Abstract
The study of key Pseudomonas aeruginosa (PA) virulence factors, the molecular basis of pathogenicity, as well as their correlation with the immune response during exacerbations in patients with non-cystic fibrosis bronchiectasis can help to identify novel targets and biomarkers for clinical management. The objective was to compare P. aeruginosa virulence and the patient’s immune response during stable phases and exacerbations of bronchiectasis. We used polymerase chain reaction (PCR) and real-time quantitative PCR (qRT-PCR) to perform molecular characterization of the genomic islands and virulence genes present in 42 P. aeruginosa strains obtained from the sputum of patients with bronchiectasis during stability and exacerbations. Immunoglobulin (Ig) and interleukin (IL) levels in 32 serum samples were analyze by ELISA and Luminex assay. A greater presence of the conjugative element pKLC102, specific virulence genes (exoS, exoY) and pyoverdine production characterize the P. aeruginosa strains obtained during exacerbations. The expression levels of type III secretion system (exoS, exoY) showed an important role in the humoral immune response during exacerbations. Exacerbations were associated with high levels of IL-6. The presence of specific genomic islands, virulence genes, and increased IL-6 levels provide an accurate characterization on bronchiectasis exacerbations. These targets could be useful in the prevention, management and treatment of these exacerbations.
Similar content being viewed by others
Introduction
Non-cystic fibrosis bronchiectasis is a chronic structural lung disease that facilitates colonization by different microorganisms and recurrent respiratory infection. The average number of exacerbations in patients with bronchiectasis is approximately 2.6 per patient per year; between 18% and 38% of these patients have three or more exacerbations, a circumstance that significantly increases hospitalization and mortality rates1. Pseudomonas aeruginosa is a major pathogen in bronchiectasis and is known for its antibiotic resistance that contributes to increased treatment failure2.
Numerous virulence factors associated with P. aeruginosa in bronchiectasis disrupt host epithelial cells and promote oxidative stress. These include the type III secretion system, quorum-sensing system proteins, elastases, alginate, pyoverdine, and pyocyanin. The type III secretion system (exoS, exoT, exoU, and exoY) regulates the expression of exotoxins. Quorum-sensing proteins (lasR/lasI and rhlR/rhlI) facilitate cell-to-cell communication. Elastases (lasA and lasB) disrupt tight junctions between host epithelial cells, while alginate (alg genes) and pigments like pyoverdine upregulate the transcription of certain elastases. Pyocyanin, which is involved in oxidative stress, promotes alterations in mitochondrial electron transport in the host3.
P. aeruginosa possesses a mosaic genome, with a conserved core that is interrupted by specific blocks of genes known as genomic islands (GEIs), acquired through horizontal gene transfer. These comprise pathogenicity, symbiosis, fitness, metabolic, and resistance islands that contribute to the adaptability, fitness, and competitiveness of the bacterium. Many GEIs have been described in the P. aeruginosa chromosome; however, GEIs are found in variable numbers in different strains4.
This complexity of the P. aeruginosa genomic machine, together with its interaction with the immune response, results in recurrent exacerbations that negatively affect disease progression and patients’ quality of life. Studies exploring the prediction of exacerbations and chronic P. aeruginosa infections based on the humoral immune response, particularly immunoglobulin (Ig) G levels, have yielded varied results1,5.
Several serological tests have been employed to identify P. aeruginosa infection in patients with cystic fibrosis, especially those who do not produce sputum. Although IgG levels correlate well with P. aeruginosa burden during chronic respiratory infection, their predictive value for exacerbations has only rarely been reported6. Recent studies have highlighted an intricate relationship between bronchiectasis, asthma, and chronic obstructive pulmonary disease, adding complexity to the search for predictive factors7.
The treatment of bronchiectasis exacerbations remains challenging. A better understanding of the molecular basis of P. aeruginosa pathogenicity and the associated host immune response could improve both the clinical management of bronchiectasis exacerbations and patients’ quality of life. This study aimed to compare the virulence factors in P. aeruginosa and the immune responses of patients during stable disease and exacerbations, aiming to identify potential future biomarkers and targets that could improve the clinical management of bronchiectasis.
Results
Genomic islands
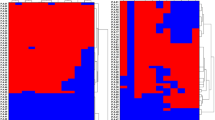
In this study of 20 patients with bronchiectasis, we analyzed 42 strains of P. aeruginosa isolated from sputum samples during an exacerbation and a stable phase in each patient (one strain per sputum sample). The median [Interquartile range, IQR] number of strains per patient was 2.00[1.00–3.00], without statistically significant differences in the number of strains collected during stability 1.00[0.00-1.75] compared to exacerbation 1.00[1.00–1.00] (Table S1 supplemental material). The presence/absence analysis of GEIs in P. aeruginosa showed no differences between the exacerbation and stable phases for PAPI-1 (60.8% vs. 57.9%, p = 0.9), PAPI-2 (73.9% vs. 73.7%, p = 0.9), PAGI-1 (73.9% vs. 84.2%, p = 0.47), PAGI-2 (43.5% vs. 36.8%, p = 0.9), PAGI-3 (91.3% vs. 84.2%, p = 0.64), PAGI-4 (60.9% vs. 57.9%, p = 0.9) with the exception of the conjugative element pKLC102 (100% vs. 73.68%, p = 0.0137*). (Fig. 1). At least one GEI was present in 100% of the strains. Six different patterns were identified based on the number of GEIs: A (6 GEIs), B (5 GEIs), C (4 GEIs), D (3 GEIs), E (2 GEIs) for strains from exacerbation and the stable phase; with one pattern identified only in the stable phase: F (7 GEIs) (Supplemental Figure S1). Among the 47.8% of strains from the exacerbation and the 15.78% of strains from the stable phase, the most frequent were PAPI-1, PAPI-2, PAGI-1, PAGI-3, PAGI-4, and pKLC102 (Pattern A). 17.4% of strains from exacerbation and 36.84% from the stable phase, presented 5 GEIs (Pattern B). The distribution of GEIs was heterogeneous but we want to highlight the high number of strains carrying the conjugative element pKLC102 during exacerbations.
Virulence factors
Statistical analysis of the virulence factors showed significant differences in exoS, exoY, and pyoverdine production in cetrimide agar between the exacerbation and stable phases. Genes exoS and exoY, encoding T3SS exotoxins, were detected at a higher frequency in exacerbation phases compared with stable phases: exoS (100 vs. 47%, p < 0.001) and exoY (100 vs. 74%, p < 0.05) (Fig. 2). Pseudomonas aeruginosa strains from both phases produced the pigments pyoverdine and pyocyanin (observed phenotype). Pyoverdine production in cetrimide agar was higher during exacerbations (57% vs. 16%, p < 0.05), while there was no difference in pyocyanin between the exacerbation and the stable phases (21.74% vs. 21.05%; not significant [ns]). One group of type IV pili was more predominant, albeit not significantly, during exacerbation than during stable phases (tfpOa, 78% vs. 68%, ns). Other groups were detected at similar rates: tfpOb (0% vs. 10.53%, ns), group II (22% vs. 21%, ns), tfpX (0% vs. 26.31%, ns), tfpY (21.7% vs. 21.05%, ns), and tfpZ (34.78% vs. 15.78%, ns). The algD, algU, and apr genes, together with the quorum-sensing proteins (lasR/lasI and rhlR/rhlI), were present in all isolates during exacerbations compared with 85% in the stable phase, but this did not reach statistical significance. The presence of lasA, lasB, plcH, plcN, toxA, fliC, fliD, lecA, lecB, phzM, phzS, and pvdS genes was not significantly different between exacerbation and stable phase (Fig. 2).
Presence/absence of cellular and secreted virulence factors in P. aeruginosa isolated from patients with bronchiectasis during exacerbations and stable phase. Virulence factors in P. aeruginosa with statistically significant differences by Fisher’s method. Exacerbation (E) vs Stable phase (SP). exoS (p < 0.0001), exoY (p < 0.05), pyoverdine (p < 0.05).
Gene expression analysis
During exacerbations, as compared to stable phases, we found trends towards overexpression of exoS, exoY, and pvdS (encoding pyoverdine production) genes; however, no statistically significant differences were found for exoS (34.78% vs. 15.78%, p = 0.2), exoY (8.69% vs. 15.78%, p = 0.6), or pvdS (8.69% vs. 15.78%, p = 0.6) (Fig. 3). After a paired sub-analysis, ExoS production increased non-significantly during exacerbations (Supplemental Figure S2).
Gene expression analysis of virulence factors (exoS, exoY, pvdS) in P. aeruginosa during exacerbation and stable phases. Fisher’s method. Overexpression (green color) was considered when the corresponding mRNA level was ≥ 2-fold higher than that of ATCC PA14. Otherwise, the result was considered negative if < 1-fold higher, and borderline if between 1- and 2-fold higher.
Immunoglobulin analysis
Our bronchiectasis population colonized by P. aeruginosa presented high levels [mg/dl] of both IgG and IgM during exacerbations (IgG, 1536 [1063–2140]; IgM, 405 [203–637. 50]) and stable phase (IgG, 1250 [0.79–2411]; IgM, 508 [267–865]). IgM was the only Ig that showed concentrations above normal values. Statistical analysis of exacerbations versus stable phase showed no significant differences in Ig levels (G, A, E, M, D) or in IgG subclasses between groups (Table 1; Fig. 4). After the paired analysis, although P. aeruginosa load did not differ between the stable phase and exacerbations IgG1 levels were higher during exacerbations compared to stable phase (Supplemental Figure S2). .
Interleukin analysis
IL-6 levels were significantly higher (p < 0.05) during exacerbations compared with stable phases, whereas the other ILs showed similar levels between groups. Statistical analysis of ILs between the exacerbation and stable phase is shown in Table 1; Fig. 5. However, after a paired sub-analysis, serum levels of IL-6, IL-7, IL-10, and IL-1 were higher during exacerbations compared to stable phase (Supplemental figure S2).
Correlation between virulence factors and immune response
The correlation between gene expression levels of exoS, exoY, and pvdS genes versus the Ig and IL concentrations was analyze during the stable phase and exacerbations by Spearman’s test. Exacerbation: exoY showed a significant inverse correlation with IgM (p = 0.045*; negative rs = -0.5110), IgG1 (p = 0.0175*; negative rs = -0.5920), IgG2 (p = 0.0008***; negative rs = -0.7684) and IgG3 (p = 0.0110*; negative rs = -0.6263). exoS showed a significant positive correlation with IgE (p = 0.0412*; rs = 0.5196). Figure 6. All other correlations analyzed during the exacerbation phase were non-significant. No correlations were detected between ILs or Igs concentrations versus the gene expression levels of exoS, exoY, and pvdS genes in stable phase.
Discussion
The present study showed that P. aeruginosa exhibited an increased number of GEIs and virulence factors during exacerbations. These results could be related to an increased pathogenic potential, as described in previous studies of P. aeruginosa strains associated with other infections. The conjugative element pKLC102, exoS, exoY, and pyoverdine production played pivotal roles, suggesting their potential as targets for future treatments aimed at mitigating exacerbations. In patients with bronchiectasis who were colonized with P. aeruginosa, we found similar IgM and IgG levels, during both exacerbations and stable phase. By contrast, higher IL-6 levels were found during exacerbations. These results emphasize the importance of inflammatory markers such as IL-6 during exacerbations and suggest the potential benefits of antimicrobials with anti-inflammatory activity (e.g., macrolides) to treat exacerbations. Non-paired and paired statistical analysis was performed in a subset of patients to obtain these results (Supplemental figure S2).
The P. aeruginosa strains from exacerbations (47.8%) and stable phase (15.78%) presented six GEIs (pattern A) and pKLC102. This is consistent with the findings reported by Morales Espinosa et al.4, who showed similar GEIs included in pattern A, with the only difference being PAGI-2 instead of PAGI-1. It is worth noting that, among the strains isolated during the stable phase, 10.52% exhibited seven GEIs, a relatively uncommon finding. Previous studies suggest that this phenomenon is linked not to increased pathogenicity, but rather to variations in insertion sites8. Therefore, while pattern A predominated in exacerbations and pattern B predominated in stable phase, previous research confirms that differences in the number of GEIs between groups are not the sole determinants of increased pathogenicity, and suggests instead that the distribution and expression of virulence genes play more crucial roles8. In fact, in our study we found a higher level of pKLC102 in the strains from the exacerbation, which might have led to an increase in pathogenicity, taking into account the dual function of this element as a genomic island and plasmid9.
The analysis of virulence factors revealed that both during exacerbations and stable phase, P. aeruginosa exhibits a wide array of active virulence factors that contribute to its pathogenic potential and ability to survive. These findings are consistent with those of numerous previous studies on P. aeruginosa strains isolated from different samples10. For instance, the type III secretion system (exoS and exoY) and pigment production in cetrimide agar (notably pyoverdine) presented a higher frequency during exacerbations compared with stable phase. These differences suggest their potential as targets for future treatments aimed at preventing exacerbations. The concurrent overexpression of multiple virulence factors may play a crucial role in P. aeruginosa survival, contributing to both disease chronicity and exacerbations. To the best of our knowledge, this is the first study reporting differences in virulence factors between P. aeruginosa recorded during exacerbations and stable phases in patients with bronchiectasis.
The analysis of Ig levels showed high levels of IgG and IgM during both exacerbations and stable phase. Other studies5,11 have reported the high accuracy of anti-P. aeruginosa (anti-PA) IgG tests for detecting chronic P. aeruginosa infection in patients with bronchiectasis or cystic fibrosis. However, while some also suggest that IgG levels can be a marker of disease severity and treatment response, our findings differ, suggesting that anti-PA IgG is unsuitable for predicting exacerbations in this group of patients. Although, IgG1 showed significant differences in some patients with a paired sub-analysis of the samples. We stress that IgM levels were higher in the stable phase than in exacerbations, possibly reflecting the chronic nature of this disease. On this issue, several studies report that certain virulence factors exert a direct action on the immune humoral response12. We found an inversely proportional correlation between the IgM, IgG1, IgG2, IgG3 levels and expression of exoY gene, and a positive correlation between IgE and expression of exoS gene in exacerbated patients that has not been reported before, suggesting a direct impact on the humoral immune response for these targets during exacerbations.
The high levels of IL-6 during exacerbations suggest its potential as a biomarker for predicting exacerbations. This finding aligns with similar results reported by Jee Youn Oh et al.13, who noted that IL-6 levels were notably elevated in patients with bronchiectasis and may require more intensive treatment in order to prevent acute exacerbation. Additionally, a study conducted by Olveira et al., focusing on fat-free mass depletion and inflammation in patients with bronchiectasis, found correlations between inflammatory IL-6 levels and exacerbations14. By contrast, Chalmers et al. assigned a more important role to IL-8, IL-1β, IL-17 and TNFα15.
This study has some limitations. The number of strains was low because we obtained them exclusively from different patients with bronchiectasis in two specific phases and only used one type of sample. Nonetheless, this study provides new data in patients with bronchiectasis and identifies important differences between the two core disease phases that could improve management. Few data have been published to date regarding the virulence factors of P. aeruginosa strains in bronchiectasis and their relationship with the immune response during both exacerbations and stable phase.
In conclusion, a greater presence of the conjugative element pKLC102, gene expression levels of specific virulence genes in P. aeruginosa and an increased IL-6 levels characterized bronchiectasis exacerbations better than increases in systemic Ig levels in this group of patients. Patients with bronchiectasis and P. aeruginosa colonization show significant increases in systemic IL-6 levels during exacerbations which may have a beneficial predictive value, as previous reports have proposed16, thus confirming that the use of antimicrobials with anti-inflammatory activity during exacerbations could have significant benefits. However, our results also suggest the importance of the expression levels of exoS and exoY genes as targets to take into account in the management and treatment of bronchiectasis, due to their influence on the humoral immune response.
Methods
Study design
This was a prospective observational study (NCT04803695) conducted at the pulmonology service of Hospital Clínic of Barcelona, a tertiary care hospital, and at the CELLEX research laboratories of IDIBAPS, both in Barcelona, Spain. The study complied with the Declaration of Helsinki (current version; Fortaleza, Brazil, October 2013) and the requirements of the 2007 Spanish Biomedical Research Act. The institution’s Internal Review Board approved the study (Clinical Research Ethical Committee of Hospital Clinic. Registry number HCB/0236). All patients gave their written informed consent.
Clinical P. aeruginosa strains isolated from 42 sputum samples were analyzed, 23 during exacerbations and 19 during stability. This was performed by isolating one strain from each sputum sample and from 32 serum samples (including healthy donor) provided by 20 consecutive patients with bronchiectasis during exacerbations and stable phase. P. aeruginosa analysis included molecular characterization of pathogenicity factors, the sputum load, and the biomarkers involved in the immune response during both clinical phases. Patients were visited every 3 months. During each visit, one sputum and serum sample was obtained, when possible, and lung function was assessed with an EasyOne™ World Spirometer (NDD Medical Technologies. Zurich. Switzerland) and classified according to the American Thoracic Society/European Respiratory Society Guidelines.
Genomic Island and virulence factor detection
The molecular characterization of different GEIs and virulence factors was performed by polymerase chain reaction (PCR) and electrophoresis. This included P. aeruginosa pathogenicity islands (PAPI-1, PAPI-2), P. aeruginosa GEIs (PAGI-1, PAGI-2, PAGI-3 and PAGI-4), a conjugative element (pKLC102), and virulence genes (type IV pili (tfpOa, tfpOb, tfpW, tfpX, tfpY, tfpZ), fliC, fliD, apr, exoT, exoS, exoY, exoU, plcH, plcN, ToxA, phzM, phzS, LecA, LecB, algD, algU, lasR, lasI, rhlR, rhlI, lasA, and lasB). Pigment production (±) was evaluated in cetrimide agar (Pseudosel Agar, BD) by qualitative observation. Colonies that appeared fluorescent green, yellow, or brown were considered pyoverdine producers; colonies that appeared blue or dark green were considered pyocyanin producers3. PCR amplification was performed with the primer pairs described by Finnan. et al. as follows17: ORF3, ORF18, and ORF42 of PAGI-1; C22 and C105 of PAGI-2; and SG8 and SG100 of PAGI-3. Amplification of genes CP10, CP44, and CP97 was performed using the primer pairs described by Klockgether et al. for pKLC102 9. The selected genes represent the left, right, and middle regions of each island. We used the primer sets proposed by Qiu et al.18 to amplify different DNA segments of PAPI-1: primer pair 976 F and PAPI-1R to detect the integration of PAPI-1 at the attB site in the locus PA0976; primer pairs 4542 F + intF and sojR + 4541 F to amplify the left and right junction sequences between the chromosome and island, respectively, when integrated into the chromosome at the attB site in the tRNA Lys gene locus PA4541.1 that corresponds to strain PA14. The primer pair intF + sojR was used to detect the presence of a circular PAPI-1. For PAPI-2, the primers PAPI-2–1 F and PAPI-2-1R were used to amplify the xerC gene at locus RS02 at the left region, and the primers PAPI-2–2 F and PAPI-2-2R were used to amplify the middle region (locus RS07 and RS08)19. The CL22 gene was chosen because it is specific to PAGI-4 20.
Virulence genes were amplified with specific primers, using PCR protocols according to the authors’ instructions21,22,23,24. Thermal cycling for the genes included an initial denaturation cycle at 94 °C for 2 min, followed by 35 cycles at 94 °C for 1 min, at the annealing temperature for 1 min, at 72 °C for 1 min, and with a final cycle of 72 °C for 2 min. The primers and conditions are shown in Table S2 and Table S3 in supplementary material. The PCR products were visualized in 2% agarose using 100 bp and 1 kb DNA ladder as molecular weight markers (Invitrogen). Next, the analysis of PCR was confirmed by random selection of different amplified products to undergo sequencing22,24. The sequences obtained were analyses by alignment with the template sequence at GenBank.
Measurement of Immunoglobulin and Interleukin levels
The immunoglobulin levels (mg/dl): IgG, IgM, IgA, IgE, IgD, subclasses of IgG (IgG1. IgG2. IgG3, IgG4) and inflammatory cytokine levels (pg/ml): IL-1 A, IL-1B, IL-4, IL-6, IL-7, IL-8, IL-10, IL-17a, TNFα and IFNγ were quantified using ELISA kits (IgG: BMS2091, IgM: BMS2098, IgA: BMS2096, IgE: BMS2097 (Invitrogen) and IgD: ab177708. abcam) and the multiplex immunoassay with Luminex technology, in a Luminex MAGPIX (Millipore).
RNA extraction and reverse transcription
Strains were grown in 10 mL of LB broth at 37 °C for 18–24 h to the late exponential phase and then collected by centrifugation. Total RNA extraction was carried out using the Qiagen RNeasy purification kit. After checking the RNA extraction quality on 1% agarose gel and measuring the RNA content (Nanodrop, ThermoFisher Scientific, France), RNA extracts were stored at − 80 °C until further use. Before cDNA synthesis, genomic DNA was removed from 1 µg of total RNA using the gDNA wipeout buffer included in the QuantitectR© reverse transcription kit (Qiagen). Reverse transcription was performed in a volume of 20 µL, including 14 µL of template RNA (extract concentrations adjusted to contain 1 µg of RNA), 1 µL of reverse transcription master mix, 4 µL RT buffer 5x (containing dNTPs and Mg2+), and 1 µL of RT primer mix. Reverse transcription was performed in a Veriti PCR Thermal Cycler (Applied Biosystems. France) for 30 min at 42 °C, followed by incubation for 3 min at 95 °C to inactivate the reverse transcriptase. All reactions, including RNA handling, were carried out on ice. The rpoD gene was used as a reference to normalize the relative amount of mRNA2.
Real-time PCR assay
This work focused on the expression of virulence factors with statistically significant differences between exacerbations and stable phase (exoS, exoY, pyoverdine production). Normalization of expression results was carried out using rpoD (reference gene to normalize the relative amount of mRNA) and the PA14 strain as a control2. A Lightcycler 96 (Roche Diagnostics, Meylan, France) was used for all quantitative PCRs. All PCR amplification reactions were performed in 96-well-plates with a 10 µL final volume containing 2.5 µL of diluted (1:10) template cDNA, 1 µL of each primer (corresponding to a final concentration of 0.5 µM), 5 µL of Quantitect SYBR Green PCR Master Mix (including MgCl2 to reach a concentration of 2.5 mM) (Qiagen), and 0.5 µL RNase/DNase free water (Qiagen). The cycling program was set as follows: (1) activation, 1 cycle at 95 °C for 15 min; (2) amplification, 40 cycles including 15 s denaturation at 95 °C, 25 s annealing at 60 °C, 15 s elongation at 72 °C; and (3) melting curve, 1 cycle including 5 s at 95 °C, 1 min at 65 °C, and a final increase to 97 °C with a transition rate of 0.11 °C/s. Each reaction was carried out in duplicate and the experiment was repeated on 2 different sets of RNA extracts (biological replicate)24.
Evaluation of real-time PCR results
Using the delta-delta Ct method, overexpression of exoS, exoY, and pvdS genes was considered when the corresponding mRNA level was ≥ 2-fold higher than that of ATCC PA14 (the rpoD gene used as reference to normalize the relative amount of mRNA). It was considered negative if < 1-fold higher, and borderline if between 1- and 2-fold higher2.
Statistical analysis
The statistical program GraphPad prism, version 8.4, was used for analysis, applying the non-parametric Fisher, Mann–Whitney and Spearman test. Data are reported as medians with percentiles (25–75%). Statistical significance was defined as p < 0.05. Differences in the expressions of genes of interest were tested by single sample t-test with cut-off values of ≤ 0.5 for under expression and ≥ 2 for overexpression.
Data availability
The Datasets generated and/or analysed during the current study are available in the repository name VirulenceBE at https://doi.org/10.34810/data1339.
References
Zhang, Y. et al. Isolated IgG2 deficiency is an independent risk factor for exacerbations in bronchiectasis. QJM: Mon. J. Associat. Physicians 115, 292–297 (2022).
Cabrera, R. et al. Resistance mechanisms and molecular epidemiology of Pseudomonas aeruginosa strains from patients with bronchiectasis. J. Antimicrob. Chemother. 77, 1600–1610 (2022).
Alonso, B. et al. Characterization of the virulence of Pseudomonas aeruginosa strains causing ventilator-associated pneumonia. BMC Infect. Dis. 20, 909 (2020).
Morales-Espinosa, R. et al. Genetic and phenotypic characterization of a Pseudomonas aeruginosa population with high frequency of genomic islands. PLoS One 7, e37459 (2012).
Suarez-Cuartin, G. et al. Anti-Pseudomonas aeruginosa IgG antibodies and chronic airway infection in bronchiectasis. Respir. Med. 128, 1–6 (2017).
Johansen, H. K. et al. Antibody response to Pseudomonas aeruginosa in cystic fibrosis patients: A marker of therapeutic success?–A 30-year cohort study of survival in Danish CF patients after onset of chronic Pseudomonas aeruginosa lung infection. Pediatr. Pulmonol. 37, 427–432 (2004).
Padilla-Galo, A. & Olveira Fuster, C. Bronchiectasis in COPD and Asthma. More than just a coincidence. Arch. Bronconeumol. (Engl. Ed.) 55, 181–182 (2019).
Gellatly, S. L. & Hancock, R. E. W. Pseudomonas aeruginosa: New insights into pathogenesis and host defenses. Pathog. Dis. 67, 159–173 (2013).
Klockgether, J., Würdemann, D., Reva, O., Wiehlmann, L. & Tümmler, B. Diversity of the abundant pKLC102/PAGI-2 family of genomic islands in Pseudomonas aeruginosa. J. Bacteriol. 189, 2443–2459 (2007).
Ertugrul, B. M., Oryasin, E., Lipsky, B. A., Willke, A. & Bozdogan, B. Virulence genes fliC, toxA and phzS are common among Pseudomonas aeruginosa isolates from diabetic foot infections. Infect. Dis. (Lond.) 50, 273–279 (2018).
Mauch, R. M. et al. Assessment of IgG antibodies to Pseudomonas aeruginosa in patients with cystic fibrosis by an enzyme-linked immunosorbent assay (ELISA). Diagn. Pathol. 9, 158 (2014).
Arora, S. K., Ritchings, B. W., Almira, E. C., Lory, S. & Ramphal, R. The Pseudomonas aeruginosa flagellar cap protein, FliD, is responsible for mucin adhesion. Infect. Immun. 66, 1000–1007 (1998).
Oh, J. Y. et al. Elevated interleukin-6 and bronchiectasis as risk factors for acute exacerbation in patients with tuberculosis-destroyed lung with airflow limitation. J. Thorac. Dis. 10, 5246–5253 (2018).
Olveira, G. et al. Fat-free mass depletion and inflammation in patients with bronchiectasis. J. Acad. Nutr. Diet. 112, 1999–2006 (2012).
Barbosa, M. & Chalmers, J. D. Bronchiectasis. Presse. Med. 52, 104174 (2023).
Menéndez, R. et al. Systemic Inflammation during and after bronchiectasis exacerbations: Impact of Pseudomonas aeruginosa. J. Clin. Med. 9, 2631 (2020).
Finnan, S., Morrissey, J. P., O’Gara, F. & Boyd, E. F. Genome diversity of Pseudomonas aeruginosa isolates from cystic fibrosis patients and the hospital environment. J. Clin. Microbiol. 42, 5783–5792 (2004).
Qiu, X., Gurkar, A. U. & Lory, S. Interstrain transfer of the large pathogenicity island (PAPI-1) of Pseudomonas aeruginosa. Proc. Natl. Acad. Sci. USA 103, 19830–19835 (2006).
Chemani, C. et al. Role of LecA and LecB lectins in Pseudomonas aeruginosa-induced lung injury and effect of carbohydrate ligands. Infect Immun 77, 2065–2075 (2009).
Petit, S.M.-C. et al. Lagooning of wastewaters favors dissemination of clinically relevant Pseudomonas aeruginosa. Res. Microbiol. 164, 856–866 (2013).
Gaines, J. M. et al. Regulation of the Pseudomonas aeruginosa toxA, regA and ptxR genes by the iron-starvation sigma factor PvdS under reduced levels of oxygen. Microbiology (Reading) 153, 4219–4233 (2007).
Kus, J. V., Tullis, E., Cvitkovitch, D. G. & Burrows, L. L. Significant differences in type IV pilin allele distribution among Pseudomonas aeruginosa isolates from cystic fibrosis (CF) versus non-CF patients. Microbiology (Reading) 150, 1315–1326 (2004).
Horna, G. et al. Specific type IV pili groups in clinical isolates of Pseudomonas aeruginosa. Int. Microbiol. 22, 131–141 (2019).
Wang, G.-Q. et al. Effect of negative pressure on proliferation, virulence factor secretion, biofilm formation, and virulence-regulated gene expression of pseudomonas aeruginosa in vitro. Biomed. Res. Int. 2016, 7986234 (2016).
Acknowledgements
Thanks go to technician Maria Pérez and Dr Marina Bantulá for their professional advice.
Funding
ISCIII-FEDER [Code: PI18/00145] grant awarded to AT and LFB; CIBER project 2018 [ES18PI01 × 1-2021] awarded to AT and LFB; ISCIII-FOS [FI19/00090] grant awarded to RLA. CB 06/06/0028/CIBER respiratory diseases (Ciberes). CIBERES is an initiative of ISCIII. 2.603/IDIBAPS. ICREA Academy award to AT. SGR 01148 (2021) from Generalitat de Catalunya to LFB. SEPAR grants 2016 [Code: 208], 2019 [Code: 628], and 2023 [Code: 1428] awarded to LFB. Funders did not play any role in the project design, data collection, data analysis, interpretation, writing of the paper, or decision to publish.
Author information
Authors and Affiliations
Contributions
RC performed experiments of virulence factors, pathogenicity islands, gene expression, and immunoglobulins, and participated in the cytokine and immunoglobulin level analyses. RLA, NRR, and AM participated in the cytokine and immunoglobulin studies. RC, LFB, and AT in data collection and reviewed participated in protocol development, study design, and study management. RC and LBF participated in data interpretation and in the writing of this manuscript. AT, LFB, LBF, VA, and NV participated in the patient recruitment and obtained respiratory specimens. RC, NV, LFB, LM, and JV participated in the identification of microorganisms. All authors participated the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All procedures in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all individual participants included in the study. Hospital Clinic ethical committee reference number: HCB/2018/0236.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cabrera, R., Rovira-Ribalta, N., Motos, A. et al. Virulence factors of Pseudomonas aeruginosa and immune response during exacerbations and stable phase in bronchiectasis. Sci Rep 15, 6520 (2025). https://doi.org/10.1038/s41598-025-91368-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-91368-3