Abstract
A key lesson from COVID-19 is the distinctive role of nurses during pandemic crises and the insights derived from their experiences. The aim of the study is to show the unique functioning of nurses in a strong and multifaceted crisis from their own point of view and to outline suggestions at the level of employees/ organizations. The primary research method was the individual in-depth interview (IDI), conducted with a purposively selected group of participants. The sample of 80 respondents was randomly selected from 1221 hospital employees who participated in a quantitative and serological study at the beginning of 2020. Nurses and midwives were included in the sampling, as an earlier study found that this occupational group had a higher risk of SARS-CoV-2 infection. A total of 26 nurses participated in structured, in-depth interviews. The study provided a comprehensive account of nurses’ organizational behavior in crisis situations, as well as an overview of how the medical center functioned during such times. It also offered recommendations to improve the resilience of healthcare facilities in the face of future crises. Both the analysis of the crisis and the proposed guidelines addressed the individual level (i.e., individual staff members) and the team or organizational level. The study also identified key similarities and differences in nurses’ responses and included recommendations for strengthening healthcare system resilience during the COVID-19 pandemic. The identified patterns—such as the absence of denial and acceptance accompanied by increasing conflict—may extend beyond the context of the COVID-19 pandemic and could be indicative of responses to future large-scale infectious outbreaks without clearly defined treatments. Recommendations for enhancing the resilience of medical centres in future crises were developed based on observed dynamics in nurses’ responses. These include fostering a “positive internal PR” around the infection control team, recognizing and reinforcing positive behaviours demonstrated during the COVID-19 crisis, and incorporating constructive crisis-time practices into standard nursing protocols.
Similar content being viewed by others
Introduction
The COVID-19 pandemic has posed several challenges to modern health care, especially infection surveillance and control. Modern infection control in Poland has been in place for the last 30 years, but several studies in various areas indicate that it is not implemented effectively (e.g.1,2,3). A quantitative survey assessing the preparedness of the largest modern teaching hospital in Poland revealed that fundamental principles of infection prevention were insufficiently known and followed by nurses. This lack of adherence was associated with significantly higher COVID-19 seroprevalence, particularly within this professional group4,5. However, this type of quantitative research does not address the underlying barriers and problems at the management level. Qualitative research can be helpful in filling this gap, allowing us to learn about the opinions of nurses. As research carried out in Denmark and Australia showed6 that not only the epidemiological conditions (number and effects of infections) influence the ability to cope with the challenge of the pandemic and the well-being of employees. The conditions of the work environment and the broader social context are alsoimportant. The organizational culture in the Polish health care system is characterized by high power distance, masculinity, and uncertainty, which does not constitute a supportive environment for nurses2,3,7. Contemporary management theory goes beyond the framework of Hofstede’s theory, especially in crisis situations.
The behaviour of nurses in medical facilities in the face of infections
Alongside the quantitative monitoring of COVID-19 infections, hospitalizations, and deaths, another important area that emerged was the subjective experience of the pandemic among nurses, along with the reactions and decisions that arose from it. There is evidence suggesting that the increase in infections and hospitalizations, and therefore the increased exposure to infection by nurses, should be associated with increased symptoms of stress. However, the relationship does not appear to be directly proportional. This is shown, for example, by comparing the response to work during COVID-19 of nurses and midwives in Denmark and Australia6. Both countries were characterised by a relatively low number of infections in the first wave of infections and a similarly unequivocal approach to the restrictions imposed. However, the nurses in Australia showed significantly more symptoms indicating stress, where there were objectively significantly fewer infections and hospitalisations than in Denmark. Evidence suggests that their responses to stress and infection risk were shaped by both individual characteristics and environmental conditions.
In the study mentioned above6, the factors associated with reduced stress reactions experienced were age and clinical experience; working full-time (rather than part-time); living in a household with school-age children (joint residence). Similar effects have been observed in other countries, including the USA and Canada. In addition to factors related to individual characteristics and describing the immediate social environment, environmental factors of a broader nature were also important, especially (subjective) trust in the actions of government agencies6.
However, research suggests that healthcare workers group, including nurses, exposed to challenging situations and emotional exhaustion may have a diminished ability to employ effective coping strategies, which can lead to negative attitudes toward their work8. This reaction can also be linked to job demands such as team climate or work pressure. While workplace and personal resources can serve as protective factors in these circumstances9,10, studies show that the tendency to perceive job demands as stressful is closely related to the level of individual personal resources11. Job demands have been shown to negatively impact and diminish the quality of the workplace environment, whereas job resources—such as organizational belonging and coworker support—can positively influence and enhance these conditions12,13,14. Another review, testing antecedents and outcomes, of work engagement among Japanese nurses confirmed a similar structure found in western countries. This means that improvement in personal or job resources (e.g. teamwork) can improve work participation in this group15.
Behaviour in a crisis situation
Crisis management has recently gained increased attention. Jaques16 described it as a continuous discipline and highlighted its evolution toward classifying different types of crises. The approach is moving toward a holistic integration of pre- and post-crisis actions. He proposed a relational model based on the dynamics of crisis response, structured around interconnected clusters of actions rather than a strict sequential process. While pre-crisis and crisis management are temporally related, elements such as crisis prevention and preparedness can overlap or occur simultaneously.
The relational model of crisis prevention16 consists of four major elements concerning crisis itself—preparedness, and prevention (pre-crisis management phase) as well as incident management and post-crisis management (crisis management phase). These include various processes and activities. These components are not necessarily sequential and may occur simultaneously, depending on the nature and origin of the crisis. Jaques’ relational model visually outlines the phases of crisis management, emphasizing pre-crisis anticipation, disruption, and post-crisis reorganization (Fig. 1). This model provides the temporal framework for our study by defining four phases of crisis response and framing how nurses’ reactions evolve over time—an evolution reflected in our staged findings. Figure 1 highlights that effective organizational change during crises follows four interconnected phases: crisis preparedness, crisis prevention, post-crisis management, and crisis incident management. Each phase requires specific strategies—from planning, training, and early risk detection to operational recovery, evaluation, and coordinated crisis response—ensuring a continuous cycle of readiness, action, and improvement.
The relational model of crisis prevention16. It illustrates the temporal stages of crisis response according to Jaques’ relational model, showing how preparedness, prevention, incident management, and post-crisis actions overlap and interact.
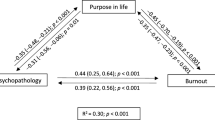
The model offers an integrated framework for crisis management, that goes beyond traditional linear approaches, thereby improving the effectiveness of crisis response. In response to the COVID-19 pandemic, organizations are updating management methods to enhance resilience, recover faster, and improve results17. This crisis prevention model offers a framework for boosting organizational resilience and fostering post-crisis growth18. It also addresses crisis dynamics, specifically describing nurses’ organizational behaviour during the pandemic (Fig. 2). Unlike other linear, literature-based models19,20, this approach offers a more dynamic perspective.
Experiencing a crisis
An innovative and strategic four-phase model can be effectively leveraged to gain deep insights into how individual employees—and, consequently, entire teams—perceive and adeptly navigate crisis situations. Within this in-depth analysis, a robust model of employee response to organizational change21,22 has been dynamically adapted from the Blanchard model23. This revised and enhanced response model is showcased in Fig. 2. It presents a modified version of Blanchard’s model adapted to the nursing context, showing how emotional and cognitive responses evolved across four stages of change—from early shock and mobilisation through adaptation and internalisation—and how different types of concerns surfaced at each stage, ranging from personal uncertainty to system-level evaluation. Concerns evolve over time—from lack of information and personal impact in the early stages, to long-term consequences and opportunities for improvement in later phases—while overall effectiveness can dip before gradually recovering as acceptance grows.
This study explored nurses’ understanding and interpretation of situations at both individual and organizational levels. We identified similarities and differences between nurses’ roles during the COVID-19 pandemic and those described in traditional crisis models. This analysis informed guidelines to better prepare nurses for future challenges across all areas of medical facility operations. We adapted Blanchard’s model to capture the specific emotional states experienced by nurses.
Material and methods
We chose to conduct our research using a qualitative, interview-based method. This approach was driven by the objective to explore nurses’ attitudes and behaviours during the pandemic and to reflect on their professional functioning in a high-risk environment that threatens both health and life. This led us to purposively select participants from a highly specialized medical facility. For our research tool, we chose a qualitative approach—specifically, in-depth individual interviews (IDIs).
Our choices regarding the study setting and research method also determined the appropriate data analysis techniques. These included the construction of a typology of attitudes and behaviours, as well as the creation and analysis of mental maps.”
-
1.
The results were presented in accordance with the four phases of the model: preparation; implementation of early and late change; and perpetuation of change. This temporal model also served as the basis for organising and analysing the interview content. Behaviour in the subsequent stages of the crisis was as follows: The initial phase pertains to the period where the immediate impacts of a fully developed crisis have not yet manifested; at this stage, we observe the early indicators and still possess the opportunity to prepare for challenging circumstances. Within our interview, questions 3, 4, and 5 specifically addressed this phase of transition. These questions were focused on anti-infection protocols during the pandemic. Nevertheless, in the participants’ responses, there was frequent mention of the preliminary stages of establishing wards for patients with COVID-19. Additionally, other questions in the interview (notably questions 6–9) were analyzed as discussions related to crisis preparation occasionally emerged in responses to these other questions.
-
2.
In the second phase, the situation is characterized by direct and personal impacts resulting from the crisis and its ramifications. It becomes imperative to enact radical alterations in our daily operations; however, during this phase, the positive outcomes of amplified employee exertion may not yet manifest at an organizational level. This phenomenon is attributable to the worsening crisis situation, which persists in its decline notwithstanding the dedicated efforts of nurses. Interview questions 6, 7, and 8 (Supplementary Material no. 1) pertain directly to this phase of transformation. These questions address the implementation of anti-infection protocols within COVID-19 wards. Additionally, responses to other questions were scrutinized, as they occasionally encompassed motifs pertaining to the initial implementation phase of change, observed through responses that compared successive operational phases during the pandemic wave.
-
3.
The third phase, termed ‘response,’ pertains to the period during which the implementation of changes has been sustained over an extended duration, allowing for the initial positive outcomes of such activities to manifest within the organization. The accumulated efforts of employees over time progressively yield beneficial effects. Employees may perceive the prevailing situation with the sentiment that “The worst is behind us." Interview questions 9 and 10 explicitly addressed this phase (refer to: Supplementary Material no. 1), focusing on the circumstances of working in a COVID ward and alterations in working conditions. Additionally, other interview questions were scrutinized, as participants occasionally introduced aspects related to the late phase of change implementation when responding to different questions.
-
4.
In the fourth phase, the response denotes the period during which the crisis subsides, and the modifications implemented in response to the crisis are fully assimilated by both the nurses and the organization. T The crisis produced lasting positive effects: new routines became embedded in staff behaviour and new patterns of cooperation emerged. Interview Questions 17 and 18 specifically pertained to this phase of transformation (please see: Supplementary Material no. 1). These questions focused on identifying practices deemed worthy of preservation and those considered superfluous or detrimental. Furthermore, other interview questions were subjected to analysis as participants occasionally referenced practices meriting consolidation, even when discussing initial stages of change implementation.
Group selection
The study was carried out at the Kraków University Hospital (UHK), the largest teaching hospital in Southern Poland. About 70% of hospital beds were at the new hospital headquarters, in operation since October 2019. In the beginning of the COVID-19 pandemic, UHK was the only hospital in the region of Małopolska where almost all patients with confirmed SARS-CoV-2 infections were hospitalized independently of their clinical status. Later, many regional COVID-19 hospitals were organised, and UHK admitted mainly patients with severe condition or with clinical complications of COVID-19 requiring specialised treatment. From March 2020, it had a universal masking policy and systems for screening, testing, and reporting COVID-19 symptoms among all healthcare workers (including physicians, nurses, and other staff) as well as patients.
The baseline survey included questions on the sociodemographic characteristics of the participants, the previous SARS-CoV-2 infection with its severity, and potential complications. Methods and population studied in the first stage of the study have previously been described in detail4.
The sample of 80 respondents was randomly selected from 1221 hospital employees who participated in a quantitative and serological study at the beginning of 2020. Only nurses and midwives were included in the sampling, as an earlier study found that this occupational group had a higher risk of SARS-CoV-2 infection5. The place of work (working on a ward for COVID patients versus a non-COVID ward) and infection (or not) with the SARS-CoV-2 virus confirmed by serology were used as the stratum. Of the 80 nurses selected, 38 worked in COVID-19 wards and 42 in non-COVID wards; 40 had been infected with SARS-CoV-2, while 40 had not. The studies involving human participants were reviewed and approved by the Jagiellonian University Bioethics Committee (protocol code 1072.6120.353.2020, date of approval 16.12.2020). Patients / participants provided their informed consent in writing to participate in this study.
Selection of research tool: In-depth individual interview (IDI)
In this study, individual in-depth interviews were applied. These interviews served as a method for gathering qualitative data to explore and understand an individual’s attitudes. Each interview followed a script outlining the main topics of discussion and typically lasted between 30 and 90 min.
For this project, in-depth individual interviews offer the opportunity for participants to speak openly about difficult topics—such as challenges in patient care, communication breakdowns among nurses, or systemic issues within the healthcare facility. This kind of self-reflection on mistakes, when gathered from multiple individuals, helps us develop tools for diagnosis and improvement. The use of this tool aligned with our main objective: to deepen our understanding of how nurses’ function in a crisis, specifically during the COVID-19 pandemic. The interview included 19 questions was used (see Supplementary Material no. 1).
A new interview protocol was specifically designed for this study. It was developed by a broad interdisciplinary scientific team (management sciences, psychology, medicine), considering existing knowledge in the field of crisis response models and the specificity of organisational behaviour of nurses.
Procedure
Research was carried out between mid-June 2021 and September 2021. Of the 80 nurses selected, 26 agreed to participate in the interview and were treated as anonymous respondents. The homogeneous sample size of 26 in this qualitative study was sufficient to explain social phenomena and achieve data saturation, according to the systematic review by Hennink and Kaiser24. Their empirical findings indicated that homogeneous qualitative research samples can achieve data saturation with as few as 9 to 17 interviews24.
All participants in our sample were fully vaccinated at the time of the study. A meeting was scheduled with each of them in the hospital and the interview was recorded after obtaining their consent. Each person answered 19 questions. Respondents were informed that they could decline to answer any questions that caused discomfort. After interviews, responses were transcribed and analysed qualitatively for study.
Given the sample size and the fluctuating nature of the pandemic (infection waves and low-incidence periods), interviews were conducted continuously, accompanied by weekly research team meetings to review progress and consider possible adjustments to the research tool. Although no preliminary study was conducted, the evaluation of the 19 questions developed by the expert team proved stable, and the research tool remained unchanged throughout the study period.
Data analysis
The analysis of the collected data was divided into three 3 stages. In the first stage, content analysis was used. The interview material was arranged in chronological order. Arranging the statements chronologically revealed that they correspond to the successive stages of crisis response (Fig. 2) described in Blanchard’s23 modified model. Content analysis was chosen as the primary method because semantic analysis of the entire dataset did not yield satisfactory results.
In the second step, content analysis continued: by categorizing statements assigned to specific time intervals into responses related to individual functioning and the activities of the ward task force (see Results 3.1.—3.4.).
In the final stage, semantic analysis was employed as a complementary method. This method provided a more detailed examination of the process outlined in the timeline (Fig. 4). Blanchard’s framework23 provided a strong basis for conducting deductive, theory-driven content analysis. This approach was justified because the study was grounded in a predefined framework. Directed content analysis, as articulated by Hsieh and Shannon25 and further developed by Assarroudi et al.26, enables a systematic exploration of how predefined categories manifest within novel empirical contexts, specifically. In this study, this approach was applied to frontline nursing practice during the COVID-19 pandemic. The use of a deductive method ensured comprehensive coverage of each theoretically relevant dimension and facilitated the rapid translation of findings into actionable recommendations for future crises. Methodological reviews emphasize that framework-based coding enhances analytical transparency and efficiency when the goal is to validate or extend existing theory27; conversely, methodologies that are purely inductive are more appropriate for researchers investigating previously unexplored phenomena28.
Results
The results for each of the four phases are presented under two themes: individual functioning and team/organisation functioning.
Individual functioning in crisis was described according to the classic crisis response model adapted for the medical sector23. Team and organisation functioning during crisis were described following Jaques’ crisis management phases16.
This method of data presentation was chosen because hospital wards operate as complex systems in crisis, where individual behaviours influence others29 and are shaped by organisational structures30. Therefore, focusing solely on either the individual or the team/organizational level would oversimplify the material and risk presenting an incomplete picture. Moreover, the relationship between the employee and their social group is found as interactive31.
Reactions of nurses at the stage of preparation for the implementation of change during the COVID-19 pandemic
At the individual level the classic model highlighted concerns about the lack of information, the personal circumstances, and the process of implementing change (e.g. “The first few weeks were total chaos, everyone was so stressed. It was one big stress. Later it turned out that we can live with it. It can even be introduced quite nicely. Everyone paid attention to it. But the beginnings were, so to speak, mega-stressful”; “The beginning was difficult. These regulations were passed verbally at the beginning. They were written somewhere. It changed from hour to hour. What was current during one duty was outdated during another”; “I think every new thing that has been introduced has been accompanied by stress. And it is a lot of stress. At the very beginning certainly. There was no information, either in the media or elsewhere, about what all the work was supposed to look like. All procedures were introduced day by day and updated day by day, so going into duty you had to find out what had changed, how what had improved.”). At this stage, the nurses’ responses mirrored those outlined in the classic model: a need for information, concern about the personal situation, and uncertainty about how the changes would be implemented. During the preparation phase, emotional responses such as shock and mobilisation were triggered primarily by information gaps and personal uncertainty rather than formal procedural changes. The model illustrates how organizational effectiveness temporarily declined even before structured implementation began.
The presence of ‘classic’ concerns in responses to interview questions (3–9) is confirmed by the word map, which represents statements related to the preparation and the initial period of change implementation (question 8 of the interview). Notably, the spotlight also revealed concerns about a lack of knowledge during the early stages of the crisis. The word map in Fig. 3 shows that in the initial phase of the crisis, nurses most strongly associated their experiences with uncertainty (“know,” “procedures,” “beginning”), fear, and concerns about work and time. These keywords reflect a mix of emotional stress and practical challenges, highlighting both anxiety and the struggle to adapt to new procedures quickly.
During the initial phase of the COVID-19 pandemic, nurses experienced anxiety and uncertainty related to admitting the first patient and entering areas where infected individuals were being treated.
At the organisational level, similar concerns were observed—such as (lack of information, personal circumstances, challenges in implementing change. However, references to organisational functioning during COVID-19 pandemic appeared more frequently than those described in the classic model. The employees perceived the situation of uncertainty and preparation as organisational chaos, primarily resulting from ward restructuring and the inconsistent implementation of new procedures. Interview data suggested that the issue lay less in the clarity of the procedures themselves described by nurses as clear and more in their constantly changing nature. The perceived sense of chaos stemmed from how procedures were introduced particularly the emergence of conflicting information. In some cases, procedures changed within a single shift, requiring immediate updates to the following team.
Reactions of nurses at an early stage of the implementation of the change during the COVID-19 pandemic
At the individual level, the model reflected concerns during the early implementation stage related to personal circumstances, the way the change was introduced, and its long-term consequences. As depicted in Fig. 4, the early phase of change implementation triggered a range of emotional states among nurses, from shock and contradiction to withdrawal and eventual mobilisation. This figure focuses on the early implementation stage of change, showing how nurses experienced a rapid sequence of emotional responses—shock, contradiction, mobilisation, and partial adaptation—amid frequent procedural changes. It highlighted how fear and uncertainty dominated initially but were gradually met with efforts to adjust despite the instability. It clearly showed how early doubts were tied primarily to personal disruption and uncertainty about the new procedures.
Modified model of response to crisis based on the Blanchard model: doubts arising during the phase of (early) change implementation21,23. Diagram adapted to illustrate emotional and behavioural reactions of nurses during the early implementation of COVID-19-related organisational changes. Based on qualitative interviews conducted in 2021 with 26 nurses from the University Hospital in Krakow. This model reflects empirical findings such as fear, uncertainty, mobilisation, adaptation in the face of rapidly changing procedures.
Regarding the functioning of individual employees in the COVID-19 pandemic, nurses were concerned about working conditions under crisis, particularly the frequent procedural changes, and reported a lack of support from those typically expected to offer guidance in such situations (e.g., infection prevention nurses, doctors). The data from interviews did not reveal signs of denial regarding situation at this stage. According to the classic triad of crisis response symptoms (shock, denial, mobilisation) only shock and mobilisation were reported in the early implementation stage. For example, participants stated: “Certainly it was a fear for one’s own health”, ‘A lot of stress and many unknowns’ and ‘At first, you know everyone was afraid’, ‘At first, I was very worried, because I didn’t know what was what, how it will spread, what complications will be”; “It was hard at first, but I can’t say what specifically, because it blurs over time. Day by day, life goes on.”; “it seems to me that it is probably not entirely dependent on emotions. As if this initial fear translated into the fact that we were very thorough, very careful how we undressed, etc., and over time it became such a mechanical activity and we did it quite quickly, much faster than at the beginning”; “the emotions were subsiding. It became more and more natural. With time, emotions decreased. The work was easier. It was peaceful.” The lack of denial was accompanied by a clear awareness of the seriousness of the situation, expressed, for instance, by fearing for the lives of loved ones and concerns about potentially infecting them through contact with hospital materials. At both the individual and interpersonal levels, attitudes toward nurses from other departments were reported to have improved. There was a noticeable reduction in conflicts and an increase in mutual support among nurses working in the COVID-19 ward (e.g. “I think that when someone needed such support, they usually knew how to organise it. Rather, in the sense that she personally went to someone who could answer the question. There were also occasional staff meetings or online meetings.”; “I thought it was great and nothing else was needed. We really had a nice team, and we worked well and one for the other could always count”).
At the organisational level, the universal model reflected the same concerns about personal circumstances and the implementation of change. However, it included more frequent references to organisational functioning during COVID-19 pandemic than the classic model. The functioning of the organisation during the pandemic revealed the consequences of decisions made during the preparation phase. Participants primarily highlighted negative aspects, including:
-
The minimal presence or complete absence of an infection prevention nurse, despite expectations for such support.
-
Over time, nurses reported no longer needed help from an infection prevention nurse and began to perceive their occasional presence as a cause for concern
-
A sense of arbitrariness and urgency in assigning nurses to the COVID-19 ward was reported, resulting from frequent rotations between wards. Nurses reported feeling overwhelmed by the constant need to onboard new staff in the COVID-19 ward and to adjust the work habits of nurses transferred from other COVID wards—challenges stemming from high staff turnover. A belief that the team’s functioning deteriorated due to the inconsistent presence of doctors outside the COVID-19 patient zone.
-
Ward overcrowding, a shortage of prepared beds, and the need to seek patient placements in other facilities.
Reactions of nurses at a later stage of implementation of the change during the COVID-19 pandemic
At the individual level, within the classic model, employees expressed concerns about the long-term consequences of the change and the degree of cooperation during its implementation. (e.g. “They influence so that I still know I have to follow these rules and procedures. On the other hand, it irritates and frustrates me that people do not follow these rules because they think they are medical people in our group, if they do not want to follow these rules”; “Some impact it certainly had, but despite this stress, no one gave up on procedures. The duties were becoming mentally heavier. But it was a stress-based burden, more emotional”).
During the COVID-19 pandemic, nurses expressed concerns about excessive working hours under the current system and a perceived lack of appreciation from management. Although there were signs of adaptation and adjustment to the situation, there was also a growing sense of non-acceptance. This suggests (again) a divergence from the classic crisis response model, where acceptance and adaptation typically occur simultaneously at this stage. At this stage nurses progressed through emotional and behavioural responses to change, moving from initial shock and withdrawal toward adaptation and eventual internalization. It also contextualizes their evolving doubts—from personal uncertainty to broader concerns about cooperation and long-term consequences.
The following word map (Fig. 5; responses to question 9 of the interview) revealed a change in attitude. Emphases on fears and knowledge were reduced, while those related to work and patients emerged. Figure 5 shows that during the later phase of change implementation, nurses’ focus shifted toward patients, work, and adapting to the situation (“got used,” “time,” “emotions”). While fear and uncertainty remained, nurses placed a stronger emphasis on practical aspects of patient care and on coping with ongoing challenges. This may indicate that concerns related to the first and second phases of the crisis response were fading, where concerns about lack of information dominated. With reduced anxiety, nurses were able to refocus on their work and patient (“it’s a little easier now, a person gets used to a given situation a bit at a certain moment. It seems to me that a person is getting used to the situation as it is”; “I guess it was looser, less fear, less fear of getting infected because it was more adapted”; “Of course, you just got used to any situation. The greatest fear was that even a man was not afraid of work, the only fear was not to infect his loved ones.”; “It was quiet. After so many months, a person already knows how to proceed. It is easier and faster for us to do it”).
It is worth emphasizing that, at the level of individual accounts, the findings showed that nurses experienced a sense of stabilization and task focus, even in the face of feeling unrecognized by management.
At the team and organizational level, we observed a shift toward routine, procedure-based work. However, this transition was accompanied by negative emotions such as anxiety and stress.
At the organisational level, the universal model reflected the same concerns as at the individual level specifically regarding the long-term consequences of the change and the scope of cooperation in its implementation. However, references to organisational functioning during the COVID-19 pandemic were more frequent than in the classic model. In the context of pandemic functioning, a clear adaptation is evident, characterized by the accelerated resolution of immediate challenges and the systematic reorganisation of work processes to enhance operational efficiency and optimise structural arrangements (e.g., the implementation of airlock rooms). This more efficient organisation of work was accompanied by a growing sense of conflicts among nurses.
During the same period, at the team/organisation level, we observed that working according to procedures was becoming an emerging routine (Fig. 6). Figure 6 indicates that in the later stage of change implementation, team and organisational discussions centered heavily on “procedures,” “work,” and “thinking” about rules and processes. There was an ongoing cognitive engagement with how to adapt and comply, alongside mentions of stress, anxiety, and the impact on both people and patient care. The process mirrored what was observed at the individual level (Fig. 5).
At the same time, issues related to team relationships gained importance. This was reflected not only in direct statements (e.g. “We have a good team, but we also don’t have problems with it, we supported each other”; “We supported each other, we kept our spirits up. If it were not enough, it would be hard. We got even closer through this period.”), but also in the mental map associated with this stage of functioning (Fig. 6). It showed many concepts related to relationships, such as “people,” “person,” “stress,” and “speaking.” These terms did not directly indicate conflict but may reflect discussions about pandemic-related issues. Based solely on the mental map, there was no clear increase in conflicts, but rather a heightened emphasis on employee relations and negative emotions, which were not necessarily linked to interpersonal issues. However, individual statements indicated explicit occurrences of conflict, including frustration resulting from persistent misunderstandings and inconsistent information between shifts, which contributed to confusion and interpersonal tensions among nurses (e.g. “We were getting a little frustrated with the whole situation due to these constant misunderstandings. It was this way, that way, and there was hardly anyone keeping up. I don’t know if there was a person who knew which procedure was up to date. One person would get angry with another because depending on what shift she was on, different information was given to her. Mostly it was chaos.”).
Reactions of nurses at the stage of consolidation of the change (wave of the COVID-19 pandemic retracting)
At the level of the individual during the consolidation stage of the classic change model, concerns arose regarding the extent of cooperation in implementing the change and the potential to enhance its outcomes. These concerns related to how the system functioned after the change was completed and/or once it had reached a level of efficiency often exceeding that before the change process began. In nurses’ universal model, the concerns focused on the ability to independently sustain effective practices established during the change implementation.
Regarding nurses’ functioning during the COVID-19 pandemic, both positive and negative signals were observed. Positive signalsappeared predominantly at the individual level, while negative signals were more evident at the organisational level. At the individual level, positive signals included adaptation to procedures required for operating a medical facility during the COVID-19 pandemic and recognition of infection prevention protocols as valuable standards applicable across wards (“Well-introduced procedures worked later, we had everything organised so that we had all the containers provided for transport, we also put everything in bags where there was no contact, we had everything prepared, so everything was fairly efficient later”; “It seems to me that what is working now is okay. Man got used to it, knows how to proceed and it should stay as it is.”). Nurses recognized the value of wearing masks and adhering to hand hygiene. Anti-infection procedures were perceived positively and considered indispensable standards, regardless of position within the medical institution. Employees repeatedly emphasized the crucial role of anti-infection measures, both for workplace safety and for protecting their family members. (“I think that it is sure to secure personal protective equipment, spatial isolation, and that it should be so simply refined that there would be no contacts between the dirty / clean wards. It was not fully organised in all departments, also at our place.”; “What is there is sufficient. Certainly, there should be enough protective equipment—I would like to see that in all wards, not just a select few. If there were a pandemic, these procedures are sufficient. When negative feedback did arise, it was sporadic and focused on specific issues such as safety footwear or overall sizing. Nevertheless, these concerns were generally viewed as minor and not detrimental to work. Thus, negative remarks were often tempered by more neutral or mitigating comments. (“To increase disinfectants at multiple points. That dispensers were available. Mandatory masks. Depends on how this develops”; “The point is to approach and take care of the patient, not to deal with the organisation of the ward, and then and the patient is waiting, because it is unacceptable. No probably not. These are just organisational issues, but yes, there were no such practices or procedures to get in the way.”).
At this stage, individual employees accepted and internalized the procedures, viewing them as essential to their work. They were not only seen as necessary within their own units but also recommended for broader adoption across the facility. Importantly, procedures were regarded as vital for protecting nurses’ families. In their reflections, employees often downplayed or rationalized the more difficult aspects of working under pandemic-related pressure and organizational change.
At the organisational level, the universal model reflected concerns similar to those at the individual level, specifically regarding cooperation during change implementation and enhancement of its outcomes. However, negative statements accumulated and outweighed positive ones. On the positive side, clear statements about good work organisation, hygiene measures, and the reasonable procedures in the facility can be noted. Negative statements included fatigue and exhaustion, concerns about duty division after COVID, apprehension regarding current working hours, and feelings of underappreciation by management outside the COVID-19 patient zone.
We propose a structured roadmap (Table 1) to guide organisations in managing change implementation and stakeholder engagement during crises. This roadmap outlines each stage employees face during challenging situations, grounded in our study findings and aligned with the Blanchard23 and Jaques16 models. The roadmap identifies key focus areas at each stage of crisis management, facilitating more effective organisational change. The main insight from the Table 1 is that during the COVID-19 pandemic, planned crisis management strategies often gave way to uncertainty, frequent procedural changes, and perceptions of “organizational chaos.” While some positive adaptations emerged over time—such as acceptance of anti-infection measures—initial phases were marked by anxiety, lack of support, and disruption to team cohesion, with early unity eroding into conflicts in later stages.
Discussion
The results outlined the adaptation process within the nurses’ community during the COVID-19 pandemic. At the individual level, the analysis of nurses’ statements suggested that the principles of the tested model were partially realized. On the organizational level, significant gaps were identified in early-stage crisis preparedness. Although organisational responses improved during the later stages, persistent stressors and a lack of recognition contributed to internal conflicts despite increased operational effectiveness.
The individual level
Phenomena identified by Blanchard23 were observed during preparation, implementation, and consolidation stages. However, no denial trend was found at the early implementation stage. Denial, a psychological mechanism rejecting threatening information32, was absent among nurses, indicating their awareness, sense of responsibility, and readiness to perform duties even in crises.
In the early phase of implementing change, integrating COVID-19-specific tasks was crucial for understanding individual experiences. Nurses faced uncertainty as they adapted to new working conditions, altering routines, and learning new tasks amidst rapid procedure updates. This uncertainty was heightened by health fears for themselves and their loved ones, especially for those in direct contact with COVID-19 patients. Yet, this period also saw strong nurse mobilization and responsibility. As frontline workers, nurses recognized their vital role and diligently adopted new procedures through self-directed learning and mutual monitoring. Consequently, new pro-social behaviors developed, and team bonds strengthened.
Sustained demands on resilience, heavy workloads, and emotional stress from patient deaths and reduced interactions with non-health staff likely led to exhaustion, job uncertainty, and health issues. This may have impaired their ability to maintain health under ongoing stress. Our research on SARS-CoV-2 incidence among general hospital staff before vaccines5 found nurses especially vulnerable. Despite similar protection protocols, most COVID-19 cases were in nurses. The high SARS-CoV-2 antibody rates in nurses at UHK suggest that work strain weakened their immunity. This supports the stress response model, where prolonged stress depletes resources, lowers immunity, and increases illness risk—even with proper infection prevention.
Polish nurses’ experiences during the pandemic mirrored those of nurses globally, experiencing anxiety and high stress regardless of direct or indirect COVID-19 patient care. In Finland33, changes in routines raised anxiety. In Taiwan22, stress was tied to increased patient responsibility and procedural discomfort. In Brazil34,35, fears stemmed from the unknown, care changes, and reduced PPE availability. Italian nurses faced similar stressors in early pandemic days35. Other studies confirm high stress in this group. Researchers suggest stress management training, counselling, and recognizing healthcare workers’ efforts13,14,36. These interventions also combat emotional burnout and are part of support programs12. Nurses in our study expressed these needs: “I would like someone to appreciate us sometimes, this work, and praise us.”; “I think fix some things in advance.”; “There were some emails about being able to use psychological support, but… you had to make an effort to get it.”
On the other hand, another Italian study37, suggests that stress and fatigue during the pandemic year may have influenced the evaluation of hospital procedures; however, our research does not support this conclusion. Nurses who were consistently present at patients’ bedsides and had to rigorously follow procedures found them demanding but developed a generally positive attitude toward these changes, expressing a strong desire to continue practices that enhance their personal safety.
Moreover, adding to the above, Kato et al.15 mentions developing skills such as teamwork (job resources) as a factor that improves work engagement among nurses. This also contributes to an increase in personal resources15. Our study confirms that during the stages of crisis management, teamwork and improvement of personal resources can support adaptation to change and better management in a difficult situation and creates psychological safety (“We supported each other, we maintained our spirits up. If it were not enough, it would be hard. We got even closer through this period.”; “There was good cooperation in the team. We looked out for each other”; “We just talk to each other, yeah? And so, mentally, we just build ourselves up, and we also stand behind ourselves”).
The experiences of Polish nurses during COVID-19 reflect international research on emotional labour. Yildiz and Altun38 found higher levels of surface acting in pandemic wards, indicating more emotional strain. Similarly, Yalçın et al.39 linked genuine emotional engagement with lower depersonalization and burnout. Our observations align, noting increased pro-social behaviour and team bonds, suggesting authentic emotional expression is protective.
Psychological resilience helps manage pandemic-related emotional demands and reduces burnout risk in nurses, as found by Pu et al.40 Our study reveals a strong need for psychological support and institutional recognition, emphasizing the importance of resilience and coping strategies. Not all emotional labour is adaptive; Diogo et al.41 show suppressed emotions can lead to exhaustion. This aligns with our findings of emotional numbness and lack of support, highlighting the need for systemic changes to prevent long-term harm among healthcare workers.
The organisational level
We studied organisational change across four phases. In the first phase, preparation, nurses experienced chaos due to altering procedures and conflicting information during the COVID-19 pandemic. The early implementation phase revealed high nurse turnover and overcrowding, with a continued sense of chaos and poor communication. Nurses faced random reassignments and perceived control rather than support from infection prevention nurses. During late implementation, nurses slowly adapted with improved reorganisation, although interpersonal conflicts arose. In the final phase, consolidation, while protection measures and improved procedures were valued, fatigue, demotivation, and undervaluation were common concerns.
Organisational readiness to manage change during the COVID-19 crisis was reflected in several key factors. These included the availability of protective measures, the ability to adapt and refine operational procedures, and strong mutual support within teams. These elements created a foundation for navigating the uncertainty of the pandemic and helped maintain a basic level of stability. However, despite these strengths, several critical support mechanisms were lacking—particularly clear and consistent communication from upper management. While most participants noted the absence of top-down guidance, they consistently emphasised the vital role played by ward nurses. These individuals served not only as coordinators but also as emotional and logistical anchors during the crisis. Their efforts highlight how mid-level leadership can compensate for organisational deficiencies and maintain operational coherence under pressure.
The CAS perspective expands leadership beyond hierarchy, emphasising dynamic problem-solving, feedback loops, and adaptive behaviours such as informal learning and flexible routines4. This lens helps explain why mid-level leadership and team initiative were crucial for resilience during the crisis. Our data supports this systems view, showing the need for leadership skills addressing team and broader organisational concerns. The CAS cycle, detailed by Choflet et al.42, includes seeing the system, regulating distress, uniting people, iterative experimentation, and encouraging leadership at all levels, enhancing institutional flexibility and resilience in future crises. The CAS lens helps interpret the emergence of adaptive behaviors, such as informal learning and flexible routines, especially during the mid and late stages (see Sections “Reactions of nurses at an early stage of the implementation of the change during the COVID-19 pandemic”–“Reactions of nurses at a later stage of implementation of the change during the COVID-19 pandemic”). Unlike linear models, CAS accounts for feedback loops and self-organization.
Further support for this systemic approach comes from a study by Heikkilä et al.43, which underscores the role of supervisor practices in managing organizational change. Their research highlights how supervisor competence—especially in communication, education, and practical know-how—can reduce stress (including “stress of conscience”) among nurses and create a more collaborative, less hierarchical culture of change.
These insights converge on a central theme: the quality of communication—both horizontal and vertical—is crucial. Strengthening communication between management and front-line workers may reduce feelings of isolation and abandonment among nurses. This aligns with our findings, where participants frequently reported a sense of being “left alone” during the most intense phases of the pandemic. Addressing this disconnect through inclusive leadership and improved dialogue could foster a more responsive and supportive organizational culture in future emergencies44.
Key factors essential for organisational learning are equally important in the context of nursing. For instance, Lyman et al.45 identified several contextual factors that limit organisation’s capacity for learning—findings that resonate, to some extent, with the results of our study involving nurses. These factors encompass psychologically safe relationships, a shared sense of purpose and motivation, adequate infrastructural support, and collective team experience.
Psychologically safe relationships are crucial for organisational learning, influencing collaboration and support27. In our study, nurses valued colleague support, especially in stable teams. High turnover, however, reduced this sense of safety and led to more conflicts. However, high turnover reduced this safety, increasing conflicts. Lyman et al.45 found adequate infrastructure crucial, impacting organisational adaptation during COVID-19, aligning with our findings. Challenges included high nurse turnover, low patient beds, COVID-19 exposure, and inadequate staffing, leading to burnout and retraining interest. Lyman et al.45 also noted turnover harmed cooperation and help-seeking, increasing conflicts and slowing organisational learning.
Recent investigations have emphasized the significance of organizational climate within healthcare contexts during the COVID-19 pandemic. A qualitative investigation into nurses’ experiences in COVID-19 intensive care units identified a “positive climate of attachment and professional commitment,”46; p. 175 wherein nurses exhibited a profound commitment to delivering quality care despite adversities. This supportive environment, characterized by multidimensional support from patients, families, team members, and community entities, was pivotal in alleviating emotional stress and promoting resilience among nurses46.
Additionally, the notion of organizational emotional climate, which involves shared perceptions of emotional experiences within workplace settings, has been associated with the well-being and performance of nurses. An investigation assessing the correlation between organizational climate and nurses’ intention to remain identified that a positive emotional climate, in conjunction with supportive leadership, significantly diminished turnover intentions. These findings concur with our observations, wherein supportive team interactions and acknowledgment from leadership were instrumental in enhancing nurses retention and morale47.
In our study, the three frameworks complemented each other by offering distinct but interconnected insights. Jaques’ model highlighted the temporal sequence of crisis management phases. Blanchard’s model illuminated the emotional and cognitive dynamics within each phase. The Complex Adaptive Systems (CAS) perspective provided a system-level lens, capturing how adaptive behaviours such as informal peer leadership and flexible routines emerged through feedback loops and self-organisation. Taken together, these models outline a temporal–emotional–systemic understanding of how nurses and organisations navigated the COVID-19 crisis.
Conclusions
This study aimed to explore the unique functioning of nurses during the multifaceted crisis of the COVID-19 pandemic from their own perspective and to offer actionable insights at both individual and organisational levels. At the individual level, nurses demonstrated a distinctive adaptation pattern that diverged from some theoretical expectations. Rather than denying the crisis, most participants showed early acknowledgment of its severity, coupled with a strong sense of responsibility. As the pandemic progressed, their coping strategies evolved into delayed acceptance and active adaptation, accompanied by increasing emotional strain and interpersonal tensions.
At the organisational level, we identified significant gaps in early-stage crisis preparedness, particularly concerning unclear communication, procedural instability, and the undervalued role of infection control teams. Although organisational responses improved during the later stages, persistent stressors and a lack of recognition contributed to internal conflicts despite increased operational effectiveness. These findings highlight the critical importance of institutional learning, stakeholder acknowledgement, and proactive crisis training.
The nurses’ response to the pandemic highlights the critical need for organisational learning to better prepare for future crises. Table 1 presents both the findings from this study and anticipated outcomes, serving as a roadmap to enhance crisis and change management within the organisation. It outlines key focus areas for each phase, guiding efforts to improve effectiveness across organisational structures.
Based on the findings of our study, we recommend the following essential steps:
-
1.
Thoroughly complete Phase 1 of the Jaques model, focusing on team and organisational functioning. This includes reviewing planning processes, systems, and manuals; conducting training simulations (such as establishing ownership, resource allocation, testing, and live simulations); implementing intervention programs; and providing ongoing psychological assessment and support.
-
2.
Preparation should specifically address the infection syndrome relevant to each medical unit. Infection team training must be integrated into the annual schedule, covering not only hygiene standards but also the medical facility’s overall response to infection crises.
-
3.
These findings indicate that, before the crisis, there was a lack of effective internal communication promoting the infection syndrome and the infection team’s role in the medical unit’s crisis response. Consequently, nurses initially distanced themselves from infection team members, sometimes viewing them as disruptive or threatening. This likely reflects limited familiarity with the infection team’s functions in both crisis and routine contexts.
Without proactive preparation, crisis situations trigger frequent changes in procedures, which in turn compound the negative consequences of inadequate planning. This lack of preparedness manifests in numerous organizational challenges during the pandemic, underscoring that the difficulties faced are largely rooted in insufficient actions taken during the preparation phase.
When the crisis / change is under control (late implementation and beyond), it becomes essential to address the human dimension of teamwork. The Jaques model mentions stakeholder management, our findings suggest that attention must extend beyond external stakeholders to include internal ones—specifically, employees who frequently reported feeling undervalued.
During this phase of crisis management / implementation of changes, it is valuable to foster a “founding myth” that celebrates the medical facility’s successful navigation of the COVID-19 crisis. Such a narrative can serve to recognize and appreciate the efforts of employees involved in the response, while also promoting the positive behaviours and attitudes that proved effective during the crisis.
Failure to adequately care for employees (stakeholders within the organisation according to the Jaques model) creates a paradox: the organisation manages challenges effectively, yet employees experience increased conflicts and misunderstandings.
Moreover, it is important to consider the characteristics of the department or team, as this can impact both organisational structure and team performance48. Based on our findings, while some organisational practices and employee attitudes may be broadly applicable, their effectiveness can be constrained by the unique context of the department in which a team operates.
In summary, this research addresses its central inquiry by demonstrating that nurses navigated the crisis through a complex interplay of professional dedication, emotional labour, and adaptive teamwork. Concurrently, organisational systems exhibited uneven development, revealing critical insights and lessons that can inform and enhance future pandemic preparedness and strategies for workforce support.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- IDI:
-
Individual deep interview
- UHK:
-
University hospital in Kraków
References
Durlak, U. et al. Is antimicrobial stewardship policy effectively implemented in polish hospitals? Results from antibiotic consumption surveillance before and during the covid-19 pandemic. Antibiotics 13, 636 (2024).
Wałaszek, M., Kołpa, M., Wolak, Z., Różańska, A. & Wójkowska-Mach, J. Poor hand hygiene procedure compliance among polish medical students and physicians-the result of an ineffective education basis or the impact of organizational culture?. Int. J. Environ. Res. Public Health 14, 1026 (2017).
Wałaszek, M. et al. Ventilator-associated pneumonia in Polish intensive care unit dedicated to COVID-19 patients. BMC Pulm. Med. 23, 443 (2023).
Żółtowska, B. et al. Preparedness of health care workers and medical students in university hospital in Krakow for COVID-19 pandemic within the CRACoV project. J. Clin. Med. 10, 3487 (2021).
Żółtowska, B. et al. The Seroprevalence of SARS-CoV-2 antibodies among healthcare workers in university hospital in Krakow before the era of vaccination. Int. J. Environ. Res. Public Health 19, 4044 (2022).
Holton, S. et al. Australian and Danish nurses’ and midwives’ wellbeing during COVID-19: A comparison study. Collegian 29, 281–287 (2022).
De Bono, S., Heling, G. & Borg, M. A. Organizational culture and its implications for infection prevention and control in healthcare institutions. J. Hosp. Infect 86, 1–6 (2014).
Bittner, J. G., Khan, Z., Babu, M. & Hamed, O. Stress, burnout, and maladaptive coping: Strategies for surgeon well-being. Bull. Am. Coll. Surg. 96, 17–22 (2011).
Le Blanc, P. M., Bakker, A. B., Peeters, M. C. W., van Heesch, N. C. A. & Schaufeli, W. B. Emotional job demands and burnout among oncology care providers. Anxiety Stress Coping 14, 243–263 (2001).
Xanthopoulou, D. et al. When do job demands particularly predict burnout?: The moderating role of job resources. J. Manag. Psychol. 22, 766–786 (2007).
Mäkikangas, A. & Kinnunen, U. Psychosocial work stressors and well-being: Self-esteem and optimism as moderators in a one-year longitudinal sample. Personal. Individ. Differ. 35, 537–557 (2003).
Barello, S. et al. Factors associated with emotional exhaustion in healthcare professionals involved in the COVID-19 pandemic: An application of the job demands-resources model. Int. Arch. Occup. Environ. Health 94, 1751–1761 (2021).
Parveen, F., Abdullah, N., Syed, T. R. & Haqqani, Q. A. Psychological impact of COVID-19 on nurses working at institute of urology & transplantation; A cross-sectional study. Mirpur J. Med. Sci. 1, 14–19 (2023).
Tomo, A. & De Simone, S. Using the job demands-resources approach to assess employee well-being in healthcare. Health Serv. Manag. Res. 32, 58–68 (2019).
Kato, Y., Chiba, R. & Shimazu, A. Work engagement and the validity of job demands-resources model among nurses in japan: A literature review. Workplace Health Saf. 69, 323–342 (2021).
Jaques, T. Issue management and crisis management: An integrated, non-linear, relational construct. Public Relat. Rev. 33, 147–157 (2007).
Reeves, M., Veeken, R. van der & Job, A. Has Your Organization Acted on What It’s Learned in the Pandemic? Harvard Business Review (2023).
Maitlis, S. Who am I now? Sensemaking and identity in posttraumatic growth. In Exploring Positive Identities and Organizations. Building a Theoretical and Research Foundation (eds Morgan Roberts, L. & Dutton, J. E.) 47–76 (Routledge Taylor & Francis Group, New York, 2009).
Duchek, S. Organizational resilience: A capability-based conceptualization. Bus. Res. 13, 215–246 (2020).
Hashemi, H., Rajabi, R. & Brashear-Alejandro, T. G. COVID-19 research in management: An updated bibliometric analysis. J. Bus. Res. 149, 795–810 (2022).
Rosiński, J. Wdrażanie zmiany postaw personelu w placówce medycznej. In Zakażenia szpitalne w jednostkach opieki zdrowotnej (eds Bulanda, M. & Wójkowska-Mach, J.) 541–554 (Wydawnictwo Lekarskie PZWL, 2016).
Kuo, F. et al. Survey on perceived work stress and its influencing factors among hospital staff during the COVID-19 pandemic in Taiwan. Kaohsiung J. Med. Sci. 36, 944–952 (2020).
Blanchard, K. Leading at a Higher Level: Blanchard on Leadership and Creating High Performing Organizations. 3rd edition, Pearson Education; 2016. ISBN-10: 0134857534, ISBN-13: 978–013485753
Hennink, M. & Kaiser, B. N. Sample sizes for saturation in qualitative research: A systematic review of empirical tests. Soc. Sci. Med 292, 114523 (2022).
Hsieh, H.-F. & Shannon, S. E. Three approaches to qualitative content analysis. Qual. Health Res. 15, 1277–1288 (2005).
Assarroudi, A., Heshmati Nabavi, F., Armat, M. R., Ebadi, A. & Vaismoradi, M. Directed qualitative content analysis: the description and elaboration of its underpinning methods and data analysis process. J. Res. Nurs. 23, 42–55 (2018).
Elo, S. & Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 62, 107–115 (2008).
Bonner, C. et al. Comparing inductive and deductive analysis techniques to understand health service implementation problems: A case study of childhood vaccination barriers. Implement. Sci. Commun. 2, 100 (2021).
Cialdini, R. B. Influence: The Psychology of Persuasion. (Harper Collins, 2009).
Hersey, P., Blanchard, K. H. & Johnson, D. E. Management of Organizational Behavior: Leading Human Resources. (Pearson, 2013).
Jia, L., Shaw, J. D., Tsui, A. S. & Park, T.-Y. A social-structural perspective on employee-organization relationships and team creativity. AMJ 57, 869–891 (2014).
Dorpat, T. A new look at denial and defense. Annu. Psychoanal. 15, 23–47 (1987).
Mattila, E. et al. COVID-19: Anxiety among hospital staff and associated factors. Ann. Med. 53, 237–246 (2021).
Santos, J. L. G. D. et al. Work environment of hospital nurses during the COVID-19 pandemic in Brazil. Int. Nurs. Rev. 68, 228–237 (2021).
Bagnasco, A., Zanini, M., Hayter, M., Catania, G. & Sasso, L. COVID 19-A message from Italy to the global nursing community. J. Adv. Nurs. 76, 2212–2214 (2020).
Alwesmi, M. B., Dator, W. L. & Karavasileiadou, S. Lived experiences of female nurses with COVID-19 deaths on their watch. Behav. Sci. 12, 470 (2022).
Magnavita, N., Soave, P. M. & Antonelli, M. A one-year prospective study of work-related mental health in the intensivists of a COVID-19 hub hospital. Int. J. Environ. Res. Public Health 18, 9888 (2021).
Yildiz, T., Erden, D., Malak, A. & Avcu, C. Covid-19 era: How does it affect nurses’ emotional labor behavior and burnout levels?. Int. J. Caring Sci. 16, 555–562 (2023).
Yalçın, B., Sarıköse, S., Göktepe, N. & Türkmen, E. The relationship between nurses’ demographic work-related variables and emotional labor behavior on nurse burnout during the COVID 19 pandemic. BMC Health Serv. Res. 25, 528 (2025).
Pu, J. et al. Psychological resilience and intention to stay among nurses: The mediating role of perceived organizational support. Front. Psychol. 15, 1407206 (2024).
Diogo, P. M. J., Sousa, M. O. C. L. E., Rodrigues, J. R. G. V., Silva, T. A. A. M. A. E. & Santos, M. L. F. Emotional labor of nurses in the front line against the COVID-19 pandemic. Rev. Bras. Enferm. 74(Suppl 1), 20200660 (2021).
Choflet, A., Packard, T. & Stashower, K. Rethinking organizational change in the COVID-19 era. J. Hospital Manag. Health Policy 5, (2021).
Heikkilä, M., Huhtala, M., Mauno, S. & Feldt, T. Intensified job demands, stress of conscience and nurses’ experiences during organizational change. Nurs. Ethics 29, 217–230 (2022).
Arcadi, P. et al. Nursing during the COVID-19 outbreak: A phenomenological study. J. Nurs. Manag. 29, 1111–1119 (2021).
Lyman, B., Horton, M. K. & Oman, A. Organizational learning during COVID-19: A qualitative study of nurses’ experiences. J. Nurs. Manag. 30, 4–14 (2022).
Khorasani, P., Ebrahimi, A., Andalib, S., Ahmadi, M. & Moosavi, S. M. H. Organizational climate of the COVID-19 intensive care units: A qualitative content analysis study. J. Caring Sci. 12, 174–180 (2023).
Hossny, E. K. et al. Influence of nurses’ perception of organizational climate and toxic leadership behaviors on intent to stay: A descriptive comparative study. Int. J. Nurs. Stud. Adv. 5, 100147 (2023).
Fagerdal, B., Lyng, H. B., Guise, V., Anderson, J. E. & Wiig, S. No size fits all – a qualitative study of factors that enable adaptive capacity in diverse hospital teams. Front. Psychol. 14, 1142286 (2023).
Author information
Authors and Affiliations
Contributions
MKL: participation in the design of the research model, participation in the design of the research tool, conducting research (interviews), participation in the analysis of the research material, integration of the interpretative part of the collected data, final editing of the text JR: participation in the design of the research model, participation in the design of the research tool, participation in the analysis of the research material, integration of the interpretative part of the collected data, participation in the final editing of the text KG: participation in the design of the research model, participation in the design of the research tool, conducting research (interviews), participation in the analysis of the research material, participation in the final editing of the text. BŻ: participation in the design of the research model, organization of the research field and selection of the group of subjects, participation in the analysis of the research material, participation in the final editing of the text IB: participation in the design of the research model, organisation of the research field and selection of the group of subjects, participation in the analysis of the research material, participation in the final editing of the text AR: participation in the design of the research model, participation in the design of the research tool, conducting research (interviews), participation in the analysis of the research material, participation in the final editing of the text JWM: participation in the design of the research model, participation in the design of the research tool, participation in the analysis of the research material, integration of the interpretative part of the collected data, participation in the final editing of the text.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study involving human participants was conducted according to the guidelines of the Declaration of Helsinki and were reviewed and approved by the Bioethics Committee of the Jagiellonian University (protocol code 1072.6120.353.2020, date of approval 16.12.2020). Patients / participants provided their informed consent in writing to participate in this study. All methods were performed in accordance with the relevant guidelines and regulations of the approving institutions.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kossowska-Lai, M., Rosiński, J., Glomb, K. et al. Nurses crisis management during COVID-19 at individual and organizational levels in a qualitative single centre study in Poland. Sci Rep 15, 33705 (2025). https://doi.org/10.1038/s41598-025-18984-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-18984-x