Abstract
Mice (Mus musculus) are one of the most commonly used animal species in basic science and translational research worldwide. Ovariectomy and hysterectomy are frequently employed to explore the systemic effects of the sex-hormone axis and other pathological conditions. While several surgical protocols exist for dorsal ovariectomy in rodents, very few address a ventral midline technique, and none are specific to the mouse model. Historically, ventral midline approaches have been considered technically challenging due to unique anatomical features, including long, thin uterine horns, fragile salpinges, short ovarian suspensory ligaments, and small animal size. This protocol provides a detailed guide for performing ovariectomy, hysterectomy, or ovariohysterectomy in mice, including the microsurgical steps required. All procedures were performed using an operative stereomicroscope under 3-5x magnification. The mean weight of the mice was 24 g (SD = 2 g), with ages ranging from 19 to 21 weeks. Of the 255 surgeries performed, 3 post-operative deaths occurred, resulting in an attrition rate of 1.18%. Post-operatively, all mice were housed in groups with fresh, paddy husk bedding, and no infections or wound breakdown were observed. Despite their small size and the manipulation of several vital anatomical structures, this procedure is easily reproducible and well-tolerated in mice.
Similar content being viewed by others
Introduction
The murine animal model (Mus musculus) is one of the most commonly used species for basic science and translational research. Compared to larger mammalian species, they reach reproductive maturity quickly, are relatively inexpensive to maintain, can be easily bred, and not difficult to handle1. The average lifespan of mice is also sufficient for studying complex disorders such as aging, neurodegenerative diseases, heart disease, obesity, and hypertension2,3,4,5,6. Despite the clear differences in size and stature from Homo sapiens, this species’ genome is remarkably similar, with around 90% of both genomes partitioned into conserved syntenic regions7. Approximately 40% of the nucleotides in humans align with those in mice7. Per the European Committee, mice comprised the majority (61%) of the 11.5 million laboratory animals used in 2011 for research7.
Among the commonly performed surgeries for this species, the ovariectomy model serves several important functions. It can be used to investigate many of the physiologic and endocrine changes that occur during menopause, including metabolic syndrome, osteoporosis, endocrine deficiency, cardiovascular disease, and even cerebrovascular diseases such as aneurysms8,9,10,11. The uterus has also become an organ of growing interest. Hysterectomy represents one of the most common surgeries for women in the United States, second only to cesarean section, with an estimated 1/3 of women undergoing the procedure by the age of 6012,13. Rodent models have been employed to study the effects of the uterus including on the ovaries, cognitive processes, and endocrine function14,15,16. A combination of both procedures, known as ovariohysterectomy, can also be performed, although more commonly conducted on rabbits or other larger, non-rodent species17.
Recently, the hysterectomy model has become relevant for cerebral aneurysm research as well18. VEGF has been implicated in the pathogenesis of both abdominal aortic and intracranial aneurysms19,20,21,22. Conflicting reports exist regarding changes in systemic VEGF levels following hysterectomy in women23,24. It is well established that VEGF plays a vital role in the vascular repair of the endometrium following the menstrual cycle, as cyclic regeneration requires a highly regulated angiogenic response25. However, Byrne et al. (2007) found significantly greater plasma VEGF levels in post-menopausal women compared to those who had undergone hysterectomy (80.4 vs. 38.4 pg/ml, p < 0.05).24 Though this animal model represents the first investigation into this topic, it is not the first investigation predicated on the uterus having a systemic role beyond that of reproduction. For instance, women with a history of hysterectomy have shown higher rates of dementia26,27. Koebele et al. (2019) discovered that hysterectomized rats exhibited detrimental effects on their ability to manage high-demand working memory loads, a phenomenon not observed in ovariohysterectomized rats15. Our investigation into the uterus’s relationship with VEGF and intracranial aneurysms remains active, with ongoing data collection related to this topic.
Despite the growing indications for the use of these models, a limited number of technical protocols exist. Ovariohysterectomy in caviomorph species is considered particularly challenging due to long and thin uterine horns, fragile salpinges, and short ovarian suspensory ligaments. For these reasons the dorsal approach for ovariectomy has been more popular and widely recommended28,29. However, depending on the experimental study design, a ventral approach may be necessary to perform a hysterectomy with or without simultaneous ovariectomy. While only one article exists that provides a technical summary of the ventral midline approach for bilateral ovariectomy in a Wistar rat, no protocol or guide has been found for the hysterectomy or ovariohysterectomy technique, especially in the mouse model30. Mice are significantly smaller than rats, averaging about 1/10th the weight (20–40 g vs. 267–500 g for females)31. Amongst the available studies that provide descriptions of the surgical procedure, they often lack specific steps needed to achieve a high level of procedural fidelity15,32.
In this manuscript, we provide a comprehensive description of three surgical procedures—hysterectomy, ovariectomy, and ovariohysterectomy—using a midline partial laparotomy approach in C57BL/6 female mice aged 19–21 weeks, purchased from Jackson Laboratory (Barr Harbor, ME, USA). The mean pre-operative weight for all mice was 24 g (SD 2 g). This study was conducted in accordance with relevant ethical guidelines and regulations. The experimental protocol was approved by the Institutional Animal Care and Use Committee (IACUC) of St. Joseph’s Hospital and Medical Center. All methods were reported in compliance with the ARRIVE guidelines.
Methods
Positioning
Mice were placed in a dorsal recumbent position, with their nose placed within a tubing apparatus to receive continuous intake of isoflurane (1.8–2.3%) delivered at 2 L/min of positive pressure (Fig. 1A). They were positioned over an absorbent waterproof pad that covered a heating pad which maintained a normothermic body temperature. Two strips of paper tape, each 2–3 cm in length, were used to secure the hind limbs in place. The abdomen was clipped and aseptically prepared using a mixture of 70% ethanol and 30% H2O solution. Buprenorphine (Pfizer Inc., NY, NY, USA) was injected subcutaneously and bupivacaine (Marcaine; Pfizer Pharmaceutical, Hospira Inc., Lake Forest, IL, USA) was injected midline along the planned incision for analgesia. All procedures were performed using an operating stereomicroscope at 3-5x magnification (World Precision Instruments, Model# PZMTIV-BS, Sarasota, FL, USA). A detailed list of the items used to perform these procedures is provided in Table 1. All numeric results are reported descriptively, and non-parametric continuous data were compared using the Wilcoxon rank-sum test in the statistical analysis platform STATA 14.2 (StataCorp LLC, College Station, TX, USA). A p-value less than 0.05 was considered statistically significant.
Positioning and relevant anatomy. Figure 1A: The mouse was positioned in dorsal recumbent position, with its nose secured in a tubing apparatus for continuous isoflurane delivery. Tissue retractors were positioned adjacent to the abdomen in preparation for the procedure. Figure 1B: The location and planned size of the incision is shown, measuring approximately 2 cm, as indicated by a ruler held next to the ink mark. Figure 1C: The opening through the linea alba is depicted, with entry into the abdominal compartment. Elevation of the abdominal musculature while expanding the opening was crucial for preventing bowel injury. Figure 1D: Relevant anatomical structures are visualized upon retracting the abdominal wall.
Incision
While elevating the skin with forceps to avoid injury to underlying structures, a midline incision was made that extended beneath the dermis but above the abdominal wall. The incision was started 0.3–0.5 cm superior to the urethral orifice and advanced approximately 2 cm superiorly, traversing one-half to three-fourths of the abdomen (Fig. 1B). With the abdominal wall still intact, blunt dissection was used to open the plane between the dermis and musculature.
Intraperitoneal access
A second incision was made through the linea alba with scissors while elevating the abdominal wall with forceps. Peritoneal cavity entrance can be easily detected and when air enters the abdomen, the organs fall away from the body wall (Fig. 1C). However in some cases the bowel may be adherent to the abdominal wall, such as in unhealthy subjects, and can be at risk of injury. While the bladder may also be at risk caudally, it is a bulbous structure and less likely to be entrapped by scissors. As the incision is extended cranially, the blunt end of an instrument can be used to ensure that the bowel is not adherent to the abdominal wall, allowing for safe extension of the opening.
Starting on the left side, the abdominal wall was retracted laterally using tissue retractors. Depending on the mouse’s age and habitus, a large fat pad of varying size overlies the lower quadrants of the peritoneum (Fig. 1D). This fat pad was gently elevated and exteriorized without injury. The fat pad was attached to the ventral side of the left uterine horn (Fig. 2A). At this junction, the uterine horn was located and traced distally until the oviduct (or Fallopian tube in humans) was identified. While the uterine horn can be easily confused for a loop of small bowel, the oviduct has a distinct, convoluted tubular appearance, confirming the correct anatomical structure and location (Fig. 2B).
Surgical maneuvers for locating the uterus and ovary. Figure 2A: The first step in the abdominal approach was the exteriorization of the fat pad. Following the ventral aspect of this tissue, the mesometrium was identified, leading to the uterine horn. Figure 2B: The uterine horn was gently elevated. Along its distal edge, a tubular structure representing the oviduct was visible. Distal to this, periovarian fat was tethered to the dorsal body wall. Figure 2C: After releasing the ovarian suspensory ligament, the uterine horn and periovarian fat pad could be easily mobilized. Within the mesometrium, the ovarian artery, uterine artery, radial arteries from the uterine artery were present, along with related veins. Depending on the specific procedure, one or all of these vessels may have needed to be sacrificed. Abbreviations: POFP; periovarian fat pad.
Ovariectomy
After identifying the oviduct, angled forceps were used to gently push any bowel that may obstruct the view of the dorsal body wall out of the way. The periovarian fat pad, which was larger than the ovary, then became visible. The ovary was embedded within this fat, located adjacent to the oviduct. Two important structures were also present within this fat: the ovarian suspensory ligament and the branches of the ovarian artery (along with related veins). A framework for the relevant arterial blood supply of the ovary and uterus is provided in Fig. 3.
Using the angled forceps, the fat was grasped firmly while avoiding inadvertent injury to the small intestine or ovary (Fig. 4A). With the non-dominant hand, the fat was slowly dissected in a piecemeal manner by applying counter pressure with the forceps (Fig. 4B). After some resistance, the ovarian suspensory ligament was released, often accompanied by a distinct snap. At this point, the uterine horn becomes very mobile as the ovary was no longer tethered to the dorsal abdominal wall (Fig. 4C).
Release of the ovarian suspensory ligament and mobilization of the uterine horn. Figure 4A: To perform either an ovariectomy or ovariohysterectomy through a ventral midline approach, the ovarian suspensory ligament had to be released. Using angled forceps, a firm grasp of the periovarian fat pad was obtained, as shown here. Special care had to be taken to avoid grasping the small bowel or other nearby structures during this maneuver. It was important to grasp deep to the ovary, as directly grasping the ovary could risk disrupting the ovarian capsule and allow for seeding of ovarian cells in the abdomen. Additionally, care had to be taken to avoid grasping the ovarian artery or any large branches, which could occur if too large of a tissue grasp was made. If this happened, the tissue was released, and a smaller grasp of the periovarian fat pad was taken. Figure 4B: With the non-dominant hand, small counter-traction movements were made to dissect through the soft tissue along the edge of the angled forceps, as depicted by the arrows. A sudden release of tension was usually felt, signifying the release of the ovarian suspensory ligament. Figure 4C. The ovary, oviduct, and uterine horn could then be easily mobilized and exteriorized. Abbreviations: POFP; periovarian fat pad, L; left.
As shown in Fig. 5A, the ovary was still be tethered to the abdomen by branches from the ovarian artery and related veins. An opening through the mesometrium membrane was made at the junction of the oviduct and most distal tip of the uterine (Fig. 5B). A braided 5.0 silk suture (Ethicon Mersilk Sutures, Johnson & Johnson Ltd., New Brunswick, NJ, USA) was tied through this opening (Fig. 5C). One knot was sufficient. The oviduct was then cut on the ovarian side of the tie and removed, leaving the uterus intact and allowing for removal of the ovary. The uterine horn was then reinserted into its original position (Fig. 5D). This procedure was then repeated on the contralateral side.
Separation of the uterine horn from the ovary and oviduct. Figure 5A: This figure demonstrates the preservation of the ovarian artery branches and radicular branches of the uterine artery after the ovarian suspensory ligament was released. Figure 5B: A small opening was made through the mesometrium membrane using the gentle spreading function of the angled forceps. Figure 5C: A 5.0 silk suture was then passed through the opening, and a knot was tied. Figure 5D A cut was made on the side of the uterine horn, allowing for the release of the uterine horn from the preserved ovary and oviduct. Abbreviations: POFP; periovarian fat pad, R; right.
Hysterectomy
To perform a hysterectomy while preserving the ovaries, a small opening was made through the mesometrium membrane at the junction of the oviduct and uterine horn using the angled forceps tips. A 5.0 silk suture was placed through this opening and tied with 1 knot. Alternatively, cautery with bipolar forceps and scissors could also be used to separate the oviduct and uterine horn. Once the uterine horn was released, a cut was made on the side of the suture towards the uterus, leaving the ovary in the abdomen. The uterine horn was then elevated with light traction, allowing for careful cauterization of the branches of the uterine loop artery (radial arteries) with bipolar forceps. This process was continued in a cranial-to-caudal direction until the cervix was reached for both uterine horns, which is just posterior to the bladder.
With both uterine horns exteriorized and the radial arteries from the uterine artery and associated veins released, a ligature was placed around the cervix. The bladder may partially obstruct the view, but switching angles from each side will provide sufficient visualization and maneuverability. After one knot was thrown, it was slid down inferiorly as much as possible before tightening. Once in position, it was tightened and a second knot was thrown in the same direction (surgeon’s knot) to firmly secure it.
Ovariohysterectomy
A combination of the procedures listed above was performed, with the exception that no ligature was placed through the mesometrium membrane at the uterine-oviduct junction. Instead, the ovary was simply released from the ovarian suspensory ligament followed by cautery and release of the blood vessels branching from the ovarian artery and associated veins. The hysterectomy procedure was then completed (Fig. 6).
Major steps related of the ovariohysterectomy. Both ovarian suspensory ligaments and ovarian arteries had been released from their respective uterine horns, allowing for exteriorization as shown here. The uterine artery and radial arteries supplying the uterine horn had also been released down to the cervix. A 5.0 silk knot was placed across the cervix, with the first knot intentionally kept loose to allow positioning lower on the cervix, followed by a second knot that was tightened. The bladder was situated midline and directly anterior to the cervix. Often, a slightly eccentric view was necessary to visualize the anatomy effectively. In this case, the uterine horns were pulled toward the operator’s right, while the bladder was shifted to the left, providing excellent visualization of the cervix.
Closure
At the time of closure, careful inspection was made to ensure there was no active bleeding. Any areas of pooled blood was evacuated using absorbent material to reduce postoperative inflammation. The abdominal wall was closed in a running fashion using a 5.0 polyglactin 910 suture (Coated Vicryl Suture, Ethicon Inc., Raritan, NJ, USA). Suturing was started at the most cranial end of the incision and continued caudally. Maintaining tension on the suture to reapproximate the abdominal edges without moving the body occasionally required counter-pressure with forceps while tightening. Four or five knots were tied to secure the suture. The abdominal wall was closely inspected for any loose sutures or gaps that could allow herniation of bowel (Supplemental Fig. 1A). Any gaps identified were oversewn with interrupted sutures to reinforce the closure.
The skin edges were then aligned using forceps in the non-dominant hand, while stainless-steel wound clips (Braintree Scientific, Braintree, MA, USA) were placed sequentially with the dominant hand (Supplemental Fig. 1B). If a clip appeared poorly placed, it was removed and replaced.
Post-operative care
The mice were placed in an autoregulated incubator with controlled temperature at 38 °C and 38% humidity. They were kept in the incubator for approximately 1–2 h until they exhibited normal spontaneous movement. Afterward, they were housed in a cage with fresh, paddy husk bedding, along with up to 3–4 other mice that underwent the same surgery. After 4–6 h post-surgery, the mice received a second subcutaneous injection of Buprenorphine for extended pain relief. Mice were monitored at least once daily by research staff, who inspected the wounds. If a wound clip appeared loose or had fallen off, it was replaced with a new clip. Wound clips were removed on post-operative day 10.
Results
Attrition rate/Complications
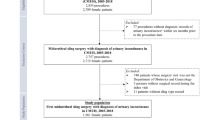
A total of 65 mice underwent ovariectomy, 124 hysterectomy, and 66 ovariohysterectomies. The sample size was based on calculations from an umbrella aneurysm study outside the scope of this manuscript. A subgroup analysis of recorded operative times was conducted for two groups of 15 mice each. In the first group (n = 15), a single surgical operator performed the entire hysterectomy procedure, with an average duration of 8:36 min (SD 1 min; range: 7:10–11:10 min). In the second group (n = 15), two surgical operators were involved: surgical operator #1 performed the opening and hysterectomy, while surgical operator #2 performed the closure. The average time for surgical operator #1 was 4:02 min (SD 0.42 min; range: 3:15–4:32 min), while surgical operator #2 took an average of 2:10 min (SD 0.28 min; range: 1:41–2:51 min). Since the opening and hysterectomy phase (performed by operator #1) took longer than the closure phase (performed by operator #2), operator #2 was ready to receive the next mouse as soon as the hysterectomy was completed. This setup significantly reduced the average time per mouse compared to a single operator performing the entire procedure: surgical operator #1 averaged 4:02 min vs. 8:36 min per mouse (p < 0.001), and surgical operator #2 averaged 2:10 min vs. 8:36 min per mouse (p < 0.001). The total operative time for the two-surgical operator setup was 77 min, compared to 129 min and 10 s with a single operator.
The attrition rate for ovariectomy, hysterectomy, and ovariohysterectomy was 1.5% (1/65, post-operative day 2), 0.8% (1/124, post-operative day 9), and 1.5% (1/66, post-operative day 3), respectively. The cumulative rate for all 3 surgeries was 1.18% (3/255). Two mice (0.83%, 2/240) sustained partial small intestine injuries during the abdominal wall opening. These injuries were repaired primarily with 6.0 Nylon sutures (Ethilon Nylon Sutures, Johnson & Johnson Ltd., New Brunswick, NJ, USA) to reapproximate the intestinal edges. There were also two instances of bladder injury. In both cases, the bladder was inadvertently punctured with the forceps tips during manipulation, leading to extravasation of urine. The first case resolved with tamponade, and the bladder began refilling as normally expected. The second case required a suture to reapproximate the bladder edges where the urine leak had occurred. These mice survived without any behavioral or weight changes. None of the mice in the study developed signs of postoperative infections or wound dehiscence. A summary of surgical procedures performed, and complications is provided in Table 2.
Discussion
Ovariectomies and hysterectomies have been used to study various physiological and disease processes. Since 1986, 9 articles detailing the ovariectomy procedure have been identified, with the majority (6/9) describing only the dorsal technique (Table 3)17,28,30,33,34,35,36,37,38. This technical protocol provides the first comprehensive surgical guide for performing a hysterectomy, ventral ovariectomy, and ovariohysterectomy in the Mus musculus species. We found that visual magnification of 3-5x with an operating stereomicroscope is necessary to conduct this surgery. Despite the small size of the animal and the manipulation of several vital anatomical structures, the procedure is easily reproducible and well-tolerated, with a relatively low attrition rate of 1.18%. While the dorsal approach for ovariectomy is considered less technically demanding and more commonly used, a ventral approach is essential for performing a hysterectomy28,29. Depending on the investigatory aims, the same ventral approach can be employed for hysterectomy, ovariectomy, or ovariohysterectomy. This consistency allows for maintaining the same experimental conditions across study groups, avoiding discrepancies that could arise from using a dorsal ovariectomy for one group and a ventral midline hysterectomy for another.
Post-operative mortality and complications
During the study period, three post-operative deaths occurred. Given that two of these mortalities were delayed (24–72 h following surgery), we suspect that they may have been related to inadvertent injury to the bowel during manipulation, leading to septicemia. The etiology of the third death on post-operative day 9 is unclear and may or may not have been directly related to the surgery. While the most technically challenging aspects of the surgery involved dissecting the periovarian fat pad and placing a silk tie through the mesometrial membrane along the oviduct, no known complications occurred during these steps. However, there were two instances during the initial opening of the abdominal wall where the small intestine was adherent to the abdominal wall and was inadvertently cut with the fine scissors. To mitigate this risk, it is advisable to elevate the abdominal wall and carefully develop the plane between the intestines with the blunt end of forceps or cotton swabs before extending the incision superiorly.
Technical considerations
Several other technical points are important to emphasize when performing this procedure. During the incision, a key step is developing the plane between the dermis and abdominal musculature using blunt dissection. If the dermis is tightly tethered to the musculature, it may be difficult to properly imbricate the skin edges after suturing the abdominal wall, especially when using wound clips. Additionally, when entering the peritoneum, maintaining a perfectly midline incision through the linea alba can be challenging, particularly as the rectus abdominis muscle thickens and dives toward the pubic bone caudally. In such cases, bipolar cautery or gentle pressure should be sufficient to control the typically minimal bleeding.
Another important consideration is to avoid violating the ovarian capsule throughout the procedure, as even slight contact with the ovary can disrupt the capsule and potentially lead to seeding of ovarian cells, which could reimplant and retain estrous activity17. To prevent this, grasp the ovarian fat a few millimeters posterior to the oviduct and ovary (Fig. 4A), then begin dissecting through the periovarian fat pad (Fig. 4B). At the same time, it is important to preserve the blood supply (i.e. ovarian artery, uterine artery, and associated branches) which if disrupted, could inadvertently injure the uterus and compromise its function in a delayed manner. There is also risk for crush injury when manipulating the uterine horns with forceps. Thus, it is important to minimize grasping the uterine horn and use gentle pressure when possible.
All intraperitoneal portions of the surgeries were started on the left side. In veterinary surgery, the right ovary has been reported to be less visible and more challenging to access than the left39,40. A similar pattern was observed in this study due to increased crowding from the bowel. Although the right side is typically approached first in other larger species, identifying and exteriorizing the left uterine horn first provided some advantage in then locating the right side41,42. Surgeon preference likely also contributed to starting on the left side as well.
Iatrogenic injury to the ureters is a known risk when performing ovariohysterectomies in larger animal species such as cats and dogs43,44. While this may be possible in mice, no known ureter injuries were observed in this study. Anatomically, the ureters are located more medially and travel along the dorsal body wall, deeper in the abdomen compared to the uterine horns. Additionally, the broad ligament supporting the uterine horns is flimsier and very mobile in mice45. This allows the uterine horns to be maneuvered into a more superficial position relative to the intrabdominal space and away from the ureters, especially when the ovarian suspensory ligament is released and the uterine horns are exteriorized. Although the ureters approach the cervix near their bladder attachments, this area is deeper, and ligature placement across the cervix maintains a plane that is superficial to the ureters. Together, these anatomical factors make iatrogenic injury to the ureters less likely. Lastly, while closing the incision may seem tedious, it is crucial to perform this step meticulously to prevent wound dehiscence. A well-approximated skin closure is essential to avoid major complications, such as infection or bowel herniation.
Comparison to previous techniques
Among the available literature on this topic, Khajuria et al. (2012) detail a similar ventral approach for ovariectomy in Wistar rats30. However, their technique involves a smaller abdominal exposure through a paramedian (0.4–0.6 cm) incision. We found a larger incision (2 cm) using a midline partial laparotomy was necessary for feasibility in the mouse model. Since the ovarian artery ligament must be preserved for the hysterectomy, externalization is not feasible through a limited exposure. Additionally, the authors also recommended the use of sterilized cotton fabric for dry bedding to prevent wound breakdown, a suggestion echoed by Sophocleous and Idris (2014)35. In our study, we used fresh paddy husk bedding without any instances of wound infections or related complications. A well-fastened abdominal closure using a running polyglactin 910 suture, along with wound clips for the skin, provided adequate protection against debris entering the wound and minimized the risk of infection. It is important to note that no antibiotics were administered in this study.
Post-operatively, mice were housed together with those that underwent the same surgery, which proved feasible without any complications related to cage-mate induced post-surgical trauma. Conflicting reports exist regarding the use of single- versus grouped-housing after surgery15,30,34,35. Although individual housing can be an option, it may not be practical depending on the size of a facility’s animal housing room and the number of mice being studied. Additionally, individual housing may increase daily husbandry costs. Van Loo et al. (2007) compared recovery in mice housed apart together with a barrier separating them, socially house mice, and individually housed mice. All subjects underwent laparotomy with the implantation of a radiotelemetry transmitter. Their findings indicated that socially housed mice were less effected by the abdominal surgery than those individually housed, based on metrics such as heart rate and behavior46. A recent follow-up study by Tirado-Muniz et al. (2023) also found that paired housing post-surgery benefited the well-being of mice without increasing trauma to the surgical incision site or disrupting wound clips47.
Refinements to the surgical technique
During the development of this technique within our laboratory, several refinements were made. We transitioned from using a silk ligature to bipolar sealing when releasing the uterine horn from the ovary. Bipolar sealing has previously been reported as an effective alternative to sutures for vaginal hysterectomies in humans48. Although some disadvantages of this technique may include the risk of iatrogenic injury by thermal spread or incorrect placement with cautery, no known complications occurred related to its use. Silk suture use can also have adverse effects, such as increased tissue reactivity, granuloma formation, and bacterial colonization49,50. Despite these limitations, braided silk sutures possess good tensile strength, knot security, excellent handling characteristics, and frequently used as a ligature in mouse surgery51,52. Overall, bipolar cautery was found to be slightly less labor-intensive, while both methods appeared to be equally effective.
Initially, the procedure was performed by a single surgical operator, which was manageable but required significant time commitments. With the assistance of a second surgical operator at an adjacent operating field, wound closure could then be delegated, which, as expected, led to a significant reduction in the operating time per surgical operator (p < 0.001). Another common issue encountered was the ligature tie slipping off the cervix after the uterus was released. We improved success in this step by using two knots in the same direction (also referred to as surgeon’s knot) instead of one and employing two needle forceps to grip the edges of the silk tie while tightening the second knot. Transfixation of the cervix with a small hemostat forceps may assist in positioning the knot at a satisfactory location. However, this method was not attempted due to the small size of the anatomical structures and the potential risk of injury during placement.
Conclusion
In this study, we successfully performed ovariectomy, hysterectomy, and combined ovariohysterectomy following the detailed protocol outlined herein. Out of 255 total surgeries, 3 post-operative deaths occurred, resulting in an attrition rate of 1.18%. Post-operatively, all mice were housed in group settings with fresh, paddy husk bedding, and no dehiscence or wound infections or were observed. Although the small size of the animal and the manipulation of several vital anatomical structures present challenges, this technique is easily reproducible and well-tolerated by the mice. These findings offer a reliable surgical approach that can be utilized for a variety of experimental applications in murine models.
Data availability
All data generated or analyzed during this study are included in this manuscript. Detailed records of the surgical procedures, attrition rates, and other relevant information are available for review. Additional data can be requested from the corresponding author.
References
Bryda, E. C. The mighty mouse: the impact of rodents on advances in biomedical research. Mo Med. 110, 207–211 (2013).
Sanchez-Varo, R. et al. Transgenic Mouse Models of Alzheimer’s Disease: An Integrative Analysis. Int. J. Mol. Sci. 23 https://doi.org/10.3390/ijms23105404 (2022).
Lutz, T. A. & Woods, S. C. Overview of animal models of obesity. Curr. Protoc. Pharmacol. Chap. 5 https://doi.org/10.1002/0471141755.ph0561s58 (2012). Unit5.61.
Cai, N., Wu, Y. & Huang, Y. Induction of Accelerated Aging in a Mouse Model. Cells 11, (2022). https://doi.org/10.3390/cells11091418
Jama, H. A. et al. Rodent models of hypertension. Br. J. Pharmacol. 179, 918–937. https://doi.org/10.1111/bph.15650 (2022).
Camacho, P., Fan, H., Liu, Z. & He, J. Q. Small mammalian animal models of heart disease. Am. J. Cardiovasc. Dis. 6, 70–80 (2016).
Breschi, A., Gingeras, T. R. & Guigó, R. Comparative transcriptomics in human and mouse. Nat. Rev. Genet. 18, 425–440. https://doi.org/10.1038/nrg.2017.19 (2017).
Medina-Contreras, J., Villalobos-Molina, R., Zarain-Herzberg, A. & Balderas-Villalobos, J. Ovariectomized rodents as a menopausal metabolic syndrome model. A minireview. Mol. Cell. Biochem. 475, 261–276. https://doi.org/10.1007/s11010-020-03879-4 (2020).
Joll, J. E. 2, Bersi, M. R., Nyman, J. S., Merryman, W. D. & nd, & Evaluation of early bilateral ovariectomy in mice as a model of left heart disease. Am. J. Physiol. Heart Circ. Physiol. 322, H1080–h1085. https://doi.org/10.1152/ajpheart.00157.2022 (2022).
Tada, Y. et al. Estrogen protects against intracranial aneurysm rupture in ovariectomized mice. Hypertension 63, 1339–1344. https://doi.org/10.1161/hypertensionaha.114.03300 (2014).
Zhou, S. et al. Age-dependent variations of cancellous bone in response to ovariectomy in C57BL/6J mice. Exp. Ther. Med. 15, 3623–3632. https://doi.org/10.3892/etm.2018.5839 (2018).
Stewart, E. A., Shuster, L. T. & Rocca, W. A. Reassessing hysterectomy. Minn. Med. 95, 36–39 (2012).
Wright, J. D. et al. Nationwide trends in the performance of inpatient hysterectomy in the United States. Obstet. Gynecol. 122, 233–241. https://doi.org/10.1097/AOG.0b013e318299a6cf (2013).
Gündoğdu, B. et al. What is the impact of PPAR-γ agonist-rosiglitazone on ovarian reserve after hysterectomy? An experimental study. Turk. J. Med. Sci. 50, 1399–1408. https://doi.org/10.3906/sag-2002-117 (2020).
Koebele, S. V. et al. Hysterectomy uniquely impacts spatial memory in a rat model: a role for the nonpregnant uterus in cognitive processes. Endocrinology 160, 1–19. https://doi.org/10.1210/en.2018-00709 (2019).
Tapisiz, O. L. et al. Does hysterectomy affect ovarian function? Histopathologic evaluation and serum FSH, inhibin A, and inhibin B levels in an experimental rat model. Eur. J. Obstet. Gynecol. Reprod. Biol. 140, 61–66. https://doi.org/10.1016/j.ejogrb.2008.04.001 (2008).
Olson, M. E. & Bruce, J. Ovariectomy, ovariohysterectomy and orchidectomy in rodents and rabbits. Can. Vet. J. 27, 523–527 (1986).
Nisson, P. L. et al. Cerebral aneurysms Differ in patients with hysterectomies. World Neurosurg. 120, e400–e407. https://doi.org/10.1016/j.wneu.2018.08.093 (2018).
Xu, B. et al. Inhibition of VEGF (vascular endothelial growth Factor)-A or its receptor activity suppresses experimental aneurysm progression in the aortic elastase infusion Model. Arterioscler. Thromb. Vasc Biol. 39, 1652–1666. https://doi.org/10.1161/atvbaha.119.312497 (2019).
Kaneko, H. et al. Role of vascular endothelial growth factor-A in development of abdominal aortic aneurysm. Cardiovasc. Res. 91, 358–367. https://doi.org/10.1093/cvr/cvr080 (2011).
Skirgaudas, M., Awad, I. A., Kim, J., Rothbart, D. & Criscuolo, G. Expression of angiogenesis factors and selected vascular wall matrix proteins in intracranial saccular aneurysms. Neurosurgery 39, 537–545. https://doi.org/10.1097/00006123-199609000-00021 (1996). discussion 545 – 537.
Nisson, P. L. et al. Vascular endothelial growth factor and the Pathogenesis of Intracranial aneurysms: a systematic review on the Missing Link in a Complex Pathway. J. Am. Heart Assoc. 13, e035638. https://doi.org/10.1161/jaha.124.035638 (2024).
Lowery, A. J. et al. The effect of menopause and hysterectomy on systemic vascular endothelial growth factor in women undergoing surgery for breast cancer. BMC Cancer. 8, 279. https://doi.org/10.1186/1471-2407-8-279 (2008).
Byrne, G. J. et al. Serum vascular endothelial growth factor in breast cancer. Anticancer Res. 27, 3481–3487 (2007).
Graubert, M. D., Ortega, M. A., Kessel, B., Mortola, J. F. & Iruela-Arispe, M. L. Vascular repair after menstruation involves regulation of vascular endothelial growth factor-receptor phosphorylation by sFLT-1. Am. J. Pathol. 158, 1399–1410. https://doi.org/10.1016/s0002-9440(10)64091-6 (2001).
Gong, J., Harris, K., Peters, S. A. E. & Woodward, M. Reproductive factors and the risk of incident dementia: a cohort study of UK Biobank participants. PLoS Med. 19, e1003955. https://doi.org/10.1371/journal.pmed.1003955 (2022).
Rocca, W. A., Grossardt, B. R., Shuster, L. T. & Stewart, E. A. Hysterectomy, oophorectomy, estrogen, and the risk of dementia. Neurodegener Dis. 10, 175–178. https://doi.org/10.1159/000334764 (2012).
Capello, V. Common surgical procedures in pet rodents. J. Exotic pet. Med. 20, 294–307 (2011).
Miwa, Y. & Sladky, K. K. Small mammals: Common Surgical procedures of rodents, ferrets, hedgehogs, and Sugar Gliders. Vet. Clin. North. Am. Exot Anim. Pract. 19, 205–244. https://doi.org/10.1016/j.cvex.2015.09.001 (2016).
Khajuria, D. K., Razdan, R. & Mahapatra, D. R. Description of a new method of ovariectomy in female rats. Rev. Bras. Reumatol. 52, 462–470 (2012).
Frohlich J. Rats and Mice. Ferrets, Rabbits, and Rodents, 345–367, (2020). https://doi.org/10.1016/B978-0-323-48435-0.00025-3
Gonzalez, M. I., Field, M. J., Bramwell, S., McCleary, S. & Singh, L. Ovariohysterectomy in the rat: a model of surgical pain for evaluation of pre-emptive analgesia? Pain 88, 79–88, (2000). https://doi.org/10.1016/s0304-3959(00)00309-2
Lasota, A. & Danowska-Klonowska, D. Experimental osteoporosis–different methods of ovariectomy in female white rats. Rocz Akad. Med. Bialymst. 49 (Suppl 1), 129–131 (2004).
Idris, A. I. Ovariectomy/orchidectomy in rodents. Methods Mol. Biol. 816, 545–551. https://doi.org/10.1007/978-1-61779-415-5_34 (2012).
Sophocleous, A. & Idris, A. I. Rodent models of osteoporosis. Bonekey Rep. 3, 614. https://doi.org/10.1038/bonekey.2014.109 (2014).
Sophocleous, A. & Idris, A. I. Ovariectomy/Orchiectomy in Rodents. Methods Mol Biol 261–267, (1914). https://doi.org/10.1007/978-1-4939-8997-3_13 (2019).
Souza, V. R. et al. Description of Ovariectomy Protocol in mice. Methods Mol. Biol. 1916, 303–309. https://doi.org/10.1007/978-1-4939-8994-2_29 (2019).
Luengo-Mateos, M. et al. Protocol for ovariectomy and estradiol replacement in mice. STAR. Protoc. 5, 102910. https://doi.org/10.1016/j.xpro.2024.102910 (2024).
Liehmann, L. M., Seny, T. & Dupré, G. Effect of patient rotation on ovary observation during laparoscopic ovariectomy in dogs. Vet. Surg. 47, O39–o51. https://doi.org/10.1111/vsu.12764 (2018).
van Nimwegen, S. A. & Kirpensteijn, J. Laparoscopic ovariectomy in cats: comparison of laser and bipolar electrocoagulation. J. Feline Med. Surg. 9, 397–403. https://doi.org/10.1016/j.jfms.2007.03.007 (2007).
Coe, R. J., Grint, N. J., Tivers, M. S., Hotston Moore, A. & Holt, P. E. Comparison of flank and midline approaches to the ovariohysterectomy of cats. Vet. Rec. 159, 309–313. https://doi.org/10.1136/vr.159.10.309 (2006).
Reece, J. F., Nimesh, M. K., Wyllie, R. E., Jones, A. K. & Dennison, A. W. Description and evaluation of a right flank, mini-laparotomy approach to canine ovariohysterectomy. Vet. Rec. 171, 248. https://doi.org/10.1136/vr.100907 (2012).
Plater, B. L. & Lipscomb, V. J. Treatment and outcomes of ureter injuries due to ovariohysterectomy complications in cats and dogs. J. Small Anim. Pract. 61, 170–176. https://doi.org/10.1111/jsap.13100 (2020).
Wormser, C., Clarke, D. L. & Aronson, L. R. End-to-end ureteral anastomosis and double-pigtail ureteral stent placement for treatment of iatrogenic ureteral trauma in two dogs. J. Am. Vet. Med. Assoc. 247, 92–97. https://doi.org/10.2460/javma.247.1.92 (2015).
Miller, A., Hong, M. K. & Hutson, J. M. The broad ligament: a review of its anatomy and development in different species and hormonal environments. Clin. Anat. 17, 244–251. https://doi.org/10.1002/ca.10173 (2004).
Van Loo, P. L. et al. Impact of ‘living apart together’ on postoperative recovery of mice compared with social and individual housing. Lab. Anim. 41, 441–455. https://doi.org/10.1258/002367707782314328 (2007).
Tirado-Muñiz, N. et al. Evaluation of cage mate-induced Postsurgical Trauma in mice. J. Am. Assoc. Lab. Anim. Sci. 62, 170–178. https://doi.org/10.30802/aalas-jaalas-22-000085 (2023).
Levy, B. & Emery, L. Randomized trial of suture versus electrosurgical bipolar vessel sealing in vaginal hysterectomy. Obstet. Gynecol. 102, 147–151. https://doi.org/10.1016/s0029-7844(03)00405-8 (2003).
Boza, S. et al. Late abscess formation caused by silk suture following hysterectomy in a female dog. Reprod. Domest. Anim. 45, 934–936. https://doi.org/10.1111/j.1439-0531.2009.01366.x (2010).
Ishikawa, K. et al. Optimal sutures for use in the abdomen: an evaluation based on the formation of adhesions and abscesses. Surg. Today. 43, 412–417. https://doi.org/10.1007/s00595-012-0249-y (2013).
Eldawoody, H. et al. Simplified experimental cerebral aneurysm model in rats: comprehensive evaluation of induced aneurysms and arterial changes in the circle of Willis. Brain Res. 1300, 159–168. https://doi.org/10.1016/j.brainres.2009.08.099 (2009).
Chen, X., Hou, D., Tang, X. & Wang, L. Quantitative physical and handling characteristics of novel antibacterial braided silk suture materials. J. Mech. Behav. Biomed. Mater. 50, 160–170. https://doi.org/10.1016/j.jmbbm.2015.06.013 (2015).
Funding
Funding to conduct this study was provided by the Neurosurgery Education Research Foundation and Bagan Family Foundation Research Grant (PLN), Brain Aneurysm Foundation (TM), Barrow Neurological Foundation (TM, TH), and the National Institutes of Health R01NS109584, R01AG07780, and R01NS109382 (TH).
Author information
Authors and Affiliations
Contributions
P.L.N was responsible for conception of the project, developing the surgical technique, drafting the manuscript, making the figures, and data acquisition. T.M. was responsible for helping to develop the surgical technique, critical review of the manuscript and data acquisition. H.U. assisted in developing the surgical technique, critical review of the manuscript, and data acquisition. O.C. assisted in data acquisition. M.T.L provided critical review of the manuscript and administrative and supervisory support of the project. T.H. provided critical review of the manuscript and administrative and supervisory support of the project.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

41598_2025_85203_MOESM1_ESM.jpg
Supplementary Material 1: Supplemental Fig. 1A. The abdominal wall was closed using a 5.0 polyglactin 910 suture in a running fashion. The final knots (five total) were tied with needle forceps at the bottom of the figure. Sufficient spacing between suture throws and appropriate tension for wound closure are demonstrated. It is common for some bites to be either too distant or too loose; if this occurs, the wound should be reinforced with additional interrupted sutures until satisfactory closure is achieved. A well-developed plane between the skin edges and the abdominal wall can be seen, which is important for preventing tethering of the skin edges that could hinder proper wound approximation. Supplemental Fig. 1B. Wound clips were employed to close the skin edges, ensuring that they were imbricated. If a clip appeared loose or poorly positioned, it should be removed and reapplied until a satisfactory closure is obtained.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nisson, P.L., Maeda, T., Uchikawa, H. et al. Ventral Midline Hysterectomy, Ovariectomy, and Ovariohysterectomy in Mus Musculus: A Surgical Protocol. Sci Rep 15, 6625 (2025). https://doi.org/10.1038/s41598-025-85203-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-85203-y