Abstract
This paper focuses on the elective surgical scheduling problem with multi-resource constraints, including material resources, such as operating rooms (ORs) and non-operating room (NOR) beds, and human resources (i.e., surgeons, anesthesiologists, and nurses). The objective of multi-resource constrained elective surgical scheduling (MESS) is to simultaneously minimize the average recovery completion time for all patients, the average overtime for medical staffs, and the total medical cost. This problem can be formulated as a mixed integer linear multi-objective optimization model, and the honey badger algorithm based on the Nash equilibrium (HBA-NE) is developed for the MESS. Experimental studies were carried out to test the performance of the proposed approach, and the performance of the proposed surgical scheduling scheme was validated. Finally, to narrow the gap between the optimal surgical scheduling solution and actual hospital operations, digital twin (DT) technology is adopted to build a physical-virtual hospital surgery simulation model. The experimental results show that by introducing a digital twin, the physical and virtual spaces of the smart hospital can be integrated to visually simulate and verify surgical processes.
Similar content being viewed by others
Introduction
In the face of mounting pressure from the aging population, continued rising healthcare demands, and budgetary constraints, many hospitals around the world are striving to improve the quality and efficiency of healthcare services with limited medical resources. In most hospitals, elective surgeries constitute a substantial portion of hospital revenue. Approximately 40% of hospital expenditure comes from operating rooms (ORs), and over 60% of inpatient admissions come from surgical operations1. Typically, surgical schedules are manually generated according to the surgeons’ personal schedules and preferences for specific ORs. The decision to schedule surgeries depends solely on the experience of hospital managers. However, due to the complexity of the scheduling problem, it is difficult to manually manage, resulting in highly inefficient hospital services. This prompted us to design a more efficient surgical scheduling system that would not only increase hospital profits but also significantly improve the quality of healthcare services provided to patients.
Recently, advances in healthcare and information technology have driven a shift in hospital operation management toward a data-driven smart hospital. The design of the smart hospital incorporates the concepts of intelligent, information-based, and digital hospitals so that people can access information about medical services quickly and accurately. Although some progress has been made in smart hospitals, the seamless integration of hospital physical systems and information systems has not yet been fully realized. Currently, the rise of digital twin, which are characterized by virtual reality interactions, real-time control, and symbiotic evolution, has made it possible to perfectly integrate physical and virtual hospitals2. Digital twin (DT)-based surgical scheduling provides a new method and concept for optimizing hospital resource allocations, increasing operational efficiency, and improving the quality of medical services3.
Unlike most of the literature on surgical scheduling, we consider both upstream and downstream activities during the stages of pre-operative preparation, anesthesia, surgery, and resuscitation. At each stage, multiple resources, including material resources, such as operating rooms (ORs) and beds in non-operating rooms (NOR beds), and human resources, such as surgeons, anesthesiologists, nurses, are taken into account. Moreover, in many surgery centers, prescheduled elective surgeries constitute the majority of surgical cases. Therefore, this study focuses on the scheduling of elective surgery and does not consider emergency cases. The issue of multi-resource constrained elective surgical scheduling (MESS) is complex because numerous factors need to be considered, such as the interests of various stakeholders (e.g., patients, medical staffs, and the hospital manager) and resource constraints. MESS can therefore be modeled based on multi-objective optimization in order to respect all interests simultaneously. Since game theory is an effective optimization technique that balances the interests of different stakeholders, this study adopts the idea of game theory to guarantee optimality among multiple objectives.
This study aimed to address a novel MESS with patient flow and an uncertain duration of operation stages. For this purpose, a honey badger algorithm based on the Nash equilibrium (HBA-NE) is proposed to solve this problem. We use data obtained from the First Affiliated Hospital of Hebei North University (FAH-HNU), a national university hospital in China. A case study is conducted to examine the efficiency of the scheduling model and the proposed algorithm under real conditions. However, in practice, there are still differences between the scheduling scheme and the actual operating conditions. To reduce scheduling deviation, a new surgical scheduling method based on digital twin is proposed. We stablish visualization models of the MESS to visually present the execution process of surgical scheduling, which is beneficial for hospital managers’ decision making. The contributions of this study are as follows:
-
(1)
The minimum average recovery completion time for patients, average overtime for medical staffs, and total medical cost are optimized simultaneously in the multiple resource-constrained surgical scheduling scenario, which is a common scenario in hospitals.
-
(2)
This paper extends the application of game theory in the surgical scheduling field. A honey badger algorithm based on the Nash equilibrium (HBA-NE) is proposed, and the excellent performance of the HBA-NE is verified by real hospital cases and comparative algorithms.
-
(3)
Digital twin technology is used to achieve real-time interaction between the surgical scheduling strategies of physical and virtual hospitals. This paper proposes the application of a DT model in a surgical scheduling system and builds a visualization platform for smart hospitals.
The remainder of this paper is organized as follows. In Sect “Related literature”, we provide a review of the related literature. In Sect “Problem formulation”, we describe the MESS problem with assumptions and develop a mathematical model. In Sect “Game theory model for the MESS problem”, the game theory model of the multi-objective MESS is presented. In Sect “Applications of the HBA-NE algorithm on multi-objective MESS”, the details of the HBA-NE algorithm for solving multi-objective MESS problems are introduced. In Sect “Computational experiments”, computational experiments are carried out, and the results are reported and analyzed. To simulate actual operations, a virtual hospital operating room model based on DT technology was constructed with the professional simulation software AnyLogic Professional 8.8.2. The paper concludes with Sect “Conclusions and management insights”, which suggests directions for future work.
Related literature
Multi-resource constrained surgical scheduling
Current research has focused mainly on the scheduling of ORs4,5. Although ORs are scarce medical resources, when planning surgeries, the downstream facilities, such as wards, intensive care units (ICUs), and post anesthesia care unit (PACU) are frequently considered1. Some studies considered downstream resources. For instance, Thomas Schneider, et al.6 discussed the problem of scheduling surgery groups while optimizing the resources of wards and the ICU. Varmazyar, et al.7 investigated stochastic OR scheduling and forecasted PACU times. Shehadeh and Padman8 addressed the master surgery schedule (MSS) by considering the constraints of multiple downstream units, namely, the ward, ICU, and PACU. Other studies considered the upstream resources such as outpatient clinics (OCs) and induction rooms (IRs). Bovim, et al.9 studied the integrated master surgery and OC scheduling problem to ensure the efficient treatment of patients. Çelik, et al.10 proposed a stochastic mixed integer programming (SMIP) model for the scheduling surgery problem with multiple ORs and IRs.
The above literature ignores human resource constraints (e.g., surgeons, anesthesiologists, and nurses) in surgical scheduling problems, resulting in surgery delays and scheduling schemes that are unfeasible in practice11. Vali-Siar, et al.12 noted that human resources, including specialized surgeons, nurses (e.g., scrub nurses, circulator nurses, and nurse anesthetists), and anesthesiologists, are needed to perform surgery in ORs. To the best of our knowledge, few studies have considered human resource constraints in surgical scheduling. Recently, Bargetto, et al.13 discussed an OR planning problem that includes human resources (i.e., surgeons and nurses) as well as common constraints (i.e., sequencing, capacity, and due date) in practice. However, Bargetto et al.’s work did not consider either multi-stage operations or the uncertainty of surgery duration. In contrast, we design a multi-stage, multi-resource constrained elective surgical scheduling (MESS) model that includes uncertainty and stochastic optimization methods to enhance the reality of modeling.
Multi-objective game optimization method
MESS is a challenging optimization problem due to its high complexity and multiple objectives14. In the presence of conflicting objectives, the optimal trade-off should be determined. Game theory studies competition and cooperation among rational decision makers and can be used to address multiple-objective optimization problems. Game theory has been widely studied, especially as one of the most competitive strategy selection methods for resource allocation optimization in the manufacturing industry15. Some researchers have used the game theory method for solving multi-objective job shop scheduling problems and achieved the best combination of optimization objectives16,17. For instance, Renna, et al.18 proposed a game theory model based on Gale-Shapley for worker assignments in dual-resource constrained (DRC) flexible job shop scheduling settings. Belabid, et al.19 developed a meta-heuristic algorithm that combines the Nash equilibrium and a genetic algorithm for solving flow shop scheduling problems. In the work of Wei, et al.20, a dynamic flexible job shop scheduling model with machine faults was established, and a multi-objective migrating bird optimization algorithm based on game theory was designed to approximate the Nash equilibrium machine allocation scheme. Because of the similarities between medical systems and production systems, some researchers have applied models and methods ranging from production to healthcare decision-making9,21. Belabid, et al.19 argued that since noncooperative game theory (e.g., Nash equilibrium) deals with how participants interact to achieve their goals, so it is the most applicable to surgical scheduling. In summary, the multi-objective optimization algorithm based on game theory can improve the convergence speed and computational efficiency. Therefore, it is necessary to develop a multi-objective optimization game method to reduce the complexity of the MESS problem and improve the decision-making efficiency of hospital managers.
Meta-heuristic algorithms for scheduling problems
The surgical scheduling problem is an NP-hard combinatorial optimization problem. The MESS system is even more difficult to solve than the traditional surgical scheduling problem because of multiple resource constraints, including material resources (e.g., ORs, NOR beds) and human resources (e.g., surgeons, anesthesiologists, nurses). A meta-heuristic algorithm can efficiently solve this problem, yield a reasonable allocation of medical resources, and improve surgery efficiency22,23. Recently, researchers have paid close attention to meta-heuristics because of their global search potential. The monarch butterfly optimization (MBO)24, hunger games search (HGS)25, honey badger algorithm (HBA)26, wild horse optimizer (WHO)27, arithmetic optimization algorithm (AOA)28, African vulture optimization algorithm (AVOA)29, and the differential evolution (DE) algorithm1 have been successfully explored in the literature. Among them, the HBA is a meta-heuristic technique proposed by Hashim, et al.26 that simulates the foraging behaviors of honey badgers. With the advantages of high flexibility, simple algorithm structure, and high convergence accuracy, the HBA has been widely used in various fields30, such as UAV path planning30, medical diagnosis systems31, and optimal energy system configuration32,33. This study proposes a new algorithm based on combining the Nash equilibrium concept with the HBA (i.e., HBA-NE) to solve the MESS problem.
Digital twin in smart hospitals
In the actual process of surgical scheduling, there is information asymmetry, such as the patient suddenly refusing to undergo surgery and the surgeon’s schedule suddenly changing. This will cause a deviation in the implementation of the MESS strategy and affect the efficiency and quality of surgical scheduling execution. To address these challenges well, digital twin (DT) technology has emerged. The concept of DT, which was first proposed by Grieves34, is “a generic, standard three-dimensional architecture including physical entities, virtual models, and their connections”35. It is one of the most promising Industry 4.0 (I4.0) enabling technologies, which realizes the convergence of the physical and digital worlds in manufacturing. Due to the properties of virtual reality interaction and symbiotic evolution, DT has been discussed in existing research to address the increasing complexity of data collection and analysis in hospital operations2,36,37. In this research field, scholars have mainly focused on the application of DT in smart hospitals, such as hospital operation and management38, intelligent health monitoring and diagnosis systems39,40,41, hospital appointment systems42, emergency department triage systems43, and IoT-aware smart hospitals44,45. Although the concept of smart hospitals has been proposed in previous research and practice, the need to cope with multiple complex tasks in hospital operations (e.g., surgical scheduling) remains unmet2. Among the various applications of DT, simulation plays a crucial role in healthcare, especially in studies such as medical resource allocation and medical activity prediction. However, integrating the physical and virtual worlds in medicine to truly achieve smart hospitals remains a challenge in the era of precision medicine46.
To the best of our knowledge, no studies have integrated the concept of DT with surgical scheduling. To fill this research gap, this paper studies the DT-driven MESS system and creates a smart hospital visualization platform based on the analysis of the status of medical resources and patient needs combined with DT technology. The DT-driven MESS includes two parts: a physical hospital and a virtual hospital. The physical hospital refers to the actual surgery system, and the virtual hospital is the virtual model of the physical hospital47. In the virtual hospital, scheduling data, such as material resources, human resources, and patient information, can be obtained from the physical hospital. These data are input into the scheduling model and proposed algorithm to simulate and obtain the surgical scheduling scheme. After validation, the final surgical scheduling strategy is fed back to the physical hospital for implementation. By combining DT technology with medical resource scheduling, there will be a new and efficient way to provide high-quality medical services for patients.
Problem formulation
Problem description
This study focused on the real elective surgical scheduling problem of a national university hospital in China with 20 ORs, 10 NOR beds, 67 surgeons, 20 anesthesiologists, and 30 nurses. There are an additional two ORs dedicated to emergency surgery. Assigning emergency surgeries was not considered in the current study. Emergency surgeries are often performed in specialized emergency ORs that are not used for elective patients48. Each day, different surgeons are responsible for the corresponding emergency surgeries. In the hospital, the elective surgery plan involves creating a waiting list by collecting surgery requests from the surgeons, which is scheduled one day in advance. Generally, the surgical procedure for elective patients usually has three stages: the pre-operative (intake) stage, peri-operative (anesthesia, surgery) stage, and post-operative (recovery) stage. A patient arriving at a hospital is first assigned to the NOR area. The patient stays in this ward until the nurse completes the check-in process. Subsequently, the patient is transported to an available OR for surgery. The resources required for this stage include human resources (e.g., surgeons, anesthesiologists, nurses) and material resources (e.g., ORs). After surgery, the patient is transferred to the NOR area for recovery. The necessary resources in the postoperative stage include beds and nurses. Obviously, the resources involved in the surgery are characterized by simultaneity and diversity. If one of the resources in the three-stage surgery flow is not available in a timely manner, then the entire procedure has to be delayed, and the efficiency of the surgery is compromised. Since elective surgery requires multiple resources and is subject to many constraints, effective OR scheduling is necessary. To this end, the current study aimed to provide an effective scheduling scheme for reducing medical staff overtime, idle OR time, and surgery delay while considering the available resources and constraints. Figure 1 shows the three stages of the surgical procedure and the multiple resources involved.
We consider the assignment of elective patients to ORs and NOR beds because they play a crucial role in influencing surgical schedules. In addition, medical resources are scarce and costly, leading to conflicting priorities among stakeholders (e.g., patients, medical staffs, and the hospital manager). The goal is to generate schedules within the planning scope that maximize the interests of stakeholders while reducing surgery delays and operating costs. More specifically, three objectives are considered to be optimized simultaneously: to enhance patient satisfaction, the average recovery completion time for all elective patients (APT) is selected as the first objective; to improve medical resource utilization, the average overtime for medical staffs (AOT) and total cost of medical resources (TC) are selected as the other two objectives. Thus, the elective surgical scheduling with multi-resource was established on this basis.
Since multiple resources are required for the three stages to be integrated into a model, a mixed-integer linear programming problem (MILP) model is proposed to formulate an elective surgical schedule. The following assumptions are made in developing our model:
-
(1)
The required human resources include surgeons, anesthesiologists and nurses. In addition, the nurses are homogeneous with no specialty constraints, who are involved in the three-stage surgery procedure49.
-
(2)
In the peri-operative stage, each surgery is assigned to a surgeon and an anesthesiologist12.
-
(3)
The whole surgery procedure for elective patients is performed on an OR, while both anesthesia and recovery processes of patients are performed on a NOR bed50.
-
(4)
All ORs are multifunctional and a patient can be operated in any OR. After surgery, the patient must be transported to a NOR bed for recovery51.
-
(5)
The surgery process that has already begun cannot be interrupted or canceled52.
-
(6)
The patient’s transfer time during anesthesia, surgery, and recovery can be negligible10.
-
(7)
Elective patients arrive to the surgery suite at the appointment time53.
-
(8)
The durations of pre-operative, peri-operative, and post-operative stages are uncertain48. It has been demonstrated that the natural logarithm of the duration is normally distributed54.
-
(9)
Eight hours is the regular open time for elective surgeries, and overtime for medical staffs are also taken into account13.
-
(10)
According to Article 36 of the “Labor Law of the People’s Republic of China” (https://flk.npc.gov.cn/), “To pay no less than 150% of the normal wages if an extension of working hours is arranged.”
Keywords
This section presents an MILP model for the elective surgical scheduling problem. Tables 1, 2, 3 and 4 summarize the notation of input parameters, indices, and decision variables used.
Mathematical model
The MESS problem can be formulated as a multi-objective optimization model, where three criteria in the objective function are minimized. These criteria include patient recovery completion time, medical staff overtime, and total cost. The present study attempts to provide a comprehensive and generalized model that is maximally applicable to different situations.
Objectives:
-
(1)
Minimizing the average recovery completion time for all patients:
-
(2)
Minimizing the average overtime for medical staffs:
-
(3)
Minimizing the total cost of medical resources:
where,
Subject to:
In the model above, Eqs. (1), (2), (3) represent the objectives of the MESS problem under investigation. The load cost/idle cost of ORs/NOR beds can be calculated by Eqs. (4), (5), (6), (7), respectively. The labor costs of surgeons, anesthesiologists, and nurses are represented by Eqs. (8), (9), (10), respectively, where overtime pay is 150% of the normal wage (see Assumption (10)). Equation (11) guarantees that the surgeon and anesthesiologist are only present during the peri-operative (i.e., anesthesia, surgery) stage. Constraint (12) indicates that each surgical operation can be performed by only one nurse. Constraints (13)–(14) guarantee that each elective patient is assigned a NOR bed or an OR for surgical operations. The completion time of operation stage j for patient i is calculated on constraint (15). Constraint (16) ensures that if treatment for a patient is not completed under anesthesia, then surgery cannot be started. Constraint (17) ensures that each patient is transferred to the NOR bed immediately after surgery without delay. Constraint (18) guarantees that one OR can only treat one patient at a time; Constraint (19) guarantees that one NOR bed can only treat one patient at a time, where L denotes an infinitely large positive value. Constraints (20)–(22) indicate that at a certain time, a surgeon, an anesthesiologist, or a nurse can only perform one surgical operation, Oij.
In general, two approaches can be used for solving multi-objective optimization problems: the weighted-sum method and Pareto method55. Idea of the weighted-sum method is to transform the multi-objective problem into a single-objective problem. However, regarding the three objectives (i.e., minAPT, minAOT, minTC) in the MESS, it seems difficult for any hospital manager to determine the relevant weights for each objective. The Pareto optimization method provides a set of alternative solutions that represents the trade-off between objectives. But in practice, it is economically difficult for hospital managers to choose from an extremely large set of solutions56. Moreover, the commonly used optimization methods cannot ensure optimality and fairness among multiple objectives. Game theory is an effective tool to balance multiple objectives and offer decision makers the alternative optimal solutions. To fully reflect the surgical processing attributes of elective patients and coordinate the interests of different stakeholders, a hybrid algorithm based on the Nash equilibrium has been used to optimize the multi-objective MESS problem.
Game theory model for the MESS problem
Surgery involves medical resources are scarce and expensive compared to the demand of patients. It is a challenge to allocate the limited medical resources efficiently, and the ideal way to allocate resources is to match the medical supply with the patient demand. In this study, MESS problem refers to the allocation of processing surgical tasks on material and human resources under uncertain durations. This can be regarded as a multi-player game involving patients, medical staffs and the hospital manager. Due to complex multi-resource constraints, diverse surgical task indicators and scarce medical resources, there are individual competing relationships in surgical scheduling.
Game relationships
Notably, national hospitals are equipped with advanced facilities and high-level surgical specialists. However, a larger number of patients’ inrush has led to the overburdened workforce and equipment, as well as long waiting queues for patients, which in turn affects patients’ choices for medical resources utilization. In the “hospital–patient” game relationship, high-quality medical services will bring a good treatment experience and improve the real payoff, but it comes with the increased patient demand and cost burdens for the hospital. In the “medical staff-hospital” game relationship, the scarcity of medical staffs, especially surgical specialists, forces hospital managers to focus on their daily scheduling and work hours. In order to provide high-quality medical services, many national hospitals in China require surgeons to be “24-hour on call”. As a result, a conflict arises between the hospital’s requirement for high-quality medical services and the overload of medical staffs. Obviously, the real-world decision-making problems involving different stakeholders, generally contain multiple and conflicting objectives. In the game, patients, medical staffs and the hospital manager all aim to maximize their own benefits, which corresponds to the objectives of minAPT, minAOT, and minTC in the MESS problem. When solving the balance between multiple objectives, the application of non-cooperative game model can provide a reasonable decision basis for decision makers and achieve the best combination of optimization objectives. Technically, the game model consists of three elements: players, strategies, and payoffs.
Players
An MESS can be regarded as a multi-objective optimization problem with stakeholders in the hospital system as players. The MESS problem is modeled as an N + W + 1-player non-cooperative game with complete information where the patient, medical staff, and hospital manager act as players in the game. The model is depicted as a 3-tuple: G = {N + W + 1, S, U}, where N + W + 1 is the set of players who participate in the game, including N patients, W medical staffs, and one hospital manager. S is the strategy set, and U is the payoff set.
Strategies
In the MESS game model, for patient i at stage j (j = 1,2,3), the surgical operation\({O_{ij}}\)involves a set \(M={M_{or}}+{M_{nor}}\)of material resources, where\({M_{or}}=\left\{ {1,2,…,{m_{or}}} \right\}\)and\({M_{nor}}=\left\{ {1,2,…,{m_{nor}}} \right\}\)represent the OR set and NOR bed set available for selection. The strategy adopted by patient i is\({s_i}=\left\{ {O{R_{i,k}},NO{R_{i,k^{\prime}}}} \right\}\), where\(k \in {M_{or}}\),\(k^{\prime} \in {M_{nor}}\).
For medical staffs, there are n elective patients need to be treated, involving surgical operation\({O_{ij}}\) to be processed. Thus, the strategy of surgeon r is\({s_r}=\left\{ {{Z_{1jr,}},{Z_{2jr}}, \ldots ,{Z_{njr}}} \right\}\), the strategy of anesthesiologist\(r^{\prime}\)is \({s_{r^{\prime}}}=\left\{ {{Z_{1jr^{\prime}}},{Z_{2jr^{\prime}}}, \ldots ,{Z_{njr^{\prime}}}} \right\},\) and the strategy of nurse\(r^{\prime\prime}\)is \({s_{r^{\prime\prime}}}=\left\{ {{Z_{1jr^{\prime\prime}}},{Z_{2jr^{\prime\prime}}}, \ldots ,{Z_{njr^{\prime\prime}}}} \right\},\) where \(Z_{{ijr}} = \left\{ \begin{gathered} 1,{\text{ }}if{\text{ }}O_{{ij}} {\text{ }}is{\text{ }}assigned{\text{ }}to{\text{ }}surgeon{\text{ }}r \hfill \\ 0,{\text{ }}otherwise \hfill \\ \end{gathered} \right.,\) \(Z_{{ijr^{\prime}}} = \left\{ \begin{gathered} 1,{\text{ }}if{\text{ }}O_{{ij}} {\text{ }}is{\text{ }}assigned{\text{ }}to{\text{ }}anesthesio\log ist{\text{ }}r^{\prime} \hfill \\ 0,{\text{ }}otherwise \hfill \\ \end{gathered} \right.,\) \(Z_{{ijr^{\prime\prime}}} = \left\{ \begin{gathered} 1,{\text{ }}if{\text{ }}O_{{ij}} {\text{ }}is{\text{ }}assigned{\text{ }}to{\text{ }}nurse{\text{ }}r^{\prime\prime} \hfill \\ 0,{\text{ }}otherwise \hfill \\ \end{gathered} \right..\)
For the hospital manager, the strategy adopted can be expressed as\(s_{h} = \left\{ {l_{1} ,l_{2} , \ldots ,l_{n} } \right\},\) denoting the relative sequence of treatment between patients.
Payoffs
The objectives of the MESS problem can be regarded as the payoffs of the corresponding players. U is the payoff set,\(U=\{ {u_1},{u_2}, \ldots ,{u_{n+w+1}}\}\), and ut denotes the payoff of player t. In the MESS game, each player attempts to maximize his or her payoff, which mainly depends on his or her playing strategy, i.e., how to schedule surgical operations on corresponding ORs and NOR beds. More specifically, for patients, the goal is to have the surgery be done as quickly as possible. For medical staffs, they are expected to complete their work with minimum overtime. For the hospital manager, the surgical efficiency should be as high as possible. Notably, the payoff of each player’s strategy is affected not only by his or her own scheduling strategy but also by the strategies selected by others.
The payoff of patient i is defined as the decreasing function of the surgery completion time and can be expressed as follows:
where,\({f_i}={C_{i3}}\)denotes the completion time of surgery for patient i. In the MESS system, ORs and NOR beds are resourced differently, and the number of skills and operating proficiency are both different among different medical staff. The actual treatment time is affected by both the material capacity and staff efficiency. Therefore, the duration of operation stage j for patient i is denoted as:
\(\mathop {{P_{ij}}}\limits^{\sim } =\left\{ \begin{gathered} \hbox{min} {P_{ijk}},\forall k{\text{ }},{\text{ }}if{\text{ }}j=2,k \in {M_{or}} \hfill \\ \hbox{min} {P_{ijk^{\prime}}},\forall k^{\prime},if{\text{ }}j=1,3,k^{\prime} \in {M_{nor}} \hfill \\ \end{gathered} \right.,\)
the payoff is greatest when patient i’s surgical completion time \({f_i}\) reaches its lower bound \({\underset{\raise0.3em\hbox{$\smash{\scriptscriptstyle-}$}}{f} _i}=\sum\nolimits_{{j=1}}^{3} {\mathop {{P_{ij}}}\limits^{\sim } }\); i.e., there is no waiting between the stages of the surgery.
The payoffs of medical staffs are defined as a decreasing function of overtime, and as shown in Eqs. (24), (25), (26).
The payoff of surgeon r:
The payoff of anesthesiologist\(r^{\prime}\):
The payoff of nurse\(r^{\prime\prime}\):
where, L is an infinitely large positive value.
In Eq. (24), the payoff is greatest when the overtime\({f_r}\)of surgeon r reaches its lower bound \(\underset{\raise0.3em\hbox{$\smash{\scriptscriptstyle-}$}}{f} _{r} = \min \left( {\sum\nolimits_{{i = 1}}^{n} {Z_{{i2r}} P_{{i2}} } - R,{\raise0.7ex\hbox{$1$} \!\mathord{\left/ {\vphantom {1 L}}\right.\kern-\nulldelimiterspace} \!\lower0.7ex\hbox{$L$}}} \right)\). In Eq. (25), the payoff is greatest when the overtime\({f_{r^{\prime}}}\)of anesthesiologist\(r^{\prime}\)reaches its lower bound\(\underset{\raise0.3em\hbox{$\smash{\scriptscriptstyle-}$}}{f} _{{r^{\prime}}} = \min \left( {\sum\nolimits_{{i = 1}}^{n} {Z_{{i2r^{\prime}}} P_{{i2}} } - R,{\raise0.7ex\hbox{$1$} \!\mathord{\left/ {\vphantom {1 L}}\right.\kern-\nulldelimiterspace} \!\lower0.7ex\hbox{$L$}}} \right)\). In Eq. (26), the payoff is greatest when the overtime\({f_{r^{\prime\prime}}}\)of nurse\(r^{\prime\prime}\)reaches its lower bound\(\underset{\raise0.3em\hbox{$\smash{\scriptscriptstyle-}$}}{f} _{{r^{\prime\prime}}} = \min \left( {\sum\nolimits_{{j = 1}}^{3} {\sum\nolimits_{{i = 1}}^{n} {Z_{{ijr^{\prime\prime}}} P_{{ij}} - R} ,{\raise0.7ex\hbox{$1$} \!\mathord{\left/ {\vphantom {1 L}}\right.\kern-\nulldelimiterspace} \!\lower0.7ex\hbox{$L$}}} } \right)\).
The payoff of the hospital manager is defined as a decreasing function of cost, as shown in Eq. (27).
The payoff is greatest when the total cost of hospital\({f_i}\)reaches its lower bound: \({\underset{\raise0.3em\hbox{$\smash{\scriptscriptstyle-}$}}{f} _h}=\hbox{min} TC=\hbox{min} \left( {TC_{{or}}^{{load}}+TC_{{or}}^{{idle}}+TC_{{nor}}^{{load}}+TC_{{nor}}^{{idle}}+T{C_{sur}}+T{C_{ano}}+T{C_{nur}}} \right)\). During surgery, if there are no idle ORs or NOR beds, then the costs of material resources and medical staff are minimal, and the hospital can obtain the maximum profit.
Nash equilibrium solution
In a Nash equilibrium, each player’s strategy is the best when given the strategies of the others. In other words, a player cannot improve his payoffs by changing his current strategy to another feasible one while the strategies of others remain unchanged. When the game reaches the equilibrium state, the solution becomes the Nash equilibrium solution. For the MESS, the Nash equilibrium is used as the solution for the N + W + 1-player (N patients, W medical staff, and one hospital manager) non-cooperative game. Thus, a Nash equilibrium point is described as a set of N + W + 1-tuple strategies\({S^*}=\{ s_{1}^{ * },s_{2}^{ * }, \ldots ,s_{{n+w+1}}^{ * }\}\), one for each player.
The Nash equilibrium can be defined as follows:
where ut is the payoff function of player t, and\(s_{t}^{ * }\)is his best strategy profile. In addition, \(s_{{ - t}}^{ * }=\{ s_{1}^{ * },s_{2}^{ * }, \ldots ,s_{{ - t}}^{ * },s_{{t+1}}^{ * }, \ldots ,s_{{n+w+1}}^{ * }\}\)are the strategies adopted by other players, excluding player t.
MESS mainly focuses three allocation problems: the surgical order of elective patients, the selection of ORs and NOR beds, and the selection of medical staffs (surgeons, anesthesiologists, and nurses). It involves three objectives that need to be optimized: the average recovery completion time (APT) for elective patients (players), the average overtime (AOT) for medical staffs (players) and the total cost of medical resources (TC) for the hospital manager (player). To balance these three objectives, we employ a non-cooperative game to ensure a Pareto-optimal solution, and obtain the optimal surgical scheduling plan through Nash equilibrium (NE). Equation (28) represents an ideal NE solution in which each player (patients, medical staffs and the hospital manager) can achieve the best payoff.
The Nash equilibrium solution is obtained when the AOT, TC and APT reach the optional optimal value (i.e., simultaneously minimized). For elective patient players, regardless of which ORs/NOR beds strategies are selected by medical staff players, the minAPT index obtained by selecting the strategy\(s_{{patient}}^{ * }=\left\{ {{M_{or}},{M_{nor}}} \right\}\)is better than that obtained by selecting other ORs/NOR beds. Similarly, the minAOT index obtained by the medical staff players selecting the elective patient strategy\(s_{{medical{\text{ }}staffs}}^{ * }=\left\{ {{s_r},{s_{r^{\prime}}},{s_{r^{\prime\prime}}}} \right\}\)is more appropriate. For the hospital manager player, regardless of which strategies of the relative sequence of treatment between patients are selected by medical staff players, the minTC index obtained by selecting the strategy\(s_{{hospital{\text{ }}manager}}^{ * }=\left\{ {{l_1},{l_2}, \ldots ,{l_n}} \right\}\)is better than that obtained by selecting other relative sequences. Therefore, for the MESS, the strategy\({S^*}=\left( {s_{{patients}}^{ * },s_{{medical{\text{ }}staffs}}^{ * },s_{{hospital{\text{ }}manager}}^{ * }} \right)\) balances the APT, AOT and TC objectives and is the optimal scheduling scheme.
Applications of the HBA-NE algorithm on multi-objective MESS
The optimal result for the MESS is derived from the Nash equilibrium point in the game. The increasing number of surgical tasks makes it difficult to effectively and efficiently address an NP-hard MESS problem. To effectively solve this problem, in this section, we propose a new hybrid meta-heuristic honey badger algorithm based on the Nash equilibrium (HBA-NE) with an exploration–exploitation ratio search strategy applied in a Nash equilibrium situation to minimize the objectives. Note that the intensity operator is employed to generate the neighborhood space of the solutions.
Workflow of the proposed algorithm
For the multi-objective MESS, this section introduces the framework of the improved HBA-NE optimization algorithm. First, the HBA creates a population that is evenly distributed to optimize the positions of individuals. Then, the Nash equilibrium technique is used to obtain the ideal values for honey badger individuals and to determine the best solution. The workflow of the method is shown in Fig. 2 and mainly includes the following steps:
Step1: Initialize the parameters and maximum number of iterations.
Step2: Generate an initial honey badger population with random positions.
Step3: For each honey badger, calculate the corresponding fitness.
Step4: Use the Nash equilibrium approach to find and record the Nash equilibrium (NEq) solutions for the current generation.
Step4-1: Calculate the optimal value of the objective function of the current generation.
Step4-2: Calculate the NEq for each honey badger individual, and record the minimum NEq as NEmin.
Step4-3: If\(q \leqslant popsize\)(popsize is population size), then go to Step4-4; otherwise, output the Nash equilibrium solutions.
Setp4-4: If\(N{E_q} - N{E_{\hbox{min} }} \leqslant \xi\)(\(\xi\)is the NE solution factor), then record the Nash equilibrium solution and q = q + 1; otherwise, q = q + 1, and go to Step4-3.
Step5: Calculate the intensity of the honey badgers, and then update the density factor.
Step6: Apply the exploration-exploitation rate search strategy (including the digging phase and honey phase) to update the positions of honey badgers.
Step7: If maximum number of iterations is reached, output the best solution; otherwise, execute Step 3 ~ Step 6.
Nash equilibrium for multi-objective MESS
The aim of the Nash equilibrium (NE) solution is to make each objective do its best to approximate its own optimal outcome without compromising the interests of the other objectives. Equation (29) represents an ideal NE solution in which each player can achieve the best benefit.
Equation (29) is an extremely strong condition that is difficult to achieve for most scheduling problems. However, the MESS game model cannot guarantee only one NE solution as there may be more than one NE solutions, or no NE solution. In the latter two cases, the players do not know what actions should be taken. To address this problem, a near Nash equilibrium (NNE) solution is proposed. The basic idea of the NNE solution is to find the minimum distance between the objective function and the optimal value under each strategy. As shown in Eq. (29), the solution with the minimum D is called the NNE solution. Specifically, in the case of no NE solution, Eq. (30) indicates the payoffs that are nearest to the ideal NE, that is, the NNE solution. However, if there is more than one NNE solution, one is randomly selected.
Honey badger algorithm based on the Nash equilibrium (HBA-NE)
The honey badger algorithm (HBA) is a meta-heuristic approach inspired by the foraging behaviors of honey badgers and was recently proposed by Hashim, et al.26. The search process in HBA is divided into two phases: exploration and exploitation. Characterized by an efficient traversing of the search space and an effective balance between exploration and exploitation, the HBA has demonstrated an excellent ability to solve optimal scheduling problems with multiple local solutions32,33. Therefore, this study adopts HBA as the basic algorithm.
However, the MESS optimization problem involves three conflicting objectives (APT, AOT, and TC) that need to be optimized simultaneously. In this case, a single-objective optimization HBA algorithm is not sufficient. To address the MESS problem in a targeted manner, the extension of HBA to multi-objective HBA becomes necessary. We use the Nash equilibrium approach to acquire a set of solutions that reflects the trade-off between conflicting objectives, enabling stakeholders to make the optimal choices. Therefore, the HBA-NE algorithm is proposed in which a three-vector code and a Nash equilibrium-based fitness function are designed to improve the performance of the HBA.
Honey Badger Algorithm (HBA)
The HBA algorithm mimics the social behavior of honey badgers when searching for food. To locate food, honey badgers use either their sense of smell and digging skills or follow honeyguide birds. Thus, the dynamic search behavior of honey badgers involves a digging phase (i.e., exploration) and a honey phase (i.e., exploitation). In the digging phase, the ability to smell honey makes it easy for honey badgers to find food through the digging and capturing process. In the honey phase, the bird leads badgers into beehives and guides them to find food. Based on the above, the mathematical formulation and procedures of the HBA are described in the following steps.
Step1: Initialize the population and positions of the honey badger, using Eq. (30).
where hbq is the position of the qth honey badger individual, ubq and lbq are the upper and lower bound values, respectively, and rn1 is a random number in the range [0,1].
Step2: Define the intensity operator by the inverse square law57 using Eq. (31).
where CS is the source strength or concentration strength,\({\psi _q}\)is the distance between the prey and the qth badge, rn2 is a random number in the range [0,1], and \(h{b_{pery}}\)denotes the position of the prey.
Step3: Update the density factor \(\alpha\), which controls the transition from exploration to exploitation using Eq. (32).
where\(- itr\)is the current iteration,\(it{r_{\hbox{max} }}\)indicates the maximum number of iterations,\(\lambda\)is a constant parameter, and its value is set to 2 by default58,59.
Step4: Escape the local optima zone. Trend modifier A is a tool that modifies search trends to allow the honey badger to fully explore the solution space. It is mathematically formulated by Eq. (33).
where,\(r{n_3}\)is a random number between 0 and 1.
Step5: Update the positions of individuals, including both the “digging phase” and the “honey phase”.
Step5-1: Digging phase (Exploration). A honey badger performs a kind of Cardioid-shaped action31. It is determined using Eq. (34).
where\(h{b_{new}}\)denotes the new position of the honey badger,\(\beta \geqslant 1\)represents the honey badger’s ability to find prey and its default value is 659,60. \(r{n_4}\),\(r{n_5}\)and\(r{n_6}\)are three different random numbers in the range [0,1].
Step5-2: Honey phase (Exploitation). The behavior of a honey badger following a honey guide bird to a beehive can be formulated using Eq. (35).
where\(r{n_7}\)represents a random number in the range [0,1].
Encoding and decoding
The encoding scheme should be able to represent the processing sequence of the surgical operation to be scheduled, so a three-vector encoding is adopted for the MESS problem. It consists of three vectors: a material resource (i.e., ORs and NOR beds) assignment vector, a human resource assignment vector (i.e., surgeons, anesthesiologists, and nurses), and a surgical operation sequence vector. In the proposed HBA-NE, a honey badger vector \(V=\left[ {{v_1},{v_2}, \ldots ,{v_{7n}}} \right]\) represents a 7n-dimensional real vector, where \({v_\rho } \in \left[ {lb,ub} \right]\), \(\rho =\left\{ {1,2, \ldots ,7n} \right\}\) defines the location index of the honey badger individual position, and n denotes the number of all patients. Specifically, \({V_1}=\left[ {{v_1},{v_2}, \ldots ,{v_{3n}}} \right]\) represents the material resource assignment; \({V_2}=\left[ {{v_{3n+1}},{v_{3n+2}}, \ldots ,{v_{6n}}} \right]\) represents the human resource assignment, where \({V^{\prime}_2}=\left[ {{v_{3n+1}},{v_{3n+2}}, \ldots ,{v_{4n}}} \right]\) denotes the surgeon assignment, \({V^{\prime\prime}_2}=\left[ {{v_{4n+1}},{v_{4n+2}}, \ldots ,{v_{5n}}} \right]\) denotes the anesthesiologist assignment, \({V_2}^{{\prime \prime \prime }}=\left[ {{v_{5n+1}},{v_{5n+2}}, \ldots ,{v_{6n}}} \right]\) denotes the nurse assignment, and \({V_3}=\left[ {{v_{6n+1}},{v_{6n+2}}, \ldots ,{v_{7n}}} \right]\) denotes the surgical operation sequence. Thereafter, \({V_1}\) is converted to the material resource assignment vector, \({V_2}\) is converted to the human resource assignment vector, and \({V_3}\) is converted to the operation sequence vector. The three-vector code is then decoded into a feasible and efficient surgery plan for MESS. To better understand this, a MESS instance is given in Table 5, which involves four elective patients, two ORs, 2 NOR beds, two surgeons, two anesthesiologists, and two nurses. Thereafter, we define \(ub= - lb=5\) and assume that the honey badger vectors are \({V_1}=\left[ { - 3.3,0.0, - 1.3, - 2.8,1.6, - 1.9,0.0, - 0.6,3.1,0.2,1.0,0.0} \right]\), \({V_2}=\left[ {1.6, - 1.4,0.8, - 2.5,0.0,1.6, - 0.6,1.0, - 0.5, - 2.0,0.2,3.2} \right]\), and \({V_3}=\left[ {1.6, - 0.8. - 4.5,4.8} \right]\).
Since the MESS is a discrete combinatorial optimization problem, a decoding mechanism needs to be created to convert the three-vector coding into a surgical scheduling scheme. The encoding and decoding process of the instance is described below.
-
(1)
Conversion of material resource (ORs and NOR beds) assignment.
For the conversion in the first part, a fixed ID for each surgical operation is given in accordance with the patient number and operation order within the patient61. The encoding of material resource assignment is illustrated in Fig. 3. After coding, the surgical operation can also be referred to by the fixed ID; for example, O21 corresponds to operation 4, as shown in Fig. 3. Then, the real number \(v\left( e \right) \in {V_1}\) is mapped to the integer \(x\left( e \right) \in \left[ {1,z\left( e \right)} \right]\) using Eq. (36).
where\(z\left( e \right)\)defines the number of ORs (NOR beds) selected for the eth individual, and round() is the function that returns the value of a number rounded upward to the nearest integer. The encoding of material resource assignment is illustrated in Fig. 3. A feasible route of material resource (ORs and NOR beds) assignment is: O11(NOR bed 1)- O12(OR 1) - O13(NOR bed 1) - O21(NOR bed 1) - O22(OR 2)- O23(NOR bed 1)- O31(NOR bed 2)- O32(OR 1)- O33(NOR bed 2)- O41(NOR bed 2)- O42(OR 2)- O43(NOR bed 2). The first number represents the corresponding surgical operation; the second one represents the material resource (ORs and NOR beds) selected for that operation. The numbers outside the brackets indicate the surgical operations, and the ones inside are the material resource (ORs and NOR beds).
-
(2)
Conversion of human resource (surgeons, anesthesiologists and nurses) assignment.
In the second part, a fixed ID for each surgical operation is given according to the patient number and the type of human resources). The encoding of human resource assignment is illustrated in Fig. 4. For instance, the anesthesiologist assigned to patient 1 has the same references as those assigned to patient 5. Assume\(z^{\prime}\left( a \right)\)is the number of human resources assigned to the ath individual. In addition, the real number \(v\left( a \right) \in {V_2}\) is mapped to the integer \(y\left( a \right) \in \left[ {1,z^{\prime}\left( a \right)} \right]\) using Eq. (37).
The encoding of human resource assignment is illustrated in Fig. 4. A feasible route of human resource (surgeons, anesthesiologists and nurses) assignment is: N1(Sur2, Ano1, Nur1)- N2(Sur1, Ano1, Nur1)- N3(Sur2, Ano2, Nur2)- N4(Sur1, Ano2, Nur2). The first number represents the corresponding surgical operation; the second one represents the material resource (ORs and NOR beds) selected for that operation. The numbers outside the brackets indicate the patient index, and the ones inside are the human resource (surgeons, anesthesiologists and nurses).
-
(3)
Conversion of surgical operation sequence.
In the third part, the largest position value (LPV) rule62 is used to construct a sorting rule in nonincreasing order of\({V_3}\). The encoding of the surgical operation sequence is illustrated in Fig. 5. A feasible route of surgical operation: N4- N1- N2- N3.
By decoding the honey badger vectors, the scheduling schemes for the MESS are obtained, as shown in Figs. 6 and 7. Figure 6 shows the assignment of the resulting material resources (ORs and NOR beds) after decoding, and Fig. 7 displays the resulting human resources assignment. In particular, the red dotted box in Fig. 7 indicates overtime for medical staffs.
Illustrative Gantt chart with ORs & NOR beds based on the example in Table 5.
An illustration of the Gantt chart with medical staff over time based on the example in Table 5.
Nash equilibrium-based fitness function
In the traditional multi-objective optimization problem, decision makers tend to find the most promising solutions using a Pareto optimal solution set, which contains a large number of non-dominated solutions. If a single non-dominated ranking is adopted, multiple schemes with the same level of non-dominated frontier are obtained. However, different schemes focus on objectives differently and it is hard for decision makers to make up reasonable selections20. To deal with this issue, the game-theory-based solution selection approach (e.g. Nash equilibrium) is proposed to produce a shortlist of Pareto optimal solutions so that decision makers can easily obtain the preferred results63. In addition, using the Nash equilibrium solution can effectively avoid emphasizing on a single objective, and ensure the optimality and fairness of each objective in the scheduling problem. In this study, the MESS is a three-objective optimization problem involving human and material constraints and multiple surgical stages. When solving the complex MESS problem, the HBA operator is simple, it easily falls into the local optima, and the balance between the exploration and exploitation stages is immature. This motivates us to design a Nash equilibrium-based fitness function (Fq) to evaluate the individuals in the population, thereby improving the performance of HBA. The formulation of Fq is shown in Eq. (38).
where the subscript q denotes the qth honey badger individual. Thus, in Eq. (38), for the qth individual, \({f_{iq}}\) denotes the completion time of surgery for patient i; \({f_{rq}}\), \({f_{r^{\prime}q}}\), and \({f_{r^{\prime\prime}q}}\) denote the overtime for surgeon r, anesthesiologist \(r^{\prime}\), and nurse \(r^{\prime\prime}\), respectively; and \({f_{hq}}\) denotes the total cost of medical resources. Equation (38) is used to find solutions that balance different stakeholder interests. That is, the payoff is greatest when patient i’s surgical completion time \({f_i}\) reaches its lower bound \({\underset{\raise0.3em\hbox{$\smash{\scriptscriptstyle-}$}}{f} _i}\); the payoff is greatest when overtime\({f_r}\),\({f_{r^{\prime}}}\),\({f_{r^{\prime\prime}}}\)of surgeon r, anesthesiologist\(r^{\prime}\)and nurse\(r^{\prime\prime}\) reaches the lower bound \({\underset{\raise0.3em\hbox{$\smash{\scriptscriptstyle-}$}}{f} _r}\),\({\underset{\raise0.3em\hbox{$\smash{\scriptscriptstyle-}$}}{f} _{r^{\prime}}}\)and \({\underset{\raise0.3em\hbox{$\smash{\scriptscriptstyle-}$}}{f} _{r^{\prime\prime}}}\), respectively; the payoff is greatest when the total cost of hospital\({f_i}\)reaches its lower bound:\({\underset{\raise0.3em\hbox{$\smash{\scriptscriptstyle-}$}}{f} _h}\). If an individual honey badger had a shorter surgery completion time, fewer overtime hours, and a lower cost per patient, then it would be assigned a greater fitness, and the individual would survive with a greater probability in the iteration. The Nash equilibrium-based fitness function can guide HBA to reach the global optimized solution and prevent the algorithm from falling into a local optimal optimum.
Computational experiments
In this section, we evaluate the performance of the proposed HBA-NE algorithm in solving the MESS problem. First, we analyze the archived data on stochastic surgery durations to obtain the required data for the input parameters. Second, based on previous studies, we select four comparative algorithms and set their parameter values. Third, we conduct a case study and algorithm performance comparison. Then, digital twin technology is applied in the virtual hospital operating room model simulation. Finally, retrospective testing verified that the proposed method performs better than in real-life practice.
Generation of the test problem
We use the data obtained from the First Affiliated Hospital of Hebei North University (FAH-HNU), a national university hospital in China. A total of 20 test instances are constructed in this paper. The problem sizes of the proposed test instances are given in Table 6, which are selected for parameter settings so that the small, middle and large scale instances are covered. All the cost parameters of the test set are summarized in Table 7.
It has been demonstrated that the empirical distribution derived from historical data is relatively accurate for describing future surgery durations64. On this basis, to obtain the required data for the input parameters, we analyze the archived data on stochastic surgery durations collected from the surgery booking department of the FAH-HNU in 2022. The surgery durations of 200 patients were sampled from the fitted distributions of the raw data (see Fig. 8) and tested using the QQ chart, as shown in Fig. 9.
We reviewed the historical durations of 22,074 elective surgery cases performed at the FAH-HNU over the year 2022 to create lognormal distribution models for each random variable. A regression model is then used to obtain the mean and standard deviation from these lognormal distributions. Thus, we conclude that the natural logarithms of the surgery durations are normally distributed, with a mean of a = 172.69 min and a standard deviation of b = 50.39 min to model the surgery duration54. The pre-operative, peri-operative, and post-operative surgery durations are shown in Table 8. Lognrnd(a,b) is a function used to generate lognormal random numbers with mean a and standard deviation b50.
Parameter settings
MESS is a complicated scheduling problem, involving multiple resource constraints (material resources and human resources) and multi-stage operations. Traditional meta-heuristic algorithms, such as Genetic Algorithm (GA) and Particle Swarm Optimization (PSO) are unable to solve large-scale MESS problems efficiently due to their weak local search capability and slow convergence speed. In contrast, HBA-NE is particularly suited for multi-resource scheduling under uncertain conditions. Because, the dynamic foraging and honey foraging behaviors of honey badgers enable the algorithm to maintain population diversity during the foraging process; by combining the Nash equilibrium-based fitness function with local search, the HBA-NE algorithm achieves a good balance between the exploration of the global search and the exploitation of the local search, so as to efficiently traverse the search space. To verify the effectiveness of the HBA-NE, it must be compared with the original HBA26 and several existing optimization algorithms, which are briefly described below:
The modified genetic algorithm (MGA) is a novel meta-heuristic algorithm obtained by improving the standard GA65. The MGA uses a mutation operator to make random changes to a single parent (mutation). Mutation helps the algorithm avoid the remaining local optima of the GA and recover lost genetic information.
The particle swarm arithmetic optimization (PSAO) is a multi-objective meta-heuristic algorithm proposed by Abdollahzadeh, et al.29. It is designed to expand the search space of PSO by combining the exploration and exploitation phases of the arithmetic optimization algorithm (AOA).
The wild horse optimizer (WHO) is a population-based algorithm developed by Naruei and Keynia27. The main inspiration of the WHO arises from the social life behavior of wild horses, such as grazing, mating, and domination. According to the WHO, the distributive power of the arithmetic operators enhances their global optimization ability.
In previous studies, the HBA, MGA, PSAO and WHO were shown to perform well in solving multi-objective scheduling problems. Thus, in this study, we consider them to be comparative algorithms. All comparative algorithms applied as references were implemented independently by our research team. Based on the relevant papers, we use the suggested control parameter settings for the comparative algorithms, as shown in Table 9.
The Nash equilibrium solution of multi-objective MESS problem is dominant, and traditional performance measures for non-dominated solutions are not applicable. Thus, the CPU time and mean ideal distance (MID) are used to measure the effectiveness of the proposed HBA-NE and competitive algorithms: HBA, MGA, PSAO and WHO. The MID measures the distance of the solutions generated by the algorithm from the ideal solution, and its mathematical expression can be referred with the details in the work of Li et al.14. Obviously, the smaller the MID, the better solution quality of the algorithm. In addition, we use the objective values of APT, AOT and TC to measure the average scheduling efficiency. The experiments were conducted on MATLAB R2022a and implemented on the computational environment with an Intel Core i7 (3.0 GHz), 16 GB of RAM, and a Windows 10 operating system. All the performance results are obtained based on the average of 20 independent runs.
Results and analysis
Algorithm performance comparison
In this section, a set of 20 test instances is used to compare the HBA-NE with the HBA, MGA, PSAO, and WHO scheduling algorithms. Each experiment is executed 20 times, and the final experimental results are derived from the average experimental results of the 20 runs. The condition of algorithm termination is the number of iterations. In this study, max_iter = 200 is set as the maximum number of iterations. The detailed algorithm performance comparison results are presented in Table 10 ~ 12, including the APT, AOT, TC, and quantitative metrics: CPU time, MID and improvement. The best values of the algorithms in each test instance are marked in bold. Some observations are summarized as follows:
-
1.
In terms of optimization objectives, the proposed HBA-NE outperforms HBA, MGA, PSAO, and the WHO in almost all test instances. In most cases, the solutions with minimum APT and TC can be achieved by HBA-NE. For the objective AOT, HBA-NE outperforms the other comparative algorithms in 16 instances. This indicates that the stochastic search process of the HBA-NE can effectively improve the search performance.
-
2.
In terms of CPU time, MID and improvement, although the HBA-NE integrates the HBA with a Nash equilibrium, it performs much faster, more efficiently than the HBA, MGA, PSAO, and WHO over all test instances. Based on the above analysis of the experimental results, it is clear that the ability of the HBA-NE to obtain the global optimal solution is superior to that of the other four comparative algorithms.
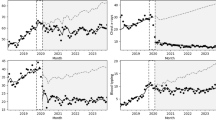
To visually compare the performance of these algorithms, Fig. 10 shows their MID trends based on the experimental results in Tables 10 and 12, where MID is used to consider convergence68. In Fig. 10, HBA-NE provides the minimum MID value for solving most of the test instances, and accordingly outperforms the other four scheduling algorithms. In addition, we select one test case no.8 including 40 elective patients, 8 ORs, 4 NOR beds, 10 surgeons, 8 anesthesiologists and 18 nurses, and plot Fig. 11 to test the convergence of the competitive algorithms, which is shown in the form of convergence curves of objectives APT, AOT, and TC. It can be seen that the solution generated by HBA-NE is super to the HGS, PSAO and MGA algorithms, and the Pareto front obtained by HBA-NE dominates the other Pareto fronts. The best solution obtained in 120 iterations of HBA-NE is even better than the solutions found by other algorithms in 200 iterations. In contrast, MGA and PSAO exhibit poor convergence abilities and converge within 150 iterations, WHO is easily trapped into local optimum. It can also be observed that the curves of PSAO, MGA, and HBA fluctuate greatly, but the curve of HBA-NE is relatively stable, which further proves the strong convergence and stability of HBA-NE.
In summary, the main advantage of the HBA-NE over other well-known metaheuristic algorithms (e.g., MGA, PSAO, WHO) is that its algorithmic structure is simpler and easier to implement. Compared to the HBA, the HBA-NE offers far greater performance and reliability in solving the MESS problem for all test instances, which indicates that the Nash equilibrium strategy can effectively improve the global search performance of meta-heuristic algorithm. In particular, hybridization of the Nash equilibrium-based fitness function with a local search allows the algorithm to achieve a good balance between the exploration of the global search and the exploitation of the local search. Moreover, the suggested surgical scheduling scheme obtained by the HBA-NE provides hospital managers with more detailed information on the results, which can help guide the planning and control of multiple medical resources.
Case study
In this subsection, the performance of HBA-NE is verified through a test case in the FAH-HNU hospital. The case study is presented in detail as follows. In the one-day surgery plan, 25 patients need to undergo surgery. The medical resources available for assignment included material resources (five ORs and three NOR beds) and human resources (five surgeons, five anesthesiologists, and seven nurses). Meanwhile, the salary costs of medical staff with different levels are considered in Table 7.
The optimal surgical scheduling scheme obtained by the HBA-NE after 200-run interactions in one experiment of test instance no.2 is shown in Figs. 12 and 13. Figure 12 reflects the Gantt chart of the surgical operations that each NOR or NOR bed needs to perform, and Fig. 13 shows the Gantt chart of the surgical operations that each medical staff needs to perform. Specifically, rectangles with different colors and numeric symbols indicate the different surgical operation strategies used for the patient. The first number on the rectangle denotes the patient index, and the second number denotes the operation stage.
For example, in Fig. 12, the upper-left purple rectangle with (5.2. S3. A4. N4) indicates that in OR4, operation stage II for patient 5 is treated by surgeon 3, anesthesiologist 4, and nurse 4. In Fig. 13, the brown rectangle corresponding to Sur2 with (11.2. O2) indicates that operation stage II for patient 11 was treated by surgeon 2 and operated on in OR 2; the purple rectangle corresponding to Ano 4 with (5.2. O4) indicates that operation stage II for patient 5 was treated by anesthesiologist 4 and operated on in OR 4; the yellow rectangle corresponding to Nur 4 with (8.1. B3) indicates that operation stage I for patient 8 was treated by nurse 4 and performed in NOR bed 3. As shown in Figs. 12 and 13, there is no overlap between different surgical operations on the same patient, and the next operation is performed only after the previous operation has been completed. The same medical staff member is not assigned to more than one OR or NOR bed simultaneously. Therefore, the scheduling scheme derived using HBA-NE is reasonable. As calculated from Fig. 12, the average recovery completion time for 25 patients is 390.241. Similarly, from Fig. 13, the average overtime of medical staffs is 2.956. The completion time of the scheduling scheme is 738.059 and the final cost medical resources is 6363.969. After normalization and dimensionless processing (Luan et al., 2023), the payoffs obtained for patients, medical staffs and hospital manager are obtained are 862, 263 and 956, respectively.
Virtual hospital operating room model simulation
Digital twin (DT) provides a two-way interaction for processing different data sources in real time and transforms information into valuable knowledge. In manufacturing environments, the prevalence of human-machine collaborative ecosystems supported by DT will eventually grow as workers’ digital skills improve. Therefore, the development of human-machine interfaces for collaborative environments is an application advantage of DT. For example, SAIC Volkswagen has established a DT-based production system to realize production process monitoring and exception handling. The system collects product and equipment data from each workshop, analyzes and processes them to form a factory-level production data report and organically combines them with the three-dimensional model of the factory to display the production status of each workshop in real time. By building a DT model of the production line, enterprises can simulate the operation of production line in real time and dynamically adjust the production plan to optimize production efficiency and reduce resource waste. DT can test different production scheduling solutions in a virtual environment to help enterprises develop the optimal production strategies and improve overall resource utilization. Due to the similarity between medical systems and production systems, some researchers have applied models and methods from production to the healthcare decision making14,21. In fact, the surgical scheduling system is analogous to the SAIC Volkswagen production scheduling system, e.g., the ORs, surgeons and patients are corresponding to the job shops, workers and workpieces. However, in the medical field, there is still a gap between the optimal surgical scheduling solution and actual hospital operations. The application of DT in intelligent hospitals can narrow this gap69. In the DT-based smart hospital platform, the operating status and task progress of surgeries in real hospitals can be accurately mapped to virtual hospitals. In this way, physical and virtual hospitals can dynamically interact and respond in real time as events occur.
Compared with traditional numerical experiments, simulation experiments based on DT models involve complex human-machine interactions related to surgical scheduling processes and involve intelligent medical data. To this end, a virtual hospital simulation model is needed to evaluate the proposed scheduling schemes for the MESS problem. Therefore, this study applied the surgical simulation system developed by our research team to build a DT-based physical-virtual hospital surgery simulation model, as shown in Fig. 14. In a virtual hospital, a surgical simulation model is established based on physical hospital data (e.g., ORs, NOR beds, surgeons, anesthesiologists, nurses, OR layout information). Using these medical resource data, the surgical scheduling scheme is obtained and simulated by DT-based surgical scheduling models and the proposed algorithm. After verification, the final scheduling strategy is fed back to the physical hospital for execution.
The optimal surgical scheduling model based on digital twin technology was realized by AnyLogic Professional 8.8.2. In the virtual hospital, the surgical scheduling model executes the scheduling plan, and the validated scheduling plan is fed back to the physical hospital. Test instance no. 9 is used to construct the simulation model. The surgical procedure used for patients at the virtual hospital is displayed in Fig. 15. The simulation processes with the virtual two-dimensional (2D) and three-dimensional (3D) models are shown in Figs. 16 and 17, respectively, in which four areas are considered: the OR region, NOR region, transition area, and polluted area. By building the 2D logical and 3D visualization models of the virtual hospital, the process of executing surgical scheduling can be visualized so that managers can easily make decisions and take action.
The experimental results show that, compared with traditional algorithms, the digital twin can visually run and verify the surgery process at a virtual hospital. Figure 18 depicts the execution results of a virtual simulation model based on the no. 9 test instance. The values of APT, AOT, and CT obtained by the DT simulation surgical scheduling model are 476.79, 1.45, and 10,372.46, respectively. To further verify the advantages of the proposed method, scheduling results without DT and with DT are compared in terms of APT, AOT and TC, as shown in Table 13. The case study shows that the proposed method can reduce the APT, AOT and TC by 12.29%, 31.93% and 1.28%, respectively; increase the average utility rate of material resources such as ORs and NOR beds by 20.46% and 7.75%, respectively; increase the average utility rate of human resources such as surgeons, anesthesiologists and nurses by 32.62%, 20.46% and 27.61% respectively. This indicates that the MESS scheme based on the digital twin has high veracity, practicality, and maneuverability. DT-driven virtual verification can quickly and easily forecast and verify surgical scheduling and medical resource utilization.
Retrospective testing
To further validate the effectiveness of the HBA-NE, the proposed method is retrospectively tested. Elective patients who underwent surgery at our partner hospital, FAH-HNU, between January 2022 and December 2022 were retrospectively enrolled in the study. Overall, 15,890 surgery samples were derived from previously submitted diagnostic case submissions from five departments: the Hepatobiliary Surgery Department, Breast Surgery Department, Gastrointestinal Surgery Department, Thoracic and Cardiovascular Surgery Department, and Urologic Surgery Department. In the retrospective test, we focused on three objectives: patient recovery completion time, medical staff overtime, and total cost. To more intuitively show the results obtained by HBA-NE in APT, AOT, and CT, five test instances (no. 2, no. 9, no. 12, no. 16, no. 20) are selected, and the results are shown in Table 14. Table 14 displays the real-life practice values (obtained by manual scheduling) and the optimal values (obtained by the HBA-NE) for APT, AOT, and TC along with the percentage improvement. Compared with those of the HBA-NE and manual scheduling, the improvements in APT, AOT and TC obtained by the HBA-NE are significant. In particular, for instances no. 2, no. 9, no. 12, no. 16, and no. 20, the improvement in APT is clear, with values reduced by 37.36%, 37.63%, 43.33%, 36.60%, and 26.68%, respectively; the improvement in AOT fluctuates widely, with values decreasing by 90.83%, 83.96%, 13.02%, 8.77%, and 13.69%, respectively; and the improvement in TC is slight, with values decreasing by 7.37%, 9.14%, 13.02%, 7.75%, and 5.41%, respectively. Furthermore, the proposed HBA-NE successfully improves APT by 35.52%, AOT by 42.05%, and TC by 7.47% on average in hospital FAH-HNU.
To show scalability and versatility of our approach, the evaluation is expanded by applying HBA-NE in case studies across hospitals of varying sizes. We perform the retrospective testing for other two hospitals in China. The problem sizes of the proposed test instances are given in Table 15, where no.21 ~ no.25 correspond to hospital A (The Fourth Hospital of Hebei Medical University), and no.26 ~ no.30 correspond to hospital B (Tianjin Medical University General Hospital). All the cost parameters of the test set are summarized in Table 16.
*¥represents the Chinese Yuan.
Table 17 displays the results of HBA-NE retrospective testing for the MESS in hospital A. For the improvement in APT, the values are reduced by 51.39%, 40.09%, 39.85%, 38.26% and 37.08%, respectively; for the improvement in AOT, the values are decreasing by 100%, 94.08%, 57.47%, 26.91% and 30.09%, respectively; and for the improvement in TC, the values are decreasing by 8.61%, 10.52%, 9.93%, 10.14% and 9.87%, respectively. Furthermore, the proposed HBA-NE successfully improves APT by 41.53%, AOT by 61.71%, and TC by 9.61% on average in hospital A.
Table 18 displays the results of HBA-NE retrospective testing for the MESS in hospital B. For the improvement in APT, the values are reduced by 36.29%, 33.83%, 33.18% and 30.98%, respectively; for the improvement in AOT, the values are decreasing by 64.07%, 16.95%, 5.04%, 2.29% and 4.92%, respectively; for the improvement in TC, the values are decreasing by 7.37%, 13.14%, 12.03%, 10.05%, 9.52% and 7.94%, respectively. Furthermore, the proposed HBA-NE successfully improves APT by 34.47%, AOT by 18.66%, and TC by 10.53on average in hospital B.
Conclusions and management insights
Conclusions
In this study, we address a multi-resource elective surgical scheduling (MESS) problem in which the availability of material resources (i.e., ORs, NOR beds) and human resources (i.e., surgeons, anesthesiologists, nurses) is considered when generating surgery schedules. A mixed integer programming model is developed to minimize patient treatment time, medical staff overtime, and total cost. Due to the characteristics of multi-objective optimization problem, a game theory approach is introduced to balance different objectives to ensure efficiency and fairness among multiple objectives. A honey badger algorithm (HBA) based on the Nash equilibrium (HBA-NE) is proposed to arrange the surgical processing sequence of patients. The proposed algorithm is numerically tested and verified using real data collected at the Department of General Surgery of a National University Hospital in China. The numerical results show that the HBA-NE yields much better non-dominated solutions for solving the MESS than do the other algorithms, such as the HBA, MGA, PSAO and WHO. The HBA-NE clearly exhibits superior performance both in terms of solution quality and computation time.
In addition, to reduce the difference between the surgical scheduling model and the actual physical model, a digital twin-driven MESS is proposed. It implements an optimal surgical scheduling model in virtual hospitals and builds a smart hospital visualization platform for hospitals. The main contribution of the current study is the creation of a new surgical scheduling architecture based on existing advanced DT technology. The process of DT surgical scheduling can replace traditional manual scheduling to ensure traceability from surgery plans to medical resources, avoiding the confusion, omission, and complexity of manual scheduling. We hope that the results of the current research will resolve the surgery scheduling problem and help hospitals achieve high-quality sustainable improvements through intelligence and digitalization.
Managerial insights
In practice, our surgical scheduling solutions determine the arrangement of ORs/NOR beds and medical staff in the hospital systemic management mode and can serve hospital managers by providing accurate surgical scheduling plans, i.e., the assignment of surgical operations and medical staffs, sequence of operations, and selection of ORs/NOR beds, surgeons, anesthesiologists, and nurses. Moreover, they also help to simultaneously balance the goals of surgical time, physician workload, and ORs/NOR beds workload in real-world hospital management, thereby improving productivity and medical resource utilization. In addition, for large-scale and complex surgery scheduling problems, the solution time of ordinary methods is too long. To compensate for this shortcoming in practical applications, we propose the HBA-NE for the research problem, which can satisfy the high demands of scheduling in operation room management. The HBA-NE algorithm is highly customized for the specific MESS problem in this paper. In real-world surgical resource management, we can study the algorithm in more detail to further evaluate its superiority. Considering the potential challenges that can be encountered when implementing HBA-NE and Dt-based scheduling in real hospitals, staff training related to data integration and computational requirements is necessary.
Limitations and future research
This paper has several limitations and avenues for future research. First, the studied MESS problem only considers the allocation and utilization of medical resources, ignoring the influence of human factors, such as medical staff fatigue and patient deterioration, on surgical scheduling. Second, the study focused on elective surgeries, which are scheduled ahead of time. However, in reality, dynamic events such as equipment failure, surgical cancelation, and emergency patient situations can cause deviations in the execution of surgical scheduling and can thus affect efficiency. In future research, the fatigue level of medical staff and the effect of patient deterioration could be taken into account in the MESS problem. In addition, future studies may consider more specific aspects of surgery scheduling, such as dealing with canceled surgeries or accommodating emergency situations. Through the combination of digital twin and surgical big data, hospitals’ physical and virtual spaces can be further integrated, thus greatly enabling complex dynamic surgical scheduling. Notably, during the last decade, DT has improved, particularly in the advanced manufacturing industry. In smart hospitals, the application of DT in surgical scheduling is still in its infancy, and the application value of DT needs to be further explored.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Dai, Z., Perera, S. C., Wang, J. J., Mangla, S. K. & Li, G. Elective surgery scheduling under uncertainty in demand for intensive care unit and inpatient beds during epidemic outbreaks. Comput. Ind. Eng. 176, 108893 (2023).
Han, Y., Li, Y., Li, Y., Yang, B. & Cao, L. Digital twinning for smart hospital operations: Framework and proof of concept. Technol. Soc. 74, 102317 (2023).
Abdulkareem, K. H. et al. Realizing an effective COVID-19 diagnosis system based on machine learning and IoT in Smart Hospital Environment. IEEE Internet Things J. 8, 15919–15928 (2021).
Bandi, C. & Gupta, D. Operating room staffing and scheduling. Manuf. Serv. Oper. Manag. 22, 958–974 (2020).
Naderi, B. et al. Increased Surgical Capacity without additional resources: generalized operating Room Planning and Scheduling. Prod. Oper. Manag. 30, 2608–2635 (2021).
Thomas Schneider, A. J., van Theresia, J., Carlier, M. & Hans, E. W. Scheduling surgery groups considering multiple downstream resources. Eur. J. Oper. Res. 282, 741–752 (2020).
Varmazyar, M., Akhavan-Tabatabaei, R., Salmasi, N. & Modarres, M. Operating room scheduling problem under uncertainty: application of continuous phase-type distributions. IISE Trans. 52, 216–235 (2020).
Shehadeh, K. S. & Padman, R. Stochastic optimization approaches for elective surgery scheduling with downstream capacity constraints: models, challenges, and opportunities. Comput. Oper. Res. 137, 105523 (2022).
Bovim, T. R., Abdullahu, A., Andersson, H. & Gullhav, A. N. Integrated master surgery and outpatient clinic scheduling. Oper. Res. Health Care. 35, 100358 (2022).
Çelik, B., Gul, S. & Çelik, M. A stochastic programming approach to surgery scheduling under parallel processing principle. Omega 115, 102799 (2023).
Hamid, M. et al. Operating room scheduling by considering the decision-making styles of surgical team members: a comprehensive approach. Comput. Oper. Res. 108, 166–181 (2019).
Vali-Siar, M. M., Gholami, S. & Ramezanian, R. Multi-period and multi-resource operating room scheduling under uncertainty: a case study. Comput. Ind. Eng. 126, 549–568 (2018).
Bargetto, R., Garaix, T. & Xie, X. A branch-and-price-and-cut algorithm for operating room scheduling under human resource constraints. Comput. Oper. Res. 152, 106136 (2023).
Li, Z., Yan, J. & Xue, J. Multi-objective fuzzy surgical scheduling during post-disaster with Nash equilibrium. Expert Syst. Appl. 238, 121945 (2024).
Atay, A., Calleja, P. & Soteras, S. Open shop scheduling games. Eur. J. Oper. Res. 295, 12–21 (2021).
Tian, S., Wang, T., Zhang, L. & Wu, X. The internet of things enabled manufacturing enterprise information system design and shop floor dynamic scheduling optimisation. Enterp. Inf. Syst. 14, 1238–1263 (2020).
Xiao, J., Zhang, W., Zhang, S. & Zhuang, X. Game theory–based multi-task scheduling in cloud manufacturing using an extended biogeography-based optimization algorithm. Concurr Eng. Res. Appl. 27, 314–330 (2019).
Renna, P., Thürer, M. & Stevenson, M. J. I.J.o.I.E.C. A game theory model based on Gale-Shapley for dual-resource constrained (DRC) flexible job shop scheduling. Int. J. Ind. Eng. Comput. 11, 173–184 (2020).
Belabid, J., Aqil, S. & Allali, K. Nash equilibrium inspired greedy search for solving flow shop scheduling problems. Appl. Intell. 53, 13415–13431 (2023).
Wei, L., He, J., Guo, Z. & Hu, Z. A multi-objective migrating birds optimization algorithm based on game theory for dynamic flexible job shop scheduling problem. Expert Syst. Appl. 227, 120268 (2023).
Wang, J. J., Dai, Z., Chang, A. C. & Shi, J. J. Surgical scheduling by fuzzy model considering inpatient beds shortage under uncertain surgery durations. Ann. Oper. Res. 315, 463–505 (2022).
Li, Z. & Chen, Y. Minimizing the makespan and carbon emissions in the green flexible job shop scheduling problem with learning effects. Sci. Rep. 13, 6369 (2023).
Yang, Y. & Li, X. A knowledge-driven constructive heuristic algorithm for the distributed assembly blocking flow shop scheduling problem. Expert Syst. Appl. 202, 117269 (2022).
Wang, G. G., Deb, S. & Cui, Z. Monarch butterfly optimization. Neural Comput. Appl. 31, 1995–2014 (2019).
Yang, Y., Chen, H., Heidari, A. A. & Gandomi, A. H. Hunger games search: visions, conception, implementation, deep analysis, perspectives, and towards performance shifts. Expert Syst. Appl. 177, 114864 (2021).
Hashim, F. A., Houssein, E. H., Hussain, K., Mabrouk, M. S. & Al-Atabany, W. Honey Badger Algorithm: New metaheuristic algorithm for solving optimization problems. Math. Comput. Simul. 192, 84–110 (2022).
Naruei, I. & Keynia, F. Wild horse optimizer: a new meta-heuristic algorithm for solving engineering optimization problems. Eng. Comput. 38, 3025–3056 (2022).
Abualigah, L., Diabat, A., Mirjalili, S., Abd Elaziz, M. & Gandomi, A. H. The arithmetic optimization algorithm. Comput. Methods Appl. Mech. Eng. 376, 113609 (2021).
Abdollahzadeh, B., Gharehchopogh, F. S. & Mirjalili, S. African vultures optimization algorithm: a new nature-inspired metaheuristic algorithm for global optimization problems. Comput. Ind. Eng. 158, 107408 (2021).
Hu, G., Zhong, J., Wei, G. SaCHBA_PDN: Modified honey badger algorithm with multi-strategy for UAV path planning. Expert Syst. Appl. 223, 119941 (2023).
Abasi, A. K., Aloqaily, M. & Guizani, M. Optimization of CNN using modified Honey Badger Algorithm for Sleep Apnea detection. Expert Syst. Appl. 229, 120484 (2023).
Fathy, A., Rezk, H., Ferahtia, S., Ghoniem, R. & Alkanhel, R. An efficient honey badger algorithm for scheduling the microgrid energy management. Energy Rep. 9, 2058–2074 (2023).
Yang, X. et al. Optimal configuration of improved integrated energy system based on stepped carbon penalty response and improved power to gas. Energy 263, 125985 (2023).
Grieves, M. Digital Twin: Manufacturing Excellence through Virtual Factory Replication. 1–7 (2015).
Yan, Q., Wang, H. & Wu, F. Digital twin-enabled dynamic scheduling with preventive maintenance using a double-layer Q-learning algorithm. Comput. Oper. Res. 144, 105823 (2022).
Croatti, A., Gabellini, M., Montagna, S. & Ricci, A. On the Integration of Agents and Digital Twins in Healthcare. J. Med. Syst. 44, 161 (2020).
Elayan, H., Aloqaily, M. & Guizani, M. Digital Twin for Intelligent Context-Aware IoT Healthcare systems. IEEE Internet Things J. 8, 16749–16757 (2021).
Fischer, G. S. et al. Using internet of things and data prediction for elastic management of human resources in smart hospitals. Eng. Appl. Artif. Intell. 87, 103285 (2020).
Rahman, M. Z. et al. An intelligent health monitoring and diagnosis system based on the internet of things and fuzzy logic for cardiac arrhythmia COVID-19 patients. Comput. Biol. Med. 154, 106583 (2023).
Zhang, J. et al. Intelligent speech technologies for transcription, disease diagnosis, and medical equipment interactive control in smart hospitals: a review. Comput. Biol. Med. 153, 106517 (2023).
Zheng, S., Zhang, F. & Sun, Q. Medical image detection and azithromycin in the treatment of pelvic inflammation based on intelligent hospital system. Microprocess Microsyst. 81, 103664 (2021).
Liang, Y. & Zhao, L. Intelligent Hospital Appointment System Based on Health Data Bank. Procedia Comput. Sci. 159, 1880–1889 (2019).
Ding, Y., Park, E., Nagarajan, M. & Grafstein, E. Patient prioritization in Emergency Department Triage Systems: an empirical study of the Canadian triage and acuity scale (CTAS). Manuf. Serv. Oper. Manag. 21, 723–741 (2019).
Rodrigues, L., Gonçalves, I., Fé, I., Endo, P. & Silva, F. A. Performance and availability evaluation of an smart hospital architecture. Computing 103, 1–35 (2021).
Uslu, B. Ç., Okay, E. & Dursun, E. Analysis of factors affecting IoT-based smart hospital design. J. Cloud Comput. 9, 67 (2020).
Liu, Y. et al. A novel cloud-based Framework for the Elderly Healthcare Services Using Digital Twin. IEEE Access. 7, 49088–49101 (2019).
Li, Z. & Chen, Y. Dynamic scheduling of multi-memory process flexible job shop problem based on digital twin. Comput. Ind. Eng. 183, 109498 (2023).
Breuer, D. J., Lahrichi, N., Clark, D. E. & Benneyan, J. C. Robust combined operating room planning and personnel scheduling under uncertainty. Oper. Res. Health Care. 27, 100276 (2020).
Belkhamsa, M., Jarboui, B. & Masmoudi, M. Two metaheuristics for solving no-wait operating room surgery scheduling problem under various resource constraints. Comput. Ind. Eng. 126, 494–506 (2018).
Wang, K., Qin, H., Huang, Y., Luo, M. & Zhou, L. Surgery scheduling in outpatient procedure centre with re-entrant patient flow and fuzzy service times. Omega 102, 102350 (2021).
Latorre-Núñez, G. et al. Scheduling operating rooms with consideration of all resources, post anesthesia beds and emergency surgeries. Comput. Ind. Eng. 97, 248–257 (2016).
Xiang, W., Yin, J. & Lim, G. An ant colony optimization approach for solving an operating room surgery scheduling problem. Comput. Ind. Eng. 85, 335–345 (2015).
Hsu, P. Y., Lo, S. H., Hwang, H. G. & Lin, B. M. T. Scheduling of Anaesthesia Operations in operating rooms. Healthcare 9, 640 (2021).
Mazloumian, M., Fazle Baki, M. & Ahmadi, M. A robust multiobjective integrated master surgery schedule and surgical case assignment model at a publicly funded hospital. Comput. Ind. Eng. 163, 107826 (2022).
Neufeld, J. S., Schulz, S. & Buscher, U. A systematic review of multi-objective hybrid flow shop scheduling. Eur. J. Oper. Res. 309, 1–23 (2023).
Zhang, Y., Wang, J. & Liu, Y. Game theory based real-time multi-objective flexible job shop scheduling considering environmental impact. J. Clean. Prod. 167, 665–679 (2017).
Kapner, D. J. et al. Tests of the Gravitational Inverse-Square Law below the dark-energy length scale. Phys. Rev. Lett. 98, 021101 (2007).
Majumdar, P., Mitra, S. & Bhattacharya, D. Honey Badger algorithm using lens opposition based learning and local search algorithm. Evol. Syst., 1–26 (2023).
Nassef, A. M., Houssein, E. H., Helmy, B. E. & Rezk, H. Modified honey badger algorithm based global MPPT for triple-junction solar photovoltaic system under partial shading condition and global optimization. Energy 254, 124363 (2022).
Nagarajan, S., Kayalvizhi, S., Subhashini, R. & Anitha, V. Hybrid honey badger-world cup algorithm-based deep learning for malicious intrusion detection in industrial control systems. Comput. Ind. Eng. 180, 109166 (2023).
Yuan, Y., Xu, H. & Yang, J. A hybrid harmony search algorithm for the flexible job shop scheduling problem. Appl. Soft Comput. 13, 3259–3272 (2013).
Wang, L. & Pan, Q. K. Fatih Tasgetiren, M. minimizing the total flow time in a flow shop with blocking by using hybrid harmony search algorithms. Expert Syst. Appl. 37, 7929–7936 (2010).
Petchrompo, S., Coit, D. W., Brintrup, A., Wannakrairot, A. & Parlikad, A. K. A review of Pareto pruning methods for multi-objective optimization. Comput. Ind. Eng. 167, 108022 (2022).
Zhang, Y., Wang, Y., Tang, J. & Lim, A. Mitigating overtime risk in tactical surgical scheduling. Omega 93, 102024 (2020).
Branda, A., Castellano, D., Guizzi, G. & Popolo, V. Metaheuristics for the flow shop scheduling problem with maintenance activities integrated. Comput. Ind. Eng. 151, 106989 (2021).
Tan, W., Yuan, X., Wang, J. & Zhang, X. A fatigue-conscious dual resource constrained flexible job shop scheduling problem by enhanced NSGA-II: an application from casting workshop. Comput. Ind. Eng. 160, 107557 (2021).
Duan, J. & Wang, J. Robust scheduling for flexible machining job shop subject to machine breakdowns and new job arrivals considering system reusability and task recurrence. Expert Syst. Appl. 203, 117489 (2022).
Maghsoudlou, H., Afshar-Nadjafi, B. & Niaki, S. T. A. A multi-objective invasive weeds optimization algorithm for solving multi-skill multi-mode resource constrained project scheduling problem. Comput. Chem. Eng. 88, 157–169 (2016).
Zhang, J. et al. Bi-level dynamic scheduling architecture based on service unit digital twin agents. J. Manuf. Syst. 60, 59–79 (2021).
Acknowledgements
This work was sponsored by National Natural Science Foundation of China NSFC (grant numbers: 72002153, 41971249). We would like to give our great appreciation to all the reviewers and editors who contributed this study.
Author information
Authors and Affiliations
Contributions
Jun Xue, Zhi Li and Shuangli Zhang wrote the main manuscript text, Shuangli Zhang prepared Figs. 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17 and 18; Tables 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17 and 18. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical statement
All methods were carried out in accordance with relevant guidelines and regulations. All experimental protocols were approved by the First Affiliated Hospital of Hebei North University. The informed consent was obtained from all subjects and/or their legal guardian(s).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xue, J., Li, Z. & Zhang, S. Multi-resource constrained elective surgical scheduling with Nash equilibrium toward smart hospitals. Sci Rep 15, 3946 (2025). https://doi.org/10.1038/s41598-025-87867-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-87867-y