Abstract
In systemic lupus erythematosus (SLE), treatment decisions are guided by clinical judgment based on disease manifestations and safety profiles rather than standardized protocols, particularly for extra-renal involvement. In this study of 356 SLE patients, 190 receiving non-biologic immunosuppressants and 166 receiving biologics, we investigated the association of clinical phenotypes with treatment initiation and the impact of damage (SLICC-DI), comorbidities, and hospitalization history on these choices. Dominant clinical phenotypes were defined qualitatively using BILAG and SLEDAI domains. Logistic regression models with Simes-Hochberg correction revealed that renal phenotypes were strongly associated with mycophenolate initiation (OR = 4.09, p < 0.001), musculoskeletal phenotypes with methotrexate (OR = 4.86, p < 0.001). Belimumab was preferentially initiated in patients with musculoskeletal involvement and high SLEDAI scores (OR = 1.84, p = 0.03; OR = 2.03, p = 0.03, respectively). Notably, the association between mycophenolate and the renal phenotype persisted in the presence of comorbidities but was not observed in patients with SLICC-DI > 0 or more than one hospitalization in the previous year. Similarly, methotrexate and belimumab associations were diminished in patients with a Charlson comorbidity index > 1 or damage (SLICC-DI > 0). This study offers novel insights into the clinical determinants of immunosuppressive therapy selection in SLE and underscore the potential for tailoring treatment strategies to individual patient profiles.
Similar content being viewed by others
Introduction
Systemic lupus erythematosus (SLE) is the paradigm of systemic autoimmune diseases, characterized by extreme heterogeneity in clinical manifestations and disease course both between patients and within patients1. Despite the advances in elucidating the molecular mechanisms underlying SLE and the development of novel therapeutic strategies, patients with SLE continue to face significantly higher morbidity, reduced quality of life, and elevated mortality rates compared to the general population2,3.
Management of SLE remains a complex challenge that international guidelines address through evidence-based strategies integrating both established core principles and the latest innovations in therapeutic approaches. One notable example is the treat-to-target (T2T) approach, initially introduced in recent years and now widely accepted as a core principle in SLE management. This strategy emphasizes the goal of achieving disease remission, or low disease activity when remission is not attainable. The European League Against Rheumatism (EULAR) recommendations endorse the T2T approach4, with accumulating evidence indicating that its implementation may contribute to improved long-term outcomes and reduced cumulative organ damage over medium-term follow-up5,6.
However, the therapeutic pathway in achieving remission in SLE remains poorly defined. Hydroxychloroquine and the judicious use of glucocorticoids, with the ultimate goal of minimizing or completely sparing their use, are regarded as cornerstone therapies in the management of SLE7,8. For patients with moderate to severe disease, an optimal therapeutic strategy has yet to be standardized. Indeed, except in cases of lupus nephritis, there is a lack of high-quality evidence guiding the choice of immunosuppressants across different clinical manifestations9. EULAR recommendations place conventional non-biologic (NBI) and biologic (BI) immunosuppressants as equally suitable options, leaving the choice of specific treatment to the clinician4. The absence of standardized choices for immunosuppressive therapy-whether NBI or BI-often results in significant variability in treatment decisions, which are influenced by factors such as disease manifestations, patient age, conception potential, comorbidities, safety profile and regulatory restrictions.
Recently, the concept of disease phenotype, a categorization based on predominant organ involvement, has been proposed to facilitate the adoption of more targeted and effective therapeutic strategies. Fanouriakis et al.8, have described dermatologic, musculoskeletal, renal, neurological and haematologic SLE as organ dominant phenotypes with different prognosis and treatment strategy. Latin American Group for the Study of Lupus (GLADEL) produced the first SLE clinical practice guidelines to clearly present different treatment strategies for different organ involvement10; in Europe, the most recent EULAR recommendations are still based on the concept of global disease activity4, however the experts produced specific statements for renal, cutaneous, neuropsychiatric and haematological SLE management4,11.
However, the complexity in lupus patients extends beyond the diverse clinical phenotypes of SLE: comorbidities and adverse events often limit therapeutic options, creating scenarios that current guidelines partially address. To further refine the therapeutic algorithm for managing moderate to severe SLE patients, registry and observational data derived from real-world experience provide invaluable insights, offering evidence that can bridge the gap between clinical guidelines and the needs of everyday practice. Using a multicentre Italian registry of patients undergoing routine clinical management, our study aims to: 1) assess the association between different clinical phenotypes and the use of specific BI or NBI therapies; and 2) evaluate the impact of various demographic and clinical factors, such as disease activity, damage, comorbidities, and hospitalization history, on the choice between BI and NBI treatments.
Methods
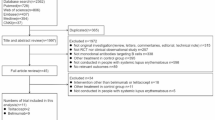
This is a cross-sectional analysis from the multicentre, non-profit, observational cohort study, the Lupus Italian REgistry (LIRE), promoted by the Italian Society of Rheumatology (SIR). The LIRE was established in 2015 and designed to assess the five-year risk and probability of efficacy and safety of NBI and BI in patients with SLE12. The patients fulfilling the 2012 Systemic Lupus International Collaborating Clinics (SLICC) were diagnosed by expert physicians13. The study included SLE patients aged 16 years or older who were initiating either a BI (such as belimumab or rituximab) or a NBI (such as methotrexate, azathioprine, cyclophosphamide, cyclosporin, tacrolimus, or mycophenolate) at their first visit, while excluding those with prior exposure to biologic drugs.
Belimumab was approved in Italy in February 2013, with reimbursement granted for adult patients with active, autoantibody-positive SLE exhibiting high disease activity despite standard therapy (SLE disease activity index, SLEDAI ≥ 10, or ≥ 8 combined with serological activity). Conventional NBI (e.g., methotrexate, azathioprine, mycophenolate, cyclophosphamide, tacrolimus) had no formal reimbursement criteria and were prescribed based on clinical judgment. The patients were enrolled between January 2015 and June 2022. All drugs analyzed in this study were accessible throughout the entire study period. The following variables were recorded: socio-demographic data, clinical and serological characteristics at disease onset (first SLE-attributable symptom) and at study entry disease duration, laboratory findings (including anti-dsDNA, C3 and C4 serum complement fractions tested in local laboratories at each centre), active clinical manifestations (ie, categorised as present/absent) according to the British Isles Lupus Assessment Group’s (BILAG) index glossary14, SLEDAI-2K)15, Physician Global Assessment (PhGA) on a scale of 0–10016; irreversible organ damage (SLICC/ACR Damage Index, SLICC-DI)17 and ongoing treatments. A high-moderate SLEDAI was defined as a baseline SLEDAI-2K score of ≥ 6. Comorbidities were evaluated using the Charlson Comorbidity Index18, and the number of hospitalizations within the 12 months prior to enrolment was recorded.
The following clinical phenotypes were analyzed according to the predominant disease manifestations, based on BILAG (mucocutaneous, neuropsychiatric, musculoskeletal, cardiorespiratory, gastrointestinal, ophthalmic, renal, and hematological) or SLEDAI domains (vasculitis, mucocutaneous, neuropsychiatric, musculoskeletal, cardiorespiratory, renal, and hematological). The total scores of both instruments were not used to quantitatively assess disease activity; instead, they were applied qualitatively to characterize the full spectrum of clinical phenotypes observed or potentially manifesting in SLE.
Study data were collected and managed using REDCap electronic data capture tools, hosted by the Italian Society for Rheumatology19. Written informed consent was obtained from all patients at the time of enrolment, covering both study participation and publication of the results.
This study was conducted in full accordance with the principles outlined in the Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of the Coordinating Center (Ethics Committee for Clinical Trials of the Province of Padua, approval code 3524/AO/15), as well as from the institutional review boards of all participating centres involved in the study.
Statistical analysis
Descriptive statistics were expressed as means (SD) and median (IQR) in case of continuous variables, as absolute and relative frequencies when categorical.
Simple correspondence analysis was employed to visualize the crude association between clinical phenotypes and treatment initiation20. Then, unadjusted and adjusted logistic regression models formally tested treatment-phenotype associations in an exploratory analysis framework: of all combinations of treatment initiation and phenotypes, we developed adjusted models only for those showing association at the univariable analysis. In addition, to control for confounding by concomitant medications, a composite treatment intensity variable was created. This continuous variable incorporated weighted contributions from hydroxychloroquine (+ 0.5), glucocorticoids (+ 1.0), and additional immunosuppressants (+ 1.5). The treatment intensity variable was standardized to a mean of zero and unit variance. Interaction effects between phenotype -including treatment intensity- and confounder variables were formally tested.
Due to the high number of statistical tests on model parameters, control of the false discovery rate was implemented using the Simes-Benjamini–Hochberg correction21,22. Missing data were excluded from the analysis.
All analyses were performed using R version 4.4.1 (R Foundation for Statistical Computing, 2024, Vienna, Austria).
Results
Clinical manifestations and phenotypes at study entry
A total of 356 patients diagnosed with SLE were enrolled in this study. Among them, 190 started NBI therapy and 166BI therapy. Baseline characteristics of these patients are reported in Table 1. The two groups had comparable mean age (42.0 years in BI vs. 43.9 years in NBI, p = 0.196), conversely, disease duration from diagnosis was higher in BI cohort (mean 12.2 years in BI vs. 9.9 years in NBI, p = 0.001). Considering clinical and immunological features at the time of enrolment, no statistically significant difference was observed in renal involvement between the two groups (38.9% in NBI vs. 33.7% in BI, p = 0.364). In contrast, anti-dsDNA antibody positivity was significantly more frequent in the BI cohort (78.2% vs. 53.2% in NBI, p < 0.001). Disease activity and damage accrual were similar in the two cohorts, as expressed by mean SLEDAI-2k and SLICC-DI.
The Charlson index, was similar in the two cohorts; however, patients in the BI cohort experienced significantly fewer hospitalizations for all causes in the 12 months preceding the start of immunosuppressive therapy compared to patients in the NBI cohort .
In our cohort, musculoskeletal was the most frequently scored BILAG domain (52.2%), followed by mucocutaneous, renal, and haematological (42.4%, 36.5%, and 32.2%, respectively). Vasculitis, ophthalmic, and gastrointestinal phenotypes were rare in our study population. Musculoskeletal involvement was the only BILAG domain significantly more frequent in the BI cohort compared to the NBI cohort (58.4% vs. 46.8%, p = 0.038) (Table 1).
Treatment and SLE phenotypes
Upon analysing pharmacological history at study entry, no substantial differences emerged between the two cohorts in terms of concomitant therapy, even when considering treatment with anticoagulants and antiplatelet therapy.
The BI cohort exhibited a higher frequency of ongoing steroid therapy at study entry (88.8% in BI cohort vs. 78% in NBI, p = 0.019) and greater steroid exposure during the course of the disease with 61.2% of BI patients having a cumulative prednisone dose > 10 g compared to 34.6% in the NBI cohort (p = 0.001). HCQ therapy was used in 71.1% of patients in the BI cohort and 68.3% in the NBI cohort (p = 0.644). Initiation of HCQ at enrolment occurred in 6.6% of patients in the NBI cohort and 2.6% in the BI cohort (p = 0.085). Belimumab was the most frequent therapy in the total cohort (141/356; 39.9%) and in BI cohort (141/165; 85.5%). In NBI cohort, mycophenolate mofetil therapy was the most frequent, followed by methotrexate and azathioprine . See supplementary Table 1 for additional data. Over time, the proportion of patients receiving BI increased steadily, while the use of NBI declined accordingly (See supplementary Fig. 2, Table 2).
Applying univariate analysis, we tested associations between BI/NBI therapies and specific SLE phenotypes in our cohort. We observed a positive association between mycophenolate treatment and renal phenotype [OR 4.09 (2.20, 7.61); p < 0.001] and methotrexate and musculoskeletal phenotype [OR 4.86 (2.19, 10.79); p < 0.001]. Treatment with belimumab was associated with musculoskeletal phenotype [OR 1.84 (1.19, 2.83); p = 0.03] and high-moderate SLEDAI score [OR 2.03 (1.22, 3.40); p = 0.03].
We observed negative associations between mycophenolate treatment and musculoskeletal phenotype [OR 0.43 (0.23, 0.79); p = 0.03]; azathioprine and high SLEDAI values [OR 0.22 (0.11, 0.44), p < 0.001]. We recorded a positive association between cyclosporin treatment and vasculitic phenotype [OR 6.85 (2.35, 19.91); p < 0.001], and haematological phenotype [OR 2.77 (1.06, 7.23); p = 0.14] however, due to a very small sample size, we considered the last one at high risk of bias (Table 2 and Fig. 1). We did not find significant associations for leflunomide, cyclophosphamide, tacrolimus and rituximab treatment. The analysis highlights a strong alignment between clinical phenotypes and treatment choices in SLE, with renal phenotypes linked to mycophenolate, cyclophosphamide and tacrolimus, and musculoskeletal phenotypes associated with methotrexate and belimumab, underscoring the phenotype-driven nature of therapeutic decisions.
Correspondence analysis: association between variables is represented as distance in a two dimensional space, the closer two variables are, the stronger the positive association is. The figure illustrates the phenotypic clustering of SLE manifestations and their corresponding therapeutic associations, emphasizing the strong phenotype-driven rationale in treatment selection, particularly the alignment of renal phenotypes with MMF, CYC, and TAC, and musculoskeletal phenotypes with MTX and BEL. AZA Azathioprine, BEL Belimumab, CYC Cyclophosphamide, CYA Cyclosporine A, LEF Leflunomide, MMF Mycophenolate mofetil, MTX Methotrexate, RTX Rituximab, TAC Tacrolimus.
Immunosuppressive treatment and interaction with comorbidities, damage and hospitalization
To further investigate the propensity for initiating either BI or NBI therapies across different phenotypes and immunosuppressants, we evaluated the interactions with potential confounding factors, including comorbidities, hospitalizations, and organ damage (Table 3). The association between mycophenolate therapy and renal phenotype was confirmed in the presence of comorbidities, but not in the case of SLICC-DI > 0 (OR 8.66, 95%CI 0.98, 76.24, p = 0.129) or more than one hospitalization in the previous year (OR 2.98, 95%CI 1.06, 8.37, p = 0.190; Table 3). The association between the musculoskeletal phenotype and methotrexate therapy remained statistically significant, except when the Charlson comorbidity index was greater than 1 (OR 4.14, 95% CI 0.57, 30.18, p = 0.333; Table 3). Belimumab and musculoskeletal phenotype remained associated in the presence of single comorbidity, but not in patients with hospitalizations- (OR 1.40, 95%CI 0.81, 2.41, p = 0.439), Charlson index > 1 (OR 1.47, 95%CI 0.67, 3.24, p = 0.582) or SLICC-DI > 0 (OR 2.51, 95%CI 0.60, 10.46, p = 0.409); similarly, the association between belimumab therapy and high/moderate SLEDAI was confirmed in the presence of single comorbidities and frequent hospitalizations but lost significance in patients with acquired damage (OR 2.29, 95%CI 0.43, 12.11, p = 0.578) and a Charlson index > 1 (OR 2.22, 95%CI 0.89, 5.57, p = 0.202; Table 3). No significant interactions were observed for cyclosporin and vasculitic phenotype. The propensity-adjusted analysis, which accounted for concomitant therapies including glucocorticoids, hydroxychloroquine, and combinations with other immunosuppressants, showed results consistent with the previous model (supplementary Table 3).
Discussion
This study provides a comprehensive real-life analysis of the factors influencing treatment decisions in SLE, considering not only disease manifestations but also acquired damage, hospitalizations and comorbidities. In our cohort, predominant disease manifestations, such as renal or musculoskeletal involvement, played a key role in treatment selection, with mycophenolate preferred for renal involvement, and methotrexate and belimumab for musculoskeletal manifestations. Belimumab use was also associated with moderate-to-high SLEDAI scores; however, this may have been influenced by country-specific regulatory prescribing requirements. The presence of acquired damage (SLICC-DI > 1) or hospitalization in the previous year reduced the likelihood of prescribing mycophenolate in cases of renal involvement. Acquired damage and a Charlson index > 1 attenuated the association to non-significance between belimumab and moderate-to-high disease activity, as well as between belimumab and methotrexate and musculoskeletal manifestations. In contrast, individual comorbidities did not significantly influence these treatment-phenotype associations.
Although the efficacy of therapeutic regimens based on mycophenolate and cyclophosphamide for renal SLE is well-documented and their use is endorsed by current international treatment guidelines4,11,23, the choice of immunosuppressive agents for specific extrarenal manifestations of SLE remains challenging due to the paucity of high-quality evidence in this area, as highlighted by a recent systematic review by Kostopoulou et al.24. A limited number of randomized controlled trials (RCTs) and prospective observational studies have investigated the use of methotrexate in the management of cutaneous and articular manifestations of SLE reporting improvements in the SLEDAI scores. Notably, disease-specific measures for musculoskeletal involvement, such as tender and swollen joint counts, as well as skin-specific indices like the Cutaneous Lupus Activity and Severity Index, were often absent in these studies, leading to a gap in the comprehensive assessment of both articular and cutaneous improvement25. Regarding belimumab, RCTs have demonstrated its significant effectiveness in patients with both joint and skin involvement in SLE26. Recent real-life data and a systematic review and meta-analysis further confirm these findings27,28,29.
However, it is well known that SLE patients included in clinical trials are not completely representative of those managed in routine clinical practice. Our study underscores how the individual complexities associated with acquired damage, comorbidities, and hospitalization history can jeopardize our confidence in managing patients with SLE. Our analysis indicated that despite the presence of dominant disease phenotypes, acquired damage (SLICC-DI > 1) or multiple hospitalizations in the past year, the likelihood of prescribing immunosuppressive therapy (mycophenolate for the renal phenotype and methotrexate for the musculoskeletal phenotype) was reduced. This trend was also observed for the use of belimumab. One possible interpretation of these findings is that treatment decisions are influenced by multiple factors beyond disease manifestations alone. Specifically, clinicians appeared to adopt a more cautious approach when managing patients deemed vulnerable, such as those at high risk of infections due to comorbidities or previous hospitalizations. An additional insight from our data highlights the role of physicians’ perceptions regarding the safety of therapies. At the time of our study, belimumab was still a relatively new treatment option, and rheumatologists had primarily gained experience with biologics in other settings, such as rheumatoid arthritis. Concerns regarding its safety profile likely influenced clinicians’ treatment decisions, particularly in patients with complex comorbidities. This reveals the crucial role that familiarity and confidence with a therapy play in its clinical use.
Data analysing the role of comorbidities in SLE treatment are scarce and information on this aspect can only be deducted by studies on safety profiles of different immunosuppressants. A recent study attempted to identify predictors of adverse events associated with conventional immunosuppressive therapy30. However, only moderate to low-quality evidence supports the prognostic value of factors such as demographic characteristics, lifestyle, comorbidities, and baseline laboratory or serologic markers. Given the need to treat moderate to severe SLE manifestations, a careful balance between benefits and harms is essential, particularly in complex patients. A Cochrane metanalysis of different RCTs found no differences between belimumab and placebo on serious infections and adverse events, although this evidence came from moderate to poor quality data31; different real life experience confirm though the good safety profile of belimumab29,32. One systematic literature review investigated adverse events rate for different SLE therapy found an increased risk of serious leukopenia and ovarian failure with cyclophosphamide compared with other NBI and belimumab, but didn’t find an increased risk of cardiovascular events or serious infections33. RCTs or their post hoc analysis often exclude patients with comorbidities, as happened with belimumab34. Consequently, real-world data, despite their inherent limitations, provide a crucial contribution to improving the management of complex SLE patients.
This study has several limitations that warrant discussion. First, the predefined design with equal sample sizes for the biologic and non-biologic cohorts does not accurately reflect the true prevalence of biologic use in the SLE population. This approach introduces a potential selection bias and may distort the observed associations with disease phenotypes. For instance, belimumab emerged as the most frequently prescribed biologic in the cohort, but its association with specific phenotypes could have been influenced by this sampling approach. Second, the study is subject to a cohort effect bias35. At the time of patient enrolment, belimumab was still relatively new, and its safety profile, particularly regarding the risk of infections or its use in patients with complex comorbidities, was not as well-established as it is today. This has likely influenced clinicians’ therapeutic preferences and led to more cautious use of belimumab, even in patients with high disease activity or musculoskeletal involvement. Since then, the increase real-world evidence has significantly expanded the understanding of belimumab’s safety and efficacy, potentially altering its current utilization patterns. In particular, robust data now support the drug’s safety and tolerability, especially with regard to its infectious risk compared to conventional immunosuppressants36. These advancements may have influenced its current use, as indicated by a rising preference for biologic treatments over time (supplementary Fig. 2), potentially reflecting evolving clinical practice standards and prescribing guidelines. Nonetheless, our findings, collected during an earlier period, may not fully capture contemporary clinical practice. In addition, anifrolumab was not available in routine clinical practice during the study period. Its recent introduction is expected to shift therapeutic strategies, emphasizing the need for updated analyses to understand the evolving landscape of SLE management37,38.
Third, the exploratory nature of our analysis, coupled with the assessment of multiple interactions, inherently reduces statistical power. This limitation may have contributed to the lack of significant associations for less commonly used therapies, such as rituximab and cyclophosphamide, with the renal phenotype. The small sample sizes for these treatments, compounded by rigorous corrections for multiple testing, underscore the need for caution when interpreting these results.
Lastly, the dynamic nature of SLE treatment decisions introduces complexity and highlights additional biases, such as the influence of physician experience and perception of treatment safety. While challenging to quantify, these factors likely have a substantial impact on therapeutic choices, particularly for patients with complex clinical profiles.
A key strength of this study lies in its use of real-life data from a large, multi-centre cohort of patients managed in specialized SLE clinics. This approach reflects the practical, day-to-day management of SLE, providing valuable insights into how expert rheumatologists navigate the complex decision-making process in treating lupus. The integration of comorbidities, hospitalization history, and cumulative damage into therapy choices offers important information on the factors influencing treatment decisions. The large cohort allows for a robust analysis of treatment patterns across various disease manifestations or "phenotypes," a concept that is increasingly important in SLE management. Moreover, our analysis highlights that clinicians’ perception of treatment safety and their familiarity with therapies significantly impact treatment choice. Interplay between clinical judgment and external factors, often steering decisions beyond the assessment of disease activity alone. This emphasizes the need for continued research and education to enhance clinicians’ confidence in using novel therapies, especially in patients with complex comorbidities or greater fragility, where clinical activity alone may not be the sole determinant. In conclusion the management of SLE presents a significant clinical challenge, as it requires harmonizing guideline-based recommendations with individualized treatment approaches.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Barr, S. G., Zonana-Nacach, A., Magder, L. S. & Petri, M. Patterns of disease activity in systemic lupus erythematosus. Arthritis Rheum. 42, 2682–2688 (1999).
Bertsias, G. K., Salmon, J. E. & Boumpas, D. T. Therapeutic opportunities in systemic lupus erythematosus: State of the art and prospects for the new decade. Ann. Rheum. Dis. 69, 1603–1611 (2010).
Bultink, I. E. M., de Vries, F., van Vollenhoven, R. F. & Lalmohamed, A. Mortality, causes of death and influence of medication use in patients with systemic lupus erythematosus vs matched controls. Rheumatology 60, 207–216 (2021).
Fanouriakis, A. et al. EULAR recommendations for the management of systemic lupus erythematosus: 2023 update. Ann. Rheum. Dis. 83, 15–29 (2024).
Parra Sánchez, A. R., Voskuyl, A. E. & Van Vollenhoven, R. F. Treat-to-target in systemic lupus erythematosus: Advancing towards its implementation. Nat. Rev. Rheumatol. 18, 146–157 (2022).
Pitsigavdaki, S. et al. Pragmatic targets for moderate/severe SLE and their implications for clinical care and trial design: sustained DORIS or LLDAS for at least 6 months is sufficient while their attainment for at least 24 months ensures high specificity for damage-free progression. Ann. Rheum. Dis. 83, 464–474 (2024).
Fanouriakis, A. et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann. Rheum. Dis. 78, 736–745 (2019).
Fanouriakis, A., Tziolos, N., Bertsias, G. & Boumpas, D. T. Update οn the diagnosis and management of systemic lupus erythematosus. Ann. Rheum. Dis. 80, 14–25 (2021).
Morand, E. F., Fernandez-Ruiz, R., Blazer, A. & Niewold, T. B. Advances in the management of systemic lupus erythematosus. BMJ 383, e073980 (2023).
Bernardo A Pons-Estel et al. First Latin American clinical practice guidelines for the treatment of systemic lupus erythematosus: Latin American Group for the Study of Lupus (GLADEL, <em>Grupo Latino Americano de Estudio del Lupus</em>)–Pan-American League of Associations of Rheumatology (PANLAR). Ann. Rheum. Dis. 77, 1549 (2018).
Fanouriakis, A. et al. 2019 update of the joint European league against rheumatism and european renal association-european dialysis and transplant association (EULAR/ERA–EDTA) recommendations for the management of lupus nephritis. Ann. Rheum. Dis. 79, 713–723 (2020).
Sebastiani, G. D. et al. Baseline characteristics of systemic lupus erythematosus patients included in the Lupus Italian registry of the Italian Society for Rheumatology. Lupus 30, 1233–1243 (2021).
Petri, M. et al. Derivation and validation of the systemic lupus international collaborating clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. 64, 2677–2686 (2012).
Isenberg, D. A. et al. BILAG 2004 Development and initial validation of an updated version of the British Isles Lupus Assessment Group’s disease activity index for patients with systemic lupus erythematosus. Rheumatology 44(7), 902–906 (2005).
Gladman, D. D., Ibañez, D. & Urowitz, M. B. Systemic lupus erythematosus disease activity index 2000. J. Rheumatol. 29, 288–291 (2002).
Piga, M. et al. Physician global assessment international standardisation consensus in systemic lupus erythematosus: The PISCOS study. Lancet Rheumatol. 4, e441–e449 (2022).
Gladman, D. et al. The development and initial validation of the systemic lupus international collaborating clinics/American College of Rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum. 39, 363–369 (1996).
Deyo, R. A., Cherkin, D. C. & Ciol, M. A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J. Clin. Epidemiol. 45, 613–619 (1992).
Harris, P. A. et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 95, 103208 (2019).
Žlahtič, B., Kokol, P., Blažun Vošner, H. & Završnik, J. The role of correspondence analysis in medical research. Front. Public Health 12, 1362699 (2024).
Haynes, W. Benjamini–Hochberg Method. in Encyclopedia of Systems Biology (eds. Dubitzky, W., Wolkenhauer, O., Cho, K.-H. & Yokota, H.) 78–78 (Springer, New York, NY, 2013). https://doi.org/10.1007/978-1-4419-9863-7_1215.
Sarkar, S. K. Simes’ Test in Multiple testing. in International Encyclopedia of Statistical Science (ed. Lovric, M.) 1325–1327 (Springer, Berlin, Heidelberg, 2011). https://doi.org/10.1007/978-3-642-04898-2_516.
Rovin, B. H. et al. KDIGO 2024 clinical practice guideline for the management of LUPUS NEPHRITIS. Kidney Int. 105, S1–S69 (2024).
Kostopoulou, M., Mukhtyar, C. B., Bertsias, G., Boumpas, D. T. & Fanouriakis, A. Management of systemic lupus erythematosus: A systematic literature review informing the 2023 update of the EULAR recommendations. Ann. Rheum. Dis. https://doi.org/10.1136/ard-2023-225319 (2024).
Sakthiswary, R. & Suresh, E. Methotrexate in systemic lupus erythematosus: a systematic review of its efficacy. Lupus 23, 225–235 (2014).
Van Vollenhoven, R. F. et al. Belimumab in the treatment of systemic lupus erythematosus: high disease activity predictors of response. Ann. Rheum. Dis. 71, 1343–1349 (2012).
Zen, M. et al. Early and late response and glucocorticoid-sparing effect of belimumab in patients with systemic lupus erythematosus with joint and skin manifestations: results from the belimumab in real life setting study-joint and skin (BeRLiSS-JS). J. Pers. Med. 13, 691 (2023).
Gatto, M. et al. Early disease and low baseline damage as predictors of response to belimumab in patients with systemic lupus erythematosus in a real-life setting. Arthritis Rheumatol. Hoboken NJ 72, 1314–1324 (2020).
Iaccarino, L. et al. Clinical predictors of response and discontinuation of belimumab in patients with systemic lupus erythematosus in real life setting. Results of a large, multicentric, nationwide study. J. Autoimmun. 86, 1–8 (2018).
Leaviss, J. et al. Prognostic factors for liver, blood and kidney adverse events from glucocorticoid sparing immune-suppressing drugs in immune-mediated inflammatory diseases: A prognostic systematic review. RMD Open 10, e003588 (2024).
Singh, J. A., Shah, N. P. & Mudano, A. S. Belimumab for systemic lupus erythematosus. Cochrane Database Syst. Rev. 2(2), CD010668 (2021).
Lin, S. et al. Efficacy and safety of belimumab in patients with lupus nephritis: a real-world retrospective observational study. Rheumatology https://doi.org/10.1093/rheumatology/kead707 (2023).
Tian, J. et al. Risk of adverse events from different drugs for SLE: A systematic review and network meta-analysis. Lupus Sci. Med. 5, e000253 (2018).
Wallace, D. et al. Safety profile of belimumab: Pooled data from placebo-controlled phase 2 and 3 studies in patients with systemic lupus erythematosus. Lupus 22, 144–154 (2013).
Ryder, N. B. The cohort as a concept in the study of social change. Am. Sociol. Rev. 30, 843–861 (1965).
Materne, E. et al. Comparative risks of infection with belimumab versus oral immunosuppressants in patients with nonrenal systemic lupus erythematosus. Arthritis Rheumatol. 75, 1994–2002 (2023).
Liu, Z., Cheng, R. & Liu, Y. Evaluation of anifrolumab safety in systemic lupus erythematosus: A meta-analysis and systematic review. Front. Immunol. 13, 996662 (2022).
Morand, E. F. et al. Efficacy of anifrolumab across organ domains in patients with moderate-to-severe systemic lupus erythematosus: A post-hoc analysis of pooled data from the TULIP-1 and TULIP-2 trials. Lancet Rheumatol. 4, e282–e292 (2022).
Acknowledgements
None
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
A.B.: conceptualization; data collection; investigation; methodology; writing original draft; A.M.: data collection, review and editing; E.S.: data collection, review and editing; D.R.: formal analysis; review and editing; E.B.: data collection, review and editing; J.B.: data collection, review and editing; F.B.P.: data collection, review and editing; E.B.: data collection, review and editing; V.C.: data collection, review and editing; L.C. : data collection, review and editing; L.C.: data collection, review and editing; I.C.: data collection, review and editing; P.C.: data collection, review and editing; F.C.: data collection, review and editing; M.C.D.: data collection, review and editing; G.E.: data collection, review and editing; S.F.: data collection, review and editing; F.F.: data collection, review and editing; M.F.: data collection, review and editing; C.G.: data collection, review and editing; M.G.: data collection, review and editing; M.G.: data collection, review and editing; S.G.: data collection, review and editing; L.I.: data collection, review and editing; A.M.: : data collection, review and editing; S.M.: data collection, review and editing; M.M.: data collection, review and editing; C.N.: data collection, review and editing; V.O.: data collection, review and editing; S.P.:data collection, review and editing; G.P.: data collection, review and editing; G.P.: data collection, review and editing; I.P.: data collection, review and editing; G.A.R.: data collection, review and editing; C.S.: data collection, review and editing; F.R.S.: data collection, review and editing; M.Z.: data collection, review and editing; G.C.: formal analysis; review and editing; C.A.S. conceptualization, formal analysis; review and editing; F.C.: data collection, review and editing; A.D.: data collection, review and editing; G.D.S.: data collection, review and editing.
Corresponding author
Ethics declarations
Competing interests
A.B. reports consulting/speaker’s fees from AstraZeneca and GSK. P.C. reports consulting fees from Astra Zeneca and GSK. F.F. reports consulting/speaker’s fees from AstraZeneca and GSK. M.G. reports consulting/speaker’s fees from AstraZeneca and GSK. S.M. reports consulting/speaker’s fees from AstraZeneca E.S. reports consulting/speaker’s fees from AbbVie, Alfa-Sigma, Lilly, UCB, Novartis A.D. reports consulting/speaker’s fees from GSK, AstraZeneca, BMS, Johnson & Johnson, Biogen, Ventus, Otsuka, Roche.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Bortoluzzi, A., Marangoni, A., Silvagni, E. et al. Factors influencing the choice of non-biologic versus biologic immunosuppressive therapy in systemic lupus erythematosus. Sci Rep 15, 35721 (2025). https://doi.org/10.1038/s41598-025-19654-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-19654-8