Abstract
Physical activity (PA) is regarded as a non-pharmacological preventive strategy against cognitive decline. This study aimed to examine the relationship between PA and cognitive function in cognitively normal older Malaysian adults from a multi-ethnic, urban-dwelling community. Participants completed a questionnaire with questions on demographic details, socioeconomic status, health conditions, and short form of the International Physical Activity Questionnaire (IPAQ). Bivariate analyses and hierarchical linear regression were conducted to examine the relationship between IPAQ and Montreal Cognitive Assessment (MoCA) scores. Among the 382 participants (median age = 66 years), 51.6% were female. Median MoCA score was 24; and IPAQ levels were 28%, 39% and 33% ‘Low’, ‘Moderate’ and ‘High’ respectively. Bivariate analysis showed MoCA scores significantly differed across IPAQ levels (p-value < 0.001). Pairwise comparisons showed significant differences between MoCA scores and ‘High’ and ‘Low’ (p-value < 0.001) and ‘Moderate’ and ‘Low’ (p-value = 0.001) IPAQ levels. Hierarchical regression of potential confounding factors showed that while lower PA, being older, being Malay and hypertension were initially associated with lower MoCA scores, the association was explained by the greater influence of education and savings. Additional research is required to gain a more comprehensive understanding of these relationships.
Similar content being viewed by others
Background
There has been a steady improvement in average life expectancy globally. According to an analysis of trends in life expectancy for 201 countries with a study period from 1950 to 2015, there has been a steady rise in the average life expectancy at birth across every studied country, with the best performing ones in the Western Europe, Northern Europe and North America1. The proportion of older persons, with chronological age ≥ 60 defined by the United Nations, is also increasing in the recent decades. In China, the proportion of older adults (65 years old and above) was observed to continuously rise from 6.96% in 2000 to 8.87% in 2010, and 13.50% in 20202. As the population ages, the number of individuals living with some form of cognitive impairment also increases. According to a systematic review conducted by Pais et al., incidence of cognitive impairment ranged from 22 to 76.8 per 1000 person-years, with a median of 53.97 per 1000 person-years3.
Ageing is an unavoidable stage of humans’ development, and it is shown to be linked with potential changes in one’s physical and cognitive functioning4,5,6. Based on previous research, memory, executive functions, attention, and processing speed are the most vulnerable cognitive functions to the ageing process7,8,9,10.Older adults who experience a decline in their physical and/or cognitive functions would become dependent on others which in turns impact their well-being11,12. Preservation of physical and cognitive functions are key factors for ensuring a good quality of life. Both physical and cognitive functions have been shown to be significant predictors of quality of life in older adults experiencing cognitive impairment13. Ageing is a risk factor for neurodegenerative disorders such as Alzheimer’s diseases (AD), Parkinson’s disease (PD) and amyotrophic lateral sclerosis (ALS)14,15. Tools such as Montreal Cognitive Assessment (MoCA) that examine global cognitive functioning are sensitive to the early signs of cognitive ageing and would be appropriate to screen for early and the Mild Cognitive Impairment (MCI)16.
However, not all older adults would experience the age-relate declines the same way. Previously it was demonstrated that while some older adults demonstrate a severe decline in their physical and cognitive functions, others would still be able to maintain their functions in various domains. The mentioned study suggested that factors such as having an active and healthy lifestyle along with being in a cognitively stimulating environment would protect older adults from the adverse effects of ageing and improve their overall well-being17. A growing body of literature indicated the effect of physical activity on older adults’ physical and cognitive well-being4,18,19,20.
Many mechanisms explain how physical activity benefits the older adults in maintaining their cognitive health. One is that with the increase of age, our brain is greatly impacted, both structurally and functionally. The deterioration of white matter integrity with age can cause slower information processing and reduced brain connectivity21 and thus elevates the risk of neurological disorders. A recent meta-analysis has shown that physical exercise can improve white matter integrity and cognitive function in older adults22. Aerobic exercise training has been demonstrated to enhance regional cerebral blood flow, according to a randomized, controlled cross-over trial conducted in sedentary older men. These observed changes in cerebral blood flow may explain the exercise-induced positive effects on cognitive performance, which could be partly mediated by improvements in glucose metabolism23.
Although many studies examined the association between physical activity and cognitive functions on older adults, the majority of studies were conducted outside of Asia, hence their results might not be applicable to the Asian countries due to the different socioeconomic status and education in such countries24,25,26.
To address this, our main objective was to explore the association between physical activity and cognitive function in a large and socioeconomically diverse sample of Malaysian older adults. Malaysia is a multicultural country in South East Asia with residents from different ethnic groups including Malays, Chinese, and Indians. This diversity allowed a more in-depth examination of the mentioned factors. Therefore, our research question was whether there is any association between physical activity and cognitive function in Malaysian older adults. We hypothesised that participants who are more physically active have better cognition, i.e., a better MoCA score (measure of cognitive functions). Moreover, we hypothesised that participants with higher level of education would have a higher MoCA score. Besides PA, the effects of age, gender, ethnicity, hypertension as well as socioeconomic variables (education levels and savings) which could influence MoCA scores would also be investigated.
Results
Sample characteristics
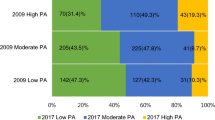
The demographic characteristics of participants (n = 382) who had completed the baseline questionnaire are presented in Table 1. There were 51.6% women with a median age of 66 years (IQR 63–70). Most participants are in the 60–69 years range (70.7%) followed by 70–79 years (27.7%) and 80–85 years (1.6%). Overall, there were 36.7% Malay, 40.8%, Chinese and 20.7% Indian participants, which are the three main ethnicities in Malaysia, and others (1.8%). 27% of participants reported themselves as having hypertension. As for the participants’ highest level of personal education, the majority had secondary and above education, with 33.5% participants having received up to secondary school education, 20.2% up to a pre-university or a diploma, and 34.5% of them had a Bachelor’s degree and above, while only 11.8% received up to primary school education. 33% of the participants had savings up to RM10,000 (US $2,250) and 12.8% had a savings between RM500,000 to a RM1,000,000 (US $112,500- $225,000). In terms of the physical activity, 28% were classified as ‘Low’, 39% as ‘Moderate’, and 33% as ‘High’ IPAQ levels.
Bivariate analysis showed that MoCA scores significantly differed across six variables, i.e., age group, ethnicity, highest education level, savings, hypertension status and IPAQ levels (Table 1) but no difference between gender. The p-values for these analyses are all less than 0.05, indicating that the observed differences are statistically significant.
Physical activity and other factors affecting cognitive function of older adults
The trend of higher MoCA scores with higher levels of IPAQ was evident, as shown in Fig. 1. A Kruskal-Wallis test revealed significant differences in MoCA scores across the levels of IPAQ (χ2 = 20.325, df = 2, p-value < 0.001). Pairwise Wilcoxon rank sum tests with continuity correction indicated significant differences in MoCA scores between ‘High’ and ‘Low’ IPAQ levels (W = 8955, p-value < 0.001), and between ‘Moderate’ and ‘Low’ IPAQ levels (W = 9910, p-value = 0.001).
The full regression model (Table 2) was statistically significant (F = 12.78, p-value < 0.001) and explained approximately 38% of the variability in MoCA scores (Adjusted R2 = 0.38). Diagnostic tests indicated no evidence of heteroscedasticity (χ2 = 15.856, p-value = 0.322), autocorrelation (DW = 2.130, p-value = 0.814), or model misspecification (F = 2.019, p-value = 0.135).
In the first block, there were significant relationships between MoCA scores, age, and ethnicity. MoCA scores decreased by approximately 0.1618 units for each one-year increase in age, assuming all other variables in the model are held constant. Regarding ethnicity, the mean MoCA scores among Chinese and Indian ethnic groups were significantly higher than those for Malays. Chinese and Indian individuals had, on average, 1.5039 and 1.5626 points higher MoCA scores, respectively, compared to Malays, holding other factors constant.
IPAQ.MET was positively associated with MoCA scores when included in the second block. Although statistically significant, the small coefficient (B = 0.0002) suggests that its influence on MoCA scores was minimal. Age and ethnicity remained significant predictors of MoCA scores.
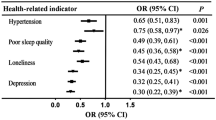
In the third block, hypertension was negatively associated with MoCA scores. Individuals with hypertension had, on average, 1.674 points lower MoCA scores compared to those without hypertension, holding other factors constant. Among the other significant predictors, age remained negatively associated with MoCA scores (B = -0.1544), indicating that for each additional year of age, MoCA scores decreased by 0.1544 points. Ethnicity also showed a significant association with MoCA scores. Compared to the reference group (Malay), Chinese individuals had MoCA scores that were, on average, 1.3571 points higher, while Indian individuals scored 1.6047 points higher. IPAQ.MET retained a small yet significant positive association with MoCA scores (B = 0.0002).
In the final block, age, ethnicity, IPAQ.MET and hypertension were no longer significant after socioeconomic variables, i.e. highest educational level and savings were included. Both variables were significantly associated with MoCA. Specifically, individuals with only primary or secondary education had significantly lower mean MoCA scores compared to those with a bachelor’s degree. Additionally, higher savings were linked to higher MoCA scores.
Discussion
We explored the potential association between physical activity (assessed by IPAQ MET scores and categories) and cognitive function (MoCA scores) in older adults, based on the data of the baseline questionnaire obtained from older adults residing in the Klang Valley area of Malaysia (MyAgeWell cohort) participating in a longitudinal, intervention study. Pairwise comparisons suggest an overall positive association existed between median MoCA score and PA level, with a significant higher in median MoCA score in participants with ‘High’ level of PA as compared to ‘Low’. Prior to the inclusion of socioeconomic variables into the model, hierarchical regression showed that low level of physical activity, being older in age, being ethnic Malay and hypertension were all significantly and negatively associated with MoCA scores. However, with the inclusion of socioeconomic variables, full regression model showed that the effects of having a lower educational level (below a Bachelor’s degree level, especially having only primary school education) and lower amount of savings, were the greatest factors that influenced the effects of PA on cognition in these in cognitively normal, urban-dwelling older adults.
The World Health Organization’s guidelines on physical activity and sedentary behaviour, include strong recommendations for individuals aged 65 and above to engage in regular physical activity. On a weekly basis, older adults should engage in a minimum of 150 to 300 minutes of moderate-intensity aerobic physical activity; or a minimum of 75–150 min of vigorous-intensity aerobic physical activity; or a comparable mix of moderate- and vigorous intensity activity27. Using the Global Physical Activity Questionnaire, it has been reported that 29.8% of Malaysian older adults were considered physically inactive28. In our study, we had similar findings where 28% of participants also showed ‘Low’ PA and therefore should be encouraged to engage in higher amount and intensity of physical activity. In a meta-analysis which explored the association between physical activity and cognitive ability using scores of seven cognitive ability assessment scales (including MoCA), it has been demonstrated that exercise was an effective means in delaying the cognitive decline of the older adults (aged 50 and above). This meta-analysis also suggested older adults to perform a minimum of moderate-intensity aerobic exercise and resistance exercise as many days as they are able in the week to improve cognitive function29. Our data showed that there were significant differences between participants who did ‘High’ and ‘Low’ (p-value < 0.001) as well as between participants who did ‘Moderate’ and ‘Low’ (p-value = 0.001) IPAQ levels but not between moderate and high, suggesting and confirming the meta-analysis that moderate PA is sufficient to preserve cognition. Thus, older adults should be encouraged to engage in at least moderate intensity PA to improve their cognitive function.
In a multinational meta-analysis and systematic review of epidemiology studies, it has been shown that the prevalence of mild cognitive impairment increases with age, from 10.9% for those between the age of 50–59 y/o, to 11.5% for 60–69 y/o and 15.76% for 70–79 y/o, to 21.27% in older adults aged ≥ 80 y/o30. Increasing age (aged 75 and above) was also linked with increased possibility of mild cognitive impairment (decreased MoCA scores), according to a Chinese cross-sectional analysis study in older adults31. Similarly, in our study, before the inclusion of socioeconomic variables into the model, hierarchical regression showed that older age was a significant variable which negatively affected MoCA scores.
Before the inclusion of socioeconomic variables into the model, hierarchical regression showed ethnicity as a significant variable influencing MoCA scores. In addition, bivariate analysis indicated that MoCA scores were significantly different across ethnic groups. The median scores for Malay, Chinese and Indian were 23, 24 and 25 respectively (data not shown), and pairwise comparison showed significant differences between ‘Malay’ and ‘Chinese’ (p-value = 0.017), and between ‘Malay’ and ‘Indian’ (p-value = 0.034). Similar observations have been made by different research groups. In a Malaysian study done in community-dwelling older adults (aged 55 and above), the authors found that for Malays, Chinese, and Indians, the corresponding mean (SD) MoCA scores were 20.44 (4.92), 23.97 (4.03), and 22.04 (4.83) (p = 0.01)32. Among ethnic Chinese and Indians, cognitive performance was favourably linked with social engagement, and among ethnic Indians, it was positively linked with lower depression ratings32. In a different study comparing the prevalence rates of cognitive impairment and dementia of Chinese and Malays among community-dwelling older adults in Singapore, it was found that, even after adjusting for demographic factors and cardiovascular health status, Malays had a nearly twofold elevated risk of cognitive impairment (diagnosis of cognitive impairment no dementia (CIND) and dementia) as compared to Chinese33. It has not been clearly understood what causes the correlation between ethnic Malay people and cognitive decline. The increased prevalence of dementia in older Malays was also reported by another Malaysian population-based study. Subsequent analysis of the same dataset demonstrated no discernible difference in years of formal education received between Malays and non-Malays34.
Hierarchical regression of our study (before the inclusion of socioeconomic variables) also shows that hypertension was a significant variable which negatively and significantly affecting MoCA score. Hypertension or high blood pressure is a global, major health problem among older adults. According to a Malaysian cross-sectional national population-based survey, the prevalence of hypertension in older adults (aged 60 and above) was 69.2% in 201535. In the past, the relationship between high blood pressure (hypertension) and cognitive impairment in older adults have been explored. A recent Indian study with recruited hypertensive patients aged between 60 and 80 reported that patients on two-year or longer anti-hypertensive treatment had significant higher MoCA scores as compared to those not receiving any anti-hypertensive drugs36. In our study, the participants were asked an open-ended question regarding their diagnosed health conditions, and thus their hypertension status was self-reported. Unlike the voluntary disclosure nature in our question, in similar studies mentioned above, a confirmed diagnosis of hypertension was made by clinicians. Around 20% of our participants did not provide any information regarding their hypertension status, or it could be that they were not aware of their hypertension status as only 27% of participants reported that they have a diagnosis of hypertension. This percentage was much less than prevalence of 69.2% in the abovementioned Malaysian survey study. Nonetheless, as a vital, modifiable risk factor for age-related cognitive decline, the effective management of hypertension should still be promoted37.
The socioeconomic status in this study was described using respondents’ educational status and savings. Our final block of full regression model showed that these are the two most important variables affecting MoCA performance, especially for those having only up to primary school education. The effects of educational status and savings masked the effects of PA, age, ethnicity and hypertension status. A Malaysian study showed that regardless of ethnic groups (Malay, Chinese, Indian), having less than 12 years of formal education were one of the common risk factors for low MoCA performance32. Similar findings could be observed in cognitively intact elderly participants in the United States38 and Greece39. It is commonly acknowledged that a main risk factor for late life cognitive impairment is low socioeconomic status40. Although the exact mechanisms by which SES influences cognitive impairment has not been clearly known, it is thought that SES may lessen cognitive impairment by building and maintaining brain reserve capacity. Levels of formal education received is a commonly used measure of cognitive reserve. Low literacy is a known risk factor for dementia and is linked to poor cognitive function41. According to the “cognitive reserve” hypothesis, brain tissue pathological burden that manifests as cognitive impairment is influenced by factors connected to intellectual stimulus, such as education, engaging occupation, mind-stimulating leisure activities, and social interactions. Having higher cognitive reserve may, by some compensating mechanism, postpone the onset of cognitive impairment or dementia symptoms due to pathological alterations in the brain42. Due to their low educational attainment, people with low SES have inadequate health literacy. There could be a general stigma associated with receiving mental health treatment at medical facilities in the community. In addition, when being compared to people with higher SES, they are less likely to get necessary health advice and show less effort to get tested for cognitive impairment. Poverty-stricken older persons lacked the resources needed to maintain excellent cognitive function, such as access to healthcare and wholesome nutrition. Because poverty-related problems can take up mental resources, poverty itself is a cause of cognitive decline. Therefore, cognitive impairment is more common found in older adults with lower socioeconomic status.
In this study, we recruited older adults who were cognitively normal as defined by their MoCA score of ≥ 13. Although the suggested cut-off score for MoCA is 26 when the screening tool was first developed16, it is later suggested that the mentioned score may not be the true reflective of mild cognitive impairment (MCI) in different country, hence, according to the cultural and educational backgrounds in a country, modifications to the cut-off score can be made43. A systematic review of the studies employed MoCA in Southeast Asia reported that in countries including Malaysia, Singapore, China, and Taiwan, researchers used a cut-off point ranged from 13 to 26 to take the educational background in these regions into account44. This study involved a representative sample consisting of participants from major ethnicities in Peninsular Malaysia (Malay, Chinese and Indian). Besides, the effects of socioeconomic status (in this case, education and savings) on cognitive function have not been well studied in the Southeast Asian context, especially in Malaysia. Although the use of IPAQ was originally intended for use in young and middle-aged adults (18–65 y/o)45, numerous studies have used it in older adult populations46. The advantages for the use of IPAQ include easy comparison of physical activity with other studies involving different age groups.
There are several limitations to this study. Outcomes from this study suggested that there is a positive correlation between the amount of physical activity and cognitive function. However, a causal relationship between these variables is not warranted dues to its cross-sectional design as all data were collected at one point in time, that is, at the beginning of a longitudinal intervention study involving physical activity and cognitive stimulation sessions. However, these baseline findings helped the researchers gain valuable insights into the factors affecting cognitive function among the Malaysian older adults. In addition, the short-form IPAQ requires participants to self-report physical activity done in the past seven days, and therefore, susceptible to recall. Besides, these findings were based on urban, community dwelling older adults, and its generalizability to other populations, such as the older adults in long-term care facilities or those staying in rural areas, remains to be elucidated. On top of that, the sample size was not very large, which may limit its generalizability.
Our cross-sectional study was able to establish the positive relative association between PA and median MoCA scores, as well as showing the effects of education level and savings on median MoCA scores. However, more longitudinal research will be needed to examine these relationships in this part of the world. Our team has an on-going, long-term intervention study (with physical activity and cognitive stimulation sessions) involving participants of different socioeconomic statuses will help us better understand these relationships. Besides, future research could be conducted to understand barriers faced by older adults which could prevent them from engaging in at least moderate amount of PA. Research in this direction would be helpful in aiding policy makers to establish policies and design effective public health programs related to the maintenance of optimal cognitive function among the older adults.
In conclusion, in accordance with previous research, our study on cognitively normal, multi-ethnic, community-dwelling older adults in Malaysia suggests that there is a positive correlation between physical activity and cognitive function. Being older, of the Malay ethnicity and having hypertension were associated with lower MoCA scores. However, our full regression model showed that having tertiary education (obtaining a Bachelor or postgraduate degrees) and having higher savings, explain the most variance in better performance in MoCA score, even masking the effects of age, ethnicity and hypertension status. Further investigations are needed for a thorough understanding of these relationships with the aim to improve or retain cognitive function in this population.
Methods
Participant recruitment
Older adults aged 60 and older were recruited as part of the MyAgeWell cohort. These participants were from the greater Klang Valley area (Kuala Lumpur and areas in Selangor) in the middle of Peninsular Malaysia, which is the cultural, commercial and economic heartbeat of Malaysia. The study has been registered on https://clinicaltrials.gov/ with the protocol number (NCT06376656), in which details of the study cohort, as well as the recruitment process and criteria, can be accessed. This study followed the principles of the Declaration of Helsinki and had obtained approval from the Sunway University Research Ethics Committee (SUREC2020/039). All participants were briefed about the study and their informed consent was obtained prior to recruitment.
Questionnaire
Montreal Cognitive Assessment: A Montreal Cognitive Assessment (MoCA) score of ≥ 13 is one of the inclusion criteria for participant recruitment16. MoCA is a one-page, performance-based cognitive instrument for the screening of mild to moderate cognitive impairment and it has been validated for its use on the older population. The highest possible score is 30. This 10- to 15-minute test has been individually administered to all participants by researchers following its original instructions. The MoCA examine several cognitive domains including visuospatial/executive function, naming, memory, attention, language, abstraction, delayed recall, and orientation. For participants who receive ≤ 12 years of education, an additional ‘correction point’ is given following the recommended education adjustment proposed by Nasreddine et al., the designer of MoCA16. The translated, national Malay version of MoCA47 was available upon participants’ request.
Baseline questionnaire: After recruitment, all participants were invited to fill in an online baseline questionnaire. The baseline questionnaire consists of 135 questions, which included demographic details, socioeconomic status, self-disclosed health conditions, and the short form of the International Physical Activity Questionnaire (IPAQ).
International Physical Activity Questionnaire: Part of the Baseline Questionnaire is composed of the short form of the International Physical Activity Questionnaire (IPAQ), which captured the participants’ physical activity (PA) in the past seven days45. The seven items of IPAQ estimates the time spent per week on moderate-to-vigorous intensity of physical activity, walking, and physical inactivity (sitting position). Responses are reported as to metabolic equivalent task (MET) minutes per week (MET min/week). The calculation of MET min is as follows: walking is 3.3 METs, moderate PA is 4.0 METs and vigorous PA is 8.0 METs. Any session of activity < 10 min is not included in the final calculation. The total METs min per week is the sum of the amount of walking (METs×min×d), the amount of moderate PA (METs×min×d), and vigorous PA (METs×min×d) in the past seven days. In addition, levels of physical activities are classified as ‘Low’, ‘Moderate’ and ‘High’ (Table 348), using a publicly available spreadsheet tool according to the 2005 revised guidelines by IPAQ Research Committee49, which tool has been widely used in many recent articles reporting physical activity of older adults50,51,52,53. The International Physical Activity Questionnaire Short Form has demonstrated good test-retest reliability, with an intraclass correlation coefficient (ICC) of 0.7954,55.
Statistical analysis
Details of study participants included age, gender, ethnicity, hypertension status, highest education level, savings, IPAQ, and MoCA scores. Categorical variables are reported as number and percentage. Bivariate associations between MoCA scores and all categorical variables were also analyzed using non-parametric tests: the Mann-Whitney U test for independent categorical variables with two groups and the Kruskal-Wallis test for independent categorical variables with more than two groups.
The relationship between IPAQ and MoCA scores was visualized by plotting the median MoCA scores across different IPAQ levels for all participants. Additionally, the non-parametric Kruskal-Wallis test was performed to examine the relationship between MoCA scores and IPAQ levels. Post-hoc pairwise comparisons were conducted using the Wilcoxon rank sum test with continuity correction to identify significant differences between specific IPAQ levels.
Hierarchical regression analysis was conducted to examine the relationship between MoCA scores and the seven independent variables (age, gender, ethnicity, hypertension, highest education level, savings, and IPAQ). The analysis was performed in a stepwise manner, entering variables in blocks to assess their incremental explanatory power. In Block 1, demographic variables (age, gender, ethnicity) were entered first. Block 2 included physical activity (IPAQ.MET). A health-related variable (hypertension status) was introduced in Block 3, followed by socioeconomic variables (highest education level, savings) in Block 4. The model’s fit was reported. Model significance and various diagnostics were also examined to ensure the robustness of the results. All analyses were conducted using R version 4.4.0, with statistical significance determined at α = 0.05.
Data availability
Limited access to data could be shared upon reasonable request. Please contact the corresponding author.
Abbreviations
- AD:
-
Alzheimer’s diseases
- ALS:
-
Amyotrophic lateral sclerosis
- IPAQ:
-
International physical activity questionnaire
- IQR:
-
Interquartile range
- MCI:
-
Mild cognitive impairment
- MET:
-
Metabolic equivalent task
- MoCA:
-
Montreal cognitive assessment
- PA:
-
Physical activity
- PD:
-
Parkinson’s disease
- SES:
-
Socioeconomic status
- y/o:
-
Years old
References
Liou, L., Joe, W., Kumar, A. & Subramanian, S. V. Inequalities in life expectancy: An analysis of 201 countries, 1950–2015. Soc. Sci. Med. 253, 112964. https://doi.org/10.1016/j.socscimed.2020.112964 (2020).
Luo, Y., Su, B. & Zheng, X. Trends and challenges for population and health during population Aging—China, 2015–2050. China CDC Wkly. 3, 593–598. https://doi.org/10.46234/ccdcw2021.158 (2021).
Pais, R., Ruano, L., O, P. C. & Barros, H. Global cognitive impairment prevalence and incidence in community dwelling older Adults-A systematic review. Geriatr. (Basel). 5 https://doi.org/10.3390/geriatrics5040084 (2020).
Bherer, L. Cognitive plasticity in older adults: Effects of cognitive training and physical exercise. Ann. N Y Acad. Sci. 1337, 1–6. https://doi.org/10.1111/nyas.12682 (2015).
Hoffstaedter, F. et al. Age-related decrease of functional connectivity additional to Gray matter atrophy in a network for movement initiation. Brain Struct. Funct. 220, 999–1012 (2015).
Villar, F., Serrat, R., Celdrán, M. & Pinazo, S. Active aging and learning outcomes: What can older people learn from participation? Adult Educ. Q. 70, 240–257 (2020).
Eich, T. S. et al. Inhibitory selection mechanisms in clinically healthy older and younger adults. J. Gerontol. Ser. B. 73, 612–621 (2018).
Friedman, N. P. & Miyake, A. Unity and diversity of executive functions: Individual differences as a window on cognitive structure. Cortex 86, 186–204 (2017).
Pliatsikas, C. et al. Working memory in older adults declines with age, but is modulated by sex and education. Q. J. Exp. Psychol. 72, 1308–1327 (2019).
Salthouse, T. A. Theoretical perspectives on cognitive aging (Psychology, 2016).
Lee, M. T., Jang, Y. & Chang, W. Y. How do impairments in cognitive functions affect activities of daily living functions in older adults? PLoS ONE. 14, e0218112 (2019).
Manning, K. M. et al. Longitudinal analysis of physical function in older adults: The effects of physical inactivity and exercise training. Aging Cell. 23, e13987 (2024).
Song, R., Fan, X. & Seo, J. Physical and cognitive function to explain the quality of life among older adults with cognitive impairment: Exploring cognitive function as a mediator. BMC Psychol. 11, 51. https://doi.org/10.1186/s40359-023-01087-5 (2023).
Hou, Y. et al. Ageing as a risk factor for neurodegenerative disease. Nat. Rev. Neurol. 15, 565–581 (2019).
Hung, C. W., Chen, Y. C., Hsieh, W. L., Chiou, S. H. & Kao, C. L. Ageing and neurodegenerative diseases. Ageing Res. Rev. 9, S36–S46 (2010).
Nasreddine, Z. S. et al. The Montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 53, 695–699. https://doi.org/10.1111/j.1532-5415.2005.53221.x (2005).
Yaffe, K. et al. Predictors of maintaining cognitive function in older adults: The health ABC study. Neurology 72, 2029–2035 (2009).
Etnier, J. L., Drollette, E. S. & Slutsky, A. B. Physical activity and cognition: A narrative review of the evidence for older adults. Psychol. Sport Exerc. 42, 156–166 (2019).
Gheysen, F. et al. Physical activity to improve cognition in older adults: Can physical activity programs enriched with cognitive challenges enhance the effects? A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Activity. 15, 1–13 (2018).
Rossi, P. G. et al. Effects of physical exercise on the cognition of older adults with frailty syndrome: A systematic review and meta-analysis of randomized trials. Arch. Gerontol. Geriatr. 93, 104322. https://doi.org/10.1016/j.archger.2020.104322 (2021).
Kuznetsova, K. A. et al. Brain white matter structure and information processing speed in healthy older age. Brain Struct. Funct. 221, 3223–3235. https://doi.org/10.1007/s00429-015-1097-5 (2016).
Zhang, W., Zhou, C. & Chen, A. A systematic review and meta-analysis of the effects of physical exercise on white matter integrity and cognitive function in older adults. Geroscience 46, 2641–2651. https://doi.org/10.1007/s11357-023-01033-8 (2024).
Kleinloog, J. P. D. et al. Aerobic exercise training improves cerebral blood flow and executive function: A randomized, controlled cross-over trial in sedentary older men. Front. Aging Neurosci. 11, 333. https://doi.org/10.3389/fnagi.2019.00333 (2019).
Henrich, J., Heine, S. J. & Norenzayan, A. The weirdest people in the world? Behav. Brain Sci. 33, 61–83 (2010).
Buchman, A. S. et al. Total daily physical activity and the risk of AD and cognitive decline in older adults. Neurology 78, 1323–1329. https://doi.org/10.1212/WNL.0b013e3182535d35 (2012).
Lenzen, S., Gannon, B. & Rose, C. A dynamic microeconomic analysis of the impact of physical activity on cognition among older people. Econ. Hum. Biol. 39, 100933. https://doi.org/10.1016/j.ehb.2020.100933 (2020).
World Health Organization, W. WHO Guidelines on Physical Activity and Sedentary Behaviour (World Health Organization, 2020).
Chan, Y. Y. et al. Prevalence and factors associated with physical inactivity among older adults in Malaysia: A cross-sectional study. Geriatr. Gerontol. Int. 20, 49–56 (2020).
Xu, L. et al. The effects of exercise for cognitive function in older adults: A systematic review and Meta-Analysis of randomized controlled trials. Int. J. Environ. Res. Public. Health. 20 https://doi.org/10.3390/ijerph20021088 (2023).
Bai, W. et al. Worldwide prevalence of mild cognitive impairment among community dwellers aged 50 years and older: A meta-analysis and systematic review of epidemiology studies. Age Ageing. 51, afac173. https://doi.org/10.1093/ageing/afac173 (2022).
Jia, X. et al. A comparison of the Mini-Mental state examination (MMSE) with the Montreal cognitive assessment (MoCA) for mild cognitive impairment screening in Chinese middle-aged and older population: A cross-sectional study. BMC Psychiatry. 21, 485. https://doi.org/10.1186/s12888-021-03495-6 (2021).
Asmuje, N. F., Mat, S., Myint, P. K. & Tan, M. P. Ethnic-Specific sociodemographic factors as determinants of cognitive performance: Cross-sectional analysis of the Malaysian elders longitudinal research study. Dement. Geriatr. Cogn. Disord. 51, 396–404. https://doi.org/10.1159/000526904 (2022).
Hilal, S. et al. Prevalence of cognitive impairment and dementia in Malays - Epidemiology of dementia in Singapore study. Curr. Alzheimer Res. 14, 620–627. https://doi.org/10.2174/1567205012666151002123813 (2017).
Hamid, T. A., Krishnaswamy, S., Abdullah, S. S. & Momtaz, Y. A. Sociodemographic risk factors and correlates of dementia in older Malaysians. Dement. Geriatr. Cogn. Disord. 30, 533–539. https://doi.org/10.1159/000321672 (2010).
Ho, B. K. et al. Trends in population blood pressure and prevalence, awareness, treatment and control of hypertension among older persons: The 2006 & 2015 National health and morbidity survey in Malaysia. PLoS ONE. 15, e0238780. https://doi.org/10.1371/journal.pone.0238780 (2020).
Panchawagh, S., Karandikar, Y. & Pujari, S. Antihypertensive therapy is associated with improved visuospatial, executive, attention, abstraction, memory, and recall scores on the Montreal cognitive assessment in geriatric hypertensive patients. Cereb. Circul. - Cognit. Behav. 4, 100165. https://doi.org/10.1016/j.cccb.2023.100165 (2023).
Ungvari, Z. et al. Hypertension-induced cognitive impairment: From pathophysiology to public health. Nat. Rev. Nephrol. 17, 639–654. https://doi.org/10.1038/s41581-021-00430-6 (2021).
White, R. S., Barber, J. M., Harp, J. P. & Jicha, G. A. Examining the effects of formal education level on the Montreal cognitive assessment. J. Am. Board. Fam Med. 35, 1043–1057. https://doi.org/10.3122/jabfm.2022.220093R1 (2022).
Konstantopoulos, K., Vogazianos, P. & Doskas, T. Normative data of the Montreal cognitive assessment in the Greek population and parkinsonian dementia. Arch. Clin. Neuropsychol. 31, 246–253. https://doi.org/10.1093/arclin/acw002 (2016).
Kelly, S. et al. Barriers and facilitators to the uptake and maintenance of healthy behaviours by people at Mid-Life: A rapid systematic review. PLoS ONE. 11, e0145074. https://doi.org/10.1371/journal.pone.0145074 (2016).
Arce Rentería, M. et al. Illiteracy, dementia risk, and cognitive trajectories among older adults with low education. Neurology 93, e2247–e2256. https://doi.org/10.1212/wnl.0000000000008587 (2019).
Cermakova, P., Formanek, T., Kagstrom, A. & Winkler, P. Socioeconomic position in childhood and cognitive aging in Europe. Neurology 91, e1602–e1610. https://doi.org/10.1212/wnl.0000000000006390 (2018).
Carson, N., Leach, L. & Murphy, K. J. A re-examination of Montreal cognitive assessment (MoCA) cutoff scores. Int. J. Geriatr. Psychiatry. 33, 379–388. https://doi.org/10.1002/gps.4756 (2018).
O’Driscoll, C. & Shaikh, M. Cross-cultural applicability of the Montreal cognitive assessment (MoCA): A systematic review. J. Alzheimers Dis. 58, 789–801. https://doi.org/10.3233/jad-161042 (2017).
Craig, C. L. et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 35, 1381–1395. https://doi.org/10.1249/01.Mss.0000078924.61453.Fb (2003).
Cleland, C., Ferguson, S., Ellis, G. & Hunter, R. F. Validity of the international physical activity questionnaire (IPAQ) for assessing moderate-to-vigorous physical activity and sedentary behaviour of older adults in the united Kingdom. BMC Med. Res. Methodol. 18, 176. https://doi.org/10.1186/s12874-018-0642-3 (2018).
Sahathevan, R. et al. A Bahasa Malaysia version of the Montreal cognitive assessment: Validation in stroke. Int. Psychogeriatr. 26, 781–786. https://doi.org/10.1017/s1041610213002615 (2014).
Cheng, H. L. A simple, easy-to-use spreadsheet for automatic scoring of the International Physical Activity Questionnaire (IPAQ) Short Form. (2016).
Sjostrom, M. et al.
Spedden, M. E., Choi, J. T., Nielsen, J. B. & Geertsen, S. S. Corticospinal control of normal and visually guided gait in healthy older and younger adults. Neurobiol. Aging. 78, 29–41. https://doi.org/10.1016/j.neurobiolaging.2019.02.005 (2019).
Mullan, B., Olivier, C. & Thøgersen-Ntoumani, C. Mind the Gap: Habit and self‐determined motivation predict health behaviours in middle‐aged and older adults. Br. J. Health. Psychol. 26, 1095–1113 (2021).
Park, S., Choi, B. H. & Jee, Y. S. Effects of plank exercise on respiratory capacity, physical fitness, and immunocytes in older adults. J. Exerc. Rehabil. 19, 332–338. https://doi.org/10.12965/jer.2346536.268 (2023).
Duarte Martins, A. et al. Effects of a 16-week high-speed resistance training program on body composition in community-dwelling independent older adults: A clinical trial. Clin. Nutr. ESPEN. 63, 84–91. https://doi.org/10.1016/j.clnesp.2024.06.010 (2024).
Jiang, S., Ng, J. Y. Y., Choi, S. M. & Ha, A. S. Relationships among eHealth literacy, physical literacy, and physical activity in Chinese university students: Cross-sectional study. J. Med. Internet Res. 26, e56386. https://doi.org/10.2196/56386 (2024).
Macfarlane, D. J., Lee, C. C., Ho, E. Y., Chan, K. L. & Chan, D. T. Reliability and validity of the Chinese version of IPAQ (short, last 7 days). J. Sci. Med. Sport. 10, 45–51. https://doi.org/10.1016/j.jsams.2006.05.003 (2007).
Acknowledgements
We would like to acknowledge Malaysian Department of Higher Education (MOHE) as the funder of this work. We are also grateful for the help of all post-doctoral research fellows, graduate research assistants, research assistants and interns in this project. We would also like to thank the participants who provided the information for the project.
Funding
This work was supported by a research grant provided by Malaysian Department of Higher Education (MOHE), namely Long Term Research Grant Scheme (LRGS/1/2019/SYUC/02/1), and Sunway University.
Author information
Authors and Affiliations
Contributions
Conceptualization, YCC; methodology, YCC, ENDL, JKLT, JC; writing—original draft preparation, ENDL; writing—review and editing, JKLT, JC, AT, WGL, SV, MJJ; figure preparation, JKLT; supervision, YCC. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chia, Y.C., Low, E.N.D., Teh, J.K.L. et al. Association between physical activity and cognitive function in a multi-ethnic Asian older adult population. Sci Rep 15, 7249 (2025). https://doi.org/10.1038/s41598-025-92074-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-92074-w