Abstract
Keratin 6 A (KRT6A) is a member of the keratin family and can participate in the occurrence and development of some tumors. However, there is still a lack of pan-cancer analysis of KRT6A in humans. We studied the pan-cancer role of KRT6A with the help of a variety of external public databases (mainly including TCGA, GTEx, HPA, TIMER2.0, UALCAN, TISIDB, GEPIA2, Kaplan-Meier Plotter, cBioPortal and TISCH2, etc.). We performed immunohistochemistry detection of KRT6A protein expression in lung adenocarcinoma (LUAD) and its adjacent normal tissues. The results showed that KRT6A mRNA and protein were differentially expressed in most tumors, and its expression and function may be regulated by DNA methylation, RNA methylation and protein phosphorylation, and were related to the prognosis and clinical subtypes of patients with different tumors. KRT6A has multiple genetic and epigenetic characteristics in different cancers, and the main type of its genetic variation is mutation. At the same time, KRT6A is closely related to tumor mutation burden (TMB), microsatellite instability (MSI), tumor stemness score (TSC), immune checkpoints, immunomodulatory genes, and tumor immune microenvironment (TIME) in different human tumors. Secondly, the expression level of KRT6A is associated with immunotherapy and drug sensitivity. In addition, bioinformatics analysis and immunohistochemistry experiments verified that KRT6A mRNA and protein were up-regulated in LUAD, and could promote the development process of LUAD by promoting processes such as epidermis development, intermediate filament cytoskeleton and cornified envelope. This is the first pan-cancer analysis of KRT6A, which provides a comprehensive and systematic understanding of its role in various human tumors, and also reveals that KRT6A is expected to become a potential prognostic biomarker and a new target for cancer immunotherapy.
Similar content being viewed by others
Introduction
To date, cancer remains a leading cause of death in humans and a public health problem facing the international community, with a huge negative impact on social health and economic livelihood around the world1,2,3,4,5. With more and more scholars investing in the research and exploration of tumor-related fields, targeted therapy and immunotherapy and other treatment methods have been continuously updated and improved, and the actual treatment effect of various tumors has been greatly improved6,7. However, due to the heterogeneity of tumors, clonal evolution, immune escape, and treatment resistance, the overall cure rate and survival prognosis of cancer patients are still unsatisfactory8,9. Therefore, the exploration and development of new and highly potential pan-cancer diagnostic and prognostic biomarkers and cancer treatment targets are still an important part of the current tumor diagnosis and treatment field10. At present, with the continuous development of high-throughput technology, people can use a variety of large-scale external public databases (such as TCGA and GTEx) to conduct systematic and comprehensive pan-cancer analysis, explore the correlation between differential expression of target genes and pan-cancer-related clinical features and patient survival prognosis, and provide a certain basis for the discovery of new promising biomarkers11,12,13,14,15. Therefore, bioinformatics analysis is often used in the study of gene expression in human pan-cancer to explore potential targets for clinical diagnosis and treatment of cancer16,17,18.
Keratin 6 A (KRT6A) is a gene encoding type II keratin, which belongs to the keratin family and plays an important role in the structural support and functional regulation of epithelial tissues such as skin, hair and nails19,20. KRT6A has been proven to have biological functions such as structural support, damage repair, mitochondrial regulation, inflammation and immune regulation, and has been widely concerned by scholars21,22. With the continuous deepening of research in related fields, more and more scholars have found that KRT6A can participate in and regulate the development process of a variety of human tumors. Chen et al. found that the expression level of KRT6A in bladder urothelial carcinoma (BLCA) tissue samples was significantly higher than that in paired normal tissue samples. KRT6A promoted the activity, proliferation and adhesion of BLCA cells by inhibiting the expression of downstream target gene miRNA (miR)-31-5p, and significantly inhibited BLCA cell apoptosis23. A study by Xu et al. showed that when the KRT6A gene was highly expressed, the proliferation, invasion and migration abilities of non-small cell lung cancer (NSCLC) cells were significantly improved, while exogenous knockout of KRT6A could significantly reverse this process. Meanwhile, high expression of KRT6A was closely related to the poor prognosis of NSCLC patients24. Che et al. further found that the high expression of KRT6A can affect the MYC signaling pathway, induce the up-regulation of glucose-6-phosphate dehydrogenase (G6PD) expression, increase the flux of the pentose phosphate pathway, and then significantly promote the growth and invasion of NSCLC cells25. In addition, some scholars have found that KRT6A is highly expressed in nasopharyngeal carcinoma (NPC) tissues compared with the corresponding normal tissues. High expression of KRT6A can regulate the Wnt/β-catenin signaling pathway, thereby significantly improving the proliferation, migration and invasion ability of tumor cells, while KRT6A silencing can hinder this process26. Thus, current studies have shown that KRT6A plays a pro-cancer role in a variety of human cancers, and there is no clear evidence that it plays a tumor-suppressing role in the occurrence and development of some tumors. In addition, the current research on KRT6A by scholars mainly focuses on a few types of tumors. The regulatory role, molecular mechanism and clinical significance of KRT6A in other tumors are still unclear. There is still a lack of comprehensive and systematic pan-cancer analysis, especially the study of the prognostic value of KRT6A and its deeper analysis in immunotherapy. In summary, the study and exploration of how KRT6A affects tumorigenesis and development and immune response can provide new strategies with great potential for tumor immunotherapy. Meanwhile, given the heterogeneity of human tumors and the variability of response to immunotherapy, further exploration of the specific role of KRT6A in human pan-cancer will help to discover promising therapeutic targets and improve the accuracy of immunotherapy.
In this study, we performed a comprehensive analysis of KRT6A in human pan-cancer using public databases such as TCGA, GTEx, HPA, TIMER2.0, UALCAN, TISIDB, GEPIA2, and cBioPortal, and explored the differential expression of KRT6A in different tumors and its correlation with patient survival prognosis, clinical subtypes, DNA methylation, RNA methylation, protein phosphorylation, single-cell distribution, TMB, MSI, TSC, immune checkpoints, immune regulatory genes, immune infiltration, immunotherapy, and drug sensitivity. In addition, we further evaluated the expression characteristics, genetic variation patterns, and related functional enrichment of KRT6A in human pan-cancer. It is worth mentioning that we also confirmed the expression difference and regulatory function of KRT6A in the clinical cohort of lung adenocarcinoma (LUAD). We hope to reveal the broad prospects of KRT6A as a target for patient survival prognosis assessment and therapeutic intervention through systematic analysis of the potential regulatory mechanisms of KRT6A in different human tumors.
Materials and methods
Overall design of the study
The overall technical route of this study is shown in Fig. 1. The abbreviations and corresponding full names are shown in Table S1.
Data acquisition and gene expression analysis
In our study, we used the UCSC Genome Browser (https://genome.ucsc.edu/index.html)27 Human Dec. 2013 (GRCh38/hg38) Assembly to obtain the specific location of KRT6A on human chromosomes. Meanwhile, we obtained the gene expression of KRT6A in multiple normal human tissues from the Genotype-Tissue Expression (GTEx) Portal website (https://gtexportal.org/home/). We further confirmed the expression of KRT6A in various human organs and tissues through the Human Protein Atlas (HPA) website (https://www.proteinatlas.org/). In addition, we used the Tumor Immune Estimation Resource 2.0 (TIMER2.0) website (https://timer.cistrome.org/)28 to analyze the differential expression of KRT6A in different tumor tissues and corresponding normal tissues in The Cancer Genome Atlas (TCGA) database (https://portal.gdc.cancer.gov). It is worth mentioning that we obtained the RNAseq data of TCGA in the format of transcripts per million reads (TPM) through the Toil process29 from UCSC XENA (https://xenabrowser.net/datapages/), and used KRT6A mRNA in TCGA and GTEx databases to analyze its differential expression in different tumor tissue samples and corresponding normal tissue samples. *, **, and *** represent P < 0.05, P < 0.01, and P < 0.001, respectively.
Differential expression of KRT6A protein in different tumor tissues and corresponding normal tissues and immunohistochemistry and Immunofluorescence staining
We used the University of Alabama at Birmingham Cancer data analysis portal (UALCAN) database (https://ualcan.path.uab.edu)30 to obtain the differential expression of KRT6A protein in different tumor tissues and corresponding normal tissues. At the same time, we used the HPA database to further explore the immunohistochemistry images of KRT6A protein in the above tumor tissues and corresponding normal tissues to verify the differential expression of KRT6A protein in different tumor tissue samples and corresponding normal tissue samples. In addition, we obtained immunofluorescence staining images of KRT6A subcellular localization using the HPA database. *, **, *** represent P < 0.05, P < 0.01 and P < 0.001, respectively.
Correlation between KRT6A expression and cancer stage, tumor grade, immune subtype and molecular subtype of pan-cancer
We used the TISIDB database (https://cis.hku.hk/TISIDB/index.php)31 to analyze the correlation between the expression level of KRT6A and the cancer stage, tumor grade, immune subtype, and molecular subtype of different tumor types. P-values less than 0.05 were considered statistically significant.
Relationship between KRT6A and survival prognosis of patients with different tumors
First, we explored the prognostic value of KRT6A in various TCGA tumor patients using the Gene Expression Profiling Interactive Analysis 2 (GEPIA2) platform (https://gepia2.cancer-pku.cn/)32 to obtain overall survival (OS) and disease free survival (DFS). In this platform, the median of KRT6A expression was used as the cutoff value for grouping (low expression group: 0–50%, high expression group: 50–100%). The log-rank test was used for hypothesis testing. Next, we used the Kaplan-Meier Plotter platform (https://kmplot.com)33,34 to obtain the correlation between the expression of KRT6A in RNAseq data and the OS and relapse free survival (RFS) of patients with different tumors. P-values less than 0.05 were considered statistically significant. Hazard ratio (HR) > 1, < 1 and = 1 represent high risk, low risk and no difference, respectively.
Genetic variation analysis of KRT6A
The cBio Cancer Genomics Portal (cBioPortal) (https://www.cbioportal.org)35,36,37 is a multidimensional cancer genomics dataset that provides interactive retrieval, visualization, and analysis of multivariate genetic variation. We used the “TCGA PanCancer Atlas Studies” in cBioPortal to obtain the genetic variations of KRT6A in different tumors, and used the “Cancer Types Summary”, “Mutations”, “Plots” and “Comparison/Survival” modules to explore the genetic changes and mutation site information. *, **, and *** represent P < 0.05, P < 0.01, and P < 0.001, respectively.
DNA and RNA methylation analysis of KRT6A
DNA methylation is one of the most common forms of epigenetic modification. DNA hypermethylation can lead to gene silencing, while reduced DNA methylation can induce relatively high gene expression38. We analyzed the KRT6A DNA promoter methylation level by searching the UALCAN database, and then determined its differential expression in different tumor tissues and corresponding normal tissues. At the same time, we used the Shiny Methylation Analysis Resource Tool (SMART) website (https://www.bioinfo-zs.com/smartapp/)39 to explore the distribution of methylation probes in the corresponding chromosomes. RNA methylation is also an important epigenetic regulatory pathway that can participate in and regulate the occurrence, development, and prognosis of different tumors40. We extracted the expression data of KRT6A gene and 44 marker genes of three types of RNA modification genes (m1A (10), m5C (13), m6A (21)) in each sample from the UCSC database, and performed log2 (x + 1) on each expression value to calculate the correlation between KRT6A and five immune pathway markers. *, **, and *** represent P < 0.05, P < 0.01, and P < 0.001, respectively.
Phosphorylation analysis of KRT6A protein
Protein phosphorylation is an important post-translational modification process, which can participate in a variety of cell growth and development, metabolic differentiation and signal transduction and other pathophysiological processes under normal circumstances. When the regulation of protein phosphorylation is abnormal, it may regulate the development process of various tumors41. Based on the protein sequence number and phosphorylation site naming rules in the Clinical Proteomic Tumor Analysis Consortium (CPTAC) database (https://cptac-data-portal.georgetown.edu), we explored the differential expression levels of different phosphorylation sites of KRT6A protein in different primary tumor tissues and corresponding normal tissues through the UALCAN website. *, **, and *** represent P < 0.05, P < 0.01, and P < 0.001, respectively.
Single-cell expression analysis of KRT6A
We used the Tumor Immune Single-cell Hub 2 (TISCH2) database (https://tisch.comp-genomics.org/home/)42 to study the single-cell expression of KRT6A mRNA in various tumor tissues and visualized it. In addition, we used the UMAP function to visualize the dimensionality reduction to explore the expression level of KRT6A in different cell types.
Correlation analysis of KRT6A with tumor mutation burden, microsatellite instability, tumor stemness score, immune checkpoint and Immunomodulatory genes
Tumor mutation burden (TMB) is the total number of base mutations in every million cells in the tumor, which has been confirmed to induce the production of tumor-specific and highly immunogenic antibodies, and can be used as a potential target for predicting the efficacy of tumor immunotherapy43. Microsatellite instability (MSI) is caused by abnormal DNA mismatch repair (MMR), which can induce gene replication disorder and the occurrence and development of tumors, and then affect the survival prognosis of tumor patients44. We investigated the correlation between KRT6A and TMB and MSI. Meanwhile, we extracted the expression profile of KRT6A gene from the pan-cancer dataset downloaded and processed in UCSC XENA database, and combined with the methylation profile DNAss of each tumor to calculate the tumor stemness score (TSC). In addition, we extracted the KRT6A gene and 60 marker genes of two types of immune checkpoint genes (inhibitory (24) and stimulatory (36)) from the pan-cancer dataset downloaded and organized from the UCSC XENA database to study the correlation of expression data in each sample. We also used the TISIDB website to explore the correlation between the expression of KRT6A and immunomodulatory genes, including immunoinhibitors, immunostimulators, major histocompatibility complexes (MHCs), chemokines and chemokine receptors, and performed Spearman test to calculate the correlation strength between KRT6A and the above immunomodulatory genes. *, **, and *** represent P < 0.05, P < 0.01, and P < 0.001, respectively.
KRT6A-related immune infiltration analysis
We extracted the expression data of KRT6A gene in each sample from the pan-cancer database downloaded and sorted from UCSC XENA database, obtained the gene expression profile of each tumor, mapped the expression profile to GeneSymbol, and used R package ESTIMATE to calculate the stromal, immune and ESTIMATE scores of each patient in each tumor according to gene expression. After that, we obtained the immune infiltration score related to KRT6A, and used the correlation test function of R package psych coefficient to calculate the Spearman’s correlation coefficient between the gene and the immune infiltration score in each tumor to determine the significantly related immune infiltration score. The TIMER2.0 database was used to evaluate the degree of immune cell infiltration in 32 cancers, and we used the database to explore the correlation between KRT6A expression and 21 common immune cells in the tumor immune microenvironment (TIME) of human cancers. P-values less than 0.05 were considered statistically significant.
Analysis of KRT6A-related genes and its protein-protein interaction network
First, we used the TCGA dataset of the GEPIA2 website and set the parameter “Similar Genes Detection” to obtain the top 100 target genes related to KRT6A. Next, we used the search tool for the retrieval of interacting genes/proteins (STRING) (https://cn.string-db.org) to search for the protein name “KRT6A”, and the organism was selected as “Homo sapiens”. The parameters were set as “minimum required interaction score (medium confidence: 0.400)” and “max number of interactors to show (1st shell: no more than 50 interactors)”. The results provided 50 proteins that interacted with KRT6A. To visualize the protein-protein interaction (PPI) network of KRT6A and its interacting proteins, we used Cytoscape software (https://cytoscape.org/) for further processing. Meanwhile, we used R packages clusterProfiler, org.Hs.eg.db and ggplot2 to perform functional enrichment analysis and result visualization of KRT6A and its related target genes, respectively. Gene ontology (GO) is the world’s largest source of gene function information, mainly composed of biological process (BP), cellular component (CC) and molecular function (MF)45,46. Kyoto encyclopedia of genes and genomes (KEGG) is a database for understanding high-level functions and utilities of biological systems from molecular-level information47,48,49. Finally, we used the TIMER2.0 database to obtain the expression of the top 10 target genes related to KRT6A in each tumor sample, and presented them in the form of a heat map. P-values less than 0.05 were considered statistically significant.
Correlation analysis between KRT6A and immune checkpoint Blockade and drug sensitivity
We used Tumor Immune Syngeneic Mouse (TISMO) (http://tismo.cistrome.org)50 to analyze the correlation between immune checkpoint blockade (ICB) treatment and KRT6A mRNA expression. In addition, we used the Gene Set Cancer Analysis (GSCA) database (https://guolab.wchscu.cn/GSCA/)51 to analyze the relationship between KRT6A mRNA expression levels and drug sensitivity. The GSCA website contains 750 small molecule drugs from the Genomics of Drug Sensitivity in Cancer (GDSC) and Cancer Therapeutics Response Portal (CTRP) databases. *, **, and *** represent false discovery rate (FDR) ≤ 0.05, FDR ≤ 0.01, and FDR ≤ 0.001, respectively. When FDR is less than or equal to 0.05, the result can be considered statistically significant.
Expression, diagnosis and prognosis analysis of KRT6A in LUAD clinical cohort
We used the TCGA and Gene Expression Omnibus (GEO) (https://www.ncbi.nlm.nih.gov/geo/) databases to obtain gene expression profiles and related clinical data of LUAD patients. The details of the relevant platform information and sample annotation are shown in Table S2. Based on the R packages ggplot2, pROC, survival, and survminer, we investigated the expression of KRT6A in LUAD and its correlation with disease diagnosis and patient prognosis. *, **, and *** represent P < 0.05, P < 0.01, and P < 0.001, respectively. P-values less than 0.05 were considered statistically significant. An area under the receiver operating characteristic (ROC) curve (AUC) of > 0.7 was considered ideal. Hazard ratio (HR) > 1, < 1 and = 1 represent high risk, low risk and no difference, respectively.
Clinical samples and immunohistochemistry
Tissue microarray (including 96 cores) was purchased from Wuhan Servicebio Technology Co., Ltd (Wuhan, Hubei, China) to analyze the expression of KRT6A protein in LUAD tissue samples and paired adjacent normal tissue samples. 30 pairs of LUAD tissue samples and adjacent normal tissue samples were obtained from 30 LUAD patients who underwent surgical resection at Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology from February 2025 to June 2025, and were fixed with formalin and embedded in paraffin. The above-mentioned patients who received treatment did not receive chemotherapy or radiotherapy before the operation. Adjacent normal tissues were sampled at a distance of 3 cm from the tumor tissues. Tumor tissues and paired normal tissues were histologically confirmed. The detailed steps of immunohistochemical staining have been described in previous studies52. Briefly, we incubated the LUAD tissue microarray with KRT6A rabbit polyclonal primary antibody (Proteintech Group, Rosemont, IL, USA) (dilution 1:100) at 4 °C overnight and washed three times with phosphate-buffered saline (PBS). The sections were then incubated with the secondary antibody (anti-Rabbit IgG-HRPpolymer) at 37 °C for 30 min and washed with PBS three times again53. Finally, the sections were developed in diaminobenzidine (Servicebio, Wuhan, Hubei, China) and microscopic images were taken using an optical microscope (Leica, Wetzlar, Germany). This study was approved by the Ethics Committee of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology. All participants provided written informed consent and complied with the declaration of Helsinki. The immunoreactivity scoring system was used for immunohistochemistry staining analysis. The percentage of positive cells was scored as follows: 0, < 5%; 1, 5–25%; 2, 25–50%; 3, 50–75%; 4, 75–100%. The staining intensity was scored as follows: 0, negative; 1, weak; 2, moderate; 3, strong. The total score was determined by the following formula: staining index = positive percentage × intensity54.
Gene set enrichment analysis of KRT6A in LUAD
We used the LinkInterpreter analysis module in the LinkedOmics database (https://linkedomics.org/login.php)55 to perform gene set enrichment analysis (GSEA) of KRT6A and its co-expressed genes in TCGA-LUAD. When FDR is less than or equal to 0.05, the result can be considered statistically significant.
Statistical analysis
Statistical analysis in this study was performed using the above online databases and R software (version 4.2.0). We used the Wilcoxon rank sum test and Pearson rank sum test to compare the differences and correlations of KRT6A expression in different tumor tissues and corresponding normal tissues, respectively. Paired sample T-test was used to evaluate the difference between tumor tissue and adjacent normal tissue. Univariate Cox regression analysis and log-rank test were used to evaluate the prognostic role of KRT6A expression in different tumor types. Spearman correlation analysis was used to analyze the relationship between KRT6A and other factors, including cancer stage, tumor grade, clinical subtype, DNA methylation, RNA methylation, protein phosphorylation, TMB, MSI, TSC, immune checkpoint, immune regulatory gene, and immune infiltration analysis. *, **, and *** represent P < 0.05, P < 0.01, and P < 0.001, respectively. P < 0.05 and/or FDR ≤ 0.05 means statistical significance.
Results
Gene location analysis and expression of KRT6A in normal tissue samples and tumor tissue samples
Based on the UCSC Genome Browser Human Dec. 2013 (GRCh38/hg38) Assembly, we found that KRT6A was mainly located at chr12:52487176–52,493,257 (Fig. 2A). The gene expression data of KRT6A in different normal human tissues from the GTEx Portal website showed that the expression level of KRT6A in “Cervix-Ectocervix”, “Esophagus-Mucosa”, “Minor Salivary Gland”, “Skin-Not Sun Exposed (Suprapubic)”, “Skin-Sun Exposed (Lower leg)” and “Vagina” tissues was significantly higher than that in other human tissues (Fig. 2B). Meanwhile, we obtained the expression of KRT6A in various human organs and tissues through the HPA website. The results showed that the expression level of KRT6A in salivary gland, esophagus, vagina, cervix, skin and tonsil was relatively high compared with other normal organs and tissues, and the enrichment in esophagus tissue was the most significant, which was consistent with the conclusion of GTEx Portal website (Fig. 2C). In addition, we used the TIMER2.0 database to analyze the expression of KRT6A in different tumor tissue samples and paired normal tissue samples adjacent to cancer. We found that the expression level of KRT6A was abnormally increased in BLCA, cervical squamous cell carcinoma and endocervical adenocarcinoma (CESC), colon adenocarcinoma (COAD), kidney chromophobe (KICH), kidney renal papillary cell carcinoma (KIRC), LUAD, lung squamous cell carcinoma (LUSC), rectum adenocarcinoma (READ), stomach adenocarcinoma (STAD), thyroid carcinoma (THCA) and uterine corpus endometrial carcinoma (UCEC) tissue samples compared with paired normal tissue samples, while the expression level was relatively low in breast invasive carcinoma (BRCA), kidney renal papillary cell carcinoma (KIRP) and prostate adenocarcinoma (PRAD) tissues (Fig. 2D, all P < 0.05). Since some tumors in the TIMER2.0 database do not have normal tissues, we combined the GTEx database and the TCGA database to analyze the expression level of the target gene KRT6A. The results showed that KRT6A was abnormally highly expressed in BLCA, CESC, esophageal carcinoma (ESCA), LUAD, LUSC, ovarian serous cystadenocarcinoma (OV), pancreatic adenocarcinoma (PAAD), thymoma (THYM) and UCEC tissue samples compared with the corresponding normal tissue samples, while the expression level was decreased in adrenocortical carcinoma (ACC), BRCA, lymphoid neoplasm diffuse large B-cell lymphoma (DLBC), glioblastoma multiforme (GBM), KICH, KIRP, acute myeloid leukemia (LAML), brain lower grade glioma (LGG), liver hepatocellular carcinoma (LIHC), PRAD, READ, skin cutaneous melanoma (SKCM), testicular germ cell tumors (TGCT) and THCA tissue samples (Fig. 2E, all P < 0.05).
Gene location analysis and gene expression of KRT6A in normal tissues and pan-cancer tissues. (A) The location of KRT6A gene in human body. (B) The expression of KRT6A mRNA in various tissues from GTEx Portal. (C) The expression level of KRT6A mRNA in normal tissues of various organs from the HPA database. (D) The expression level of KRT6A mRNA in pan-cancer tissues and paired adjacent normal tissues in TCGA database was analyzed by TIMER2.0. (E) Differential expression of KRT6A mRNA in tumor tissues and corresponding normal tissues from TCGA and GTEx databases. *, **, and *** represent P < 0.05, P < 0.01, and P < 0.001, respectively.
Expression of KRT6A protein in tumor tissue samples and paired normal tissue samples, immunohistochemistry and Immunofluorescence images
After our study using the UALCAN database, we found that the expression level of KRT6A protein in COAD, head and neck squamous cell carcinoma (HNSC), LUAD, LUSC, PAAD and UCEC tissues was significantly higher than that in the corresponding normal tissues. Meanwhile, we further analyzed the immunohistochemical results in the HPA database and found that the differential expression of KRT6A protein in the above six tumor tissues and corresponding normal tissues was consistent with the results of the UALCAN database (Fig. 3A-F). In addition, based on the immunofluorescence results of the HPA database, we also found that KRT6A was mainly located in the cytoplasm of HaCaT, hTCEpi and U2OS cells, specifically in intermediate filaments (Fig. 3G).
Expression levels, immunohistochemistry and immunofluorescence images of KRT6A protein in different tumor tissues and corresponding normal tissues. (A–F) The expression levels of KRT6A protein in COAD, HNSC, LUAD, LUSC, PAAD and UCEC tumor tissues and corresponding normal tissues and immunohistochemistry images. (G) Immunofluorescence staining images of KRT6A subcellular localization in the HPA database. *, **, *** represent P < 0.05, P < 0.01 and P < 0.001, respectively.
Expression of KRT6A in pan-cancer cancer stage, tumor grade, immune subtype and molecular subtype
We used the TISIDB platform to analyze the expression of KRT6A in cancer stages, tumor grades, immune subtypes, and molecular subtypes in different tumor types. Our results showed that the expression level of KRT6A tended to decrease with the increase of cancer stage in BRCA, ESCA and HNSC patients, while it tended to increase with the increase of cancer stage in COAD, KIRC, LUAD and TGCT patients (Fig. 4A, all P < 0.05). Meanwhile, we found that the expression level of KRT6A in HNSC, LIHC, PAAD, STAD and UCEC patients with different tumor grades was significantly different (Fig. 4B, all P < 0.05). Next, we explored the correlation between KRT6A expression and immune subtypes in human pan-cancer. The immune subtypes were mainly divided into C1 (wound healing), C2 (IFN-gamma dominant), C3 (inflammatory), C4 (lymphocyte depleted), C5 (immunologically quiet) and C6 (TGF-b dominant). The results showed that the expression level of KRT6A in patients with BLCA, BRCA, CESC, cholangio carcinoma (CHOL), HNSC, KIRC, LUAD, LUSC, PAAD, PRAD, sarcoma (SARC), SKCM, STAD and TGCT with different immune subtypes was significantly different (Fig. 4C, all P < 0.05). It is worth mentioning that we also found that the expression of KRT6A in patients with different molecular subtypes of BRCA, COAD, ESCA, HNSC, KIRP, LUSC, OV and UCEC was also significantly different (Fig. 4D, all P < 0.05). In summary, KRT6A is differentially expressed in cancer stages, tumor grades, immune subtypes, and molecular subtypes of different tumor types.
Correlation between KRT6A expression and cancer stage, tumor grade, immune subtype, and molecular subtype in different cancer types. (A) The expression of KRT6A in different cancer stages of BRCA, COAD, ESCA, HNSC, KIRC, LUAD and TGCT. (B) The expressionof KRT6A in different tumor grades of HNSC, LIHC, PAAD, STAD and UCEC. (C) The expression of KRT6A in different immune subtypes of BLCA, BRCA, CESC, CHOL, HNSC, KIRC, LUAD, LUSC, PAAD, PRAD, SARC, SKCM, STAD and TGCT. (D) The expression of KRT6A in different molecular subtypes of BRCA, COAD, ESCA, HNSC, KIRP, LUSC, OV and UCEC. Generally, P values less than 0.05 were considered statistically significant.
Correlation between KRT6A and survival prognosis of patients with different tumors
To further study and explore the potential prognostic value of KRT6A in different tumors, we performed univariate Cox regression and log-rank test. Based on the results of GEPIA2 analysis, we found that high expression of KRT6A in patients with KIRC, LUAD, PAAD and SKCM predicted worse OS (Fig. 5A, all HR > 1 and P < 0.05). Meanwhile, high expression of KRT6A predicted worse DFS in LUAD and PAAD patients, but also indicated higher DFS in CESC patients (Fig. 5B, all P < 0.05). In addition, we analyzed the relationship between KRT6A expression and prognosis of patients with different tumors through the Kaplan-Meier Plotter website. Compared with patients with low KRT6A expression, patients with high KRT6A expression in BLCA (Fig. 5C), KIRC (Fig. 5H), LUAD (Fig. 5J), OV (Fig. 5L) and PAAD (Fig. 5N) had worse OS, while patients with BRCA (Fig. 5D), LIHC (Fig. 5I) and SARC (Fig. 5P) had higher OS. Notably, the expression level of KRT6A was negatively correlated with the RFS of BRCA (Fig. 5E) and PAAD (Fig. 5O) patients, while it was positively correlated with the RFS of CESC (Fig. 5F), ESCA (Fig. 5G), LUSC (Fig. 5K), OV (Fig. 5M) and SARC (Fig. 5Q) patients.
The relationship between KRT6A expression level and pan-cancer prognosis based on GEPIA2 and Kaplan-Meier Plotter. (A, B) The correlation between KRT6A expression and OS and DFS in different cancer types was analyzed based on GEPIA2. (C–Q) The correlation between KRT6A expression and OS and RFS in different cancer types was analyzed based on Kaplan-Meier Plotter. Generally, P values less than 0.05 were considered statistically significant.
KRT6A gene alterations in pan-cancer
In order to study the mutation of KRT6A gene in pan-cancer, we used cBioPortal online platform to conduct correlation research based on TCGA database. We found that the mutation frequency of KRT6A gene was higher in SKCM, UCEC, ACC and DLBC (> 4%), and mutation, amplification and deep deletion were the main genetic variation types of KRT6A (Fig. 6A). Meanwhile, we found 164 mutation sites in KRT6A gene, and missense was the most important mutation type (Fig. 6B). The correlation between the putative copy-number alteration (CNA) of KRT6A and its gene expression in pan-cancer is shown in Fig. 6C and D. In addition, the gene alterations of TTN, MUC16, ADAM21P1, TTC9-DT, SYNJ2BP-COX16, IGHJ4, ADAM20P1, SNORD56B, LINC01500 and LINC00520 were more prevalent in KRT6A altered groups than in unaltered groups (Fig. 6E, all P < 0.05).
Different genomic profiles associated with KRT6A expression and integrated analysis of complex tumor genomic and clinical profiles. (A) Summary of genetic alterations of KRT6A in the TCGA pan-cancer dataset based on cBioPortal database analysis. (B) Mutation types, numbers and sites of KRT6A gene genetic variation. (C, D) The correlation between the putative CNA of KRT6A and its expression in pan-cancer. (E) Comparison of the mutation frequency of related genes between the KRT6A gene altered group and the unaltered group. *, **, *** represent P < 0.05, P < 0.01 and P < 0.001, respectively.
Relationship between KRT6A and DNA methylation and RNA methylation
DNA promoter methylation plays a vital role in the occurrence and development of human pan-cancer. We used the UALCAN website to analyze the expression of KRT6A promoter methylation in different tumor tissues and their corresponding normal tissues. The results showed that the KRT6A DNA promoter methylation level in BLCA, BRCA, CESC, COAD, ESCA, HNSC, KIRC, KIRP, LIHC, LUAD, LUSC, PAAD, READ, TGCT, THCA and UCEC tissue samples was significantly lower than that in normal tissue samples (Fig. 7A, all P < 0.01). At the same time, we used the SMART database to study the methylation probes of KRT6A, and found that it had 9 methylation probes, including cg11471401, cg10580110, cg16112157, cg04880990, cg03462053, cg20359793, cg00213044, cg10934546 and cg05824973 (Fig. 7B). In addition, in order to have a deeper understanding of the potential molecular mechanism of KRT6A in different tumors, we further analyzed the expression levels of the marker genes of KRT6A gene and 44 three types of RNA modification (m1A (10), m5C (13), m6A (21)) genes in each sample, and found that the expression of KRT6A was related to the RNA modification genes of multiple tumors (Fig. 7C). The above correlation study of KRT6A gene can improve our understanding of the potential molecular mechanism of different tumors and propose promising new strategies for the treatment of such diseases.
The relationship between KRT6A and methylation and methyltransferase. (A) The promoter methylation level of KRT6A in BLCA, BRCA, CESC, COAD, ESCA, HNSC, KIRC, KIRP, LIHC, LUAD, LUSC, PAAD, READ, TGCT, THCA and UCEC compared with the corresponding normal tissues. (B) Chromosomal distribution of KRT6A-related methylation probes. (C) Correlation between KRT6A expression and m1A, m5C and m6A regulatory genes, with red labels representing positive correlation and blue labels representing negative correlation. *, **, and *** represent P < 0.05, P < 0.01, and P < 0.001, respectively.
Phosphorylation analysis of KRT6A protein
In this study, we performed a comprehensive analysis of the changes in KRT6A protein phosphorylation levels in different tumor types in the Clinical Proteomic Tumor Analysis Consortium (CPTAC) dataset, and evaluated the changes in KRT6A phosphorylation sites and corresponding protein phosphorylation levels in different tumor types. We observed unique patterns of KRT6A phosphorylation in different tumor types in the CPTAC dataset, with higher phosphorylation levels at COAD (S22, S60, and S176), HNSC (S19, S19S22, S22, S31, S35, S41, S41S44, S44, S58, S60, S60S67, S60Y62, S67, S71, S71S76, and Y62), LUAD (S19, S60, and S71), LUSC (S19, S19S22, S31, S41, S41S44, S44, S60, S71, S76, S176, S227, S332, S348, S354, S540S541, and T290), and PAAD (S19, S19S22, S44, S60, and S71) sites compared with the corresponding normal tissues, while lower phosphorylation levels were observed at BRCA (S58 and S67), KIRC (S176), LUAD (S176) and OV (S71) sites (Fig. 8A-H, all P < 0.05). The phosphorylation status of KRT6A is a fine-tuned and dynamic process, showing different patterns and changes in different tumor types. This finding not only emphasizes that KRT6A can participate in and regulate the development process of a variety of malignant tumors, but also emphasizes its potential significance in the context of cancer biology.
Phosphorylation analysis of KRT6A protein in different tumor types. (A–H) Based on the CPTAC dataset, UALCAN was used to analyze the expression differences of different phosphorylation sites of KRT6A protein in normal tissues and primary tumor tissues of 8 tumor types (BRCA, COAD, HNSC, KIRC, LUAD, LUSC, OV and PAAD). *, **, and *** represent P < 0.05, P < 0.01, and P < 0.001, respectively.
Single-cell expression analysis of KRT6A in different tumor tissues
To determine the specific cell types expressing KRT6A in different tumor tissues, we analyzed the single-cell expression in the pan-cancer dataset using the TISCH2 database. As shown in Fig. 9A, the heat map showed the relative expression level of KRT6A in human pan-cancer cell types. We found that KRT6A is widely present in various immune cells and malignant cells. Notably, KRT6A was highly expressed in malignant cells. To further validate these findings, we downloaded the CESC_GSE168652, CHOL_GSE138709, ESCA_GSE160269, HNSC_GSE103322, NSCLC_GSE148071, and PAAD_GSE165399 datasets from TISCH2 for manual single-cell analysis. The UMAP plots showed that KRT6A was mainly highly expressed in malignant cells in the above six datasets, and the expression in other immune cells was relatively low (Fig. 9B-G). Thus, the increased expression level of KRT6A in malignant cells indicates that KRT6A plays a vital role in the malignant progression of tumors.
Single-cell expression analysis of KRT6A in pan-cancer. (A) Clustering heatmap of KRT6A mRNA expression levels in different tumors. (B–G) Expression distributions of KRT6A mRNA in different cell types in CESC_GSE168652, CHOL_GSE138709, ESCA_GSE160269, HNSC_GSE103322, NSCLC_GSE148071 and PAAD_GSE165399 datasets.
Correlation between KRT6A and TMB, MSI, TSC, immune checkpoints, Immunomodulatory genes, and immune infiltration
We also performed correlation analysis of KRT6A with TMB and MSI, which are closely related to ICB sensitivity. The results showed that the expression of KRT6A was significantly positively correlated with TMB in BRCA, CESC, KICH and KIRC, while it was negatively correlated with TMB in KIRP, PRAD and SKCM (Fig. 10A, all P < 0.05). Meanwhile, high expression of KRT6A predicted higher MSI in LUSC, SARC, TGCT and uveal melanoma (UVM), and lower MSI in ESCA, HNSC, PRAD and SKCM (Fig. 10B, all P < 0.05). In addition, we also found that the expression of KRT6A was positively correlated with TSC in BRCA, CESC, CHOL, PRAD, SARC, THCA and THYM, while negatively correlated with TSC in HNSC, pheochromocytoma and paraganglioma (PCPG) and TGCT (Fig. 10C, all P < 0.05). Subsequently, we analyzed the correlation between KRT6A and 60 immune checkpoint genes (including 36 immunostimulatory factors and 24 immunosuppressive factors). We found that there were more than or equal to 10 immune checkpoint genes in THCA, LUSC, PRAD, OV, BRCA, BLCA, TGCT, COAD, THYM, HNSC, LIHC, CESC, LUAD, ESCA, STAD, PAAD, READ, KIRC, UCEC and SARC that were significantly correlated with the expression of KRT6A (Fig. 10D, P < 0.05), as shown in Table S3. It is worth mentioning that we also studied the relationship between KRT6A and immunomodulatory genes in human pan-cancer, including immunoinhibitors, immunostimulators, MHCs, chemokines and chemokine receptors. In some cancers, the expression level of KRT6A is associated with immune regulatory genes (Fig. 10E-I).
Correlation analysis of KRT6A expression level with TMB, MSI, TSC, immune checkpoint and immune regulatory genes. (A) Radar chart of the correlation between KRT6A expression and TMB. (B) Radar chart of the correlation between KRT6A expression and MSI. (C) Radar chart of the correlation between KRT6A expression and TSC. (D) Correlation between KRT6A expression and pan-cancer immune checkpoints. (E–I) Correlation of KRT6A expression with pan-cancer immunomodulatory genes. Red and blue represent positive and negative correlations, respectively. *, **, and *** represent P < 0.05, P < 0.01, and P < 0.001, respectively.
At the same time, we also found that the expression level of KRT6A gene was significantly correlated with the immune infiltration-related score of human pan-cancer. High expression of KRT6A predicted higher stromal scores in BRCA, LUAD, COAD, PRAD, THCA, OV, TGCT, LIHC and CHOL, and lower stromal scores in LAML, UCEC, KIRP, STAD and LUSC (Fig. 11A, all P < 0.05). In addition, the expression of KRT6A was significantly positively correlated with the immune score of BRCA, COAD, PRAD, BLCA, THCA, OV, CESC and LIHC, while it was negatively correlated with the immune score of LUSC, TGCT, UCEC, STAD, HNSC, SKCM and mesothelioma (MESO) (Fig. 11B, all P < 0.05). As the expression level of KRT6A increased, the ESTIMATE scores of BRCA, COAD, PRAD, BLCA, THCA, OV, LUAD, and LIHC increased, while the ESTIMATE scores of STAD, LUSC, UCEC, and SKCM decreased (Fig. 11C, all P < 0.05). It is worth mentioning that we used the TIMER2.0 website to study the relationship between the expression level of KRT6A and the infiltration level of multiple immune cells in TCGA pan-cancer. Our study mainly used XCELL, CIBERSORT, CIBERSORT-ABS, QUANTISEQ, MCPCOUNTER, TIDE and EPIC algorithms to evaluate the results. Our results showed that the expression level of KRT6A was positively correlated with myeloid dendritic cells, myeloid-derived suppressor cells (MDSC), mast cells, neutrophils and cancer associated fibroblasts in the TIME of multiple tumors, while it was negatively correlated with T cells CD8+, plasmacytoid dendritic cells, T cells CD4+, B cells, NK cells, T cells gamma delta, T cells regulatory (Tregs), endothelial cells, hematopoietic stem cells and macrophages (Fig. 11D, all P < 0.05). In summary, KRT6A is closely related to TMB, MSI, TSC, immune checkpoint genes, immune regulatory genes, and immune infiltration, thereby affecting the immune response process of human pan-cancer. This study is expected to provide a deeper understanding of the immune regulation mechanism of tumors, which is crucial for improving the actual efficacy of immunotherapy.
Correlation analysis of KRT6A expression level and pan-cancer immune infiltration. (A) The relationship between KRT6A expression and stromal cells in TCGA pan-cancer tissues was evaluated based on StromalScore. (B) The relationship between KRT6A expression and immune cell infiltration in TCGA pan-cancer tissues was evaluated based on ImmuneScore. (C) The relationship between KRT6A expression and tumor purity in TCGA pan-cancer tissues was evaluated based on ESTIMATEScore. (D) The correlation between KRT6A expression and immune cell infiltration in TCGA pan-cancer was analyzed using TIMER2.0. Generally, P values less than 0.05 were considered statistically significant.
KRT6A-related gene analysis and PPI network diagram
In order to further study the specific mechanism of KRT6A in the occurrence and development of pan-cancer, we screened out KRT6A interacting proteins for PPI network analysis, and KRT6A-related genes for enrichment analysis. First, we established the PPI network diagram of KRT6A and its top 50 interacting proteins through the STRING database to analyze the interaction between them, and visualized it with the help of Cytoscape software (Fig. 12A), and showed the number of interactions of 50 interacting proteins (Fig. 12B). Secondly, we used the Sangerbox3.0 website to perform enrichment analysis on KRT6A and its related genes. The GO-BP results showed that the above genes were mainly involved in the processes of epidermis development, epidermal cell differentiation and keratinocyte differentiation (Fig. 12C, P < 0.05). The GO-CC results showed that these genes could participate in the formation of cornified envelope, cell-cell junction and desmosome (Fig. 12D, P < 0.05). GO-MF results showed that these genes could participate in the regulation of structural constituent of cytoskeleton, structural molecule activity and calcium ion binding (Fig. 12E, P < 0.05). In addition, KEGG results showed that KRT6A and its related genes may affect the development of tumors through estrogen signaling pathway, IL-17 signaling pathway, p53 signaling pathway and other pathways (Fig. 12F, P < 0.05). More interestingly, we also explored the expression of the top 10 KRT6A-related target genes in human pan-cancer, including keratin 6B (KRT6B), desmoglein 3 (DSG3), keratin 5 (KRT5), keratin 6 C (KRT6C), gap junction protein beta 2 (GJB2), desmocollin 2 (DSC2), small proline rich protein 1B (SPRR1B), keratin 16 (KRT16), stratifin (SFN) and keratin 14 (KRT14). The results showed that the expression levels of the above 10 KRT6A-related genes in most tumor tissue samples were positively correlated with KRT6A, emphasizing their potential interaction in the development of different tumors (Fig. 12G, P < 0.05).
Interaction network of KRT6A binding proteins, enrichment analysis of KRT6A-related genes, and expression levels of the top 10 KRT6A-related target genes in pan-cancer tissues. (A) PPI network diagram of KRT6A and its interacting proteins. (B) The interaction degree of the top 50 interacting proteins of KRT6A. (C–F) GO-BP, GO-CC, GO-MF and KEGG enrichment analysis of KRT6A and its related genes. (G) Expression of the top 10 target genes related to KRT6A in TCGA pan-cancer. Generally, P values less than 0.05 were considered statistically significant.
Correlation analysis between KRT6A and ICB treatment and drug sensitivity
We used the TISMO database to correlate the expression level of KRT6A gene in different cancer types with ICB treatment (including anti-PD-1, anti-PD-L1, anti-PD-L2 and anti-CTLA-4) to further study and explore the potential role and correlation of KRT6A gene in ICB treatment of different cancers. Tumor models included are: mammary cancer (4T1, E0771, EMT6, T11, KPB25L, p53-2225 L and p53-2336R), colorectal carcinoma (CT26 and MC38), gastric adenocarcinoma (YTN16), head and neck squamous cell carcinoma (MOC22), hepatocellular carcinoma (BNL-MEA), lung carcinoma (LLC), melanoma (B16, YUMM1.7, D3UV2 and D4M.3 A.3) and sarcoma (402230). First, we compared the expression level of KRT6A gene among different tumor models and ICB treatments, before and after ICB treatment, and between responders and non-responders. The results showed that the expression level of KRT6A in responders of B16_GSE151829_antiCTLA4 (n = 9) and YTN16_GSE146027_day7_antiCTLA4 (n = 9) was significantly increased compared with baseline, and there was no significant difference in other ICB treatments. Meanwhile, the expression level of KRT6A in non-responders in p53-2336R_GSE124821_end_antiCTLA4&antiPD1 (n = 11) was decreased compared with baseline (Fig. 13A, all FDR ≤ 0.05). In addition, we used the GSCA website to study the association between KRT6A and drug sensitivity in human tumors. First, based on the CTRP database, we analyzed the relationship between KRT6A mRNA and drug sensitivity and found that the expression of KRT6A was negatively correlated with the 50% inhibitory concentration (IC50) values of Afatinib, Erlotinib, Gefitinib, Ibrutinib, Lapatinib, Neratinib, PD 153,035, Saracatinib and Vandetanib (Fig. 13B, all FDR ≤ 0.05). Secondly, we also analyzed the GDSC database and found that the higher the expression of KRT6A mRNA, the lower the IC50 values of 17-AAG, 681,640, Afatinib, AICAR, Bleomycin, Bosutinib, Cetuximab, Docetaxel, Epothilone B, Erlotinib, Gefitinib, JNK Inhibitor VIII, Lapatinib, RO-3306, Trametinib and WZ-1-84 (Fig. 13C, all FDR ≤ 0.05). Therefore, we believe that the expression level of KRT6A can guide us to formulate personalized anti-tumor treatment strategies for patients.
Correlation analysis between KRT6A expression and ICB treatment and drug sensitivity. (A) Comparison of KRT6A gene expression levels between different tumor models and ICB treatment, before and after ICB treatment, and between responders and non-responders. (B) Correlation between CTRP drug sensitivity and KRT6A mRNA expression. (C) Correlation between GDSC drug sensitivity and KRT6A mRNA expression. *, **, and *** represent FDR ≤ 0.05, FDR ≤ 0.01, and FDR ≤ 0.001, respectively. FDR values less than or equal to 0.05 were considered statistically significant.
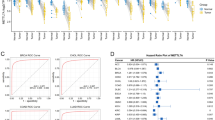
Correlation verification of KRT6A in LUAD clinical cohort
In order to further verify the above results, we selected the LUAD clinical cohort to explore the expression difference and regulatory function of KRT6A in more depth. First, we combined multiple external public datasets in the TCGA and GEO databases. The results showed that KRT6A mRNA was abnormally highly expressed in LUAD tissues compared with normal lung tissues (P < 0.05), KRT6A showed high diagnostic performance (AUC > 0.7), and high expression of KRT6A predicted worse prognosis in LUAD patients (HR > 1, P < 0.05) (Fig. 14A-D). In addition, in order to test the expression of KRT6A protein in the primary tumor tissue and adjacent normal tissue of LUAD patients, we performed immunohistochemistry staining and imaging of LUAD tissue microarray and found that the expression level of KRT6A protein in LUAD tissue samples was significantly higher than that in adjacent normal tissue samples (Fig. 14E). It is worth mentioning that, in order to further explore the specific mechanism and function of KRT6A in regulating the development of LUAD, we performed GSEA analysis of KRT6A and its co-expressed genes in LUAD based on the TCGA database using the LinkedOmics platform. The GO-BP results showed that KRT6A and its co-expressed genes were mainly involved in the positive regulation of skin development, epidermis development and peptide cross-linking (Fig. 14F, FDR ≤ 0.05). The GO-CC results showed that the above genes mainly promoted the formation of intermediate filament cytoskeleton, cornified envelope and cell-substrate junction (Fig. 14G, FDR ≤ 0.05). GO-MF results showed that high expression of KRT6A and its co-expressed genes could induce structural constituent of cytoskeleton, cell adhesion molecule binding and protease binding (Fig. 14H, FDR ≤ 0.05). Subsequently, we performed KEGG enrichment analysis, and the results showed that the above genes were mainly involved in the negative regulation of butanoate metabolism and valine, leucine and isoleucine degradation processes (Fig. 14I, FDR ≤ 0.05). In summary, these findings are consistent with our previous research results, further confirming the expression and regulatory role of KRT6A in LUAD.
Validation analysis of KRT6A in LUAD clinical cohort. (A–D) Based on the clinical data sets of TCGA and GEO, the expression of KRT6A in LUAD and its correlation with disease diagnosis and patient prognosis were verified. (E) Representative immunohistochemistry images of KRT6A in tumor tissues and adjacent normal tissues of LUAD patients. (F–I) GSEA analysis of KRT6A in the LUAD cohort was performed thru the LinkedOmics database, and the bar charts show the GO-BP, GO-CC, GO-MF and KEGG analysis results related to the KRT6A gene, respectively. *, **, and *** represent P < 0.05, P < 0.01, and P < 0.001, respectively. Generally, P < 0.05 and/or FDR ≤ 0.05 were considered statistically significant.
Discussion
KRT6A is a member of the keratin family, which not only participates in the formation of epithelial tissues such as human skin, nails and hair, but also has biological functions such as damage repair, mitochondrial regulation and immune regulation19,22. In recent years, with the continuous deepening of research, KRT6A has been proved to participate in and regulate the proliferation, migration and invasion of various tumor cells to affect the development process of different tumors, such as BLCA, NSCLC, NPC, COAD and PAAD, and is closely related to the survival prognosis of these tumor patients23,24,25,26,56,57,−58. However, the expression level, molecular mechanism, and relationship with TIME and treatment sensitivity of KRT6A in human pan-cancer are still unclear. Therefore, it is necessary to conduct a comprehensive and systematic pan-cancer analysis to explore the biological activity and potential therapeutic value of KRT6A from the perspective of the overall tumor. In this study, we used a variety of bioinformatics methods to reveal the differential expression of KRT6A in different tumors and its expression levels in different cancer stages, tumor grades, immune subtypes, and molecular subtypes, and explored the survival and prognostic value of KRT6A in human tumors. At the same time, we also analyzed the gene mutation, DNA methylation, RNA methylation and protein phosphorylation levels of KRT6A in human pan-cancer. In addition, we explored the single-cell expression distribution of KRT6A and studied the correlation between KRT6A and TMB, MSI, TSC, immune checkpoints, immune regulatory genes, and immune infiltration. More interestingly, we also evaluated the relationship between KRT6A and ICB treatment and drug sensitivity. Finally, we further verified the expression difference and regulatory function of KRT6A in the LUAD clinical cohort to confirm its potential mechanism in regulating the development process of LUAD.
Based on the TCGA and GTEx databases, we found that KRT6A mRNA was highly expressed in 9 cancer types and lowly expressed in 14 cancer types. The over expression and/or low expression of KRT6A mRNA in the above different tumors may be affected by epigenetics, lineage plasticity, microRNA targeting, microenvironment regulation, and genetic inactivation59,60,61,62. Meanwhile, the differential expression of KRT6A protein was further demonstrated by UALCAN and HPA databases. Based on the TISIDB platform, we also found that the expression of KRT6A was different when multiple tumors were in different clinical stages and grades. More interestingly, the expression level of KRT6A was significantly correlated with different immune subtypes and molecular subtypes of cancer, which also suggested that we could further explore the regulatory function and molecular mechanism of KRT6A in cancer by targeting specific immune or molecular subtypes. In addition, we also analyzed the correlation between the expression level of KRT6A and the survival prognosis of tumor patients. The results showed that the high expression of KRT6A predicted poor OS, DFS and RFS in most tumor patients. Previous in vivo and in vitro experiments have confirmed that KRT6A can promote the development of tumors and predict the poor prognosis of individual tumors63,64which is consistent with the above research results.
Hereditary or acquired chromosomal aberrations can regulate the development of different human tumors by up-regulating or down-regulating the expression levels of genes related to cell proliferation and differentiation, cell cycle and apoptosis. It has been confirmed that normal cells can be transformed into cancer cells by somatic mutations of key genes65,66. The KRT6A gene is located at chr12:52487176–52,493,257. It has been reported that KRT6A mutations can destroy keratin structure, activate inflammatory and immune pathways, and then induce diseases such as congenital pachyonychia67,68. However, there is still a lack of research on the changes of KRT6A gene in human tumors. Here, we found that mutation, amplification and deep deletion were the main types of variation of KRT6A gene, which could occur in various cancer types. Compared with the unaltered groups, the changes of TTN, MUC16, ADAM21P1, TTC9-DT, SYNJ2BP-COX16, IGHJ4, ADAM20P1, SNORD56B, LINC01500 and LINC00520 in the KRT6A altered groups were significantly increased. DNA methylation is a common type of epigenetic modification, which can play a vital role in gene expression, genome stability and tumor development by changing the structure of chromosomes, DNA conformation and stability69,70. It has been reported that abnormal DNA promoter methylation can participate in and regulate cell proliferation and development, induce cell senescence and apoptosis, and then accelerate the development of tumors71,72. In this study, our evidence showed that the DNA methylation level of KRT6A was down-regulated in most tumors, which was also consistent with the high expression of KRT6A mRNA. In addition, RNA methylation has now been shown to affect mRNA stability, splicing, and translation, regulate gene expression levels, and participate in the occurrence, development, and prognosis of various tumors73,74,75. Our study found that the expression of KRT6A was positively correlated with the RNA modification genes of most tumors. Therefore, further studies are needed to investigate the genetic alterations of KRT6A and the specific relationship between DNA and RNA methylation and the expression level of KRT6A in different tumors.
Protein phosphorylation is an important post-translational modification process in cells. It regulates the function and activity of proteins by adding phosphate groups to specific amino acid residues of proteins, and then participates in biological functions such as enzyme activity, intermolecular interaction and cell signal transduction76. It has been reported that protein phosphorylation can also participate in and regulate the proliferation, migration, invasion and immune escape of tumor cells, thus affecting the development of tumors77,78. In our study, multiple sites of KRT6A protein were highly phosphorylated in COAD, HNSC, LUAD, LUSC and PAAD tissues compared with the corresponding normal tissues. However, there is currently a lack of basic research verification of the phosphorylation modification of KRT6A protein, and more experiments are needed in the future to evaluate the potential role of KRT6A protein phosphorylation modification in the development of cancer.
TMB and MSI are ideal biomarkers for survival prognosis of patients with different tumors, and are also regarded as predictors of the efficacy of tumor immunotherapy43,79. In general, human tumors with high TMB and MSI expression have better response results to immunotherapy80. Our results showed that high expression of KRT6A predicted higher TMB in BRCA, CESC, KICH, and KIRC, and also indicated higher MSI in LUSC, SARC, TGCT, and UVM. Meanwhile, TSC is a quantitative indicator constructed based on the expression characteristics of stem cell-related genes. A higher TSC usually indicates higher epithelial-mesenchymal transition activity, cancer stem cell characteristics and genomic instability, and predicts stronger tumor invasion and metastasis ability81,82. Our study found that the expression level of KRT6A was positively correlated with the TSC of BRCA, CESC, CHOL, PRAD, SARC, THCA and THYM. In addition, immune checkpoint genes can maintain the balance of the immune system by inhibiting or promoting the function of immune cells, and are also important targets for ICB treatment of various cancers83. Immunomodulatory genes can affect the occurrence and development of tumors by regulating the activity, proliferation, and differentiation of immune cells, as well as the interaction between immune cells and tumor cells84. Our results showed that KRT6A was correlated with immune checkpoint genes, immunomodulatory genes, stromal scores, immune scores, and ESTIMATE scores in most tumor types, suggesting that KRT6A could interact with a variety of tumor cells and immune cells, thereby regulating the development of tumors.
TIME plays a vital role in the occurrence and development, migration and invasion, metastasis and diffusion of different human tumors, as well as in cancer diagnosis, treatment and prognosis85,86. The TIME is composed of cellular and non-cellular components, and the cellular components mainly include immune cells and fibroblasts87. Our study found that the expression of KRT6A was positively correlated with myeloid dendritic cells, MDSC, mast cells, neutrophils and cancer associated fibroblasts in the TIME of multiple tumors, and negatively correlated with T cells CD8+, plasmacytoid dendritic cells, T cells CD4+, B cells, NK cells, T cells gamma delta, Tregs, endothelial cells, hematopoietic stem cells and macrophages. Myeloid dendritic cells, MDSC, mast cells, neutrophils and cancer associated fibroblasts have been proven to be important promoters of the occurrence and development of various tumors. Myeloid dendritic cells can promote the occurrence and development of cancer by antigen presentation and induction of immune tolerance88. MDSC can support tumor growth by suppressing anti-tumor immune responses, promoting angiogenesis and tumor metastasis89. Inflammatory mediators released by mast cells can promote tumor cell proliferation, angiogenesis, and metastasis90. Neutrophils can play a pro-tumor role by releasing factors that support tumor growth and angiogenesis91. In addition, cancer associated fibroblasts can play a pro-cancer role by remodeling the tumor microenvironment, promoting angiogenesis, and supporting tumor cell survival and proliferation92. It is worth mentioning that immune-related cells such as T cells CD8+, T cells CD4+, B cells, NK cells, T cells gamma delta, endothelial cells and hematopoietic stem cells can inhibit the development of human pan-cancer. Among them, T cells CD8 + and T cells CD4 + can interact with each other and directly kill tumor cells through the perforin and granzyme pathways93,94. B cells play a role in cancer suppression by secreting antibodies and participating in immune regulation95. The results of Marhamati et al. also confirmed that the expression level of KRT6A in ESCA was negatively correlated with the infiltration of immune cells such as B cells and T cells CD4+, and the overexpression of KRT6A predicted a poor prognosis for ESCA patients63. NK cells, as innate immune cells, can secrete cytokines to kill cancer cells96. T cells gamma delta can kill cancer cells through multiple pathways such as secreting tumor growth inhibitory factors97. In addition, endothelial cells and hematopoietic stem cells can also affect the occurrence and development of different tumors by regulating tumor angiogenesis, affecting tumor nutrition supply, and participating in genetic engineering modification98,99,100. Based on the results of this study, we believe that KRT6A may selectively regulate the infiltration level of the above-mentioned immune cells, mediate the immune escape process of tumor cells, and then affect the development process of different tumors. However, these regulatory relationships have not been verified by a large number of basic experimental studies. In the future, we need to consider starting from this perspective to conduct more in-depth research and exploration.
The immunotherapeutic drugs commonly used in clinical practice at the present stage mainly include PD-1, PD-L1 and CTLA-4 inhibitors, which are widely used because they can be used as an alternative to autonomous treatment or can be administered in combination with other treatment regimens such as chemotherapy and/or radiotherapy, and have shown significant practical therapeutic effects in most human tumors101,102. In order to further understand the potential application value of KRT6A in tumor immunotherapy, we further studied the expression of KRT6A in different tumor models and treatment regimens using the TISMO database. The results showed that the expression level of KRT6A in responders was significantly higher than that of baseline after anti-CTLA-4 treatment, suggesting that subjects with high expression of KRT6A were more likely to produce effects after anti-CTLA-4 treatment. This also highlights the importance of considering the expression level of KRT6A and its association with immunotherapy when developing personalized treatment strategies to maximize treatment effects. It is worth mentioning that we also studied the correlation between KRT6A mRNA and the sensitivity of anti-cancer drugs with the help of CTRP and GDSC databases. The results of the CTRP database showed that the IC50 values of 9 drugs were negatively correlated with the overexpression of KRT6A. Meanwhile, the IC50 values of 16 drugs in the GDSC database were negatively correlated with the high expression of KRT6A. The IC50 values of Afatinib, Gefitinib and Erlotinib in the above two databases all showed a significant negative correlation with KRT6A, indicating that the expression of KRT6A can affect the anti-tumor therapeutic effect of the above drugs. Gefitinib and Erlotinib are first-generation reversible epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors, and Afatinib is an irreversible EGFR and human epidermal growth factor receptor 2 (HER2) tyrosine kinase inhibitor. All of them are used for the first-line treatment of NSCLC patients with EGFR mutation positive, which can significantly improve the OS and progression-free survival (PFS) of patients103,104. Currently, the above-mentioned drugs are mainly used in the clinic for NSCLC patients with EGFR mutations. The relevant clinical trials in other types of tumors are still relatively scarce. In the future, multi-center large-sample clinical trials are still needed to further verify our conjecture.
Based on the current research direction, we further explored and confirmed the expression difference and regulatory function of KRT6A in the LUAD clinical cohort. The analysis results of the three datasets in the GEO database all showed that KRT6A mRNA was highly expressed in LUAD tissues, had high diagnostic performance, and predicted a worse prognosis for patients. These results are consistent with the analysis results of the TCGA database we previously analyzed. Meanwhile, our immunohistochemistry results showed that the expression level of KRT6A protein in LUAD tissue samples was significantly higher than that in adjacent normal tissue samples, which was consistent with the analysis results of UALCAN and HPA databases in the previous study. KRT6A has been shown to be abnormally highly expressed in LUAD, which can promote the proliferation and metastasis of LUAD cells by regulating tumor stem cell conversion and epithelial-mesenchymal transition, and predicts positive lymph node metastasis and higher clinical stage of patients105. In addition, KRT6A can upregulate the expression level of G6PD and increase the pentose phosphate pathway to support the growth and proliferation of LUAD cells25. Exogenous inhibition or knockout of KRT6A can significantly inhibit LUAD cell proliferation and tumor growth64. It is worth mentioning that highly expressed KRT6A and its co-expressed genes can also promote processes such as epidermis development, intermediate filament cytoskeleton, and cornified envelope106,107which is also consistent with our GSEA analysis results. Combined with the research results of KRT6A and tumor clinical subtypes, gene genetic changes, DNA methylation, RNA methylation, protein phosphorylation, TIME and drug treatment in this study, we speculate that KRT6A may participate in the regulation of LUAD development and survival prognosis through the above pathways and mechanisms, but there is no in vivo and in vitro experiments to further verify, these scientific problems need us to carry out more in-depth research and exploration in the future.
Although our study has conducted a comprehensive and systematic analysis of KRT6A and used a variety of external public databases for cross-validation, there are still some limitations in this study. First, our pan-cancer research results are based on bioinformatics analysis, and only some features of KRT6A have been confirmed by immunohistochemistry in LUAD. Further studies should pay attention to exogenous inhibition and/or induction of KRT6A expression, and use in vitro and/or in vivo experiments to verify our predictions. Secondly, although we first proposed that the expression of KRT6A is closely related to the prognosis and immune infiltration of patients with different human tumors, we currently lack direct evidence that KRT6A regulates immune infiltration to affect the occurrence and development of cancer, and the exact mechanism of action still needs to be studied in more depth. In addition, we urgently need large-scale clinical cohort studies to explore the actual predictive value of KRT6A for the prognosis of pan-cancer and the efficacy of immunotherapy, which requires a lot of time and energy.
Conclusion
In summary, this comprehensive and systematic pan-cancer study of a single gene mainly describes the differential expression of KRT6A in different tumors and its correlation with patient survival prognosis, clinical subtypes, DNA methylation, RNA methylation, protein phosphorylation, single-cell distribution, TMB, MSI, TSC, immune checkpoints, immune regulatory genes, immune infiltration, immunotherapy, and drug sensitivity. Secondly, we further evaluated the expression characteristics, genetic variation patterns, and related functional enrichment of KRT6A in human pan-cancer. In addition, we also confirmed the expression differences and regulatory functions of KRT6A in the LUAD clinical cohort. The results showed that KRT6A was differentially expressed in a variety of tumor types, and it is expected to become a very potential biomarker related to the survival prognosis and immunity of tumor patients. This study clarified the potential role of KRT6A in tumorigenesis from multiple perspectives, and provided new insights for in-depth study of the specific mechanism of KRT6A in the development process and actual treatment of tumors.
Data availability
The databases used in this study are all publicly available and can be found in the TCGA database (https://portal.gdc.cancer.gov), the UCSC XENA database (https://xenabrowser.net/datapages/), the UCSC Genome Browser (https://genome.ucsc.edu/index.html), the GTEx Portal website (https://gtexportal.org/home/), the HPA website (https://www.proteinatlas.org/), the TIMER2.0 website (https://timer.cistrome.org/), the UALCAN database (https://ualcan.path.uab.edu), the TISIDB database (https://cis.hku.hk/TISIDB/index.php), the GEPIA2 platform (https://gepia2.cancer-pku.cn/), the Kaplan-Meier Plotter platform (https://kmplot.com), the cBioPortal platform (https://www.cbioportal.org), the SMART website (https://www.bioinfo-zs.com/smartapp/), the CPTAC database (https://cptac-data-portal.georgetown.edu), the TISCH2 database (https://tisch.comp-genomics.org/home/), the STRING website (https://cn.string-db.org), the TISMO platform (http://tismo.cistrome.org), the GSCA database (https://guolab.wchscu.cn/GSCA/), the GEO database (https://www.ncbi.nlm.nih.gov/geo/), and the LinkedOmics database (https://linkedomics.org/login.php).
References
Siegel, R. L., Kratzer, T. B., Giaquinto, A. N., Sung, H. & Jemal, A. Cancer statistics, 2025. CA Cancer J. Clin. 75, 10–45. https://doi.org/10.3322/caac.21871 (2025).
Schwartz, S. M. Epidemiology of cancer. Clin. Chem. 70, 140–149. https://doi.org/10.1093/clinchem/hvad202 (2024).
Qiang, Y. et al. Tumor organoid model and its Pharmacological applications in tumorigenesis prevention. Curr. Mol. Pharmacol. 16, 435–447. https://doi.org/10.2174/1874467215666220803125822 (2023).
Alwahsh, M., Abumansour, H., Althaher, A. R. & Hergenröder, R. Metabolic profiling techniques and their application in cancer research. Curr. Pharm. Anal. 20, 485–499. https://doi.org/10.2174/0115734129317614240809053901 (2024).
Joyson, P. et al. An update on recently developed analytical and Bio-analytical methods for some anticancer drugs. Curr. Pharm. Anal. 19, 117–135. https://doi.org/10.2174/1573412919666221123110420 (2023).
Boshuizen, J. & Peeper, D. S. Rational cancer treatment combinations: an urgent clinical need. Mol. Cell. 78, 1002–1018. https://doi.org/10.1016/j.molcel.2020.05.031 (2020).
Mullard, A. Addressing cancer’s grand challenges. Nat. Rev. Drug Discov. 19, 825–826. https://doi.org/10.1038/d41573-020-00202-0 (2020).
Martinez-Jimenez, F. & Chowell, D. Genetic immune escape in cancer: timing and implications for treatment. Trends Cancer. 11, 286–294. https://doi.org/10.1016/j.trecan.2024.11.002 (2025).
Dagogo-Jack, I. & Shaw, A. T. Tumour heterogeneity and resistance to cancer therapies. Nat. Rev. Clin. Oncol. 15, 81–94. https://doi.org/10.1038/nrclinonc.2017.166 (2018).
Passaro, A. et al. Cancer biomarkers: emerging trends and clinical implications for personalized treatment. Cell 187, 1617–1635. https://doi.org/10.1016/j.cell.2024.02.041 (2024).
Wang, Z., Jensen, M. A. & Zenklusen, J. C. A practical guide to the cancer genome atlas (TCGA). Methods Mol. Biol. 1418, 111–141. https://doi.org/10.1007/978-1-4939-3578-9_6 (2016).
Consortium, G. T. Human genomics. The Genotype-Tissue expression (GTEx) pilot analysis: multitissue gene regulation in humans. Science 348, 648–660. https://doi.org/10.1126/science.1262110 (2015).
Liu, Y., Zhang, S., Liu, K., Hu, X. & Gu, X. Advances in drug discovery based on network Pharmacology and omics technology. Curr. Pharm. Anal. 21, 33–43. https://doi.org/10.1016/j.cpan.2024.12.002 (2024).
Chen, J., Lin, A. & Luo, P. Advancing pharmaceutical research: A comprehensive review of cutting-edge tools and technologies. Curr. Pharm. Anal. 21, 1–19. https://doi.org/10.1016/j.cpan.2024.11.001 (2024). https://doi.org/.
Shahrajabian, M. H. & Sun, W. L. Survey on Multi-omics, and Multi-omics data analysis, integration and application. Curr. Pharm. Anal. 19, 267–281. https://doi.org/10.2174/1573412919666230406100948 (2023).
Qiu, J. et al. Pan-cancer analysis identifies AIMP2 as a potential biomarker for breast cancer. Curr. Genomics. 24, 307–329. https://doi.org/10.2174/0113892029255941231014142050 (2023).
Jiang, M. et al. Integrated analysis of clinical outcome of mesenchymal stem Cell-related genes in Pan-cancer. Curr. Genomics. 25, 298–315. https://doi.org/10.2174/0113892029291247240422060811 (2024).
Zhang, Y. et al. Pan-Cancer Single-Cell analysis revealing the heterogeneity of Cancer-Associated fibroblasts in skin tumors. Curr. Gene Ther. https://doi.org/10.2174/0115665232331353240911080642 (2024).
Forrest, C. E., Casey, G., Mordaunt, D. A., Thompson, E. M. & Gordon, L. Pachyonychia congenita: A spectrum of KRT6a mutations in Australian patients. Pediatr. Dermatol. 33, 337–342. https://doi.org/10.1111/pde.12841 (2016).
Chang, H. H., Dreyfuss, J. M. & Ramoni, M. F. A transcriptional network signature characterizes lung cancer subtypes. Cancer 117, 353–360. https://doi.org/10.1002/cncr.25592 (2011).
Kalabusheva, E. P. et al. A kaleidoscope of keratin gene expression and the mosaic of its regulatory mechanisms. Int. J. Mol. Sci. 24, 5603. https://doi.org/10.3390/ijms24065603 (2023).
Smack, D. P., Korge, B. P. & James, W. D. Keratin and keratinization. J. Am. Acad. Dermatol. 30, 85–102. https://doi.org/10.1016/s0190-9622(94)70012-5 (1994).
Chen, Y. et al. KRT6A expedites bladder cancer progression, regulated by miR-31-5p. Cell. Cycle. 21, 1479–1490. https://doi.org/10.1080/15384101.2022.2054095 (2022).
Xu, Q. et al. Keratin 6A (KRT6A) promotes radioresistance, invasion, and metastasis in lung cancer via p53 signaling pathway. Aging (Albany N Y). 16, 7060–7072. https://doi.org/10.18632/aging.205742 (2024).
Che, D. et al. KRT6A promotes lung cancer cell growth and invasion through MYC-Regulated Pentose phosphate pathway. Front. Cell. Dev. Biol. 9, 694071. https://doi.org/10.3389/fcell.2021.694071 (2021).
Chen, C. & Shan, H. Keratin 6A gene Silencing suppresses cell invasion and metastasis of nasopharyngeal carcinoma via the beta–catenin cascade. Mol. Med. Rep. 19, 3477–3484. https://doi.org/10.3892/mmr.2019.10055 (2019).
Burgess, D. J. Reaching completion for GTEx. Nat. Rev. Genet. 21, 717. https://doi.org/10.1038/s41576-020-00296-7 (2020).
Li, T. et al. TIMER2.0 for analysis of tumor-infiltrating immune cells. Nucleic Acids Res. 48, W509–W514. https://doi.org/10.1093/nar/gkaa407 (2020).
Vivian, J. et al. Toil enables reproducible, open source, big biomedical data analyses. Nat. Biotechnol. 35, 314–316. https://doi.org/10.1038/nbt.3772 (2017).
Chandrashekar, D. S. et al. An update to the integrated cancer data analysis platform. Neoplasia 25. UALCAN, 18–27. https://doi.org/10.1016/j.neo.2022.01.001 (2022).
Ru, B. et al. TISIDB: an integrated repository portal for tumor-immune system interactions. Bioinformatics 35, 4200–4202. https://doi.org/10.1093/bioinformatics/btz210 (2019).
Tang, Z., Kang, B., Li, C., Chen, T. & Zhang, Z. GEPIA2: an enhanced web server for large-scale expression profiling and interactive analysis. Nucleic Acids Res. 47, W556–W560. https://doi.org/10.1093/nar/gkz430 (2019).
Gyorffy, B. Integrated analysis of public datasets for the discovery and validation of survival-associated genes in solid tumors. Innov. (Camb). 5, 100625. https://doi.org/10.1016/j.xinn.2024.100625 (2024).
Gyorffy, B. Transcriptome-level discovery of survival-associated biomarkers and therapy targets in non-small-cell lung cancer. Br. J. Pharmacol. 181, 362–374. https://doi.org/10.1111/bph.16257 (2024).
Wu, P. et al. Integration and analysis of CPTAC proteomics data in the context of cancer genomics in the cBioPortal. Mol. Cell. Proteom. 18, 1893–1898. https://doi.org/10.1074/mcp.TIR119.001673 (2019).
Gao, J. et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal. 6, pl1. https://doi.org/10.1126/scisignal.2004088 (2013).
Cerami, E. et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2, 401–404. https://doi.org/10.1158/2159-8290.CD-12-0095 (2012).
Baylin, S. B. & Herman, J. G. DNA hypermethylation in tumorigenesis: epigenetics joins genetics. Trends Genet. 16, 168–174. https://doi.org/10.1016/s0168-9525(99)01971-x (2000).
Li, Y., Ge, D. & Lu, C. The SMART app: an interactive web application for comprehensive DNA methylation analysis and visualization. Epigenetics Chromatin. 12, 71. https://doi.org/10.1186/s13072-019-0316-3 (2019).
Han, X., Wang, M., Zhao, Y. L., Yang, Y. & Yang, Y. G. RNA methylations in human cancers. Semin Cancer Biol. 75, 97–115. https://doi.org/10.1016/j.semcancer.2020.11.007 (2021).
Pan, S. & Chen, R. Pathological implication of protein post-translational modifications in cancer. Mol. Aspects Med. 86, 101097. https://doi.org/10.1016/j.mam.2022.101097 (2022).
Han, Y. et al. TISCH2: expanded datasets and new tools for single-cell transcriptome analyses of the tumor microenvironment. Nucleic Acids Res. 51, D1425–D1431. https://doi.org/10.1093/nar/gkac959 (2023).
Jardim, D. L., Goodman, A., de Melo Gagliato, D. & Kurzrock, R. The challenges of tumor mutational burden as an immunotherapy biomarker. Cancer Cell. 39, 154–173. https://doi.org/10.1016/j.ccell.2020.10.001 (2021).
Hause, R. J., Pritchard, C. C., Shendure, J. & Salipante, S. J. Classification and characterization of microsatellite instability across 18 cancer types. Nat. Med. 22, 1342–1350. https://doi.org/10.1038/nm.4191 (2016).
Ashburner, M. et al. Gene ontology: tool for the unification of biology. The gene ontology consortium. Nat. Genet. 25, 25–29. https://doi.org/10.1038/75556 (2000).
Gene Ontology, C. et al. The gene ontology knowledgebase in 2023. Genetics 224, iyad031. https://doi.org/10.1093/genetics/iyad031 (2023).
Kanehisa, M. & Goto, S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 28, 27–30. https://doi.org/10.1093/nar/28.1.27 (2000).
Kanehisa, M. Toward Understanding the origin and evolution of cellular organisms. Protein Sci. 28, 1947–1951. https://doi.org/10.1002/pro.3715 (2019).
Kanehisa, M., Furumichi, M., Sato, Y., Kawashima, M. & Ishiguro-Watanabe, M. KEGG for taxonomy-based analysis of pathways and genomes. Nucleic Acids Res. 51, D587–D592. https://doi.org/10.1093/nar/gkac963 (2023).
Zeng, Z. et al. TISMO: syngeneic mouse tumor database to model tumor immunity and immunotherapy response. Nucleic Acids Res. 50, D1391–D1397. https://doi.org/10.1093/nar/gkab804 (2022).
Liu, C. J. et al. GSCA: an integrated platform for gene set cancer analysis at genomic, Pharmacogenomic and Immunogenomic levels. Brief. Bioinform. 24, bbac558. https://doi.org/10.1093/bib/bbac558 (2023).
Mori, H. & Cardiff, R. D. Methods of immunohistochemistry and immunofluorescence: converting invisible to visible. Methods Mol. Biol. 1458, 1–12. https://doi.org/10.1007/978-1-4939-3801-8_1 (2016).
Xiao, J., Kuang, X., Dai, L., Zhang, L. & He, B. Anti-tumour effects of keratin 6A in lung adenocarcinoma. Clin. Respir J. 14, 667–674. https://doi.org/10.1111/crj.13182 (2020).
Wang, W. et al. Pan-cancer analysis reveals MTTP as a prognostic and immunotherapeutic biomarker in human tumors. Front. Immunol. 16, 1549965. https://doi.org/10.3389/fimmu.2025.1549965 (2025).
Vasaikar, S. V., Straub, P., Wang, J. & Zhang, B. LinkedOmics: analyzing multi-omics data within and across 32 cancer types. Nucleic Acids Res. 46, D956–D963. https://doi.org/10.1093/nar/gkx1090 (2018).
Harada-Kagitani, S. et al. Keratin 6A is expressed at the invasive front and enhances the progression of colorectal cancer. Lab. Invest. 104, 102075. https://doi.org/10.1016/j.labinv.2024.102075 (2024).
Yang, Y. et al. Sinapine thiocyanate exhibited anti-colorectal cancer effects by inhibiting KRT6A/S100A2 axis. Cancer Biol. Ther. 24, 2249170. https://doi.org/10.1080/15384047.2023.2249170 (2023).
Zhang, J. et al. Alteration of tumor-associated macrophage subtypes mediated by KRT6A in pancreatic ductal adenocarcinoma. Aging (Albany N Y). 12, 23217–23232. https://doi.org/10.18632/aging.104091 (2020).
Diggins, N. L. & Hancock, M. H. Viral MiRNA regulation of host gene expression. Semin Cell. Dev. Biol. 146, 2–19. https://doi.org/10.1016/j.semcdb.2022.11.007 (2023).
Gibney, E. R. & Nolan, C. M. Epigenetics and gene expression. Heredity (Edinb. 105, 4–13. https://doi.org/10.1038/hdy.2010.54 (2010).
Shivdasani, R. A. MicroRNAs: regulators of gene expression and cell differentiation. Blood 108, 3646–3653. https://doi.org/10.1182/blood-2006-01-030015 (2006).
Terekhanova, N. V. et al. Epigenetic regulation during cancer transitions across 11 tumour types. Nature 623, 432–441. https://doi.org/10.1038/s41586-023-06682-5 (2023).
Marhamati, S. et al. KRT6A, KRT6B, PKP1, and PKP3 as key hub genes in esophageal cancer: A combined bioinformatics and experimental study. Biochem. Biophys. Rep. 43, 102095. https://doi.org/10.1016/j.bbrep.2025.102095 (2025).
Zhou, J. et al. Identification of SRXN1 and KRT6A as key genes in Smoking-Related Non-Small-Cell lung cancer through bioinformatics and functional analyses. Front. Oncol. 11, 810301. https://doi.org/10.3389/fonc.2021.810301 (2021).
Pandya, P. H., Murray, M. E., Pollok, K. E. & Renbarger, J. L. The Immune System in Cancer Pathogenesis: Potential Therapeutic Approaches. J. Immunol. Res. 4273943. (2016). https://doi.org/10.1155/2016/4273943 (2016).
Martinez-Jimenez, F. et al. A compendium of mutational cancer driver genes. Nat. Rev. Cancer. 20, 555–572. https://doi.org/10.1038/s41568-020-0290-x (2020).
Abdollahimajd, F. et al. Pachyonychia congenita: a case report of a successful treatment with Rosuvastatin in a patient with a KRT6A mutation. Br. J. Dermatol. 181, 584–586. https://doi.org/10.1111/bjd.17276 (2019).
Spaunhurst, K. M. et al. Pachyonychia congenita patients with mutations in KRT6A have more extensive disease compared with patients who have mutations in KRT16. Br. J. Dermatol. 166, 875–878. https://doi.org/10.1111/j.1365-2133.2011.10745.x (2012).
Mattei, A. L., Bailly, N. & Meissner, A. DNA methylation: a historical perspective. Trends Genet. 38, 676–707. https://doi.org/10.1016/j.tig.2022.03.010 (2022).
Wang, M., Ngo, V. & Wang, W. Deciphering the genetic code of DNA methylation. Brief. Bioinform. 22, bbaa424. https://doi.org/10.1093/bib/bbaa424 (2021).
Papanicolau-Sengos, A. & Aldape, K. D. N. A. Methylation profiling: an emerging paradigm for cancer diagnosis. Annu. Rev. Pathol. 17, 295–321. https://doi.org/10.1146/annurev-pathol-042220-022304 (2022).
Nishiyama, A. & Nakanishi, M. Navigating the DNA methylation landscape of cancer. Trends Genet. 37, 1012–1027. https://doi.org/10.1016/j.tig.2021.05.002 (2021).
Han, M. et al. Effects of RNA methylation on tumor angiogenesis and cancer progression. Mol. Cancer. 22, 198. https://doi.org/10.1186/s12943-023-01879-8 (2023).
An, Y. & Duan, H. The role of m6A RNA methylation in cancer metabolism. Mol. Cancer. 21, 14. https://doi.org/10.1186/s12943-022-01500-4 (2022).
Yang, B. et al. RNA methylation and cancer treatment. Pharmacol. Res. 174, 105937. https://doi.org/10.1016/j.phrs.2021.105937 (2021).
Bilbrough, T., Piemontese, E. & Seitz, O. Dissecting the role of protein phosphorylation: a chemical biology toolbox. Chem. Soc. Rev. 51, 5691–5730. https://doi.org/10.1039/d1cs00991e (2022).
Singh, V. et al. Phosphorylation: implications in cancer. Protein J. 36, 1–6. https://doi.org/10.1007/s10930-017-9696-z (2017).
Watanabe, N. & Osada, H. Phosphorylation-dependent protein-protein interaction modules as potential molecular targets for cancer therapy. Curr. Drug Targets. 13, 1654–1658. https://doi.org/10.2174/138945012803530035 (2012).
Zhang, P., Liu, M., Cui, Y., Zheng, P. & Liu, Y. Microsatellite instability status differentially associates with intratumoral immune microenvironment in human cancers. Brief. Bioinform. 22, bbaa180. https://doi.org/10.1093/bib/bbaa180 (2021).
Palmeri, M. et al. Real-world application of tumor mutational burden-high (TMB-high) and microsatellite instability (MSI) confirms their utility as immunotherapy biomarkers. ESMO Open. 7, 100336. https://doi.org/10.1016/j.esmoop.2021.100336 (2022).
Loh, J. J. & Ma, S. Hallmarks of cancer stemness. Cell. Stem Cell. 31, 617–639. https://doi.org/10.1016/j.stem.2024.04.004 (2024).
Zhang, Y. et al. Tumor stemness score to estimate epithelial-to-mesenchymal transition (EMT) and cancer stem cells (CSCs) characterization and to predict the prognosis and immunotherapy response in bladder urothelial carcinoma. Stem Cell. Res. Ther. 14, 15. https://doi.org/10.1186/s13287-023-03239-1 (2023).
Postow, M. A., Sidlow, R. & Hellmann, M. D. Immune-Related adverse events associated with immune checkpoint Blockade. N Engl. J. Med. 378, 158–168. https://doi.org/10.1056/NEJMra1703481 (2018).
Pansy, K. et al. Immune regulatory processes of the tumor microenvironment under malignant conditions. Int. J. Mol. Sci. 22, 13311. https://doi.org/10.3390/ijms222413311 (2021).
Liu, C. et al. Tumor microenvironment and immunotherapy of oral cancer. Eur. J. Med. Res. 27, 198. https://doi.org/10.1186/s40001-022-00835-4 (2022).
Xiao, Y. & Yu, D. Tumor microenvironment as a therapeutic target in cancer. Pharmacol. Ther. 221, 107753. https://doi.org/10.1016/j.pharmthera.2020.107753 (2021).
Sharma, P., Hu-Lieskovan, S., Wargo, J. A., Ribas, A. & Primary Adaptive, and acquired resistance to cancer immunotherapy. Cell 168, 707–723. https://doi.org/10.1016/j.cell.2017.01.017 (2017).
Collin, M. & Bigley, V. Human dendritic cell subsets: an update. Immunology 154, 3–20. https://doi.org/10.1111/imm.12888 (2018).
Kumar, V., Patel, S., Tcyganov, E. & Gabrilovich, D. I. The nature of Myeloid-Derived suppressor cells in the tumor microenvironment. Trends Immunol. 37, 208–220. https://doi.org/10.1016/j.it.2016.01.004 (2016).
Aponte-Lopez, A. & Munoz-Cruz, S. Mast cells in the tumor microenvironment. Adv. Exp. Med. Biol. 1273, 159–173. https://doi.org/10.1007/978-3-030-49270-0_9 (2020).
McFarlane, A. J., Fercoq, F., Coffelt, S. B. & Carlin, L. M. Neutrophil dynamics in the tumor microenvironment. J. Clin. Invest. 131, e143759. https://doi.org/10.1172/JCI143759 (2021).
Biffi, G. & Tuveson, D. A. Diversity and biology of Cancer-Associated fibroblasts. Physiol. Rev. 101, 147–176. https://doi.org/10.1152/physrev.00048.2019 (2021).
Park, J., Hsueh, P. C., Li, Z. & Ho, P. C. Microenvironment-driven metabolic adaptations guiding CD8(+) T cell anti-tumor immunity. Immunity 56, 32–42. https://doi.org/10.1016/j.immuni.2022.12.008 (2023).
Borst, J., Ahrends, T., Babala, N., Melief, C. J. M. & Kastenmuller, W. CD4(+) T cell help in cancer immunology and immunotherapy. Nat. Rev. Immunol. 18, 635–647. https://doi.org/10.1038/s41577-018-0044-0 (2018).
Conejo-Garcia, J. R., Biswas, S., Chaurio, R. & Rodriguez, P. C. Neglected no more: B cell-mediated anti-tumor immunity. Semin Immunol. 65, 101707. https://doi.org/10.1016/j.smim.2022.101707 (2023).
Vivier, E. et al. Natural killer cell therapies. Nature 626, 727–736. https://doi.org/10.1038/s41586-023-06945-1 (2024).
Gao, Z. et al. Gamma delta T-cell-based immune checkpoint therapy: attractive candidate for antitumor treatment. Mol. Cancer. 22, 31. https://doi.org/10.1186/s12943-023-01722-0 (2023).
Wang, Y. Y., Wu, Z. Z., Huang, C. F. & Sun, Z. J. Tumor-host colluding through erythroid progenitor cells: mechanisms and opportunities. Cancer Lett. 563, 216193. https://doi.org/10.1016/j.canlet.2023.216193 (2023).
Sobierajska, K., Ciszewski, W. M., Sacewicz-Hofman, I. & Niewiarowska, J. Endothelial cells in the tumor microenvironment. Adv. Exp. Med. Biol. 1234, 71–86. https://doi.org/10.1007/978-3-030-37184-5_6 (2020).
McDonald, L. T. et al. Hematopoietic stem cell-derived cancer-associated fibroblasts are novel contributors to the pro-tumorigenic microenvironment. Neoplasia 17, 434–448. https://doi.org/10.1016/j.neo.2015.04.004 (2015).
Robert, C. A decade of immune-checkpoint inhibitors in cancer therapy. Nat. Commun. 11, 3801. https://doi.org/10.1038/s41467-020-17670-y (2020).
Postow, M. A., Callahan, M. K. & Wolchok, J. D. Immune checkpoint Blockade in cancer therapy. J. Clin. Oncol. 33, 1974–1982. https://doi.org/10.1200/JCO.2014.59.4358 (2015).
Laskin, J. et al. NRG1 fusion-driven tumors: biology, detection, and the therapeutic role of Afatinib and other ErbB-targeting agents. Ann. Oncol. 31, 1693–1703. https://doi.org/10.1016/j.annonc.2020.08.2335 (2020).
Yang, Z. et al. Comparison of gefitinib, erlotinib and Afatinib in non-small cell lung cancer: A meta-analysis. Int. J. Cancer. 140, 2805–2819. https://doi.org/10.1002/ijc.30691 (2017).
Yang, B. et al. KRT6A promotes EMT and cancer stem cell transformation in lung adenocarcinoma. Technol. Cancer Res. Treat. 19, 1533033820921248. https://doi.org/10.1177/1533033820921248 (2020).
Shi, P. & Chen, W. Genetic distinctiveness in lung adenocarcinoma and lung squamous cell carcinoma cancer: identifying key genomic signatures through differentially expressed gene analysis. Curr. Cancer Drug Targets. https://doi.org/10.2174/0115680096372957250322174718 (2025).
Sun, K. et al. Regulation of early diagnosis and prognostic markers of lung adenocarcinoma in immunity and hypoxia. Sci. Rep. 13, 6459. https://doi.org/10.1038/s41598-023-33404-8 (2023).
Funding
This work was supported by National Natural Science Foundation of China (No. 81902347), and the Hubei Provincial Science and Technology Project of China (No. 2024BEB008).
Author information
Authors and Affiliations
Contributions
Y.L., W.P. and N.Z. developed the idea and Y.L., X.L. and Z.X. selected the corresponding methodological content; Y.L., Z.X. and X.Z. performed the preliminary data analysis; Y.L., X.L., Z.X., W.T. and Q.S. wrote the manuscript; W.P., N.Z., Q.W. and R.Z. reviewed and edited the article; W.P. and N.Z. managed the project. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology. All participants provided written informed consent and complied with the declaration of Helsinki.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lv, Y., Liu, X., Xiao, Z. et al. Comprehensive pan-cancer analysis of KRT6A as a prognostic and immune biomarker. Sci Rep 15, 35728 (2025). https://doi.org/10.1038/s41598-025-19599-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-19599-y
















