Abstract
This study investigated the relationship between the frailty index and all-cause and cause-specific mortality in patients with depression. We recruited 2,669 participants with depression from the National Health and Nutrition Examination Survey (NHANES) from 2005 to 2018 and quantified their frailty status using a 53-item frailty index. Cox proportional hazards models were used to estimate hazard ratios (HR) and their 95% confidence intervals (CI). The median (IQR) frailty score was 0.3 (0.2, 0.4). During a median follow-up of 7.1 years, 342 all-cause deaths (including 85 cardiovascular deaths and 70 cancer deaths) were recorded. Compared to the lowest frailty index tertile, the adjusted HR (95% CI) for all-cause mortality in the highest tertile was 2.91 (1.97, 4.3), for cardiovascular mortality was 3.13 (1.37, 7.19), and for cancer mortality was 2.3 (1.05, 5.03). Each unit increase in the frailty index (log-transformed) was associated with a 241% increase in all-cause mortality (P < 0.001), a 233% increase in cardiovascular mortality (P < 0.001), and a 185% increase in cancer mortality (P < 0.001). These results were consistent across analyses stratified by age, gender, race, BMI, hypertension, and diabetes. This study suggests that the frailty index is positively associated with all-cause and cause-specific mortality in patients with depression. The frailty index could serve as a prognostic indicator, and frailty interventions should be an important part of managing patients with depression.
Similar content being viewed by others
Introduction
Depression is a common and serious mental disorder affecting millions of people worldwide. It impacts not only an individual’s mood and behavior but also has extensive negative effects on physical health1. Depressed patients often experience sleep disturbances, changes in appetite, weight fluctuations, and fatigue, which can further lead to decreased quality of life and functional impairment2. Additionally, depression is closely associated with various chronic diseases (such as cardiovascular disease, diabetes, and obesity), increasing the overall disease burden and mortality risk for patients3. Although numerous studies have shown an association between depression and higher mortality rates, the specific mechanisms remain unclear and require further exploration.
Frailty is an age-related syndrome characterized by a decline in multiple physiological systems, leading to increased vulnerability to external stressors4. Frailty is not limited to the elderly; it can also occur in middle-aged individuals with chronic diseases or functional impairments. The frailty status is typically quantified through a comprehensive assessment of various health indicators, including cognitive function, daily activity capability, comorbidities, physical performance, and laboratory results. The frailty index, as a multidimensional health status assessment tool, can reflect an individual’s overall health status and susceptibility to multiple diseases5. In recent years, frailty has gained widespread attention in clinical and research fields as an independent prognostic indicator.
In 2015, Almeida et al. found that current depressive symptoms significantly increased mortality rates among older men over 75 years old in Australia, with this association primarily explained by frailty6. In 2021, Arts et al. showed that frailty is an important predictor of mortality in late-life depression patients in the Netherlands, with higher frailty levels associated with higher mortality risks7. These studies emphasize the importance of addressing frailty in the management of depression in the elderly. However, few studies have focused on the relationship between the frailty index and mortality risk in depressed adults in the United States, leaving this area underexplored. Therefore, we conducted this cohort study to investigate the relationship between the frailty index and all-cause and cause-specific mortality in patients with depression. By systematically analyzing data from the National Health and Nutrition Examination Survey (NHANES) from 2005 to 2018, we aim to reveal the impact of the frailty index on the prognosis of depressed adults in the U.S. and provide valuable references for clinical practice.
Methods
Study population and data collection
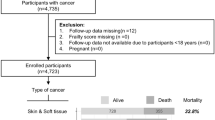
This study is a retrospective cohort study utilizing data from the NHANES. NHANES is a nationally representative survey conducted by the National Center for Health Statistics (NCHS). Since the PHQ-9 score was used as the diagnostic standard for depression in this study and was only available in the NHANES cycles from 2005 to 2018, data for this study were sourced from these cycles. The NHANES study protocol was approved by the NCHS Research Ethics Review Board, and participants provided written informed consent at enrollment. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines. Participants included in this study met the following criteria: a PHQ-9 score ≥ 10, indicating the presence of depression; exclusion criteria were loss to follow-up, missing frailty index data, missing covariate data, and pregnancy. Ultimately, 2,669 participants with depression were included in the analysis. (Fig. 1)
Measurement of frailty index
The frailty index model was calculated based on the standard procedure developed by Searle et al., which aggregates deficits from multiple systems. In this study, we used a model including 53 deficits across seven systems, assigning values between 0 and 1 based on the severity of the deficits. The seven systems included:1. Cognition: One question on whether the individual has confusion and memory problems.2. Dependency: 20 questions on difficulties with daily living activities.3. Depressive Symptoms: Seven questions based on the Patient Health Questionnaire (PHQ-9)0.4. Comorbidities: 13 items, involving self-reported arthritis, thyroid problems, chronic bronchitis, malignancies, heart failure, coronary heart disease, angina, hypertension, heart attack, stroke, diabetes, renal failure, and urinary incontinence.5. Hospital Utilization and Healthcare Access: Five questions on general health status, current health status compared to a year ago, overnight hospital stays in the past year, frequency of healthcare use in the past year, and number of prescription medications.6. Physical Performance and Anthropometry: One item on body mass index.7. Laboratory Values: Six items, involving HbA1c, red blood cell count, hemoglobin, red cell distribution width, lymphocyte percentage, and segmented neutrophil percentage. The frailty index was expressed as the ratio of accumulated deficits to the total number of deficits8.
Mortality outcomes
The survival status of participants was determined using the NHANES public use linked mortality file. Follow-up mortality was only assessed until December 2019 because the NHANES National Death Index is updated every four years, and the latest released follow-up data is up to December 31, 2019. Specific causes of death were defined using the International Classification of Diseases, 10th Revision (ICD-10). We examined all-cause mortality and cause-specific mortality, including cardiovascular disease (ICD-10: I00-I09, I11, I13, I20-I51) and malignant neoplasms (ICD-10: C00-C97). The baseline NHANES data collection served as the starting point for calculating survival time.
Covariates
Age, gender, Body Mass Index (BMI), race, marital status, educational level, poverty income ratio (PIR), smoking status, alcohol consumption, total physical activity time, hypertension, and diabetes were obtained from home interviews. Specific definitions were as follows: age as a continuous variable, recording the actual age of participants; gender as recorded; race/ethnicity categorized as non-Hispanic white, non-Hispanic black, Mexican American, other Hispanic, and other races; marital status categorized as married, unmarried, cohabitating, and others (including widowed, divorced, or separated); BMI as a continuous variable, calculated based on the participant’s height and weight; poverty income ratio categorized as 1-1.3, 1.31–3.50, and > 3.50; educational level categorized as less than high school, high school or equivalent, and more than high school; smoking status categorized as never smoked (smoked less than 100 cigarettes in a lifetime), former smoker (smoked more than 100 cigarettes but not currently smoking), and current smoker (smoked more than 100 cigarettes and currently smoking sometimes or every day);9 alcohol consumption categorized as never drinkers (less than 12 drinks in a lifetime), former drinkers (drank at least 12 times a year but not in the past year, or did not drink in the past year but drank at least 12 times in a lifetime), and current drinkers, further categorized into current heavy drinkers (women drinking at least 3 drinks a day, men drinking at least 4 drinks a day, or binge drinking at least 5 days a month), current moderate drinkers (women drinking at least 2 drinks a day, men drinking at least 3 drinks a day, or binge drinking at least 2 days a month), and current light drinkers (women drinking no more than 1 drink a day, men drinking no more than 2 drinks a day);10 total physical activity time as a continuous variable, indicating the time spent on activities such as walking, cycling, working, and recreational activities in a week;11 hypertension determined by average systolic BP ≥ 140 mmHg and/or diastolic BP ≥ 90 mmHg, self-reported diagnosis, or use of antihypertensive medications; diabetes determined by a physician diagnosis, HbA1c level ≥ 6.5%, fasting glucose level ≥ 7.0 mmol/L, random/2-hour OGTT glucose level ≥ 11.1 mmol/L, or use of diabetes medications/insulin; hyperlipidemia defined as meeting any one of the following: (1) use of lipid-lowering medications; (2) triglyceride level ≥ 150 mg/dL; (3) high cholesterol (total cholesterol ≥ 200 mg/dL, or LDL ≥ 130 mg/dL, or HDL < 40 mg/dL).
Statistical analysis
All analyses were performed using R statistical software (http://www.R-project.org, The R Foundation) and Free Statistics software version 1.7. Two-sided P values below 0.05 were considered statistically significant. Categorical variables were represented by proportions (%) while continuous variables were described by the mean (standard deviation, SD) or median (interquartile range, IQR), as appropriate. The frailty index was input as both a categorical variable (tertiles) and a continuous variable (log-transformed). To compare the differences across groups, one-way analyses of variance (normal distribution), Kruskal–Wallis tests (skewed distribution), and chi-square tests (categorical variables) were undertaken. Kaplan-Meier survival analysis and Cox proportional hazards models were used to evaluate the association between the frailty index and all-cause and cause-specific mortality. Three statistical models were fitted. Model 1: adjusted for age (continuous variable), race (non-Hispanic white, non-Hispanic black, Mexican American, other Hispanic, and other races), and gender (male or female). Model 2: further adjusted for marital status (married, unmarried, cohabiting, and others), BMI (continuous variable), poverty income ratio (PIR) (1-1.3, 1.31–3.50, and > 3.50), educational level (less than high school, high school or equivalent, and more than high school), smoking status (never smoked, former smoker, and current smoker), total physical activity time (continuous variable), and alcohol consumption (never drinker, former drinker, and current drinker). Model 3: further adjusted for diabetes (no or yes), hyperlipidemia (no or yes), and hypertension (no or yes).
Restricted cubic spline models were used to estimate and visualize the dose-response relationship between the frailty index and the risks of all-cause and cause-specific mortality. Stratified analyses were conducted by age (< 65 years, ≥ 65 years), gender (male, female), race (white, others), BMI (< 30, ≥ 30 kg/m2), hypertension, and diabetes status. The P value for the interaction term between the frailty score and stratified variables was used to test the significance of the interaction. To test the robustness of the results, the following sensitivity analyses were performed: (1) Excluding participants with a history of cardiovascular disease at baseline. (2) Excluding participants with a history of cancer at baseline. (3) Using multiple imputation methods to handle missing data. Additionally, we introduced the Fine-Gray sub-distribution hazard model in the sensitivity analyses to evaluate sub-hazard ratios (SHR) in the presence of competing risks. These analyses validated the main results’ robustness and reliability by refitting the models of the frailty index and mortality risk.
Results
Baseline characteristics
In Table 1, A total of 2,669 participants with depression were included in the study and divided into three groups based on the frailty index: Tertile 1 (0.089–0.236), Tertile 2 (0.236–0.343), and Tertile 3 (0.343–0.743). Baseline characteristics showed that participants with a higher frailty index (Tertile 3) were more likely to be female, older, have a higher BMI, have hypertension and diabetes, and have less total physical activity time (all P values < 0.001).
Follow-up results
During a median follow-up of 7.1 years, 342 all-cause deaths (12.8%), including 85 cardiovascular deaths (3.18%) and 70 cancer deaths (2.62%), were recorded. The all-cause mortality rates in Tertile 1, Tertile 2, and Tertile 3 were 3.8%, 11.1%, and 23.5%, respectively; the cardiovascular mortality rates were 0.8%, 2.7%, and 6.1%; and the cancer mortality rates were 1.0%, 2.1%, and 4.7%.
Survival analysis
In Fig. 2, Kaplan-Meier survival analysis showed significant differences in all-cause mortality, cardiovascular mortality, and cancer mortality among different frailty index tertiles (log-rank test, all P values < 0.001). In Table 2, Further multivariate Cox regression model results were as follows: (1) All-cause mortality: compared to Tertile 1, the adjusted HR (95% CI) for Tertile 2 was 1.88 (1.26–2.81), and for Tertile 3 was 2.91 (1.97–4.3), P-trend < 0.001. (2) Cardiovascular mortality: compared to Tertile 1, the adjusted HR (95% CI) for Tertile 2 was 2.16 (0.92–5.10), and for Tertile 3 was 3.13 (1.37–7.19), P = 0.004. (3) Cancer mortality: compared to Tertile 1, the adjusted HR (95% CI) for Tertile 2 was 1.38 (0.61–3.13), and for Tertile 3 was 2.30 (1.05–5.03), P = 0.018. Each unit increase in the frailty index (log-transformed) was associated with a 241% increase in all-cause mortality (P < 0.001), a 233% increase in cardiovascular mortality (P < 0.001), and a 185% increase in cancer mortality (P < 0.001).
Spline analysis and stratified analysis
As shown in Fig. 3, the spline analysis revealed a significant dose-response relationship between the frailty index and the risks of all-cause mortality, cardiovascular mortality, and cancer mortality. Increased frailty index was positively associated with the increased risk of all three types of mortality. Further stratified analysis showed that the positive association between the frailty index and mortality risk was consistent across different subgroups, including age, gender, race, BMI, hypertension, and diabetes status (Fig. 4).
The dose‒response association of the frailty score with all-cause mortality (A), CVD mortality (B), and cancer mortality (C) among participants with depression. This spline model was adjusted for age, race, and gender, marital status, BMI, PIR group, educational level, smoking status, PA total time, alcohol intake, diabetes, hyperlipidemia, and hypertension. CVD cardiovascular disease.
Subgroup analyses of the association of the frailty score with all-cause mortality among participants with depression. HR (95% CI) was assessed by the Cox proportional hazards model. The model was adjusted for age, race, and gender, marital status, BMI, PIR group, educational level, smoking status, PA total time, alcohol intake, diabetes, hyperlipidemia, and hypertension.
Sensitivity analysis
In Table 3, to verify the robustness of our main findings, we conducted several sensitivity analyses, all based on data from the multivariable Cox regression model (Model 3). (1) Excluding participants with a history of cardiovascular disease at baseline: compared to Tertile 1, the adjusted HR (95% CI) for Tertile 2 was 1.94 (1.26–2.99), and for Tertile 3 was 2.65 (1.70–4.12), P-trend < 0.001. Each unit increase in the frailty index (log-transformed) was associated with a 184% increase in all-cause mortality (P < 0.001). (2) Excluding participants with a history of cancer at baseline: compared to Tertile 1, the adjusted HR (95% CI) for Tertile 2 was 1.79 (1.16–2.76), and for Tertile 3 was 2.59 (1.69–3.97), P-trend < 0.001. Each unit increase in the frailty index (log-transformed) was associated with a 211% increase in all-cause mortality (P < 0.001). (3) Multiple imputation for missing data: compared to Tertile 1, the adjusted HR (95% CI) for Tertile 2 was 1.74 (1.17–2.59), and for Tertile 3 was 2.62 (1.77–3.87), P-trend < 0.001. Each unit increase in the frailty index (log-transformed) was associated with a 185% increase in all-cause mortality (P < 0.001). As shown in Table Supplement 1, for CVD mortality, the SHR (95% CI) for Tertile 3 was 2.56 (1.13–5.79), with a P-trend of 0.024. For cancer mortality, the SHR (95% CI) for Tertile 3 was 2.33 (1.02–5.32), with a P-trend of 0.028.
Discussion
This study found a significant positive association between the frailty index and all-cause and cause-specific mortality in patients with depression. Specifically, a higher frailty index was significantly associated with increased risks of all-cause mortality, cardiovascular mortality, and cancer mortality. This finding supports the potential of the frailty index as a prognostic tool in patients with depression, suggesting that clinical interventions should consider frailty status.
First, our results are consistent with previous studies on frailty and mortality. Arts et al. found that frailty is a significant predictor of mortality in late-life depression patients. In their study, 27 out of 103 frail depressed patients (26.2%) died during follow-up, compared to 35 out of 275 non-frail depressed patients (12.7%)7. Additionally, Kim et al. found in their study on the elderly population in Korea that frailty was significantly associated with mortality and healthcare utilization. In their study, the coexistence of depressive mood and frailty significantly increased hospitalization days (average hospitalization days of 19.3 days vs. 11.2 days, P < 0.001) and the use of long-term care services (7.1% vs. 2.4%, P < 0.001)12.
Second, this study shows that the frailty status of depressed patients affects not only all-cause mortality but also significantly impacts cardiovascular and cancer-specific mortality. This finding is consistent with the study by Peng et al., which included 58 prospective cohort studies involving over 1.85 million participants. The study found that compared to robust adults, frail adults had significantly increased risks of all-cause mortality, cardiovascular mortality, cancer mortality, and respiratory disease mortality13. Our further subgroup analysis showed that the frailty index was positively associated with mortality risk across different age groups, genders, races, BMI categories, and statuses of hypertension and diabetes. This finding underscores the importance of the frailty index as a broadly applicable prognostic indicator. The study by Hamada et al. also indicated that frailty was associated with high mortality risk in depressed patients, regardless of other covariates. In their study, patients who were frail and had moderate to severe depressive symptoms had a significantly higher mortality rate (HR = 3.26, 95% CI: 1.16–9.15, P = 0.025)14. Additionally, our sensitivity analyses showed that even after excluding participants with a baseline history of cardiovascular disease or cancer, the association between the frailty index and mortality remained significant. This suggests that the impact of frailty on mortality in depressed patients is robust and consistent.
An important finding of this study is the significant dose-response relationship between the frailty index and the risks of all-cause, cardiovascular, and cancer mortality in depressed patients. Compared to the lowest frailty index tertile, the highest tertile group had a 291% increase in the risk of all-cause mortality, a 313% increase in cardiovascular mortality, and a 230% increase in cancer mortality (P < 0.001). This result is in line with the study by Kawada et al., which found that higher frailty levels were associated with higher mortality risks in elderly patients15.
In this study, we found that depressed females were more likely to be frail, consistent with previous research findings16. Females are more prone to low body weight, muscle weakness, and sarcopenia compared to males17. As age increases, women are more likely to face nutritional deficiencies, making them more susceptible to reaching frailty thresholds. Moreover, we observed that participants with higher frailty scores were often drinkers, had higher BMI, and had less total physical activity time. Numerous studies have shown that nutritional intake, lifestyle habits, diseases, and psychological factors all contribute to the development and progression of frailty18,19,20. These variable characteristics suggest that frailty is a reversible comprehensive health state. Therefore, multidimensional preventive or intervention measures should be taken to address frailty issues in depressed patients. Currently, there are no clinical trials specifically targeting the prevention or improvement of frailty in depressed patients, and whether reversing individual frailty can reduce the risk of adverse outcomes remains to be further studied.
Mechanism discussion
The frailty status in depressed patients may increase mortality risk through various biological mechanisms. First, both depression and frailty are associated with chronic inflammatory responses, which can lead to an increased risk of cardiovascular disease and cancer21. Second, depressed patients often experience lifestyle changes, such as unhealthy diets and lack of exercise, which can exacerbate frailty and increase mortality risk22. Additionally, frailty may affect cognitive function and daily activity capability, making patients more prone to accidental injuries and infections, thereby increasing mortality risk23.
Strengths and limitations
This study has several strengths. It is the first systematic analysis of the relationship between the frailty index and mortality risk in depressed adults in the U.S., intentionally including younger participants to fill a key gap in frailty research. By doing so, we can better understand the frailty status of depressed patients across different age groups and its impact on mortality risk, providing stronger evidence for clinical practice. The study used a large, nationally representative sample from NHANES, resulting in high external validity and generalizability. Furthermore, we employed rigorous statistical methods, including multivariate adjustments and sensitivity analyses, to ensure the robustness and reliability of the results.
However, this study also has some limitations. First, some depression-related data and the measurement of the frailty index were self-reported by participants, which may be subject to self-report bias. To mitigate this, NHANES adheres to standardized and meticulously controlled procedures to ensure the reliability and completeness of the data. Second, although we have attempted to control for confounding factors, there may still be unmeasured or unknown confounders. Additionally, NHANES does not provide detailed data on antidepressant use, which limits our ability to analyze the potential impact of different classes of antidepressants on frailty, particularly considering their metabolic side effects. Lastly, due to the observational nature of the study, we cannot establish causal relationships or assess the potential prognostic benefits of frailty interventions. Further research is needed to evaluate frailty interventions.
Conclusion
In summary, this study indicates that the frailty index is an important indicator for assessing the mortality risk in depressed patients, suggesting that the management of frailty status should be emphasized in clinical practice to improve prognosis in these patients.
Data availability
Publicly available datasets were analyzed in this study. All data entered the analysis were from NHANES, which is publicly accessible to all.
References
Monroe, S. M. & Harkness, K. L. Major depression and its recurrences: life course matters. Annu. Rev. Clin. Psychol. 18, 329–357 (2022).
Dai, L. L. et al. Anxiety and depressive symptoms among COVID-19 patients in Jianghan Fangcang Shelter Hospital in Wuhan, China. PLoS One 15, e0238416 (2020).
Feng, Z., Tong, W. K., Zhang, X. & Tang, Z. Prevalence of depression and association with all-cause and cardiovascular mortality among individuals with type 2 diabetes: a cohort study based on NHANES 2005–2018 data. BMC Psychiatry 23, 490 (2023).
Guida, J. L. et al. Measuring aging and identifying aging phenotypes in cancer survivors. J. Natl. Cancer Inst. 111, 1245–1254 (2019).
Kojima, G., Iliffe, S. & Walters, K. Frailty index as a predictor of mortality: a systematic review and meta-analysis. Age Ageing 47, 193–200 (2018).
Almeida, O. P. et al. Depression, frailty, and all-cause mortality: a cohort study of men older than 75 years. J. Am. Med. Dir. Assoc. 16, 296–300 (2015).
Arts, M. H. L. et al. Frailty as a predictor of mortality in late-life depression. J. Clin. Psychiatry 82, 20m13277 (2021).
Searle, S. D., Mitnitski, A., Gahbauer, E. A., Gill, T. M. & Rockwood, K. A standard procedure for creating a frailty index. BMC Geriatr. 8 (2008).
Tang, H., Zhang, X., Luo, N., Huang, J. & Zhu, Y. Association of dietary live microbes and nondietary prebiotic/probiotic intake with cognitive function in older adults: evidence from NHANES. J. Gerontol. Biol. Sci. Med. Sci. 79, glad175 (2024).
Rattan, P. et al. Inverse association of telomere length with liver disease and mortality in the US population. Hepatol. Commun. 6, 399–410 (2022).
Liang, J. et al. Association between joint physical activity and dietary quality and lower risk of depression symptoms in US adults: cross-sectional NHANES study. JMIR Public Health Surveill. 9, e45776 (2023).
Kim, Y., Kim, J., Kim, M., Song, K. & Choi, M. Association of depressive mood and frailty with mortality and health care utilization: Korean National Cohort Study. J. Am. Med. Dir. Assoc. 24, 504–510 (2023).
Peng, Y., Zhong, G. C., Zhou, X., Guan, L. & Zhou, L. Frailty and risks of all-cause and cause-specific death in community-dwelling adults: a systematic review and meta-analysis. BMC Geriatr. 22, 725 (2022).
Hamada, S. et al. Association of coexistence of frailty and depressive symptoms with mortality in community-dwelling older adults: Kashiwa Cohort Study. Arch. Gerontol. Geriatr. 119, 105322 (2024).
Kawada, T. Depression and all-cause mortality in older adults: a risk assessment. Geriatr. Gerontol. Int. 19, 366–366 (2019).
O’Caoimh, R. et al. Prevalence of frailty in 62 countries across the world: a systematic review and meta-analysis of population-level studies. Age Ageing 50, 96–104 (2021).
Phung, L. A., Karvinen, S. M., Colson, B. A., Thomas, D. D. & Lowe, D. A. Age affects myosin relaxation states in skeletal muscle fibers of female but not male mice. PLoS One 13, e0199062.
de Labra, C., Guimaraes-Pinheiro, C., Maseda, A., Lorenzo, T. & Millán-Calenti, J. C. Effects of physical exercise interventions in frail older adults: a systematic review of randomized controlled trials. BMC Geriatr. 15 (2015).
Ho, L. Y. W., Cheung, D. S. K., Kwan, R. Y. C., Wong, A. S. W. & Lai, C. K. Y. factors associated with frailty transition at different follow-up intervals: a scoping review. Geriatr. Nurs. 42, 555–565 (2021).
Lorenzo-López, L. et al. Nutritional determinants of frailty in older adults: a systematic review. BMC Geriatr. 17 (2017).
Dantzer, R. et al. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat. Rev. Neurosci. 9, 46–56 (2008).
Delgado-Velandia, M., Maroto-Rodríguez, J., Ortolá, R., Rodríguez-Artalejo, F. & Sotos-Prieto, M. The role of lifestyle in the association between frailty and all-cause mortality amongst older adults: a mediation analysis in the UK Biobank. Age Ageing 52, afad092 (2023).
Doi, T. et al. Car accidents associated with physical frailty and cognitive impairment. Gerontology 66, 624–630 (2020).
Acknowledgements
We thank Huanxian Liu (Department of Neurology, Chinese PLA General Hospital, Beijing, China), and Haoxian Tang (Department of Clinical Medicine, Shantou University Medical College, Shantou, Guangdong, China) for their valuable comments on the study design and manuscript.
Funding
This study was supported by China Scholarship Council(grant No. 201906070289), Startup Fund for Scientific Research, Fujian Medical University (grant No. 2022QH1268). The funders had no role in the study design, analysis, decision to publish, nor preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
X.L., Y.H. and Y.W. participated in the design of research schemes, extracted, and analyzed the data, and wrote the main manuscript text. C.L. and Y.H. collected the data. Y.Z., P.C. and B.X. participated in the design of research schemes. X.L. reviewed the manuscript. All authors contributed to the article and approved the submitted version. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
Ethics approval was obtained from the NCHS Ethics Review Committee, and participants provided written informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, X., Wang, Y., Huang, Y. et al. Association between frailty index and mortality in depressed patients: results from NHANES 2005–2018. Sci Rep 15, 3305 (2025). https://doi.org/10.1038/s41598-025-87691-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-87691-4
Keywords
This article is cited by
-
Relationship of the oxidative balance score with the risk of frailty and mortality in patients with asthma: a mediation analysis of NHANES
BMC Pulmonary Medicine (2025)
-
Population-based validation of a frailty index using electronic regional healthcare records for public health use
Scientific Reports (2025)
-
The association between frailty and recurrent pregnancy loss in reproductive-aged women: a cross-sectional study
Scientific Reports (2025)