Abstract
The potential role of hydrogen sulfide (H2S) in the modulation of neuropathic pain is increasingly recognized. This study investigated the therapeutic effect of intraperitoneal injection of the H2S donor sodium hydrosulfide (NaHS) on neuropathic pain. Utilizing the spared nerve injury (SNI) model in mice, the research investigates the role of astrocytes and the excitatory neurotransmitter glutamate in chronic pain. The findings reveal that sodium hydrosulfide (NaHS), an H2S donor, effectively enhances the mechanical pain threshold and thermal pain escape latency in SNI mice. The study further demonstrates NaHS’s potential in reducing glutamate levels in the spinal cord and the discharge frequency of neurons in the primary somatosensory cortex hindlimb region (S1HL) brain area, suggesting a novel therapeutic approach for neuropathic pain through the modulation of astrocyte function and EAAT2 expression.
Similar content being viewed by others
Introduction
With societal development, non-cancer chronic pain has become an increasingly severe health issue. The number of patients worldwide is rapidly rising, significantly impacting the quality of life and associated with complications such as depression, anxiety, and sleep disorders, further exacerbating the health burden on individuals1,2,3,4,5,6,7. Chronic pain not only poses a challenge to individuals but also exerts immense pressure on healthcare and socio-economic systems, consuming vast medical resources8. In response, the scientific community is thoroughly exploring the mechanisms of chronic pain, integrating findings from neuroscience, molecular biology, and immunology, progressively unraveling the mysteries of pain9,10. Research has delved into pain mechanisms from neuronal activity to molecular signaling, mainly focusing on neuronal plasticity, including peripheral and central sensitization. This reveals the nervous system’s response to injury and its relationship with neuropathic pain11,12,13.
Hydrogen sulfide (H2S), the third gaseous signaling molecule after nitric oxide and carbon monoxide, has attracted considerable attention due to its wide-ranging physiological and pathological effects14. These effects include vasodilation of smooth muscle, modulation of synaptic activity, induction of hippocampal long-term potentiation, and involvement in processes such as inflammation and cell apoptosis15. Recent studies have indicated that H2S plays a critical role in the regulation of various types of pain, especially in neuropathic pain, where H2S significantly alters pain thresholds by regulating the expression and synthesis of cystathionine β-synthase (CBS) in the spinal cord. Moreover, inhibition of CBS activity can alleviate hyperalgesia, suggesting that the CBS-H2S signaling pathway may be a novel target for treating neuropathic pain16. Furthermore, exogenous hydrogen sulfide has demonstrated potential in alleviating neuropathic pain. For instance, slow-release hydrogen sulfide donors, by releasing H2S, reduce neuropathic pain induced by paclitaxel or oxaliplatin, and hydrogen sulfide inhalation can enhance pain thresholds in mice while inhibiting spinal cord microglial activation17. These studies reveal the role of H2S in endogenous pain regulation and demonstrate its development potential as an exogenous therapeutic agent.
Historically, astrocytes in the central nervous system have been primarily regarded as supporting cells and received relatively little attention18,19. However, with an increasing understanding of glial cell interactions, research on astrocytes has gained prominence. Under healthy conditions, astrocytes support neuronal metabolism and maintain synaptic function by regulating extracellular potassium, glutamate, and water balance. They facilitate the development, maturation, and maintenance of synapses by forming barriers around synapses and regulating the local environment20,21,22. In the development of chronic pain, abnormal activation of astrocytes is closely associated with neuronal hyperexcitability and inflammatory responses, directly contributing to the formation and persistence of pain23,24. Studies have shown that activation of astrocytes through low-intensity transcranial direct current stimulation or chemogenetic methods can reduce injury-induced neuroplasticity and reverse abnormal pain, providing new therapeutic avenues for chronic pain treatment25. As a result, increasing attention has been given in recent years to the role of H2S in the modulation of astrocytes. Research by Shayea AMF et al. suggests that the H2S donor GYY4137 can alleviate the activation of astrocytes in the spinal cord of streptozotocin-induced diabetic rats17. These studies suggest that H2S may alleviate neuropathic pain by affecting the function of astrocytes.
In conclusion, H2S, by modulating ion channels and alleviating inflammation, provides a novel perspective for treating chronic pain. As a natural gaseous signaling molecule, H2S interacts with other molecules within the body and exhibits inherent biocompatibility, offering broad prospects for clinical applications. Although H2S holds great potential for treating chronic pain, its precise mechanisms remain unclear, particularly concerning its interaction with astrocytes, which requires further investigation. This study aims to explore the relationship between H2S and astrocytes in greater depth, providing innovative and practical strategies for treating chronic pain.
Methods
Animals
Adult male C57BL/6 mice, 8 weeks old, weighing 20–25 g, were procured from Liaoning Immortality Biological Technology Co., Ltd. (license: SCXK (Liao) 2023-KY-039). Within typical laboratory circumstances (12-hour light-dark cycle, lights on at 07:30 and off at 19:30; temperature maintained at 25 ± 2˚C; relative humidity 50–60%), they were kept in standard polycarbonate cages, with 4–6 individuals per cage. All experimental procedures were conducted in accordance with the guidelines for the care and use of laboratory animals and were approved by the Ethics Committee of Cangzhou Central Hospital (Ethics Number 2024-066-01). A total of 102 mice were used, with 12 mice per group for behavioral studies and 4–5 per group for neurophysiological experiments.
Spared nerve injury model and NaHS treatment
In this study, neuropathic pain was induced in mice through the preparation of the Spared Nerve Injury (SNI) model. In essence, anesthesia was induced in mice using 5% sevoflurane until the loss of the righting reflex was observed. Subsequently, the mice were carefully positioned in a supine posture on a surgical table equipped with a warming blanket, and anesthesia was maintained at 3% sevoflurane. The surgical site was prepared by shaving, disinfection, and draping. An incision was made along the path of the sciatic nerve, followed by blunt dissection of the skin to expose the sciatic nerve branches, including the peroneal, tibial, and sural nerves. The tibial and sural nerves were meticulously ligated using 8 − 0 nylon sutures and then cut at the distal end of the ligation, while the peroneal nerve remained intact. Subsequently, the skin was sutured, and the mice were returned to their housing cages once they had regained consciousness. In the sham surgery group, mice underwent nerve exposure without further manipulation. Prepare a NaHS solution by dissolving 5.6 mg of NaHS (Kainuo Trading Co., Ltd, Jiaxing, China) in 10 ml of physiological saline to achieve a concentration of 10 µmol/ml. Following SNI surgery, intraperitoneal injections of the NaHS solution are administered at 9:00 AM daily from day 0 to day 14, at a dosage of 100 µmol/kg based on the body weight of the mice. The control group receives intraperitoneal injections of an equivalent volume of physiological saline.
Mechanical withdrawal threshold test
Before the test, mice were placed in the behavioral testing room for 30 min beforehand to acclimate to the environment. In a quiet experimental environment with appropriate lighting, the mice to be tested were placed on a metal grid with openings. The test mice were placed on a metal mesh platform in a quiet experimental environment with appropriate lighting. Conventional von Frey filaments (0.04, 0.07, 0.16, 0.4, 0.6, 1, 1.4, 2, and 4 g) were used to assess mechanical pain thresholds. The testing began with the filament of the lowest force, progressing in ascending order. If no paw withdrawal response was observed, the response was negative even when the von Frey filament bent by more than 90°. Filaments with higher force were subsequently applied. The force of the filament that elicited a paw withdrawal response in the mouse was recorded as the mechanical withdrawal threshold.
Thermal withdrawal latency test
Before the test, mice were placed in the behavioral testing room for 30 min in advance to acclimate to the environment. Set the hot plate analgesia meter to 50 ℃ and surround the hot plate with a transparent, perforated glass cover. Place the mice on the hot plate and start the timer simultaneously. A positive response is indicated by the mouse licking its hind paws, jumping on the spot, or withdrawing its legs markedly. Immediately stop the timer upon observing any of these behaviors and record the latency of the response.
Neurophysiological electrode implantation
Microwire electrodes (Samtec16, Kodo Brain-Machine Technology Co., Ltd.) were implanted seven days before model preparation. In brief, mice were placed in a chamber pre-filled with 3% sevoflurane for anesthesia. Once the righting reflex disappeared, they were fixed in a stereotaxic instrument, with anesthesia maintained using 3% sevoflurane. The skin was disinfected with 75% alcohol, the hair on the mouse’s head was removed, and the skin was incised. Blunt dissection was used to expose the periosteum and skull. The primary somatosensory cortex of the hindlimb (S1HL), located according to the Allen Mouse Brain Atlas (S1HL, positioned at -0.5 mm anterior to Bregma, 1.5 mm lateral, 1 mm depth), was accessed using a high-speed drill for small animals. The microwire electrode was inserted into the S1 cortical area (DV = −1 mm) through the bone hole at a rate of 100 μm/min. It was then fixed with dental cement (batch number 20230301, Shanghai New Century Dental Materials Co., Ltd.). After full recovery, the mice were returned to their cages. The firing frequency of neurons in the S1HL brain region of mice was recorded on day 14 after SNI (spinal cord injury) preparation on a hot plate at 50 ℃ for 10 s. The firing frequency record is done through NeuroStudio software (Jiangsu Boen Technology Co., Ltd.). Subsequently, we analyzed the EEG data using NeuroExplorer software (Plexon Inc., USA).
Light-dark box test
The main body of the light-dark box is a rectangular acrylic box divided into two equal areas by a rectangular partition. One area has a white background with a light source on top, while the other area has a black background with no light source. The partition has a semicircular opening at the bottom, allowing mice to shuttle between the two regions freely. At the start of the experiment, the light source is turned on with a brightness of 500 lx. Mice are placed in the light area, and an infrared camera records their movements within 5 min. The exploration time in the light area is analyzed using Labmaze 3.0 software (Beijing Zhongshidichuang Science and Technology Development Co., Ltd.). After each experiment, feces are removed, the bottom is sprayed with 75% alcohol and wiped with a clean cloth to prevent the residual odor of the previous mouse from affecting the experimental results.
Forced swimming test
The forced swimming test was conducted on days 16 and 17 post-SNI preparation. 30 min before the start of the experiment, the mice were transferred to the behavioral experiment room to acclimate to the experimental environment. The forced swimming experiment was conducted in a transparent acrylic cylindrical tank filled with water at 25 ℃, with a water height of about 10 cm. On day 16, mice were placed in the water for a 15-minute swimming training session. On day 17, the test was conducted; after 30 min of acclimation to the laboratory environment, mice were placed in the water for 6 min. The last 4 min of the mice’s floating, swimming, and struggling behaviors were recorded and analyzed.
Immunofluorescence staining
After the behavioral experiments, 6 mice per group were randomly selected for immunofluorescence staining (n = 6). In brief, the mice were euthanized under deep anesthesia with 8% sevoflurane, followed by perfusion with 4 ℃ Phosphate buffered saline (PBS) and neutral polyformaldehyde. The lumbar spinal cord tissues were then exposed and isolated. After 24 h of fixation in neutral polyformaldehyde, the spinal cord tissues were dehydrated in a 30% sucrose solution. Once dehydration was complete, the tissues were cryosectioned into 40 μm thick slices. The sections were incubated in 0.5% Triton X-100 for 30 min, followed by a 30 min room temperature incubation in immunoblocking solution. Subsequently, we incubated them overnight at 4℃ with GFAP mouse monoclonal antibody (dilution 1:200, Thermo Fisher Scientific, Wuhan, China) and EAAT2 rabbit polyclonal antibody (dilution 1:200, Wanlei Bio, Shenyang, China). This was followed by adding goat anti-rabbit FITC (dilution 1:500, Beyotime, Shanghai, China) fluorescent secondary antibodies and incubating for 1 h at room temperature in the dark. Finally, the cell nuclei were stained with DAPI, and the sections were covered in a coverslip. Imaging was performed using a confocal microscope (CSIM110, Beijing Century Sunny Technology Co., Ltd., China), and quantitative analysis was conducted using Image J software.
Glutamate concentration determination
Following the completion of behavioral testing, 6 mice were randomly selected from each group to measure the spinal cord glutamate concentration (n = 6). The detection protocol strictly followed the instructions provided by the glutamate assay kit from Solarbio (Beijing, China). Essentially, under deep anesthesia with 8% sevoflurane, the mice were dissected to extract the spinal cord, and 50 mg of fresh spinal cord tissue was cut and homogenized in 1 ml of PBS at 4 °C. The homogenate was centrifuged at 10,000 g for 10 min, and the supernatant was separated and preserved. The remaining spinal cord tissue was stored at -80 °C for subsequent Western blot analysis. Following this, we prepared duplicate samples for each tissue specimen according to the manufacturer’s enzymatic reaction guidelines. Finally, the absorbance at 340 nm was measured using an ELISA reader, and the results were calculated.
Western blot
The spinal cord tissue was placed in a lysis buffer containing grinding beads and homogenized at 4 ℃, 10,000 g for 10 min (n = 6). Protein-containing supernatant was collected. The BCA technique was used to determine the protein concentration. Loading buffer was added to the protein samples, which were then heated at 95 ℃ for 5 min to denature the proteins. Gel electrophoresis was conducted with 30 µg of protein per well. After electrophoresis, proteins were transferred to a polyvinylidene fluoride (PVDF) membrane and blocked with Quickblock™ (P0252, Beyotime, Shanghai, China) for 15 min. EAAT1 rabbit polyclonal antibody (dilution 1:1000, Wanlei Bio, Shenyang, China), EAAT2 rabbit polyclonal antibody (dilution 1:1000, Wanlei Bio, Shenyang, China), and GADPH rabbit polyclonal antibody (dilution 1:1000, Wanlei Bio, Shenyang, China) were added and incubated overnight at 4 ℃. After washing 3 times with TBS-T (ST673, Beyotime, Shanghai, China), the membrane was incubated for 1 h with horseradish peroxidase-labeled goat anti-rabbit IgG (H + L) antibody (dilution 1:1000, Beyotime, Shanghai, China). Following washing, the PVDF membrane was incubated with BeyoECL Plus (Beyotime, Shanghai, China) for 5 min and visualized using a chemiluminescence imaging system (MiniChemi610, Sainsmart Technology Co., Ltd.). Analysis was performed using Image J software, with the expression level of the target protein reflected by the ratio of the target protein band grayscale value to the GADPH band grayscale value.
Statistical analysis
We performed statistical calculations using the R4.3.1 software with the ‘pwr’ package based on preliminary results from the mechanical pain threshold measurements. The sample size was determined using the pwr.anova.test function with a significance level set at 0.05, a power of 0.8, and an effect size of 0.5. This calculation indicated that 12 animals per group would be required. Results are presented as mean ± standard deviation. Shapiro-Wilk test was used to assess the normality of data. A comparison between the two groups was performed using the unpaired student t-test. In comparison, differences among four groups were analyzed using one-way Analysis of Variance, followed by Tukey’s post hoc test where applicable. Repeated measures data were analyzed using two-way Analysis of Variance. The level of significance was set at P < 0.05.
Results
SNI induces chronic pain
Prior to the preparation of the SNI model (Day 0), the mechanical pain threshold and thermal pain latency of two groups of mice were assessed to ensure that they exhibited a similar baseline pain sensation (n = 12 per group). The results demonstrated no statistically significant differences between the two groups on Day 0. Subsequently, on Days 1, 3, 7, and 14 post-model preparation, further measurements were taken of the mechanical pain threshold and thermal pain latency of the two groups of mice (Fig. 1). The findings demonstrated that compared to the Sham group, the mice that had undergone SNI exhibited a markedly diminished mechanical pain threshold and thermal pain latency at these time points. This suggests that SNI can result in long-term hyperalgesia (Fig. 2a,b). To objectively and accurately evaluate the pain induced by SNI, we conducted hot plate tests on Day 14 post-model preparation. We monitored the firing of neurons in the S1HL of the mice using implanted microelectrodes. The findings revealed that, compared to the Sham group, the firing frequency of neurons in the S1HL region of SNI mice was markedly elevated, thereby substantiating the hypothesis that SNI can induce pain sensitization (Fig. 2c,e).
SNI-induced chronic pain. (a,b) Comparative statistical graphs of mechanical pain threshold and thermal pain latency at pre-operation and 1, 3, 7, and 14 days after SNI in the two groups of mice (n = 12). *P < 0.05. (c,d) Bar graphs of representative neuron spikes in the S1HL brain region of the two groups of mice. (e) Comparison of neuron average spikes in the S1HL brain region of the two groups of mice, where each point represents the average number of spikes for 27 neurons from 4 mice in the sham group and 33 neurons from 5 mice in the SNI group. Data were expressed as mean ± SD and analyzed using two-tailed unpaired t-test.
Chronic pain leads to depressive-like behaviors
Chronic pain is often accompanied by symptoms similar to depression. To explore this, we conducted the light-dark box test on the 15th day following the preparation of the mouse model and the forced swimming test on the 16th and 17th days to observe the behavioral changes in the two groups of mice (Fig. 1). The results from the light-dark box test showed that, compared to the Sham group, there was no significant difference in the total distance traveled by the SNI group mice. Still, their exploratory behavior in the bright area was significantly reduced (Fig. 3a,c). In the forced swimming test, the floating time of the SNI group mice was significantly increased compared to the Sham group (Fig. 3d,e). These findings suggest that SNI may induce depressive-like behaviors in mice.
SNI-induced depression-like behaviors. (a–c) Representative trajectory graphs from the light-dark box test of the two groups of mice, as well as statistical results of locomotor distance and time in the lightbox. (d,e) Representative time raster plots from the forced swim test in the two groups of mice and time statistical graphs of floating duration. Data were expressed as mean ± SD and analyzed using two-tailed unpaired t-test.
SNI leads to abnormal activation of spinal astrocytes and glutamate accumulation
Glial fibrillary acidic protein (GFAP) is an intermediate filament protein primarily expressed in astrocytes of the central nervous system and is a biomarker commonly used to label reactive astrocytes. GFAP expression increases in response to central nervous system injury or disease. Using immunostaining for GFAP, we observed that SNI causes an increase in reactive astrocytes and hypertrophy of astrocyte morphology in the spinal cord (Fig. 4a,b). Under physiological conditions, about 80% of the glutamate released into the synaptic cleft is absorbed and recycled by astrocytes through transporters. Combined with our previous observation of increased neuronal discharge frequency in the S1HL brain region, this suggests a possible dysfunction in the normal functions of astrocytes. Therefore, we measured the glutamate levels in the spinal cord of the two groups of mice. The results showed that compared to the Sham group, the glutamate levels in the SNI group mice were significantly increased (Fig. 4c).
Astrocyte activation and increased glutamate levels induced by SNI in spinal cord tissue. (a) Representative spinal cord tissue samples underwent immunofluorescent staining, with GFAP labeling reactive astrocytes shown in green and DAPI labeling cell nuclei shown in blue. Scale bar = 20 μm. (b) Comparative analysis of GFAP-positive areas between the two groups of mice. (c) Comparison of glutamate levels in spinal cord tissue between the two groups of mice. Data were expressed as mean ± SD and analyzed using two-tailed unpaired t-test.
Decreased expression of EAAT2 may be an important mechanism in SNI-induced chronic pain
Glutamate transporters have five subtypes, namely EAAT1, EAAT2, EAAT3, EAAT4, and EAAT5. According to the single-cell sequencing data from the brain tissue in the alzdata.org database, we found that only EAAT1 and EAAT2 are highly expressed in astrocytes (Fig. 5a,b and Supplementary Fig. 1a–c). The accumulation of glutamate caused by astrocyte dysfunction may be related to the abnormal expression of EAAT1 and EAAT2. To assess this, we used Western Blot technology to detect the expression levels of EAAT1 and EAAT2 in two groups of mice. The results showed that compared to the Sham group, the expression of EAAT2 in the spinal cord of SNI mice was significantly reduced. In contrast, the expression level of EAAT1 did not differ significantly (Fig. 5c). These results suggest that the abnormal expression of EAAT2 may be an important pathogenic mechanism for SNI-induced chronic pain.
Aberrant EAAT2 expression may be one of the mechanisms underlying chronic pain caused by SNI. (a,b) Cellular expression profiles of EAAT1 and EAAT2 proteins in the brain. (c–e) Representative protein blots of EAAT1 and EAAT2 from the two mice groups and quantitative analysis results. Data were expressed as mean ± SD and analyzed using two-tailed unpaired t-test.
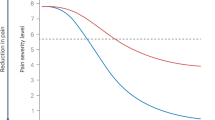
NaHS treatment alleviates SNI-induced pain hypersensitivity
Our previous research has demonstrated that NaHS can effectively alleviate neuropathic pain. Consistent with this, the results of the current study indicate that, compared to the SNI group treated with the vehicle, the SNI group treated with NaHS exhibited a significant increase in mechanical pain threshold and thermal pain latency. However, in the sham group, there was no significant difference in mechanical pain and thermal pain latency between mice treated with the vehicle and those treated with NaHS (Fig. 6a,b). The neurophysiological monitoring results from the hot plate test also showed similar outcomes: the firing frequency of S1HL neurons in the SNI group treated with NaHS was reduced compared to the SNI group treated with the vehicle. In contrast, in the sham group, there was no significant difference in the firing frequency of S1HL neurons between mice treated with the vehicle and those treated with NaHS (Fig. 6c,g). These findings suggest that NaHS has the potential to mitigate chronic pain induced by SNI.
NaHS treatment can alleviate chronic pain induced by SNI. (a,b) Comparative statistical graphs of mechanical pain threshold and thermal pain latency at pre-operation, and 1, 3, 7, and 14 days after SNI in the four groups of mice. *P < 0.05. (c–f) Representative neuron discharge histograms for the four groups of mice. (g) Comparison of the average spikes in neurons of the S1HL brain region across the four groups of mice. Each point represents the average spike count of 25 neurons from 4 mice in the Sham + V group, 33 neurons from 5 mice in the Sham + NaHS group, 27 neurons from 5 mice in the SNI + V group, and 31 neurons from 5 mice in the SNI + NaHS group. Data were expressed as mean ± SD and analyzed by ANOVA with a Tukey post hoc test.
NaHS treatment alleviates depression-like behavior
We further investigated the behavioral effects of NaHS. The results from the light-dark box test indicated that, compared to the control group treated with vehicle after spinal nerve injury (SNI), SNI mice treated with NaHS exhibited a significant increase in the time spent exploring the bright area. However, in the sham group, there was no significant difference in the time spent exploring the bright area between mice treated with vehicle and those treated with NaHS (Fig. 7a,c). The forced swimming test results showed that, compared to the control group treated with vehicle after SNI, the floating time of SNI mice treated with NaHS was significantly reduced. Similarly, there was no significant difference in the sham group’s floating time between mice treated with vehicle and those treated with NaHS (Fig. 7d,e). These findings suggest that NaHS has the potential to alleviate depressive-like behaviors induced by SNI.
NaHS treatment can alleviate depression-like behaviors induced by SNI. (a) Trajectory plots of the light-dark box test for the four groups of mice. (b) Comparison of locomotor distance among the four groups of mice. (c) Comparison of time spent in the light box by the four groups of mice. (d) Time grid of the force swim test for the four groups of mice. (e) Comparison of floating duration among the four groups of mice. Data were expressed as mean ± SD and analyzed by ANOVA with a Tukey post hoc test.
The potential link between the protective effect of NaHS and enhanced EAAT2 expression
To further clarify the mechanism by which NaHS improves neuropathic pain, we utilized immunofluorescence techniques to evaluate the effects of NaHS treatment. The results showed that the NaHS treatment significantly increased the expression of EAAT2 in astrocytes. (Figure 8a,b). This suggests that NaHS can dramatically improve the reactive astrocytes induced by SNI. We further measured the levels of glutamate in spinal cord tissues to assess whether NaHS improved the glutamate transport function of astrocytes (Fig. 8c). The results indicated that, compared to the SNI + Vehicle group, the glutamate levels in the SNI + NaHS group significantly decreased. Subsequently, we used Western blot technology to assess the effect of NaHS treatment on EAAT2. The results showed that, compared to the SNI + Vehicle group, EAAT2 expression in the SNI + NaHS group mice significantly increased (Fig. 8d,e). In summary, NaHS treatment alleviates central sensitization and depression-like behavior by increasing the expression of EAAT2 in astrocytes, thereby enhancing the glutamate transport function of astrocytes.
The mechanism of NaHS alleviating neuropathic pain may be associated with inhibition of astrocyte activation and increased expression of EAAT2. (a) Representative immunofluorescent staining of spinal cord tissue in four groups of mice, with GFAP labeling astrocytes displayed in red, EAAT2 in green and DAPI marking cell nuclei in blue. Scale bar = 20 μm. (b) Comparative analysis of EAA2 occupancy in GFAP-positive area from the four groups of mice. (c) Comparison of glutamate levels in spinal cord tissue among the four groups of mice. (d, e) Representative protein blots of EAAT2 from the four mice groups and quantitative analysis results. Data were expressed as mean ± SD and analyzed by ANOVA with a Tukey post hoc test.
Discussion
This study provides compelling evidence that reactive astrocytes contribute to the chronic neuropathic pain caused by SNI. A novel finding of this study is that reactive astrocytes lead to decreased expression of EAAT2, resulting in the accumulation of the excitatory neurotransmitter glutamate and an increase in neuronal discharge in the S1HL. The study also discovered that using the H2S donor NaHS can effectively improve chronic neuropathic pain, and its protective effect is associated with the improvement of reactive astrocytes and an increase in EAAT2 expression. Therefore, this study demonstrates that H2S could be a potent treatment method with tremendous potential for relieving chronic neuropathic pain (Fig. 9).
Overactivation of astrocytes may be a crucial mechanism in neuropathic pain, resulting in reduced EAAT2 expression. We induced neuropathic pain through spared nerve injury and detected overactivation of astrocytes in spinal cord tissues. This was accompanied by a reduction in EAAT2 expression, accumulation of glutamate, and, from a neurophysiological perspective, an increase in neuronal firing activity in the S1HL brain region.
SNI is a commonly used experimental model to study chronic neuropathic pain26,27,28. In this study, chronic neuropathic pain was induced by ligating and transecting the proximal end of the tibial and common peroneal nerves, and pain conditions were assessed using mechanical pain thresholds and hot plate escape latency. The results showed that this model could stably maintain a pain phenotype up to 14 days post-SNI, consistent with the study of Zhang G29. Recent reports have highlighted potential differences in pain sensitivity between male and female animals, particularly in non-neuronal components of neuropathic pain30. While this issue warrants further exploration, we chose to use male animals in this study due to challenges in controlling for hormonal cycle variations when using female mice. These hormonal fluctuations can introduce biases in behavioral assessments, which may affect the consistency of the results. Therefore, we selected male mice to avoid these confounding factors. In vivo, neurophysiological techniques were used to collect the discharge conditions of neurons in the S1HL brain area 14 days post-SNI to evaluate the pain condition more objectively. The results showed that SNI significantly increased the discharge frequency, consistent with the study of Jin Y31. Multiple studies have pointed out that chronic pain not only affects the physical state of patients but can also lead to psychological and emotional problems, especially depression32,33,34. In this study, light-dark box tests and forced swimming tests were conducted post-SNI to assess levels of depression in mice. The results showed that in the light-dark box test, SNI led to a significant reduction in exploration time in the light area and total exploration distance; in the forced swimming test, it significantly increased floating time in mice. This suggests that SNI not only causes chronic pain but also leads to depression-like behavior in mice.
Astrocytes undergo a series of reactive changes during chronic neuropathic pain known as astrocyte activation. One of the markers of astrocyte activation is an increase in the expression of GFAP. The immunofluorescence results of this study showed the same result, with a significant increase in GFAP staining area in the SNI group mice. GFAP is a specific intermediate filament protein of astrocytes, and its increased expression level typically indicates morphological and functional changes in astrocytes. Activated astrocytes become more extensive in volume, branched, and may undergo transcriptional changes, affecting surrounding neurons and other glial cells35. Our previous results showed a significant increase in spikes in neurons of the S1HL brain region, which is usually associated with elevated levels of the excitatory neurotransmitter glutamate. Our study confirmed this. To explore the reason for the increased glutamate levels, we looked into glutamate transporters and found that only EAAT1 and EAAT2 proteins are highly expressed in astrocytes among the five transporters. We quantitatively analyzed the expression levels of EAAT1 and EAAT2 proteins using Western Blot technology. The study results showed that SNI could cause a significant reduction in the expression of the glutamate transporter protein EAAT2 but not EAAT1, which is consistent with the research of Nicholson KJ36.
H2S as an emerging biological signaling molecule is gradually recognized for its potential in the medical field. Numerous studies have shown a complex relationship between H2S and neuropathic pain. Research indicates that cystathionine gamma-lyase can promote visceral pain by targeting Cav3.2 T-type Ca2+ channels (T channels) and transient receptor potential ankyrin-137. However, many studies confirm that exogenous H2S can produce anti-inflammatory effects, alleviating neuropathic pain. Our preliminary results also confirm that H2S alleviates neuropathic pain by regulating neuronal excitability through Nrf238. These results highlight the characteristic bell-shaped biphasic effect of H2S. Our study shows that the exogenous use of the H2S donor NaHS can significantly increase the mechanical pain threshold and thermal pain escape latency in SNI mice. Our results show that NaHS significantly reduces the spinal cord’s glutamate content and neurons’ discharge frequency in the S1HL brain area. In the central nervous system, H2S can regulate astrocyte function. Li X et al. found that LPS promotes the proliferation of A1 astrocytes in mouse hippocampal tissue induced by cerebral ischemia-reperfusion, which can be inhibited by the H2S donor NaHS39; research by Kimura Y et al. suggests that H2S can induce Ca2+ influx into astrocytes40. The study by Opere CA et al. suggests that H2S donors can inhibit glutamatergic neurotransmission in isolated bovine and porcine retinas, but the precise regulatory mechanisms remain unclear41. Our study similarly confirms that H2S can alleviate the increase in reactive astrocytes caused by SNI. We also innovatively found that H2S can increase the expression of EAAT2, which may be the reason for the reduction of glutamate accumulation in the spinal cord. Although our innovative findings show that H2S can improve the increase in reactive astrocytes caused by SNI and regulate the expression of EAAT2, the specific mechanism by which H2S regulates astrocytes is unclear. Chronic pain is often comorbid with depression. Research by Lv XJ et al. demonstrated that astrocyte activation in the ventral hippocampus can promote depressive-like behaviors in chronic pain mouse models42. This study highlights the significant role of astrocytes in the interplay between chronic pain and mood disorders. Our findings further show that H2S exhibits great potential in reducing depressive-like behaviors in animal models, possibly related to its effects on astrocyte function.
Current research has developed several H2S donors, such as hydrogen sulfide precursors and H2S-releasing compounds, which allow for the controlled release of H2S in the body. These donors provide better control over the release of H2S, reducing the risks associated with direct gas inhalation. Developing safer and more efficient H2S donors will be crucial for advancing its clinical application. Compared to existing treatments for neuropathic pain, particularly those targeting glial cell function, H2S-based therapies offer a novel approach. However, their therapeutic potential still requires careful optimization of delivery methods and dosage to ensure both safety and efficacy.
However, this study is still limited in terms of breadth and depth. It has been shown that intrathecal injection of NaHS can induce transient hyperalgesia43. Whether the intraperitoneal injection method used in this study affects pain sensitivity remains unknown. Further exploration will be conducted in future experiments to investigate this. The survey by Miraei et al. shows that SNI leads to an initial upregulation and subsequent downregulation of EAAT2 expression. At the same time, the research by Li M indicates that GluT downregulation typically precedes or co-occurs with the onset of pain hypersensitivity44. Therefore, an optimal timing for NaHS treatment might offer improved efficacy. However, this study only investigated one-time points for NaHS administration, and further research will explore more suitable treatment windows.
In summary, this study highlights the therapeutic potential of H2S as a medical agent for neuropathic pain. Using the H2S donor, NaHS, demonstrates its efficacy in alleviating neuropathic pain by regulating reactive astrocyte function and enhancing EAAT2 expression. These findings provide valuable insights into the underlying mechanisms and open new avenues for developing clinical treatment strategies targeting neuropathic pain. Future research should focus on elucidating the precise molecular pathways through which H2S modulates astrocyte activity and exploring its broader applications in other neurological disorders associated with astrocyte dysfunction.
Data availability
The data that support the findings of this study are within the manuscript and its Additional files, and more data can be obtained from the corresponding author upon reasonable request.
References
Cohen, S. P., Vase, L. & Hooten, W. M. Chronic pain: an update on burden, best practices, and new advances. Lancet 397, 2082–2097. https://doi.org/10.1016/S0140-6736(21)00393-7 (2021).
Hartvigsen, J. et al. What low back pain is and why we need to pay attention. Lancet 391, 2356–2367. https://doi.org/10.1016/S0140-6736(18)30480-X (2018).
Ho, E. K. et al. Psychological interventions for chronic, non-specific low back pain: systematic review with network meta-analysis. BMJ 376, e067718. https://doi.org/10.1136/bmj-2021-067718 (2022).
Monticone, M. et al. Cognitive-behavioural treatment for subacute and chronic neck pain. Cochrane Database Syst. Rev. CD010664 https://doi.org/10.1002/14651858.CD010664.pub2 (2015).
Malfliet, A. et al. Brain changes associated with cognitive and emotional factors in chronic pain: a systematic review. Eur. J. Pain 21, 769–786. https://doi.org/10.1002/ejp.1003 (2017).
Arango-Davila, C. A. & Rincon-Hoyos, H. G. Depressive disorder, anxiety disorder and Chronic Pain: multiple manifestations of a common clinical and Pathophysiological Core. Rev. Colomb Psiquiatr. (Engl. Ed.) 47, 46–55. https://doi.org/10.1016/j.rcp.2016.10.007 (2018).
Backryd, E. & Alfoldi, P. Chronic pain and its relationship with anxiety and depression. Lakartidningen 120, 23010 (2023).
Kohrt, B. A., Griffith, J. L. & Patel, V. Chronic pain and mental health: integrated solutions for global problems. Pain 159 (1), S85–S90. https://doi.org/10.1097/j.pain.0000000000001296 (2018).
Fisher, L. E. & Lempka, S. F. Neurotechnology for pain. Annu. Rev. Biomed. Eng. 25, 387–412. https://doi.org/10.1146/annurev-bioeng-111022-121637 (2023).
McCracken, L. M., Yu, L. & Vowles, K. E. New generation psychological treatments in chronic pain. BMJ 376, e057212. https://doi.org/10.1136/bmj-2021-057212 (2022).
Kuner, R. & Flor, H. Structural plasticity and reorganisation in chronic pain. Nat. Rev. Neurosci. 18, 20–30. https://doi.org/10.1038/nrn.2016.162 (2016).
Ji, R. R., Nackley, A., Huh, Y., Terrando, N. & Maixner, W. Neuroinflammation and central sensitization in chronic and widespread pain. Anesthesiology 129, 343–366. https://doi.org/10.1097/ALN.0000000000002130 (2018).
Bliss, T. V., Collingridge, G. L., Kaang, B. K. & Zhuo, M. Synaptic plasticity in the anterior cingulate cortex in acute and chronic pain. Nat. Rev. Neurosci. 17, 485–496. https://doi.org/10.1038/nrn.2016.68 (2016).
Rangel-Galván, M., Rangel-Galván, V. & Rangel-Huerta, A. T-type calcium channel modulation by hydrogen sulfide in neuropathic pain conditions. Front. Pharmacol. 14, 1212800. https://doi.org/10.3389/fphar.2023.1212800 (2023).
Cirino, G., Szabo, C. & Papapetropoulos, A. Physiological roles of hydrogen sulfide in mammalian cells, tissues, and organs. Physiol. Rev. 103, 31–276. https://doi.org/10.1152/physrev.00028.2021 (2023).
Gui, Y. et al. Endogenous CBS-H2S pathway contributes to the development of CCI-induced neuropathic pain. Neurochem. Res. 41, 1381–1389. https://doi.org/10.1007/s11064-016-1842-z (2016).
Shayea, A. M. F. et al. Chronic treatment with hydrogen sulfide donor GYY4137 mitigates microglial and astrocyte activation in the spinal cord of streptozotocin-induced diabetic rats. J. Neuropathol. Exp. Neurol. 79, 1320–1343. https://doi.org/10.1093/jnen/nlaa127 (2020).
Zhou, B., Zuo, Y. X. & Jiang, R. T. Astrocyte morphology: diversity, plasticity, and role in neurological diseases. CNS Neurosci. Ther. 25, 665–673. https://doi.org/10.1111/cns.13123 (2019).
Blanco-Suarez, E., Caldwell, A. L. & Allen, N. J. Role of astrocyte-synapse interactions in CNS disorders. J. Physiol. 595, 1903–1916. https://doi.org/10.1113/JP270988 (2017).
Simard, M. & Nedergaard, M. The neurobiology of glia in the context of water and ion homeostasis. Neuroscience 129, 877–896. https://doi.org/10.1016/j.neuroscience.2004.09.053 (2004).
Nedergaard, M. & Verkhratsky, A. Artifact versus reality–how astrocytes contribute to synaptic events. Glia 60, 1013–1023. https://doi.org/10.1002/glia.22288 (2012).
Verkhratsky, A. et al. Neurological diseases as primary gliopathies: a reassessment of neurocentrism. ASN Neuro 4 https://doi.org/10.1042/AN20120010 (2012).
Djukic, B., Casper, K. B., Philpot, B. D., Chin, L. S. & McCarthy, K. D. Conditional knock-out of Kir4.1 leads to glial membrane depolarization, inhibition of potassium and glutamate uptake, and enhanced short-term synaptic potentiation. J. Neurosci. 27, 11354–11365. https://doi.org/10.1523/JNEUROSCI.0723-07.2007 (2007).
Cui, Y. et al. Astroglial Kir4.1 in the lateral habenula drives neuronal bursts in depression. Nature 554, 323–327. https://doi.org/10.1038/nature25752 (2018).
Takeda, I. et al. Controlled activation of cortical astrocytes modulates neuropathic pain-like behaviour. Nat. Commun. 13, 4100. https://doi.org/10.1038/s41467-022-31773-8 (2022).
Baron, R., Binder, A. & Wasner, G. Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatm ent. Lancet Neurol. 9, 807–819. https://doi.org/10.1016/S1474-4422(10)70143-5 (2010).
Guida, F. et al. Behavioral, biochemical and electrophysiological changes in spared ner ve injury model of neuropathic pain. Int. J. Mol. Sci. 21, 3396. https://doi.org/10.3390/ijms21093396 (2020).
Jang, J. H. et al. Acupuncture alleviates chronic pain and comorbid conditions in a mouse model of neuropathic pain: the involvement of DNA methylation in the prefrontal cortex. Pain 162, 514–530. https://doi.org/10.1097/j.pain.0000000000002031 (2021).
Zhang, G. et al. Antinociceptive effect of isoorientin against neuropathic pain induced by the chronic constriction injury of the sciatic nerve in mice. Int. Immunopharmacol. 75, 105753. https://doi.org/10.1016/j.intimp.2019.105753 (2019).
Coraggio, V. et al. Neuroimmune-driven neuropathic pain establishment: a focus on gender differences. Int. J. Mol. Sci. 19. https://doi.org/10.3390/ijms19010281 (2018).
Jin, Y. et al. Thalamocortical circuits drive remifentanil-induced postoperative hype ralgesia. J. Clin. Invest. 132. https://doi.org/10.1172/jci158742 (2022).
Yamauchi, N. et al. Chronic pain-induced neuronal plasticity in the bed nucleus of the str ia terminalis causes maladaptive anxiety. Sci. Adv. 8, eabj5586. https://doi.org/10.1126/sciadv.abj5586 (2022).
Kerckhove, N. et al. Ethosuximide improves chronic pain-induced anxiety- and depression-lik e behaviors. Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 29, 1419–1432. https://doi.org/10.1016/j.euroneuro.2019.10.012 (2019).
Mullins, P. M., Yong, R. J. & Bhattacharyya, N. Associations between chronic pain, anxiety, and depression among adult s in the United States. Pain Pract. 23, 589–594. https://doi.org/10.1111/papr.13220 (2023).
Wang, X. et al. Activation of astrocyte gq pathway in hippocampal CA1 region attenuate s anesthesia/surgery induced cognitive dysfunction in aged mice. Front. Aging Neurosci. 14, 1040569. https://doi.org/10.3389/fnagi.2022.1040569 (2022).
Nicholson, K. J., Gilliland, T. M. & Winkelstein, B. A. Upregulation of GLT-1 by treatment with ceftriaxone alleviates radicul ar pain by reducing spinal astrocyte activation and neuronal hyperexci tability. J. Neurosci. Res. 92, 116–129. https://doi.org/10.1002/jnr.23295 (2014).
Terada, Y. & Kawabata, A. H2S and Pain: a novel aspect for Processing of somatic, visceral and neuropathic Pain signals. Handb. Exp. Pharmacol. 230, 217–230. https://doi.org/10.1007/978-3-319-18144-8_11 (2015).
Wang, J. et al. H2S alleviates neuropathic pain in mice by Nrf2 signaling pathway acti vation. J. Mol. Neurosci. 73, 456–468. https://doi.org/10.1007/s12031-023-02134-x (2023).
Li, X., Yin, X., Pang, J., Chen, Z. & Wen, J. Hydrogen sulfide inhibits lipopolysaccharide-based neuroinflammation-induced astrocyte polarization after cerebral ischemia/reperfusion injury. Eur. J. Pharmacol. 949, 175743. https://doi.org/10.1016/j.ejphar.2023.175743 (2023).
Kimura, H., Nagai, Y., Umemura, K. & Kimura, Y. Physiological roles of hydrogen sulfide: synaptic modulation, neuropro tection, and smooth muscle relaxation. Antioxid. Redox. Signal. 7, 795–803. https://doi.org/10.1089/ars.2005.7.795 (2005).
Njie-Mbye, Y. F., Opere, C. A., Chitnis, M. & Ohia, S. E. Hydrogen sulfide: role in ion channel and transporter modulation in the eye. Front. Physiol. 3, 295. https://doi.org/10.3389/fphys.2012.00295 (2012).
Lv, X. J. et al. Glia-derived adenosine in the ventral hippocampus drives pain-related anxiodepression in a mouse model resembling trigeminal neuralgia. Brain Behav. Immun. 117, 224–241. https://doi.org/10.1016/j.bbi.2024.01.012 (2024).
Zhao, S. et al. Upregulation of spinal NMDA receptors mediates hydrogen sulfide-induced hyperalgesia. J. Neurol. Sci. 363, 176–181. https://doi.org/10.1016/j.jns.2016.02.058 (2016).
Li, M. & Yang, G. A mesocortical glutamatergic pathway modulates neuropathic pain independent of dopamine co-release. Nat. Commun. 15, 643. https://doi.org/10.1038/s41467-024-45035-2 (2024).
Funding
Cangzhou Science and Technology Key R&D Plan Project (Grant No. 213106089).
Author information
Authors and Affiliations
Contributions
Xu-Peng Wang was responsible for the design of the study. Man-Man Qi and Heng-Yue Peng were responsible for the data collection, statistical analysis, and the experiments. Tian-Ge Zhang and Yan Li were responsible for the experiments. Meng-Ya Gao and Wen-Bo Sun confirmed the authenticity of all raw data. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All experiments were approved by the Ethics Committee of Cangzhou Central Hospital under the registration number 2024-066-01. The study was conducted and reported in compliance with the ARRIVE guidelines (https://arriveguidelines.org), ensuring transparent and detailed reporting of all in vivo experiments.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qi, MM., Peng, HY., Zhang, TG. et al. NaHS modulates astrocytic EAAT2 expression to impact SNI-induced neuropathic pain and depressive-like behaviors. Sci Rep 15, 2874 (2025). https://doi.org/10.1038/s41598-025-86885-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-86885-0
Keywords
This article is cited by
-
An Enigma of Brain Gasotransmitters: Hydrogen Sulfide and Depression
NeuroMolecular Medicine (2025)