Abstract
Sepsis is a leading cause of mortality among ICU patients. Although APACHE IV and SOFA scores are widely employed for prognostic assessment, their complexity and dependence on extensive data may limit their effectiveness in early risk identification. The MELD-XI score, derived from serum total bilirubin and creatinine, offers a simple calculation method and has demonstrated strong prognostic value in liver disease, organ transplantation, and cardiovascular conditions. However, its prognostic utility in ICU patients with sepsis has not been systematically evaluated. In this study, we retrospectively analyzed 16,691 adult patients diagnosed with sepsis within 48 h of ICU admission using data from the eICU Collaborative Research Database. Through the application of a generalized additive model and a two-stage linear regression model, we identified for the first time a significant nonlinear association and a threshold effect between MELD-XI scores and 30-day all-cause mortality. The turning point was determined at a MELD-XI score of 25.74, with mortality risk increasing by 1.1% per unit below the threshold and by 5.5% per unit above it. Stratified subgroup analyses confirmed the consistency of this association across most clinical categories. These findings suggest that the MELD-XI score may serve as a simple, accessible, and complementary tool for early risk stratification and clinical decision-making in ICU patients with sepsis.
Similar content being viewed by others
Introduction
Sepsis is the leading cause of death in ICU patients worldwide. In 2017, there were 48.9 million new cases of sepsis and 11 million sepsis-related deaths globally, representing 19.7% of all deaths worldwide1. Its high morbidity and mortality present significant challenges to healthcare systems. Early identification of high-risk patients is crucial in clinical practice for developing personalized treatment strategies, optimizing resource allocation, and improving patient prognosis.
The APACHE IV(Acute Physiology and Chronic Health Evaluation IV) and SOFA(Sequential Organ Failure Assessment) scores, commonly used in clinical settings, are essential tools for the prognostic assessment of sepsis2,3. However, their complexity and reliance on comprehensive data may result in delayed evaluation. In contrast, the MELD-XI(Model for End-Stage Liver Disease Excluding International Normalized Ratio) score4 is calculated using serum total bilirubin and creatinine, according to the formula: MELD-XI = 5.11 × ln(serum total bilirubin) + 11.76 × ln(serum creatinine) + 9.44 4,5. Both serum total bilirubin and creatinine are strongly associated with the prognosis of patients with sepsis6,7,8. The MELD score has been widely used to assess mortality risk and guide organ transplant allocation in patients with liver disease and has demonstrated high accuracy in predicting prognosis9,10 and mortality in conditions such as heart failure11. However, the relationship between MELD-XI scores and mortality in septic patients in the ICU remains insufficiently explored.
Therefore, based on data from the eICU Collaborative Research Database (eICU-CRD), this study examines the correlation between the MELD-XI score and the 30-day all-cause mortality rate in patients who developed sepsis within 48 h of ICU admission.
Methods
Data source
The data for this study were obtained from the eICU Collaborative Research Database (eICU-CRD), developed jointly by the Massachusetts Institute of Technology and Philips Healthcare12. This database includes clinical data from over 200,000 critically ill patients across 335 intensive care units in 208 hospitals in the United States, spanning from 2014 to 2015. It encompasses a wide range of variables, such as demographic information, vital signs, laboratory tests, diagnoses, treatments, and outcomes. Access to the database is granted only after completion of the Collaborative Institutional Training Initiative (CITI). The first author of this study (Jiehe Mai) obtained access to the eICU-CRD and was responsible for data extraction (certification number: 67879753). The security architecture of the eICU-CRD, independently evaluated by privacy experts (Privacert, Cambridge, Massachusetts), was certified as compliant with the Safe Harbor standard for re-identification risk (Health Insurance Portability and Accountability Act certification number: 1031219-2). Approval was waived by the Institutional Review Board of the Massachusetts Institute of Technology (Cambridge, MA, USA) for this retrospective study. Informed consent was also waived by the Institutional Review Board of the Massachusetts Institute of Technology (Cambridge, MA, USA) because only de-identified data were used.All operations followed the principles outlined in the Declaration of Helsinki and complied with the STROBE guidelines for observational studies.
Study population
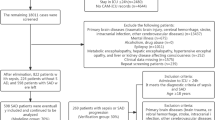
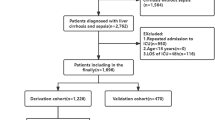
All relevant data for patients diagnosed with sepsis within 48 h of ICU admission were retrieved from the eICU Collaborative Research Database (eICU-CRD) using Structured Query Language (SQL). Inclusion criteria consisted of adult patients (age > 18 years) diagnosed with sepsis within 48 h of ICU admission. Sepsis was defined as suspected or confirmed infection combined with an acute increase in the Sequential Organ Failure Assessment (SOFA) score of ≥ 2 points13. The site of infection was identified using International Classification of Diseases, Ninth Revision (ICD-9) codes recorded in the eICU-CRD. Exclusion criteria included (1) Age ≤ 18 years, (2) Not the first ICU admission, (3) Length of hospital stay or ICU stay < 48 h, (4) Non-septic patients, (5) Patients diagnosed with sepsis more than 48 h after ICU admission, (6) Missing data on serum total bilirubin and creatinine within the time window from − 6 to 48 h after ICU admission. The flow chart of the study is shown in Fig. 1.
Variables
Baseline demographic information, including age and sex, was obtained from the patient form. Records of dialysis treatment in the medical history were used to identify patients with prior renal replacement therapy. Comorbidities—including congestive heart failure, cardiac arrhythmias, chronic lung disease, severe liver disease, renal failure, malignancy, and metastatic solid tumors—were extracted based on the APACHE IV scoring system. Septic shock was identified using diagnostic records. Severity of illness was assessed using the Glasgow Coma Scale (GCS), APACHE IV score, and SOFA score. Laboratory parameters included the peak values of total bilirubin, serum creatinine, and lactate levels within 48 h of ICU admission.
Scoring formula
The MELD-XI score was calculated using the following formula:
MELD-XI = 5.11 × ln (serum total bilirubin) + 11.76 × ln (serum creatinine) + 9.444,5. According to the United Network for Organ Sharing (UNOS) modification guidelines14, the lower limit for serum creatinine was set at 1.0 mg/dL and the upper limit at 4.0 mg/dL. Serum creatinine values for patients receiving preoperative dialysis were uniformly set at 4.0 mg/dL to ensure stability and comparability in MELD-XI scoring.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation (SD), and categorical variables were presented as frequencies and percentages. Patients were stratified into tertiles based on MELD-XI scores. One-way analysis of variance (ANOVA) was used to compare continuous variables across groups, and the chi-square test was applied for categorical variables. To evaluate the potential nonlinear relationship between MELD-XI score and 30-day all-cause mortality in ICU patients with sepsis, a generalized additive model (GAM) with a logistic regression link function was employed. The smoothing term was fitted using penalized cubic regression splines. This method avoids the need for a predefined functional form and enables flexible modeling of complex dose–response relationships. Confounding variables were selected based on prior association with mortality or a ≥ 10% change in effect estimate15. Adjusted covariates included ethnicity, age, septic shock, site of infection (lung, urinary tract, skin/bone/joint), history of dialysis, cardiac arrhythmia, severe liver disease, renal failure, malignancy, metastatic solid tumors, as well as APACHE IV score, SOFA score, GCS score, and lactate level. To further investigate potential inflection points in the relationship between MELD-XI score and mortality risk, a two-piecewise linear regression model was applied. The optimal turning point was determined using an iterative search method based on likelihood maximization. The log-likelihood ratio test (LRT) was used to compare the goodness-of-fit between a unilinear model and the segmented model. Odds ratios (ORs) for MELD-XI score below and above the inflection point were calculated separately, and 95% confidence intervals (CIs) were estimated using bootstrap resampling methods to assess effect differences across score intervals16. Stratified analyses were performed to evaluate the robustness of the findings. All statistical analyses were conducted using R software (version 4.2.0) and EmpowerStats (X&Y Solutions, Inc., Boston, MA).
To address missing values in key covariates, we used the predictive mean matching (PMM) algorithm from the mice package in R to perform five imputations for lactate (27.3%), APACHE IV (9.3%), and GCS (16.7%), all with missing rates below 30%. The pooled results were used for subsequent analyses to minimize potential bias.
Results
Basic characteristics
In this study, 16,691 adult patients with sepsis admitted to the ICU were included and categorized into three groups based on MELD-XI score tertiles: low (9.4–12.5), medium (12.5–21.5), and high (21.5–46) score ranges. The overall MELD-XI score was 17.69 ± 7.16. Statistically significant differences were observed among the three groups in terms of demographic characteristics, laboratory parameters, site of infection, disease severity, comorbidities, and 30-day mortality (all P < 0.001).
The high MELD-XI group had a greater proportion of male patients, significantly higher APACHE IV and SOFA scores, and lower Glasgow Coma Scale (GCS) scores. Laboratory tests revealed significantly elevated levels of total bilirubin, serum creatinine, and lactate in this group compared to the medium and low MELD-XI groups. In terms of infection site, abdominal cavity infections and septic shock were more common in the high MELD-XI group. Comorbidity analysis showed the highest prevalence of heart failure, severe liver disease, and renal failure in this group. Additionally, patients with a history of dialysis were only observed in the high MELD-XI group. The 30-day mortality rate was 20.27% in the high MELD-XI group, significantly higher than in the medium (16.69%) and low (11.32%) groups (P < 0.001). Detailed group characteristics are presented in Table 1.
Unadjusted association between baseline variablesand 30-day mortality
Each one-point increase in the MELD-XI score was associated with a 4% increase in the 30-day risk of death (OR = 1.04, 95% CI: 1.04–1.05, P < 0.0001). Using the lowest tertile group as the reference, the risk of death was higher by 57% in the middle tertile group (OR = 1.57, 95% CI: 1.41–1.75) and by 99% in the highest tertile group (OR = 1.99, 95% CI: 1.79–2.21), with all differences reaching statistical significance (P < 0.0001). Older age, elevated total bilirubin, serum creatinine, and lactate levels, as well as higher APACHE IV and SOFA scores, were associated with an increased risk of 30-day mortality. In contrast, higher GCS scores were significantly associated with a reduced risk of death (P < 0.0001). Pulmonary infections and septic shock were also linked to a higher risk of mortality. In contrast, skin/bone/joint infections (OR = 0.74, P = 0.0012) and a history of dialysis (OR = 0.71, P = 0.0006) were associated with lower mortality risk.
Comorbidities such as severe liver disease, malignant tumors, metastatic solid tumors, cardiac arrhythmias, and renal failure were significantly associated with an increased risk of death. Sex and most infection sites were not significantly related to mortality risk. Detailed results are presented in Table 2.
Multivariable logistic regression analyses in different adjustment models
Further multivariate analysis demonstrated a significant positive association between the MELD-XI score and 30-day all-cause mortality (Table 3). In the fully adjusted model, for every 1-point increase in the MELD-XI score, the risk of 30-day all-cause mortality increased by 2% (OR = 1.02, 95% CI: 1.01–1.02; P = 0.00019). Compared to the lowest MELD-XI tertile (T1), the 30-day all-cause mortality rate in the highest tertile was 23% higher (OR = 1.23, 95% CI: 1.07–1.41; P = 0.00354), while the middle tertile was associated with a 13% higher mortality rate (OR = 1.13, 95% CI: 1.00–1.28; P = 0.04348). The trend tests across all models were statistically significant (all P-values < 0.01), emphasizing the strong and consistent positive association between MELD-XI scores and 30-day all-cause mortality.
Identification of nonlinear relationships and threshold effect analysis
Figure 2 shows a nonlinear relationship between MELD-XI score and 30-day mortality in ICU patients with sepsis (P for nonlinearity < 0.001). The inflection point for MELD-XI was 25.74. This difference was confirmed to be statistically significant by the likelihood ratio test of the two-piecewise linear regression model (P = 0.007, Table 4). Specifically, when MELD-XI < 25.74, the association with mortality was not statistically significant (OR = 1.005, 95% CI: 0.993–1.018; P = 0.389). However, when MELD-XI ≥ 25.74, each 1-point increase in MELD-XI was associated with a 4.8% higher risk of 30-day mortality (OR = 1.048, 95% CI: 1.016–1.081; P = 0.00287), indicating that 25.74 may serve as a mortality risk threshold, above which the risk increases significantly.
A nonlinear association between the MELD-XI score and 30-day mortality was identified using a generalized additive model (GAM). The solid blue line represents the fitted smooth curve, while the shaded grey area indicates the 95% confidence intervals. MELD-XI was used as the independent variable. The model was adjusted for ethnicity, gender, age, septic shock, pulmonary infection, renal/urinary tract infection, skin/bone/joint infection, history of dialysis, cardiac arrhythmias, severe liver disease, renal failure, malignant cancer, metastatic solid tumor, Lactate, APACHE IV score, SOFA score, and GCS score. Abbreviations: MELD-XI, Model for End-Stage Liver Disease excluding INR.
Stratified analysis
To evaluate the robustness of the association between the MELD-XI score and 30-day all-cause mortality, a stratified subgroup analysis was performed using multiple imputation data (Fig. 3). The results demonstrated a consistent positive association across most subgroups, with odds ratios (ORs) ranging from approximately 1.02 to 1.13, supporting the score’s robust prognostic value across diverse ICU populations. Notably, the association was most pronounced in patients with a history of dialysis (OR = 1.13, 95% CI: 1.07–1.20), substantially higher than that in patients without dialysis (OR = 1.05), indicating that the MELD-XI score may have increased predictive power in individuals with impaired renal function. Significant associations were also observed in patients with comorbid cardiac arrhythmias (OR = 1.04), severe liver disease (OR = 1.06), renal failure (OR = 1.02), malignant cancer (OR = 1.05), and metastatic solid tumors (OR = 1.04), all with P < 0.05. Subgroup analysis by age revealed stronger associations in patients younger than 65 years (OR = 1.06) compared to those aged 65 or older (OR = 1.03). Similarly, patients with higher disease severity, as indicated by elevated APACHE IV (≥ 81: OR = 1.03) and SOFA scores (≥ 9: OR = 1.03), showed stronger associations than those with lower scores.
Subgroup analysis of the association between MELD-XI score and 30-day mortality in ICU patients with sepsis.Multivariable logistic regression models were used to assess the association between MELD-XI score and mortality risk across clinical subgroups. Odds ratios (ORs) and their 95% confidence intervals (CIs) are presented. The x-axis is plotted on a logarithmic scale; the vertical dashed line represents the reference value of OR = 1, with points to the right indicating increased mortality risk. Abbrevations: GCS, Glasgow Coma Scale; SOFA, Sequential Organ Failure Assessment; APACHE IV, Acute Physiology and Chronic Health Evaluation IV; MELD-XI, Model for End-Stage Liver Disease Excluding INR.
Discussion
In this retrospective cohort study, we included 16,691 patients diagnosed with sepsis within 48 h of ICU admission using data from the eICU database to evaluate the association between MELD-XI score and 30-day all-cause mortality. The results demonstrated that MELD-XI was an independent predictor of 30-day mortality in this population, with a significant nonlinear relationship and a threshold effect. Higher MELD-XI scores were significantly associated with increased mortality risk, and subgroup analyses further confirmed the robustness of these findings. This evidence supports the potential utility of the MELD-XI score in early risk stratification and clinical management of sepsis in the ICU.
In sepsis, the liver, as a crucial metabolic and immune organ, is vulnerable to injury from inflammatory mediators, pathogens, and toxins, which can lead to dysfunction or even failure, thereby significantly increasing mortality risk, with rates reported as high as 38.2%–68%17. Serum total bilirubin, an important biochemical indicator of liver function, has also been shown to correlate closely with mortality in sepsis6,7. Additionally, acute kidney injury (AKI) is a common complication, associated with a hospital mortality rate of 9.1%18, and patients requiring dialysis face a mortality rate of up to 43.6%19. The MELD-XI score, which is calculated based on serum bilirubin and creatinine levels, is highly valuable for early risk stratification in sepsis patients20. Compared with APACHE IV and SOFA scores that depend on multiple organ parameters and complex calculations2,3, MELD-XI relies on only two routine laboratory indicators (total bilirubin and creatinine), making it more suitable for rapid risk assessment in critically ill patients, especially in clinical environments with limited data or time constraints, where it offers greater practicality21. Furthermore, our results indicate that lactic acid plays a partial mediating role in the association between MELD-XI and 30-day mortality, with approximately 19.6% of the total effect attributable to the lactate pathway. This finding supports the hypothesis that liver and kidney dysfunction in sepsis can lead to metabolic disturbances and exacerbate disease severity. Specifically, the liver and kidney impairment reflected by the MELD-XI score may elevate lactic acid levels by impairing its metabolism and clearance, thereby increasing the mortality risk of affected patients.
In this study, we identified a significant nonlinear association between the MELD-XI score and 30-day all-cause mortality in ICU patients with sepsis, indicating a distinct threshold effect. The risk of death increased gradually at scores below 25.74 but rose sharply when the MELD-XI score exceeded this threshold. This inflection point may represent a critical threshold beyond which hepatic and renal dysfunction overwhelm the body’s compensatory mechanisms, resulting in the loss of internal homeostatic regulation. Hepatic and renal functions play vital roles in metabolic regulation and systemic homeostasis. Sepsis, characterized by a systemic inflammatory response to infection, often involves elevated inflammatory cytokines such as TNF-α, IL-6, and IL-1β22,23. Liver dysfunction can impair ammonia metabolism and mitochondrial activity, amplifying the inflammatory cascade24. Simultaneously, renal insufficiency contributes to toxin accumulation and electrolyte imbalance25. Recent studies have highlighted the important pathophysiological role of the liver-kidney axis in sepsis, where bidirectional dysfunction may exacerbate systemic inflammation and organ failure. Specifically, hepatic impairment may hinder the clearance of gut-derived toxins and inflammatory mediators, placing additional burden on renal excretory pathways and forming a vicious cycle of multiorgan dysfunction26,27. This feedback loop may help explain the sharp rise in mortality observed beyond the MELD-XI inflection point (≥ 25.74), as it likely reflects the exhaustion of hepatic-renal compensatory reserve. However, the magnitude of this threshold effect may also be influenced by methodological factors, such as the fixed creatinine value assigned to dialysis patients under the MELD-XI scoring criteria, which could potentially lead to bias in the observed outcomes.
Therefore, the MELD-XI score not only reflects the degree of organ dysfunction but may also serve as a potential alternative indicator of hepatorenal dysfunction in critically ill patients with sepsis. Based on the inflection point identified in this study (25.74), patients with higher MELD-XI scores should warrant heightened clinical attention. These patients should be evaluated in the context of their overall condition, with priority given to continuous and dynamic monitoring. At an appropriate time, liver-protective treatments (e.g., artificial liver support systems) or renal replacement therapy (RRT) should be considered to improve prognosis and guide resource allocation28,29. Additionally, future studies should conduct mechanistic research to further explore the biological plausibility of this threshold and provide a foundation for optimizing early intervention strategies. Although this threshold appears biologically plausible and statistically significant, its clinical applicability should be further validated in prospective, multicenter studies to ensure its feasibility and effectiveness in real-world clinical decision-making.
Strengths and limitations
This study was conducted using the Electronic Intensive Care Unit Collaborative Research Database, a large-scale, multicenter intensive care dataset comprising 16,691 ICU patients with sepsis, which enhances the reliability and statistical power of our findings. Although previous studies have examined the prognostic value of the MELD-XI score, our analysis identified a nonlinear association between the MELD-XI score and mortality and further revealed a specific turning point, offering a valuable reference for future research on sepsis risk stratification and clinical decision-making. Nonetheless, several limitations should be acknowledged. First, as a retrospective analysis, the study is inherently subject to residual confounding, despite adjustment for multiple covariates. Second, although multiple imputation was applied to address missing data and reduce potential bias, the possibility of residual selection bias cannot be entirely excluded. Third, the data were derived from U.S. community hospitals, where illness severity was generally mild; therefore, the generalizability of our findings to specialized intensive care units or non-Western populations with different ethnic backgrounds and healthcare systems may be limited and requires further external validation. Fourth, for patients with a history of dialysis, we assigned a fixed serum creatinine value of 4.0 mg/dL in accordance with MELD-XI scoring criteria to ensure consistency and comparability. This approach may have artificially inflated MELD-XI scores in this subgroup, potentially contributing to the paradoxical finding of lower unadjusted mortality and the strong association observed in the subgroup analysis due to misclassification bias.
Building on these findings, future research may focus on the following areas: First, the prognostic value of the MELD-XI score in sepsis should be validated in independent, prospective cohorts to enhance its external validity. Second, the MELD-XI score could be integrated with existing prognostic systems—such as SOFA, qSOFA, and lactate levels—to develop a composite prognostic model with improved predictive accuracy and clinical applicability. Finally, given the significantly increased risk of mortality observed when the MELD-XI score exceeds 25.74, future intervention trials could assess whether risk stratification based on this threshold can guide timely and targeted clinical management strategies, ultimately improving patient outcomes.
Conclusion
This study found a nonlinear relationship and threshold effect between the MELD-XI score and 30-day mortality in ICU patients with sepsis. When the MELD-XI score exceeds 25.74, the risk of death rises significantly. As a simple and practical scoring tool, MELD-XI may aid in early risk assessment in clinical settings. Further prospective studies are needed to validate this threshold and assess its utility in guiding treatment decisions.
Data availability
The data that support the findings of this study are available from the eICU Collaborative Research Database, which is publicly accessible at https://eicu-crd.mit.edu/. Access to the database requires completion of a data use agreement and relevant training.
References
Rudd, K. E. et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the global burden of disease study. Lancet 395(10219), 200–211. https://doi.org/10.1016/S0140-6736(19)32989-7 (2020).
van Vught, L. A. et al. Incidence, risk factors, and attributable mortality of secondary infections in the intensive care unit after admission for sepsis. JAMA 315, 1469079. https://doi.org/10.1001/jama.2016.2691 (2016).
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315, 801–810. https://doi.org/10.1001/jama.2016.0287 (2016).
Assenza, G. E. et al. MELD-XI score and cardiac mortality or transplantation in patients after Fontan surgery. Heart 99, 491–496. https://doi.org/10.1136/heartjnl-2012-303347 (2013).
Wernly, B. et al. Model for end-stage liver disease excluding INR (MELD-XI) score in critically Ill patients: Easily available and of prognostic relevance. PLoS ONE 12(2), e0170987. https://doi.org/10.1371/journal.pone.0170987 (2017).
Yang, Z. X., Lv, X. L. & Yan, J. Serum total bilirubin level is associated with hospital mortality rate in adult critically ill patients: A retrospective study. Front. Med. (Lausanne). 4(8), 697027. https://doi.org/10.3389/fmed.2021.697027 (2021).
Patel, J. J. et al. The association of serum bilirubin levels on the outcomes of severe sepsis. J. Intensive Care Med. 30(1), 23–29. https://doi.org/10.1177/0885066613488739 (2015).
Bellomo, R. et al. Acute kidney injury in sepsis. Int. J. Mol. Sci. 25(11), 5924. https://doi.org/10.3390/ijms25115924 (2024).
Malinchoc, M. et al. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 31(4), 864–871. https://doi.org/10.1053/he.2000.5852 (2000).
Wiesner, R. et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology 124(1), 91–96. https://doi.org/10.1053/gast.2003.50016 (2003).
Yamada, T. et al. Model of ng-TeEnd-stage liver disease excluding INR (MELD-XI) scoring system provides additional Lorm prognostic information in patients admitted with acute decompensated heart failure. J. Am. Coll. Cardiol. 67(13), 1418. https://doi.org/10.1016/S0735-1097(16)31419-X (2016).
Pollard, T. J. et al. The eICU collaborative research database, a freely available multi-center database for critical care research. Sci. Data. 11(5), 180178. https://doi.org/10.1038/sdata.2018.178 (2018).
Lambden, S. et al. The SOFA score-development, utility and challenges of accurate assessment in clinical trials. Crit Care. 23(1), 374. https://doi.org/10.1186/s13054-019-2663-7 (2019).
Martin, A. P. et al. Overview of the MELD score and the UNOS adult liver allocation system. Transpl. Proc. 39(10), 3169–3174. https://doi.org/10.1016/j.transproceed.2007.04.025 (2007).
Jaddoe, V. W. et al. First trimester fetal growth restriction and cardiovascular risk factors in school age children: Population based cohort study. BMJ 23(348), g14. https://doi.org/10.1136/bmj.g14 (2014).
Lin, L. et al. The analysis of threshold effect using empower stats software. Chin. J. Epidemiol. 34, 1139–1141 (2013).
Kobashi, H. et al. Sepsis-associated liver injury: Incidence, classification and clinical significance. Hepatol. Res. 43(3), 255–266. https://doi.org/10.1111/j.1872-034X.2012.01069.x (2013).
Jia, H. M. et al. The attributable mortality of sepsis for acute kidney injury: A propensity-matched analysis based on multi-center prospective cohort study. Ren. Fail. 45, 2162415. https://doi.org/10.1080/0886022X.2022.2162415 (2023).
Sakhuja, A. et al. Acute kidney injury requiring dialysis in severe sepsis. Am. J. Respir. Crit. Care Med. 192(8), 951–957. https://doi.org/10.1164/rccm.201502-0329OC (2015).
Deo, S. V. et al. Model for end-stage liver disease excluding international normalized ratio (MELD-XI) score predicts heart transplant outcomes: Evidence from the registry of the united network for organ sharing. J. Heart Lung Transplant. 35(2), 222–227. https://doi.org/10.1016/j.healun.2015.10.008 (2016).
Arslan, F. et al. The prognostic significance of MELD-XI in patients admitted to the intensive care unit for respiratory failure. Thorac. Res. Pract. 26(3), 115–124. https://doi.org/10.4274/ThoracResPract.2024.24047 (2025).
Hoshino, K. et al. Usefulness of plasminogen activator inhibitor-1 as a predictive marker of mortality in sepsis. J. Intensive Care. 11(5), 42. https://doi.org/10.1186/s40560-017-0238-8 (2017).
Vincent, J. et al. Frequency and mortality of septic shock in Europe and North America: A systematic review and meta-analysis. Crit. Care. 23(1), 196. https://doi.org/10.1186/s13054-019-2478-6 (2019).
Garibay, P. R. D. et al. Critical care hepatology: definitions, incidence, prognosis and role of liver failure in critically Ill patients. Crit Care. 26(1), 289. https://doi.org/10.1186/s13054-022-04163-1 (2022).
Wang, M. et al. Toll-like receptor 4 signaling pathway mediates both liver and kidney injuries in mice with hepatorenal syndrome. Am. J. Physiol. Gastrointest. Liver Physiol. 323(5), G461–G476. https://doi.org/10.1152/ajpgi.00048.2022 (2022).
Dou, J. et al. The interplay of cross-organ immune regulation in inflammation and cancer. MedComm (2020). 6(7), e70249. https://doi.org/10.1002/mco2.70249 (2025).
Bauer, M. The liver-gut-axis: Initiator and responder to sepsis. Curr. Opin Crit. Care. 28(2), 216–220. https://doi.org/10.1097/MCC.0000000000000921 (2022).
Dai, Z. S. et al. Efficacy of a novel artificial liver versatile plasma purification system in patients with acute-on-chronic liver failure. World J. Gastroenterol. 31(14), 103892. https://doi.org/10.3748/wjg.v31.i14.103892 (2025).
Yagnik, K. et al. Factors affecting continuous renal replacement therapy (CRRT) in patients with septic shock: An analysis of a national inpatient sample database. Cureus. 16(11), e74356. https://doi.org/10.7759/cureus.74356 (2024).
Acknowledgements
AcknowledgmentsThe authors extend their gratitude to all participants and staff involved with the eICU Collaborative Research Database (eICU-CRD) database for their valuable contributions.
Funding
None.
Author information
Authors and Affiliations
Contributions
JM, YW formulated the research questions and designed the study. TY and ZZ performed the literature search. JM extracted the clinical data from the eICU database, and JM, XL analyzed the data.JM drafted the manuscript. ZZ and HL critically reviewed, edited, and approved the manuscript. JM and XL finalized the manuscript based on the comments of all authors. All authors provided comments and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Ethical approval was waived by the Institutional Review Board of the Massachusetts Institute of Technology (Cambridge, MA, USA) for this retrospective study due to the lack of direct patient intervention and the use of a security schema certified to meet the HIPAA Safe Harbor standard for re-identification risk by an independent privacy expert (Privacert, Cambridge, MA; Certification No. 1031219-2). The study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki and adhered to all relevant institutional guidelines.
Consent for publication
Not applicable.
Informed consent
The requirement for informed consent was waived by the Institutional Review Board of the Massachusetts Institute of Technology (Cambridge, MA, USA) because only de-identified data were used.
Clinical trial number
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mai, J., Wang, Y., Li, X. et al. The association between the MELD-XI score and 30-day mortality in ICU patients with sepsis: a retrospective cohort study. Sci Rep 15, 35121 (2025). https://doi.org/10.1038/s41598-025-19074-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-19074-8