Abstract
Research links gait impairment in Alzheimer’s disease (AD) to cognitive abnormalities, brain atrophy, or amyloid-β (Aβ) deposition, with the exact cause unclear. This study investigated the relationship between gait, neuroimaging biomarkers, and cognition across the AD spectrum. We recruited 48 AD dementia patients, 27 with prodromal AD, and 41 cognitively unimpaired individuals, analyzing associations among gait parameters, cognitive scores, Aβ deposition, and cortical atrophy. Path and receiver operating characteristic (ROC) analyses evaluated gait impairment’s interdependent interactions and diagnostic potential. Prodromal AD and AD dementia patients showed significantly slower gait pace than CU (p = 0.014 [velocity], p = 0.003 [step length]), linked to attention and executive functions, widespread Aβ deposition, and cortical atrophy, in the inferior parietal lobule, middle temporal gyrus, precuneus, and insula. Compared to CU, AD dementia patients exhibited greater gait variability and phase (p = 0.017 [step length standard deviation], p = 0.001 [double support percentage]), significantly correlated with cognition and Aβ deposition. Path analysis revealed a combined influence of Aβ deposition, cognitive impairment, and cortical atrophy on gait impairment, with > 80% observed gait impairments directly affected by Aβ deposition. ROC curves for diagnosing AD stages showed significant areas under the curve, suggesting gait characteristics as noninvasive biomarkers for early AD diagnosis and progression monitoring.
Similar content being viewed by others
Introduction
Gait impairment in patients with various neurodegenerative disorders1,2, such as vascular dementia3, cerebral amyloid angiopathy4, and frontotemporal dementia5, can present without primary motor dysfunction. This implies that gait is a goal-oriented behavior6 that requires higher-level cognitive processes7 in addition to basic motor functions. Higher-level cognitive input is crucial for effective gait control, especially in complex environments or when multitasking. Dual-task experiments have demonstrated that cognitive impairment predominantly affects gait pace, indicating that effective gait control requires attention8.
Gait impairment is also linked to Alzheimer’s disease (AD)9,10. Studies based on positron emission tomography (PET) and structural magnetic resonance imaging (MRI) have associated gait pattern disturbances with AD neuropathological biomarkers. Specifically, cortical amyloid-β (Aβ) deposition was demonstrated to be associated with gait pace changes in AD11. Brain morphometrical changes have been shown to correlate with quantified gait parameters and dual-task gait performance in patients with mild cognitive impairment (MCI)12. However, the comprehensive relationships among these pathologic and structural changes, cognition, and gait in AD remain to be elucidated.
Despite the association between AD and gait alterations, the mechanisms behind these changes over the whole spectrum of AD remain largely unexplored. Studies have exclusively investigated this association in MCI or AD but not in AD spectrum. Given that AD symptoms worsen progressively, it is critical to monitor these correlations as the disease progresses.
This study aimed to explore gait impairment across the full spectrum of AD. To ensure population homogeneity, patients diagnosed with biologically defined AD were exclusively recruited. Gait parameters indicative of AD and its stages were identified, along with their correlations with cognition and neuroimaging biomarkers, such as Aβ deposition and cortical atrophy. Path analysis was employed to elucidate the mechanisms by which the interdependent relationships among these symptoms affect gait impairment.
Methods
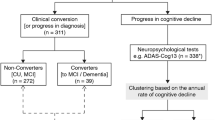
Study participants
We prospectively enrolled 116 consecutive participants from the Memory Disorder Clinic of Wonju Severance Christian Hospital between January 2022 and May 2023. Participants were categorized into three diagnostic groups: (1) AD dementia, (n = 48) consisting of those who met the criteria for probable AD13 with evidence of AD pathophysiological processes; (2) prodromal AD, (n = 27) comprising those who met the clinical criteria for MCI due to AD14 and (3) cognitively unimpaired (CU), (n = 41) including those without a history of neurologic or psychiatric illness, abnormalities on neurologic examination, or objective memory impairment. Cognitive impairment was defined as lower than -1.5 standard deviations of age- and education-adjusted norm in one or more cognitive domains in full neuropsychological test (see Neuropsychological tests section below). Exclusion criteria included individuals with a medical history of cerebral infarction; cerebral hemorrhage; parkinsonism; or recent knee, hip joint, or spine surgeries. Additionally, patients presenting with symptoms including dizziness, tremor, bradykinesia, gait disturbance, postural instability, or acute pain affecting the lumbar vertebrae, pelvis, or lower extremities while walking were excluded. All 116 participants finally registered for this study underwent brain T1-weighted MRI, 18F-florbetaben PET, neuropsychological tests, and apolipoprotein E genotyping. Clinical diagnosis was determined by two neurologists based on mutual consensus. (JH Hong and MS Baek).
Quantified gait analysis
Participants were instructed to walk barefoot at their normal walking speed 10 times on the GAITRite Electronic Walkway (CIR Systems Inc., Peekskill, NY, USA), which is a 6-m-long and 0.6-m-wide walkway with pressure-activated sensors that measure temporal and spatial gait parameters. Gait velocity, step length, step length standard deviation (SD), base width, swing percentage, double support percentage, double support time SD, and cadence were averaged over 10 trials. Gait velocity and step length were considered as gait pace, step length SD and double support time SD as gait variability, while swing percentage and double support percentage as gait phases, as previously described1. Leg length was measured from the medial ankle to the anterior inferior iliac spine.
Neuropsychological tests
The Seoul Neuropsychological Screening Battery (SNSB)15 was utilized for conducting neuropsychological tests. This battery assesses attention, language, visuospatial, verbal and visual memory, and frontal/executive functions, and includes the Clinical Dementia Rating Sum of Boxes and Mini-Mental State Examination. Cognitive domain composite scores for attention, language, visuospatial, memory, and executive functions were calculated16. Specifically, the following test items in the SNSB were included to construct the five cognitive domain composite scores: digit span forward and backward for the attention domain; the Korean version of the Boston Naming Test and calculation for the language; the copying item of the Rey-Osterrieth Complex Figure Test for the visuospatial domain; immediate recall, 20-min delayed recall, and recognition items of the Rey-Osterrieth Complex Figure Test and Seoul Verbal Learning Test for the memory domain; and the semantic and phonemic Controlled Oral Word Association Test and Stroop color reading test for the executive domain.
Image acquisition and preprocessing
Sagittal T1-weighted cranial MRI scans were acquired using magnetization prepared rapid acquisition gradient-echo sequences (3 T Siemens MRI; Siemens, Erlangen, Germany) with the following parameters: slice thickness of 0.9 mm, pixel size of 0.4492 × 0.4492 mm, repetition time of 2000 ms, echo time of 2.43 ms, filp angle of 9°, matrix size of 512 × 512 pixels. Images were reconstructed to 512 × 512 over a 256 mm field of view. These scans were processed using FreeSurfer v.7.4.0 (https://surfer.nmr.mgh.harvard.edu). The Desikan-Killiany (DK) atlas was used to compute regional cortical thickness17. The cortical thickness of 14 composite regions of interest (ROIs) across both hemispheres were computed using the 68 DK regions18. The FreeSurfer pipeline was used to estimate the intracranial volume (ICV) of each participant.
Three-dimensional Aβ PET images were acquired (Discovery STe PET/CT; GE Healthcare, Milwaukee, WI, USA) within 15 min from 90 min after injection of 18F-florbetaben. During the acquisition of Aβ PET images, a head holder was utilized to minimize head movement during the scan. Brain computed tomography images were also captured for attenuation correction. The PET images were reconstructed in a 256 × 256 × 223 matrix with 2.34 × 2.34 × 3.2 mm voxel size using the ordered-subsets expectation maximization algorithm with six iterations and 16 subsets. Subsequently, PET images were partial-volume effect corrected using a region-based voxel-wise method19. Surface-based standard uptake value ratio (SUVR) maps in the cortical gray matter were calculated using cerebellar gray matter as a reference20 in Statistical Parametric Mapping v.12 (Wellcome Trust Centre for Neuroimaging). The regional Aβ SUVRs were determined for each DK region and composite ROI by averaging the SUVRs at vertices within each specified region.
Statistical analyses
For demographic variables, continuous variables are presented as the mean ± SD, whereas dichotomous variables are presented as counts. The AD dementia group had 11 missing cognitive scores because of participants’ inability to carry out the assessments. The CU group had one missing apolipoprotein E4 value. Missing values were addressed using list-wise deletion. For continuous variables, either a two-sided Student’s or Welch’s t-test was applied, whereas a two-sided Fisher’s exact test was used for discrete variables.
Group comparisons for continuous gait parameters were performed using analysis-of-covariance (ANCOVA) and linear contrast methods based on linear regression models. P-values were computed using a non-parametric permutation method, following a Kolmogorov–Smirnov normality test. Age, sex, years of education, and leg length were used as covariates.
To investigate the association of gait parameters with regional Aβ deposition, regional cortical thickness, and cognitive domain composite scores, Pearson partial correlation coefficients were computed, further adjusting for age, sex, years of education, and leg length. In the analysis involving cortical thickness, ICV was added as a covariate. Multiple comparison corrections for each gait parameter were applied to five cognitive scores and cortical regions, consisting of DK regions and composite ROIs, using the Benjamini–Hochberg false discovery rate procedure.
Path analysis was performed to understand the potential causal relationships between gait impairment and Aβ deposition, cortical atrophy, and cognitive impairment. Path models included three pathways from Aβ SUVR to cortical thickness, cognitive scores, and gait parameters11, along with two pathways from cortical thickness to cognitive scores and gait parameters21. Due to the limited understanding of the causal relationship between gait parameters and cognitive scores, a covariance rather than a direct relationship between these two was included. All pathways were adjusted for age, sex, years of education, and ICV, with additional adjustments for leg length in pathways involving gait parameters. Path coefficients were estimated using a covariance-based maximum likelihood approach. Model fit was assessed using the standardized root mean square residual (SRMR), comparative fit index (CFI), and Tucker–Lewis index (TLI). A model with a SRMR < 0.08, CFI > 0.90, and TLI > 0.90 was considered a satisfactory fit22, whereas that with an SRMR < 0.08, CFI > 0.95, and TLI > 0.95 was considered a good fit23. The statistical significance of path coefficients and the size of indirect and total effects were determined using bias-corrected bootstrap confidence intervals generated from 10 000 bootstrap resamples.
Receiver operating characteristic (ROC) analysis was conducted to evaluate the discriminatory capability of gait parameters in identifying CU, prodromal AD, and AD dementia. For each pair, binary logistic regression models incorporating various gait parameter combinations were constructed. The area under the ROC curve (AUROC) quantified classification performance, with statistical significance assessed as described for the path analysis. Statistical analyses were conducted using MATLAB R2023b (MathWorks, Natick, MA, USA).
Results
Demographic and clinical characteristics
Participants with prodromal AD were older than those in the CU and AD dementia groups (Table 1). In the CU group, seven participants were Aβ-positive, indicating a preclinical AD stage. The total cognitive score and cognitive domain composite scores were lowest in the AD dementia group. Scores for attention and language were not significantly different between the CU and prodromal AD groups.
Characteristic gait patterns
For all participants, gait parameters with descriptive statistics for the three diagnostic groups displayed in Fig. 1A. A detailed summary of the normality tests and ANCOVA results is provided in Supplementary Table S1. Gait pace was slower, whereas gait variability was greater in the AD dementia group than in the CU group. Gait pace was also slower in the prodromal AD group than in the CU group. Gait phase parameters were different between the AD dementia and CU groups. Few differences were observed between the prodromal AD and AD dementia groups. When amyloid-positive CU individuals were excluded from the CU group, the statistical significance of the pairwise group comparisons remained largely consistent with the results obtained when amyloid-positive CU individuals were included (Supplementary Table S2).
Differences in gait parameters among diagnostic groups. (A) Significant p-values shown after adjustment for age, sex, years of education, and leg length (*p < 0.05, **p < 0.01, ***p < 0.001). (B) Heatmaps showing the partial cross-correlation matrix between gait parameters and cognitive domain composite scores. Partial correlation coefficients were computed for these variables after adjusting for age, sex, years of education, and leg length (left), as well as for clinical diagnostic groups (right). Circle colors and sizes represent Pearson’s partial correlation coefficients and uncorrected p-values, respectively. Yellow asterisks represent significant partial correlations after correcting for multiple comparisons (false discovery rate). CU, cognitively unimpaired; AD, Alzheimer’s disease; SD, standard deviation.
Associations between cognitive domain composite scores and gait patterns
Velocity, step length, swing percentage, and double support percentage correlated significantly with all five cognitive domain composite scores (left panel, Fig. 1B). Despite little difference across the groups, cadence correlated with attention and executive function scores. After accounting for spurious associations between gait parameters and cognitive domain composite scores and adjusting for group effects, attention and executive function scores remained associated with gait parameters (right panel, Fig. 1B). Faster velocity and longer step length were associated with better attention and executive function scores, while five gait parameters (velocity, step length, swing percentage, double support percentage, and cadence) remained associated with the executive function score.
Association between Aβ deposition and gait patterns
Velocity, step length, swing percentage, and double support percentage were associated with Aβ deposition across all cortical areas, even after correcting for multiple comparisons (Fig. 2A). Increased Aβ deposition was associated with slower velocity, shorter step length, and swing percentage, and increased double support percentage. Composite ROI analysis showed significant associations in most regions except in the bilateral medial temporal area (Supplementary Table S3).
Association between neuroimaging biomarkers and gait parameters. The brain maps show the association of gait parameters with amyloid-β (Aβ) deposition (A) and cortical thickness (B) in regions defined according to the Desikan–Killiany (DK) cortical atlas. Regions showing significant associations after correcting for multiple comparisons using the false discovery rate procedure across DK regions for each gait parameter are colored. Color scales represent the negative logarithms of non-adjusted p-values. The images were generated using the MATLAB package59.
Association between cortical thickness and gait patterns
Cortical thickness was associated with gait pace, particularly in the left entorhinal cortex (EC), right middle temporal gyrus (MTG), and right insula (Fig. 2B). Slower velocity was associated with decreased cortical thickness in the right inferior temporal gyrus, left insula, right precuneus, and right inferior parietal lobule (IPL). Analysis of the cortical thickness in composite ROIs showed significant correlations between slower gait pace and cortical atrophy in the EC, insula, and bilateral temporoparietal and medial parietal areas (Supplementary Table S4).
Path analysis
Gait velocity, step length, swing percentage, and double support percentage were included as indicators in the path models owing to their significant associations with neuroimaging biomarkers and total cognitive scores (gait velocity, r = 0.3799, p < 0.0001; step length, r = 0.4034, p < 0.0001; swing time percentage, r = 0.3620, p < 0.001; double support percentage, r = -0.3792, p < 0.0001). The global Aβ SUVR, or average SUVR of all vertices in the cortex, was utilized to estimate its involvement and correlation with gait impairment. Owing to their significant association with gait parameters in the composite ROI analysis, indicators derived from bilateral measurements in the insula, precuneus, MTG, inferior temporal gyrus, IPL, and EC were used for evaluating cortical thickness.
Path models incorporating cortical thickness in key regions of the MTG, IPL, precuneus, and insula showed satisfactory or good fits with the observed data (Fig. 3). Models using cortical thickness in the MTG and IPL showed good fit when used in combination with velocity, step length, swing percentage, and double support percentage (Supplementary Table S5). More details are presented in Supplementary Tables S6–S9.
Schematic representations of path models illustrating relationships between global amyloid-β deposition, regional cortical thickness, total cognition, and gait impairment. Red paths indicate significant path coefficients. (A) Models incorporating cortical thickness in the middle temporal gyrus demonstrating good fit for velocity and step length. (B) Models incorporating cortical thickness in the middle temporal gyrus demonstrating good fit for swing time and double support percentages. (C) Models incorporating cortical thickness in the inferior parietal lobule and precuneus demonstrating good and satisfactory fits with all four gait parameters. (D) Models incorporating cortical thickness in the insula demonstrating satisfactory fit with step length. Amy, amyloid-β; SUVR, standardized uptake ratio value; CTh, cortical thickness; Cog; cognitive score; Gait, gait parameter; MTG, middle temporal gyrus; IPL, inferior parietal lobule; Swing %, Swing percentage; Double support %, double support percentage.
Significant direct effects of cortical thickness in the MTG on velocity and step length were observed (Fig. 3A). When the gait parameters were changed to swing and double support percentage, the model did not show significant path coefficients from cortical thickness to gait parameters (Fig. 3B). Models including cortical thickness in the IPL and precuneus showed similar path profiles, exhibiting significant direct effects originating from global Aβ deposition to gait parameters and nonsignificant direct effects originating from cortical thickness to gait parameters (Fig. 3C). A notable exception was the model with cortical thickness in the insula, which demonstrated significant paths both from cortical thickness to step length and from global Aβ deposition to step length (Fig. 3D). This model also showed a significant indirect effect of Aβ deposition on step length, which was not observed in other models (Supplementary Table S10). Notably, in all of these models, indirect effects accounted for less than 20% of the total effects originating from global Aβ deposition to gait parameters, whereas direct effects contributed to over 80%; nonetheless, total effects remained significant in all models.
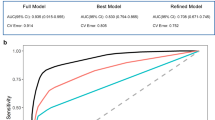
Receiver operating characteristics analysis
Velocity, step length, swing percentage, and double support percentage were incorporated first in ROC analysis (Model A, Fig. 4), all with satisfactory or good fits in their path models. These parameters significantly differentiated CU from prodromal AD and AD dementia groups; however, they did not significantly differentiate prodromal AD and AD dementia groups. Adding gait variability parameters (Model C, Fig. 4) marginally improved the AUROC values, though not significantly compared with those in Model A. However, adding base width significantly improved classification performance between prodromal AD and AD dementia groups, as shown in comparisons between Models B and A and between Models D and A. When amyloid-positive CU individuals were excluded from the CU group, the AUROC values were largely unchanged compared to the case where these individuals were included (Supplementary Figure S1).
Receiver operating characteristic (ROC) curves classifying diagnostic groups in Alzheimer’s disease using gait parameters. Binary logistic regression models were constructed for each classification. Statistical significance was assessed using bias-corrected confidence intervals of the area under the ROC curve (AUROC), based on 10 000 bootstrap samples. Model A incorporated four gait parameters in the path analysis, with the path models involving these parameters demonstrating satisfactory or good fit. Models B, C, and D additionally employed base width, gait variability (step length and double support time standard deviations), and both parameters, respectively, all demonstrating significant mean differences. Red lines in legends denote significant differences in AUROC values between the models. CU, cognitively unimpaired; AD, Alzheimer’s disease; AUROC, area under receiver operating characteristic curve; CI, confidence interval; SD, standard deviation.
Discussion
This study investigated the association of gait with cognition and neuroimaging biomarkers of Aβ deposition and cortical atrophy across the AD spectrum. Gait pace was significantly slower in the prodromal AD group than in the CU group, reflecting early-stage AD deterioration and decrease in gait velocity with disease progression. Additionally, gait pace was linked to the attention and executive function cognitive domains and Aβ deposition across many cortical areas. It was also associated with cortical atrophy in the IPL and insula. Gait phase and variability were more impaired in participants with AD dementia than in those with CU, exhibiting distinctive associations with cognition and neuroimaging biomarkers. Path analysis revealed that gait patterns are simultaneously influenced by Aβ deposition, cognitive impairment, and cortical atrophy in the IPL, MTG, precuneus, and insula. ROC analysis demonstrated that these gait patterns can be used to differential diagnosis of subgroups across the AD spectrum.
Collectively, these findings demonstrate that gait pace is reduced in AD, consistent with previous studies1,24,25,26 associating lower gait pace with various forms of dementia, including AD. The findings further indicated that gait pace becomes impaired during the early AD stages. The identified differences among the groups in this study aligned with the findings of previous studies showing gait pace deterioration as an early indicator of AD progression27. Moreover, its association with the attention and executive function cognitive domains suggests a correlation with the initial stages of AD, as deficits in these domains typically manifest early in the condition28. These domains are also related to the default mode and salience networks (DMN and SN, respectively), which are affected in early AD29. The DMN detects environmental events30 and facilitates attentional resource allocation31, while the SN is associated with working memory32, a key component of function execution. The SN encompasses the insula33, while the DMN comprises the IPL and precuneus34; the present study identified a correlation between gait velocity and cortical atrophy in both these regions. Any impairment in these two cognitive domains and in related network resources, can affect the organization of goal-oriented behaviors35 such as gait, causing careless gait and poor limb coordination7. In addition, gait pace was associated with Aβ deposition in several areas, another hallmark of early-stage AD36, in line with previous studies11,37.
This study revealed notable differences in gait variability and phase between the CU and AD dementia groups but not between the CU and prodromal AD groups. Thus, gait parameters likely undergo alterations as the disease progresses. Similar to gait pace, previous studies have reported that gait variability is impaired during the disease stage and can even differentiate AD from other dementias1,9,24. The association of increased gait phase, particularly double support percentage, with the disease consistent with previous research25, suggests that individuals with AD pathology may necessitate a more dynamically stable gait compared to CU individuals38,39, similar to the increased need for gait stability observed with aging, as reflected in a higher double support percentage40,41. Cholinergic dysfunction mediated by Aβ depositions may contribute to gait variability, either directly by affecting cholinergic motor control42 or indirectly through impaired attention and executive function43. In addition, impaired vestibular and visual function in the advanced stages of AD may be related to changes in gait variability and phase44,45. The weak association between cortical atrophy and these gait parameters may reflect the influence of other mechanisms unrelated to cortical atrophy, such as white matter disintegrity46 or hyperintensities47. Thus, longitudinal studies are needed to evaluate the changes in gait parameters throughout AD progression.
The integration of multimodal sensory inputs may be crucial for gait, as demonstrated in the path analysis comprising cortical thickness in pertinent areas. The IPL plays a critical role in gait by processing signals from visual, vestibular, and somatosensory cortices48, while the MTG facilitates gait regulation by integrating multimodal sensory information49 and relaying it to motor and premotor areas. The shared neural substrates for cognition and motor control in these regions50 suggest their involvement in a common neural mechanism related to sensory feedback for gait modification51. Being essential for gait coordination, the insula processes sensory inputs, triggering responses in the anterior cingulate cortex30 and subsequently influencing the motor system52. Of note, insula dysfunction affects self-awareness and hazard assessment53.
By examining the pathways between neuroimaging biomarkers and gait parameters, the putative origins of gait impairment can be identified. In models including the MTG and insula, the pathway from cortical atrophy to gait impairment was identified to be significant, suggesting that compromised sensory integration possibly due to atrophy may explain this impairment. However, in models including the IPL and precuneus, the pathway from cortical atrophy to gait impairment was found to be insignificant, indicating other influencing factors beyond atrophy. All path models with satisfactory fit showed statistically significant may direct effects of Aβ deposition on gait pace and phase. This suggested that Aβ toxicity directly contributes to gait impairment, potentially owing to oxidative damage, neuroinflammation, and cholinergic system disruption54.
Gait parameters influenced by cortical atrophy and amyloid deposition, as demonstrated in path models with satisfactory or good fit, successfully differentiated individuals with AD dementia and prodromal AD from CU individuals, highlighting their potential for AD screening and early detection. Moreover, the additional inclusion of base width in ROC analysis improved the identification of later stages in the AD spectrum, despite its lack of association with neuroimaging biomarkers. This may stem from a complex interplay with other gait parameters and associations55,56 with late-stage AD symptoms, such as mood deficits57,58 and impaired vestibular functions44.
The study had some limitations. One of them was that it focused on linear associations for the advantage of lower variance across different samples, despite the fact that AD symptoms often interact in a complex and nonlinear way. Another limitation was that the path analysis did not allow for definitive conclusions about the causality between gait and AD symptoms. Future studies should incorporate tau PET scans and emphasize causation through longitudinal follow-up, utilizing advanced methodologies such as latent growth curve or nonlinear mixed-effect models.
Conclusions
This study showed that structural abnormalities within cortical regions for multimodal sensory inputs, together with widespread Aβ deposition, detrimentally influence gait during AD progression. The insights acquired from this study can provide a basis for developing diagnostic modalities that can facilitate preemptive AD screening and the use of gait in assessment of AD progression in routine clinical practice. Furthermore, understanding the potential effect of current anti-Aβ therapeutics on gait in patients with AD may offer valuable insights for improved drug assessment.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to privacy restrictions but are available from the corresponding author on reasonable request.
References
Darweesh, S. K. L. et al. Quantitative gait, cognitive decline, and incident dementia: The Rotterdam Study. Alzheimers Dement 15, 1264–1273 (2019).
Verghese, J. et al. Abnormality of Gait as a predictor of Non-Alzheimer’s dementia. N. Engl. J. Med. 347, 1761–1768 (2002).
Verghese, J., Wang, C., Lipton, R. B., Holtzer, R. & Xue, X. Quantitative gait dysfunction and risk of cognitive decline and dementia. J. Neurol. Neurosurg Psychiatry 78, 929–935 (2007).
Sharma, B. et al. GAIT in cerebral amyloid angiopathy. J. Am. Heart Assoc. 11 (2022).
Allali, G. et al. Frontotemporal dementia: Pathology of gait?. Mov. Disord. 25, 731–737 (2010).
Takakusaki, K. Neurophysiology of gait: From the spinal cord to the frontal lobe. Mov. Disord. 28, 1483–1491 (2013).
Yogev-Seligmann, G., Hausdorff, J. M. & Giladi, N. The role of executive function and attention in gait. Mov. Disord. 23, 329–342 (2007).
Montero-Odasso, M., Muir, S. W. & Speechley, M. Dual-Task complexity affects GAIT in people with mild cognitive impairment: the interplay between GAIT variability, dual tasking, and risk of falls. Arch. Phys. Med. Rehabil. 93, 293–299 (2012).
Pieruccini-Faria, F. et al. Gait variability across neurodegenerative and cognitive disorders: Results from the Canadian Consortium of Neurodegeneration in Aging (CCNA) and the Gait and Brain Study. Alzheimers Dement 17, 1317–1328 (2021).
Cedervall, Y., Halvorsen, K. & Åberg, A. C. A longitudinal study of gait function and characteristics of gait disturbance in individuals with Alzheimer’s disease. Gait Posture 39, 1022–1027 (2014).
Del Campo, N. et al. Relationship of regional brain β-amyloid to gait speed. Neurology 86, 36–43 (2015).
Grijalva, C., Toosizadeh, N., Sindorf, J., Chou, Y. & Laksari, K. Dual-task performance is associated with brain MRI Morphometry in individuals with mild cognitive impairment. J. Neuroimaging 31, 588–601 (2021).
McKhann, G. M. et al. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7, 263–269 (2011).
Albert, M. S. et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7, 270–279 (2011).
Ryu, H. H. & Yang, D. W. The Seoul neuropsychological screening battery (SNSB) for comprehensive neuropsychological assessment. Dementia Neurocognit. Disord. 22(1) (2023).
Ahn, H.-J. et al. Seoul Neuropsychological Screening Battery-Dementia version (SNSB-D): a useful tool for assessing and monitoring cognitive impairments in dementia patients. J. Korean Med. Sci. 25, 1071 (2010).
Desikan, R. S. et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. NeuroImage 31, 968–980 (2006).
Cho, H. et al. Tau PET in Alzheimer disease and mild cognitive impairment. Neurology 87, 375–383 (2016).
Thomas, B. A. et al. The importance of appropriate partial volume correction for PET quantification in Alzheimer’s disease. Eur. J. Nucl. Med. Mol. Imaging 38, 1104–1119 (2011).
Bullich, S. et al. Optimal reference region to measure longitudinal amyloid-β change with 18F-florbetaben PET. J. Nucl. Med. 58, 1300–1306 (2017).
Tian, Q., Studenski, S. A., Resnick, S. M., Davatzikos, C. & Ferrucci, L. Midlife and Late-Life Cardiorespiratory fitness and brain volume changes in late Adulthood: Results from the Baltimore Longitudinal Study of Aging. J. Gerontol. A Biol. Sci. Med. 71, 124–130 (2015).
Byrne, B. M. Structural Equation Modeling with EQS and EQS/WINDOWS: Basic Concepts, Applications, and Programming (SAGE, 1994).
Hu, L. & Bentler, P. M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 6, 1–55 (1999).
Mc Ardle, R. et al. Do Alzheimer’s and Lewy body disease have discrete pathological signatures of gait?. Alzheimer’s Dementia 15(10), 1367–1377 (2019).
Merory, J. R. et al. Quantitative gait analysis in patients with dementia with Lewy bodies and Alzheimer’s disease. Gait Posture 26(3), 414–419 (2007).
Nadkarni, N. K. et al. Spatial and temporal gait parameters in Alzheimer’s disease and aging. Gait Posture 30(4), 452–454 (2009).
Rosso, A. L. et al. Slowing gait and risk for cognitive impairment. Neurology 89, 336–342 (2017).
Guarino, A. et al. Executive functions in alzheimer disease: A systematic review. Front Aging Neurosci. 10 (2019).
Fredericks, C. A. et al. Early affective changes and increased connectivity in preclinical Alzheimer’s disease. Alzheimers Dement Diagnosis Assess. Dis. Monit. 10, 471–479 (2018).
Menon, V. & Uddin, L. Q. Saliency, switching, attention and control: a network model of insula function. Brain Struct. Funct. 214, 655–667 (2010).
Parr, T. & Friston, K. J. Working memory, attention, and salience in active inference. Sci. Rep. 7 (2017).
Fox, M. D. et al. The human brain is intrinsically organized into dynamic, anticorrelated functional networks. Proc. Natl. Acad. Sci. USA 102, 9673–9678 (2005).
Seeley, W. W. et al. Dissociable intrinsic connectivity networks for salience processing and executive control. J. Neurosci. 27, 2349–2356 (2007).
Andrews-Hanna, J. R., Smallwood, J. & Spreng, R. N. The default network and self-generated thought: Component processes, dynamic control, and clinical relevance. Ann. N. Y. Acad. Sci. 1316, 29–52 (2014).
Lee, B., Kim, J. S. & Chung, C. K. Parietal and medial temporal lobe interactions in working memory goal-directed behavior. Cortex 150, 126–136 (2022).
Thal, D. R., RüB, U., Orantes, M. & Braak, H. Phases of Aβ-deposition in the human brain and its relevance for the development of AD. Neurology 58, 1791–1800 (2002).
Dao, E. et al. Cerebral amyloid-β deposition is associated with impaired gait speed and lower extremity function. J. Alzheimers Dis. 71, S41–S49 (2019).
Williams, D. S. & Martin, A. E. Gait modification when decreasing double support percentage. J. Biomech. 92, 76–83 (2019).
Winter, D. A. et al. Biomechanical walking pattern changes in the fit and healthy elderly. Physical therapy 70, 340–347 (1990).
Kim, H. K. et al. Gait parameters in Healthy Older Adults in Korea. J. Move. Disord. (2024)
Noh, B. et al. Age-specific differences in gait domains and global cognitive function in older women: Gait characteristics based on gait speed modification. PeerJ 8, e8820 (2020).
Schirinzi, T. et al. Amyloid-Mediated cholinergic dysfunction in motor impairment related to Alzheimer’s disease. J. Alzheimers Dis. 64, 525–532 (2018).
Perry, R. J. & Hodges, J. R. Attention and executive deficits in Alzheimer’s disease: A critical review. Brain 122, 383–404 (1999).
Nakamagoe, K. et al. Vestibular function impairment in Alzheimer’s disease. J. Alzheimers Dis. 47, 185–196 (2015).
Gago, M. F. et al. Role of the visual and auditory systems in postural stability in Alzheimer’s disease. J. Alzheimers Dis. 46, 441–449 (2015).
Olazarán, J. et al. Clinical and anatomical correlates of GAIT dysfunction in Alzheimer’s disease. J. Alzheimers Dis. 33, 495–505 (2012).
Ezzati, A. et al. Relationship of white matter hyperintensity and cortical volume with gait velocity in older adults (P4.040). Neurology 86 (2016).
Hou, J. et al. Translingual neural stimulation affects resting-state functional connectivity in mild-moderate traumatic brain injury. J Neuroimaging 32, 1193–1200 (2022).
Onitsuka, T. et al. Middle and inferior temporal gyrus gray matter volume abnormalities in chronic schizophrenia: an MRI study. Am. J. Psychiatry 161, 1603–1611 (2004).
Grande, G. et al. Measuring gait speed to better identify prodromal dementia. Exp. Gerontol. 124, 110625 (2019).
Takakusaki, K., Takahashi, M., Noguchi, T. & Chiba, R. Neurophysiological mechanisms of gait disturbance in advanced Parkinson’s disease patients. Neurol. Clin. Neurosci. 11, 201–217 (2022).
Crottaz-Herbette, S. & Menon, V. Where and when the anterior cingulate cortex modulates attentional response: Combined FMRI and ERP evidence. J. Cogn. Neurosci. 18, 766–780 (2006).
Bonthius, D. J., Solodkin, A. & Van Hoesen, G. W. Pathology of the insular cortex in Alzheimer disease depends on cortical architecture. J. Neuropathol. Exp. Neurol. 64, 910–922 (2005).
Hampel, H. et al. The amyloid-Β pathway in Alzheimer’s disease. Mol. Psychiatry 26, 5481–5503 (2021).
Murri, M. B. et al. Instrumental assessment of balance and gait in depression: A systematic review. Psychiatry Res. 284, 112687 (2019).
Kumar, D., Villarreal, D. J. & Meuret, A. E. Walking on the bright side: Associations between affect, depression, and gait. PLoS ONE 16, e0260893 (2021).
Lyketsos, C. G. et al. Neuropsychiatric symptoms in Alzheimer’s disease. Alzheimers Dement 7, 532–539 (2011).
Craig, D. A cross-sectional study of neuropsychiatric symptoms in 435 patients with Alzheimer’s disease. Am. J. Geriatr. Psychiatry 13, 460–468 (2005).
Scholtens, L. H., de Lange, S. C. & van den Heuvel, M. P. Simple brain plot. Zenodo https://doi.org/10.5281/zenodo.5346593 (2021).
Acknowledgements
We thank Hyun Ji Lee, Ji Young Lee, and Seo Hee Kim at Wonju Severance Christian Hospital for their technical assistance with participant enrollment, gait analysis, and neuropsychological testing.
Funding
This study was supported by a National Research Foundation (NRF) grant provided by the Korea government (NRF2022R1C1C1012535) to M.S. Baek, an NRF grant provided by the Korea government (RS-2024-00358576) to S.W. Kim, and a National Institute for Health and Care Research (NIHR) fellowship to R. Mc Ardle (NIHR 301677). Additionally, the study was supported by grants from the NIHR Newcastle Biomedical Research Centre (BRC) at the Newcastle upon Tyne Hospitals National Health Service (NHS) Foundation Trust, Newcastle University, and the Cumbria, Northumberland, Tyne and Wear (CNTW) NHS Foundation Trust.
Author information
Authors and Affiliations
Contributions
SWK, DHK, and MSB devised the project and the main conceptual ideas. SWK, DHK, and MSB drafted the manuscript. SWK, DHK, JYH, KRM, DJ, IH, RMA, JSK, and MSB reviewed and revised the manuscript. SWK, DHK, IH, JSK, and MSB analyzed the data. SWK, DHK, and MSB interpreted the study findings. MSB led data collection. MSB supervised the work. All authors read and approved the final manuscript and had final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
This study was approved by the institutional review board of Wonju Severance Christian Hospital (Ref# CR322029). The research protocol conformed with the principles of the Declaration of Helsinki and its subsequent revisions. Written informed consent was obtained from all participants and/or their legal guardians.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, SW., Kim, D.H., Hong, J.Y. et al. Gait impairment associated with neuroimaging biomarkers in Alzheimer’s disease. Sci Rep 15, 5539 (2025). https://doi.org/10.1038/s41598-025-90020-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-90020-4