Abstract
Atherosclerosis (AS) is a chronic vascular disease characterized by inflammation of the arterial wall and the formation of cholesterol plaques. Hashimoto’s thyroiditis (HT) is an autoimmune disorder marked by chronic inflammation and destruction of thyroid tissue. Although previous studies have identified common risk factors between AS and HT, the specific etiology and pathogenic mechanisms underlying these associations remain unclear. We obtained relevant datasets for AS and HT from the Gene Expression Omnibus (GEO). By employing the Limma package, we pinpointed common differentially expressed genes (DEGs) and discerned co-expression modules linked to AS and HT via Weighted Gene Co-expression Network Analysis (WGCNA). We elucidated gene functions and regulatory networks across various biological scenarios through enrichment and pathway analysis using Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG). Core genes were identified using Cytoscape software and further validated with external datasets. We also conducted immune infiltration analysis on these core genes utilizing the CIBERSORT method. Lastly, Single-cell analysis was instrumental in uncovering common diagnostic markers. Based on differential analysis and WGCNA, we identified 119 candidate genes within the cohorts for AS and HT. KEGG and GO enrichment analyses indicate that these genes are significantly involved in antigen processing and presentation, along with various immune-inflammatory pathways. Two pivotal genes, PTPRC and TYROBP, were identified using five algorithms from the cytoHubba plugin. Validation through external datasets confirmed their substantial diagnostic value for AS and HT. Moreover, the results of Gene Set Enrichment Analysis (GSEA) indicated that these core genes are significantly enriched in various receptor interactions and signaling pathways. Immune infiltration analysis revealed a strong association of lymphocytes and macrophages with the pathogenesis of AS and HT. Single-cell analysis demonstrated predominant expression of the core genes in macrophages, monocytes, T cells and Common Myeloid Progenitor (CMP). This study proposes that an aberrant immune response might represent a shared pathogenic mechanism in AS and HT. The genes PTPRC and TYROBP are identified as critical potential biomarkers and therapeutic targets for these comorbid conditions. Furthermore, the core genes and their interactions with immune cells could serve as promising targets for future diagnostic and therapeutic strategies.
Similar content being viewed by others
Introduction
Atherosclerosis (AS) is a chronic inflammatory disease marked by endothelial cell damage and cholesterol accumulation, which initiates an immune-inflammatory response, resulting in vessel wall thickening and plaque formation1. This disease process is a primary contributor to cardiovascular diseases worldwide, substantially altering vascular structure and function, and is strongly linked with critical complications such as myocardial infarction and stroke2,3. Driven by shifts in global lifestyles and the rise in aging populations, the incidence of AS continues to grow each year. The research delineated in the Global Burden of Disease Study highlights a significant rise in the incidence of cardiovascular diseases over a span from 1990 to 2019, where the number of cases escalated from 271 million to an alarming 523 million. Additionally, deaths attributed to cardiovascular conditions showed a consistent upward trajectory, climbing from 12.1 million to 18.6 million4,5. On a different note, Hashimoto’s Thyroiditis (HT), a prevalent autoimmune disorder of the thyroid, is marked by persistent thyroid gland inflammation and the generation of autoantibodies that frequently result in hypothyroidism. The disease typically presents with symptoms of hypothyroidism and thyroid enlargement, and in severe cases, it may precipitate a temporary hyperthyroid phase6. The pathogenesis of HT is multifaceted, involving genetic, environmental, and immunological factors7,8. Furthermore, HT often manifests alongside other autoimmune disorders, including rheumatoid arthritis and systemic lupus erythematosus, indicating a more extensive pattern of immune system malfunction9. Patients with HT exhibit an elevated cardiovascular (CV) risk. Numerous studies have demonstrated that hypothyroidism heightens the risk of cardiovascular diseases and AS, exhibiting strong independent correlations with aortic AS and myocardial infarction10,11. Moreover, a meta-analysis by Ochs et al. revealed that the risk of coronary heart disease (CHD) in individuals with subclinical hypothyroidism increases by approximately 20%. These findings highlight the tight link between thyroid dysfunction and AS. The thyroid gland plays an essential role in regulating metabolism and cardiovascular function. Its dysfunction can directly impact vascular health and exacerbate the progression of AS via effects on lipid metabolism, endothelial function, and inflammatory responses10,11. Therefore, delineating the interrelationship between HT and AS is essential for the effective prevention and management of cardiovascular diseases.
Although the precise mechanisms linking AS and HT remain elusive, both conditions underscore the critical role of inflammation and immune system dysregulation. AS typically begins with the subendothelial accumulation of low-density lipoprotein (LDL), provoking a localized inflammatory response12. This inflammation is intensified as macrophages ingest LDL and transform into foam cells, leading to endothelial damage and hardening of the vascular wall13. Conversely, the pathogenesis of HT involves intricate interactions among various immune cells and inflammatory mediators within the thyroid gland. Notably, there is a marked increase in T lymphocytes, B lymphocytes, and their subsets, which exacerbate the condition by secreting a range of cytokines (such as IL-1, IL-6, TNF-α) and chemokines (such as CXCL10, CCL2). These immune mediators not only sustain the chronic inflammatory state in the thyroid but also induce structural and functional impairments6,14. Furthermore, both diseases share a heightened immune-inflammatory response, exemplified by elevated levels of biomarkers like C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor (TNFα), indicating active inflammation and reflecting disease severity and progression15,16,17,18. This shared characteristic of immune-inflammatory response enhances our understanding of the interaction mechanisms between diseases and supports the development of new therapeutic approaches, thereby potentially improving treatment efficacy. Therefore, comprehensive research into these common pathological features is vital for devising broad-spectrum therapeutic strategies.
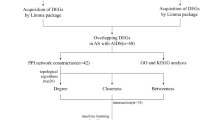
Despite numerous studies establishing a correlation between AS and HT, a clear consensus on their common etiology and pathogenesis remains elusive. Consequently, this study aims to enhance targeted clinical interventions by thoroughly analyzing the shared pathogenic mechanisms of these diseases. Leveraging gene expression profiles from public databases, we conducted DEG analysis and WGCNA to identify key genes implicated in both conditions. Additionally, through functional enrichment analysis, we explored relevant biological pathways. Utilizing five algorithms from the Cytohubba plugin, this study also delineated the core genes of these diseases and examined their associations with immune cell infiltration in AS and HT. Employing single-cell technology, we conducted a deeper analysis of these core gene expressions within diverse immune cells from patients with AS. The methodology and principal findings of this research are depicted in Fig. 1. Through this comprehensive series of analyses, we aspire to deepen our understanding of the comorbidity mechanisms between AS and HT and to identify potential therapeutic targets that could enhance patient outcomes.
Materials and methods
Data source
We sourced transcriptome datasets (GSE100927, GSE28829, GSE138198, and GSE29315) and a single-cell dataset (GSE155512) from the GEO database. Regarding AS, the dataset GSE100927 (platform: GPL17077) comprised 69 atherosclerotic and 35 healthy arterial samples. GSE28829 (platform: GPL570) included 16 late-stage and 13 early-stage atherosclerotic plaque samples. Additionally, GSE155512 (platform: GPL24676) encompassed 3 atherosclerotic samples. For HT, dataset GSE138198 (platform: GPL6244) contained 13 HT and 3 normal thyroid samples, while GSE29315 (platform: GPL8300) included 6 HT and 8 thyroid hyperplasia samples.
Differential gene expression screening
We performed gene expression analysis on datasets GSE28829 and GSE138198 for AS and HT, respectively. DEGs were identified using the Limma package in R (Version 4.4.0, released on June 10, 2024), adhering to criteria of Log2|fold change (FC)|> 1 and adjusted p value < 0.05. We generated volcano plots and heatmaps for the top 20 ranked DEGs using the ‘ggplot’ package. The ‘VennDiagram’ package was then employed to identify common DEGs between AS and HT.
Construction and module analysis of WGCNA
A methodology known as WGCNA enhances the investigation of biologically meaningful co-expressed gene modules and probes the connections between gene networks and diseases. In our research, we utilized the ‘WGCNA’ package in R to develop a gene co-expression network, targeting the exploration of associations between genes and phenotypes19. Initially, we selected the upper quartile of genes displaying the greatest median absolute deviation (MAD). Subsequently, we computed the Pearson correlation matrix for all gene pairings and crafted a weighted adjacency matrix using average linkage along with weighted correlation coefficients. The adjacency matrix was established by applying a ‘soft’ thresholding power (b), which was then converted into a topological overlap matrix (TOM). For clustering genes with analogous expression patterns, we implemented average linkage hierarchical clustering based on TOM-derived dissimilarity, setting a threshold for the minimum module size at 60. Finally, we examined the similarity among genes within these modules, defined a threshold for cutting the module dendrogram, and amalgamated several modules. The WGCNA analysis enabled us to pinpoint significant modules related to AS and HT, and to create visual representations of characteristic gene networks.
GO and KEGG enrichment analysis
GO and KEGG analysis facilitate systematic annotation and enrichment of gene functions and biological metabolic pathways, thereby enriching our understanding of the functional aspects contained within biological data20,21,22,23. We performed these analyses using the ‘clusterProfiler’ package in R, identifying significant pathways at a threshold of P < 0.05. The results were visualized using the ‘ggplot2’ package.
PPI network construction and cluster analysis
We employed the STRING database (http://string-db.org, released on June 12, 2024) to extract gene interactions. The resulting protein–protein interaction (PPI) network was visualized utilizing Cytoscape (version 3.10.1, released on June 12, 2024), with an interaction score threshold exceeding 0.4. Further, we performed cluster analysis through the MCODE algorithm integrated within the Cytoscape plugin24. The defined parameters for this analysis were a degree cutoff of 2, a node score cutoff of 0.2, a K-core of 2, and a maximum depth of 100.
Selection and validation of core genes
We utilized five algorithms from the cytoHubba plugin—MCC, MNC, Degree, EPC, and Bottleneck—to identify the top 10 genes ranked by each method. Subsequently, we employed the Jvenn online tool (https://jvenn.toulouse.inrae.fr/app/example.html, released on June 12, 2024)25 to intersect the genes identified by these algorithms, identifying two shared core genes. For validation, datasets GSE100927 and GSE29315 were used for AS and HT, respectively, with the expression of core genes confirmed using the ‘ggpubr’ R package. Additionally, we conducted Receiver Operating Characteristic (ROC) curve analysis using the ‘pROC’ R package, utilizing the Area Under the Curve (AUC) as a measure of reliability.
Gene set enrichment analysis
Upon pinpointing the central genes, GSEA was utilized for AS and HT employing the ‘clusterProfiler’ package. Patients diagnosed with AS or HT were categorized into groups with high and low gene expression, determined by the median expression levels of the central genes. GSEA was then applied to compute enrichment scores for gene sets, which illuminated differing functional phenotypes. Additionally, GSEA facilitated the comparison of biological pathways between the two expression groups, referencing the c5.go.bp.v7.5.1.entrez.gmt gene set. Gene sets achieving a p value < 0.05, a normalized enrichment score (NES) > 1, and a false positive rate (FDR) q-value < 0.05 were deemed significantly enriched. Enrichment plots prominently displayed the top five activating and inhibiting pathways for each essential gene in both conditions.
Immune infiltration analysis
Immune cell infiltration was assessed using the CIBERSORT algorithm to investigate the associations between different immune cell populations and disease conditions. This algorithm deciphers the composition of immune cells from gene expression data. Using the CIBERSORT R package26 and the LM22 gene signature from the CIBERSORT website, we quantified 22 types of immune cells. Pearson correlation analysis was then used to elucidate the relationships between various immune cell phenotypes and critical genes, which were visually represented in lollipop plots.
Single-cell sequencing analysis
Due to the absence of suitable single-cell RNA sequencing (scRNA-seq) datasets for HT, we downloaded only the AS scRNA-seq dataset GSE155512 from the GEO database. We conducted downstream analyses using the Seurat R package (version 4.4.0, released on June 16, 2024)27. Initially, we created a Seurat object from the read single-cell expression data and conducted quality control, excluding cells with fewer than 50 expressed genes and those with a mitochondrial gene expression ratio exceeding 5%. The data underwent normalization via the LogNormalize technique, followed by the identification of 1500 highly variable genes through the ‘FindVariableFeatures’ function. Principal Component Analysis (PCA) was then executed, along with cluster analysis using Seurat’s ‘FindClusters’ function. Additionally, t-distributed stochastic neighbor embedding (t-SNE) was utilized for nonlinear dimensionality reduction, facilitating the visualization of the data in t-SNE plots.
Results
Identification of differentially expressed genes
In the AS dataset GSE28829, we identified 308 DEGs, of which 257 were upregulated and 51 were downregulated. Similarly, in the HT dataset GSE138198, 1773 DEGs were identified, with 899 upregulated and 874 downregulated. The expression patterns of DEGs in both conditions are depicted using volcano plots (Fig. 2A,B). The top 20 DEGs for AS and HT are represented in heatmaps (Fig. 2C,D). Notably, there is a shared differential expression of 75 genes between AS and HT (Fig. 3A,B).
WGCNA analysis of AS and HT
We performed WGCNA on the AS dataset GSE28829 and the HT dataset GSE138198 to identify highly associated modules. No significant outliers were found in either dataset. For GSE28829, a “soft” threshold of β = 12 was established based on scale independence and mean connectivity (Supplementary material 1), and 10 modules were detected. Clinical correlation analysis indicated that the “MEturquoise” and “MEred” modules exhibited the strongest positive and negative correlations with AS, respectively (MEturquoise: r = 0.82, p = 4e−08; MEred: r = − 0.74, p = 5e−06) (Fig. 4A,C). Similarly, for GSE138198, a “soft” threshold of β = 10 was selected, identifying 10 modules. The “MEblack” and “MEcyan” modules showed the highest positive and negative correlations with HT, respectively (MEblack: r = 0.77, p = 4e−04; MEcyan: r = − 0.91, p = 1e−06) (Fig. 4B,D). Subsequently, these pivotal modules were targeted for further analysis. Intersection analysis of the genes from these key modules identified 45 potential driver genes common to both AS and HT (Fig. 5D).
Enrichment analysis of genes jointly driving AS and HT
We identified 75 common DEGs between AS and HT and discovered 45 overlapping genes within key modules. To ensure comprehensive coverage of potential key genes, we merged the DEGs with genes from these modules. After eliminating duplicates, 119 candidate genes were identified, which are hypothesized to jointly contribute to the pathogenesis of both diseases (Supplementary material 2). Subsequent GO and KEGG enrichment analyses were conducted on these genes. The GO analysis indicated that biological process (BP) genes are predominantly involved in antigen processing and presentation, crucial for T-cell activation and immune response regulation, through the presentation of exogenous and endogenous peptide antigens via MHC class I and II molecules. Cellular component (CC) genes were mainly enriched in locations such as the external side of the plasma membrane, secretory granule membrane, endocytic vesicle membrane, and MHC protein complex. Molecular function (MF) genes showed enrichment in activities like MHC protein complex binding, immunoglobulin binding, and MHC class II protein complex binding, which are integral to immunoglobulin receptor activity (Fig. 5A,B). The KEGG analysis revealed significant enrichment in pathways associated with Staphylococcus aureus infection, phagosome, tuberculosis, systemic lupus erythematosus, and alcoholic liver disease (Fig. 5C).
Selection and verification of core genes
We inputted 119 candidate genes into the STRING online database and subsequently constructed their PPI network using Cytoscape software, which resulted in 78 nodes and 472 links after isolating genes (Fig. 6A). Using the MCODE plugin, we identified a cluster consisting of 19 nodes and 141 edges, scoring 15.667 (Fig. 6B). We employed five different algorithms to calculate gene scores and identified the top 10 core genes (Fig. 6C). From these analyses, two core genes, PTPRC and TYROBP, emerged (Supplementary material 3). We subsequently validated their expression levels across four datasets, noting that their expression was elevated in AS and HT compared to controls (Figs. 7A–D and 8A–D). Additionally, the diagnostic efficacy of these genes was evaluated across four distinct datasets, with AUC values exceeding 0.9, confirming their high diagnostic potential for AS and HT (Figs. 7E–H and 8E–H).
Enrichment analysis of merged genes. (A,B) Circle plot and bubble plot of GO enrichment analysis includes biological process, cellular component and molecular function. (C) Bubble plot of KEGG enrichment analysis. (D) Venn diagram of core genes. GO, Gene Ontology; KEGG, Kyoto Encyclopedia of Genes and Genomes.
Validation of the expression level and diagnostic efficacy of PTPRC gene. The violin plots of PTPRC gene in GSE28829 (A), GSE100927 (B), GSE138198 (C) and GSE29315 (D). The ROC curves of PTPRC gene in GSE28829 (E), GSE100927 (F), GSE138198 (G) and GSE29315 (H). *p < 0.05; **p < 0.01;***p < 0.001; ****p < 0.0001.
Validation of the expression level and diagnostic efficacy of TYROBP gene. The violin plots of TYROBP gene in GSE28829 (A), GSE100927 (B), GSE138198 (C) and GSE29315 (D). The ROC curves of TYROBP gene in GSE28829 (E), GSE100927 (F), GSE138198 (G) and GSE29315 (H). *p < 0.05; **p < 0.01;***p < 0.001; ****p < 0.0001.
GSEA analysis of core genes
GSEA was performed on two core genes within the AS and HT datasets (Figs. 9, 10). The analysis, conducted using the “GSEA” software package, highlighted the top five upregulated and downregulated pathways. In both disease cohorts, these core genes were implicated in cytokine-cytokine receptor interactions and pathways related to systemic lupus erythematosus. Furthermore, all genes showed enrichment in a variety of immune and inflammatory pathways, including the chemokine signaling pathway, toll-like receptor signaling pathway, T cell receptor signaling pathway, and the complement and coagulation cascades.
Immune cell infiltration and its association with core genes
To elucidate the immune landscape and investigate potential immune mechanisms, we analyzed the distribution of 22 immune cell types in the GSE100927 and GSE138198 datasets using the CIBERSORT algorithm, presenting the results in bar graphs (Figs. 11A and 12A). In the AS cohort, increased counts of memory B cells, regulatory T cells, follicular helper T cells, gamma delta T cells, M0 macrophages, and activated mast cells were observed. Conversely, levels of naive B cells, plasma cells, naive CD4 + T cells, activated CD4 + memory T cells, resting NK cells, monocytes, activated dendritic cells, M1 macrophages, M2 macrophages, and resting mast cells were reduced. In HT, there was an elevation in memory B cells and M1 macrophages, while activated NK cells, monocytes, M0 macrophages, resting mast cells, and neutrophils showed lower levels (Figs. 11B and 12B). In both conditions, memory B cells consistently exhibited elevated levels, while monocytes and resting mast cells showed decreased counts. Additionally, a correlation analysis between core genes and immune cells was conducted (Figs. 11C,D and 12C,D). Spearman correlation tests revealed significant associations between hub genes and macrophages, T cells, and monocytes.
Immune infiltration analysis of AS. (A) Histogram of proportion of immune cells. (B) Comparison of immune cell proportion between AS and controls (Willcoxon’s test). (C) Correlation between PTPRC and immune cells content in AS. (D) Correlation between TYROBP and immune cells content in AS. *p < 0.05; **p < 0.01;***p < 0.001.
Immune infiltration analysis of HT. (A) Histogram of proportion of immune cells. (B) Comparison of immune cell proportion between HT and controls (Willcoxon’s test). (C) Correlation between TYROBP and immune cells content in HT. (D) Correlation between TYROBP and immune cells content in HT. *p < 0.05; **p < 0.01;***p < 0.001.
Expression of core genes in single cells
We acquired single-cell data from GSE155512 and performed single-cell analysis using the Seurat software package, with cell clustering executed via the t-SNE algorithm. Following data quality control, low-quality cells were excluded (Fig. 13A). Cells from three samples were organized into seven subgroups, including chondrocytes, macrophages, endothelial cells, T cells, monocytes, CMP and smooth muscle cells (Fig. 13B). The analysis revealed that PTPRC and TYROBP were predominantly expressed in macrophages, monocytes, T cells and CMP (Fig. 13C).
Discussion
Research indicates that both AS and HT are associated with immune system involvement and inflammatory responses28,29. The development of AS initiates with damage to vascular endothelial cells, which in turn activates the immune system. This activation prominently features inflammatory cells including monocytes, macrophages, and T-cells. These cells migrate to the subendothelial regions of blood vessels, establishing the primary sites for atherosclerotic plaque formation. Notably, macrophages undergo transformation into foam cells through the absorption of oxidized low-density lipoprotein (oxLDL) and the activation of receptors including LOX-1 and CD36, thereby becoming essential components of atherosclerotic plaques. Furthermore, macrophages contribute to the release of inflammatory factors such as IL-1β and TNF-α via the NF-κB pathway, thereby exacerbating the inflammatory response and accelerating the progression of AS12,13. Concurrently, T-cells recognize vascular-specific antigens, such as oxidized low-density lipoprotein, and provoke the release of pro-inflammatory cytokines, including IFN-γ, TNF-α, IL-1, and IL-6. This activity intensifies the inflammatory response within plaque regions and promotes the recruitment and activation of additional immune cells30,31. Specifically, Th1 cells enhance macrophage uptake and activation of s through their production of IFN-γ. Regulatory T-cells (Tregs), although playing a limited role in controlling these inflammatory responses, contribute to the persistence and exacerbation of the inflammatory milieu. The behavior of these immune cells not only influences the level of inflammation but also potentially affects the stability of the plaques, thereby increasing the risk of rupture—a major risk factor for acute cardiovascular events such as myocardial infarction and stroke32,33,34. In the pathogenesis of HT, specific autoantibodies, including anti-thyroid peroxidase (TPO) and anti-thyroglobulin (Tg) antibodies, play a pivotal role. These antibodies attach to particular target molecules on thyroid cell surfaces, thereby stimulating the immune response. This activation leads to an accumulation of inflammatory cells such as macrophages and T-cells within the thyroid tissue, accompanied by the release of cytokines and chemokines, including IL-1, IL-6, TNF-α and IFN-γ. These mediators not only intensify the inflammatory response and facilitate further migration and activation of immune cells but also directly impair thyroid cell functionality, disrupting their ability to synthesize hormones35,36. Moreover, the persistent inflammatory response induces oxidative stress and activates chronic tissue repair mechanisms within the thyroid, which may exacerbate thyroid structure damage. Over time, this chronic damage can result in thyroid tissue fibrosis, a direct outcome of prolonged inflammation37,38,39. In conclusion, macrophages and T-cells play a fundamental role in the pathogenesis of AS and HT, driving disease progression through their involvement in inflammatory processes and immune regulation. Future research is directed towards elucidating the mechanisms of action of these cells, with the aim of developing targeted therapies such as modulating specific receptor activities or enhancing regulatory T-cell functions. These advancements aim to effectively control inflammatory responses, improve treatment outcomes, and pioneer new strategies for disease management. Such progress not only has the potential to enhance patient quality of life but also offers significant theoretical and practical insights for the clinical treatment of cardiovascular and autoimmune diseases.
The precise mechanisms underlying AS and HT remain elusive, which has prompted this study to undertake a comprehensive bioinformatics analysis aimed at elucidating the shared mechanisms, pathways, and immune infiltration characteristics of AS and HT. Our analysis identified two pivotal genes, PTPRC and TYROBP. Results of the GSEA demonstrate a significant association between the elevated expression of specific genes and enhanced interactions with numerous receptors, alongside involvement in various receptor signaling pathways. Further examination of immune infiltration has uncovered a notable correlation between the expression of these genes and the prevalence of macrophages and lymphocytes in the development of AS and HT. Single-cell analysis showed that PTPRC and TYROBP are predominantly expressed in macrophages, monocytes, T cells, and common CMP. Moreover, immune profiles from patients with AS and HT demonstrated increased levels of memory B cells in affected individuals. Consequently, we propose that there may be shared pathogenic processes between AS and HT, possibly linked to memory B cells.
The involvement of B cells in the progression of AS is complex and presents conflicting evidence. Studies have demonstrated that various B cell subtypes exert both promotive and inhibitory effects on atherogenesis. B cells can recognize oxidized low-density lipoprotein (ox-LDL) and generate specific antibodies, leading to the formation of immune complexes. These aggregates build up within the vascular endothelium, possibly triggering inflammatory responses that facilitate the formation and growth of atherosclerotic plaques. Moreover, B cells might secrete pro-inflammatory cytokines, including IL-6 and TNF-α, further exacerbating local inflammation and vascular damage29,40. Ox-LDL not only triggers inflammation and oxidative stress in endothelial cells but also facilitates the recruitment and activation of leukocytes by modulating immune cell activity, such as that of macrophages, thereby exacerbating vascular inflammation and dysfunction. These processes underscore the critical role of B cells in AS and highlight their potential as therapeutic targets12,31,41. Conversely, regulatory B cells (Bregs), particularly those producing interleukin-10 (IL-10), known as B10 cells, exert substantial anti-inflammatory and immunomodulatory effects in the disease. By secreting IL-10, these B cells help mitigate inflammatory responses, thus safeguarding the vascular wall against further damage. Research indicates that B10 cells’ development and function necessitate a diverse range of antigen receptors and Toll-like receptor (TLR) signaling. These cells are crucial in modulating autoimmunity and inflammation, particularly within the spleens of adult mice, where B10 cells proliferate significantly and are more prevalent in aged mice and those susceptible to autoimmune diseases42,43,44. Furthermore, B cells are crucial in the pathogenesis of HT due to their production of specific autoantibodies, such as TPO antibodies and Tg antibodies. These autoantibodies target and bind to molecules on thyroid cells, triggering immune responses that promote inflammation and the gradual deterioration of thyroid tissue8,45,46. Furthermore, studies have shown that B cells significantly influence the pathogenesis of HT by modulating the functions of T cells. During the initial stages of HT, B cells contribute to the regulation of autoimmune responses by secreting immunomodulatory factors, such as IL-10, which significantly impact the behavior of Th1 and Th2 cells and subsequently influence the long-term progression of the disease47. Recent advances indicate that targeted therapeutic approaches that focus on B cell functions—such as the use of combined monoclonal antibodies and chimeric molecules of thyroid protein epitopes—may modulate autoreactive B cells and potentially alleviate or reverse the progression of HT48,49. This strategy, which involves inhibiting the overactivation of B cells, promoting the apoptosis of specific B cells, and regulating cytokines and chemokines, opens new avenues for treating HT and allows for more precise management of autoimmune thyroiditis. Future studies may delve into methods for modulating the activity or specific functions of B cells to develop novel treatments for both AS and HT. Potential approaches could include small molecule inhibitors, monoclonal antibodies, or other biologics that target B cell surface receptors or secreted cytokines50. Additionally, leveraging advanced gene editing technologies, such as CRISPR/Cas9, to precisely regulate specific gene expression in B cells may represent an effective treatment method. The development of these therapeutic strategies necessitates a profound understanding of the role of B cells in these diseases and a comprehensive grasp of the intricate interactions within the immune system.
PTPRC, also known as CD45, is a tyrosine phosphatase receptor ubiquitously present on all nucleated leukocytes, playing an essential role in the activation of T cells and B cells mediated by antigen receptors51,52. PTPRC modulates cell signaling by regulating the activity of Janus kinases (JAK) and Src family kinases (SFKs). It mainly acts by dephosphorylating tyrosine kinases within the JAK family, thereby inhibiting their activity. This function is crucial in both the activation and regulation of immune cells53,54,55. Additionally, PTPRC exhibits various isoforms across different immune cells due to its multiple splicing variants, each significantly influencing cell function and activity. For instance, the CD45RA isoform is primarily expressed in naïve T cells that have not yet been activated by antigens, while the CD45RO isoform is predominantly found in memory T cells. This differential expression of isoforms highlights their distinct roles in cell activation and signal transduction56. In the study of autoimmune diseases, memory T cells expressing CD45RO exhibit heightened reactivity to specific autoantigens. Furthermore, inflammatory states and infections modulate the expression of these PTPRC isoforms. For instance, during sepsis, the expression of CD45RO on lymphocytes may decrease, while the expression of CD45RA can vary depending on the cell type and inflammatory stimuli56,57. PTPRC’s role in the immune system is extensive, encompassing not only adaptive immunity but also a critical function in innate immunity. For example, in mast cells, PTPRC regulates antigen-induced immune responses through Fc receptor-mediated signaling pathways. In dendritic cells, it acts as a key regulator of TLR signaling, which is essential for pathogen recognition and the activation of innate immune responses52,58. The regulatory functions of PTPRC are invaluable in studying AS, notably through its indirect control over the composition and activity of inflammatory cells within plaques. This control is primarily exerted through the anti-inflammatory actions of regulatory T cells and B cells, effectively reducing inflammation and preventing the destabilization of plaques33. Numerous studies have established a close association between increased expression of PTPRC and the onset and progression of AS59,60,61,62. This multifunctional regulatory mechanism highlights the importance of PTPRC as a potential therapeutic target for cardiovascular diseases, offering new avenues for future research aimed at combating AS. Additionally, genetic studies on HT have identified specific variations in the PTPRC gene that increase susceptibility to autoimmune diseases, such as Type 1 diabetes and Graves’ disease. PTPRC may significantly influence aberrant autoimmune responses by regulating lymphocyte signal transduction and activation63,64. This implies a possible role for PTPRC in HT, although further studies are required to substantiate this hypothesis. Dysfunctional PTPRC may lead to the dysregulation of autoimmune responses, resulting in attacks on thyroid tissue, which underscores a potentially critical role in HT65,66. This connection opens new avenues for future research that could clarify the specific pathogenesis of HT and identify potential therapeutic targets. In conclusion, the roles of PTPRC in studies on HT and AS mutually reinforce its broad applications in immune regulation. Therefore, a deeper exploration of the interactions between PTPRC and other immune regulatory molecules could uncover the complex networks involved in pathological states, setting the stage for the development of more comprehensive treatment approaches.
TYROBP (also known as DAP12) is a transmembrane adaptor protein extensively expressed in human immune cells, including natural killer (NK) cells, macrophages, and specific T cell subsets67,68. This protein features an Immunoreceptor Tyrosine-based Activation Motif (ITAM) essential for signaling processes. Upon ligand binding to immune cell surface receptors, TYROBP’s ITAM domain is phosphorylated, initiating the activation of key signaling molecules such as the tyrosine kinases Syk and ZAP70. This activation triggers a cascade of intracellular signaling events, including cell activation, proliferation, cytokine release, and cytotoxic functions69,70. The phosphorylated ITAM can also recruit and activate additional crucial signaling molecules, such as phosphoinositide 3-kinase (PI3K), small GTPase RAS, and phospholipase C gamma (PLCγ), facilitating various biological responses like transcription, cell proliferation, and cytokine release71,72. Studies have demonstrated that TYROBP plays a pivotal role in the progression of AS through its signaling pathways. In macrophages, TYROBP directly affects lipid uptake and processing. The phosphorylation of TYROBP’s ITAM domain, mediated by Src family kinases, occurs upon receptor activation when macrophages engage low-density lipoprotein (LDL) via receptors such as CD36 and SR-A73,74. This phosphorylated ITAM then serves as a signaling hub, further recruiting and activating Syk. Syk’s activation initiates signaling cascades involving pathways such as PI3K and PLCγ. PI3K activation leads to the production of PIP3, which in turn activates the Akt signaling pathway, impacting cell survival and proliferation. Simultaneously, PLCγ activation results in the generation of diacylglycerol (DAG) and inositol trisphosphate (IP3), which regulate intracellular calcium signaling and protein kinase C activation75,76. This cascade of activated signaling pathways results in macrophages engulfing and accumulating oxidized LDL, thereby transforming into foam cells. This transformation increases intracellular oxidative stress and inflammatory responses, exacerbating AS77,78. Furthermore, TYROBP is crucial in autoimmune diseases like HT, influencing immune responses involving macrophages and NK cells. NK cells, which are capable of producing cytokines such as IL-10, regulate immune balance and play various roles in the initiation, progression, and alleviation of autoimmune and autoinflammatory diseases79,80. Studies indicate that in the pathogenesis of HT, the influx of macrophages and dendritic cells is directly triggered by inflammatory events. These cells impact thyroid cell growth and function through pathways mediated by interleukins such as IL-1 and IL-6. This process facilitates lymphocyte recognition of self-antigens, leading to considerable generation of autoreactive CD4 + T cells, CD8 + cytotoxic T cells, and immunoglobulin G (IgG) autoantibodies. Additionally, research suggests that the interplay between macrophages, dendritic cells, and T cells amplifies the inflammatory response, culminating in the production of diverse inflammatory cytokines that are vital for the progression of HT65,81. Genetic research also reveals that genetic variations associated with TYROBP may increase susceptibility to autoimmune diseases. Specific genetic markers identified in genome-wide association studies (GWAS) related to autoimmunity may enhance disease risk by influencing molecules in immune regulation pathways, such as TYROBP. These genetic variations significantly affect immune cell functions, particularly those of T cells and regulatory T cells, thereby playing a pivotal role in the development of autoimmune diseases. These findings offer new targets for the treatment of autoimmune diseases and enhance our understanding of their pathogenic mechanisms82. Therefore, based on prior research, TYROBP is likely to serve as a biomarker for patients with AS and HT.
This study boasts several significant strengths. We implemented a comprehensive and intricate bioinformatics analysis approach to investigate the interactions between AS and HT. By examining the shared molecular mechanisms and pathways of AS and HT, we pinpointed crucial genes and immune infiltration characteristics. These were corroborated through external datasets, thereby enhancing the predictive accuracy. Our findings potentially illuminate the shared mechanisms underpinning AS and HT. Nevertheless, it is important to acknowledge the limitations of this study. Firstly, the data were sourced from the GEO database, which could have inconsistencies in collection and processing methods, potentially affecting the accuracy and reliability of our analyses. Variations in processing methods and technical platforms across laboratories could introduce biases. Additionally, our analysis primarily focused on gene expression changes without directly measuring protein expression and activity. Considering that gene expression levels do not always correlate with protein functions, our findings necessitate further validation at the protein level. Consequently, future research should prioritize multidimensional data integration, enhance quality control, expand sample sizes, and experimentally validate the functions of identified genes and proteins. Such approaches will foster a more comprehensive understanding of the pathogenic mechanisms of AS and HT and identify more precise clinical treatment targets.
Conclusion
In this research, we pinpointed two key genes, PTPRC and TYROBP, crucial for AS and HT, and elucidated shared regulatory pathways and common immune characteristics. This led to the development of an effective diagnostic model. Further analysis using CIBERSORT revealed a significant correlation between the expression of these core genes and immune cell infiltration. Additionally, single-cell sequencing analysis demonstrated that these genes are primarily expressed in macrophages, monocytes, T cells, and CMPs. Our findings enhance the understanding of the molecular mechanisms underlying both diseases by highlighting key genes and immune regulatory pathways. These achievements not only deepen our knowledge of the pathologies of AS and HT but also set the stage for further clinical research and therapeutic development.
Data availability
The datasets GSE100927, GSE28829, GSE155512, GSE138198, and GSE29315 for this study can be found in the https://www.ncbi.nlm.nih.gov/geo/. The data supporting the findings of this study are available from the corresponding author upon a reasonable request.
Abbreviations
- AS:
-
Atherosclerosis
- HT:
-
Hashimoto’s thyroiditis
- GO:
-
Gene ontology
- KEGG:
-
Kyoto Encyclopedia of Genes and Genomes
- GEO:
-
Gene Expression Omnibus
- PPI:
-
Protein–protein interaction
- DEGs:
-
Differentially expressed genes
- WGCNA:
-
weighted gene coexpression network
- GSEA:
-
Gene Set Enrichment Analysis
- scRNA-seq:
-
single-cell RNA sequencing
- NES:
-
normalized enrichment score
- FDR:
-
false positive rate
- TOM:
-
topological overlap matrix
- MAD:
-
median absolute deviation
- ROC:
-
Receiver Operating Characteristic
- AUC:
-
Area Under the Curve
- t-SNE:
-
t-distributed stochastic neighbor embedding
References
Wolf, D. & Ley, K. Immunity and inflammation in atherosclerosis. Circ. Res. 124(2), 315–327 (2019).
Kruk, M. E. et al. Mortality due to low-quality health systems in the universal health coverage era: A systematic analysis of amenable deaths in 137 countries. Lancet 392(10160), 2203–2212 (2018).
Herrington, W., Lacey, B., Sherliker, P., Armitage, J. & Lewington, S. Epidemiology of atherosclerosis and the potential to reduce the global burden of atherothrombotic disease. Circ. Res. 118(4), 535–546 (2016).
Song, P. et al. Global and regional prevalence, burden, and risk factors for carotid atherosclerosis: A systematic review, meta-analysis, and modelling study. Lancet Glob. Health 8(5), e721–e729 (2020).
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 76(25), 2982–3021 (2020).
Antonelli, A., Ferrari, S. M., Corrado, A., Di Domenicantonio, A. & Fallahi, P. Autoimmune thyroid disorders. Autoimmun. Rev. 14(2), 174–180 (2015).
Ralli, M. et al. Hashimoto’s thyroiditis: An update on pathogenic mechanisms, diagnostic protocols, therapeutic strategies, and potential malignant transformation. Autoimmun. Rev. 19(10), 102649 (2020).
Weetman, A. P. An update on the pathogenesis of Hashimoto’s thyroiditis. J. Endocrinol. Investig. 44(5), 883–890 (2021).
Ferrari, S. M. et al. The association of other autoimmune diseases in patients with Graves’ disease (with or without ophthalmopathy): Review of the literature and report of a large series. Autoimmun. Rev. 18(3), 287–292 (2019).
Hak, A. E. et al. Subclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: The Rotterdam study. Ann. Intern. Med. 132(4), 270–278 (2000).
Imaizumi, M. et al. Risk for ischemic heart disease and all-cause mortality in subclinical hypothyroidism. J. Clin. Endocrinol. Metab. 89(7), 3365–3370 (2004).
Jiang, H. et al. Mechanisms of oxidized LDL-mediated endothelial dysfunction and its consequences for the development of atherosclerosis. Front. Cardiovasc. Med. 9, 925923 (2022).
Blagov, A. V. et al. The role of macrophages in the pathogenesis of atherosclerosis. Cells 12(4), 522 (2023).
Zhang, Q. Y. et al. Lymphocyte infiltration and thyrocyte destruction are driven by stromal and immune cell components in Hashimoto’s thyroiditis. Nat. Commun. 13(1), 775 (2022).
Paffen, E. & DeMaat, M. P. C-reactive protein in atherosclerosis: A causal factor?. Cardiovasc. Res. 71(1), 30–39 (2006).
Attiq, A., Afzal, S., Ahmad, W. & Kandeel, M. Hegemony of inflammation in atherosclerosis and coronary artery disease. Eur. J. Pharmacol. 966, 176338 (2024).
Erge, E. et al. A novel inflammatory marker for the diagnosis of Hashimoto’s thyroiditis: Platelet-count-to-lymphocyte-count ratio. Diseases 11(1), 15 (2023).
Lazúrová, I., Jochmanová, I., Benhatchi, K. & Sotak, S. Autoimmune thyroid disease and rheumatoid arthritis: Relationship and the role of genetics. Immunol. Res. 60(2–3), 193–200 (2014).
Langfelder, P. & Horvath, S. WGCNA: An R package for weighted correlation network analysis. BMC Bioinform. 9, 559 (2008).
Gene Ontology Consortium. The gene ontology resource: 20 years and still GOing strong. Nucleic Acids Res. 47(D1), D330–D338 (2019).
Ogata, H. et al. KEGG: Kyoto Encyclopedia of Genes and Genomes. Nucleic Acids Res. 27(1), 29–34 (1999).
Kanehisa, M. Toward understanding the origin and evolution of cellular organisms. Protein Sci. 28(11), 1947–1951 (2019).
Kanehisa, M., Furumichi, M., Sato, Y., Kawashima, M. & Ishiguro-Watanabe, M. KEGG for taxonomy-based analysis of pathways and genomes. Nucleic Acids Res. 51(D1), D587–D592 (2023).
Shannon, P. et al. Cytoscape: A software environment for integrated models of biomolecular interaction networks. Genome Res. 13(11), 2498–2504 (2003).
Bardou, P., Mariette, J., Escudié, F., Djemiel, C. & Klopp, C. jvenn: An interactive Venn diagram viewer. BMC Bioinform. 15(1), 293 (2014).
Bindea, G. et al. Spatiotemporal dynamics of intratumoral immune cells reveal the immune landscape in human cancer. Immunity 39(4), 782–795 (2013).
Stuart, T. et al. Comprehensive integration of single-cell data. Cell 177(7), 1888-1902.e1821 (2019).
Hinkley, H., Counts, D. A., VonCanon, E. & Lacy, M. T cells in atherosclerosis: Key players in the pathogenesis of vascular disease. Cells 12(17), 2152 (2023).
Popa-Fotea, N. M., Ferdoschi, C. E. & Micheu, M. M. Molecular and cellular mechanisms of inflammation in atherosclerosis. Front. Cardiovasc. Med. 10, 1200341 (2023).
Elyasi, A. et al. The role of interferon-γ in cardiovascular disease: An update. Inflamm. Res. 69(10), 975–988 (2020).
Wu, M. Y., Li, C. J., Hou, M. F. & Chu, P. Y. New insights into the role of inflammation in the pathogenesis of atherosclerosis. Int. J. Mol. Sci. 18(10), 2034 (2017).
Chen, J. et al. The emerging role of Th1 cells in atherosclerosis and its implications for therapy. Front. Immunol. 13, 1079668 (2022).
Spitz, C. et al. Regulatory T cells in atherosclerosis: Critical immune regulatory function and therapeutic potential. Cell. Mol. Life Sci. 73(5), 901–922 (2016).
Kuan, R., Agrawal, D. K. & Thankam, F. G. Treg cells in atherosclerosis. Mol. Biol. Rep. 48(5), 4897–4910 (2021).
Fröhlich, E. & Wahl, R. Thyroid autoimmunity: Role of anti-thyroid antibodies in thyroid and extra-thyroidal diseases. Front. Immunol. 8, 521 (2017).
Dersch, R. et al. Anti-thyroid peroxidase and anti-thyroglobulin autoantibodies in the cerebrospinal fluid of patients with unipolar depression. J. Clin. Med. 9(8), 2391 (2020).
da Silva, G. B., Yamauchi, M. A. & Bagatini, M. D. Oxidative stress in Hashimoto’s thyroiditis: Possible adjuvant therapies to attenuate deleterious effects. Mol. Cell Biochem. 478(4), 949–966 (2023).
Kochman, J., Jakubczyk, K., Bargiel, P. & Janda-Milczarek, K. The influence of oxidative stress on thyroid diseases. Antioxidants (Basel) 10(9), 1442 (2021).
Batóg, G. et al. The interplay of oxidative stress and immune dysfunction in Hashimoto’s thyroiditis and polycystic ovary syndrome: A comprehensive review. Front. Immunol. 14, 1211231 (2023).
Malekmohammad, K., Bezsonov, E. E. & Rafieian-Kopaei, M. Role of lipid accumulation and inflammation in atherosclerosis: Focus on molecular and cellular mechanisms. Front. Cardiovasc. Med. 8, 707529 (2021).
Meng, Q., Liu, H., Liu, J., Pang, Y. & Liu, Q. Advances in immunotherapy modalities for atherosclerosis. Front. Pharmacol. 13, 1079185 (2022).
Tsiantoulas, D., Diehl, C. J., Witztum, J. L. & Binder, C. J. B cells and humoral immunity in atherosclerosis. Circ. Res. 114(11), 1743–1756 (2014).
Cerqueira, C., Manfroi, B. & Fillatreau, S. IL-10-producing regulatory B cells and plasmocytes: Molecular mechanisms and disease relevance. Semin. Immunol. 44, 101323 (2019).
Yanaba, K., Bouaziz, J. D., Matsushita, T., Tsubata, T. & Tedder, T. F. The development and function of regulatory B cells expressing IL-10 (B10 cells) requires antigen receptor diversity and TLR signals. J. Immunol. 182(12), 7459–7472 (2009).
Subhi, O. et al. Genetic relationship between Hashimoto’s thyroiditis and papillary thyroid carcinoma with coexisting Hashimoto’s thyroiditis. PLoS ONE 15(6), e0234566 (2020).
Li, Q., Yang, W., Li, J. & Shan, Z. Emerging trends and hot spots in autoimmune thyroiditis research from 2000 to 2022: A bibliometric analysis. Front. Immunol. 13, 953465 (2022).
Rydzewska, M., Jaromin, M., Pasierowska, I. E., Stożek, K. & Bossowski, A. Role of the T and B lymphocytes in pathogenesis of autoimmune thyroid diseases. Thyroid Res. 11, 2 (2018).
Ralchev, N. R. et al. Selective silencing of disease-associated B lymphocytes from Hashimoto’s thyroiditis patients by chimeric protein molecules. Int. J. Mol. Sci. 23(23), 15083 (2022).
Tywanek, E., Michalak, A., Świrska, J. & Zwolak, A. Autoimmunity, new potential biomarkers and the thyroid gland-the perspective of Hashimoto’s thyroiditis and its treatment. Int. J. Mol. Sci. 25(9), 4703 (2024).
Guo, M. et al. Mapping the path towards novel treatment strategies: A bibliometric analysis of Hashimoto’s thyroiditis research from 1990 to 2023. Front. Endocrinol. (Lausanne) 14, 1277739 (2023).
Al Barashdi, M. A., Ali, A., McMullin, M. F. & Mills, K. Protein tyrosine phosphatase receptor type C (PTPRC or CD45). J. Clin. Pathol. 74(9), 548–552 (2021).
Rheinländer, A., Schraven, B. & Bommhardt, U. CD45 in human physiology and clinical medicine. Immunol. Lett. 196, 22–32 (2018).
Irie-Sasaki, J. et al. CD45 is a JAK phosphatase and negatively regulates cytokine receptor signalling. Nature 409(6818), 349–354 (2001).
Penninger, J. M., Irie-Sasaki, J., Sasaki, T. & Oliveira-dos-Santos, A. J. CD45: New jobs for an old acquaintance. Nat. Immunol. 2(5), 389–396 (2001).
Yamada, T., Zhu, D., Saxon, A. & Zhang, K. CD45 controls interleukin-4-mediated IgE class switch recombination in human B cells through its function as a Janus kinase phosphatase. J. Biol. Chem. 277(32), 28830–28835 (2002).
Muraro, P. A., Pette, M., Bielekova, B., McFarland, H. F. & Martin, R. Human autoreactive CD4+ T cells from naive CD45RA+ and memory CD45RO+ subsets differ with respect to epitope specificity and functional antigen avidity. J. Immunol. 164(10), 5474–5481 (2000).
Ahmed, M. G. T., Limmer, A. & Hartmann, M. CD45RA and CD45RO are regulated in a cell-type specific manner in inflammation and sepsis. Cells 12(14), 1873 (2023).
Piercy, J., Petrova, S., Tchilian, E. Z. & Beverley, P. C. CD45 negatively regulates tumour necrosis factor and interleukin-6 production in dendritic cells. Immunology 118(2), 250–256 (2006).
Tchilian, E. Z. & Beverley, P. C. Altered CD45 expression and disease. Trends Immunol. 27(3), 146–153 (2006).
Nie, H., Yan, C., Zhou, W. & Li, T. S. Analysis of immune and inflammation characteristics of atherosclerosis from different sample sources. Oxid. Med. Cell. Longev. 2022, 5491038 (2022).
Ma, Y. et al. Identification of common mechanisms and biomarkers for dermatomyositis and atherosclerosis based on bioinformatics analysis. Skin Res. Technol. 30(6), e13808 (2024).
Su, W. et al. Exploring the pathogenesis of psoriasis complicated with atherosclerosis via microarray data analysis. Front. Immunol. 12, 667690 (2021).
Stanford, S. M., Mustelin, T. M. & Bottini, N. Lymphoid tyrosine phosphatase and autoimmunity: Human genetics rediscovers tyrosine phosphatases. Semin. Immunopathol. 32(2), 127–136 (2010).
Xu, Y. & Fisher, G. J. Receptor type protein tyrosine phosphatases (RPTPs): Roles in signal transduction and human disease. J. Cell Commun. Signal 6(3), 125–138 (2012).
Chistiakov, D. A. Immunogenetics of Hashimoto’s thyroiditis. J. Autoimmune Dis. 2(1), 1 (2005).
Zikherman, J. et al. PTPN22 deficiency cooperates with the CD45 E613R allele to break tolerance on a non-autoimmune background. J. Immunol. 182(7), 4093–4106 (2009).
Haure-Mirande, J. V., Audrain, M., Ehrlich, M. E. & Gandy, S. Microglial TYROBP/DAP12 in Alzheimer’s disease: Transduction of physiological and pathological signals across TREM2. Mol. Neurodegener. 17(1), 55 (2022).
Wu, J., Cherwinski, H., Spies, T., Phillips, J. H. & Lanier, L. L. DAP10 and DAP12 form distinct, but functionally cooperative, receptor complexes in natural killer cells. J. Exp. Med. 192(7), 1059–1068 (2000).
Fasbender, F., Claus, M., Wingert, S., Sandusky, M. & Watzl, C. Differential requirements for Src-family kinases in SYK or ZAP70-mediated SLP-76 phosphorylation in lymphocytes. Front. Immunol. 8, 789 (2017).
Ma, J., Jiang, T., Tan, L. & Yu, J. T. TYROBP in Alzheimer’s disease. Mol. Neurobiol. 51(2), 820–826 (2015).
Mócsai, A., Ruland, J. & Tybulewicz, V. L. The SYK tyrosine kinase: A crucial player in diverse biological functions. Nat. Rev. Immunol. 10(6), 387–402 (2010).
Chu, E., Mychasiuk, R., Hibbs, M. L. & Semple, B. D. Dysregulated phosphoinositide 3-kinase signaling in microglia: Shaping chronic neuroinflammation. J. Neuroinflamm. 18(1), 276 (2021).
Miller, Y. I., Choi, S. H., Fang, L. & Tsimikas, S. Lipoprotein modification and macrophage uptake: Role of pathologic cholesterol transport in atherogenesis. Subcell. Biochem. 51, 229–251 (2010).
Moore, K. J. et al. Loss of receptor-mediated lipid uptake via scavenger receptor A or CD36 pathways does not ameliorate atherosclerosis in hyperlipidemic mice. J. Clin. Investig. 115(8), 2192–2201 (2005).
Solinas, G. & Becattini, B. PI3K and AKT at the interface of signaling and metabolism. Curr. Top. Microbiol. Immunol. 436, 311–336 (2022).
Tanaka, S. & Baba, Y. B cell receptor signaling. Adv. Exp. Med. Biol. 1254, 23–36 (2020).
Gruber, E. J., Aygun, A. Y. & Leifer, C. A. Macrophage uptake of oxidized and acetylated low-density lipoproteins and generation of reactive oxygen species are regulated by linear stiffness of the growth surface. PLoS ONE 16(12), e0260756 (2021).
Guo, X. et al. TREM2 promotes cholesterol uptake and foam cell formation in atherosclerosis. Cell. Mol. Life Sci. 80(5), 137 (2023).
Kucuksezer, U. C. et al. The role of natural killer cells in autoimmune diseases. Front. Immunol. 12, 622306 (2021).
Fogel, L. A., Yokoyama, W. M. & French, A. R. Natural killer cells in human autoimmune disorders. Arthritis Res. Ther. 15(4), 216 (2013).
Zhao, Z., Gao, Y., Pei, X., Wang, W. & Zhang, H. Causal role of immune cells in Hashimoto’s thyroiditis: Mendelian randomization study. Front. Endocrinol. (Lausanne) 15, 1352616 (2024).
Okada, Y. & Yamamoto, K. Genetics and functional genetics of autoimmune diseases. Semin. Immunopathol. 44(1), 1–2 (2022).
Acknowledgements
The authors wish to thank GEO for providing open access to the database.
Funding
This work was supported by National Construction Project for Traditional Chinese Medicine Specialties with Advantages (Gan Cai She Zhi [2024] No. 39) (Translated name); NATCM’s Project of High-level Construction of Key TCM Disciplines (zyyzdxk-2023113); Jiangxi Province Key Laboratory of Traditional Chinese Medicine for Cardiovascular Diseases (2024SSY06301); National Natural Science Foundation of China (82374367); Natural Science Foundation of Jiangxi Province (20242BAB26163, 20232BAB206144).
Author information
Authors and Affiliations
Contributions
All authors have read and approved the final manuscript. Y.M. and J.L. conducted the bioinformatics research. Y.M., S.W., and J.H. designed the research methods. Y.M., Q.W., and Z.Z. analyzed the data. Y.M. and Y.L. wrote the paper. J.W. led the entire research project and reviewed and approved the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ma, Y., Wu, S., Lai, J. et al. Exploring the comorbidity mechanisms between atherosclerosis and hashimoto’s thyroiditis based on microarray and single-cell sequencing analysis. Sci Rep 15, 1792 (2025). https://doi.org/10.1038/s41598-025-85112-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-85112-0