Abstract
Dental simulation head model laboratories are crucial for clinical simulation training for stomatological students, yet the maintenance of their dental unit waterlines (DUWLs) has been overlooked. This study investigated water contamination in DUWLs within these laboratories and proposed solutions. Water samples were collected from 12 dental chairs in three laboratories at three time points: the beginning, middle, and end of the semester. At the start of the semester, severe contamination was observed, with colony counts of 11,586\(\:\pm\:\)1715 CFU/ml for high-speed handpieces and 5375\(\:\pm\:\)874 CFU/ml for three ways syringes. As the semester progressed, colony counts gradually decreased but remained above clinical thresholds. Both 20 mg/L organochlorine disinfectant and 20 mg/L chlorine dioxide were effective in reducing bacterial contamination below standard ranges three days post-disinfection. Microbial diversity analysis revealed Proteobacteria and Bacteroidota as the dominant bacterial phyla, with Ascomycota as the dominant fungal phylum. Potentially pathogenic bacteria such as Pseudomonas, Burkholderia-Caballeronia-Paraburkholderia, Ralstonia, Mycobacterium, Legionella, Paenibacillus, Streptomyces, Acinetobacter, and Prevotella, as well as fungi like Fusarium and Penicillium, were detected. Therefore, urgent attention is needed to address DUWL contamination in dental laboratories, and it is recommended to disinfect DUWLs using either 20 mg/L organochlorine disinfectant or 20 mg/L chlorine dioxide every three days.
Similar content being viewed by others
Background
Dental simulation head model laboratories constitute a vital role in stomatological education, with the primitive objective of cultivating the clinical proficiency of dental students. In the laboratory, students engage in the practice of various dental treatments such as tooth preparation, restoration and endodontic therapy on simulation heads, which utilize dental unit waterlines (DUWLs). DUWLs are composed of narrow and elongated interconnected tubes and linked to high-speed handpieces and three ways syringes. The combination of factors such as small tube diameters, high surface-to-volume ratios, rough surface, and slow water flow rates, facilitate the formation and residence of biofilms on the inner walls of the tubes1,2. Furthermore, debris, microorganisms, and chemical reagents generated during students’ practice may enter and deposit in the waterlines, leading to water quality deterioration and an increased risk of cross-infection, thereby affecting the health of both teachers and students.
Nevertheless, the disinfection and maintenance of DUWLs in dental simulation head model laboratories have been overlooked for an extended period. The majority of current research focuses on the DUWLs in clinical settings, including contamination levels, bacterial species, harm to patients, and sterilization management (disinfectant types, concentrations, and disinfection frequencies)1,3. Various regulations have been formulated to control clinical DUWLs contamination. In 1996, the American Dental Association (ADA) set a limit of ≤ 200 CFU/mL on the aerobic mesophilic heterotrophic bacteria in the output water of the dental unit4. In 2003, the US Centers for Disease Control and Prevention (CDC) recommended that the bacteria in dental unit water should not be less than 500 CFU/mL5. Moreover, in some EU countries, the drinking water standard of < 100 CFU/ml is referenced6. And in 2024, China also clarified in the standard for prevention and control of healthcare associated infection in dental outpatient department and clinic that the water from DUWLs should meet the drinking water standard (< 100 CFU/ml)7. The primary sources of contamination in clinics are bacteria from tap water and patients, in addition to the initial contamination of DUWLs among new and never used dental chairs8. Currently, medical regulatory authorities have established the testing of DUWLs in clinics as a standard regulatory requirement9. However, the contamination of DUWLs in dental simulation head model laboratories remains an overlooked area, with no pertinent reports to date.
This study analyzed the contamination level of DUWLs periodically through a semester-long investigation, and assessed the disinfection effects of two commonly used disinfectants (20 mg/L organochlorine disinfectant and 20 mg/L chlorine dioxide). Additionally, we utilized high-throughput sequencing technology to identify the microbial communities. This study seeks to elevate awareness regarding the serious contamination of DUWLs in dental simulation head model laboratories and proposes viable strategies for mitigating such contamination.
Methods
Study subjects
Three oral simulation head model laboratories from the School of Stomatology, Zhejiang Chinese Medical University were selected, with each laboratory featuring identically arranged DUWLs (Fig. 1a). The three laboratories were simultaneously opened to three classes in the same grade during one semester, with consistent usage frequency and duration in order to minimize sample error among the three laboratories. All the laboratories had not undergone systematic DUWL disinfection or maintenance procedures before. For each laboratory we chose 12 simple dental chairs (SDCs) (NISSIN NS-1000, China) (marked in blue on Fig. 1a) equipped with oral treatment devices including high-speed handpieces and three ways syringes. The DUWLs in the three laboratories were immediately disinfected out of biosafety concerns after sampling. The municipal tap water used in the laboratories met the microbial standards outlined in the Chinese national standard (GB/T 5750.12–2006). Tap water tests were conducted both before and after the study, with the results confirming compliance with the Chinese national standard.
Study design. (a) shows the oral simulation head model laboratory waterway system. The chosen subjects are marked in blue. (b) depicts the cross-section of waterlines. (c) illustrates the experimental protocol for assessing water sample contamination levels and disinfection efficacy, as well as the procedure for performing biodiversity analysis on the biofilm formed within the water pipe.
Water sample collection
Water samples were collected from three laboratories at the beginning (Laboratory A), middle (Laboratory B), and end (Laboratory C) of the semester (Fig. 1). For each time point, water samples were collected from the waterlines of one high-speed handpiece and one three ways syringe on each dental chair, with two samples collected from each waterline as duplicates. For the three ways syringe waterline, we removed the replaceable jet heads of the syringe, pressed the water spray button for 30 s, then wiped and sterilized the connector with 75% ethanol and collected 10 ml of water from the syringe using a sterile sampling bottle. For the high-speed handpiece waterline, the handpiece was not installed, we stepped back the metal cap, then rinsed, wiped and sampled as described above. All water samples were stored in a 4 °C refrigerator within 30 min after collection and inoculated within 6 h.
Disinfection
250 mg/tablet organic chlorine effervescent tablets (Health Essence, China) and 100 mg/tablet chlorine dioxide effervescent tablets (Basteur, China) were prepared respectively with purified water to form chlorine-containing disinfectants at a concentration of 20 mg/L, which were prepared and used immediately. The 12 SDCs in laboratory B were randomly divided into two groups, with one group disinfected using 20 mg/L organochlorine disinfectant and the other using 20 mg/L chlorine dioxide disinfectant. First, the dental instruments attached to the SDC were removed, 1 L of disinfectant was filled in a separate water reservoir, followed by continuous drainage for 2 min, static placement for 20 min, and finally rinsing with 1 L of tap water. Water samples were collected before disinfection, immediately after disinfection, and 3 and 7 days after disinfection.
Bacterial culture
100 µl of each water sample was inoculated onto a nutrient agar plate. The plates were incubated at 37 °C for 48 h in an incubator. Viable bacterial counts were calculated as CFU/ml, and a colony count exceeding 100 CFU/ml was considered contaminated.
Statistical analysis
Statistical analysis was carried out using SPSS 24.0. The Shapiro-Wilk test was used to assess the normality of the experimental data, and the F-test with P > 0.05 was used to verify the homogeneity of variances. Independent T-tests were conducted to analyze the contamination levels of the high-speed handpiece and three ways syringe waterlines at different time points. The contamination rate was calculated as follows:
Paired T-tests were used to statistically analyze the bacterial colony counts in water samples before and after disinfection to assess the disinfection effect. Independent T-tests were used to analyze the contamination levels of the high-speed handpiece and three ways syringe waterlines. A P-value < 0.05 was considered statistically significant.
Biofilm sample collection
Eight biofilm samples were randomly obtained from the water pipes of four SDCs equipped with high-speed handpieces (Group 1) and three ways syringes (Group 2) in Laboratory A at the beginning of the study. Prior to sample collection, the water pipes underwent a 30-second flushing procedure and were sterilized using 75% ethanol, then detached from the control device. A sterile scissor was used to excise and discard a 5-millimeter segment from the tube’s anterior end. An aseptic nasal swab, measuring 2 mm in diameter and 17 millimeters in length, was inserted into the tube, rotating and traversing for 30 s to maximize biofilm collection. The swab’s head was subsequently preserved in an EP tube. All EP tubes were promptly stored at -80 °C within a thirty-minute timeframe to ensure sample integrity.
DNA extraction, 16 S rDNA and ITS gene sequencing and data analysis
Biofilm samples were centrifuged at 8000 g for 3 minutes with ddH2O, and the sediment was collected. DNA was extracted using the CTAB kit (Hangzhou Zeheng Biotechnology, China) following the manufacturer’s instructions. PCR amplification was performed with primers targeting the V3-V4 hypervariable regions of bacterial 16S rRNA genes (341F: 5’-CCTAYGGGRBGCASCAG-3’, 806R: 5’-GGACTACNNGGGTATCTAAT-3’) and the fungal ITS genes (ITS1F: 5’-CTTGGTCATTTAGAGGAAGTAA − 3’, ITS2R: 5’-GCTGCGTTCTTCATCGATGC-3’). The amplicon pools were prepared for sequencing using the Illumina NovaSeq 6000 platform (Shanghai Wei Huan Biological Technology, Shanghai, China). The sequences were analyzed employing Qiime 2.
Results
Current status of DUWLs contamination
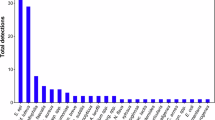
The bacterial colony counts and contamination rates in the waterlines of high-speed handpieces and three ways syringes at different time points are shown in Table 1; Fig. 2. At the beginning, middle, and end of the semester, the bacterial colony counts in the waterlines of both high-speed handpieces and three ways syringes exceeded the standard of 100 CFU/ml, indicating a high level of contamination with a contamination rate of 100%. As students used the equipment and the waterlines were flushed more frequently, the bacterial colony counts in the waterlines of both high-speed handpieces and three ways syringes significantly decreased during the middle and end of the semester.
Disinfection
Our previous study has demonstrated that 20 mg/L organochlorine disinfectant and 20 mg/L chlorine dioxide are effective in inactivating Escherichia coli and Staphylococcus aureus10. Therefore, these two disinfectants were selected in this study for the disinfection of DUWLs in dental laboratories.
The results indicated that both disinfectants exhibited good bactericidal efficacy (Table 2; Fig. 3), with a significant reduction in bacterial colony counts in the waterlines after disinfection (P < 0.05), and the contamination rate dropped to 0%. Until one week post-disinfection, the colony counts remained significantly lower than those before disinfection (P < 0.05). However, compared to the immediate post-disinfection, the colony counts had increased significantly at this time point (P < 0.05), with the contamination rate rising to 100%, suggesting that a weekly disinfection frequency is insufficient to meet the requirements for colony control. Moreover, the average colony count remained below 100 CFU/ml three days post-disinfection, with approximately one-third of the waterlines contaminated. Additionally, there was no statistically significant difference in the bactericidal effect between the two disinfectants (P > 0.05).
Colony counts before and after disinfection of chlorine dioxide and organochlorine disinfectants. (a) and (b) show the colony counts in the waterlines before and after disinfection for high-speed handpieces and three ways syringes, respectively. (c) (d) and (e) show the colony counts immediately post-disinfection, three days post-disinfection and one week post-disinfection, respectively. The dotted line stands the contamination line, over which indicates contamination. Dio and org are chlorine dioxide disinfectant and organochlorine disinfectant, respectively. Paired T-tests were conducted. *P<0.05, **P<0.01, ***P<0.001.
Microbial community composition of the laboratory DUWL biofilm
The main phyla of bacteria were Proteobacteria (63.17% in Group 1, 59.35% in Group 2) and Bacteroidota (29.04% in Group 1, 31.44% in Group 2) and that of fungi was Ascomycota (99.45% in Group 1, 98.24% in Group 2) in all samples. At the class level, Alphaproteobacteria (43.41% in Group 1, 39.53% in Group 2), Bacteroidia (29.04% in Group 1, 31.44% in Group 2), and Gammaproteobacteria (19.75% in Group 1, 19.82% in Group 2) were the dominant classes of bacteria, and Sordariomycetes (96.08% in Group 1, 61.44% in Group 2) and Eurotiomycetes (3.36% in Group 1, 36.80% in Group 2) were the dominant classes of fungi. The most abundant genera of bacteria were Novosphingobium (32.25%) and Pseudomonas (12.59%) in Group 1, and Sphingobium (21.77%) and Pseudomonas (15.09%) in Group 2. The most abundant genera of fungi were Fusarium (96.01% in Group 1, 61.46% in Group 2) and Penicillium (3.36% in Group 1, 36.81% in Group 2). The relative abundance of microbial community composition at genus level is illustrated in Fig. 4.
Potential human pathogens detected in biofilm samples comprised 9 bacterial genera and 2 fungal genera. Specifically, the bacterial genera with a relative abundance over 1% included Pseudomonas (12.59% in Group 1, 15.09% in Group 2), Burkholderia-Caballeronia-Paraburkholderia (4.11% in Group 1, 4.45% in Group 2), Mycobacterium (2.14% in Group 2), and Ralstonia (1.79% in Group 1). Other pathogenic bacterial genera were Legionella, Paenibacillus, Streptomyces, Acinetobacter, and Prevotella. Notably, the fungal genera Fusarium and Penicillium were identified as the most abundant and potentially pathogenic to humans in both groups.
Discussion
In 1963, Blake first discovered the presence of a significant number of bacteria in DUWLs and raised the concern of cross-infection risks11. Since then, DUWL contamination has gradually garnered attention in oral clinical management. A survey in Switzerland found that 70% of DUWLs were contaminated with a high number of aerobic mesophilic heterotrophic bacteria and 90% of dental offices had a medium level of air contamination12. The primary reasons for DUWL contamination include: (1) bacteria inherently present in the water supply system13; (2) back-suction of dental handpieces14; (3) biofilm formation within the waterlines15; (4) water stagnation due to narrow lumens, slow water flow, and the intermittent use patterns15,16,17,18. Studies have shown that bacteria in DUWLs mainly consist of bacteria unique to the water supply system, opportunistic pathogens, and oral flora, including Staphylococcus, Streptococcus, Actinomyces, and Legionella pneumophila19,20,21. Additionally, fungi (such as Candida albicans), viruses, and parasites have also been found1,22,23,24. These microorganisms not only contaminate the water quality at the outlet but may also appear in aerosols generated during the operation of dental instruments, thereby increasing the risk of cross-infection, especially opportunistic infections25. In 2012, Lancet reported a case of an 82-year-old patient who died from Legionella infection, with a medical history revealing only two dental treatments and no other evident exposure risks18. In 2016, 71 children were diagnosed with odontogenic nontuberculous mycobacterial infections after receiving endodontic treatment26.
However, contamination in DUWLs within dental laboratories has been overlooked for an extended period. This study represents the first to focus on contamination in the waterlines of SDCs in oral simulation head model laboratories. The findings reveal that the average colony count in unsterilized DUWLs amounts to 1.2 × 104 CFU/ml, significantly exceeding the domestic water quality standard of 100 CFU/ml. Existing research has demonstrated that, in clinical settings, colony counts in DUWLs can reach as high as 1.4 × 105 and 1.8 × 106 CFU/ml27,28. Notably, the colony count in the laboratory DUWLs examined in this study was slightly lower than those observed in clinical environments, potentially due to the use of resin teeth or autoclaved isolated teeth for student practice, thereby avoiding contamination from aspirated patient saliva, as typically encountered in clinical practices14,29. The contamination rate was 100% in three laboratories at the beginning, middle, and end of the semester, which may be attributed to the configuration of the laboratory waterline system, where 40 SDC waterlines are interconnected in series, thereby enhancing the likelihood of contamination throughout the entire laboratory. Furthermore, the average colony count detected in high-speed handpiece waterlines was generally higher than that in three ways syringes at various time points, indicating that the back-suction effect of high-speed handpieces significantly contributed to waterline contamination. Additionally, a correlation was identified between the degree of contamination in SDC waterlines and their frequency of use; specifically, the highest colony counts in high-speed handpiece and three-way syringe waterlines were observed at the beginning of the semester, following a downtime in holiday. As usage frequency increased, the contamination level decreased during the middle and end of the semester, yet remained at a high level overall. These findings suggest that DUWLs in laboratories are prone to the accumulation of various dirt and microorganisms during use, with bacteria readily proliferating within the pipes and forming biofilms in the downtime that are difficult to eliminate, thus posing potential sources of infection30. Based on the aforementioned rationale, CDC recommends rinsing as a physical means of reducing contamination during clinical procedures, with each patient undergoing rinsing for 20–30 s post-treatment5. However, rinsing alone is insufficient. A study has demonstrated that while rinsing significantly reduces colony counts in the output water, it still fails to meet the acceptable standard31, which is similar to the results of our study. Consequently, regular disinfection and maintenance of DUWLs are imperative.
The utilization of chemical disinfectants for the cleansing of DUWLs is considered the most expedient and efficacious approach to manage contamination, encompassing hydrogen peroxide, chlorine-containing disinfectants, slightly acidic electrolyzed water, etc32,33,34,35. Illustratively, Ditommaso et al. found that hydrogen peroxide (Peroxy Ag+) at 600 ppm could rapidly kill 99.99% of Legionella in DUWLs36; Agahi et al. sanitized DUWLs weekly using 0.2% chlorhexidine and found that colony counts in water samples decreased to less than 200 CFU/ml after four weeks37. Chlorine dioxide and organochlorine disinfectants are frequently employed in dental clinics owing to their superior bactericidal efficacy, good biosafety, operational simplicity and controllable costs1. The organochlorine disinfectant, with trichloroisocyanuric acid (TCCA) as its primary constituent, has been proven to be a safe and effective alternative to free chlorine for the disinfection of drinking water38. TCCA, in solid form, is easy to handle and highly stable38. Our preceding study has proved that relative to 20 ml/L organochlorine disinfectants, 20 ml/L chlorine dioxide exhibits enhanced antimicrobial efficacy while inducing minimal cytotoxicity and minimal corrosion to equipment, thereby rendering it a safer option for sustained utilization10. Furthermore, it is less prone to generating harmful disinfection by-products such as chlorite and chlorate10. In terms of biofilm control, chlorine dioxide has exhibited efficacy due to its non-reactivity with most biofilm constituents, which facilitates penetration through the biofilm matrix and enables the inactivation of the bacteria harbored within39. Additionally, TCCA can rapidly establish an equilibrium with high chlorine content upon dissolution in water, rendering it a promising candidate for the control of planktonic growth and the cultivability of biofilms38. To verify the disinfection efficacy of both in laboratory DUWLs, we employed the 20 mg/L of organochlorine disinfectant and the 20 mg/L of chlorine dioxide, respectively, for DUWL disinfection. The results showed that both disinfectants were capable of effectively eradicating bacteria in the waterlines. Especially three days post-disinfection, the colony counts sustained below 100 CFU/ml. Therefore, in contrast to the daily disinfection requirement for DUWLs in clinical settings, we propose that disinfection of DUWLs in oral simulation head model laboratories should be conducted every three days. Furthermore, we suggest the implementation of rigorous “shock treatments” in the beginning and the end of each semester, aimed at minimizing the growth of biofilms and eradicating any biofilms formed during the downtime30.
Furthermore, we assessed the microbiota diversity of biofilm in DUWLs of high-speed handpieces and three ways syringes in oral simulation head model laboratories. In our study, the dominant bacteria at the phylum level was Proteobacteria, representing over 60% of the total sequences, and the abundant fungi was Ascomycota at the phylum level, with Sordariomycetes and Eurotiomycetes being prevalent at the class level. These findings align with previous reports on DUWLs in clinics40,41,42. The primary bacteria genera detected in our study were Novosphingobium, Pseudomonas and Sphingobium, which have also been reported as predominant in clinical settings, albeit with variations in the ratios and diversity of micro-organisms observed across studies40,41,42,43,44. The majority of bacteria detected in DUWLs of oral teaching laboratories were heterotrophic, belonging to common environmental, soil-associated, and aquatic species, with low pathogenicity. When comparing the bacterial species present in the waterlines of high-speed handpieces and three-way syringes in our laboratory settings, we observed minimal differences, with one notable exception: the polycyclic aromatic hydrocarbon-degrading bacterium, Novosphingobium. This bacterium was abundant in the waterlines of high-speed handpieces (32%), whereas it was scarcely detected in those of three ways syringes (1.10%), and it is an aquatic heterotroph. However, in clinical settings, where devices are exposed to the oral cavity, the microbial composition in DUWLs becomes more complex1. Therefore, it may be of greater significance to detect and discuss the differences in bacterial contamination between the waterlines of high-speed handpieces and three ways syringes in clinical practice. Nevertheless, there is currently a scarcity of research addressing the distinct bacterial species present in the waterlines of clinical three ways syringes and high-speed handpieces, as well as the specific reasons for these differences.
Some opportunistic pathogens that can cause disease in immunocompromised people have also been identified in DUWLs. In our study, opportunistic pathogens accounted for approximately 20% of the total bacteria genera in terms of relative abundance, which was close to clinical findings; the opportunistic pathogens found in common with clinical DUWLs were Pseudomonas, Burkholderia-Caballeronia-Paraburkholderia, Ralstonia, Mycobacterium, Legionella, Acinetobacter and Prevotella41,42,44. These opportunistic pathogens like Legionella and Pseudomonas can contaminate surrounding air and surfaces, and cause various infection45. Legionella primarily causes Legionnaires’ disease with fever, chills, chest pain, and respiratory distress46, while Pseudomonas can lead to localized oral infections and, in immunocompromised individuals, systemic infections like bacteremia46. Additionally, the abundant fungi at the genus level in our study were Fusarium and Penicillium, both of which have potential pathogenic properties. Penicillium, a common genus found in aquatic environmental studies, is known to cause respiratory diseases such as allergic rhinitis as an allergen agent47. Conversely, few studies have reported Fusarium as the dominant fungi in DUWL biofilm. Fusarium can cause both systemic infections and local infections, such as keratitis, and it can be disseminated through hand-eye contact and aerosols48, posing a significant risk in oral simulation head model laboratories where students may lack adequate precautions. Students may be infected through inhalation of aerosols, direct contact with contaminated water, or indirect contact with contaminated equipment during training.
Notably, the configurations and operational patterns of oral simulation head model laboratories may exacerbate the risk of infection due to aerosols and splatter, which harbor microbes from DUWLs49, such as Legionella, Pseudomonas, Fusarium and Penicillium, as aforementioned. A study simulating dental procedures and evaluating distribution of aerosols and splatter concluded that the highest contamination was confined to 1.0–1.5 m from the source, with a maximum dissemination distance reaching 4 m50. And aerosols below 15 μm can persist in the air for an average of 7.13 min and can travel an average distance of 25.45 m from their source51. Considering the aforementioned layout of our laboratory, with adjacent SDCs separated by approximately 1.2 m, this distance is significantly less than the clinically recommended spacing requirements for SDCs, which advocate for a minimum distance of 2.4 m in the absence of physical barriers7. Furthermore, during class, the 40 SDCs in the laboratory are in operation simultaneously, with a practice duration that far exceeds that of actual clinical treatments. Hence, the dissemination of aerosols and splatter in laboratories is substantially more severe than that in clinical settings, leading to a marked increase in the risk of laboratory infection. These findings underscore the potential adverse effects of DUWLs in oral laboratories, even in a non-diagnostic environment, and emphasize the importance of regular control of microbial contamination in laboratory DUWLs.
To the best of our knowledge, our study represents the pioneering endeavor to concentrate on the contamination of DUWLs in oral education settings. While offering valuable insights, this study has its limitations. Firstly, this study only enrolled three oral simulation head model laboratories at a single university, potentially hindering the generalizability of the results to all dental laboratories. Secondly, the assessment of disinfection efficacy relied solely on the reduction in colony counts, without delving into the composition of the colonies post-disinfection. Lastly, the investigation into the interactions among microorganisms within biofilms, their pathogenicity, and antibiotic resistance may not have been sufficiently in-depth. Nevertheless, this study introduces a novel perspective and draws attention to the critical issue of contamination control in dental simulation head model laboratories.
Conclusion
In conclusion, our findings indicate that contamination of DUWLs in oral simulation head model laboratories is also a cause for concern, particularly following extended periods of inactivity (such as at the beginning of a semester). The microbial community composition is similar to the previous reports of DUWLs in clinical settings. 9 bacterial genera and 2 fungal genera of potential human pathogens are detected in the biofilm samples, posing a potential risk of infection through hand-eye contact and aerosol transmission. The average bacterial count in DUWLs remained below 100 CFU/ml within three days post-disinfection with 20 mg/L of organochlorine or chlorine dioxide disinfectant. Consequently, we recommend that managers of oral laboratories implement regular disinfection using 20 mg/L of organochlorine disinfectant or 20 mg/L of chlorine dioxide every three days, and that both teachers and students should adopt adequate protective measures to mitigate the risk of infections in the laboratory.
Data availability
The datasets generated and analysed during the current study are available in the GSA repository (Accession number CRA020991, https://bigd.big.ac.cn/gsa/browse/CRA020991).
Abbreviations
- SDC:
-
Simple dental chair
- DUWL:
-
Dental unit waterline
- ADA:
-
American Dental Association
- CDC:
-
Centers for Disease Control and Prevention
- TCCA:
-
Trichloroisocyanuric acid
References
Spagnolo, A. M., Sartini, M. & Cristina, M. L. Microbial Contamination of Dental Unit waterlines and potential risk of infection: A narrative review. Pathog Basel Switz. 9, 651 (2020).
Hong, F., Chen, P., Yu, X. & Chen, Q. The application of silver to Decontaminate Dental Unit Waterlines-a systematic review. Biol. Trace Elem. Res. 200, 4988–5002 (2022).
Bayani, M., Raisolvaezin, K., Almasi-Hashiani, A. & Mirhoseini, S. H. Bacterial biofilm prevalence in dental unit waterlines: A systematic review and meta-analysis - PubMed. (2023). https://pubmed.ncbi.nlm.nih.gov/36934281/
ADA statement on dental unit waterlines. Adopted by the ADA Board of Trustees, December 13, 1995 and the ADA Council on Scientific Affairs, September 28, 1995. Northwest. Dent. 75, 25–26 (1996).
Kohn, W. G. et al. Guidelines for infection control in dental health care settings–2003. J. Am. Dent. Assoc. 1939. 135, 33–47 (2004).
Walker, J. T. et al. Microbial biofilm formation and contamination of dental-unit water systems in general dental practice - PubMed. (2000). https://pubmed.ncbi.nlm.nih.gov/10919792/
Beijing & National Health Commission of the PRC. National Health Commission of the PRC. Standard for prevention and control of healthcare associated infection in dental outpatient department and clinic [WS/T 842–2024].( (2024).
Baudet, A., Lizon, J., Lozniewski, A., Florentin, A. & Mortier, É. Bacterial contamination of new dental unit waterlines and efficacy of shock disinfection. BMC Microbiol. 24, 529 (2024).
Hof, H. & Schrecker, J. Fusarium spp.: infections and intoxications - PubMed. (2024). https://pubmed.ncbi.nlm.nih.gov/39386384/
Yue, C., Yuya, H., Zhihuan, L., Zimo, W. & Jianying, F. Study on the disinfection effect of chlorine dioxide disinfectant (ClO2) on dental unit waterlines and its in vitro safety evaluation. BMC Oral Health. 24, 648 (2024).
The Incidence and Control of Bacterial. Infection in Dental Spray reservoirs. Br. Dent. J. 233, 397–400 (2022).
Kadaifciler, D. G. & Cotuk, A. Microbial contamination of dental unit waterlines and effect on quality of indoor air. Environ. Monit. Assess. 186, 3431–3444 (2014).
Holinger, E. P. et al. Molecular analysis of point-of-use municipal drinking water microbiology. Water Res. 49, 225–235 (2014).
Lewis, D. L. & Boe, R. K. Cross-infection risks associated with current procedures for using high-speed dental handpieces - PubMed. (1999). https://pubmed.ncbi.nlm.nih.gov/1537909/
Ma, H., Bw, B., Jj, S. & W, C. An in-vitro dynamic flow model for translational research into dental unit water system biofilms. J. Microbiol. Methods 171, (2020).
If, S. & R, S. D, K., L, L. Substantivity of hypochlorous acid-based disinfectant against biofilm formation in the dental unit waterlines. J. Conserv. Dent. JCD 20, (2017).
Sedlata Juraskova, E. et al. Legionella spp. in dental unit waterlines. Bratisl Lek Listy. 118, 310–314 (2017).
Ricci, M. L. et al. Pneumonia associated with a dental unit waterline. Lancet Lond. Engl. 379, 684 (2012).
Cicciù, M. Water Contamination risks at the Dental Clinic. Biology 9, 43 (2020).
Szymańska, J. & Sitkowska, J. Bacterial contamination of dental unit waterlines. Environ. Monit. Assess. 185, 3603–3611 (2013).
Fiorillo, L. We do not eat alone: formation and maturation of the oral microbiota. Biology 9, 17 (2020).
Singh, R. et al. Microbial diversity of biofilms in dental unit water systems. Appl. Environ. Microbiol. 69, 3412–3420 (2003).
Putnins, E. E., Di Giovanni, D. & Bhullar, A. S. Dental unit waterline contamination and its possible implications during periodontal surgery. J. Periodontol. 72, 393–400 (2001).
Khatoonaki, H. et al. Isolation and identification of potentially pathogenic free-living amoeba in dental-unit water samples. J. Water Health. 20, 1126–1136 (2022).
Volgenant, C. M. C. & de Soet, J. J. Cross-transmission in the Dental Office: Does this make you ill? Curr. Oral Health Rep. 5, 221–228 (2018).
Singh, J. et al. Invasive Mycobacterium abscessus outbreak at a Pediatric Dental Clinic - PubMed. (2021). https://pubmed.ncbi.nlm.nih.gov/34113683/
Watanabe, A., Tamaki, N., Yokota, K., Matsuyama, M. & Kokeguchi, S. Monitoring of bacterial contamination of dental unit water lines using adenosine triphosphate bioluminescence - PubMed. (2016). https://pubmed.ncbi.nlm.nih.gov/27597265/
Ji, X. Y. et al. Three key factors influencing the bacterial contamination of dental unit waterlines: A 6-year survey from 2012 to 2017 - PubMed. (2019). https://pubmed.ncbi.nlm.nih.gov/30565215/
Whitehouse, R. L., Peters, E., Lizotte, J. & Lilge, C. Influence of biofilms on microbial contamination in dental unit water - PubMed. (1999). https://pubmed.ncbi.nlm.nih.gov/1806595/
Samaranayake, L., Fakhruddin, K., Sobon, N. & Osathanon, T. Dental unit waterlines: Disinfection and management. Int. Dent. J. 74, S437–S445 (2024). (2024).
Whitehouse, R. L., Peters, E., Lizotte, J. & Lilge, C. Assessment of nosocomial bacterial contamination in dental unit waterlines: Impact of flushing - PubMed. (2020). https://pubmed.ncbi.nlm.nih.gov/32071534/
O’Donnell, M. J., Boyle, M. A., Russell, R. J. & Coleman, D. C. Management of dental unit waterline biofilms in the 21st century. Future Microbiol. 6, 1209–1226 (2011).
Pawar, A., Garg, S., Mehta, S. & Dang, R. Breaking the chain of infection: Dental unit water quality control. J. Clin. Diagn. Res. JCDR. 10, ZC80–84 (2016).
Costa, D., Girardot, M., Bertaux, J., Verdon, J. & Imbert, C. Efficacy of dental unit waterlines disinfectants on a polymicrobial biofilm. Water Res. 91, 38–44 (2016).
Wu, M. et al. Disinfection methods of dental unit waterlines contamination: A systematic review. J. Med. Microbiol. 71, (2022).
Ditommaso, S., Giacomuzzi, M., Ricciardi, E. & Zotti, C. M. Efficacy of a low dose of Hydrogen Peroxide (Peroxy Ag+) for Continuous Treatment of Dental Unit Water lines: Challenge Test with Legionella pneumophila serogroup 1 in a simulated Dental Unit Waterline. Int. J. Environ. Res. Public. Health. 13, 745 (2016).
Agahi, R. H. et al. Effect of 0.2% chlorhexidine on microbial and fungal contamination of dental unit waterlines - PubMed. (2014). https://pubmed.ncbi.nlm.nih.gov/25097645/
Oliveira, I. M., Gomes, I. B., Simões, L. C. & Simões, M. Chlorinated cyanurates and potassium salt of peroxymonosulphate as antimicrobial and antibiofilm agents for drinking water disinfection - PubMed. (2022). https://pubmed.ncbi.nlm.nih.gov/34921876/
Envirotek Worldwide. Treatment of Biofilms with Chlorine Dioxide. [Brochure]. (2015). https://www.envirotekww.com.
Dang, Y. et al. Assessment of microbiota diversity in dental unit waterline contamination - PubMed. (2022). https://pubmed.ncbi.nlm.nih.gov/35036099/
Chen, P. et al. The importance of biofilm contamination control for dental unit waterlines: a multicenter assessment of the microbiota diversity of biofilm in dental unit waterlines - PubMed. (2023). https://pubmed.ncbi.nlm.nih.gov/38174123/
Zhang, Z. et al. Human papillomavirus and cervical cancer in the microbial world: exploring the vaginal microecology - PubMed. (2024). https://pubmed.ncbi.nlm.nih.gov/38333037/
Watanabe, A., Tamaki, N., Matsuyama, M. & Kokeguchi, S. Molecular analysis for bacterial contamination in dental unit water lines - PubMed. (2016). https://pubmed.ncbi.nlm.nih.gov/27196554/
Yoon, H. Y. & Lee, S. Y. An Assessment of the bacterial diversity found in Dental Unit waterlines using the Illumina MiSeq. Biocontrol Sci. 24, 201–212 (2019).
Abusalim, G. S. Prevalence and investigations of bacterial contamination in dental healthcare associated environment. J. King Saud Univ. Sci. 34, 102153 (2022).
Optenhövel, M., Mellmann, A. & Kuczius, T. Occurrence and prevalence of Legionella species in dental chair units in Germany with a focus on risk factors - PubMed. (2023). https://pubmed.ncbi.nlm.nih.gov/37698817/
Li, L., Guan, K. & Zheng, S. G. Biochemical characteristics and allergenic activity of Common Fungus Allergens - PubMed. (2020). https://pubmed.ncbi.nlm.nih.gov/31309887/
Samaranayake, L., Fakhruddin, K., Sobon, N. & Osathanon, T. Dental Unit Waterlines: Disinfection and Management - PubMed. (2024). https://pubmed.ncbi.nlm.nih.gov/39515931/
Poolkerd, W. et al. Metataxonomics study of dental bioaerosols affected by waterline disinfection. BMC Oral Health. 24, 1575 (2024).
Allison, J. R. et al. Evaluating aerosol and splatter following dental procedures: Addressing new challenges for oral health care and rehabilitation - PubMed. (2021). https://pubmed.ncbi.nlm.nih.gov/32966633/
Komperda, J. et al. Computer simulation of the SARS-CoV-2 contamination risk in a large dental clinic. Phys. Fluids Woodbury N. 1994 33, 033328 (2021).
Acknowledgements
The authors would like to acknowledge the support and guidance received from Professor Yuanyuan Xie for refining the language of this work.
Funding
The present work was supported by Natural Science Foundation of Zhejiang Province (No. ZCLTGY24H1402) and National College Students Innovation and Entrepreneurship Training Program of China (No. 202310344032).
Author information
Authors and Affiliations
Contributions
Biyao Li, Yuya Hu made substantial contributions to the design, data analysis, and manuscript drafting. Jianying Feng supervised the entire study, while Yiqi Wang, Chengqi Zhang, Zimo Wang and Xujie Peng significantly contributed to the development of the study concept and provided crucial revisions for essential intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, B., Hu, Y., Wang, Y. et al. Periodic detection and disinfection maintenance of dental unit waterlines in dental simulation head model laboratories. Sci Rep 15, 5234 (2025). https://doi.org/10.1038/s41598-025-89010-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-89010-3