Abstract
Patients with complex coronary artery disease (CAD) often have poor clinical outcomes. This study aimed to develop a predictive model for assessing the 1-year risk of major adverse cardiovascular events (MACE) in patients with stable complex CAD, using retrospective data collected from January 2020 to September 2023 at Guangzhou Red Cross Hospital. The goal was to enable early risk stratification and intervention to improve clinical outcomes. A total of 369 patients were included and randomly divided into a training set (70%) for model development and a validation set (30%) for performance evaluation. Predictive factors were selected using least absolute shrinkage and selection operator (LASSO) regression, followed by logistic regression to construct the model and create a nomogram. Seven independent predictors were identified: functional SYNTAX score (OR 1.257, 95% CI 1.159–1.375), low-density lipoprotein cholesterol (LDL-C, OR 1.487, 95% CI 1.147–1.963, /1mmol/L), left ventricular ejection fraction (LVEF, OR 0.934, 95% CI 0.882–0.985, /1%), albumin (OR 0.889, 95% CI 0.809–0.974, /1g/L), pulse pressure ≥ 72 mmHg (OR 3.358, 95% CI 1.621–7.118), angiotensin-converting enzyme 2 (ACE2) ≥ 27.5 U/L (OR 2.503, 95% CI 1.290–5.014), and diabetes (OR 2.261, 95% CI 1.186–4.397). Among these, the functional SYNTAX score was the strongest predictor. The area under the receiver operating characteristic curve (AUC) was 0.843 for the training set and 0.844 for the validation set, with Youden indices of 0.561 and 0.601, respectively. Calibration curves and decision curve analysis demonstrated good predictive accuracy and clinical utility of the model. These findings suggest that the developed model has strong predictive performance for 1-year MACE risk in patients with complex CAD, and early risk stratification and intervention based on this model may improve clinical outcomes.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the leading cause of death worldwide, with increasing prevalence and mortality rates, and coronary artery disease (CAD) remains the primary contributor, posing a significant threat to human health and a growing socioeconomic burden1. Complex CAD, which includes multivessel disease and lesions with complex morphology2, is a particularly severe subtype of CAD, often accompanied by comorbidities such as diabetes mellitus and hypertension. This type of CAD is associated with poor prognosis and has shown a rising prevalence over time. Despite considerable advancements in the diagnosis and treatment of CAD in modern medicine, the clinical outcomes of patients with complex CAD remain suboptimal, with delayed prevention and treatment being one of the major contributing factors. For patients with complex CAD, fractional flow reserve (FFR) and the SYNTAX score are commonly used to assess lesion severity and guide treatment strategies. However, FFR involves invasive procedures and pharmacological administration, which carry safety risks, and it is challenging to comprehensively evaluate the entire coronary tree in a single procedure. The SYNTAX score, which is based on the anatomical characteristics of coronary arteries, often fails to reflect the true severity of the disease. Computed tomography-derived fractional flow reserve (CT-FFR), an emerging noninvasive quantitative metric, combined with the SYNTAX score, offers a promising solution to these limitations.
The DISCOVER-FLOW trial3, a multicenter prospective study, demonstrated that CT-FFR has good diagnostic accuracy (84.3%) and specificity (82.2%) in identifying patients requiring revascularization, with a strong correlation to invasive FFR (R = 0.717, P < 0.001). The NXT trial4 further confirmed that CT-FFR has high sensitivity (86%, 95% CI 77%–92%) and specificity (79%, 95% CI 72%–84%) in detecting myocardial ischemia, which helps optimize treatment decisions and reduces unnecessary invasive procedures. Additionally, CT-FFR measurements have demonstrated reproducibility across different operators, with a low coefficient of variation of only 3.6% (95% CI 2.3%–4.6%)5. Currently, the application of CT-FFR in the diagnosis and management of coronary artery disease is being increasingly promoted and is expected to become a cost-effective first-line diagnostic tool in the future.
The functional SYNTAX score (FSS), based on CT-FFR, has been shown to guide risk stratification in patients with multivessel disease, yielding results comparable to those obtained via invasive pressure wire assessments, with better concordance than the anatomical SYNTAX score (ASS) (Kappa 0.32 vs. 0.19)6. FSS has also been validated as a superior predictor of major adverse cardiovascular events (MACE) in patients with triple-vessel disease and has led to changes in revascularization strategies for some patients7. This study aims to develop a predictive model to assess the 1-year risk of MACE in patients with complex CAD by combining FSS with traditional risk factors, facilitating early identification of high-risk patients and targeted interventions to improve clinical outcomes and optimize healthcare resource allocation.
Materials and methods
Definitions
-
(1)
Stable CAD (Chronic Coronary Syndrome)8: A range of clinical manifestations or syndromes caused by structural and/or functional changes associated with chronic disease of the coronary arteries and/or microcirculation. This includes: suspected CAD patients with stable angina symptoms and/or dyspnea; suspected CAD patients with newly developed heart failure or left ventricular dysfunction; asymptomatic or symptomatically stable patients within 1 year post-acute coronary syndrome (ACS) or recent revascularization; asymptomatic or symptomatic patients diagnosed for the first time or more than 1 year post-revascularization; patients with angina suspected to be caused by vasospasm or microvascular disease; and asymptomatic CAD patients identified during screening.
-
(2)
Complex CAD9,10: Defined as anatomical stenosis ≥ 50% in two or more major coronary arteries or the left main artery as identified by coronary computed tomography angiography (CCTA), or as meeting the criteria for multivessel disease2. This includes: left main or proximal left anterior descending artery lesion, chronic total occlusion, trifurcation lesion, complex bifurcation lesion, heavy calcification, severe tortuosity, aorto-ostial stenosis, diffusely diseased and narrowed segments distal to the lesion, thrombotic lesion, and lesion length > 20 mm. Usually, clinical conditions and baseline comorbidities of the patient need to be considered comprehensively.
-
(3)
MACE11: Defined as a composite of acute myocardial infarction, stroke, cardiovascular death, hospitalization for unstable angina or revascularization, and hospitalization for heart failure.
Study population
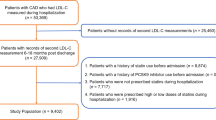
This study retrospectively analyzed 369 patients who underwent CCTA at Guangzhou Red Cross Hospital from January 2020 to September 2023 and met the criteria for "stable complex CAD" (see flowchart in Fig. 1). Inclusion criteria: (1) Patients aged ≥ 18 years with chronic coronary syndrome; (2) Patients meeting the above definition of complex CAD; (3) Patients with hospitalization records within one month before or after undergoing CCTA. Exclusion criteria: (1) Patients diagnosed with ACS during the current hospitalization; (2) Patients with malignant tumors, autoimmune vasculitis, mental disorders, or requiring hemodialysis; (3) Patients participating in other drug/device studies or with an expected life expectancy of less than one year. This study complies with the Declaration of Helsinki, and the acquisition and publication of research data were approved by the Ethics Committee of Guangzhou Red Cross Hospital (approval number: 2024–187-01) with written informed consent obtained from all patients.
Equipment information
The CCTA images in this study were acquired from three different CT scanners: (1) Hispeed ZX (large combination spiral type), manufactured by GE (General Electric) Company, USA; (2) Brilliance CT 64 Slice (large combination 128-slice spiral type ≥ 500mA), manufactured by Philips Company; (3) Spectral CT, manufactured by Philips Medical Systems Netherlands B.V.
Data collection and preprocessing
Clinical data collection included demographic characteristics, personal history, physical examinations upon admission, laboratory tests, and imaging studies. The CCTA images of the enrolled patients were analyzed for CT-FFR using RuiXin-FFR (version 1.0, Raysight Medical, China), conducted at Shenzhen Raysight Medical Technology Co., Ltd. Based on the CCTA and CT-FFR reports, two attending physicians or senior-level physicians independently calculated the ASS and FSS for each patient using the online SYNTAX Score calculator (https://syntaxscore.org/, including the scoring criteria) (Fig. 2A): (1) ASS: Vessels with anatomical stenosis ≥ 50% identified by the CCTA report were classified as lesion sites (e.g., regions marked by red and yellow triangles both qualify). The ASS was calculated using the online SYNTAX Score calculator based on the number of lesions in the patient’s coronary artery tree and the corresponding imaging features. (2) FSS: Vessels with anatomical stenosis ≥ 50% and CT-FFR ≤ 0.8 at the same site were classified as lesion sites (e.g., regions marked by red triangles meet the criteria, while those marked by yellow triangles do not). The FSS was similarly calculated using the online SYNTAX Score calculator based on the number of lesions in the patient’s coronary artery tree and the corresponding imaging features.
(A) Illustration of the SYNTAX score. (B) Coefficient plot of the 9 predictors preliminarily selected by LASSO regression. The coefficient corresponding to a variable represents the effect of a unit change in that variable on the outcome event (MACE). A positive value indicates a positive correlation (risk factor), while a negative value indicates a negative correlation (protective factor). (C) LASSO coefficient profiles of the 56 candidate predictors. (D) A coefficient profile plot against the log (Lambda) sequence. A vertical line indicates the value selected using tenfold cross-validation, where the optimal Lambda resulted in 7 predictors with non-zero coefficients (Lambda = 0.0396).
Based on the upper limit of normal clinical values, N-terminal prohormone of brain natriuretic peptide (NT-proBNP) and high-sensitivity troponin T (hs-TnT) were converted into binary variables using cutoff values of 125 pg/mL and 0.014 μg/L, respectively. For angiotensin-converting enzyme 2 (ACE2), D-dimer, pulse pressure, high-sensitivity C-reactive protein (hs-CRP), and other continuous variables, due to their excessively large or small ranges, this study used the occurrence of MACE as the dependent variable and the optimal cutoff values based on the ROC curve of the full dataset to convert them into binary variables. The 369 enrolled patients were randomly divided into a training set (N = 258) for model construction and a validation set (N = 111) for evaluating model performance in a 7:3 ratio.
Statistical methods
All statistical analyses in this study were performed using R software (version 4.3.2). Continuous variables conforming to normal distribution were expressed as x̅ ± s, while those not conforming to normal distribution were expressed as M (Q1, Q3). Comparisons between groups were conducted using the independent sample t-test for normal data and the rank-sum test for non-normal data. Categorical variables were expressed as n(%), and comparisons between groups were performed using the χ2 test or Fisher’s exact test. For missing data, variables with missing rates ≥ 20% were excluded, while those with missing rates < 20% were imputed using simple imputation: the median was used for continuous variables, and the mode for categorical variables. Based on the training set, predictive factors were selected using LASSO regression, and a risk prediction model was established using logistic regression, with a nomogram constructed. The predictive performance of the model was evaluated through ROC curves, calibration curves, decision curves, and reasonableness analysis in both the training and validation sets. All statistical tests were two-sided, with P < 0.05 considered statistically significant.
Results
Study population characteristics
A total of 369 patients were included in the study, with a mean age of (70.38 ± 9.22) years, and 242 males (65.58%). Among them, 145 patients (39.30%) experienced MACE within 1 year. Of the patients with MACE, 49.7% were hospitalized for unstable angina or underwent revascularization procedures, and 31.7% were hospitalized for heart failure. The mean ASS and FSS were 11.00 (9.00, 14.00) and 10.00 (7.00, 13.00), respectively. There were no statistically significant differences in baseline characteristics between the training and validation sets, with all indicators showing P > 0.05 (baseline characteristics are shown in Table 1).
Selected predictors and construction model
Using the training set, 56 variables, excluding ASS (due to multicollinearity with FSS), were subjected to dimensionality reduction via LASSO regression with tenfold cross-validation. The optimal model was determined by selecting the minimum lambda value (0.0396). The results identified 9 risk predictors (Fig. 2B–D): FSS, low-density lipoprotein cholesterol (LDL-C), NT-proBNP ≥ 125 pg/mL, hs-CRP ≥ 4.73 mg/L, left ventricular ejection fraction (LVEF), albumin, pulse pressure ≥ 72 mmHg, ACE2 ≥ 27.5 U/L, and diabetes. Based on these 9 predictors, a risk prediction model was constructed using Logistic regression with stepwise backward selection, and a nomogram was plotted (Fig. 3). Logistic regression finally included 7 independent risk predictors: FSS, LDL-C, LVEF, albumin, pulse pressure ≥ 72 mmHg, ACE2 ≥ 27.5 U/L, and diabetes (Table 2). The model’s Akaike information criterion (AIC) was 262.5.
Predictive model nomogram: Based on the values of each predictor for a patient, the corresponding scores can be obtained from the nomogram. These scores are summed to calculate the total score. The total score is then used to determine the corresponding predicted probability, providing the 1-year MACE probability for the patient.
Model performance validation
The predictive performance of the model was evaluated using the ROC curve (Fig. 4A). The AUC for the training and validation sets was 0.843 and 0.844, respectively. Sensitivity was 0.867 and 0.851, specificity was 0.694 and 0.750, Youden index was 0.561 and 0.601, F1-score was 0.733 and 0.777, and Kappa value was 0.524 and 0.586. When comparing the AUC of the functional score model (developed in this study) with the anatomical score model, FSS alone, and ASS alone, results showed that the functional score model had the highest AUC (Fig. 4B). The Hosmer–Lemeshow χ2 test was used to evaluate model fit, with χ2 values of 11.513 (P = 0.174) and 8.519 (P = 0.385) for the training and validation sets, respectively.
(A) ROC curve of the nomogram. (B) Comparison of ROC curves among the established predictive model and other models and risk factors. “FSS” = Functional SYNTAX score, “ASS” = Anatomical SYNTAX score, "Mod-FSS" = The predictive model established in this study, "Mod-ASS" = The predictive model with “FSS” replaced by "ASS."
Using 500 bootstrap samples, calibration curves were plotted (Fig. 5A-B), which demonstrated good calibration of the model, with mean absolute errors of 0.042 and 0.045, Dxy values of 0.686 and 0.689, and Brier scores of 0.159 and 0.160 for the training and validation sets, respectively. Similarly, clinical decision curves generated using 500 bootstrap samples (Fig. 5C-D) showed that at prediction probability thresholds in the range of 0.05–0.78 for the training set and 0.03–0.97 for the validation set, the net clinical benefit of using the predictive model exceeded both the “no intervention” and “full intervention” strategies, suggesting good clinical applicability of the model. Nomoscores were calculated for patients using the nomogram, and boxplots were created after grouping patients by MACE status (Fig. 5E-F). The results indicated significant differences in Nomoscore distributions between the groups in both the training and validation sets (P < 0.001), supporting the strong risk stratification performance of the nomogram. Based on the Nomoscores of patients from the full dataset, the optimal ROC cutoff (109.6) was calculated to categorize patients into high-risk (Nomoscore ≥ 110) and low-risk (Nomoscore < 110) groups.
Evaluation of the predictive model: (A) Calibration curve for the training cohort. The closer the “Apparent” curve and the “Bias-corrected” curve are to the “Ideal” curve, the better the predictive performance of the model. (B) Calibration curve for the validation cohort. (C) Clinical decision curve for the training cohort. The “Nomo” (red curve) represents clinical decisions made based on the predictive model. The “All” (gray line) reflects the scenario where all patients receive intervention, while the “None” (black line) represents the scenario where no patients receive intervention. The area where the red curve lies above both the “None” line and the “All” line indicates that the strategy using the predictive model provides greater net benefit compared to either intervening in all patients or withholding intervention altogether. (D) Clinical decision curve for the validation cohort. (E) Boxplot of group distributions based on Nomoscore in the training cohort. (F) Boxplot of group distributions based on Nomoscore in the validation cohort.
Discussion
Based on the characteristics of the patients included in this study, Logistic regression analysis identified FSS, LDL-C, LVEF, albumin, pulse pressure ≥ 72 mmHg, ACE2 ≥ 27.5 U/L, and diabetes as independent predictors of 1-year MACE in patients with stable complex CAD.
CT-FFR, with its advantages of being non-invasive, accurate, comprehensive, and reproducible, plays a significant role in cardiac functional assessment and has been incorporated into guidelines as a supplementary diagnostic tool, particularly for patients with complex CAD12. Currently, commercial platforms for obtaining CT-FFR via on-site workstations are available, demonstrating excellent diagnostic accuracy (80.6%, 95%CI 80.5%-80.7%), sensitivity (88.1%, 95% CI 82.4%-93.7%), and specificity (75.6%, 95% CI 69.6%-81.7%)13. The introduction of on-site workstations has made the clinical application of CT-FFR more efficient and convenient. The SYNTAX score is a commonly used quantitative measure for assessing the severity of disease in patients with complex CAD. However, ASS reflects only the anatomical coronary lesions and may overestimate the severity of the disease, potentially interfering with the selection of the optimal treatment strategy. FSS, which combines CT-FFR with the SYNTAX score, provides an assessment of the functional severity of coronary lesions, offering better guidance for treatment planning. Studies have shown that FSS provides risk stratification results for multivessel disease patients that are comparable to those obtained using pressure wire-measured FFR (21.6 ± 7.8 vs. 21.2 ± 8.8, P = 0.589), with greater consistency than ASS (kappa 0.32 vs. 0.19)6. Furthermore, compared to ASS, FSS is a better predictor of MACE in patients with three-vessel disease (AUC: 0.81 vs. 0.75, P = 0.01)7. This study also concluded that FSS is the best independent predictor of 1-year MACE in patients with stable complex CAD (OR = 1.258, P < 0.001). Therefore, for patients diagnosed with complex CAD via CCTA or coronary angiography, even if their condition is stable, further evaluation with CT-FFR is recommended to assess the disease using FSS. For the population included in this study, disease progression in elderly CAD patients is often unpredictable and rapid. Any exacerbation of the condition would impose a significant burden on the patient. Moreover, elderly patients are often less willing to undergo invasive coronary angiography. Thus, CCTA and CT-FFR could be considered as regular evaluation tools for this population, with treatment plans optimized based on the results of these assessments.
LDL-C, known as "bad cholesterol," is considered a major causative factor for atherosclerotic cardiovascular disease (ASCVD) due to its role in promoting inflammation and foam cell formation through oxidized LDL-C, leading to atherosclerosis and cardiovascular damage14,15. Retrospective database analyses have shown that LDL-C is independently associated with the risk of MACE in ASCVD patients (HR = 1.19, 95% CI 1.16–1.22, /1mmol/L)16. A 10-year follow-up study further demonstrated that elevated LDL-C levels are independently associated with an increased risk of cardiovascular mortality, even in low-risk ASCVD populations17. The results of this study indicate that elevated LDL-C is an independent risk factor for 1-year MACE in patients (OR = 1.487, 95% CI 1.147–1.963, /1 mmol/L). Therefore, lowering LDL-C levels can improve clinical outcomes regardless of baseline conditions and risk stratification. In this study population, cholesterol control remains suboptimal, primarily due to unhealthy lifestyles, insufficient chronic disease management, and poor adherence to lipid-lowering therapies. Thus, clinicians should emphasize the combined use of medications and the promotion of healthy lifestyle interventions.
LVEF reflects cardiac function and structural remodeling and is considered a valuable diagnostic and prognostic tool18. A cohort study of ASCVD patients showed that those with an LVEF below 65% had a 1.3-fold higher risk of MACE compared to those with an LVEF ≥ 65%, while patients with an LVEF < 55% had a mortality risk more than 3.5 times higher than those with an LVEF ≥ 55%19. Consistent with these findings, this study also identified reduced LVEF as an independent risk factor for MACE. However, large cohort studies have reported a U-shaped, rather than linear, relationship between LVEF and mortality risk, with the lowest risk observed when LVEF is between 60 and 65%20. Elevated LVEF beyond the normal range may indicate a compensatory response in the pre-heart failure stage. Therefore, for CAD patients with concomitant heart failure, early initiation of the “new quadruple” therapy for heart failure is recommended, regardless of whether LVEF is already reduced, to delay ventricular remodeling and improve clinical outcomes.
Human serum albumin, the most abundant carrier protein in plasma, binds to various ligands (including drugs) and plays an important role in the transport, distribution, and metabolism of substances21. Hypoalbuminemia typically reflects conditions such as malnutrition, chronic disease, or inflammation. Numerous studies have demonstrated that hypoalbuminemia is a strong predictor of increased all-cause and cardiovascular mortality22. Additionally, hypoalbuminemia at admission is associated with elevated mortality, while normalization of albumin levels before discharge is linked to a lower risk of death23. Supplementing human albumin is a reasonable therapeutic strategy for patients with hypoalbuminemia; however, its efficacy requires further investigation. In general, improving nutritional intake and managing underlying diseases should be prioritized in patients with hypoalbuminemia. For elderly patients requiring intravenous infusion of human albumin, the infusion rate and dosage should be strictly controlled to avoid precipitating or exacerbating heart failure symptoms.
Pulse pressure, defined as the difference between systolic and diastolic blood pressure, is an important indicator of arterial elasticity, with elevated pulse pressure commonly caused by large artery stiffness. High pulse pressure (≥ 60 mmHg) is a functional marker of target organ damage, and hypertensive patients with high pulse pressure have a significantly increased risk of MACE compared to those with normal pulse pressure (HR = 1.57, 95% CI 1.12–2.22, P = 0.01)24. A multicenter observational study demonstrated that the prevalence of elevated pulse pressure (≥ 60 mmHg) increases linearly with age (R2 = 0.979) and is independently associated with increased cardiovascular risk (OR = 3.41, 95% CI 3.08–3.77)25. The conclusions of this study are similar; however, the definition of high pulse pressure in this study was set at ≥ 72 mmHg, which was determined as the optimal ROC cutoff based on the full dataset, possibly reflecting the predominantly elderly population included in the study. Therefore, this conclusion may not be generalizable to all populations. Nevertheless, it is well-established that actively managing blood pressure, implementing antiplatelet and lipid-lowering therapies, and promoting a healthy lifestyle in patients with high pulse pressure are beneficial and can reduce the risk of MACE.
ACE2 plays a critical role in the progression of CVD, particularly in the development of hypertension and heart failure with reduced ejection fraction26. A global multicenter cohort study demonstrated that increased plasma ACE2 concentrations are associated with a higher risk of mortality (HR = 1.35 /SD, 95% CI 1.29–1.43) and identified ACE2 as the best predictor of mortality risk27. Similarly, this study concluded that ACE2 ≥ 27.5 U/L (normal range: 6.0–86.0 U/L) is an independent risk factor for MACE. The 27.5 U/L threshold is not a high value within the normal range but rather the optimal ROC cutoff determined from the full dataset. The findings of this study suggest that maintaining relatively low plasma ACE2 levels is beneficial for the cardiovascular system. For example, the early use of ACE inhibitor (ACEI) in hypertensive and heart failure patients can confer significant benefits. However, ACE2 concentration is not routinely measured in clinical practice, particularly in smaller hospitals, and prior studies on ACE2 remain limited. These factors restrict the generalizability of this study’s conclusions. Therefore, further research is needed to confirm the impact of ACE2 concentrations on the human body and to explore its risk thresholds.
Diabetes is a traditional risk factor for CAD, with hyperglycemia and insulin resistance being key mechanisms in the progression of atherosclerosis and its complications28. Studies have shown that type 2 diabetes is a significant prognostic predictor in CAD patients, and effective glycemic control can substantially improve their outcomes29. Randomized controlled trials have demonstrated that diabetic patients with multivessel CAD have higher 5-year all-cause mortality rates following any revascularization strategy compared to non-diabetic patients30. Therefore, it is essential for patients with diabetes to actively manage blood glucose levels and adopt healthier lifestyles. For those with concomitant heart failure, the "new quadruple " therapy is particularly recommended for heart failure management.
For patients with stable complex CAD, the predictive model established in this study can be used for disease assessment. Patients with a Nomoscore < 110 can be managed with secondary prevention of CAD and undergo regular follow-ups based on their individual conditions (e.g., after one year). For patients with a Nomoscore ≥ 110, elective revascularization is recommended in addition to secondary prevention of CAD. High-risk patients with an FSS < 22 are advised to undergo percutaneous coronary intervention (PCI), while those with an FSS ≥ 22 or left main CAD combined with diabetes are recommended to undergo coronary artery bypass grafting (CABG).
It is important to note that the 1-year MACE incidence in this study was 39.30%, which is higher than the rates reported in most studies. We consider the following reasons for this discrepancy: First, this study defined MACE using a "five-point MACE" criterion (a composite of acute myocardial infarction, stroke, cardiovascular death, hospitalization for unstable angina or revascularization, and hospitalization for heart failure), which naturally results in a higher event rate compared to studies using the "three-point MACE" definition (a composite of acute myocardial infarction, stroke, and cardiovascular death). Second, the population in this study consisted of patients with "complex CAD," whose MACE incidence is significantly higher than that of the general “CAD” population. Third, the average age of the study cohort was higher than that of most studies, and there were regional differences in the population. These factors all contribute to the statistical outcomes of the endpoint events. Age, as an important prognostic predictor for CAD patients, has been well-documented in previous studies. However, this study’s predictive model did not include “age” as a variable, which warrants further consideration. Upon reviewing the data, we found that the study population had a relatively high mean age (70.38 ± 9.22 years) with a narrow distribution range, leading to statistically insignificant differences between groups. This limitation may affect the model’s applicability to populations in other age ranges, particularly the middle-aged population, which has shown an increasing incidence of CAD in recent years. Additionally, it should be noted that the assessment of coronary artery anatomical stenosis in this study was based on CCTA findings rather than the “gold standard” of coronary angiography. Although CCTA, as a non-invasive modality, has been shown to have good diagnostic performance for anatomical evaluation in patients with chronic coronary syndromes, this distinction should be considered31. In summary, the results of this study are based on the characteristics of the current sample, and the lack of external validation necessitates caution when applying the model to other populations with different characteristics.
Limitations
(1) This study is a single-center, small-scale retrospective study, which is subject to selection bias. The regional characteristics of the enrolled patients are strong, the age distribution is narrow, and there is a lack of an external validation cohort. The stability and clinical applicability of the predictive model require further improvement. (2) Coronary artery calcification scoring was not performed in this study. Although we excluded as many patients with severe coronary calcification as possible, the presence of calcified plaques may still affect the accuracy of CT-FFR results. (3) The study follow-up period included the outbreak of the COVID-19 pandemic, which may have led to an underestimation of the actual incidence of endpoint events due to difficulties in seeking medical care. Conversely, the insufficient treatment of underlying diseases and the increased risk of pneumonia and other infections may have resulted in an overestimation of the actual incidence of endpoint events.
Conclusion
This study constructed a clinical predictive model based on CT-FFR-derived FSS through retrospective analysis to evaluate the 1-year MACE risk in patients with complex CAD. The results demonstrated that the model has good predictive performance and clinical utility, offering the potential to guide risk stratification and improve patient outcomes through tailored clinical management. However, the study population was limited to a specific regional cohort with a narrow age distribution. Future multicenter studies and external validation are urgently needed to further assess the model’s applicability and value.
Data availability
To protect patient confidentiality, the raw data used in this study are not publicly accessible but are available from the corresponding author or first author upon reasonable request. The dataset is stored in a controlled-access repository at Guangzhou Red Cross Hospital.
Change history
28 May 2025
The original online version of this Article was revised: In this article Weiqing Luo and Chen Li should have been denoted as equally contributing authors.
10 April 2025
A Correction to this paper has been published: https://doi.org/10.1038/s41598-025-96993-6
References
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol 76, 2982–3021 (2020).
Writing Committee Members et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: A report of the American college of Cardiology/American heart association joint committee on clinical practice guidelines. J. Am. Coll. Cardiol. 79, e21–e129 (2022).
Koo, B.-K. et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol 58, 1989–2973 (2011).
Nørgaard, B. L. et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol 63, 1145–1155 (2014).
Gaur, S. et al. Fractional flow reserve derived from coronary CT angiography: variation of repeated analyses. J Cardiovasc Comput Tomogr 8, 307–314 (2014).
Collet, C. et al. Fractional Flow Reserve Derived From Computed Tomographic Angiography in Patients With Multivessel CAD. J Am Coll Cardiol 71, 2756–2769 (2018).
Qiao, H. Y. et al. Prognostic implication of CT-FFR based functional SYNTAX score in patients with de novo three-vessel disease. Eur Heart J Cardiovasc Imaging https://doi.org/10.1093/ehjci/jeaa256 (2020).
Vrints, C. et al. 2024 ESC Guidelines for the management of chronic coronary syndromes. Eur Heart J 45, 3415–3537 (2024).
Witberg, G. et al. Heart team/guidelines discordance is associated with increased mortality: data from a national survey of revascularization in patients with complex coronary artery disease. Circ Cardiovasc Interv 14, e009686 (2021).
Kawashima, H. et al. Diagnostic concordance and discordance between angiography-based quantitative flow ratio and fractional flow reserve derived from computed tomography in complex coronary artery disease. J Cardiovasc Comput Tomogr 16, 336–342 (2022).
Bosco, E., Hsueh, L., McConeghy, K. W., Gravenstein, S. & Saade, E. Major adverse cardiovascular event definitions used in observational analysis of administrative databases: a systematic review. BMC Med Res Methodol 21, 241 (2021).
Rajiah, P., Cummings, K. W., Williamson, E. & Young, P. M. CT fractional flow reserve: a practical guide to application, interpretation, and problem solving. Radiographics 42, 340–358 (2022).
Hwang, D. et al. Diagnostic performance of on-site automatic coronary computed tomography angiography-derived fractional flow reserve. Korean Circ J 54, 382–394 (2024).
Pirillo, A., Casula, M., Olmastroni, E., Norata, G. D. & Catapano, A. L. Global epidemiology of dyslipidaemias. Nat Rev Cardiol 18, 689–700 (2021).
Khatana, C. et al. Mechanistic insights into the oxidized low-density lipoprotein-induced atherosclerosis. Oxid Med Cell Longev 2020, 5245308 (2020).
Morgan, C. L. et al. Risk of major adverse cardiovascular events associated with elevated low-density lipoprotein cholesterol in a population with atherosclerotic cardiovascular disease with and without type 2 diabetes: a UK database analysis using the clinical practice research datalink. BMJ Open 13, e064541 (2023).
Abdullah, S. M. et al. Long-term association of low-density lipoprotein cholesterol with cardiovascular mortality in individuals at low 10-year risk of atherosclerotic cardiovascular disease. Circulation 138, 2315–2325 (2018).
Marwick, T. H. Ejection fraction pros and cons: JACC state-of-the-art review. J Am Coll Cardiol 72, 2360–2379 (2018).
Liu, Y. et al. Association of ejection fraction with mortality and cardiovascular events in patients with coronary artery disease. ESC Heart Fail 9, 3461–3468 (2022).
Wehner, G. J. et al. Routinely reported ejection fraction and mortality in clinical practice: where does the nadir of risk lie?. Eur Heart J 41, 1249–1257 (2020).
Rabbani, G. & Ahn, S. N. Structure, enzymatic activities, glycation and therapeutic potential of human serum albumin: a natural cargo. Int J Biol Macromol 123, 979–990 (2019).
Manolis, A. A., Manolis, T. A., Melita, H., Mikhailidis, D. P. & Manolis, A. S. Low serum albumin: a neglected predictor in patients with cardiovascular disease. Eur J Intern Med 102, 24–39 (2022).
Akirov, A., Masri-Iraqi, H., Atamna, A. & Shimon, I. Low albumin levels are associated with mortality risk in hospitalized patients. Am J Med 130(1465), e11-1465.e19 (2017).
Mancusi, C. et al. Higher pulse pressure and risk for cardiovascular events in patients with essential hypertension: the Campania salute network. Eur J Prev Cardiol 25, 235–243 (2018).
Moyá-Amengual, A. et al. Elevated pulse pressure and cardiovascular risk associated in Spanish population attended in primary care: IBERICAN study. Front Cardiovasc Med 10, 1090458 (2023).
Úri, K. et al. Circulating ACE2 activity correlates with cardiovascular disease development. J Renin Angiotensin Aldosterone Syst 17, 1470320316668435 (2016).
Narula, S. et al. Plasma ACE2 and risk of death or cardiometabolic diseases: a case-cohort analysis. Lancet 396, 968–976 (2020).
Bornfeldt, K. E. & Tabas, I. Insulin resistance, hyperglycemia, and atherosclerosis. Cell Metab 14, 575–585 (2011).
Ahmad, A. et al. Precision prognostics for cardiovascular disease in Type 2 diabetes: a systematic review and meta-analysis. Commun Med (Lond) 4, 11 (2024).
Head, S. J. et al. Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: a pooled analysis of individual patient data. Lancet 391, 939–948 (2018).
Bergamaschi, L. et al. The role of non-invasive multimodality imaging in chronic coronary syndrome: anatomical and functional pathways. Diagnostics (Basel) 13, 2083 (2023).
Funding
This study was supported by Guangzhou Science and Technology Program Project funded by the Guangzhou Science and Technology Bureau (Grant Number: 2023A03J0982).
Author information
Authors and Affiliations
Contributions
All the authors contributed to this manuscript and approved the submitted version of the manuscript. Shaoheng Zhang, Weiqing Luo and Chen Li conceived designed the research strategy. Weiqing Luo wrote the manuscript text. Shaoheng Zhang, Chen Li and Guangdong Yan revised the manuscript. Weiqing Luo, Zhichuan Huang and Yilin Yue collected the clinical data. Shaoheng Zhang, Deguang Yang and Guangdong Yan contributed to the analysis and interpretation of the data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: In the original version of this Article, Affiliation 2 and 1 were not listed in the correct order. Full information regarding the corrections made can be found in the correction for this Article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Luo, W., Li, C., Yan, G. et al. Predictive model development combining CT-FFR and SYNTAX score for major adverse cardiovascular events in complex coronary artery disease. Sci Rep 15, 7152 (2025). https://doi.org/10.1038/s41598-025-91708-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-91708-3