Abstract
Drug-coated balloon (DCB) treatment is an emerging strategy for de novo coronary artery disease (CAD), but procedural optimization remains uncertain. This study analyzed 317 patients who underwent DCB-based intervention for de novo CAD and angiographic follow-up: SR (successful, stent-like result: diameter stenosis < 20% at follow-up angiography, n = 84, 93 lesions) and Non-SR (n = 224, 358 lesions) groups. Baseline clinical and lesion characteristics were similar, except that SR lesions had larger diameter. In SR lesions, specialty balloons were more frequently utilized (p = 0.025), and maximal balloon diameter and balloon-to-artery ratio were significantly greater compared to Non-SR lesions (p < 0.001 and p = 0.008). At a median 8-month follow-up, SR lesions exhibited larger minimal luminal diameter (MLD) and lower late lumen loss, with negative values indicating positive vessel remodeling. In multivariate analysis, post-DCB MLD (odds ratio 1.17 per 0.1 mm increase, p < 0.001) and balloon-to-artery ratio (odds ratio 1.43 per 0.1 increase, p = 0.002) were independent predictors for successful angiographic outcomes with thresholds of 1.95 mm for post-DCB MLD and 1.13 for balloon-to-artery ratio. In 47 patients, IVUS guidance resulted in balloon-to-artery ratio of 1.23 as calculated by QCA. The study demonstrated the importance of achieving maximal post-DCB MLD through aggressive lesion predilation, underscoring the need for refining procedural strategies.
NCT04619277 (Impact of Drug-Coated Balloon Treatment in De Novo Coronary Lesion).
Similar content being viewed by others
Introduction
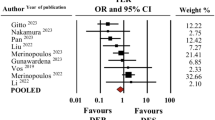
Drug-coated balloon (DCB) treatment represents an emerging therapeutic strategy for the management of obstructive coronary artery disease (CAD)1. Its established safety and efficacy profiles in addressing conditions such as in-stent restenosis (ISR)2 have spurred ongoing investigations aimed at elucidating its applicability across a broader spectrum of CAD including de novo native coronary lesions1,2,3. In a meta-analysis, the use of DCBs was shown to have an efficacy profile comparable to drug-eluting stents (DES) in the treatment of de novo lesions, resulting in similar outcomes across clinical endpoints, including target lesion or vessel revascularization, myocardial infarction, and mortality3. However, DCB treatment was associated with poorer angiographic surrogate endpoint such as a significantly higher percentage diameter stenosis (%DS) and smaller minimal luminal diameter (MLD) at angiographic follow-up3.
Optimal lesion preparation is increasingly recognized as a pivotal step to enhance the efficacy of DCB treatment1,4. This approach is instrumental for ensuring effective plaque modification and achieving sufficient luminal gain to restore and accommodate physiologic coronary blood flow. Additionally, it facilitates drug transfer to a broader contact area, thereby enhancing the therapeutic benefits of DCB treatment with the concept of “leaving nothing behind”. In previous study exploring key procedural factors in treating ISR lesions using DCBs, the predictors of target lesion failure (TLF) included residual DS ≥ 20%, DCB-to-stent ratio ≤ 0.91, and inflation time ≤ 60 s, emphasizing the importance of procedural optimization5. However, for de novo coronary lesions, there has been a lack of studies exploring specific procedure-related factors predictive of successful DCB outcomes. In this study, we aimed to evaluate the prognostic value of various procedure-related factors on angiographic outcomes in patients undergoing DCB treatment for de novo lesions.
Results
Study population
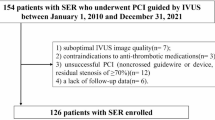
This study was based on the all-comers prospective registry that was conducted at Korea University Ansan Hospital from July 2019 to February 2023 (Impact of Drug-Coated Balloon Treatment in De Novo Coronary Lesion; NCT04619277). A total of 308 patients who underwent angiographic follow-up were analyzed. Exclusions were made for individuals with ISR, restenosis after DCB treatment (n = 2), heavily calcified lesions treated by rotational atherectomy (n = 1), coronary lesions in grafted vessels or transplanted hearts (n = 1), and coronary lesions unsuitable for QCA measurement, such as chronic total occlusion lesions (n = 5) (Fig. 1).
This study specifically focused on identifying crucial procedural steps to achieve favorable angiographic results comparable to those of DESs. Given that earlier studies reported a mean %DS of approximately 20% after paclitaxel-based DES implantation (Supplementary Table 1 and Supplementary Figure 1)6,7, the study population was categorized into two groups based on follow-up angiographic findings: the SR (successful, stent-like result, %DS < 20%, n = 84, 93 lesions) group and the Non-SR group (%DS ≥ 20%, n = 224, 358 lesions) (Fig. 1). During a median follow-up of 24.0 months (interquartile range [IQR]: 13.8–34.6), the overall incidence of TLF was 5.2% (16/308) in the study population.
Baseline clinical characteristics
The baseline clinical characteristics of the study population are shown in Table 1. In overall study population treated with DCBs, 78.0% (240/308) presented with acute coronary syndrome, with 26.3% (81/308) experiencing acute MI. Chronic kidney disease was present in 13.3% (41/308) of the patients, while 28.4% (87/308) had left ventricular dysfunction. Baseline clinical characteristics, including demographics, comorbidities, cardiac risk factors, laboratory findings, and angiographic disease extent, were comparable between the SR and Non-SR groups.
Lesion and procedural characteristics
In terms of lesion characteristics (Table 2), 74.3% (335/451) of the target lesions were located in the major epicardial arteries, and 74.7% (337/451) were classified as type B2 or C according to the American College of Cardiology/American Heart Association classification. Lesion location and complexity were similar between the two groups. There was a difference in SR according to angiographic lesion morphology (concentric, eccentric, and multiple irregularities) (p = 0.042); however, no significant trend was observed across lesion morphology types (p for trend = 0.267). Angiographic calcification severity was associated with SR (p = 0.048), with a trend toward lower success rates as calcification severity increased (p for trend = 0.035). Quantitatively, angiographic lesion characteristics were comparable, except for a larger RVD in the SR compared to the Non-SR group (2.66 ± 0.48 vs. 2.49 ± 0.47 mm; p = 0.001).
Regarding procedural characteristics, specialty balloons (scoring: 96.5% and non-compliant balloon: 3.5%) were more frequently used for lesion preparation in the SR group (54.8% vs. 41.9%; p = 0.025). Regarding the DCB profile, the SR group displayed significantly larger values for maximal balloon diameter (3.19 ± 0.52 vs. 2.90 ± 0.48 mm; p < 0.001) and B-A ratio (1.129 ± 0.107 vs. 1.095 ± 0.109; p = 0.008) compared to the Non-SR group. The occurrence of angiographically significant coronary artery dissection did not show any significant difference between the groups. Post-DCB QCA measurements of RVD, MLD, and acute luminal gain showed significantly larger values in the SR group.
Angiographic follow-up: vessel remodeling and MLD changes
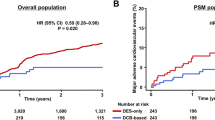
The median duration from the index PCI to angiographic follow-up was 8.0 months (IQR: 6.0–11.0). Follow-up QCA measurements of RVD and MLD showed significantly larger values in the SR than in the Non-SR group. In particular, the degree of LLL showed significant difference between the groups (− 0.21 ± 0.32 vs. 0.11 ± 0.41 mm; p < 0.001), with the SR group exhibiting a negative mean LLL value, indicative of positive vessel remodeling after DCB treatment. The distribution curves of MLD changes are shown in Fig. 2. Both the SR and Non-SR groups exhibited a significant difference between post-DCB and follow-up MLD measurements in pairwise comparisons. Specifically, MLD measurements significantly increased in the SR group (post-DCB vs. follow-up: 2.14 ± 0.47 vs, 2.37 ± 0.38 mm, p < 0.001) and decreased in the Non-SR group (post-DCB vs. follow-up: 1.83 ± 0.44 vs. 1.72 ± 0.48 mm, p < 0.001). The percentage increase in MLD was 13.41 ± 18.51% in the SR group and − 4.20 ± 23.32% in the non-SR group (p < 0.001).
Predictors of successful angiographic outcomes: multivariate analysis and ROC curves
In multivariate logistic regression analysis (Table 3), we systematically examined a wide range of peri-procedural factors including lesion characteristics, procedural parameters, and angiographic QCA measurements, for predicting optimal angiographic outcome. Following forward conditional analysis, post-DCB MLD (per 0.1 mm increase; odds ratio [SR] 1.168, 95% confidence interval [CI] 1.141–1.198; p < 0.001) and B-A ratio (per 0.1 increase; SR 1.432, 95% CI 1.318–1.547; p = 0.002) remained as robust independent predictors for successful angiographic outcomes following DCB treatment. Correlation analysis also demonstrated no inter-dependence between post-DCB MLD and B-A ratio (Pearson’s correlation coefficient r = − 0.065, p = 0.171). In ROC curve analyses, the optimal thresholds for predicting successful DCB outcome based on the Yuden index was determined as 1.940 mm for post-DCB MLD (area under curve [AUC] 0.684) and 1.126 for B-A ratio (AUC 0.578) (Fig. 3). Combining these factors increased the overall predictive power to an AUC of 0.703.
ROC curve analyses generated for predicting optimal DCB outcome. ROC curves generated by post-DCB MLD (Left), balloon-to-artery ratio (Middle), and the combined variable of post-DCB MLD and balloon-to-artery ratio (Right). AUC, area under the curve; DCB, drug-coated balloon; MLD, minimal luminal diameter; ROC, receiver operating characteristic.
We conducted an additional logistic regression analysis to evaluate the impact of fulfilling the thresholds derived from the ROC analysis—post-DCB MLD (≥ 1.940 mm) and balloon-to-artery (B-A) ratio (≥ 1.126)—on SR. Among the 65 lesions that met both thresholds, 28 (43.1%) achieved SR, whereas only 15 of 148 lesions (10.1%) in the group that did not meet either threshold were SR. In the group that met only one threshold (238 lesions), 50 (21.0%) achieved SR. Consequently, achieving either threshold was associated with 2.845 times higher odds of SR (OR = 2.845, 95% CI: [1.59, 5.09], p < 0.001), while achieving both thresholds yielded 6.710 times higher odds of SR (OR = 6.710, 95% CI: [3.25, 13.87], p < 0.001) compared to achieving neither threshold (Supplementary Table 2).
Impact of IVUS guidance on vessel measurements and balloon sizing
Our study included a subgroup of 47 patients who received IVUS-guided DCB treatment for a total of 56 de novo lesions. We compared IVUS measurements and the balloon sizes utilized in these procedures with the RVD obtained from QCA (Table 4). Compared to QCA, IVUS revealed significantly larger vessel diameters based on the external elastic membrane diameter. The nominal diameter of pre-dilation balloons chosen by attending interventionists was 11% greater compared to QCA-derived RVD (B-A ratio: 1.11 ± 0.14). Ultimately, IVUS guidance resulted in a final B-A ratio of 1.23 ± 0.14, as calculated by QCA.
Discussion
In this all-comer prospective study, we investigated the prognostic significance of various procedural characteristics on angiographic outcomes of DCB treatment for de novo coronary lesions. The key findings of the present study were as follows: First, notable disparities were observed in procedural characteristics between the lesions demonstrating successful, stent-like DCB results (SR) at angiographic follow-up and those not (Non-SR), particularly with the use of balloons with larger B-A ratio identified as an independent predictor of the success. Second, the significance of this distinct procedural step was corroborated by an improved immediate post-DCB angiographic outcomes, with a greater acute luminal gain and a larger MLD. Finally, these differences ultimately translated into a more favorable follow-up angiographic outcome in the SR group, characterized by a larger final MLD and positive vessel remodeling (Fig. 4).
Current expert consensus documents commonly recommend a B-A ratio of approximately 0.8 to 1.0 for DCB angioplasty1,4. This recommended range considered to balance adequate lesion expansion and drug delivery against the potential risks of vessel injury. However, these recommendations are largely based on expert experience and consensus opinion, rather than robust clinical data1,4. Moreover, these guidelines do not provide detailed guidance on the measurement methods for determining RVD, such as whether visual assessment or QCA should be used, or whether to consider the distal, proximal, or mean RVD.
Historically, in the pre-stent, percutaneous transluminal coronary angioplasty (PTCA) era, a higher B-A ratio of >1.0 was often suggested8,9. Specifically, lesion preparation conducted by balloons with B-A ratio ranging from 0.9 to 1.3, as assessed by cine angiography, yielded optimal outcomes by minimizing dissections and residual stenosis10. The positive impact of oversized devices on procedural and clinical outcomes was also well documented for the DES therapy11. These insights from the historical studies are particularly relevant to our findings, emphasizing the importance of oversized ballooning in lesion preparation. Specifically, our data demonstrated that a 0.1 increase in the B-A ratio was associated with 43.2% increase in the odds of achieving favorable angiographic outcome at the median 8-month follow-up. In this context, a recent study explored a DCB strategy involving gradual, prolonged predilation with perfusion balloons, targeting a B-A ratio greater than 1:1 (a range of 1.0 to 1.1 strongly recommended)12. This approach demonstrated an acceptable procedural success rate and favorable 24-month clinical outcomes in high-risk acute coronary syndrome patient subsets. Notably, although limited by a small sample size (n = 30), this study highlighted the feasibility of a predilation strategy involving a B-A ratio exceeding the recommended range12. Given these insights, a stepwise predilation strategy, gradually dilating from low pressure, may help mitigate serious vascular injury and acute recoil. These findings collectively suggest that further well-designed clinical investigations are warranted to refine the optimal B-A ratio and improve procedural strategies for achieving better angiographic and clinical outcomes in DCB treatment for de novo CAD.
It is widely acknowledged that RVD is typically larger by intravascular imaging (IVI) than by angiography13. An earlier study by Stone GW et al. demonstrated that IVUS-guidance, compared to angiography-guided PTCA, resulted in balloon upsizing in 73% of participants, increasing B-A ratio from 1.12 ± 0.15 to 1.30 ± 0.17 (p < 0.0001)8. This IVUS-guided PTCA led to a significant decrease in mean angiographic %DS and an increase in MLD, without significantly increasing peri-procedural complications8. The benefits of IVUS- versus angiography-guided PCI have also been well recognized in DES therapy14,15. In the ULTIMATE trial, IVUS-guided PCI led to more frequent post-dilation using larger balloons at higher pressures, resulting in a significantly greater MLD after DES implantation14,15. These specific procedural characteristics are suggested to translate into improved clinical outcomes14,15. Furthermore, a pooled analysis based on two randomized clinical trials (IVUS-XPL and ULTIMATE), stent oversizing of stent-to-vessel ratio of 1.1 to 1.3 was associated with better angiographic and clinical outcomes14,15,16,17.
The present study demonstrated that IVUS measures larger vessel diameters than QCA. Evidence from the PTCA era highlights that successful angioplasty requires sufficient vessel overstretching up to the adventitial layer18. Angiography, being limited to a two-dimensional lumen view and highly dependent on projection angle, often results in vessel under-sizing, as demonstrated previously13. Balloon sizing based solely on luminography risks under-dilation, particularly in vessels with significant atherosclerotic burden. In contrast, IVUS-guided assessment provides detailed visualization from the lumen to the external elastic membrane (EEM), enabling precise balloon selection essential for optimizing angioplasty outcomes. Accordingly, the ULTIMATE III trial recently demonstrated that, despite comparable baseline lesion RVDs, IVUS-guidance led to the use of significantly larger balloons compared to angiography guidance, leading to lower LLL in patients undergoing DCB treatment for de novo CAD19. Our analysis provides evidence that IVUS guidance led to a higher B-A ratio of 1.23 ± 0.14 through a more detailed assessment of target lesion anatomy. Further studies are warranted to determine more detailed, systematic balloon sizing strategy based on IVI and its impact on patient outcomes after DCB treatment. Moreover, future investigations should also assess the cost-effectiveness of IVI guidance in DCB treatment, balancing its clinical benefits against the economic challenges of its routine implementation20.
A previous study demonstrated that post-procedural MLD significantly predicted successful DCB treatment in de novo small vessel CAD21. Our study consistently demonstrated these findings, underscoring the importance of achieving sufficient luminal enlargement immediately after the procedure. Numerous studies on stent-based PCI have consistently shown a strong association between larger final stent dimensions and reduced rates of ISR, supporting the concept of “the larger, the better”15,17,22,23. In the context of DCB treatment, this relationship is particularly pertinent since DCBs, unlike stents, do not provide scaffolding to maintain vessel patency. Evidences from the PTCA era showed that repeated balloon overstretch using balloons with bigger B-A ratio alleviated early vessel recoil24. Furthermore, adequate luminal gain after PCI might facilitate the restoration of coronary laminar flow, leading to a favorable shear stress environment. Shear stress, the force exerted by blood flow on the vessel wall, plays a pivotal role in vascular biology and regulating vessel healing25. In the case of DCB treatment, enlarged lumen without residual metallic scaffold might promote a favorable hemodynamic microenvironment, potentially reducing the risks of abnormal vasomotion, thrombus formation, and neointimal proliferation/restenosis25,26.
In our study, specialty balloons, predominantly scoring balloons, were more frequently used in SR group. However, they were not identified as an independent predictor in the multivariable logistic regression analysis. This observation should be interpreted with caution, as it does not necessarily imply that specialty balloons are ineffective. Instead, their impact may have been overshadowed in the presence of stronger predictive factors such as B-A ratio or post-DCB MLD, which are more directly linked to immediate postprocedural outcomes. Furthermore, the relatively marginal difference in specialty balloon use between groups (54.8% in the SR group vs. 41.9% in the Non-SR group; p = 0.025), reflecting limited variability in procedural strategies, may have further reduced the statistical power to detect its independent effect.
Scoring balloons play a crucial role in controlled plaque modification, achieving sufficient luminal gain, and reducing the risk of serious vessel injury during the course of various endovascular intervention27,28. Their positive impact in DCB treatment has been well demonstrated in treating coronary ISR29,30. Moreover, a recent study demonstrated that the utilization of a scoring balloon was associated with reduced risk of severe dissection and more favorable angiographic outcomes in treating de novo coronary lesions31. Accordingly, in our study, despite the larger maximum balloon diameter and B-A ratio observed in the SR group compared to the Non-SR group, there was no significant difference in the occurrence of coronary dissection in our study. These findings underscore the complexity of factors influencing DCB treatment outcomes and suggest that scoring balloons might still play a valuable, albeit not singularly decisive, role within the broader context of procedural strategy. Future studies with larger cohorts and more standardized procedural strategies are required to further investigate the incremental value of specialty balloons in optimizing DCB outcomes.
In the present study, only paclitaxel-coated balloons were used, which limits the generalizability of our findings to limus-coated balloons. The AUC value obtained from the ROC analysis for the B-A ratio was relatively modest. Given the current recommendation of a B-A ratio between 0.8 and 1.0, attending interventionists tend to adhere closely this range, resulting in constrained variability in B-A ratio values (mean ± standard deviation: 1.102 ± 0.109; median [interquartile range]: 1.097 [1.029–1.162], Supplemental Fig. 2)1,4. Such limited variability or high correlation among procedural variables can compromise the discriminatory capacity of ROC model, thereby yielding a lower AUC32. Analyzing a more extensive dataset and incorporating diverse pre-dilation strategies in the future studies may contribute to achieving higher AUC values. The observational nature of this registry-based study, with pre-dilation techniques and balloon sizing left to the discretion of interventionalists, may introduce selection bias and confounding factors, underscoring the need for cautious interpretation and future randomized controlled trials to validate these findings. Additionally, angiographic lesion morphology (concentric vs. eccentric) and calcification severity, despite their potential impact on lesion outcomes, were not identified as independent predictors of SR. The influence of these lesion characteristics may be overshadowed by stronger predictors, such as procedural factors (B-A ratio) and immediate post-procedural results (post-DCB MLD), highlighting the importance of procedural optimization in coronary DCB treatment. Given the limited sensitivity and specificity of standalone angiography in assessing coronary calcification and eccentricity33,34, further studies incorporating detailed IVI-based evaluations are warranted.
Our study contributes significantly to the ongoing discussion about the optimal procedural steps and the appropriate application of DCB therapeutic strategies in de novo CAD. Given the historical precedents in the PTCA era and insights from stent therapy, specifically the concept of “the larger, the better”, our findings suggest the potential benefits of considering a higher B-A ratio to achieve maximal final MLD for successful DCB treatment. Future research, especially studies incorporating IVI, is essential to further optimize DCB treatment strategies and improve patient outcomes.
Methods
Study population
This study was based on the all-comers prospective registry that was conducted at Korea University Ansan Hospital from July 2019 to February 2023 (Impact of Drug-Coated Balloon Treatment in De Novo Coronary Lesion; NCT04619277). This registry encompasses patients with significant CAD undergoing DCB-based percutaneous coronary intervention (PCI) with either DCB-only, or in combination with drug-eluting stent (DES) implantation for de novo lesions in native coronary arteries. Patients were excluded if they had a life expectancy of less than two years or declined to provide consent. Those with suboptimal DCB treatment procedures, characterized by delayed DCB delivery (exceeding 60 s), failure to deliver DCB at least by the second attempt, or insufficient inflation time (less than 30 s), were also ineligible. Patients underwent clinical follow-up after the index procedure through regularly scheduled outpatient clinic visits at 3- to 5- months interval or telephone interviews were conducted in cases where in-person visits were unavailable.
This study analyzed a total of 317 patients underwent DCB-based PCI for de novo CAD and angiographic follow-up (Fig. 1). We further analyzed a subgroup of 47 patients who underwent intravascular ultrasound (IVUS)-guided DCB treatment in our cohort. This study was conducted in accordance with the Declaration of Helsinki (2013). Ethical approval was granted by the Ethics Committee of Korea University Ansan Hospital, with approval number [2019AS0162]. Written informed consent was obtained from all participants.
DCB treatment procedure
The DCB treatment procedure adhered to international and Asia–Pacific consensus recommendations, involving aggressive pre-dilation using a semi-compliant balloon, non-compliant balloon, or scoring balloon, as determined by the attending interventionist’s discretion1,4. Our DCB registry meticulously records detailed information throughout the DCB treatment procedural steps, encompassing the types of pre-dilation balloon (semi-compliant, non-compliant, or scoring), the length and diameter of the balloons, and the maximum inflation pressure and diameter achieved during balloon inflation. In cases of type A to C dissections following pre-dilation, stenting was deferred unless flow limitation developed. Bail-out stenting was reserved for type D or more severe coronary dissections. The DCBs used were all paclitaxel-based devices (SeQuent Please or SeQuent Please NEO: B. Braun Melsungen AG, Melsungen, Germany) and inflated for a minimum of 30 s, mostly extending beyond 60 s, based on the attending interventionist’s discretion.
Definition of successful angiographic results
This study specifically focused on identifying crucial procedural steps to achieve favorable angiographic results comparable to those of DESs. Earlier studies that compared paclitaxel-based DES versus bare metal stent reported a mean %DS of 20.2%, ranging from 17.4 to 26.1%, in DES arm at angiographic follow-up (Supplementary Table 1 and Supplementary Figure 1)6,7. In the present study, a successful, stent-like DCB treatment result was defined as DCB-treated lesions exhibiting %DS less than 20%, with no signs of residual dissection or aneurysmal deformation observed at angiographic follow-up. The study population was categorized into two groups based on follow-up angiographic findings: the SR (successful, stent-like result, %DS < 20%) group and the Non-SR group (Fig. 1).
Coronary angiography and Quantitative Coronary Angiography (QCA) analysis
A minimum of two orthographic views were obtained to assess pre-procedural and post-procedural angiographic characteristics of the target lesions. Follow-up angiographies were recorded with projection angles similar to the final angiographies of the index procedure. Calcification severity of target lesions was classified into three categories based on previously established angiographic criteria33. Lesion morphology was classified into three categories (concentric, eccentric, and multiple irregularities) based on qualitative assessment in at least two projections, as previously described35. The procedural efficacy and angiographic outcomes of DCB treatment were quantitatively assessed using QCA measurements. High-resolution angiograms, obtained using a standardized protocol, were digitally stored and analyzed with a dedicated QCA software system (e.g., CAAS II QCA, Pie Medical Imaging BV, Maastricht, The Netherlands). Two expert researchers (Jiho Hyun and Hye Young Heo), blinded to the study purpose, independently rated calcification severity (Cohen’s kappa = 0.91) and lesion morphology (Cohen’s kappa = 0.89); and measured the QCA parameters before, immediately after the DCB treatment, and during the follow-up angiography. These measurements included lesion length, reference vessel diameter (RVD), MLD, %DS, and acute luminal gain, as per established recommendations36. Specifically, RVD was derived by an interpolated method, a broadly accepted and well-validated method by QCA36. Balloon-to-artery ratio (B-A ratio) was calculated as the maximal diameter of either pre-dilation balloon or DCB, whichever was larger, actually inflated during each procedure, divided by the target lesion RVD. Positive vessel remodeling was defined, according to QCA, as a target lesion exhibiting a negative value in LLL.
Clinical follow-up and study endpoints
Clinical endpoint was target lesion failure (TLF), a composite of cardiac death, target vessel myocardial infarction (MI; excluding periprocedural MI and which not clearly linked to the target vessel), and clinically-driven target lesion revascularization at the longest follow-up available. Cardiac death was defined as any death that was not clearly of extracardiac origin, including MI. Clinically-driven target lesion revascularization was defined based on angiographic findings of %DS ≥ 50% during follow-up, accompanied by one or more of the following criteria: recurrent angina pectoris related to the target vessel, objective ischemic signs at rest or during exercise tests, abnormal fractional flow reserve results, or when %DS was ≥ 70%, even without ischemic signs or symptoms, in adherence to the Academic Research Consortium criteria37.
Statistical analysis
Continuous variables are expressed as means ± standard deviations and dichotomous variables as counts and percentages. QCA measurements obtained before and immediately after DCB treatment, as well as those obtained at angiographic follow-up, were compared between the SR and Non-SR lesions. Continuous variables were compared using Student’s t-test or Mann–Whitney U-test, and categorical variables were compared using Pearson’s chi-square or Fisher’s exact test. Paired measurements were analyzed using the paired t-test to assess differences. Stepwise binary logistic regression analysis was performed to explore the potential associations between procedure-related factors and angiographically successful DCB outcomes. Covariates that were statistically significant in univariate analysis or deemed clinically relevant were included in the multivariate model using the forward conditional method. Receiver-operating characteristic (ROC) curves were generated for a specific procedural factor to determine the optimal threshold value for predicting favorable angiographic outcomes (the MedCalc software, version 22.021, Ostend, Belgium). Binary logistic regression was also employed to evaluate the association between SR and the thresholds derived from ROC analysis (post-DCB MLD ≥ 1.940 mm and B-A ratio ≥ 1.126), dividing the entire patients into three groups based on threshold fulfillment. Odds ratios were calculated between the groups to predict SR: Group 1 (neither threshold met), Group 2 (one threshold met) and Group 3 (both thresholds met) (Supplementary Table 2). Statistical analyses were performed using the SPSS software (version 20.0; IBM Corp., Armonk, NY, USA) and statistical significance was set at p values of < 0.05.
Data availability
The corresponding author has full access to the study data, and anonymized data will be available upon reasonable request from a qualified researcher.
References
Jeger, R. V. et al. Drug-coated balloons for coronary artery disease: Third report of the International DCB Consensus Group. JACC Cardiovasc Interv 13, 1391–1402. https://doi.org/10.1016/j.jcin.2020.02.043 (2020).
Neumann, F. J. et al. ESC/EACTS Guidelines on myocardial revascularization. EuroIntervention 14(1435–1534), 2019. https://doi.org/10.4244/EIJY19M01_01 (2018).
Sanz Sanchez, J. et al. Drug-Coated balloons vs drug-eluting stents for the treatment of small coronary artery disease: A meta-analysis of randomized trials. Catheter Cardiovasc. Interv. 98, 66–75. https://doi.org/10.1002/ccd.29111 (2021).
Her, A. Y. et al. Drug-coated balloon treatment in coronary artery disease: Recommendations from an Asia-Pacific Consensus Group. Cardiol. J. 28, 136–149. https://doi.org/10.5603/CJ.a2019.0093 (2021).
Rhee, T. M. et al. Impact of optimized procedure-related factors in drug-eluting balloon angioplasty for treatment of in-stent restenosis. JACC Cardiovasc. Interv. 11, 969–978. https://doi.org/10.1016/j.jcin.2018.02.002 (2018).
Lansky, A. J. et al. Non-polymer-based paclitaxel-coated coronary stents for the treatment of patients with de novo coronary lesions: Angiographic follow-up of the DELIVER clinical trial. Circulation 109, 1948–1954. https://doi.org/10.1161/01.CIR.0000127129.94129.6F (2004).
Colombo, A. et al. Randomized study to assess the effectiveness of slow- and moderate-release polymer-based paclitaxel-eluting stents for coronary artery lesions. Circulation 108, 788–794. https://doi.org/10.1161/01.CIR.0000086926.62288.A6 (2003).
Stone, G. W. et al. Improved procedural results of coronary angioplasty with intravascular ultrasound-guided balloon sizing: The CLOUT Pilot Trial. Clinical Outcomes With Ultrasound Trial (CLOUT) Investigators. Circulation 95, 2044–2052. https://doi.org/10.1161/01.cir.95.8.2044 (1997).
Azuma, A. et al. Quantitative measurements of balloon-to-artery ratios in coronary angioplasty. J. Cardiol. 21, 879–888 (1991).
Nichols, A. B., Smith, R., Berke, A. D., Shlofmitz, R. A. & Powers, E. R. Importance of balloon size in coronary angioplasty. J. Am. Coll. Cardiol. 13, 1094–1100. https://doi.org/10.1016/0735-1097(89)90267-2 (1989).
Kitahara, H. et al. Impact of stent size selection on acute and long-term outcomes after drug-eluting stent implantation in de novo coronary lesions. Circ. Cardiovasc. Interv. 10, e004795. https://doi.org/10.1161/CIRCINTERVENTIONS.116.004795 (2017).
Fukuoka, R. et al. Novel stentless strategy with perfusion and drug-coated balloons for treating acute coronary syndrome. J. Soc. Cardiovasc. Angiogr. Interv. 3, 101175. https://doi.org/10.1016/j.jscai.2023.101175 (2024).
Goto, K. et al. Lumen measurements from quantitative coronary angiography and IVUS: A PROSPECT substudy. JACC Cardiovasc. Imaging 9, 1011–1013. https://doi.org/10.1016/j.jcmg.2015.07.006 (2016).
Gao, X. F. et al. 3-year outcomes of the ULTIMATE trial comparing intravascular ultrasound versus angiography-guided drug-eluting stent implantation. JACC Cardiovasc. Interv. 14, 247–257. https://doi.org/10.1016/j.jcin.2020.10.001 (2021).
Zhang, J. et al. Intravascular ultrasound versus angiography-guided drug-eluting stent implantation: The ULTIMATE trial. J. Am. Coll. Cardiol. 72, 3126–3137. https://doi.org/10.1016/j.jacc.2018.09.013 (2018).
Hong, S. J. et al. Effect of intravascular ultrasound-guided vs angiography-guided everolimus-eluting stent implantation: The IVUS-XPL randomized clinical trial. JAMA 314, 2155–2163. https://doi.org/10.1001/jama.2015.15454 (2015).
Lee, S. Y. et al. Procedural characteristics of intravascular ultrasound-guided percutaneous coronary intervention and their clinical implications. J. Am. Heart Assoc. 11, e025258. https://doi.org/10.1161/JAHA.122.025258 (2022).
Alfonso, F. & Scheller, B. State of the art: Balloon catheter technologies - drug-coated balloon. EuroIntervention 13, 680–695. https://doi.org/10.4244/EIJ-D-17-00494 (2017).
Gao, X. F. et al. Intravascular ultrasound vs angiography-guided drug-coated balloon angioplasty: The ULTIMATE III trial. JACC Cardiovasc. Interv. 17, 1519–1528. https://doi.org/10.1016/j.jcin.2024.04.014 (2024).
Hong, D. et al. Cost-effectiveness of intravascular imaging-guided complex PCI: Prespecified analysis of RENOVATE-COMPLEX-PCI trial. Circ. Cardiovasc. Qual. Outcomes 17, e010230. https://doi.org/10.1161/CIRCOUTCOMES.123.010230 (2024).
Kang, W. C. et al. Predictors of favorable angiographic outcomes after drug-coated balloon use for de novo small vessel coronary disease (DCB-ONLY). Angiology 72, 986–993. https://doi.org/10.1177/00033197211015534 (2021).
Kastrati, A. et al. Predictive factors of restenosis after coronary stent placement. J. Am. Coll. Cardiol. 30, 1428–1436. https://doi.org/10.1016/s0735-1097(97)00334-3 (1997).
Kasaoka, S. et al. Angiographic and intravascular ultrasound predictors of in-stent restenosis. J. Am. Coll. Cardiol. 32, 1630–1635. https://doi.org/10.1016/s0735-1097(98)00404-5 (1998).
Daniel, W. C. et al. Incidence and treatment of elastic recoil occurring in the 15 minutes following successful percutaneous transluminal coronary angioplasty. Am. J. Cardiol. 78, 253–259. https://doi.org/10.1016/s0002-9149(96)00273-1 (1996).
Gijsen, F. et al. Expert recommendations on the assessment of wall shear stress in human coronary arteries: Existing methodologies, technical considerations, and clinical applications. Eur. Heart J. 40, 3421–3433. https://doi.org/10.1093/eurheartj/ehz551 (2019).
Kim, S. et al. Favorable vasomotor function after drug-coated balloon-only angioplasty of de novo native coronary artery lesions. J. Clin. Med. 11, 299. https://doi.org/10.3390/jcm11020299 (2022).
Horie, K., Tanaka, A., Taguri, M. & Inoue, N. Impact of scoring balloons on percutaneous transluminal angioplasty outcomes in femoropopliteal lesions. J. Endovasc. Ther. 27, 481–491. https://doi.org/10.1177/1526602820914618 (2020).
Schmidt, T. et al. Safety and efficacy of lesion preparation with the AngioSculpt Scoring Balloon in left main interventions: the ALSTER Left Main registry. EuroIntervention 11, 1346–1354. https://doi.org/10.4244/EIJY15M05_04 (2016).
Kufner, S. et al. Neointimal modification with scoring balloon and efficacy of drug-coated balloon therapy in patients with restenosis in drug-eluting coronary stents: A randomized controlled trial. JACC Cardiovasc. Interv. 10, 1332–1340. https://doi.org/10.1016/j.jcin.2017.04.024 (2017).
Bonaventura, K. et al. Systematic scoring balloon lesion preparation for drug-coated balloon angioplasty in clinical routine: Results of the PASSWORD observational study. Adv. Ther. 37, 2210–2223. https://doi.org/10.1007/s12325-020-01320-2 (2020).
Shin, E. S. et al. Impact of scoring balloon angioplasty on lesion preparation for DCB treatment of coronary lesions. J. Clin. Med. 12, 6254. https://doi.org/10.3390/jcm12196254 (2023).
Kundu, S., Mazumdar, M. & Ferket, B. Impact of correlation of predictors on discrimination of risk models in development and external populations. BMC Med. Res. Methodol. 17, 63. https://doi.org/10.1186/s12874-017-0345-1 (2017).
Mintz, G. S. et al. Patterns of calcification in coronary artery disease. A statistical analysis of intravascular ultrasound and coronary angiography in 1155 lesions. Circulation 91, 1959–1965. https://doi.org/10.1161/01.cir.91.7.1959 (1995).
Mintz, G. S. et al. Limitations of angiography in the assessment of plaque distribution in coronary artery disease: A systematic study of target lesion eccentricity in 1446 lesions. Circulation 93, 924–931. https://doi.org/10.1161/01.cir.93.5.924 (1996).
Ambrose, J. A. et al. Angiographic morphology and the pathogenesis of unstable angina pectoris. J. Am. Coll. Cardiol. 5, 609–616. https://doi.org/10.1016/s0735-1097(85)80384-3 (1985).
Suzuki, N. et al. Clinical expert consensus document on quantitative coronary angiography from the Japanese Association of Cardiovascular Intervention and Therapeutics. Cardiovasc. Interv. Ther. 35, 105–116. https://doi.org/10.1007/s12928-020-00653-7 (2020).
Cutlip, D. E. et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation 115, 2344–2351. https://doi.org/10.1161/CIRCULATIONAHA.106.685313 (2007).
Acknowledgements
We thank Hangseok Choi for statistical analysis; Ji Ho Hyun and Hye Young Heo for their assistance in measuring QCA; and Minjung Lee and Hye Young Heo for the administrative assistance in managing the research.
Funding
This study is funded by the Grants from National Research Foundation of Korea (NRF) funded by the Korean government [Grant number: RS-2021-NR063386 (NRF-2021R1F1A1061337) to S.K.] [Grant number: RS-2023-00210960 to D.O.K.], Korea University Grant [Grant number K1923481, K2022971, K2111151, and K2211921 to S.K.; and K2225581 to D.O.K.].
Author information
Authors and Affiliations
Contributions
D.O.K., E-S.S., and S.K. conceptualized the study. E-S.S. and S.K. designed the study protocol. D.O.K., S.K., A-Y.H. and E-S.S. wrote the original manuscript. S.K., J-S.L., Y-H.K., S-Y.L., S.H.K., J-C.A., and W–H.S. contributed to the data acquisition. D.O.K., S.K., B.K. and E-S.S. supervised analysis and interpretation. S.K., J-S.L., Y-H.K., S-Y.L., S.H.K., J-C.A., and W–H.S. contributed to data analyses and interpretation. All the authors have read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Twitter Handle
Achieving maximal post-DCB lumen gain through oversized ballooning was identified as the key predictor for favorable angiographic outcomes after DCB treatment for de novo coronary artery disease, underscoring the need for refining lesion predilation strategies. (#Drug-coated Balloons, , #De novo CAD, #Maximal post-DCB lumen gain, #Lesion predilation, and #Oversized ballooning).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kang, D.O., Lee, JS., Kim, B. et al. Predictors of optimal angiographic lesion outcomes in drug-coated balloon treatment for de novo coronary artery disease. Sci Rep 15, 9391 (2025). https://doi.org/10.1038/s41598-025-92052-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-92052-2