Abstract
This study aimed to explore the relationship between the triglyceride-glucose (TyG) index and silent myocardial infarction (SMI) in the general population, with a focus on elucidating potential links and contributing to the understanding of risk factors for undetected cardiac events. This prospective cohort study was carried out within a community-based population, using data from the Atherosclerosis Risk in Communities study in the United States. The dataset included information on demographics, cardiovascular risk factors, blood lipids, liver and kidney function, and other variables. Participants were categorized into four quartiles based on their TyG index scores. Cox regression analysis was used to examine the relationship between the different ranges of TyG indices and SMI. In total, 14,211 community residents were enrolled and followed up for 36 years. Among them, 7,316 (51.48%) developed SMI. TyG index measurements were divided into quartiles: Q1 (≤ 8.26), Q2 (8.26–8.62), Q3 (8.62–9.02), and Q4 (≥ 9.02). Restricted cubic spline curves indicated that higher TyG indices correlated with a greater risk of SMI. Results of the Kaplan–Meier analysis suggested that participants with a higher TyG index had a lower cumulative survival rate for SMI (P < 0.001). Through multivariate Cox regression analysis, the TyG index was identified as an independent predictor of SMI risk (P < 0.001). Further stratified analyses reinforced the link between the TyG index and the risk of SMI, demonstrating its consistent influence across diverse population subsets. Mediation analysis revealed significant effects of hypertension, diabetes, body mass index and sex on SMI risk. The overall effect sizes ranged from 1.77 to 1.95, with direct effects accounting for 52.7–99.6% and mediation effects ranging from 0.4 to 47.3%. In the general population, the TyG index as an independent predictor of SMI risk, emphasizing its importance in cardiovascular disease assessment.
Similar content being viewed by others
Introduction
Silent myocardial infarction (SMI), which often presents without obvious symptoms like chest pain or shortness of breath, is commonly overlooked or misdiagnosed, making accurate detection challenging in the general population1,2,3,4. SMI is responsible for about half of all myocardial infarctions, with prevalence rates ranging from 22 to 60%1,5,6. Because SMI has insidious characteristics, it is easy to delay treatment. Studies have revealed that mortality in patients with SMI is three times higher than that in patients with acute MI7,8,9, hinting at a potentially robust association between SMI and the elevated risk of cardiovascular incidents as well as mortality. Given the high incidence and serious outcomes of SMI, early screening and identification of high-risk populations are essential for its prevention and management.
Prior investigations have revealed that individuals with diabetes exhibit a notably elevated predisposition to SMI, with a prevalence rate as high as 44.3%10. However, a history of diabetes only reflects the clinical background and does not allow for dynamic monitoring and evaluation. The main clinical features of diabetes include impaired glucose and lipid metabolism, with insulin resistance (IR) being a key underlying factor11. Therefore, we hypothesize that IR may be a significant factor contributing to the increased risk of SMI in diabetic patients12 and could serve as an effective indicator for the early identification of SMI. However, routine monitoring of IR levels is challenging due to the difficulty of rapid quantification. Hence, the identification of straightforward markers for the dynamic evaluation of IR holds paramount importance for the timely recognition of individuals at heightened risk for SMI, facilitating early intervention and improved patient outcomes.
The triglyceride-glucose (TyG) index serves as a straightforward marker for IR. A robust association has been noted between the TyG index and IR, with the TyG index exhibiting high diagnostic precision for IR. Prior studies have reported an area under the receiver operating characteristic curve of 0.858, further substantiating its accuracy in identifying with IR13,14,15,16,17. Investigations have additionally unveiled a tight connection between the TyG index and the vulnerability to both angina and acute myocardial infarction, emphasizing its potential as a predictive marker for adverse cardiovascular outcomes18,19. Notwithstanding the aforementioned, the investigation into the nexus between the TyG index and the risk of SMI in the general population remains scant. Hence, the present study endeavors to delve into the relationship between TyG levels and SMI risk through a prospective cohort analysis, with the ultimate objective of ascertaining the potential utility of the TyG index as a discerning marker for pinpointing individuals who are predisposed to a heightened SMI risk.
Methods
Study design and participants
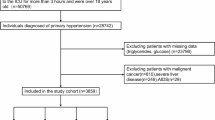
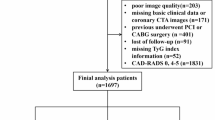
This research utilized data from the Atherosclerosis Risk in Communities (ARIC) study; the database is managed by the Biological Samples and Data Storage Information Coordinating Center under the National Heart, Lung, and Blood Institute20. The ARIC is a multicenter prospective cohort analysis in a US community-based population with the primary aim of exploring risk factors associated with cardiovascular and cerebrovascular disease. The data were collected from 15,792 residents in four communities in the United States between 1987 and 2022. Follow-up was performed every 3 to 4 years through 2022, with 10 follow-ups over 36 years. The protocol of this study underwent rigorous scrutiny and was granted approval by the ethics review boards of the collaborating community-based research institutions and the Human Ethics Committee of West China Hospital, Sichuan University (approval number 2021 [1631]). All research activities were conducted in strict adherence to the ethical guidelines outlined in the Declaration of Helsinki, ensuring the protection of participants’ rights and well-being. All participants provided written informed consent.
The study was designed as a prospective cohort study, including a community population initially enrolled in the ARIC study. The specific inclusion criteria were: (1) participants aged between 45 and 64 years, and (2) long-term residents of the study community. Participants were followed over time to observe and assess the occurrence of SMI. Exclusion criteria: (1) Lack of key indicators such as blood sugar, triglycerides, etc.; (2) Total number of dropouts. Ultimately, the study included 14,211 participants who met all the eligibility criteria and were monitored prospectively for the occurrence of new SMI events.
TyG index calculation
The TyG index was derived from baseline fasting triglyceride and plasma glucose levels. The calculation was performed using the formula: triglycerides (mg/dL) × fasting plasma glucose (mg/dL)/2, where 1 dL is equivalent to 0.1 L. TyG index measurements were divided into quartiles: Q1 (≤ 8.26), Q2 (8.26–8.62), Q3 (8.62–9.02), and Q4 (≥ 9.02). The division into quartiles was chosen to categorize the data into four equal groups, ensuring an even distribution of participants across the TyG index range.
Data collection
In the ARIC study, various data, including demographic information, vital signs, smoking and alcohol consumption status, routine blood parameters, lipid-related markers, blood glucose levels, and renal function indicators, were collected at enrollment. Follow-up assessments were conducted every 3–4 years. Additional data gathered encompassed details pertaining to lifestyle patterns, hospital admissions, medical diagnoses and therapeutic interventions, as well as the occurrence of cardiovascular occurrences, such as coronary artery disease and congestive heart failure. Hyperlipidemia was characterized by a serum triglyceride level exceeding 1.7 mmol/L, total cholesterol levels higher than 5.72 mmol/L, or low high-density lipoprotein levels below 0.9 mmol/L.
Research indicators
The main outcome of the study was the occurrence of SMI. The diagnosis of SMI is based on the detection of changes in baseline and follow-up electrocardiograms (ECGs), where the baseline ECG shows no evidence of myocardial infarction, but new Q waves, ST segment abnormalities, or other typical signs of myocardial infarction appear in subsequent follow-up ECGs. Additionally, participants must not have reported any symptoms associated with myocardial infarction, such as chest pain or shortness of breath, nor have any recorded diagnosis of myocardial infarction during the baseline and follow-up periods21,22. Electrocardiographic evidence of MI was determined based on the Minnesota Code (MC), which includes major Q/QS abnormalities (MC 1.1 or MC 1.2) or minor Q/QS abnormalities (MC 1.3) combined with major ST-T abnormalities (MC 4.1, MC 4.2, MC 5.1, or MC 5.2)21,22.
Statistical analysis
In this study, Categorical variables have been depicted through frequencies (%) and were subjected to group-wise comparisons employing the chi-squared test. Meanwhile, continuous variables are represented as means with accompanying standard deviations (X ± S) and were compared utilizing either the t-test or ANOVA. For variables exhibiting non-normal distributions, comparisons were facilitated by employing the median along with the interquartile range or resorting to the Mann-Whitney U test for statistical analysis. Furthermore, to evaluate the potential nonlinear association between the TyG index and the risk of SMI, restricted cubic spline curves were implemented. Kaplan-Meier survival analysis was used to analyze differences in cumulative survival among populations with varying SMI levels across the TyG index population. Cox proportional hazards regression models were employed to assess the relationship between varying levels of the TyG index and the risk of SMI. To further dissect this association, subgroup analyses were performed, examining the interplay between the TyG index and SMI risk across various subgroups, encompassing sex, age cohorts, body mass index (BMI) categories, smoking and drinking status, as well as the presence of hyperlipidemia, diabetes, and hypertension. Mediation analysis was also performed to investigate the indirect effects of potential mediators on the relationship between the TyG index and SMI risk. The analysis aimed to quantify the extent to which variables such as sex, BMI, hypertension, diabetes, and hyperlipidemia mediated this association. The total, direct, and indirect effects of these factors were estimated using statistical models to assess their mediating influence.The SPSS version 26.0 and R version 4.3.0 was adopted.
Results
Participant baseline demographics and clinical profiles stratified by the TyG index levels
This study included 14,211 community residents, among whom 7316 (51.48%) cases of SMI were observed during the follow-up. The participants were divided into four distinct quartiles (Q1 to Q4) according to their TyG index values: Q1 (n = 3,553), Q2 (n = 3,554), Q3 (n = 3,551), and Q4 (n = 3,553). Individuals in the higher TyG index quartiles exhibited higher age, BMI, heart rate, and severity of hypertension and diabetes, as well as increased levels of glucose, triglycerides, hemoglobin, white blood cells, platelets, neutrophils, lymphocytes, total cholesterol, low-density lipoprotein, and uric acid. Conversely, the lower TyG index quartiles (Q1 and Q2) were characterized by a higher proportion of female participants and higher rates of alcohol consumption. Additionally, these groups showed elevated levels of high-density lipoprotein and creatinine. The differences across all groups were statistically significant (P < 0.05) (Table 1).
Correlation between elevated TyG indices and SMI incidence
In the community population, individuals with elevated TyG indices showed a higher incidence of SMI. The differences in SMI incidence across the quartile groups of the TyG index were statistically significant (Fig. 1).
Correlation between the TyG index and SMI risk
Restricted cubic spline analysis demonstrated a significant positive association between increased TyG index levels and an elevated risk of SMI. Participants with higher TyG indices had a greater likelihood of developing SMI (Fig. 2).
Association between the TyG index and survival rates
Kaplan-Meier survival analysis demonstrated that individuals in the community population with higher TyG indices had the lowest cumulative survival rates for SMI events (Fig. 3).
Analysis of the TyG index and SMI risk
To evaluate the relationship between the TyG index and the risk of SMI, four distinct models were formulated, as presented in Table 2. In Model 1 (univariate Cox regression), a positive association was found, with higher TyG index quartiles (Q2, Q3, and Q4) showing progressively higher risks of SMI compared to Q1. In Model 2, after adjusting for age, sex, and BMI, though it was weaker for Q2, the positive association remained. In Model 3, after further adjusting for factors such as heart rate, alcohol consumption, smoking status, history of hypertension, and diabetes, the strength of the association was weakened, particularly for Q2 and Q3. In Model 4, after adjusting for some biochemical markers, the strength of the association reduced, with the P-value approaching non-significance. Across all models, a positive correlation was observed between higher TyG index levels and increased SMI risk. However, the strength of this association diminished as additional covariates were introduced.
Subgroup analysis
Subgroup analysis revealed that the TyG index was significantly and independently associated with the risk of SMI in the subgroups of sex, BMI, smoking, drinking, diabetes, hypertension, hyperglycemia, and hyperlipidemia (Table 3).
Effects of mediating factors
Mediation analysis showed that sex, BMI, hypertension, and diabetes significantly influenced the risk of SMI (P < 0.001). Diabetes had a total effect on the SMI risk of 1.8, with nearly equal direct and mediating effects (52.7% and 47.3%, respectively). Hyperlipidemia had the highest total effect on SMI risk, at 1.95, but its mediating effect was minimal (0.4%) and non-significant (P = 0.91). These results are detailed in Table 4.
Discussion
The present study delved into the potential association between the TyG index and the incidence of SMI within a community-based, prospective cohort design. The results underscore a direct and robust correlation between elevated TyG indices and an augmented risk of SMI, which persists as a significant predictor even subsequent to adjustments for multiple confounding factors. Notably, the TyG index emerges as an independent marker of SMI, with individuals in the highest quartile exhibiting the poorest survival outcomes in terms of SMI events. Subgroup analyses reinforce this robust association, revealing consistency across diverse demographic and clinical profiles, such as sex, age cohorts, smoking habits, diabetic status, and hyperlipidemia. Mediation analysis disentangles the underlying mechanisms, revealing diabetes and hypertension as the primary mediators of the TyG index-SMI risk relationship. Conversely, hyperlipidemia exerts its greatest influence on SMI risk through direct pathways, with minimal mediation through the TyG index. Although participants’ health status (such as smoking and diabetes) was recorded multiple times during the follow-up, other pathological processes (such as new chronic diseases, progression of comorbidities, or new medication use) may not have been fully recorded or updated, and these unmeasured changes could affect the prognosis. Despite adjusting for covariates, unmeasured factors (such as subclinical inflammation, metabolic abnormalities, or psychological factors) could still influence patient outcomes, introducing bias and thereby limiting the generalizability and causal inference of the results.
Prior investigations have established the TyG index as an independent indicator to cardiovascular disease (CVD) risk. For example, a Koreanprospective cohort study underscored the TyG index’s predictive prowess for incident CVD15. Among non-diabetic adults, an elevated TyG index emerged as a potent harbinger of ischemic heart disease, underscoring its potential as an early, preclinical marker of cardiovascular risk23. A meta-analysis of 20,403 participants across cohort studies validated the TyG index as an independent prognosticator of major adverse cardiovascular and cerebrovascular events, as well as all-cause mortality in MI patients24. An additional meta-analysis fortified this notion, revealing that a high TyG index is associated with heightened risk, severity, and poorer outcomes in coronary artery disease25. While these studies collectively underscore the TyG index’s link to diverse CVD manifestations23,26,27,28,29, a dearth of research specifically exploring its relationship with silent myocardial infarction (SMI) remains. This knowledge gap has hindered the TyG index’s broader application in comprehensive CVD risk evaluation. Our study bridges this divide by elucidating a distinct association between elevated TyG index levels and an increased SMI risk, thereby positioning the TyG index as a valuable predictive tool for SMI. These findings suggest that the TyG index could be used for early risk stratification and preventive strategies in the general population, helping to complement and enhance the accuracy of existing risk assessment tools.
The exact mechanisms through which the TyG index impacts the occurrence of SMI remain unclear. It is likely linked to metabolic and vascular disturbances caused by IR, which elevates the risk of cardiovascular events, including SMI30. First, a higher TyG index reflects more severe IR. IR leads to various metabolic disturbances that can impair myocardial blood flow, potentially resulting in SMI. Moreover, the TyG index, as a dependable marker of IR, is linked to the release of inflammatory mediators that damage endothelial cells and disrupt endothelial function. This imbalance may contribute to the formation of atherosclerotic plaques, offering a potential mechanism connecting the TyG index to the development of SMI14,31,32,33. Moreover, an elevated TyG index indicates higher levels of blood glucose and triglycerides, suggesting a disturbed metabolic state. This metabolic dysfunction, which is closely related to IR, can lead to dyslipidemia, which is another major risk factor for CVD. Therefore, the TyG index may contribute to SMI risk through multiple interrelated metabolic and inflammatory pathways.
Our research revealed that SMI occurrence was more prevalent among females, a finding consistent with those of previous studies5. In the subgroup analysis, the odds ratio (OR) for SMI in females was 1.647, significantly higher than the OR for males at 1.243 (P < 0.001). This highlights the important role that sex plays in the development of SMI, with females being at a higher risk than males. The sex disparity in SMI risk may be attributed to physiological, metabolic, and hormonal differences. In particular, reduced estrogen levels in middle-aged and older females may diminish estrogen’s effects on ion channel activities in sensory neurons and rapid pain modulation via estrogen receptors. This reduction could raise pain thresholds, making females less sensitive and more tolerant to pain than males, potentially leading to undetected SMI events34,35. This finding suggests that the TyG index could be especially useful for assessing SMI risk in females. While hypertension, diabetes, and hyperlipidemia are considered significant cardiovascular risk factors, their impact on the association between the TyG index and SMI varies considerably. In particular, the risk of SMI appears to be reduced in diabetic patients, possibly due to ongoing diabetes management that helps mitigate the risk of SMI.
Although hyperlipidemia is typically considered a risk factor for CVD, its mediating role in the relationship between the TyG index and SMI appears to be minimal. This suggests that the influence of hyperlipidemia on the risk of SMI primarily occurs through direct pathways rather than being mediated by the TyG index. However, the TyG index may play a more significant role in this context, possibly because it is closely associated with lipid metabolism disorders and effectively captures the main impact of hyperlipidemia on the risk of SMI. Other metabolic abnormalities included in the TyG index may overshadow the mediating effect of hyperlipidemia, thereby reducing its impact. These results highlight the significance of the TyG index as a comprehensive marker of metabolic disturbances and their link to SMI risk. Additional research is necessary to clarify the mechanisms and interactions between the TyG index and SMI, potentially offering new perspectives for SMI prevention and treatment.
This study faced some limitations. First, the TyG index was not consistently monitored during the follow-up period, preventing analysis of how changes in the TyG index might influence SMI risk. Secondly, the specific causes of SMI were not investigated, which limited our ability to explore how the TyG index relates to various SMI etiologies. Additionally, the study’s findings are based on a population from various communities in the United States and have not been confirmed in other geographical areas. Furthermore, the severity of the SMIs identified was not evaluated in this research. Lastly, The TyG index inherently includes measurements of glucose and triglycerides, and incorporating diabetes and hyperlipidemia as adjustment variables in the model may lead to collinearity issues, thereby affecting the independent interpretation of the association between the TyG index and SMI risk. This could potentially weaken the model’s ability to evaluate the standalone effect of the TyG index. Nonetheless, we chose to include these variables to achieve a more comprehensive control of confounding factors.
Conclusions
This prospective cohort study in a community population identified an independent association between elevated TyG indices and a higher risk of SMI. This association enables healthcare providers to formulate more specific preventive measures based on the TyG index, introducing novel strategies for early detection and intervention in cardiovascular health, with the ultimate goal of reducing the occurrence of cardiovascular events in patients.
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
Qureshi, W. T. et al. Silent myocardial infarction and long-term risk of heart failure: the ARIC study. J. Am. Coll. Cardiol. 71(1), 1–8. https://doi.org/10.1016/j.jacc.2017.10.071 (2018).
Aghdam, M. R. F., Vodovnik, A. & Sund, B. S. Correction: Sudden death associated with silent myocardial infarction in a 35-year-old man: a case report. J. Med. Case Rep. 12(1), 52. https://doi.org/10.1186/s13256-018-1613-3 (2018).
Mozaffarian, D. et al. Executive summary: heart disease and stroke Statistics–2016 update: a report from the American heart association. CIRCULATION 133(4), 447–454. https://doi.org/10.1161/CIR.0000000000000366 (2016).
Gul, Z. & Makaryus, A. N. Silent myocardial ischemia. https://doi.org/10.1080/00325481.1989.11700774 (2019).
Kolesova, M. V. & Minor, S. Silent myocardial infarction: a case report. Cureus 15(8), e43906. https://doi.org/10.7759/cureus.43906 (2023).
Zhang, Z. M. et al. Race and sex differences in the incidence and prognostic significance of silent myocardial infarction in the atherosclerosis risk in communities (ARIC) study. Circulation 133(22), 2141–2148 (2016).
Schelbert, E. B. et al. Prevalence and prognosis of unrecognized myocardial infarction determined by cardiac magnetic resonance in older adults. Jama 308(9), 890–896 (2012).
Sheifer, S. E. et al. Prevalence, predisposing factors, and prognosis of clinically unrecognized myocardial infarction in the elderly. J. Am. Coll. Cardiol. 35(1), 119–126. https://doi.org/10.1016/s0735-1097(99)00524-0 (2000).
Sigurdsson, E. et al. Unrecognized myocardial infarction: epidemiology, clinical characteristics, and the prognostic role of angina pectoris. The Reykjavik study. Ann. Intern. Med. 122(2), 96–102. https://doi.org/10.7326/0003-4819-122-2-199501150-00003 (1995).
Siddiq, M. et al. Diabetes mellitus with silent myocardial ischemia: a single-center cross-Sectional study of Karachi. Pak. J. Pharm. Res. Int. 2021, 56–60. https://doi.org/10.9734/jpri/2021/v33i29b31589 (2021).
Ginsberg, H. N. Insulin resistance and cardiovascular disease. J. Clin. Investig. 106(4), 453–458 (2000).
Gast, K. B. et al. Insulin resistance and risk of incident cardiovascular events in adults without diabetes: meta-analysis. PloS One 7(12), e52036 (2012).
Park, K. et al. Elevated TyG index predicts progression of coronary artery calcification. Diabetes Care. 42 (8), 1569–1573. https://doi.org/10.2337/dc18-1920 (2019).
Sánchez-Íñigo, L. et al. The TyG index May predict the development of cardiovascular events. Eur. J. Clin. Invest. 46 (2), 189–197. https://doi.org/10.1111/eci.12583 (2016).
Moon, J. H. et al. Triglyceride-Glucose index predicts future atherosclerotic cardiovascular diseases: a 16-Year Follow-up in a prospective, Community-Dwelling cohort study. Endocrinol. metab. 38(4), 406–417. https://doi.org/10.3803/EnM.2023.1703 (2023).
Zhao, Y. et al. Elevated triglyceride-glucose index predicts risk of incident ischaemic stroke: the rural Chinese cohort study. Diabetes Metab. 47(4), 101246. https://doi.org/10.1016/j.diabet.2021.101246 (2021).
Kurniawan, L. B. & Triglyceride-Glucose Index As, A. Biomarker of insulin resistance, diabetes mellitus, metabolic syndrome, and cardiovascular disease: a review. EJIFCC 35(1), 44–51 (2024).
Rafiee, H. et al. Association of triglyceride glucose index with cardiovascular events: insights from the Isfahan cohort study (ICS). Eur. J. Med. Res. 29(1), 135. https://doi.org/10.1186/s40001-024-01728-4 (2024).
Rokicka, D. et al. The prognostic impact of insulin resistance surrogates in patients with acute myocardial infarction with and without type 2 diabetes. Cardiovasc. Diabetol. 23(1), 147. https://doi.org/10.1186/s12933-024-02240-z (2024).
Aric Investigators. The atherosclerosis risk in communit (ARIC) study: design and objectives. Am. J. Epidemiol. 129(4), 687–702 (1989).
Cheng, Y. J. et al. Association between silent myocardial infarction and long-term risk of sudden cardiac death. J. Am. Heart Assoc. 10(1), e017044. https://doi.org/10.1161/JAHA.120.017044 (2020).
Zhang, Z. M. et al. Electrocardiographic QRS-T angle and the risk of incident silent myocardial infarction in the atherosclerosis risk in communities study. J. Electrocardiol. 50(5), 661–666. https://doi.org/10.1016/j.jelectrocard.2017.05.001 (2017).
Park, B. et al. The triglyceride-glucose index predicts ischemic heart disease risk in Koreans: a prospective study using National health insurance service data. Cardiovasc. Diabetol. 19(1), 210. https://doi.org/10.1186/s12933-020-01186-2 (2020).
Liu, H. et al. The association of triglyceride–glucose index with major adverse cardiovascular and cerebrovascular events after acute myocardial infarction: a meta-analysis of cohort studies. Nutr. Diabetes. 14(1), 39 (2024).
Liang, S. et al. Triglyceride-glucose index and coronary artery disease: a systematic review and meta-analysis of risk, severity, and prognosis. Cardiovasc. Diabetol. 22(1), 170. https://doi.org/10.1186/s12933-023-01906-4 (2023).
Hao, Q., Yuanyuan, Z. & Lijuan, C. The prognostic value of the triglyceride glucose index in patients with acute myocardial infarction. J. Cardiovasc. Pharm. T 28, 10742484231181846. https://doi.org/10.1177/10742484231181846 (2023).
Xiong, S. et al. A synergistic effect of the triglyceride-glucose index and the residual SYNTAX score on the prediction of intermediate-term major adverse cardiac events in patients with type 2 diabetes mellitus undergoing percutaneous coronary intervention. Cardiovasc. Diabetol. 21(1), 115. https://doi.org/10.1186/s12933-022-01553-1 (2022).
Wang, L. et al. Triglyceride-glucose index predicts adverse cardiovascular events in patients with diabetes and acute coronary syndrome. Cardiovasc. Diabetol. 19, 1–11 (2020).
Luo, E. et al. High triglyceride-glucose index is associated with poor prognosis in patients with acute ST-elevation myocardial infarction after percutaneous coronary intervention. Cardiovasc. Diabetol. 18(1), 150. https://doi.org/10.1186/s12933-019-0957-3 (2019).
Košuta, D. et al. The correlation between the Triglyceride-Glucose index and coagulation markers in patients with recent acute myocardial infarction. Dis. MAark. 2022, 6206802. https://doi.org/10.1155/2022/6206802 (2022).
Liu, Q. et al. Triglyceride-glucose index associated with the risk of cardiovascular disease: the Kailuan study. Endocrine 75(2), 392–399. https://doi.org/10.1007/s12020-021-02862-3 (2021).
Mao, Q. et al. The triglyceride-glucose index predicts coronary artery disease severity and cardiovascular outcomes in patients with non-ST-segment elevation acute coronary syndrome. Dis. Mark. 2019, 6891537. https://doi.org/10.1155/2019/6891537 (2019).
Alizargar, J. et al. Use of the triglyceride-glucose index (TyG) in cardiovascular disease patients. Cardiovasc. Diabetol. 19(1), 8. https://doi.org/10.1186/s12933-019-0982-2 (2020).
Aguilar, D. et al. Clinically unrecognized Q-wave myocardial infarction in patients with diabetes mellitus, systemic hypertension, and nephropathy. Am. J. Cardiol. 94(3), 337–339 (2004).
Pride, Y. B., Piccirillo, B. J. & Gibson, C. M. Prevalence, consequences, and implications for clinical trials of unrecognized myocardial infarction. Am. J. Cardiol. 111(6), 914–918 (2013).
Acknowledgements
We would like to thank all the participants of this project.
Funding
This work was supported by the National Natural Science Foundation of China (72374148), the Sichuan Science and Technology Program (2023YFS0027, 2023YFS0240, 2023NSFSC1652, 2023YFS0074), and the Sichuan Provincial Health Commission (ZH2024-101, ZH2024-102, ZH2024-108).
Author information
Authors and Affiliations
Contributions
RL, and MT conceived the study design. MD, DL, YL, and MT collected the epidemiological and clinical data. MD, DL and YL summarized the data and performed the statistical analysis. MD, QZ, WZ, and YG interpreted the data and drafted the manuscript. YZ, and LR participated in the design of the study, acquired the data and helped to revise the manuscript. All the authors have accepted responsibility for the entire content of this submitted manuscript and approved submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable. This study utilized data from publicly available databases, which do not contain any identifiable individual person’s data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dai, M., Li, D., Yu, J. et al. Association between the triglyceride-glucose index and silent myocardial infarction in the general population. Sci Rep 15, 8571 (2025). https://doi.org/10.1038/s41598-025-92779-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-92779-y