergency department or on scene. Most commonly, patients succumb to traumatic injuries due to haemorrhage and the most effective way to ‘save some time’ and prevent anaemic hypoxia is by replacing lost blood7. Therefore, a need to bridge a time-critical gap of a life-threatening insult and probable mortality is required, in such de facto high conflict areas. This study has aimed to address certain environmental/contextual factors to enable an out-of-hospital early blood transfusion system. This study would be the first to our knowledge to investigate the feasibility of blood transport using ambulances in a lower- and middle-income country setting, such as South Africa. There is currently a paucity in South African research regarding the viability of blood in this environment.
Methods
To achieve this aim, it was fundamental to first ascertain if blood, as a scarce resource, would remain viable on (un-airconditioned) ambulance vehicles during protracted periods and in real-world settings, and if transported in the most cost-effective way by using cooler-boxes, ice packs and temperature loggers. The blood was tested weekly for percentage plasma haemolysis, and for lipid peroxidation at the end of the study, as lipid peroxidation is a marker for cell degradation and would be increased if haemolysis has occurred8. Viability was determined by transporting PRBC in ambulance vehicles and comparing them to controls stored in refrigerators at selected ambulance bases. This is particularly important in early blood transfusion interventions in the pre-hospital setting or if there is a need to cost-effectively transport blood through the existing infrastructure of an ambulance system.
The research hypotheses to be tested in the study were as follows:
H1.1 The blood packs transported on ambulances in cooler boxes (Treatment group) would undergo haemolysis at a faster rate than the blood packs stored in refrigerators at ambulance bases (Control group).
H1.2 However, the haemolysis level of blood packs handled in the manner of the Treatment group would be projected to remain below the 0.8% threshold for at least two weeks. Using an experimental design, this study consisted of what we called a ‘blood-run’ which was to determine the viability of transported blood in the out-of-hospital setting. According to the clinical guidelines for the use of blood and blood products in South Africa, the clinical use of whole blood is limited, with packed red blood cells (PRBCs) being favoured in most situations requiring an increase in oxygen-carrying capacity9. Whole blood has a shorter shelf-life of 21 days compared to the 42-day expiry of PRBCs, and many of its clotting factors deteriorate within hours of donation. The Trauma Society of South Africa’s Massive Transfusion/Massive Haemorrhage Protocol advocates for two initial units of PRBCs before activating the full/massive transfusion protocol, which relies on component therapy rather than whole blood10. Considering PRBCs are the most used blood product in trauma centres in South Africa, they were selected for this study.
The PRBC were transported on ambulance vehicles (as the ‘treatment’ arm), without being used in transfusions. Blood was randomly distributed between 6 ambulance bases in Cape Town, South Africa namely: The Cape Peninsula University of Technology and College of Emergency Care bases, the Red Cross Air Mercy Service, as well as the four key divisions (Northern, Southern, Western and Eastern) of the Provincial Government of the Western Cape Emergency Medical Services (PGWC EMS). Four packs of PRBC were housed at each ambulance base mentioned, resulting in a modest total of twenty-four PRBC packs used in this study, due to the scarcity of blood in a developing country context and resultant ethical constraints. This study was done over a 42-day storage period. The PRBC units provided for research were non-returnable to the WCBS, due to the uncertainty of the PRBC viability under the environmental conditions being tested. Importantly, the PRBC used were all collected from different donors by WCBS on the same day using the usual rigorous collection protocol; thus all expired on the same day to remove age of blood as a confounding factor. The PRBC collected is suspended in an additive solution: Saline-Adenine-Glucose-Mannitol (SAGM), which is the standard solution for PRBC storage in South Africa.
At each base, two of the four PRBC units were randomly assigned to the control group and stored in a temperature-controlled refrigerator (maintained between 1°−6 °C). The new refrigerator used at the ambulance base to store the PRBCs was a standard 50-liter countertop Defy model, that could maintain temperatures between 0 °C and − 20 °C.
The remaining two units of PRBC (at each base) were labelled, ‘day’ and ‘night’ and were transported by the Emergency Care providers on the day and night shift, respectively. These ‘treatment’ PRBC units were transported in a cooler box constructed from glass matt reinforced polyester (fibre-glass) with a gloss white gelcoat finish, supplied by Composite Compact Solutions (with 6.5 L capacity). These cooler boxes also include sealed edges which minimises thermal exchange and contains an elastic retainer to ensure ice- packs are accommodated. In addition to the cooler box, ice packs were required to ensure the cold chain is maintained. We used one ice pack initially in the cooler box, and later increased the number of ice packs from 1 to 2. These ice packs were gelled water-based solution, composed of DPA-free, food grade ADPE plastic (supplied by Seagull) and measures 4 cm x 12 cm x 18 cm. These ice packs were stored at −18 °C to ensure the cooling effect of the ice packs remained for 8 h or more. In the case of this study, blood could remain up to 24 h with the frozen ice packs and the specified cooler box mentioned above, as estimated by the WCBS standard operating procedures. The PRBC was transported using the same materials the WCBS uses to transport their red cell products between blood banks, hospitals and wards. Additionally, a digital temperature logger by Testo was added in the cooler box to track the blood temperatures. The Testo (T2 184) digital display temperature logger measures temperatures between − 30 °C and 70 °C +/- 0.3 °C, well within the 1°−10 °C specification required for this study.
This was an unpaired study, whereby the ‘control’ and ‘treatment’ units were assigned independently. Each treatment PRBC was rotated between the refrigerator and the ambulance, 12 h in a refrigerator (1–6 °C), followed by ~ 12 h in an ambulance (1–10 °C), that corresponds to each day or night shift, as the study took place under operational conditions.
The temperature of the blood transported was recorded the moment it was removed from the refrigerator as well as when it was returned to the ambulance base, after a 12-hour day/night shift. The actual duration of the ‘blood run’ varied, sometimes by hours, as the study was conducted under emergency operational conditions where shifts ‘shift’. As a quality indicator, the transportation temperature of blood had to remain between 1°−10 °C to support PRBC viability.
The PRBC packs were transported daily for 42 days, which marks the expiry of the PRBC, as stipulated by the Clinical Guidelines for the Use of Blood Products in South Africa. Throughout the study period, the PRBC storage temperatures in refrigerators were to be maintained between 1 °C and 6 °C, and transportation temperatures between 1 °C and 10 °C, also in accordance with the guidelines. On a weekly basis, the PRBC were assessed for their viability. All four units of PRBC were collected and tested for haemolysis levels using the Hemocue® Plasma/Low haemoglobin (Hb) System to determine the plasma haemolysis, and a HemoSmart® Gold Hb meter to determine the haematocrit and total haemoglobin. The HemoSmart® Gold Hb meter, is the chosen device used for this study as it is a portable palm-sized device that can measure both haemoglobin and haematocrit in < 5 s. This device requires 1 µl of whole blood or venous blood, ideal for a fingerprick test. The haemoglobin range of 4–24 g/dL can be tested on this device, covering both high and low haemoglobin levels. The HemoSmart® Gold Hb meter uses test strips and automatically calibrates when a new test strip is inserted11.
The percentage of hemolysis in a PRBC unit was calculated as follows12:
Percentage Haemolysis = (100 – Haematocrit (%)) x Plasma Haemoglobin (g/dL)) divided by Total Haemoglobin (g/dL).
The temperatures of the PRBC were recorded continuously using temperature loggers and recorded every 12 h by emergency care practitioners. These recorded temperatures were evaluated weekly for haemolysis through colorimetric/visual assessment of the PRBC packs, as well as using a HemoCue® Plasma/Low Hb System to determine percentage haemolysis of the PRBC. This was recorded as a corroborating PRBC quality indicator to document PRBC viability. At the end of the study, day 42, a conjugated diens (CD) as well as a thiobarbituric acid reactive substances (TBARS) were measured on all PRBC as markers of the level of oxidative damage to the lipids.
The CD levels were measured as described by Recknagel and Glende13, with minor modifications and entailed the following: extraction was performed after one-to-one dilution of PRBC in phosphate buffered saline, followed by 80 min chloroform-methanol incubation at room temperature. The organic layer was then washed by adding Hydrochloric acid followed by centrifugation. The lipid layer was transferred to an Eppendorf tube and allowed to air-dry overnight. The residual was then reconstituted using 1 mL of cyclohexane and then vortexed for 30 s. Thereafter, 300 µl of this mixture (for all 24 PRBC) was transferred into a microtiter plate reader in triplicate. A wavelength scan was performed between 220 and 320 nanometers (nm), to determine absorbance at 234 nm with a microplate reader (Perkin Elmer) against a cyclohexane blank. Results were expressed Abs234/g wet weight of the tissue.
The TBARS were measured using the method of Draper et al., 199314 with minor modifications and entailed the following: 50 µl supernatant from centrifuged PRBC was added to 6.25 µl 4mM cold ETOH and 50 µl 0.2 M ortho-phosphoric acid. After mixing, 6.25 µl TBA reagent (0.11 M in 0.1 M NaOH) was added to the mixture and mixed again, before microcentrifuge tube lids were punctured, and tubes heated at 90˚C for 45 min. Thereafter, the tubes were placed on ice for 2 min and then placed at RT for 5 min. One mL of n-butanol and 100 µl saturated NaCl (sodium chloride) were added to the tubes and mixed, followed by centrifugation at 12 000 rpm for 2 min at 4˚C. The top butanol phase (300 µl) of all samples was added into a microtiter plate in triplicate. The first three wells consisted of n-butanol (A1-A3) and was used as a control. The absorbance was read at 532 nm using a microplate reader. The result of lipid peroxidation was expressed as nmol malondialdehyde (MDA).
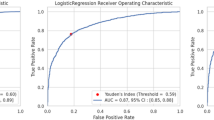
Statistical analysis was done using R statistical software15. Due to the non-linear trend observed in haemolysis levels (see Fig. 1 below), a generalised additive model was used to model the relationship between haemolysis level and time and simultaneously test for a significant difference in haemolysis level between the treatment and control groups. This model is more flexible than conventional methods such as analysis of variance (ANOVA) by incorporating a smooth term for non-linear relationships. At the same time, it avoids overfitting by penalising excessive ‘wiggliness’ in the fitted curve. Effects were considered statistically significant at P < 0.05.
Results
Percentage haemolysis of all 24 packs of PRBC over a 42-day period are depicted in Fig. 1. The trend for all samples appeared similar. Percentage haemolysis over the 42-day PRBC shelf-life period had increased, as expected, and at an increasing rate after day 35. Figure 1 indicates an outlier in the control group on day 1, marked with a high haemolysis percentage in comparison to the other PRBCs at the start of this study. Using an extreme outlier fence of Q1–3 IQR and Q3 + 3 IQR (where Q1 and Q3 are the first and third quartiles and IQR is the interquartile range), this blood pack’s haemolysis level was an extreme outlier already at Day 1. This was likely due to causes involving the handling of the blood following donation.
The minimum level of haemolysis in both the treatment and control groups was < 0.2% on day 1, marking the start of the study. Apart from the outlier, all units in the control group remained below the maximum acceptable level of haemolysis of 0.8%, on the last day, day 42. By comparison, three of the twelve units in the treatment group exceeded the maximum acceptable level of haemolysis of 0.8%, by day 42 (two of these only marginally).
Generalised additive model for haemolysis trajectory
A generalised additive model (GAM) was fit to the data with haemolysis level (measured as a percent) as the response variable and two predictor variables, Day (days elapsed, taking values of 1, 7, 14, 21, 28, 35, 42), and Group (Treatment, PRBC that were transported in ambulance vehicles, and Control, PRBC that were kept in a refrigerator at the respective ambulance bases). The relationship between haemolysis level and day was modelled using a penalised cubic regression spline fitted using the mgcv package in R16,17. The outlier blood pack in the Control group, mentioned earlier, was omitted from the data for modelling purposes.
The p-value for the smooth term (not shown in Table 1) was obtained using an approximate F test and was < 10−15, indicating that the smooth term on day is statistically significant. The p-value for Group in Table 1 indicates that there is a statistically significant difference in haemolysis level between the Treatment group and the Control group; the haemolysis level of the Treatment group was, on average, higher by about 0.05%. It follows that research hypothesis H1.1 is supported, namely that haemolysis occurs at a faster rate in the Treatment group than in the Control group. However, when a GAM including an interaction effect between day and group was fitted, a likelihood ratio test found that it was not a significantly better fit (p-value = 0.86). This means, in effect, that there is no evidence that the rate of increase in haemolysis level over time differs between the treatment and control groups. Rather, the treatment group already had a higher average haemolysis level on day 1, so the difference between the groups may not be attributable to the treatment effect (i.e., due to being transported in cooler boxes on ambulance).
The model’s adjusted R2 (multiple coefficient of determination) was 0.707, which suggests strong explanatory power for a model with only two predictors. This model was used to predict the haemolysis trajectory over 42 days (Fig. 2), starting from the day of the blood donation. The predicted values were plotted together with 95% prediction limits. For the Treatment group, the predicted haemolysis level after 42 days was 0.72%, with 95% prediction interval (0.67%, 0.76%). For the Control group, the predicted haemolysis level after 42 days was 0.66%, with 95% prediction interval (0.62%, 0.71%).
Using the investr R package18 the GAM’s inverse function was estimated and used to predict how many days would elapse before a blood pack would reach the threshold of 0.8% haemolysis. For the Treatment group, the threshold was projected to be reached between days 43 and 44, with a 95% prediction interval of (42.7, 45.1). For the Control group, the threshold was projected to be reached between days 44 and 45, with a 95% prediction interval of (43.6, 46.4). What this implies is, firstly, that blood packs stored in cooler boxes on ambulances in the manner of the Treatment group are more than 95% likely to remain below the 0.8 haemolysis threshold until their normal expiry date (42 days). Secondly, it implies that the projected lifespan of a blood pack is only about one day shorter when handled in the manner of the Treatment group as compared to being stored in a refrigerator at the base in the manner of the Control group. This evidence supports research hypothesis H1.2, which turns out to have been conservative: the blood packs taken onto ambulances and kept in cooler boxes are projected to remain below the 0.8% haemolysis threshold for about six weeks, far longer than the hypothesised two weeks. The narrowness of the above prediction intervals suggests that despite the small sample size of 24 units used in the study (23 included in the model, due to the outlier), it was sufficient to obtain fairly precise estimates concerning the haemolysis levels that would be expected for any PRBC handled under these experimental conditions, in the field.
Frequency, time and temperature
In most cases the PRBC were in transit for 10–12 h (with intermittent stops between calls) with ice packs and a temperature logger. The number of hours elapsed between the blood’s removal from the refrigerator and its return is seen in Fig. 3, Panel a. In most cases the blood pack was away from the ambulance base for 10–12 h, with a rare occurrence of blood being away from the ambulance base for 24 h, and a few instances of less than 10 h.
No association was found at 5% significance level between temperature change and time elapsed (Kendall’s nonparametric correlation coefficient; p-value: 0.128). Moreover, no significant difference was found in the mean temperature of a blood pack when it left the base and when it returned to base (paired t-test p-value: 0.399). This suggests that the cold-chain management method used for the ‘blood-run’ on the emergency vehicles was effective. The blood transportation range is between 1˚C-10˚C. The blood temperature upon return from the blood-run was below 10˚C in most cases and rarely exceeded temperatures of 10 ˚C (Fig. 3, Panel b). Ten of the twelve blood packs in the treatment group had temperatures logged, and while eight of the ten exceeded 10 ˚C at least once during the study, these occasions were rare, and 11 ˚C was exceeded on only four occasions. Only two blood packs were ever below 1 ˚C on return to base (one of them on two occasions).
Lipid peroxidation levels
When comparing the Treatment group of the CD and TBARS test against the Control group (Fig. 4), a two-tailed t-test found no significant (p = 0.6768) differences in the mean TBARS levels when comparing the treatment and control groups. A similar result was shown for the mean CD levels between the two groups, with p = 0.2459 (Fig. 4).
Discussion
This research study yielded some unprecedented results in the South African context that support the viability (in terms of cold-chain, haemolysis and oxidative stress) of PRBC in the pre-hospital setting. The primary objective of the study was to determine whether PRBC would remain viable in transit on ambulance vehicles. One of the quality indicators to determine the viability of blood was haemolysis not exceeding 0.8% (as per European guidelines adopted in South Africa). Certain factors such as transportation, processing, handling, temperature and storage of blood could exacerbate the onset of haemolysis19. Premature PRBC haemolysis is an obvious marker of PRBC that has been stored in an incorrect manner20. One of the most interesting findings in this study was that the PRBC in ambulance transit remained, for the most part, between the recommended transportation temperature of between 1˚C–10˚C21. Having blood in ambulance transport for approximately 12 h, with ambient temperatures being high, we found that one ice pack for 1 PRBC was insufficient. Two PRBC exceeded 10˚C upon return to the ambulance base, but all other parameters regarding the integrity of blood was still within normal range. After the practitioner reported the PRBC exceeding 10˚C, adjustments were made immediately to all ambulance bases indicating that 2 ice packs should be used for 1 PRBC. However, some outliers were then reported of PRBC being returned to the ambulance base below 1˚C. This was due to a (small) minority of practitioners being cautious about PRBC exceeding 10˚C by adding a third ice pack. When the practitioners applied the recommended 2 ice packs per 1 PRBC method, the PRBC remained within the recommended transportaion range of 1˚C − 10˚C. In the United States of America, anecdotal temperature trends from an aeromedical environment using also cooler boxes aligned with those obtained in this study, although that was an observational report22.
Haemolysis levels were tested on both the Control and Treatment PRBC on days 1, 7, 14, 21, 28, 35, and lastly 42 (PRBC expiry). The results indicated that haemolysis had increased from day 1 – day 42 of storage and transportation as suggested by Arif et al.23. An outlier with a starting haemolysis of > 0.7% was identified on day 1 of testing which was one of the Control PRBC, prior to it being distributed to the ambulance bases. This could be due to various factors, such as incorrect storage and transportation of PRBC after blood donation, possible bacterial growth in the blood pack, traumatic phlebotomy technique by new staff, rapid resuspension of blood to mix with the anticoagulant or the selection of an incorrect spin on the centrifuge24. Another interesting finding was that, excluding the outlier, PRBC of both the Control and Treatment groups were < 0.8% (the maximum acceptable level of haemolysis as per the adopted European Guidelines) after day 35. On day 42, three of the Treatment PRBC were slightly above 0.8% haemolysis, while the Control PRBC other than the outlier were below the 0.8% haemolysis level. The results therefore support the viability of PRBC in ambulance transit. However, considering the haemolysis findings above, it would be a safety threshold recommendation to use PRBC in ambulance vehicles only until day 35, or to return them to the transfusion service earlier to prevent wastage.
The temperature of the PRBC in ambulance transit was also monitored as the PRBC would remain in transit for the duration of the shift being 10–12 h. The blood would then be returned to the temperature-controlled refrigerators at the end of the shift. Blood can be stored in the cooler box, provided to prehospital staff for up to 24 h with ice packs, maintaining the recommended transportation temperature range of 1˚C-10˚C25. However, certain factors can confound the desired temperature range, since ambient temperatures of ambulance vehicles without air conditioners, as in this study, can (in theory) exacerbate the rate of haemolysis. Daily temperature highs and lows in Cape Town during the study period averaged 23 degrees celsius (°C) and 12 °C respectively, with a maximum temperature of 28 °C and a minimum of 9 °C. Further research would be needed to assess the impact of higher ambient temperatures during summer, when outside temperatures occasionally exceed 35 °C. However, a GAM fit to the treatment group only (results not shown) with shift (day/night) as a factor found no significant difference in haemolysis between blood packs on the night shift vs. the day shift (p-value: 0.49). This suggests that the change in ambient temperature between day and night had little impact on haemolysis under the experimental conditions.
Due to the good cold-chain management in this study, we did not increase the stress in cells and thus oxidative stress was not increased, as evidenced by our TBARS and CD results. The suggested conditions for blood to be transported on ambulance vehicles with the use of cooler boxes and ice packs are: 1 PRBC with 2 ice packs, blood should be transported up to day 35 only from the day bled, ice packs should be alternated at the start of each shift (every 10–12 h) as in this study. This considers all possible external factors encountered to allow the cold-chain management of the PRBC in this study to be maintained, and the PRBC to remain below the 0.8% acceptable haemolysis percentage. This study demonstrates compliance with the desired transportation temperature range of 1˚C-10˚C as per the clinical guidelines of South Africa. We note that the use of PRBC is indicated early (in stage 2 of shock classification)26, for which point-of-care testing (POCT) is enabling. In South Africa, there are various POCT devices that can measure haemoglobin as well as lactate levels, that can be utilized to enhance pre-hospital patient assessment and management such as the epoc® Blood Analysis System that uses just a few drops of blood drops to measure electrolytes, metabolites as well as blood gases in less than 1 minute. The i-STAT 1 System can test lactate and haemoglobin in approximately 2 minutes and lastly the HemoCue® device that is a portable device used for haemoglobin testing and offers rapid, accurate results. The HemoCue® 301 has demonstrated its feasibility/accuracy when haemoglobin results were compared to a central laboratory in South Africa27. A study done by Uyoga et al.28, advocates for point-of-care Hb devices to be more widely available for hospitals across sub-Saharan Africa as it will support the promptness in requests for blood transfusion. This notion would also suit the pre-hospital setting, to ensure the emergency care practitioners could promptly assess the patients Hb levels and make timeous, informed decisions regarding early blood transfusion. The findings of this preliminary study and validation of statistical analyses would pave the way for clinical trial research to allow for implementation of these findings. Our findings cohere well with a study of red cell concentrate quality after repeated air rescue mission transports for prehospital transfusion in Germany where the logistics and maintenance of the thermal conditions were found to be safe and feasible29.
Conclusion
The findings of this study were specifically based on environmental and handling factors that contributed to the PRBC haemolysis. The limitations include resource and research scope limitations. We were unable to test for other biochemical markers such as potassium, 2,3-DPG, lactate, etc., and as the pilot took place in a single season, the impact of weather extremes due to seasonality is not explored. The resource-constrained setting (LMIC) limited the sample size. Donor-related factors such as donor genetic variability can contribute to an increase in haemolysis levels; this study did not test for genetic variability.
The objective of this study was to determine the viability of PRBC in the EMS setting, prior to the onset of haemolysis. The integrity of the PRBC was found to be well preserved since the cold-chain management of the PRBC was well maintained, using a cost-effective method of transporting the PRBC in a cooler box with 2 ice packs for one unit of PRBC. The PRBC percentage haemolysis at the end of the 42-day expiry reached a maximum level of 0.8% which aligns with the acceptable haemolysis percentage of the European Guidelines. While this was only a pilot study and more research would be required to make clinical recommendations, it at very least demonstrates the value of undertaking such research.
Lastly, the markers for the indication of oxidative stress, being CD and TBARS that was done at the end of the 42-day period, showed no statistically significant changes. All the specifications that were observed indicated that PRBC could remain viable in the EMS setting, up to the point of transfusion decision. Whilst contemporary literature26,30 focuses on clinical indications and biomedical complexity of transfusions, this finding validates the study protocol and control of environmental conditions (notwithstanding the impacts of global warming) to reduce oxidative stress and haemolysis of PRBC in the out-of-hospital setting. This is highly relevant to supporting the provision of early blood transfusion in the community or transportation of PRBC by ambulance in low- and middle-income countries during everyday operations31 or in humanitarian emergencies.
Data availability (and R code)
The data files and R code used in this study are available via Open Science Framework (OSF). The R script contains all code necessary to reproduce the analyses and figures presented in the article. The link to the OSF repository is https://osf.io/3nzb8/?view_only=8311768e920a492b8bfe6f66e185d928.
Abbreviations
- CD:
-
Conjugated dienes
- GAM:
-
generalised additive model
- Hb:
-
Haemoglobin
- MDA:
-
Malondialdehyde
- NaCl:
-
Sodium Chloride
- PGWC EMS:
-
Provincial Government of the Western Cape Emergency Medical Services
- POCT:
-
Point-of-care testing
- PRBC:
-
Packed Red Blood Cells
- TBARS:
-
Thiobarbituric acid reactive substances
- WCBS:
-
Western Cape Blood Service
- WHO:
-
World Health Organisation
References
World Health Organization. [cited 16 July 2021]. (2021). Available from: https://www.who.int/news-room/fact-sheets/deail/injuries-and-violence
Eastridge, B., Holcomb, J. & Shackelford, S. Outcomes of traumatic haemorrhagic shock and the epidemiology of preventable death from injury. Transfusion 59 (S2), 1423–1428. https://doi.org/10.1111/trf.15161 (2019).
Spinella, P. Zero preventable deaths after traumatic injury. J. Trauma. Acute Care Surg. 82 (6S), S2–S8. https://doi.org/10.1097/TA.0000000000001425 (2017).
Holcomb, J. et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma. JAMA 313 (5), 471. https://doi.org/10.1001/jama.2015.12 (2015).
Jooste, B. Cape Town is stab capital of SA [Internet]. Iol.co.za. 2010. Available from: https://www.iol.co.za/news/cape-town-is-stab-capital-of-sa-731954
Head, T. & Nyanga Western Cape, has a murder rate of one in every 206 people [Internet]. (2017). Available from: https://www.thesouthafrican.com/news/nyanga-highest-murder-rate-south-africa/
Bowdler, N. Air ambulance first in UK to carry blood [Internet]. BBC News. 2012 [cited 16 July 2021]. Available from: https://www.bbc.com/news/health-16928621
Sawas, A. & Pentyala, S. Evaluation of lipid peroxidation in red blood cells by monitoring the uptake of sucrose and phenol red. J. Appl. Toxicol. 24 (3), 223–229. https://doi.org/10.1002/jat.976 (2004).
Bellairs, G. R. M. & Ingram, C. Clinical Guidelines for use of blood products in South Africa. 6th ed. [Date Accessed: 13 April 2025] (2023).
Trauma Society of South Africa. Massive Transfusion/Massive Haemorrhage Protocol. [online] (2023). Available at: https://www.traumasa.co.za/protocols/ [Accessed 26 Jul. 2025].
Halomedicals Hemoglobinometer catalogue. [pdf] (2020). Available at: https://halomedicals.com/wp-content/uploads/2020/08/Hemoglobinometer-Catalogue.pdf [Accessed 27 Jul. 2025].
Sahoo, J. et al. Changes in hematological and biochemical parameters and rate of hemolysis during the storage of packed RBC units: A prospective study. J. Lab. Physicians. 17, 88–94. https://doi.org/10.25259/jlp_212_2024 (2025).
Recknagel, R. & Glende, E. [40] spectrophotometric detection of lipid conjugated dienes. Methods Enzymol. 105, 331–337 (1984).
Draper, H. H. et al. A comparative evaluation of thiobarbituric acid methods for the determination of malondialdehyde ibiological materials. Free Radical Bio Med. 15, 353–363 (1993).
R: The R Project for Statistical Computing [Internet]. R-project.org. 2020 [cited 21 July 2021]. Available from: https://www.r-project.org/
Wood, S. N. Fast stable restricted maximum likelihood and marginal likelihood Estimation of semiparametric generalized linear models. J. Royal Stat. Soc. (B). 73 (1), 3–36 (2011).
Wood, S. N. Generalized Additive Models: An Introduction with R (2nd edition). Chapman and Hall/CRC. (2017).
Greenwell, B. M. & Schubert Kabban, C. M. investr: An R Package for Inverse Estimation. The R Journal. ;6(1), 90–100. (2014). https://doi.org/10.32614/RJ-2014-009
Zimmermann, R. et al. In vitro quality control of red blood cell concentrates outdated in clinical practice. Transfus. Clin. Biol. 10 (4), 275–283. https://doi.org/10.1016/s1246-7820(03)00032-6 (2003).
Sawant, R., Jathar, S., Rajadhyaksha, S. & Kadam, P. Red cell hemolysis during processing and storage. Asian J. Transfus. Sci. 1 (2), 47. https://doi.org/10.4103/0973-6247.33446 (2007).
South African National Blood Service (SANBS) and the Western Province Blood Transfusion Service (WPBTS). Standards of Practice for Blood Transfusion in South Africa. 7th ed. South Africa, p.28. (2016).
Conterato, M. [Internet]. [cited 11 July 2021]. (2016). Available from: https://www.jems.com/patient-care/trauma/implementing-protocols-to-administer-blood-products-in-the-out-of-hospital-setting/
Arif, S., Yadav, N., Rehman, S. & Mehdi, G. Study of hemolysis during storage of blood in the blood bank of a tertiary health care centre. Indian J. Hematol. Blood Transfus. 33 (4), 598–602. https://dx.doi.org/10.1007%2Fs12288-016-0769-5 (2016).
Dhawan, H., Sachdeva, P., Gupta, A., Sharma, R. & Marwaha, N. Hemolysis during component preparation: an inadvertent cause. Asian J. Transfus. Sci. 11 (2), 79. https://doi.org/10.4103/ajts.ajts_89_16 (2017).
Hardwick, J. Blood storage and transportation. ISBT Sci. Ser. 3 (2), 177–196. https://doi.org/10.1111/j.1751-2824.2008.00196.x (2008).
Bonanno, F. G. Management of hemorrhagic shock: physiology approach, timing and strategies. J. Clin. Med. 12 (1), 260. https://doi.org/10.3390/jcm12010260 (2023).
Jaggernath, M. et al. Diagnostic accuracy of the Hemocue HB 301, stat-Site MHGB and urit-12 point-of-care hemoglobin meters in a central laboratory and a community-based clinic in durban, South Africa. PLOS ONE. 11 (4). https://doi.org/10.1371/journal.pone.0152184 (2016).
Uyoga, S. et al. Point-of‐care haemoglobin testing in African hospitals: A neglected essential diagnostic test. Br. J. Haematol. 193 (5), 894–901. https://doi.org/10.1111/bjh.17431 (2021).
Boecker, C. et al. Noninferior red cell concentrate quality after repeated air rescue mission transport for prehospital transfusion. Transfus. Med. Hemother. 49 (3), 172–179 (2022). PMID: 35813604; PMCID: PMC9209961.
Trudeau, J. D., Dawe, P. & Shih, A. W. Massive hemorrhage and emergency transfusion. In: Clarke G, Chargé S, editors. Clinical Guide to Transfusion [Internet]. Ottawa: Canadian Blood Services, [Accessed 08 April 2025]. Chapter 11. (2021). Available at https://professionaleducation.blood.ca/en/transfusion/clinical-guide-transfusion
Zalgaonker, M., Naidoo, N. & Christopher, L. D. Penetrating injury from interpersonal violence and related haemorrhagic shock resuscitation practices in an urban South African emergency medical service. Australian J. Paramedicine Sage. 18, 1–9. https://doi.org/10.33151/ajp.18.873 (2023).
Acknowledgements
Western Cape Blood Service (Dr Gregory Bellairs) is acknowledged for the provision of blood, pro bono. Western Cape Emergency Medical Services, Western Cape College of Emergency Care, Cape Peninsula University of Technology (Dr LD Christopher: Department of Emergency Medical Sciences) and Red Cross Air Mercy Service (Mr Ashwin Krishna) are acknowledged for facilitating data collection in the field.
Funding
Cape Peninsula University of Technology, University Research Fund (Reference: URF/Z Abdul).
Author information
Authors and Affiliations
Contributions
ZA is credited for Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. NN is credited for Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.TF is credited for Conceptualization, Data curation, Formal Analysis, Methodology, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. JM is credited for Formal Analysis, Investigation, Methodology, Resources, Validation, Writing – original draft. JB is credited for Formal Analysis, Investigation, Methodology, Resources, Validation, Writing – original draft. DB is credited for Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Clinical trial number: not applicable. Ethics approval was obtained from the Health and Wellness Sciences Research Ethics Committee (HWS REC) as an Institutional Review Board (IRB) at the Cape Peninsula University of Technology (Ref.: CPUT/HW-REC 2017/H32). No adverse events or ethical breaches were encountered.
Consent for publication
All participating practitioners provided informed consent to participate in the research and to publish findings. Data was anonymised.
Consent to participate
All participants provided written informed consent to participate, with the option of withdrawal at any time and without reprisal. No patients were enrolled, and no actual blood transfusions were conducted.
Declaration on human experiments
All methods were carried out in accordance with relevant guidelines and regulations of: National Department of Health Research Ethics Committee, Western Cape Health Department, Professional Board for Emergency Care (PBEC)-Health Professions Council of South Africa (HPCSA) and Western Cape Blood Service.
All experimental protocols were duly approved by the CPUT Faculty of Health and Wellness Research Committee and Institutional Higher Degrees Committee (HDC). Informed consent was obtained from all participants enrolled in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zeenat, A., Navindhra, N., Thomas, F. et al. A pilot experimental study of cold-chain management, haemolysis and oxidative stress of packed red blood cells in early blood transfusion: toward a blood viability model in the out-of-hospital setting. Sci Rep 15, 35613 (2025). https://doi.org/10.1038/s41598-025-18923-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-18923-w