Abstract
Parkinson’s disease (PD) is a progressive neurodegenerative condition. One of the unmet medical needs in PD, are tools for better diagnosis, prognosis, and efficacy of treatment, which reflects the disease course of the individual patient. Alpha-Synuclein (α-Synuclein) is a hallmark of synucleinopathies such as PD, where α-Synuclein aggregates are deposited. Calpain-1 is an enzyme, located in the presynaptic terminal, and shown to be active as an early event related to aggregation of α-Synuclein. The aim of this study was to develop and evaluate a competitive ELISA, targeting a Calpain-1 specific cleavage site of α-Synuclein, named α-Syn-C, and evaluate it in serum from patients diagnosed with PD and comparing to healthy matched donors. A monoclonal antibody was raised against the α-Synuclein fragment generated by cleavage of Calpain-1 and employed in an ELISA assay. The assay was developed, technically evaluated, and quantified in two independent cohorts of patients diagnosed with PD and compared to the healthy donors. The discovery cohort showed α-Syn-C was significantly upregulated in patients with PD compared to healthy donors (p =0.0007), with a diagnostic value of AUC = 0.83. The evaluation cohort showed similar results with an ability to differentiate PD patients from healthy donors (p < 0.0001) with an AUC = 0.85. These findings are exploratory and hypothesis generating, indicating the α-Syn-C biomarker may be useful in managing PD patients, and needs to be validated in larger cohorts and longitudinal studies.
Similar content being viewed by others
Introduction
Parkinson’s disease (PD) is a progressive neurodegenerative condition, characterized by the cardinal features with presence of bradykinesia, rest tremor and rigidity1. The motor signs are often preceded by non-motor functions including sleep, depression, anxiety, and urinary dysfunction. The motor dysfunction is due to the loss of dopamine containing neurons in the substantia nigra pars compacta (SNc), a part of the midbrain which plays a role in the regulation of movement. There is no clear cause, no cure, and as a result of an aging population, the prevalence of PD is expected to rise steadily to 13 million individuals worldwide in 20402. The onset of PD is diagnosed by a neurological and physical exam, including review of symptoms, genetics, and medical history.
Clinically, two major subtypes of PD can be defined, namely tremor-dominant PD with relative absence of other motor symptoms and non-tremor dominant PD. However, there is a general understanding that PD is highly heterogeneous upon diagnosis, also in rate of progression3. Generally, 50% of PD patients have reached key milestones, such as either postural instability or dementia within 4 years from diagnosis, where 25% have a good 10-year prognosis. For the progressive group of patients the number of severe symptoms increases, where increased medication is provided to manage the symptoms, leading to increased risk of side effects contributing to increased disability4,5. Dividing patients into subtypes divided by symptoms and how symptoms evolve, may therefore be a path forward6. To eliminate adverse events for progressive patients, there is a need for better diagnostic, prognostic, and efficacy of treatment tools, reflecting the individual patient. Importantly, there is a lack of blood-based biomarkers for PD, hence there is an intense search for novel biomarker candidates falling into the mentioned categories, particularly those identifying the subset of patients with a rapidly progressing disease, i.e. those in urgent need of intervention.
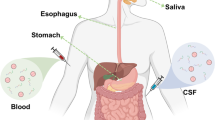
Alpha-Synuclein (α-Synuclein) is a hallmark of all synucleinopathies, including PD, dementia with Lewy bodies (DLB), and multiple system atrophy (MSA). All these diseases, are determined by α-Synuclein aggregates and deposition7. The α-Synuclein protein is composed by an N-terminal region (amphipathic region), Central Region (NAC region necessary for aggregation), and C-terminal Region (Acidic tail), comprising a 140 amino acid sequence. Posttranslational modifications and fragmentation of α-Synuclein, has previously been described in the C-terminal truncation of α-Synuclein8. One of the enzymes who are thought to perform this processing, is Calpain-1, which is interesting considering its calcium dependence and localization at presynaptic terminal, and interestingly this cleavage has been indicated be an early event related to aggregation of α-Synuclein, a hallmark of PD9,10. Cleavage sites of α-Synuclein by Calpain-1, was previously identified by Duffin et al.12, who discovered a cleavage site between amino acid 122 and 123, resulting in an upstream neoepitope. In vivo, they showed how Calpain-1 cleaved α-Synuclein lead to formation of Calpain-1 aggregates of α-Synuclein in PD and dementia with Lewy bodies (DLB), together with the fragments being present in human brains and co-localized with neurons in PD and DLB brains.
We hypothesized that this specific fragment of α-Synuclein cleaved by Calpain-1 could be applied as a blood-based biomarker for Parkinson’s disease. The aim of this study was to develop and validate a competitive ELISA, targeting a Calpain-1 generated fragment of α-Synuclein, named α-SYN-C, and evaluate its association with Parkinson’s disease in comparison to healthy donors.
Results
Specificity, accuracy, and precision of the α-SYN-C assay
The α-SYN-C assay target a neoepitope fragment located in the C-terminal region of α-Synuclein (Fig. 1A). The human sequence was aligned using UNIPROT, and the corresponding sequence in mouse, rat, and bovine are 100% aligned (Fig. 1B). The hybridomas producing the best monoclonal antibodies were screened for reactivity towards the standard peptide (synthetic peptide for calibration curve) and native material (human serum). The clone NBH-499-1 was chosen for assay development and determined as an IgG1 subtype. To evaluate the specificity of the α-SYN-C assay, the mAb was tested towards the elongated peptide, truncated peptide, non-sense standard peptide, non-sense coater, and full-length α-Synuclein protein, and showed no reactivity towards those peptides (Fig. 1C). In vitro cleavage experiments confirmed that cleavage of α-Synuclein by Calpain-1 resulted in the generation of the α-SYN-C fragments within 1 h of cleavage after which they decreased. No reactivity was found towards the non-cleaved α-Synuclein or Calpain-1 (Fig. 2) confirming very high specificity of the assay for the cleavage epitope. Technical validation was performed to evaluate the novel α -SYN-C assay. Overall, the α-SYN-C assay demonstrated good technical performance (Table 1), including accepted inter- and intra-variations, analyte stability, and no interference from hemoglobin, lipemia and biotin.
Overview of α-SYN-C assay specificity. (A) Structure of α-Synuclein, indicating the α-SYN-C assay targeting the C-terminal region of α-Synuclein. (B) Sequence alignment of the targeted α-Synuclein sequence in human, mouse, bovine, and rat species (blue box). The sequence was aligned using UNIPROT. (C) Specificity of the α-SYN-C assay. Reactivity towards the standard peptide (EAYEMPSEEGYQDYEPEA), truncated peptide (AYEMPSEEGY), elongated peptide (NEAYEMPSEEG), full-length α-Synuclein (MDVFMKGLSKAKEGVVAAAEKTKQGVAEAAGKTKEGVLYVGSKTKEGVVHGVATVAEKTKEQVTNVGGAVVTGVTAVAQKTVEGAGSIAAATGFVKKDQLGKNEEGAPQEGILEDMPVDPDNEAYEMPSEEGYQDYEPEA), and non-sense standard peptide (ELPARITPSQ). No background signal was detected when coating with a non-sense coating peptide (ELPARITPSQ-Biotin). Signals are shown as relative luminescence (RLU) per second, as a function of standard peptide.
Specificity of α-SYN-C towards Calpain-1 fragments of α-Synuclein. α-SYN-C fragments were cleaved after 1 h, 3 h and 6 h of incubation with α-Synuclein and Calpain-1 (n = 3 for all settings). The negative controls included cleavage buffer, the enzyme Calpain-1, and intact α-Synuclein. No statistical differences were found between the full-length α-synuclein and α-synuclein Cleaved by Calpain-1 (p = 0.100 for all three times). Data are depicted as mean ± 95%CI.
α-SYN-C is elevated in patients with Parkinson’s disease compared to healthy controls – results from the discovery and evaluation cohort
Two study cohorts were included to test the biological utility of the assay. The discovery cohort included patients with Parkinson’s disease (mean age: 73.7 years, 50.0% male), and healthy donors (mean age: 59.5 years, 56.3% male), Table 2. Here α-SYN-C was significantly elevated in serum from patients with Parkinson’s disease compared to healthy donors (p = 0.0007, Fig. 3A) and presented an AUROC of 0.83 (95%CI: 0.69–0.98, p = 0.0014, Fig. 3B). The evaluation cohort included patients with Parkinson’s disease (mean age: 64.2 years, 50% male), and healthy donors (mean age: 60.3, 60% male), Table 2. Here α-SYN-C was significantly elevated in serum from patients with Parkinson’s disease compared to healthy donors (p < 0.0001, Fig. 4A), and presented an AUROC of 0.85 (95% CI: 0.74-0.96, p = 0.0001, Fig. 4B).
Discovery Cohort: Serum levels of α-SYN-C is upregulated in patients with Parkinson’s disease. A) Healthy donors (n = 16), and Parkinson’s disease (n = 16). Statistical differences between the healthy donors and patients with Parkinson’s disease were calculated using a Mann-Whitney U-test, and shown as mean±95% CI. B) The diagnostic potential was calculated by the area under the Receiver Operating Curve (ROC). ***p<0.001.
Evaluation Cohort: Serum levels of α-SYN-C is upregulated in patients with Parkinson’s disease.A) Healthy donors (n = 15), and Parkinson’s disease (n = 30). Statistical differences between the healthy donors and patients with Parkinson’s disease were calculated using a Mann-Whitney U-test, and shown as mean±95% CI. B) The diagnostic potential was calculated by the area under the Receiver Operating Curve (ROC).****p < 0.0001.
Discussion
In this study, we developed, validated, and evaluated a competitive ELISA for detection of α-SYN-C using a monoclonal antibody targeting the N-terminal cleavage site of Calpain-1 cleaved α-Synuclein. The main findings of this study were as follows: (1) development of a robust and specific α-SYN-C assay towards the sequence EAYEMPSEEG; (2) α-SYN-C was detectable in human serum; (3) α -SYN-C was upregulated in patients diagnosed with Parkinson’s disease compared to healthy donors. To our knowledge, this is the first study to develop and technically validate a blood-based biomarker quantifying the levels of a specific fragment targeting α-Synuclein degraded by Calpain-1, followed by biological evaluation in serum from patients with Parkinson’s disease.
The α -SYN-C assay is characterized as a technically robust and accurate assay by showing acceptable dilution recovery, interference, and stability tests. The intra- and inter-variation was accepted with values of 5.8% and 12.8%, respectively. The assay was further characterized as being specific towards the N-terminal cleavage site of α-SYN-C after cleavage by Calpain-1, with highest activity after 1 h of incubation, which confirmed that Calpain-1 cleaves and generate the targeted fragment.
Calpain-1 has previously known to be involved in formation and secretion of Aβ in Alzheimer’s disease, indicating its role in neurological disorders13. Cleavage sites of Calpain-1 for α-Synuclein was originally identified by Mishizen-Ebert et al. in 200314, while the site targeting in this assay was identified by Dufty et al. in 2007, who indicated that this cleavage could contribute to the initiation of the synucleinopathy, i.e.trigger aggregation and thereby play an important role in the initiation of PD12. How fragmented α-Synuclein contribute to maintaining tissue homeostasis and function needs further evaluation, but studies have showed truncated α-Synuclein fragments are linked to neurotoxicity in healthy individuals and PD patients15,16. Previously developed biomarkers targeting α-Synuclein has been focusing on targeting the intact protein, by immunohistochemistry, ELISA, western blot, Luminex, and mass spectrometry17. To achieve the unmet need, of finding patients with early PD, progressive patients, and identify who benefits from a given treatment, pathologically generated fragments of α-Synuclein could aid this need. Limitations of the study include assessment of α-SYN-C in two relatively small cohorts with cross sectional designs. Moreover, limited clinical information was available for the investigated patient cohorts, which highlights the exploratory nature of this study.
In conclusion, this is the first study to quantitatively measure a specific fragment of α-Synuclein degraded by Calpain-1 in serum from PD patients and demonstrate their clinical utility as a diagnostic tool. Since α-Synuclein is well-established to have an important role in PD pathology, easily accessible tools to quantify changes in serum, could provide valuable information for assessing patients’ suitability for targeted treatments, thereby addressing the current gap in biomarkers for clinical management and trials.
Materials and methods
Synthetic peptides used for generation of monoclonal antibodies, assay development and assay validation were purchased from Genscript (Piscataway, NJ, US) (Table 3).
Monoclonal antibody development, production, and characterization
Monoclonal antibodies were generated by immunization of the following amino acid sequence 122’ ↓EAYEMPSEEG’132, targeting a Calpain-1 cleaved α-Synuclein sequence. Immunization was initiated by subcutaneous injection of 200 µl emulsified antigen and 100 µg of immunogenic peptide (EAYEMPSEEG-GGC-KLH) in 4- to 6-week-old Balb/C mice using Stimmune (Thermo Fisher, MA, USA). Immunizations were repeated every second week. The mouse with the highest stable serum titer were selected for fusion and boosted intravenously with 50 µg immunogenic peptide in 100 µl 0.9% NaCl solution 3 days before isolation of the spleen for cell fusion. Hybridoma cells were produced by fusion of the mouse spleen cells with SP2/0 myeloma cells as described by Gefter et al.18. The generated clones were plated into a 96-well microtiter plates for further growth, and the limiting dilution method was applied to promote monoclonal growth. Reactivity to the supernatant were tested by an indirect ELISA performed on streptavidin-coated plates. EAYEMPSEEG-K-Biotin was used as screening peptide, while the standard peptide EAYEMPSEEGYQDYEPEA was used to further test the specificity of the newly developed antibody clones. Supernatant was collected from the hybridoma cells and purified using HiTrap affinity columns (GEHealthcare Life Science, Little Chalfront, Buckinghamshire, UK) according to manufacturer’s instructions and antibody isotype was determined using Rapid ELISA Mouse monoclonal antibody Isotyping Kit (Invitrogen, Carlsbad, CA, USA) following the manufacturer’s protocol.
Reactivity towards human serum was tested with purchased samples from a commercial supplier (Valley Biomedical, Winchester, VA). The monoclonal antibodies were selected to specifically recognize the standard peptide (EAYEMPSEEGYQDYEPEA), and not an elongated or truncated sequence of the peptides (NEAYEMPSEEG and AYEMPSEEG, respectively).
α-SYN-C assay development
Development of the competitive colorimetric immunoassay included preliminary optimizing experiments to identify the right reagents, concentrations, incubation-time and -temperature. The final α-Synuclein assay is a competitive ELISA, named α-SYN-C with the procedure as follows: A 96-well streptavidin-coated microplate (Greiner Bio-One, Kremsmünster, Austria) was coated with 2 ng/mL biotinylated synthetic peptide (EAYEMPSEEG-K-Biotin) dissolved in assay buffer (25 mM phosphate buffered saline (PBS), 1% bovine serum albumin, 0.1% Tween-20, 0.36% Bronidox, 8 g/L NaCl, adjusted to pH 7.4 at 20 °C) and incubated for 30 min at 20 °C with constant shaking (300 rpm) in darkness. Next, 20 µL/well of standard peptide (50 ng/mL) and samples were added to the appropriate wells, followed by the addition of 100 µL/well of HRP-labelled antibody diluted in assay buffer to a concertation of 281 ng/mL and incubated for 1 h at 20 °C with constant shaking (300 rpm) in darkness. After each incubation step, wells were washed five times with the washing buffer (20mM Tris, 50mM NaCl, pH 7.2). The TMB solution were put at room temperature 60 min prior to use and 100 µL/well were added to plate and incubated for 15 min at 20 °C with constant shaking (300 rpm) in darkness. The reaction was stopped by adding 100 µl/well of 1% H2SO4. The absorbance was measured at 450 nm with 650 nm as a reference within 30 min on a microplate absorbance reader (VersaMax, Molecular Devices, CA, USA). A standard curve was plotted using a 4-parameter logistic curve fit Y = (A − D)/(1 + (x/C)^B) + D, where R > 0.9. Data were analyzed using the SoftMax Pro version 7.0.3 software.
Technical evaluation
Assay linearity was determined by two-fold dilutions of four human serum samples and calculated as percentage of recovery of the undiluted sample. To determine the assay accuracy, standard peptide and a human serum sample with a known high α-SYN-C concentration were spiked, and calculated as the percentage recovery of the measured value and the expected concentration of the peptide or human serum sample. Specificity of the generated monoclonal antibody was calculated as percentage of signal inhibition by two-fold diluted standard peptide (EAYEMPSEEGYQDYEPEA), elongated peptide (NEAYEMPSEEG), truncated peptide (AYEMPSEEG), and non-sense peptide (ELPARITPSQ). Interference of substances present in blood, was tested by adding a low/high content of hemoglobin (2.50/5 mg/mL), lipemia/lipids (1.50/5 mg/mL) and biotin (5–100 ng/mL) to a serum sample with a known concentration of α-SYN-C. The normal reference levels for hemoglobin, lipemia/lipids and biotin were 0–10 mg/dL (0–0.0016 mmol/L), < 150 mg/dl (< 1.69 mmol/L) and 0.22–3.00 ng/ml, respectively. The stability of the analyte was examined through temperature tests (0, 2-, 4-, 24-, and 48-hours of incubation at either 4–20°C), and five freeze-thaw cycles of human serum samples. The recovery was calculated with 0 h/0 cycle of the sample as a reference. The intra- and inter-assay variation was determined by 10 independent runs of eight quality controls and two kit control runs in double determinations, while the measurement range was defined as the range between lower limit of measurement range (LLMR) and the upper limit of measurement range (ULMR) on the 10 runs. The standard curves from the 10 independent runs were used to determinate the IC50 (half-maximal inhibition concentration). All samples for the technical validation and biological measurements were run in double determination.
In vitro cleavage
Human recombinant α-Synuclein (cat no. AG938, Sigma-Aldrich, Darmstadt, Germany), was cleaved with Native human Calpain-1 (cat. No. ab91019, abcam, Cambridge, UK). The α-Synuclein was reconstituted in MilliQ water and mixed in a 10:1 concentration with Calpain-1 in cleavage buffer (100 mM HEPES, 100 mM NaCl, 10 mM CaCl2, 2 mM Zn acetate, pH 7.5). As controls, the cleavage buffer, and the cleavage buffer with α-Synuclein or Calpain-1 were mixed in separate vials. Cleavages were performed for 1 h, 3 h, and 6 h at 37 °C, and subsequently stopped by 50 µM EDTA. Samples were analyzed in the α-SYN-C assay.
Biological evaluation of α-SYN-C in a discovery and evaluation cohort
The biological capability of α-SYN-C was evaluated in two independent cohorts (discovery and evaluation) in serum samples obtained from the commercial vendors Proteogenex (Culver City, CA, USA), and was approved by the local ethical committee (Russian Oncological Research Center, Blokhin Rams Ethics Committee review form, Protocol no. PG-ONC 2003/1), and BioIVT (Westerbury, NY, USA). Informed consent was obtained from all participants. The discovery cohort included healthy donors (n=16) and patients with Parkinson’s disease (n = 16), while the evaluation cohort included healthy donors (n=15) and patients with Parkinson’s disease (n = 30). The study was executed in compliance with the Helsinki Declaration of 2013. Serum samples were obtained and stored at −80oC until biomarker analysis.
Animals
All animals were treated according to the guidelines for animal welfare. Monoclonal antibody production in mice was approved by the Danish National Authority (The Animal Experiments Inspectorate) under approval number 2013-15-2934-00956. The study is reported in accordance with ARRIVE guidelines. Mice were purchased from Brogaarden, Denmark, and sacrificed by cervical dislocation.
Statistical analysis
Patient characteristics are presented as a number (frequency) and percentage for categorical variables and either mean with standard deviation or mean with range for continuous variables. Statistical differences between the full-length α-Synuclein and α-Synuclein cleaved by Calpain-1 during the cleavage experiments (1 h, 3 h, and 6 h), together with healthy donors and patients with Parkinson’s disease in the two assessed cohorts were calculated using a Mann-Whitney U-test. The diagnostic potential was calculated by the area under the Receiver Operating Curve (ROC). Graphs are shown as mean ± 95% CI. For all statistical analyses performed, a P-value below 0.05 was considered significant. Statistical analysis and graphs were performed using GraphPad Prism version 9 (GraphPad Software, Inc., La Jolla, CA) and MedCalc version 19.3 (MedCalc Software, Ostend, Belgium).
Data availability
All data from this study are included in this article. Data are kept on file and are not publicly available, due to privacy data legislation. Requests can be directed to the corresponding author.
References
Port, R. J. et al. People with Parkinson’s disease: what symptoms do they most want to improve and how does this change with disease duration?? J. Parkinsons Dis. 11, 715–724 (2021).
Ray Dorsey, E. et al. Global, regional, and National burden of Parkinson’s disease, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 17, 939 (2018).
Greenland, J. C., Williams-Gray, C. H. & Barker, R. A. The clinical heterogeneity of Parkinson’s disease and its therapeutic implications. Eur. J. Neurosci. 49, 328–338 (2019).
Kalia, L. V. & Lang, A. E. Parkinson’s disease. Lancet (London England). 386, 896–912 (2015).
Vu, T. C., Nutt, J. G. & Holford, N. H. G. Progression of motor and nonmotor features of Parkinson’s disease and their response to treatment. Br. J. Clin. Pharmacol. 74, 267–283 (2012).
Lawton, M. et al. Developing and validating Parkinson’s disease subtypes and their motor and cognitive progression. J. Neurol. Neurosurg. Psychiatry. 89, 1279–1287 (2018).
Meade, R. M., Fairlie, D. P. & Mason, J. M. Alpha-synuclein structure and Parkinson’s disease. Mol. Neurodegener. 14, 1–14 (2019).
Li, W. et al. Aggregation promoting C-terminal Truncation of α-synuclein is a normal cellular process and is enhanced by the Familial Parkinson’s disease-linked mutations. Proc. Natl. Acad. Sci. U S A. 102, 2162–2167 (2005).
Mishizen-Eberz, A. J. et al. L. D. Cleavage of α-Synuclein by Calpain: potential role in degradation of fibrillized and nitrated species of α-Synuclein. Biochemistry 44, 7818–7829 (2005).
Mizuta, I. et al. F. J. Multiple candidate gene analysis identifies α-synuclein as a susceptibility gene for sporadic Parkinson’s disease. Hum. Mol. Genet. 15, 1151–1158 (2006).
Karsdal, M. et al. Biochemical markers and the FDA critical path: how biomarkers May contribute to the Understanding of pathophysiology and provide unique and necessary tools for drug development. Biomarkers 14, 181–202 (2009).
Dufty, B. M. et al. Calpain-cleavage of alpha-synuclein: connecting proteolytic processing to disease-linked aggregation. Am. J. Pathol. 170, 1725–1738 (2007).
Nixon, R. A. et al. Calcium-activated neutral proteinase (calpain) system in aging and Alzheimer’s disease. Ann. N Y Acad. Sci. 747, 77–91 (1994).
Mishizen-Eberz, A. J. et al. Distinct cleavage patterns of normal and pathologic forms of alpha-synuclein by Calpain I in vitro. J. Neurochem. 86, 836–847 (2003).
Liu, C. W. et al. A precipitating role for truncated alpha-synuclein and the proteasome in alpha-synuclein aggregation: implications for pathogenesis of Parkinson disease. J. Biol. Chem. 280, 22670–22678 (2005).
Murray, I. V. J. et al. Role of alpha-synuclein carboxy-terminus on fibril formation in vitro. Biochemistry 42, 8530–8540 (2003).
Atik, A., Stewart, T. & Zhang, J. Alpha-Synuclein as a biomarker for Parkinson’s disease. https://doi.org/10.1111/bpa.12370
Gefter, M. L., Margulies, D. H. & Scharff, M. D. A simple method for polyethylene glycol-promoted hybridization of mouse myeloma cells. Somatic Cell. Genet. 3, 231–236 (1977).
Acknowledgements
We would like to thank Inge Kolding for her help during the initial steps of antibody development.
Author information
Authors and Affiliations
Contributions
S.H.N. was the main author of the manuscript. S.H.N. and C.M.H. carried out the biomarker development and validation. S.H.N carried out statistical analysis in discussion with M.K., M.B., and K.H. All authors were involved in the interpretation of the data. All authors edited the manuscript and approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
SHN, CMH, MB, MAK and KH are full-time employees at Nordic Bioscience A/S. Nordic Bioscienceis a privately-owned, small–medium-size enterprise (SME) partly focused on developing biomarkers. None of the authors received fees, bonuses, or other benefits for the work described in the manuscript. SHN, MAK, and KH hold stocks in Nordic Bioscience A/S.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Holm Nielsen, S., Møller Hausgaard, C., Benmarce, M. et al. A fragment of Calpain-1 cleaved α-Synuclein quantified in serum is upregulated in patients with Parkinson’s disease. Sci Rep 15, 12081 (2025). https://doi.org/10.1038/s41598-025-92726-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-92726-x