Abstract
The objective of this study was to evaluate the use of scout views as an adjunct tool in CT-guided intervention. Therefore, different devices used for interventional procedures were assigned to three different groups and placed onto an Alderson phantom. Different body diameters were simulated by adding PMMA/aluminum plates. Multiple scout views (ap) were acquired using a standard CT-scanner with different scan parameters. The visibility of the devices was semi-quantitatively scored by three readers. The interrater reliability was calculated using the intraclass correlation coefficient (ICC). The detectability of the 11 different interventional devices was calculated depending on tube potential, tube current–time product, and the thickness of the additional tissue equivalent. Statistical significance was evaluated using Wilcoxon signed-rank test (with Pratt modification) and the Mann–Whitney-U test, respectively. The ICC over all measurements for the three readers as well as the ICC for the three different devices groups was regarded excellent (> 0.9). The device detectability was significantly different for the different additional tissue thicknesses as well as for the three device groups. Material detectability over all readers improved with higher doses. Defining a median visibility of 3 (“good”) or 4 (“very good”) as a cut-off value for clinical routine use, we consider a combination of ≥ 80kVp / ≥ 60 mAs or ≥ 90 kVp / ≥ 40 mAs as reasonable scan parameters in normal and overweight patients in our CT setup. In conclusion, CT scout views have a potential use as an additional tool in CT-guided-intervention by enabling fluoroscopy-like planar imaging that may help to visualize dynamic events such as contrast injection or guidewire manipulation.
Similar content being viewed by others
Introduction
CT-guidance is an indispensable tool for percutaneous image-guided interventions in radiology. It is used in a broad variety of minimally invasive procedures such as biopsies of solid structures, drainage of fluid collections, placement of catheters (e.g. nephrostomy, suprapubic catheter) as well as local-ablative therapies such as radiofrequency ablation (RFA), cryoablation, microwave ablation (MWA) or electrochemotherapy (ECT)1. CT creates distortion- and (almost) artifact-free cross-sectional images of all parts of the body and therefore allows precise needle placement even in challenging anatomical situations. The standard procedure in interventional CT is usually an iterative approach: After diagnostic CT images are obtained, a trajectory is planned based on these images. Then the needle is incrementally advanced towards the lesion while repetitive thin-section low-dose CT scans are acquired to compare the actual needle position within the patient to the planned trajectory2. Although 2D real-time imaging with CT is available (CT fluoroscopy), it comes with the burden of increased radiation exposure to the patient as well as to the interventionalist3,4,5.
However, in certain CT-guided interventions, real-time fluoroscopic imaging might facilitate the procedure by visualizing dynamic events such as the injection of contrast agents or manipulation with guide wires6. Some groups and manufacturers have addressed this need by placing a C-arm in front of the CT7,8,9. However, every CT scanner has the intrinsic ability to generate fluoroscopic-like planar images. Therefore, the aim of this study is to systematically evaluate the possible use of scout views in CT-guided interventions.
Methods
Phantom
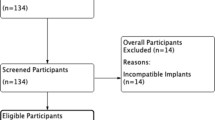
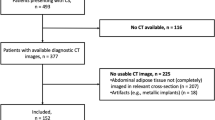
An antropomorphic Alderson phantom (Atom Dosimetry Verification Phantom, CIRS Inc., Norfolk, VA, USA) with an abdominal cross-sectional diameter of 20 × 30 cm was placed onto 1, 4 and 8 composite plates, respectively. Each plate consisted of 20 mm PMMA and 2 mm aluminum (representing 25 mm of tissue equivalent material), resulting in an additional tissue thickness of 25 mm, 100 mm and 200 mm, respectively. According to O’Neill et al. these phantom sizes correspond to patients with a body mass index of approximately 22 (normal weight), 27 (overweight) and 33 (adiposity stage 1), respectively10.
Materials
Different standard interventional devices used for interventional procedures (n = 11) were placed onto the Alderson phantom: a 5F vascular access sheath with dilator (Cordis Avanti, Cordis Germany GmbH, Deutschland), single action biopsy devices of different diameters (14G, 16G, 18G; Manan Medical Products, USA), chiba needles of different diameters (17G, 22G, 25G; Cook Medical Deutschland GmbH, Germany) and different guide wires (0.035″ TERUMO Glidewire, TERUMO Deutschland GmbH, Germany; 0.035″ TERUMO Radiofocus Sheath guidewire; 0.035″ Boston Amplatz Superstiff, Boston Scientific Medizintechnik GmbH, Germany; 0.038″ Cordis Avanti Sheath Mini-wire). Based on the imaging characteristics and similarity in detectability during a standard fluoroscopic examination, the devices were assigned to three different groups that were used for further statistical analysis (see Table 1). Group 1 consisted of the 5F sheath, the three biopsy devices (14G, 16G, 18G) and the 17G chiba needle. Group 2 comprised the 22G and 25G chiba needles as well as the three different 0.035″ steel guidewires. The hydrophilic Glidewire was allocated to group 3. A photography of the experimental setting can be seen in Fig. 1.
Scan parameters
The phantom and the devices were placed at the isocenter of a clinical MDCT scanner (Somatom Force, Siemens Healthineers, Erlangen, Germany). Multiple scout views in the a.-p.-direction were acquired by systematically modifying tube potential (70 kVp, 80 kVp, 90 kVp, 100 kVp, 110 kVp, 120 kVp) and tube-current time product (20 mAs, 30 mAs, 40 mAs, 50 mAs, 60 mAs for 25 mm/100 mm/200 mm additional tissue thickness; 80mAs, 120 mAs, 160 mAs for 100 mm and 200 mm additional tissue thickness). The CTDIvol and DLP for each scan were recorded.
For an indicative comparison of dose parameters of our approach with a standard fluoroscopic approach, the phantom was imaged using a standard angiography suite (Artis pheno, Siemens Healthineers, Erlangen, Germany). A standard clinical abdomen protocol (with reduced dose settings) was used. The collimation was adjusted to 10 cm (cranio-caudal direction) and a fluoroscopy loop of the phantom (with 25 mm/100 mm additional tissue thickness) was acquired. Dose parameters (dose area product) were extracted from the DICOM meta data. Effective dose was calculated using standard conversions factors for the abdomen according to AAPM11.
Reader study
The resulting images were independently reviewed by three readers on a diagnostic DICOM-calibrated monitor (EIZO Radiforce, EIZO Europe GmbH, Germany) using a client–server PACS installation (Visage 7, Visage Imaging, Berlin, Germany). Image window settings could be modified at the discretion of the readers. The images were presented in random order and without any meta information with regard to the scan protocol. The detectability of the different devices was semi-quantitatively evaluated using a 5-point Likert scale (0—not visible, 1—poor, 2—moderate, 3—good, 4—very good). The readers were motivated to fully exploit the range of the Likert scale.
In order to establish reasonable scan parameters for practical use, a median visibility of 3 (“good”) or 4 (“very good”) was considered sufficient for clinical routine use by two interventional radiologists not involved in the study reading and therefore defined as the cut-off value for detectability in our study.
Statistics
For statistical analysis, the open-source software package “R” (version 3.6.3, R Foundation for Statistical Computing, Vienna, Austria, https://www.R-project.org) and Microsoft Excel (Microsoft Corp., Redmond, WA, USA) were used. The interrater reliability was calculated using the intraclass correlation coefficient (ICC). The results for the three different readers were pooled and the detectability of the 11 different interventional devices was calculated depending on tube potential, tube current–time product, and the thickness of the additional tissue equivalent. Statistical significance was evaluated using Wilcoxon signed-rank test (with Pratt modification) and the Mann–Whitney-U test, respectively.
Biopsy—proof-of-concept
In a second step, a custom phantom was made of gelatine and an iodinated contrast-agent (Imeron 400, Bracco Imaging, Konstanz, Germany) as a proof-of-concept for lesion targeting. The phantom was placed at the isocenter of the MDCT scanner and a diagnostic scan was acquired. The image dataset was reconstructed and the target was identified. The laser guidance of the scanner was used to target the slice of interest. From now on, the step-wise advancement of the needle was monitored using repetitive scout view acquisitions in an iterative approach. The success of the approach was proven using an intralesional placement of a guidewire as well as an injection of a small amount of contrast media.
Results
Reader study
Overall visibility
The device detectability over all readers, devices and scan parameters was significantly different for the different additional tissue thicknesses between the three groups (25 mm (small): median = 3 (good) [IQR 2.5–4.0], 100 mm (medium): median = 3 (good) [IQR 1.5–4], 200 mm (large): median = 0 (not visible) [IQR 0–2]; p < 0.05 for all tests). The results are illustrated in Figs. 2 and 3.
The device detectability over all readers, tissue thicknesses and scan parameters was significantly different for the different device groups (group 1: median = 4 (very good) [IQR 2–4], group 2: median = 2.75 (moderate / good) [IQR 0.5–3.0], group 3: median = 1.5 (poor / moderate)[IQR 0–2]; p < 0.05 for all tests). The results are illustrated in Figs. 2 and 3.
Material detectability over all readers improved with higher doses. This was achieved by increasing either tube current or tube potential (Fig. 4).
Cutoff value
As outlined in detail in the methods section, a median visibility of 3 (“good”) or 4 (“very good”) was considered sufficient for clinical routine use.
Devices in group 1 reached a median visibility ≥ 3 for all datasets in the small phantom (CTDIvol ≥ 0.01 mGy), for all datasets ≥ 80 kVp (CTDIvol ≥ 0.02 mGy) in the medium-sized phantom and for all datasets ≥ 100 kVp/ ≥ 80 mAs (CTDIvol ≥ 0.18 mGy) or ≥ 120 kVp/ ≥ 30 mAs (CTDIvol ≥ 0.11 mGy) using the large phantom.
Devices in group 2 reached a median visibility ≥ 3 for all datasets using the small phantom, for datasets ≥ 80 kVp/ ≥ 60 mAs (CTDIvol ≥ 0.06 mGy) or ≥ 90 kVp/ ≥ 40 mAs (CTDIvol ≥ 0.06 mGy) using the medium sized phantom and for all datasets ≥ 120 kVp/ ≥ 120 mAs (CTDIvol ≥ 0.44 mGy) for the large phantom.
The device in group 3 did not reach a median visibility ≥ 3 for all dose levels and phantom sizes.
The results are illustrated in Fig. 3. In summary, the combination of ≥ 80 kVp/ ≥ 60 mAs or ≥ 90 kVp/ ≥ 40 mAs can be regarded as reasonable scan parameters in normal and overweight patients in our CT setup. In obese patients, the scan parameters must be adjusted accordingly (e.g. 120 kVp/120 mAs).
Intraclass correlation
A total of 1386 measurements were recorded (25 mm: 6 different tube potentials, 5 different mAs settings, 11 devices / 100 mm and 200 mm: 6 different tube potentials, 8 different mAs settings, 11 devices). The intraclass correlation coefficient (ICC) over all measurements for the three readers were 0.956 [95% CI: 0.952–0.96] for relative agreement (Model: twoway, Type: consistency’, ICC(C,1)) and 0.947 [95% CI: 0.922–0.962] for absolute agreement (Model: twoway, Type: agreement; ICC(A,1)). According to Koo and Li an ICC value above 0.90 can be considered as an excellent agreement12. Therefore, the results of the different readers were pooled (median) for the evaluation.
ICC was calculated for the three device groups (1–3). For group 1 (n = 630 / 5 devices) the ICC was 0.974 [0.970–0.978] for relative agreement (ICC(C,1)) and 0.969 [0.957–0.977] for absolute agreement (ICC(A,1)). For group 2 (n = 630 / 5 devices) the ICC was 0.946 [0.937–0.953] for relative agreement (ICC(C,1)) and 0.923 [0.854–0.964] for absolute agreement (ICC(A,1)). For group 3 (n = 126, 1 device) the ICC was 0.924 [0.910–0.936] for relative agreement (ICC(C,1)) and 0.914 [0.886–0.934] for absolute agreement (ICC(A,1)).
Dose
The standard settings for the abdominal scout view in clinical routine at the scanner used for this study were 120kVp / 19mAs, equivalent to a calculated CTDIvol of 0.07 mGy as recorded from the CT dose report. When compared to the minimum dose levels necessary to reach the cut-off level as described above, it can be seen, that devices from group 1 and 2 can be reliably visualized in the small and medium sized phantom at dose levels below or comparable to clinical routine scout view acquisition (Table 2). The concept of scout view guided intervention offers potential for dose reduction as a cross-sectional image is replaced with a quasi-projection acquisition.
Dose from the fluoroscopic image acquisition in the angiography suite was 0.008 mSv (25 mm additional tissue thickness) and 0,01 mSv (10 cm additional tissue thickness) for a 10 cm cranio-caudal collimation, respectively. A comparable acquisition using our scout approach would result in an estimated dose in the range of approximately 0.0015 mSv for the “small” phantom (0.01 mGy*10 cm*0.015 mSv*mGy−1*cm−1) and 0.003 mSv/0,009 mSv (0.02/0.06 mGy*10 cm*0.015 mSv*mGy−1*cm1) for the medium sized phantom and material group A / B, respectively.
Biopsy—proof-of-concept
The biopsy was performed as outlined in the Materials & Methods section and is illustrated in Fig. 5. The target in the custom-made phantom was punctured with a needle in a stepwise approach using repetitive (collimated) scout views. The success of the procedure and the potential use in clinical routine was shown by inserting and visualizing a guidewire and by performing a contrast injection in the target structure of the phantom. The depth of the lesion and the success of the puncture was evaluated by tactile feedback (loss of resistance). Additional CT scans were acquired for illustrative purposes.
(A/B): Visualization of the target structure in two planes (scout ap-view/lateral-view) and initial needle placement (C): Advancement of the needle into the target structure (scout ap-view). (D/F): A guidewire is introduced into the target structure (D: scout ap-view, F: lateral reconstruction of a CT scan for illustrative purposes). E/G: Iodinated contrast agent is injected into the target structure (E: scout ap-view, F: lateral reconstruction of a CT scan for illustrative purposes). Scan parameters for the scout were: 100kVp / 50 mAs.
Discussion
As described in the introduction, the standard procedure for CT-guided intervention is an iterative approach. Several additional tools are available to facilitate the procedure such as electromagnetic navigation or laser-guidance13,14,15,16. However, there still is a clinical need for fluoroscopic monitoring of devices in certain indications and the usage of real-time CT scanning (CT fluoroscopy) is limited by a a substantial radiation burden for both, the patient and the interventionalist, despite several technical advances to minimize the exposure17,18.
The approach described in this paper utilized the inherent 2D-imaging capabilities of CT scanners to acquire projection-like 2D images. This is applicable in every CT scanner but usually only used to generate the scout views for examination planning. While the image quality of these scout views is inferior when compared with dedicated radiography or fluoroscopy units, our results suggests that it is still sufficient for basic guidance during percutaneous interventions.
The potential advantage of a combined 2D-/3D-approach as described herein is the combination of the static high-resolution cross-sectional image with a potentially dynamic fluoroscopy-like view that allows a real-time control of the needle position. The principle need of combined 2D-/3D-approaches is well documented in the literature with custom made setups and in the portfolio of the manufacturers of imaging equipment with fixed combinations of CT and angio7,8,19,20,21.
There are a couple of shortcomings of the approach described herein that need to be addressed. First, to date, the use of CT scout views for interventional purposes has only been sparsely described in medical literature22. However, it is well documented that scout views are more than just simple imaging for planning of CT scans23. There are a couple of case reports that describe a potential benefit from including the scout view in routine CT reading as unexpected relevant findings may be identified, thereby underlining a potential diagnostic value of scout views24,25. In clinical routine, the position and integrity of central venous catheters is reviewed on scout view prior to their use for high-power flow injection of contrast agents. Furthermore, attenuation measured on scout views is routinely used for automatic exposure controls in CT.
Furthermore, while the scout-view approach does not require additional hardware in or in front of the CT scanner, no implementation of this technique can be found on commercially available scanners yet. There is no software-guidance that facilitates the process of the repetitive fluoro-like acquisition of scout views during an interventional procedure. However, combined 2D-/3D-approaches for biopsy-guidance have already been implemented in advanced angiography and x-ray / fluoroscopy systems or hybrid CT / angiography systems, that combine two different hardware units as described above19,20. However, such setups may require patient movement between two modalities whereas the integrated approach does not. As CT is still the most important modality for the guidance of non-vascular interventional procedures, it seems reasonable to upgrade CT with a 2D real-time guidance function. Based on our results we believe that enrichment of the CT scanner software with features, that enable a repetitive acquisition of a collimated scout view in real-time or—at least—in a reasonable time frame will be helpful. The increasing width of CT detectors facilitates the potential use of scout views as larger areas can be covered without table movement.
With respect to patient dose, the CTDIvol value provided by the dose report was 0.07 mGy for the clinical standard ap-scout settings. CTDIvol values given in the literature for CT-fluoroscopy acquisition settings are in the range of 0.50 mGy18. A direct comparison of our approach with standard 2D-fluoroscopy remains challenging due to the different physical units, dose parameters and measurement concepts (e.g. phantom vs. air kerma) as well as the associated uncertainties when utilizing different conversion factors. Furthermore, dose in fluoroscopy is highly dependent on the acquisition parameters of the angiography unit that is used for the intervention. However, our indicative comparison with dose values of the same phantom from a standard angiography suite suggests, that the dose of the scout views are of the same order of magnitude.
It is also known that ‘slit-scanning’ techniques show an advantageous dose performance as compared to conventional projection radiography, so it seems reasonable to assume that our approach is dose-efficient26. Furthermore, one could argue that the availability of a low-dose scout view might lead to a reduction in the number of control CT scans and thus lead to a dose reduction for the patient. However, this will have to be proven in clinical studies, when scout view technique may be available in clinical scanners.
We only evaluated ap-scout views with respect to image quality, mainly due to our experimental setting using the antropormophic phantom and the additional tissue simulation and device placed upon the phantom. We also used ap-views only in our proof-of-concept study. In a real patient setting, the use of other (arbitrary) viewing angles is usually desirable (e.g. to monitor the depth position of a puncture needle) and—in case of lateral projections—can be readily realized using standard CT equipment. Depending on the body position other scout projections might require a higher dose setting to maintain the same image quality as in ap-views. However, this effect also occurs in standard 2D-fluoroscopy and does not change the overall result of our approach.
Finally, the image quality of scout views of standard CT scanners is usually not optimized to meet diagnostic standards as delivered by dedicated 2D x-ray equipment23,27,28. However, we were able to demonstrate that this image quality is still sufficient to guide standard interventional procedures. Since the scout view has traditionally only been used to define the anatomical scan range in CT, it is not optimized for diagnostic image quality, yet. It seems reasonable to expect a significant increase in image quality when the acquisition parameters and post-processing algorithms are specifically adjusted.
In conclusion, we have demonstrated the potential usability of CT scout views as an additional tool in CT-guided intervention in a proof-of-concept study. This approach may facilitate interventional procedure which benefit from a visualization of dynamic events such as contrast injection or guidewire manipulation. Although the image quality will be inferior to a flat panel detector in an angio system, it seems worthwhile to further optimize CT scout view scanning capabilities with respect to fluoroscopy-like imaging, quality of image reconstruction and usability of the user interface.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Furlow, B. CT-Guided interventional radiology. Radiol. Technol. 90, 581–597 (2019).
Sarti, M., Brehmer, W. P. & Gay, S. B. Low-dose techniques in CT-guided interventions. Radiographics 32, 1109–1119. https://doi.org/10.1148/rg.324115072 (2012).
Prosch, H. et al. CT fluoroscopy-guided vs. multislice CT biopsy mode-guided lung biopsies: Accuracy, complications and radiation dose. Eur. J. Radiol. 81, 1029–1033. https://doi.org/10.1016/j.ejrad.2011.01.064 (2012).
Fukushima, Y. et al. Patients’ radiation dose in computed tomography-fluoroscopy-guided percutaneous cryoablation for small renal tumors. Eur. J. Radiol. 144, 109972. https://doi.org/10.1016/j.ejrad.2021.109972 (2021).
Floridi, C. et al. Precision imaging guidance in the era of precision oncology: An update of imaging tools for interventional procedures. JCM 11, 4028. https://doi.org/10.3390/jcm11144028 (2022).
Sommer, C. M. et al. Combined CT- and fluoroscopy-guided nephrostomy in patients with non-obstructive uropathy due to urine leaks in cases of failed ultrasound-guided procedures. Eur. J. Radiol. 80, 686–691. https://doi.org/10.1016/j.ejrad.2010.09.035 (2011).
Erinjeri, J. P. et al. Utilization of integrated angiography-CT interventional radiology suites at a tertiary cancer center. BMC Med. Imaging 20, 114. https://doi.org/10.1186/s12880-020-00515-x (2020).
Pfaff, J. et al. Influence of a combined CT/C-arm system on periprocedural workflow and procedure times in mechanical thrombectomy. Eur. Radiol. 27, 3966–3972. https://doi.org/10.1007/s00330-017-4762-7 (2017).
Wada, D. et al. First installation of a dual-room IVR-CT system in the emergency room. Scand. J. Trauma Resusc. Emerg. Med. 26, 17. https://doi.org/10.1186/s13049-018-0484-3 (2018).
O’Neill, S. et al. Using body mass index to estimate individualised patient radiation dose in abdominal computed tomography. Eur. Radiol. Exp. 2, 38. https://doi.org/10.1186/s41747-018-0070-5 (2018).
McCollough, C., Cody, D., Edyvean, S. et al. The measurement, reporting, and management of radiation dose in CT. AAPM (2008)
Koo, T. K. & Li, M. Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 15, 155–163. https://doi.org/10.1016/j.jcm.2016.02.012 (2016).
Becker, L. S. et al. fully integrated laser guidance for CT-based punctures: A study in phantoms and patients. J. Vasc. Interv. Radiol. 34, 130–138. https://doi.org/10.1016/j.jvir.2022.09.014 (2023).
Ringe, K. I., Pöhler, G. H., Rabeh, H. & Wacker, F. Electromagnetic navigation system-guided microwave ablation of hepatic tumors: A matched cohort study. Cardiovasc. Intervent. Radiol. 44, 500–506. https://doi.org/10.1007/s00270-020-02761-6 (2021).
Scharll, Y. et al. Laser target system in combination with an aiming device for percutaneous CT-guided interventions—An accuracy study. Acad. Radiol. 30, 3047–3055. https://doi.org/10.1016/j.acra.2023.03.028 (2023).
Lin, C.-Y. et al. Improving puncture accuracy in percutaneous CT-guided needle insertion with wireless inertial measurement unit: A phantom study. Eur. Radiol. 33, 3156–3164. https://doi.org/10.1007/s00330-023-09467-6 (2023).
Matsui, Y. et al. radiation exposure of interventional radiologists during computed tomography fluoroscopy-guided renal cryoablation and lung radiofrequency ablation: Direct measurement in a clinical setting. Cardiovasc. Intervent. Radiol. 39, 894–901. https://doi.org/10.1007/s00270-016-1308-3 (2016).
Wagner, M. G. et al. Ultra-low radiation dose CT fluoroscopy for percutaneous interventions: A porcine feasibility study. Radiology 291, 241–249. https://doi.org/10.1148/radiol.2019181362 (2019).
Kwak, D. H. et al. Hybrid CT-angiography (Angio-CT) for combined CT and fluoroscopic procedures in interventional radiology enhances utilization. Abdom. Radiol. 47, 2704–2711. https://doi.org/10.1007/s00261-022-03576-4 (2022).
Feinberg, N. et al. Improved utilization following conversion of a fluoroscopy suite to hybrid CT/Angiography system. J. Vasc. Interv. Radiol. 31, 1857–1863. https://doi.org/10.1016/j.jvir.2020.05.028 (2020).
Knox, J. A. et al. Synergy in IR–Hybrid CT/C-arm in the setting of critical trauma. Emerg. Radiol. 29, 605–609. https://doi.org/10.1007/s10140-022-02015-7 (2022).
Nunninger, M. et al. Scout-guided needle placement—A technical approach for dose reduction in CT-guided periradicular infiltration. Neuroradiology 62, 341–346. https://doi.org/10.1007/s00234-019-02339-1 (2020).
Gaspoz, F. et al. Precision and accuracy of measurements on CT scout view. J. Med. Imaging Radiat. Sci. 46, 309–316. https://doi.org/10.1016/j.jmir.2015.06.006 (2015).
Johnson, P. T. et al. The CT scout view: Does it need to be routinely reviewed as part of the CT interpretation?. Am. J. Roentgenol. 202, 1256–1263. https://doi.org/10.2214/AJR.13.10545 (2014).
Orman, G. et al. Scout view in pediatric CT neuroradiological evaluation: Do not underestimate!. Childs Nerv. Syst. 30, 307–311. https://doi.org/10.1007/s00381-013-2288-0 (2014).
Nauer, C. B. et al. Effective doses from scan projection radiographs of the head: Impact of different scanning practices and comparison with conventional radiography. AJNR Am. J. Neuroradiol. 30, 155–159. https://doi.org/10.3174/ajnr.A1293 (2009).
Colello, M. J. et al. Predicting pathologic bone lesions using scout computed tomography (CT) imaging. Sarcoma 2020, 1–8. https://doi.org/10.1155/2020/5105196 (2020).
Theocharopoulos, N. et al. CT evaluation of the low severity cervical spine trauma: When is the scout view enough?. Eur. J. Radiol. 75, 82–86. https://doi.org/10.1016/j.ejrad.2009.03.024 (2010).
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
DC: acquisition and analysis of data TW: study design, acquisition, analysis and interpretation of data SW: conception and design of study, substantial revision of manuscript FW: conception and design of study, substantial revision of manuscript CvF: conception and design of study, interpretation of data, draft and substantial revision of manuscript All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Conroy, D., Werncke, T., Waldeck, S. et al. The potential use of scout views as an adjunct tool in CT-guided intervention. Sci Rep 15, 34298 (2025). https://doi.org/10.1038/s41598-025-22040-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-22040-z